Social Aspects of Diabetic Foot: A Scoping Review
Abstract
1. Introduction
2. Materials and Methods
3. Eligibility Criteria
4. Search Strategy
5. Data Charting Process
6. Data Items
7. Synthesis of Results
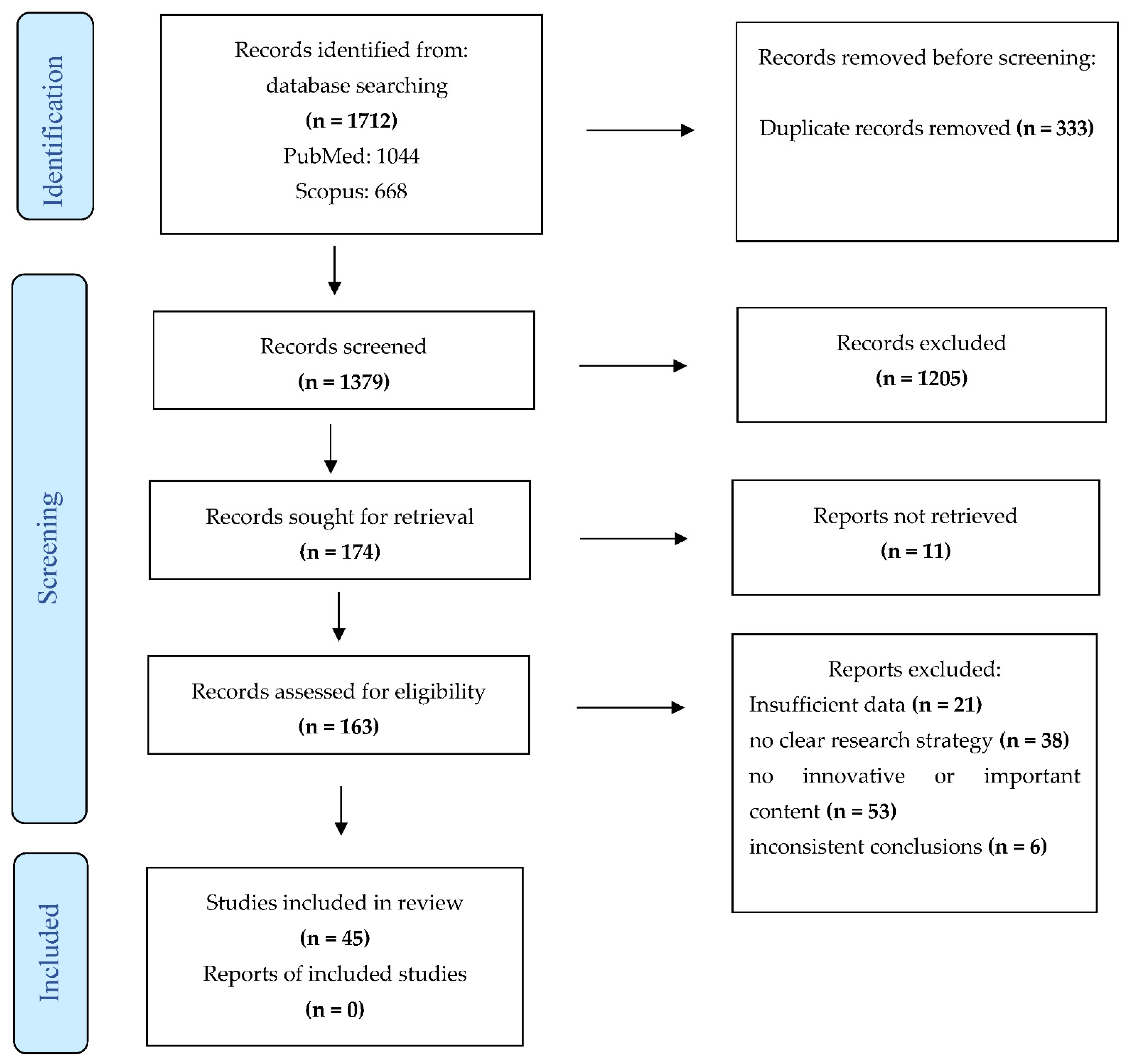
8. Results
9. Selection and Characteristics of Sources of Evidence
10. Results of Individual Sources of Evidence
10.1. Gender Variables and Diabetic Foot
10.2. Socioeconomic Status and Diabetic Foot
10.3. Quality of Life and Social Capital
10.4. Medical Consequences and Diabetic Foot
10.5. Main Indicators
11. Discussion and Summary of Evidence
12. Limitations
13. Conclusions and Recommendations
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Ahmad Sharoni, Siti K., Mohamed N. Mohd Razi, Nor F. Abdul Rashid, and Yusuf E. Mahmood. 2017. Self-efficacy of foot care behaviour of elderly patients with diabetes. Malaysian Family Physician 12: 2–8. [Google Scholar] [PubMed]
- Al Ayed, Mousab, Mutasem Ababneh, Asirvatham Alwin Robert, Nasser Al Misfer, Maria Cruz, Hesiel C. Austria, and Mohamed Al Dawish. 2020. Factors Associated with Health-Related Quality of Life in Patients With Diabetic Foot Ulcer: A Cross-Sectional Study From Saudi Arabia. Cureus 12: e8658. [Google Scholar] [CrossRef] [PubMed]
- Amin, Leila, Baiju R. Shah, Arlene S. Bierman, Lorraine L. Lipscombe, Caixia F. Wu, Denise S. Feig, and Gillian L. Booth. 2014. Gender differences in the impact of poverty on health: Disparities in risk of diabetes-related amputation. Diabetic Medicine 31: 1410–17. [Google Scholar] [CrossRef]
- Coleman, James S. 1988. Social capital in the creation of human capital. American Journal of Sociology 94: S95–S120. [Google Scholar] [CrossRef]
- Coleman, James S. 1990. Foundations of Social Theory. Cambridge: Harvard University Press. [Google Scholar]
- De Silva, Ambepitiyawaduge P., Sudirikku H. De Silva, Rashan Haniffa, Isurujith K. Liyanage, Saroj A. Jayasinghe, Prasad Katulanda, Chandrika N. Wijeratne, Sumedha Wijeratne, and Lalini C. Rajapakse. 2016. A survey on socioeconomic determinants of diabetes mellitus management in a lower middle income setting. International Journal for Equity in Health 15: 74. [Google Scholar] [CrossRef]
- Downs, Sara H., and Nick Black. 1998. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. Journal of Epidemiology and Community Health 52: 377–84. [Google Scholar] [CrossRef]
- Elkhider, Alaa, Ahmed O. Almobark, Safaa Badi, Hanan Tahir, Azza Ramadan, Abbas A. Khalil, Elamin Elshaikh, and Mohamed H. Ahmed. 2021. Risk factors associated with lower extremity amputation in Sudanese individuals with diabetes: The need for improvement in primary health care system. Journal of Family Medicine and Primary Care 10: 985–90. [Google Scholar] [CrossRef]
- Elrayah-Eliadarous, Hind A., Claes G. Östenson, Mohammed Eltom, Pia Johansson, Vibeke Sparring, and Rolf Wahlström. 2017. Economic and social impact of diabetes mellitus in a low-income country: A case-control study in Sudan. Journal of Diabetes 9: 1082–90. [Google Scholar] [CrossRef]
- Fejfarová, Vladimíra, Alexandra Jirkovská, Eva Dragomirecká, Frances Game, Robert Bém, Michal Dubský, Veronika Wosková, Marta Křížová, Jelena Skibová, and Stephanie Wu. 2014. Does the diabetic foot have a significant impact on selected psychological or social characteristics of patients with diabetes mellitus? Journal of Diabetes Research 2014: 371938. [Google Scholar] [CrossRef] [PubMed]
- Goodridge, Donna, Elly Trepman, and John M. Embil. 2005. Health-related quality of life in diabetic patients with foot ulcers: Literature review. Journal of Wound, Ostomy, and Continence Nursing 32: 368–77. [Google Scholar] [CrossRef]
- Goodridge, Donna, Elly Trepman, Jeff Sloan, Lorna Guse, Laurel A. Strain, John McIntyre, and John M. Embil. 2006. Quality of life of adults with unhealed and healed diabetic foot ulcers. Foot & Ankle International 27: 274–80. [Google Scholar] [CrossRef]
- Herber, Oliver R., Wilfried Schnepp, and Monika A. Rieger. 2007. A systematic review on the impact of leg ulceration on patients’ quality of life. Health and Quality of Life Outcomes 5: 44. [Google Scholar] [CrossRef] [PubMed]
- Hicks, Caitlin. W., Joseph K. Canner, Nicolas Mathioudakis, Ronald L. Sherman, Kathryn Hines, Christopher Lippincott, James H. Black III, and Christopher J. Abularrage. 2018. Neighborhood socioeconomic disadvantage is not associated with wound healing in diabetic foot ulcer patients treated in a multidisciplinary setting. Journal of Surgical Research 224: 102–11. [Google Scholar] [CrossRef] [PubMed]
- Hjelm, Katarina, Per Nyberg, and Jan Apelqvist. 2002. Gender influences beliefs about health and illness in diabetic subjects with severe foot lesions. Journal of Advanced Nursing 40: 673–84. [Google Scholar] [CrossRef] [PubMed]
- Iversen, Marjolein M., Grethe S. Tell, Birigitte Espehaug, Kristian Midthjell, Marit Graue, Berit Rokne, Line I. Berge, and Truls Østbye. 2015. Is depression a risk factor for diabetic foot ulcers? 11-years follow-up of the Nord-Trøndelag Health Study (HUNT). Journal of Diabetes and Its Complications 29: 20–25. [Google Scholar] [CrossRef]
- Jaksa, Peter J., and James L. Mahoney. 2010. Quality of life in patients with diabetic foot ulcers: Validation of the Cardiff Wound Impact Schedule in a Canadian population. International Wound Journal 7: 502–7. [Google Scholar] [CrossRef]
- Jarl, Gustav, John Alnemo, Roy Tranberg, and Lars O. Lundqvist. 2019. Gender differences in attitudes and attributes of people using therapeutic shoes for diabetic foot complications. Journal of Foot and Ankle Research 12: 21. [Google Scholar] [CrossRef]
- Kawachi, Ichiro, and Bruce P. Kennedy. 1997. Health and social cohesion: Why care about income inequality? BMJ (Clinical Research Ed.) 314: 1037–40. [Google Scholar] [CrossRef] [PubMed]
- Kawachi, Ichiro, Bruce P. Kennedy, and Kimberly Lochner. 1997a. Long live community: Social capital as public health. The American Prospect 35: 56–59. [Google Scholar]
- Kawachi, Ichiro, Bruce P. Kennedy, Kimberly Lochner, and Deborah Prothrow-Stith. 1997b. Social capital, income inequality, and mortality. American Journal of Public Health 87: 1491–98. [Google Scholar] [CrossRef]
- Korzon-Burakowska, Anna, and Piotr Dziemidok. 2011. Diabetic foot—The need for comprehensive multidisciplinary approach. Annals of Agricultural and Environmental Medicine 18: 314–17. [Google Scholar] [PubMed]
- Kuang, Dan, Danfeng F. Gu, Hong Cao, Qinfang F. Yuan, Zhixia X. Dong, Dan Yu, and Xiaoming M. Shen. 2021. Impacts of psychological resilience on self-efficacy and quality of life in patients with diabetic foot ulcers: A prospective cross-sectional study. Annals of Palliative Medicine 10: 5610–18. [Google Scholar] [CrossRef] [PubMed]
- Lael-Monfared, Elahe, Hadi Tehrani, Zahara E. Moghaddam, Gordon A. Ferns, Maryam Tatari, and Alireza Jafari. 2019. Health literacy, knowledge and self-care behaviors to take care of diabetic foot in low-income individuals: Application of extended parallel process model. Diabetes & Metabolic Syndrome 13: 1535–41. [Google Scholar] [CrossRef]
- Lamchahab, Fatima Z., Nadia El Kihal, Ibtissam Khoudri, Abdelmjid Chraibi, Badreddine Hassam, and Mohamed Ait Ourhroui. 2011. Factors influencing the awareness of diabetic foot risks. Annals of Physical and Rehabilitation Medicine 54: 359–65. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Leese, Graham P., Zhiqiang Feng, Robert M. Leese, Chris Dibben, and Alistair Emslie-Smith. 2013. Impact of health-care accessibility and social deprivation on diabetes related foot disease. Diabetic Medicine 30: 484–90. [Google Scholar] [CrossRef] [PubMed]
- Lo, Zhiwen J., Naren K. Surendra, Akshar Saxena, and Josip Car. 2021. Clinical and economic burden of diabetic foot ulcers: A 5-year longitudinal multi-ethnic cohort study from the tropics. International Wound Journal 18: 375–86. [Google Scholar] [CrossRef]
- Lochner, Kimberly, Ichiro Kawachi, and Bruce P. Kennedy. 1999. Social capital: A guide to its measurement. Health & Place 5: 259–70. [Google Scholar] [CrossRef]
- Lopes, Geysa, Isaura Rolim, Renata S. Alves, Talitha Pessoa, Evanira R. Maia, Maria Lopes, Ana Morais, and R. Queiroz. 2021. Social representations on diabetic foot: Contributions to PHC in the Brazilian Northeast. Representações sociais sobre pé diabético: Contribuições para Atenção Primária à saúde no Nordeste brasileiro. Ciencia & Saude Coletiva 26: 1793–803. [Google Scholar] [CrossRef]
- Matricciani, Lisa, and Sara Jones. 2015. Who cares about foot care? Barriers and enablers of foot self-care practices among non-institutionalized older adults diagnosed with diabetes: An integrative review. The Diabetes Educator 41: 106–17. [Google Scholar] [CrossRef]
- Meijer, Jan W., Jan Trip, Sonia M. Jaegers, Thera P. Links, Andrew J. Smits, Johan W. Groothoff, and Willem H. Eisma. 2001. Quality of life in patients with diabetic foot ulcers. Disability and Rehabilitation 23: 336–40. [Google Scholar] [CrossRef]
- Misliza, Ahmad, and Silvi M. Ayu. 2009. Sociodemographic and lifestyle factors as the risk of diabetic foot ulcer in the university of malaya medical centre. Journal of Health and Translational Medicine 12: 15–21. [Google Scholar]
- Nabuurs-Franssen, Marrigje H., Maya S. Huijberts, Arie C. Nieuwenhuijzen Kruseman, Jan Willems, and Nicolaas C. Schaper. 2005. Health-related quality of life of diabetic foot ulcer patients and their caregivers. Diabetologia 48: 1906–10. [Google Scholar] [CrossRef] [PubMed]
- National Collaborating for Methods and Tools. 2010. Quality Checklist for Health Care Intervention Studies. Hamilton: McMaster University. Available online: http://www.nccmt.ca/resources/search/9;2008 (accessed on 23 March 2022).
- Nurhikmah, Lia, Dewi Gayatri, and Tuti Nuraini. 2019. Body image related to quality of life diabetic ulcer patients. Enfermeria Clinica 29: 373–78. [Google Scholar] [CrossRef]
- Pedras, Susana, Estela Vilhena, Rui Carvalho, and Maria G. Pereira. 2020. Quality of Life Following a Lower Limb Amputation in Diabetic Patients: A Longitudinal and Multicenter Study. Psychiatry 83: 47–57. [Google Scholar] [CrossRef] [PubMed]
- Perrin, Byron M., Penny Allen, Marcus J. Gardner, Adrew Chappell, Bronwyn Phillips, Claire Massey, Isabelle Skinner, and Timothy C. Skinner. 2019. The foot-health of people with diabetes in regional and rural Australia: Baseline results from an observational cohort study. Journal of Foot and Ankle Research 12: 56. [Google Scholar] [CrossRef] [PubMed]
- Polikandrioti, Maria, Georgios Vasilopoulos, Ioannis Koutelekos, Georgios Panoutsopoulos, Georgia Gerogianni, Fotoula Babatsikou, Afroditi Zartaloudi, and Georgia Toulia. 2020. Quality of Life in Diabetic Foot Ulcer: Associated Factors and the Impact of Anxiety/Depression and Adherence to Self-Care. The International Journal of Lower Extremity Wounds 19: 165–79. [Google Scholar] [CrossRef]
- Putnam, Robert D. 1993a. Making Democracy Work: Civic Traditions in Modern Italy. Princeton: Princeton University Press. [Google Scholar]
- Putnam, Robert D. 1993b. The prosperous community: Social capital and public life. The American Prospect 13: 35–42. [Google Scholar]
- Putnam, Robert D. 2020. Bowling alone: America’s declining social capital: Journal of democracy (1995). In The City Reader. London: Routledge, pp. 142–50. [Google Scholar]
- Ragnarson Tennvall, Gunnel, and Jan Apelqvist. 2000. Health-related quality of life in patients with diabetes mellitus and foot ulcers. Journal of Diabetes and Its Complications 14: 235–41. [Google Scholar] [CrossRef]
- Reis, Josè, Robson Wanzeller, Wilame M. Meireles, Mariseth C. Andrade, Victor Gomes, Josè Arrais, and Geraldo Ishak. 2020. Demographic and socioeconomic profiles of patients admitted with diabetic foot complications in a tertiary hospital in Belem—Para. Revista do Colegio Brasileiro de Cirurgioes 47: e20202606. [Google Scholar] [CrossRef]
- Rerkasem, Kittipan. 2011. Seminar review: Sociocultural practices and epidemiology of diabetic foot problem: Lessons from a study in Chiang Mai University Hospital, Thailand. The International Journal of Lower Extremity Wounds 10: 86–90. [Google Scholar] [CrossRef]
- Salameh, Basma S., Jihad Abdallah, and Enab O. Naerat. 2020. Case-Control Study of Risk Factors and Self-Care Behaviors of Foot Ulceration in Diabetic Patients Attending Primary Healthcare Services in Palestine. Journal of Diabetes Research 2020: 7624267. [Google Scholar] [CrossRef]
- Salomé, Geraldo M., Sergio A. de Almeida, and Lydia M. Ferreira. 2015. Association of sociodemographic factors with hope for cure, religiosity, and spirituality in patients with venous ulcers. Advances in Skin & Wound Care 28: 76–82. [Google Scholar] [CrossRef]
- Salomé, Geraldo M., Sergio A. de Almeida, Maria T. de Jesus Pereira, Marcelo R. Massahud, Jr., Carmelita N. de Oliveira Moreira, Maria J. de Brito, and Lydia M. Ferreira. 2016. The Impact of Venous Leg Ulcers on Body Image and Self-esteem. Advances in Skin & Wound Care 29: 316–21. [Google Scholar] [CrossRef]
- Shankar, Pooja, Vikram S. Grewal, Sunil Agrawal, and Sreeni V. Nair. 2020. A study on quality of life among lower limb amputees at a tertiary prosthetic rehabilitation center. Medical Journal, Armed Forces India 76: 89–94. [Google Scholar] [CrossRef] [PubMed]
- Sheen, Yijing J., Peitseng T. Kung, Weiyin Y. Kuo, Liting T. Chiu, and Wenchen C. Tsai. 2018. Impact of the pay-for-performance program on lower extremity amputations in patients with diabetes in Taiwan. Medicine 97: e12759. [Google Scholar] [CrossRef] [PubMed]
- Tan, Sheena, Hazel Horobin, and Thanaporn Tunprasert. 2019. The lived experience of people with diabetes using off-the-shelf prescription footwear in Singapore: A qualitative study using interpretative phenomenological analysis. Journal of Foot and Ankle Research 12: 19. [Google Scholar] [CrossRef]
- Tatulashvili, Sopio, Guy Fagherazzi, Courtney Dow, Régis Cohen, Sandrine Fosse, and Hélène Bihan. 2020. Socioeconomic inequalities and type 2 diabetes complications: A systematic review. Diabetes & Metabolism 46: 89–99. [Google Scholar] [CrossRef]
- Vedhara, Kavita, Angela Beattie, Chris Metcalfe, Suzanne Roche, John Weinman, Nicky Cullum, Patricia Price, Colin Dayan, Ashley R. Cooper, Rona Campbell, and et al. 2012. Development and preliminary evaluation of a psychosocial intervention for modifying psychosocial risk factors associated with foot re-ulceration in diabetes. Behaviour Research and Therapy 50: 323–32. [Google Scholar] [CrossRef]
- Wu, Haibin, Karen N. Eggleston, Jieming Zhong, Ruying Hu, Chunmei Wang, Kaixu Xie, Yiwei Chen, Xiangyu Chen, and Min Yu. 2018. How do type 2 diabetes mellitus (T2DM)-related complications and socioeconomic factors impact direct medical costs? A cross-sectional study in rural Southeast China. BMJ Open 8: e020647. [Google Scholar] [CrossRef]
- Yan, Ruihong, Fang Yu, Kara Strandlund, Jing Han, Na Lei, and Yinghong Song. 2021. Analyzing factors affecting quality of life in patients hospitalized with chronic wound. Wound Repair and Regeneration 29: 70–78. [Google Scholar] [CrossRef]
- Yildiz, Ebru, and Türkinaz Aşti. 2015. Determine the relationship between perceived social support and depression level of patients with diabetic foot. Journal of Diabetes and Metabolic Disorders 14: 59. [Google Scholar] [CrossRef] [PubMed]
- Zhang, George Q., Jospeh K. Canner, Elliott Haut, Ronald L. Sherman, Christopher J. Abularrage, and Caitlin. W. Hicks. 2021. Impact of Geographic Socioeconomic Disadvantage on Minor Amputation Outcomes in Patients With Diabetes. The Journal of Surgical Research 258: 38–46. [Google Scholar] [CrossRef] [PubMed]
| References/Country | Research Type | Population/Sample Size | Instrument | Aim | Results |
|---|---|---|---|---|---|
| (Reis et al. 2020) Brazil | Descriptive, cross-sectional, unicentric, and analytical study | 57 patients with diabetic foot | Questionnaire | Evaluate risk factors for lower limb amputations | Patients with diabetic foot follow-up have a low socioeconomic profile |
| (Lo et al. 2021) Singapore | Longitudinal study | 1729 patients treated for DFUs | Descriptive statistics, Kaplan–Meier survival analyses, Cox proportional hazard models | Analyze the clinical and economic burden of DFU | There was a significant clinical and economic burden of DFUs, with a high wound-per-patient ratio and escalating healthcare costs corresponding to more proximal amputation levels |
| (Leese et al. 2013) | Cohort study | 15,983 patients with diabetes | Community and hospital data | Determine whether geography and/or social deprivation influences the occurrence of foot ulcers or amputations in patients with diabetes | Social deprivation is an important factor, especially for the development of foot ulcers |
| (Sheen et al. 2018) Taiwan | Cohort study | 9738 patients with diabetes with amputations | Taiwan National Health Insurance Research Database | Effects of adopting a nationalized policy to decrease amputation risk in diabetes previously | Diabetes in patients with low socioeconomic status is associated with an increased risk of amputations |
| (Perrin et al. 2019) Australia | Cohort study | 899 patients with diabetes | Multivariable analysis | Explore the associations between demographic, socio-economic, and diabetes-related variables with diabetes-related foot morbidity in people residing in regional and rural Australia | Men access health services less than women because they think they have less time for their own health |
| (Goodridge et al. 2005) | Review of qualitative and quantitative studies | \ | Qualitative and quantitative studies analysis | Social effect of diabetic foot ulcers | Diabetic foot ulcers have a huge negative psychological and social effect |
| (Iversen et al. 2015) Norway | Longitudinal study | 36,031 patients | Hospital Anxiety and Depression Scale | Prospectively examine whether depressive symptoms increase the risk of diabetes and a diabetic foot ulcer | Symptoms of depression at baseline are associated with an increased risk of a diabetic foot ulcer |
| (Herber et al. 2007) | Systematic review | 24 articles | Analyzed journal articles | Describe or measure the impact of leg ulceration on patients’ quality of life (QoL) in order to improve the content of an educational program that aims to enhance self-care agency in leg ulcer patients | Woman patients seemed to have fewer complaints regarding pain than male patients |
| (Jarl et al. 2019) | Questionnaire-based study | 1230 patients with diabetes who had been fitted with therapeutic shoes | Questionnaire | Compare attitudes and attributes of women and men using therapeutic shoes for diabetic foot complications. | Men had worse foot complications. Women had worse general health, lower internal locus of control regarding ulcer prevention, and more negative attitudes toward therapeutic shoes |
| (Amin et al. 2014) Canada | Cohort study | 606,494 patients with diabetes | Administrative health databases analysis | Assess the combined impact of socio-economic status and gender on the risk of diabetes-related lower extremity amputation within a universal healthcare system | There are marked socioeconomic status and gender disparities in the risk of lower extremity amputation among patients with diabetes. Men living in low-income neighborhoods were at the greatest risk |
| (Wu et al. 2018) China | Cross-sectional study | Individuals diagnosed with T2DM in the local diabetes management system, and who had 2015 insurance claims in the social security system | A cross-sectional study using data from the region’s diabetes management system, social security system, and death registry system, 2015 | Evaluate type 2 diabetes mellitus (T2DM)-related direct medical costs by complication type and complication number, and assess the impacts of complications as well as socioeconomic factors on direct medical costs | Complications significantly aggravated expenditures on T2DM Proper management and the prevention of related complications are urgently needed to reduce the growing economic burden of diabetes |
| (Al Ayed et al. 2020) Saudi Arabia | Cross-sectional study | 81 patients with DFU | Questionnaire. Short-Form 36-Item Survey (SF-36) | Estimate the HRQOL and its related risk factors in patients with foot ulcers associated with type 2 diabetes mellitus | The patients with DFU in Saudi Arabia generally revealed lower HRQOL |
| (Goodridge et al. 2006) | Cross-sectional study | 104 patients. (57 with unhealed ulcers and 47 with healed ulcers) | Questionnaire. Short Form 12 (SF-12). Cardiff Wound Impact Scale (CWIS) | Evaluate the quality of life in patients with unhealed and healed diabetic foot ulcers | Individuals with diabetic foot ulcers experience a profound compromise of physical quality of life, which is worse in those with unhealed ulcers. |
| (Salameh et al. 2020) Palestine | Case-control study | 413 diabetic patients | Interviews; Questionnaires Diabetes Foot Self-Care Behavior Scale | Identify certain sociodemographic, lifestyle, self-care, and foot examination factors that predict the development of diabetic foot ulcers in Palestine | Poor self-care behaviors were associated with DFU |
| (De Silva et al. 2016) | Cross-sectional descriptive study | 202 patients with diabetes mellitus | Questionnaire | Describe the socioeconomic determinants of management and complications of diabetes mellitus in a lower-middle-income setting. | Diabetes mellitus patients, irrespective of their socioeconomic status, are poorly managed and have high rates of complications. |
| (Yildiz and Aşti 2015) | Statistical evaluation | 128 patients | Statistical evaluation (Pearson chi-square, Fisher Exact and Likelihood ratio, chi-square, Student t-test, and one way analysis of variance, Levene’s test, One-way ANOVA, Welch and Games Howell tests) | Take essential precautions to generate proper solutions and treatment processes and make supportive plans for patients with developing diabetic foot and depression. | In the treatment and care of the patients with diabetic foot, anxiety and depression status of the patients, as well as physical status, should also be evaluated routinely. |
| (Korzon-Burakowska and Dziemidok 2011) | Literature review | \ | Literature review | Global problem of diabetic foot with particular consideration of those affected by environmental factors. | Patients who attend multidisciplinary diabetic foot clinics have an increased limb survival rate |
| (Elrayah-Eliadarous et al. 2017) Sudan | Case-Control study | 375 persons with diabetes 375 persons non-diabetic | Interviews | Examine the economic and social effects attributed to diabetes in Sudan | The high economic burden and adverse social effects on people with diabetes and their families in Sudan call for the development of evidence-based policy and program strategies for the prevention and management of diabetes, with an emphasis on low-resource communities. |
| (Lamchahab et al. 2011) | Prospective study | Diabetic patients hospitalized | Medical examination; Questionnaires | Identify factors influencing diabetic patients’ awareness of the risk of foot problems. | In diabetes, there is still a need for easily assimilated, locally provided patient education. |
| (Hjelm et al. 2002) | Explorative study | 10 women and 11 men under 65 years and 6 women and 12 men over 65 years with present or previous diabetic foot lesions managed at a specialized multidisciplinary diabetic foot clinic. | Interviews | Explore beliefs about health and illness among patients with severe diabetic foot lesions that might affect self-care practice and care-seeking behavior. | The present study emphasizes the need to take into account the existence of different beliefs about health and illness, especially regarding gender, in the prevention and management of the diabetic foot. |
| (Lael-Monfared et al. 2019) | Cross-sectional study | 400 patients | Questionnaires | Determining the relationship between health literacy, knowledge, and self-care behaviors to take care of the diabetic foot in low-income individuals, based on the extended parallel process model (EPPM). | Levels of knowledge and health literacy of patients were very poor overall, and the self-care behaviors were not appropriate. |
| (Nabuurs-Franssen et al. 2005) | Multicenter study | 294 patients | Questionnaire | The effect of a foot ulcer on health-related quality of life (HRQoL) of patients with diabetes mellitus and their caregivers is unclear and was therefore evaluated prospectively in this multicenter study. | Diabetic patients with a healed foot ulcer had a higher HRQoL than patients with a persisting ulcer. |
| (Polikandrioti et al. 2020) | Cross-sectional study | 195 patients | Data collection | Assess the impact of patients’ characteristics, anxiety/depression, and adherence to guidelines on the QoL of patients with diabetic ulcer. | DFU is a challenge for DM individuals, healthcare professionals, and for the health system of each country. Exploring factors affecting QoL and specifically anxiety/depression and adherence to self-care should be included in designing treatment strategies to tailor the needs of these specific groups of patients. |
| (Jaksa and Mahoney 2010) Canada | 30 patients | Questionnaires | Evaluate and validate the Cardiff Wound Impact Schedule (CWIS), a disease-specific quality-of-life measure, in a diabetic foot ulcer (DFU) population. | However, there was no significant difference in mean CWIS scores between categories of wound severity. | |
| (Elkhider et al. 2021) Sudan | Cross-sectional health facility-based study | 315 patients with diabetes | Direct interviewing | Assess the prevalence and risk factors associated with LEA in diabetic foot ulcer (DFU) patients. | The primary risks factors associated with amputation were the presence of neuropathy and ulcer size > 2.5 cm. |
| (Lopes et al. 2021) Brazil | Qualitative study | 100 patients | openEVOC software | Identify the structuring elements guiding the establishment of the social representations of diabetic foot among people with diabetes mellitus. | The representational structure is based on subjective, valuating, and attitudinal contents. |
| (Ahmad Sharoni et al. 2017) Malaysia | Randomized controlled trial | 76 patients | Data were analyzed with Mixed Design Analysis of Variance using the Statistical Package for the Social Sciences version 22.0. | Evaluate the effectiveness of health education programs based on the self-efficacy theory on foot self-care behavior for older adults with diabetes. | The self-efficacy enhancing program improved foot self-care behavior with respect to the delivered program. |
| (Salomé et al. 2016) | Multicenter, prospective, descriptive, analytical, clinical study. | 59 patients | Questionnaires | Evaluate self-esteem and body image in patients with venous leg ulcers (VLUs). | Patients with VLUs had low self-esteem and negative feelings about their bodies. |
| (Matricciani and Jones 2015) | An integrative, systematic literature review and a deductive thematic analysis | 130 different studies | Literature review | Appropriate and timely foot self-care practices may prevent diabetes-related foot complications. | Foot self-care practices appear underutilized as primary prevention measures by older adults and are instead adopted only once complications have already occurred. |
| (Zhang et al. 2021) Maryland | Retrospective analysis of records | 7415 patients with diabetes underwent minor amputation | Data collection from HSCRC database | To assess the association of geographic socioeconomic disadvantage with short- and long-term outcomes after minor amputation in patients with diabetes. | Geographic socioeconomic disadvantage is independently associated with both short- and long-term outcomes after minor diabetic amputations in Maryland. |
| (Hicks et al. 2018) Maryland | Retrospective review | 277 patients with 621 wounds were treated during the study period. | Area deprivation index (ADI) stratified by quartile (from ADI-0, least, through ADI-3, most). Predictors of wound healing were assessed using Cox proportional hazards models | To quantify the effects of neighborhood socioeconomic deprivation on wound healing among a cohort of patients with diabetic foot ulceration (DFU) treated in a multidisciplinary setting. | Wound healing was largely dependent on wound characteristics and vascular status rather than patient demographics or neighborhood socioeconomic disadvantage. Use of a multidisciplinary approach to the management of DFU may overcome the negative effects of socioeconomic disadvantage frequently described in the diabetic population. |
| (Fejfarová et al. 2014) Czech Republic | Case-control study | 104 patients with and 48 without DF | The World Health Organization Quality of Life Assessment (WHOQOL-BREF), geriatric depression scale (GDS), visual analogue scale (VAS) | To compare selected psychological and social characteristics between diabetic patients with and without the DF (controls). | Compared to controls, patients with DF had a significantly worse quality of life in the area of health and standard of living as shown by lower physical health domain and environment domain that negatively correlated with diabetes duration. |
| (Rerkasem 2011) Thailand | Multicenter, epidemiologic study | 511 patients with diabetes | Data found in a database with patients involved in multidisciplinary foot care at Maharaj Nakorn Chiang Mai Hospital, Chiang Mai, Thailand. | To evaluate complications of diabetes such as foot ulcers or amputation | The prevalence of foot ulcers in diabetic patients was 12.5% and the amputation rate was 1.4%. |
| (Pedras et al. 2020) Portugal | A multicenter, longitudinal study with four-time assessments | 206 individuals hospitalized with diabetic foot ulcer indicated for an LLA | Revised Impact of Event Scale; Barthel Index; Hospital Anxiety and Depression Scale and SF-36. | (1) To analyze the relationship between emotional reactions (anxiety, depression, and traumatic stress symptoms) and functionality level, before and after an LLA due to diabetic foot ulcer, and mental/physical quality of life. (2) To analyze the mediator role of social support between emotional reactions and mental/physical quality of life. | Anxiety symptoms before surgery and depression symptoms one month after surgery contribute to Mental Component Score (MCS) ten months after surgery. |
| (Meijer et al. 2001) Netherlands | A cross-sectional patient-control study | 14 patients with clinical stable foot ulcers vs. 24 unknown patients with DFUs | QoL was assessed with the RAND-36, the Barthel Index, and the Walking and Walking Stairs Questionnaire (WSQ). | To compare QoL between diabetic patients with (former or present) and without foot ulcer. | Marked and significant differences were found in physical functioning, social functioning, physical role, and health experience between the 2 groups |
| (Misliza and Ayu 2009) Malaysia | Case-control study | 125 cases, 250 controls | Data were collected via face-to-face interview using a structured questionnaire. | To identify specific socio-demographic and lifestyle factors associated with foot ulcer in Type 1 and Type 2 diabetes patients. | Results showed that diabetic patients at younger age group, 44 years old and less (OR 5.90 95% CI 2.31, 15.10), Indian (OR 3.24 95% CI 1.66, 6.30), and smoker (OR 3.85 95% CI 1.77, 8.35) were the independent risk factor for diabetic foot ulcer. |
| (Vedhara et al. 2012) UK | Case-control study | 10 individuals were randomized to receive the intervention and 5 individuals to usual care | These observations were supported in the descriptive findings obtained from questionnaires measuring mood, cognitions, behavior, and social support. | To develop a therapeutic model that informed the content, structure, and format of a psychosocial intervention designed to modify the psychosocial risk factors associated with reulceration. | The intervention appears to offer an acceptable and effective way of modifying the psychosocial risk factors associated with re-ulceration. |
| (Tatulashvili et al. 2020) France | Systematic review | 28 studies included | PubMed and EMBASE were searched for English-language observational studies evaluating the prevalence or incidence of micro- and macrovascular complications according to individual and geographical socioeconomic status (SES). | To collect data on risk of complications according to socioeconomic status in patients with T2D. | Among the 28 included studies, most described a clear relationship between SES and diabetes complications, especially retinopathy and cardiopathy. However, very few studies adjusted their analyses according to HbA1c level. |
| (Shankar et al. 2020) India | Descriptive, tertiary-care center-based cross-sectional study | 150 patients | The WHOQOL-BREF (field trial version) self-administered questionnaire was used as the data collection tool. | To study the quality of life (QoL) among lower limb amputees (LLAs) at a tertiary prosthetic rehabilitation center. | Results of this study reinforce the fact that amputation continues to be associated with lower QoL scores. |
| (Tan et al. 2019) | Qualitative study | 8 people with diabetes who received prescription footwear | semi-structured interview | To understand some people’s personal experience of using off-the-shelf prescription footwear. | Empowering patients with choice to select from a range of therapeutic yet normalized footwear could increase the level of security and acceptance they experience with its use. |
| (Nurhikmah et al. 2019) Indonesia | Cross-sectional study | 97 diabetic ulcer patients | Data were collected using the body image questionnaire to assess the body image and Short Form 36 (SF 36) questionnaire to assess the quality of life. | To identify the relationship between body image with the quality of life of diabetic ulcer patients. | The result showed that there was a significant relationship between body image and quality of life of diabetic ulcer patients |
| (Yan et al. 2021) China | Cross-sectional survey | 216 patients with chronic wound | Self-Rating Depression Scale (SDS). Self -Rating Anxiety Scale (SAS). Perceived Social Support Scale (PSSS). Health-related quality of life scale (SF-36). | This study aims to investigate the HRQOL of hospitalized patients with chronic wound and achieve the following objectives: (1) To analyze the impact of demographic and disease characteristics, mental stress (anxiety and depression) on their HRQOL; (2) to explore social support whether impact their HRQOL by buffering their mental stress or not. | 1. The HRQOL of hospitalized patients with chronic wounds was poor, and sleep status, diagnosis, pain, retirement status, and whether the wound has odor were the main demographic and disease characteristic factors that affected their HRQOL. 2. Perceived social support improved the HRQOL of hospitalized patients with chronic wound by buffering their mental stress. |
| (Kuang et al. 2021) China | Prospective cross-sectional study | 98 DFU patients | Connor-Davidson resilience scale (CD-RISC); diabetes management self-efficacy scale (DMSES); QoL was assessed by the 36-item short-form (SF-36) | To analyze the risk factors of self-efficacy and QoL. Then, to analyze the predictors of psychological resilience among the participants. | Low psychological resilience and older age were identified as risk factors of self-efficacy. On the contrary, low psychological resilience, older age, lower perceived social support, and higher level of glycated hemoglobin were identified as risk factors of QoL. Finally, males had lower psychological resilience than females and those receiving more social support had higher psychological resilience than participants receiving less social support. |
| (Salomé et al. 2015) | Primary, prospective, descriptive, analytical, and clinical study. | Fifty adult patients with DFUs | Questionnaires | Evaluate levels of spirituality and hope in patients with diabetic foot ulcers (DFUs) according to sociodemographic factors. | Patients with DFUs, especially women and older adults, had a low sense of hope and spirituality. |
| (Ragnarson Tennvall and Apelqvist 2000) | Quantitative study | 457 patients | Questionnaires; the euroQol quality of life (QoL) questionnaire including a visual analogue scale (VAS) | Investigate HRQL in patients with diabetes and foot problems and to analyze whether EQ-5D is an acceptable instrument for differentiating patients with current foot ulcers from patients with primary healed ulcers or patients who have undergone minor or major amputations. | Patients with current foot ulcers experience lower HRQL than those who have healed primarily without any amputation. |
| Indicators | Definition |
|---|---|
| DFS (Diabetic Foot Ulcer Scale | It is a specific instrument designed to assess the impact of foot ulcers and their treatment on quality of life in people with diabetes. |
| DCP (Diabetes Care Profile) | It is an instrument that assesses the social and psychological factors related to diabetes and its treatment (Fitzgerald et al.) |
| DHP (Diabetes Health Profile) | It is a multidimensional, diabetes-specific, patient self-report outcome measure of the psychological and behavioral impact of living with diabetes. |
| DQOL (Diabetes Quality of Life Measure) | It is an instrument that has been widely used to measure quality of life among diabetes patients. |
| DIMS (Diabetes Impact Management Scale) | It is an easily administered questionnaire with internal consistency and test–retest reliability. |
| EQ-5D (EuroQol) | It is an instrument that evaluates the generic quality of life developed in Europe and is widely used |
| DFSBS (Diabetes Foot Self-Care Behavior Scale) | It is used to measure the self-care behavior of diabetes patients in the study; it contains 7 items. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Costa, D.; Ielapi, N.; Caprino, F.; Giannotta, N.; Sisinni, A.; Abramo, A.; Ssempijja, L.; Andreucci, M.; Bracale, U.M.; Serra, R. Social Aspects of Diabetic Foot: A Scoping Review. Soc. Sci. 2022, 11, 149. https://doi.org/10.3390/socsci11040149
Costa D, Ielapi N, Caprino F, Giannotta N, Sisinni A, Abramo A, Ssempijja L, Andreucci M, Bracale UM, Serra R. Social Aspects of Diabetic Foot: A Scoping Review. Social Sciences. 2022; 11(4):149. https://doi.org/10.3390/socsci11040149
Chicago/Turabian StyleCosta, Davide, Nicola Ielapi, Francesco Caprino, Nicola Giannotta, Antonio Sisinni, Andrea Abramo, Lwanga Ssempijja, Michele Andreucci, Umberto Marcello Bracale, and Raffaele Serra. 2022. "Social Aspects of Diabetic Foot: A Scoping Review" Social Sciences 11, no. 4: 149. https://doi.org/10.3390/socsci11040149
APA StyleCosta, D., Ielapi, N., Caprino, F., Giannotta, N., Sisinni, A., Abramo, A., Ssempijja, L., Andreucci, M., Bracale, U. M., & Serra, R. (2022). Social Aspects of Diabetic Foot: A Scoping Review. Social Sciences, 11(4), 149. https://doi.org/10.3390/socsci11040149








