Abstract
Diabetic foot ulcer (DFU) is a severe complication of diabetes mellitus (DM). Patients with DFU have increased mortality and morbidity as well as decreased quality of life (QoL). The present scoping review aims to study the social issues of diabetic foot. Following PRISMA guidelines, the review was conducted in two databases (Scopus and Pubmed) with the use of the following keywords: “social aspects and diabetic foot”, “social characteristics and diabetic foot”, “social issues and diabetic foot”, “demographic profiles and diabetic foot”, “social determinants and diabetic foot”, “social capital and diabetic foot”, “social characteristics and gender and diabetic foot”, “social profiles and diabetic foot”, “social relationships and diabetic foot” and “social risk and diabetic foot”, from July to August 2021. Predetermined exclusion and inclusion criteria were selected. Forty-five studies (quantitative and qualitative) were eligible for inclusion in this review. Gender problems, socioeconomic status, social capital, and medical problems were the most important negative variables for diabetic foot. All the included variables reveal that the social impact of diabetic foot is the most important factor for management and prevention, in terms of aggravation and more, of the diabetic foot.
1. Introduction
Diabetic foot ulcer (DFU) is a complication of diabetes mellitus (DM). The prevalence of diabetic foot in the world is about 6%, and it is estimated that approximately one out of every six diabetic individuals will experience a foot ulcer in their life. In those individuals, DFU increases mortality and morbidity as well as the risk of going through amputation. Patients with DFU, especially if it does not heal or recurs, report poor quality of life (QoL) (Polikandrioti et al. 2020). DFU is associated with frequent hospitalization and rising costs of treatment (Polikandrioti et al. 2020; Zhang et al. 2021; Reis et al. 2020). DFU pathophysiology is due to neuropathy, trauma, and peripheral artery occlusive disease (PAOD) (Misliza and Ayu 2009; Korzon-Burakowska and Dziemidok 2011). Peripheral neuropathy, including both sensory and motor fibers as well as autonomic nerve fibers, is often an underdiagnosed complication in patients with diabetes. Diabetic patients with neuropathy have a considerably increased risk of developing ulceration compared to patients who do not have this complication (Korzon-Burakowska and Dziemidok 2011). Neuropathies in diabetic patients occur in one out of every two patients. Motor nerve fiber dysfunction leads to a deformity of the foot that later results in callus formation because of altered weight-bearing. Furthermore, sensory neuropathy causes a lack of pain sensation in the foot, making the patient unaware of the trauma (Korzon-Burakowska and Dziemidok 2011; Kuang et al. 2021). The ulcers in diabetic patients usually occur on the forefoot, and they are usually painless due to the neuropathy. Peripheral artery occlusive disease worsens the diabetic foot ulcer condition and increases the risk of amputation because of the impaired healing condition (Korzon-Burakowska and Dziemidok 2011). Banal skin injuries, such as those caused by footwear or by cutting nails, are often the triggering factors in developing DFU. Diabetic patients with neuropathy develop a foot deformity that leads to increased skin pressure while walking, which may be responsible for the first trauma in developing a DFU (Korzon-Burakowska and Dziemidok 2011). The presence of diabetic foot ulcers has already been assessed as a factor that negatively impacts the quality of life in diabetic patients (Goodridge et al. 2006). The DFU condition causes negative effects that concern social situations as well (Goodridge et al. 2005). There is a study suggesting that strong social support could improve the patient’s daily life skills, their medical compliance, reduce depression and anxiety, and enhance the patient’s confidence in overcoming the disease (Yan et al. 2021). Lower limb amputation, which not infrequently follows the DFU condition, has a negative impact on these patients’ lives (Pedras et al. 2020) and puts them at risk of losing their independence, with social, psychological, and economic effects (Shankar et al. 2020). The degree of depression in these patients decreases as family or friend support increases (Yildiz and Aşti 2015). There are differences based on gender and age; specifically, younger age and female gender, on average, are associated with a lower grade of spirituality, while a lower hope of healing is associated with older age (Salomé et al. 2015). Moreover, the male gender is characterized by worse foot complications, while the female gender has been found to be in worse general health and has more adverse attitudes towards therapeutic shoes. Female patients’ concerns should be paid more attention by clinicians (Jarl et al. 2019). Women are more active in prevention and self-care, and they try to adapt to the situation, while men more frequently seek help for acute problems, and they have a more pessimistic view of the future (Hjelm et al. 2002). Socio-economic status has been found to be a factor in the increased incidence of lower limb amputations (Amin et al. 2014). In more detail, it has been shown that people with lower-limb complications who live in rural areas and have a greater social disadvantage have a 50% higher likelihood of lower limb amputation (Perrin et al. 2019).
2. Materials and Methods
Figure 1 presents a flowchart of the scoping review and article selection process used in this study, which adhered to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines.
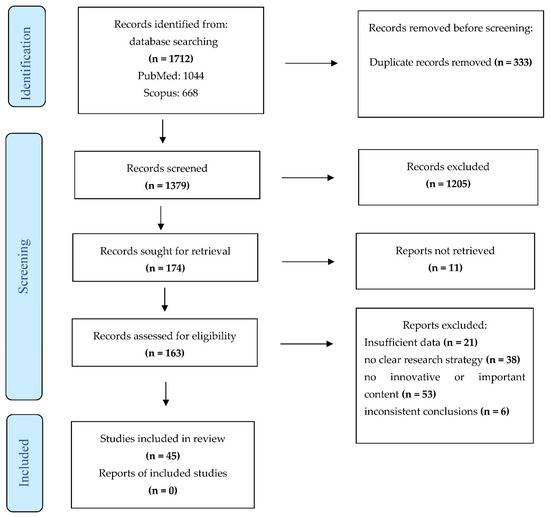
Figure 1.
PRISMA flow diagram.
3. Eligibility Criteria
We decided to use all articles with specific information, clear social variables, and the correct definition, epidemiology, pathogenesis, etiology, classification, indicators, and scale used for diabetic foot. Trials, reviews, and original articles were used in this review. Only English publications were considered. We included quantitative and qualitative studies. We excluded studies with these exclusion criteria: Not English language; too specific or articles not related to social aspects; articles that study specific populations or social aspects; not responding properly to our research question; and insufficient data.
4. Search Strategy
We searched for all studies published from 2000 to 2021 using two databases, Scopus and PubMed. These databases were preferred because they contain significant elements from the biomedical sciences, psychology, and sociology literature. The following keywords were applied in the databases during the literature search: “social aspects and diabetic foot” or “social characteristics and diabetic foot” or “social issues and diabetic foot” or “demographic profiles and diabetic foot” or “social determinants and diabetic foot” or “social capital and diabetic foot” or “social characteristics and gender and diabetic foot” or “social profiles and diabetic foot” or “social relationships and diabetic foot” or “social risk and diabetic foot”. The research was restricted to human studies published in the English language.
5. Data Charting Process
Two of the authors (the first and last) jointly developed a data extraction tool to determine which variables to extract. Following this, two authors (the second and the second-to-last) independently extracted data from all the studies, discussed the results, and continuously updated the data extraction tool. However, if there was any doubt regarding an article, it was discussed by the authors and a consensus was reached. We extracted the data from the selected studies according to a standardized data extraction form.
6. Data Items
We abstracted data on article characteristics (e.g., author(s), year of publication, country of origin), the aim of the paper, research design, participants (e.g., sample size), concept (e.g., assessment method, questionnaires used, and their authors alongside the time of assessment), context, and key findings, including statistical significance for quantitative data and themes for qualitative data. This phase was made possible using the Downs and Black quality checklist (Downs and Black 1998). It is a system used to validate, with a strong methodology (National Collaborating for Methods and Tools 2010), the studies used for this review.
7. Synthesis of Results
Synthesis of the information extracted, identifying patterns, and similarities and differences in the variables examined in this scoping review was performed.
8. Results
The literature search retrieved 1712 results. Of the 1712 articles we identified in our search, we screened 1379 titles and abstracts of articles. Out of these, we reviewed 163 full-text articles assessed for eligibility and included 45 studies in our analysis.
9. Selection and Characteristics of Sources of Evidence
The selection process is summarized in the PRISMA flow chart. Initially, three authors were involved in title and abstract screening; after these authors had extracted all the search results, duplicates were removed. In the second step, we screened all titles and abstracts for relevance to decide whether the full paper should be obtained. In the end, a full-text screening of all relevant articles was performed to exclude studies that did not meet the inclusion criteria. Decisions on the inclusion of studies and the interpretation of data were resolved by discussion among the reviewers. Specifically, the study selection was carried out in different phases. Data from all studies meeting the inclusion criteria were extracted and tabulated. We decided to use 45 articles based on the following variables: (1) Insufficient data; (2) no clear research strategy; (3) no innovative or important content; and (4) inconsistent conclusions. Table 1 shows the principal characteristics of the included studies.

Table 1.
Characteristics of included studies.
10. Results of Individual Sources of Evidence
The analysis identified a variegated series of problems concerning the social, and therefore relational, aspects of diabetic foot. In particular, after careful analysis of the selected literature, in the case of diabetic foot, social issues are many because it changes the quality of life of those who have this complication. Specifically, the macro-social issues in this diabetic complication concern gender, socioeconomic status, the social capital of the patients, the mutation of lifestyle, and the quality of life (Lael-Monfared et al. 2019). In summary, many studies have shown how social factors are associated with diabetic foot and the medical problems related to this complication.
The Downs and Black Scale used in this review evidenced the appropriate design for qualitative and quantitative studies included according to the following issues: Reporting, external validity, internal validity (bias and confounding), and statistical power.
10.1. Gender Variables and Diabetic Foot
Many studies revealed that there is a gender difference in diabetic foot ulcers. In fact, a study by Reis et al. states that there is a higher prevalence of diabetes mellitus in women. However, in men, there is a higher risk of developing diabetic foot and its complications (Reis et al. 2020). A study by Pedras et al. states that diabetic foot ulcers are more prevalent in male patients (Pedras et al. 2020). Lo et al. report that there is a higher proportion of male patients around the world with DFU and consider the increased physical work of males a possible hypothesis for the gender difference (Lo et al. 2021). A study by Leese et al. analyzed certain risk factors and revealed that the male gender and other factors are associated with major and minor amputations (Leese et al. 2013). Sheen et al. reported that the male sex may be associated with a higher risk of lower limb amputations because the prevalence of peripheral arterial disease was higher in men than in women, and it is known that peripheral arterial disease is an important risk factor for amputation (Sheen et al. 2018). Perrin et al. determined that men’s access to health services is less compared to women because they think they have less time for their own health (Perrin et al. 2019). Goodridge et al. studied risk factors for ulcer development, and, moreover, the most important risk factor was the male gender (Goodridge et al. 2006). As stated by Iversen et al., significant predictors of DFU are male gender and older age (Iversen et al. 2015). Herber et al. reported a gender analysis in which it was revealed that female patients seemed to have fewer complaints regarding pain compared to male patients (Herber et al. 2007). A study by Jarl et al. reports that women had worse general health and a negative attitude towards therapeutic shoes, but nevertheless, men had worse foot complications (Jarl et al. 2019). As stated by Amin et al., men have a greater impact on socio-economic status (Amin et al. 2014). A study by Wu et al. analyzed that males might have a higher willingness to pay and spend much more attention on their healthcare (Wu et al. 2018) and Ahmad Sharoni et al. stated that, in males, foot self-care behavior was higher than in females (Ahmad Sharoni et al. 2017). As Al Ayed et al. report, in Saudi Arabia, the prevalent constraints of gender segregation and the restrictions imposed by the male guardianship system negatively affect the health-related QoL of females, and for this reason, they have larger ulcer sizes, higher frequencies of unhealed ulcers, and advanced Wagner grades (Al Ayed et al. 2020). A study by Zhang et al. reports that there are certain demographic factors associated with increased odds of 30-day readmission, such as female sex, black race (vs. white), older age, and others (Zhang et al. 2021). There are some studies that claim there is no difference between genders, such as the study by Goodridge et al. that reports that between unhealed and healed ulcer groups, there were no significant differences in gender distribution, age, and general health self-rating (Goodridge et al. 2005), and a study by Salameh et al. reported that there are no differences between DFU and non-DFU groups in terms of gender, as well as other factors (Salameh et al. 2020). Regarding marital status, Pedras et al. analyzed that almost all patients were married, and the main caregiver reported being the patient’s spouse or an offspring. It shows the importance of the role of the family, which seems to be responsible for helping the patient take care of her/his feet (Pedras et al. 2020).
10.2. Socioeconomic Status and Diabetic Foot
First of all, socioeconomic status (SES) is a complicated and multifactorial index that allows one to understand the socio-economic position of an individual based on different sub-categories of indicators (Zhang et al. 2021). In diabetic patients, this index is related to DFU (Hicks et al. 2018). Many studies, in particular, demonstrated how much worse healthcare outcomes are in patients with a socioeconomic disadvantage (Hicks et al. 2018; Tatulashvili et al. 2020). It is clear why this happens. The lower the socio-economic availability, the lower the access to treatment and therefore the possibility of preventing, or at least limiting, the aggravation of complications (Tatulashvili et al. 2020); in particular, SES is important in diabetic patients as a risk factor for different kinds of diabetic complications. Many of the articles report these data. In this regard, for example, the connection between socioeconomic positions and the prevalence of diabetes is very strong (De Silva et al. 2016): Low SES is associated with unhealthy attitudes, low access to treatment, abnormal activity in care, and a high number of diabetes complications. SES appears to be particularly associated with a higher proportion of microvascular pathologies analyzed among high-socioeconomic patients as well as a higher proportion of macrovascular illness, as compared to lower socioeconomic groups (De Silva et al. 2016). A final result that appears interesting concerns the relationship between education and SES: Low access to the care system, dietary, and low hygiene rules (Lamchahab et al. 2011). In this way, SES is very important because it is linked to other social variables. Therefore, the economic burden of diabetic foot can be seen at the national level, within healthcare systems, and, perhaps most dramatically, at the parental and personal level (Tatulashvili et al. 2020; De Silva et al. 2016).
10.3. Quality of Life and Social Capital
Complications in diabetic patients are related to the quality of life (Nabuurs-Franssen et al. 2005). In particular, the QoL changes because sometimes this disease causes amputations, and mobility becomes very difficult. The role, in particular, of foot amputations on health-related QoL in patients with diabetes mellitus is very important (Nabuurs-Franssen et al. 2005). In particular, qualitative approaches have demonstrated through many observations that diabetic foot complications have a dangerous negative social and mental aftermath (De Silva et al. 2016). These dimensions are the main components of the quality of life. Furthermore, many studies have shown how QoL, as an indicator, is a dependent variable (Polikandrioti et al. 2020; Al Ayed et al. 2020; Nabuurs-Franssen et al. 2005; Jaksa and Mahoney 2010). In this case, the most important result concerns an early exit from the world of work, with an early exit rate that ranges between 50% and 79% of cases (Nabuurs-Franssen et al. 2005). With this variable, there is another impact on the quality of life in diabetic people, that is, body image changes. In fact, there are many negative psychological and sociological effects on patients with diabetes because many complications are permanent, and for this reason, they change the anatomical and functional activity of the body (Nurhikmah et al. 2019; Salomé et al. 2016). In addition, according to one study, approximately 56.7% (Nurhikmah et al. 2019) of diabetic patients have a negative body image. This variable is very important for the social impact of diabetic foot because the body image of diabetic patients is an important social element for all relations. In fact, all variables about which we have spoken are related to the ability of someone who has diabetes to maintain or create social relations. More accurately, we are talking about the concept of social capital, which was used for the first time in sociology and explains the set of relationships and networks available to an individual (Lochner et al. 1999). Nowadays, this concept is linked to the health of all people (Kawachi and Kennedy 1997; Kawachi et al. 1997a, 1997b). In particular, in diabetic patients, as in all people with chronic diseases, social capital may be reduced (Coleman 1988, 1990; Putnam 1993a, 1993b, 2020). In this way, a diabetic person is more likely to be alone; in particular, qualitative studies have demonstrated that individuals with diabetic foot have more difficulty relating and sharing their illness experiences with friends or parents (Vedhara et al. 2012). Furthermore, low social capital is associated with poorer health conditions, which can be related to ulceration risk (Vedhara et al. 2012). This is a significant problem for those who live with a diabetic person because it reduces social support. Social support is an important component of social capital, and it is a personal prevention factor during a stressful health-related experience and may be necessary for the patient’s ability to accept and cohabitate. Matricciani et al., for example, showed the association between social capital and better foot self-care, concerning the positive role of large social capital and self-care behaviors (Matricciani and Jones 2015). What has been said so far is strictly related to the cultural sphere of reference. It is important because knowledge of the sociocultural imagination of diabetic foot is important for understanding the pathological process and the development of pharmacological and care approaches (Lopes et al. 2021).
10.4. Medical Consequences and Diabetic Foot
Regarding the medical consequences of DFU, we can consider many disorders. Pain is associated with a worsening condition both in the psychological and physical spheres, because in the presence of this symptom, patients are not adherent to foot self-care. Therefore, preventive multidisciplinary interventions are required when pain is present (Pedras et al. 2020). Amputations and other surgical procedures may be necessary after aggravation of the condition and are associated with a lower health-related QoL (Polikandrioti et al. 2020; Reis et al. 2020; Korzon-Burakowska and Dziemidok 2011; Rerkasem 2011; Ragnarson Tennvall and Apelqvist 2000). Ulcers have both a predictive role and consequences for DFU and are associated with a low quality of life (Polikandrioti et al. 2020; Korzon-Burakowska and Dziemidok 2011; Perrin et al. 2019; Rerkasem 2011; Ragnarson Tennvall and Apelqvist 2000; Meijer et al. 2001; Elkhider et al. 2021; Fejfarová et al. 2014). Decreased physical mobility is an evident consequence of the physical restrictions imposed by DFU or its risk factors, and it is certainly associated with a low quality of life. Particular attention should be paid to patient mobility in these patients, recommending activities such as physical training (Polikandrioti et al. 2020; Ragnarson Tennvall and Apelqvist 2000; Meijer et al. 2001). Mental disorders play an important role in DFU patients. Depression is considered both a risk factor and a clinical consequence. Depression is present in DFU patients, particularly after ulceration, determining poor compliance in the successive healing steps. For these patients, social support should be considered. As a risk factor, depression is associated, together with anxiety, with poor compliance with glycemic control, and, consequently, it has negative effects on future wound healing, determining a worse condition (Polikandrioti et al. 2020; Iversen et al. 2015; Salomé et al. 2016; Vedhara et al. 2012; Elrayah-Eliadarous et al. 2017). Sleep disorders are considered consequences of the negative effects of DFU on the psychological sphere (Salomé et al. 2016). Stress and suicidal tendencies are possible consequences of the chronicity of this condition (Goodridge et al. 2006; Iversen et al. 2015). Neuropathy, which is associated with poor glycemic control and is considered a risk factor for DFU, together with angiopathy, is a determinant of a low grade of mobility (Korzon-Burakowska and Dziemidok 2011; Perrin et al. 2019; Lo et al. 2021; Salameh et al. 2020; Rerkasem 2011; Meijer et al. 2001; Fejfarová et al. 2014). Some conditions determined by low compliance with glycemic control are considered important risk factors, such as retinopathy (Lo et al. 2021; Al Ayed et al. 2020; Elkhider et al. 2021), foot sensory loss (Salameh et al. 2020), and nephropathies (Lo et al. 2021; Salameh et al. 2020; Elkhider et al. 2021). In addition, the presence of foot calluses, together with hypertension (Lo et al. 2021; Fejfarová et al. 2014), dyslipidemia, heart diseases (Lo et al. 2021), Charcot osteoarthropathy (Korzon-Burakowska and Dziemidok 2011), and infections (Korzon-Burakowska and Dziemidok 2011; Perrin et al. 2019) are considered independent risk factors.
10.5. Main Indicators
An interesting result achieved in this review consists of the attempt to systematize the indicators mostly used in the study of the relationship between diabetic foot and social aspects. For these reasons, they are summarized in Table 2.

Table 2.
Main indicators.
11. Discussion and Summary of Evidence
The aim of our review was to analyze the social aspects of diabetic foot. This meant studying complex groups of social variables. In fact, diabetes, and in particular, diabetic foot, is a disease condition that is particularly long-standing and difficult to manage. First, by analyzing the literature available on the subject, it was possible to detect a generalized superficial view of the social factors in question. In part, this is because multidisciplinary knowledge is not widely adopted, especially the sociological approach. However, the link between social issues and diabetes complications, in particular a low level of SES, is linked to diabetic complications (Tatulashvili et al. 2020). Adverse social conditions are dangerous not only for the patients but also for their parents (Elrayah-Eliadarous et al. 2017). This is a significant problem because the social capital of diabetics is reduced and the probability of aggravating their disease state increases (Jaksa and Mahoney 2010). In particular, the increasing incidence of diabetic complications is related to the quality of life of the population (Jaksa and Mahoney 2010). The correlation between all these variables has a further impact on the QoL of these subjects: They change their social life, they do not work, and they do not accept their body image. It is clear that the medical-only approach is not enough to improve the lives of these people. Another element that we have observed concerning the type of studies used is analyzing the social problems due to diabetic foot. As Pedras et al. (2020) asserted, there are many scientific studies that prove that not only clinical variables but also socio-demographic factors are important in the process of diabetic foot ulceration. However, while there are many quantitative studies, they are without deep analyses of the state and subjective experience of the illness; this condition, in fact, is possible to study from a qualitative approach. In this way, it is possible to detect what happens in the life and body of a diabetic person, and there is, indeed, a significant change in the individual’s life, according to Salomé et al. (2016): Movement, sorrow, sleep problems, exudate, strong smells, pruritus, and work problems. All this leads to problems with social acceptance (Tan et al. 2019). Another social problem is the relationship between diabetic foot and gender: There is evidence that shows women have a higher probability of developing diabetes and its most significant complications. Furthermore, gender plays an important role in the beliefs about health and illness (Hjelm et al. 2002). Jarl et al. showed how men have a greater aptitude for therapeutic approaches, such as therapeutic footwear, than women (Jarl et al. 2019). Gender, as demonstrated by the research carried out by Amin et al. (2014), is also related to SES, and is “greater among men (adjusted Q1:Q5 hazard ratio 1.41, 95% CI 1.30–1.54; P < 0.0001 for all male gender–socio-economic status interactions) than women (hazard ratio 1.20, 95% CI 1.06–1.36). Overall, the incidence of lower extremity amputation was higher among men than women (hazard ratio for men vs women: 1.87, 95% CI 1.79–1.96), with the greatest disparity between men in the lowest socio-economic status category and women in the highest (hazard ratio 2.39, 95% CI 2.06–2.77 and hazard ratio 2.30, 95% CI 1.97–2.68, for major and minor amputation, respectively)”. Besides, medical problems are linked to a high cost for the health economy (Amin et al. 2014; Al Ayed et al. 2020). In this way, health inequality is very high. In fact, there is a high link between the economic burden and adverse social and medical problems in people with diabetic foot (Elrayah-Eliadarous et al. 2017). Moreover, all these problems are linked to the cost of the healthcare system and parents of people with diabetic foot. Therefore, because diabetic foot is associated with comorbidities and complications, it has a substantial effect on the cost of care (Lael-Monfared et al. 2019; Sheen et al. 2018; Elrayah-Eliadarous et al. 2017). The economic and social burdens are higher for diabetic patients with an associated comorbid condition than for those with only diabetes (Elrayah-Eliadarous et al. 2017).
12. Limitations
This review has important limitations. All the articles included were written in English. Many studies that met the criteria have a low level of evidence. Most studies used a sample method. It is not possible to generalize the presented outcomes. The different kinds of sociological and statistical instruments used in the studies vary, and this is another limitation.
13. Conclusions and Recommendations
This review shows that people’s daily, social, and personal lives, as well as their participation in several activities, were affected when diabetic patients presented with DFU. DFU can affect QoL, influencing social, psychological, physical, and economic aspects.
Moreover, this review deeply and systematically analyzed not only social aspects but also the main sociological indicators, which may be effectively used in research practice and sociological management of DFU.
Therefore, it is pivotal that healthcare professionals realize that a holistic approach is required to assess the overall impact of DFU to deliver effective treatment and care.
Author Contributions
Conceptualization, D.C., N.I., and R.S.; methodology, D.C., N.I., and R.S.; validation, D.C., N.I., F.C., N.G., A.S., A.A., L.S., M.A., U.M.B., and R.S.; formal analysis, D.C., N.I., M.A., U.M.B., and R.S.; data curation, D.C., N.I., F.C., N.G., A.S., A.A., L.S., M.A., U.M.B., and R.S.; writing—original draft preparation, D.C., N.I., F.C., N.G., A.S., A.A., L.S., M.A., U.M.B., and R.S.; writing—review and editing, D.C., N.I., M.A., U.M.B., and R.S.; visualization, N.I., F.C., N.G., A.S., A.A., L.S., M.A., U.M.B., and R.S.; supervision, D.C., N.I., and R.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
Any of the information present in this study can be obtained from the authors on request.
Conflicts of Interest
There are no competing interests to declare.
References
- Ahmad Sharoni, Siti K., Mohamed N. Mohd Razi, Nor F. Abdul Rashid, and Yusuf E. Mahmood. 2017. Self-efficacy of foot care behaviour of elderly patients with diabetes. Malaysian Family Physician 12: 2–8. [Google Scholar] [PubMed]
- Al Ayed, Mousab, Mutasem Ababneh, Asirvatham Alwin Robert, Nasser Al Misfer, Maria Cruz, Hesiel C. Austria, and Mohamed Al Dawish. 2020. Factors Associated with Health-Related Quality of Life in Patients With Diabetic Foot Ulcer: A Cross-Sectional Study From Saudi Arabia. Cureus 12: e8658. [Google Scholar] [CrossRef] [PubMed]
- Amin, Leila, Baiju R. Shah, Arlene S. Bierman, Lorraine L. Lipscombe, Caixia F. Wu, Denise S. Feig, and Gillian L. Booth. 2014. Gender differences in the impact of poverty on health: Disparities in risk of diabetes-related amputation. Diabetic Medicine 31: 1410–17. [Google Scholar] [CrossRef]
- Coleman, James S. 1988. Social capital in the creation of human capital. American Journal of Sociology 94: S95–S120. [Google Scholar] [CrossRef]
- Coleman, James S. 1990. Foundations of Social Theory. Cambridge: Harvard University Press. [Google Scholar]
- De Silva, Ambepitiyawaduge P., Sudirikku H. De Silva, Rashan Haniffa, Isurujith K. Liyanage, Saroj A. Jayasinghe, Prasad Katulanda, Chandrika N. Wijeratne, Sumedha Wijeratne, and Lalini C. Rajapakse. 2016. A survey on socioeconomic determinants of diabetes mellitus management in a lower middle income setting. International Journal for Equity in Health 15: 74. [Google Scholar] [CrossRef]
- Downs, Sara H., and Nick Black. 1998. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. Journal of Epidemiology and Community Health 52: 377–84. [Google Scholar] [CrossRef]
- Elkhider, Alaa, Ahmed O. Almobark, Safaa Badi, Hanan Tahir, Azza Ramadan, Abbas A. Khalil, Elamin Elshaikh, and Mohamed H. Ahmed. 2021. Risk factors associated with lower extremity amputation in Sudanese individuals with diabetes: The need for improvement in primary health care system. Journal of Family Medicine and Primary Care 10: 985–90. [Google Scholar] [CrossRef]
- Elrayah-Eliadarous, Hind A., Claes G. Östenson, Mohammed Eltom, Pia Johansson, Vibeke Sparring, and Rolf Wahlström. 2017. Economic and social impact of diabetes mellitus in a low-income country: A case-control study in Sudan. Journal of Diabetes 9: 1082–90. [Google Scholar] [CrossRef]
- Fejfarová, Vladimíra, Alexandra Jirkovská, Eva Dragomirecká, Frances Game, Robert Bém, Michal Dubský, Veronika Wosková, Marta Křížová, Jelena Skibová, and Stephanie Wu. 2014. Does the diabetic foot have a significant impact on selected psychological or social characteristics of patients with diabetes mellitus? Journal of Diabetes Research 2014: 371938. [Google Scholar] [CrossRef] [PubMed]
- Goodridge, Donna, Elly Trepman, and John M. Embil. 2005. Health-related quality of life in diabetic patients with foot ulcers: Literature review. Journal of Wound, Ostomy, and Continence Nursing 32: 368–77. [Google Scholar] [CrossRef]
- Goodridge, Donna, Elly Trepman, Jeff Sloan, Lorna Guse, Laurel A. Strain, John McIntyre, and John M. Embil. 2006. Quality of life of adults with unhealed and healed diabetic foot ulcers. Foot & Ankle International 27: 274–80. [Google Scholar] [CrossRef]
- Herber, Oliver R., Wilfried Schnepp, and Monika A. Rieger. 2007. A systematic review on the impact of leg ulceration on patients’ quality of life. Health and Quality of Life Outcomes 5: 44. [Google Scholar] [CrossRef] [PubMed]
- Hicks, Caitlin. W., Joseph K. Canner, Nicolas Mathioudakis, Ronald L. Sherman, Kathryn Hines, Christopher Lippincott, James H. Black III, and Christopher J. Abularrage. 2018. Neighborhood socioeconomic disadvantage is not associated with wound healing in diabetic foot ulcer patients treated in a multidisciplinary setting. Journal of Surgical Research 224: 102–11. [Google Scholar] [CrossRef] [PubMed]
- Hjelm, Katarina, Per Nyberg, and Jan Apelqvist. 2002. Gender influences beliefs about health and illness in diabetic subjects with severe foot lesions. Journal of Advanced Nursing 40: 673–84. [Google Scholar] [CrossRef] [PubMed]
- Iversen, Marjolein M., Grethe S. Tell, Birigitte Espehaug, Kristian Midthjell, Marit Graue, Berit Rokne, Line I. Berge, and Truls Østbye. 2015. Is depression a risk factor for diabetic foot ulcers? 11-years follow-up of the Nord-Trøndelag Health Study (HUNT). Journal of Diabetes and Its Complications 29: 20–25. [Google Scholar] [CrossRef]
- Jaksa, Peter J., and James L. Mahoney. 2010. Quality of life in patients with diabetic foot ulcers: Validation of the Cardiff Wound Impact Schedule in a Canadian population. International Wound Journal 7: 502–7. [Google Scholar] [CrossRef]
- Jarl, Gustav, John Alnemo, Roy Tranberg, and Lars O. Lundqvist. 2019. Gender differences in attitudes and attributes of people using therapeutic shoes for diabetic foot complications. Journal of Foot and Ankle Research 12: 21. [Google Scholar] [CrossRef]
- Kawachi, Ichiro, and Bruce P. Kennedy. 1997. Health and social cohesion: Why care about income inequality? BMJ (Clinical Research Ed.) 314: 1037–40. [Google Scholar] [CrossRef] [PubMed]
- Kawachi, Ichiro, Bruce P. Kennedy, and Kimberly Lochner. 1997a. Long live community: Social capital as public health. The American Prospect 35: 56–59. [Google Scholar]
- Kawachi, Ichiro, Bruce P. Kennedy, Kimberly Lochner, and Deborah Prothrow-Stith. 1997b. Social capital, income inequality, and mortality. American Journal of Public Health 87: 1491–98. [Google Scholar] [CrossRef]
- Korzon-Burakowska, Anna, and Piotr Dziemidok. 2011. Diabetic foot—The need for comprehensive multidisciplinary approach. Annals of Agricultural and Environmental Medicine 18: 314–17. [Google Scholar] [PubMed]
- Kuang, Dan, Danfeng F. Gu, Hong Cao, Qinfang F. Yuan, Zhixia X. Dong, Dan Yu, and Xiaoming M. Shen. 2021. Impacts of psychological resilience on self-efficacy and quality of life in patients with diabetic foot ulcers: A prospective cross-sectional study. Annals of Palliative Medicine 10: 5610–18. [Google Scholar] [CrossRef] [PubMed]
- Lael-Monfared, Elahe, Hadi Tehrani, Zahara E. Moghaddam, Gordon A. Ferns, Maryam Tatari, and Alireza Jafari. 2019. Health literacy, knowledge and self-care behaviors to take care of diabetic foot in low-income individuals: Application of extended parallel process model. Diabetes & Metabolic Syndrome 13: 1535–41. [Google Scholar] [CrossRef]
- Lamchahab, Fatima Z., Nadia El Kihal, Ibtissam Khoudri, Abdelmjid Chraibi, Badreddine Hassam, and Mohamed Ait Ourhroui. 2011. Factors influencing the awareness of diabetic foot risks. Annals of Physical and Rehabilitation Medicine 54: 359–65. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Leese, Graham P., Zhiqiang Feng, Robert M. Leese, Chris Dibben, and Alistair Emslie-Smith. 2013. Impact of health-care accessibility and social deprivation on diabetes related foot disease. Diabetic Medicine 30: 484–90. [Google Scholar] [CrossRef] [PubMed]
- Lo, Zhiwen J., Naren K. Surendra, Akshar Saxena, and Josip Car. 2021. Clinical and economic burden of diabetic foot ulcers: A 5-year longitudinal multi-ethnic cohort study from the tropics. International Wound Journal 18: 375–86. [Google Scholar] [CrossRef]
- Lochner, Kimberly, Ichiro Kawachi, and Bruce P. Kennedy. 1999. Social capital: A guide to its measurement. Health & Place 5: 259–70. [Google Scholar] [CrossRef]
- Lopes, Geysa, Isaura Rolim, Renata S. Alves, Talitha Pessoa, Evanira R. Maia, Maria Lopes, Ana Morais, and R. Queiroz. 2021. Social representations on diabetic foot: Contributions to PHC in the Brazilian Northeast. Representações sociais sobre pé diabético: Contribuições para Atenção Primária à saúde no Nordeste brasileiro. Ciencia & Saude Coletiva 26: 1793–803. [Google Scholar] [CrossRef]
- Matricciani, Lisa, and Sara Jones. 2015. Who cares about foot care? Barriers and enablers of foot self-care practices among non-institutionalized older adults diagnosed with diabetes: An integrative review. The Diabetes Educator 41: 106–17. [Google Scholar] [CrossRef]
- Meijer, Jan W., Jan Trip, Sonia M. Jaegers, Thera P. Links, Andrew J. Smits, Johan W. Groothoff, and Willem H. Eisma. 2001. Quality of life in patients with diabetic foot ulcers. Disability and Rehabilitation 23: 336–40. [Google Scholar] [CrossRef]
- Misliza, Ahmad, and Silvi M. Ayu. 2009. Sociodemographic and lifestyle factors as the risk of diabetic foot ulcer in the university of malaya medical centre. Journal of Health and Translational Medicine 12: 15–21. [Google Scholar]
- Nabuurs-Franssen, Marrigje H., Maya S. Huijberts, Arie C. Nieuwenhuijzen Kruseman, Jan Willems, and Nicolaas C. Schaper. 2005. Health-related quality of life of diabetic foot ulcer patients and their caregivers. Diabetologia 48: 1906–10. [Google Scholar] [CrossRef] [PubMed]
- National Collaborating for Methods and Tools. 2010. Quality Checklist for Health Care Intervention Studies. Hamilton: McMaster University. Available online: http://www.nccmt.ca/resources/search/9;2008 (accessed on 23 March 2022).
- Nurhikmah, Lia, Dewi Gayatri, and Tuti Nuraini. 2019. Body image related to quality of life diabetic ulcer patients. Enfermeria Clinica 29: 373–78. [Google Scholar] [CrossRef]
- Pedras, Susana, Estela Vilhena, Rui Carvalho, and Maria G. Pereira. 2020. Quality of Life Following a Lower Limb Amputation in Diabetic Patients: A Longitudinal and Multicenter Study. Psychiatry 83: 47–57. [Google Scholar] [CrossRef] [PubMed]
- Perrin, Byron M., Penny Allen, Marcus J. Gardner, Adrew Chappell, Bronwyn Phillips, Claire Massey, Isabelle Skinner, and Timothy C. Skinner. 2019. The foot-health of people with diabetes in regional and rural Australia: Baseline results from an observational cohort study. Journal of Foot and Ankle Research 12: 56. [Google Scholar] [CrossRef] [PubMed]
- Polikandrioti, Maria, Georgios Vasilopoulos, Ioannis Koutelekos, Georgios Panoutsopoulos, Georgia Gerogianni, Fotoula Babatsikou, Afroditi Zartaloudi, and Georgia Toulia. 2020. Quality of Life in Diabetic Foot Ulcer: Associated Factors and the Impact of Anxiety/Depression and Adherence to Self-Care. The International Journal of Lower Extremity Wounds 19: 165–79. [Google Scholar] [CrossRef]
- Putnam, Robert D. 1993a. Making Democracy Work: Civic Traditions in Modern Italy. Princeton: Princeton University Press. [Google Scholar]
- Putnam, Robert D. 1993b. The prosperous community: Social capital and public life. The American Prospect 13: 35–42. [Google Scholar]
- Putnam, Robert D. 2020. Bowling alone: America’s declining social capital: Journal of democracy (1995). In The City Reader. London: Routledge, pp. 142–50. [Google Scholar]
- Ragnarson Tennvall, Gunnel, and Jan Apelqvist. 2000. Health-related quality of life in patients with diabetes mellitus and foot ulcers. Journal of Diabetes and Its Complications 14: 235–41. [Google Scholar] [CrossRef]
- Reis, Josè, Robson Wanzeller, Wilame M. Meireles, Mariseth C. Andrade, Victor Gomes, Josè Arrais, and Geraldo Ishak. 2020. Demographic and socioeconomic profiles of patients admitted with diabetic foot complications in a tertiary hospital in Belem—Para. Revista do Colegio Brasileiro de Cirurgioes 47: e20202606. [Google Scholar] [CrossRef]
- Rerkasem, Kittipan. 2011. Seminar review: Sociocultural practices and epidemiology of diabetic foot problem: Lessons from a study in Chiang Mai University Hospital, Thailand. The International Journal of Lower Extremity Wounds 10: 86–90. [Google Scholar] [CrossRef]
- Salameh, Basma S., Jihad Abdallah, and Enab O. Naerat. 2020. Case-Control Study of Risk Factors and Self-Care Behaviors of Foot Ulceration in Diabetic Patients Attending Primary Healthcare Services in Palestine. Journal of Diabetes Research 2020: 7624267. [Google Scholar] [CrossRef]
- Salomé, Geraldo M., Sergio A. de Almeida, and Lydia M. Ferreira. 2015. Association of sociodemographic factors with hope for cure, religiosity, and spirituality in patients with venous ulcers. Advances in Skin & Wound Care 28: 76–82. [Google Scholar] [CrossRef]
- Salomé, Geraldo M., Sergio A. de Almeida, Maria T. de Jesus Pereira, Marcelo R. Massahud, Jr., Carmelita N. de Oliveira Moreira, Maria J. de Brito, and Lydia M. Ferreira. 2016. The Impact of Venous Leg Ulcers on Body Image and Self-esteem. Advances in Skin & Wound Care 29: 316–21. [Google Scholar] [CrossRef]
- Shankar, Pooja, Vikram S. Grewal, Sunil Agrawal, and Sreeni V. Nair. 2020. A study on quality of life among lower limb amputees at a tertiary prosthetic rehabilitation center. Medical Journal, Armed Forces India 76: 89–94. [Google Scholar] [CrossRef] [PubMed]
- Sheen, Yijing J., Peitseng T. Kung, Weiyin Y. Kuo, Liting T. Chiu, and Wenchen C. Tsai. 2018. Impact of the pay-for-performance program on lower extremity amputations in patients with diabetes in Taiwan. Medicine 97: e12759. [Google Scholar] [CrossRef] [PubMed]
- Tan, Sheena, Hazel Horobin, and Thanaporn Tunprasert. 2019. The lived experience of people with diabetes using off-the-shelf prescription footwear in Singapore: A qualitative study using interpretative phenomenological analysis. Journal of Foot and Ankle Research 12: 19. [Google Scholar] [CrossRef]
- Tatulashvili, Sopio, Guy Fagherazzi, Courtney Dow, Régis Cohen, Sandrine Fosse, and Hélène Bihan. 2020. Socioeconomic inequalities and type 2 diabetes complications: A systematic review. Diabetes & Metabolism 46: 89–99. [Google Scholar] [CrossRef]
- Vedhara, Kavita, Angela Beattie, Chris Metcalfe, Suzanne Roche, John Weinman, Nicky Cullum, Patricia Price, Colin Dayan, Ashley R. Cooper, Rona Campbell, and et al. 2012. Development and preliminary evaluation of a psychosocial intervention for modifying psychosocial risk factors associated with foot re-ulceration in diabetes. Behaviour Research and Therapy 50: 323–32. [Google Scholar] [CrossRef]
- Wu, Haibin, Karen N. Eggleston, Jieming Zhong, Ruying Hu, Chunmei Wang, Kaixu Xie, Yiwei Chen, Xiangyu Chen, and Min Yu. 2018. How do type 2 diabetes mellitus (T2DM)-related complications and socioeconomic factors impact direct medical costs? A cross-sectional study in rural Southeast China. BMJ Open 8: e020647. [Google Scholar] [CrossRef]
- Yan, Ruihong, Fang Yu, Kara Strandlund, Jing Han, Na Lei, and Yinghong Song. 2021. Analyzing factors affecting quality of life in patients hospitalized with chronic wound. Wound Repair and Regeneration 29: 70–78. [Google Scholar] [CrossRef]
- Yildiz, Ebru, and Türkinaz Aşti. 2015. Determine the relationship between perceived social support and depression level of patients with diabetic foot. Journal of Diabetes and Metabolic Disorders 14: 59. [Google Scholar] [CrossRef] [PubMed]
- Zhang, George Q., Jospeh K. Canner, Elliott Haut, Ronald L. Sherman, Christopher J. Abularrage, and Caitlin. W. Hicks. 2021. Impact of Geographic Socioeconomic Disadvantage on Minor Amputation Outcomes in Patients With Diabetes. The Journal of Surgical Research 258: 38–46. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).