Abstract
The aim of this study was to identify factors associated with improved motor function of the lower extremities in response to mesenchymal stem cell (MSC) therapy in patients with ischemic stroke. This study was a post hoc analysis of data from a prospective, open-label, randomized controlled trial of MSC therapy for patients with ischemic stroke patients associated with severe middle cerebral artery territory (STARTING-2 trial). Lower limb motor function was scored based on the lower limb of Fugl–Meyer assessment (FMA-LL) score before MSC therapy and at 3 months after stroke. All FMA-LL changes greater than or equal to six points were considered clinically significant. Univariate and multivariate binary logistic regression models were used to determine possible predictors of clinically significant lower limb motor response to MSC therapy. Twelve (33%) of the thirty-six patients receiving MSC therapy reached a minimal clinically important difference (MCID) of FMA-LL. The two independent factors with the greatest impact on response to MSC therapy for achieving an MCID in FMA-LL score were: (1) the time from stroke onset to MSC therapy, and (2) age (p < 0.05). In addition, obese stroke patients responded better to MSC therapy than stroke patients with normal weight. In conclusion, this post hoc analysis might suggest the need for recruiting stroke patients at younger and early after stroke onset in future clinical trials of MSC therapy for stroke.
1. Introduction
Many stroke survivors continue to suffer from significant motor impairments []. Ambulation is an essential part of disability in stroke patients. One-third to two-thirds of stroke survivors have reduced ambulatory capacity []. Impairment of lower extremity motor has been known as one of the major contributors to ambulatory disability after stroke [,]. Although most post-stroke care in the subacute phase depends on rehabilitation interventions, the improvement in lower extremity motor function, especially in patients with severe ischemic stroke, is still a challenge [].
Stem cell therapy is an emerging paradigm in stroke treatment and is considered a potential regenerative strategy for patients with fixed neurologic deficits. Animal models of ischemic stroke have shown that stem cells transplanted into the brain can lead to functional improvement []. We have previously reported the results of the STARTING (STem cell Application Researches and Trials In NeuroloGy) trial, a randomized controlled trial of intravenous application of autologous mesenchymal stem cells (MSCs), culture-expanded with fetal bovine serum (FBS), in the subacute phase of stroke []. More recently, the STARTING-2 trial showed that MSC therapy improved lower extremity motor function in patients with subacute stroke with no significant adverse effects []. However, there was a relatively large standard deviation in the change of lower limb score of the Fugl–Meyer assessment (FMA-LL) that was measured as the lower extremity motor function in patients with stroke suggesting a highly variable response to MSC therapy. Multiple interacting factors are likely to affect motor recovery in stroke patients []; however, little is known about the factors that predict the efficacy of MSC therapy.
The aim of this study was to identify factors associated with improved motor function in response to MSC therapy in patients with ischemic stroke. The identification of these associated factors will enable the design of individual treatment plans and accurate stratification of patients for better outcomes after MSC therapy.
2. Materials and Methods
2.1. Study Design
This was a post hoc analysis of a prospective, open-label, randomized controlled trial with blinded outcome evaluation in patients with severe middle cerebral artery territory infarct investigated in the STARTING-2 trial []. The trial was registered at ClinicalTrials.gov (NCT01716481). The STARTING-2 trial protocol was approved by the Korean Food and Drug Administration (No. 12218) and the Institutional Review Board of the Samsung Medical Center (IRB-2011-10-047). Written informed consent was obtained from all patients and/or from their first-degree relatives.
Participants were randomly assigned in a 2:1 ratio to receive intravenous MSC injections (intervention group) or standard care alone (control group). After randomization, each participant received conventional rehabilitation during hospitalization. Participants in the intervention group underwent MSC treatment.
2.2. Participants
Of the 85 patients screened, 25 patients did not meet the inclusion or exclusion criteria and were excluded, and 60 patients were recruited. Of these, 15 patients were included in the control group and 39 in the MSC group were added to the final ITT analysis []. transcranial magnetic stimulation (TMS)-induced motor evoked potentials (MEPs) could not be evaluated in 3 of 39 patients in the MSC group due to craniotomy. Finally, this post hoc analysis was performed in 36 patients in the MSC group with ischemic stroke.
2.3. Post Hoc Analysis
The post hoc analysis evaluated the relationship between potential relating factors and change in FMA-LL from baseline to 3 months after MSC injection. Patients were stratified into good responders and poor responders, defined as patients achieving a minimal clinically important difference (MCID ≥ 6 points) of FMA-LL after MSC injection [].
The potential associated factors were selected for this post hoc analysis because of their relating value in previous studies on motor recovery in stroke rehabilitation. For the baseline descriptive characteristics, age, sex, body mass index (BMI), and time since stroke onset were recorded at baseline in each patient [,,,]. Participants were classified into three groups based on their age: young (age <50 years), middle-age (50 ≤ age < 65 years), old age (≤65 years). In addition, based on obesity status, subjects were classified into four groups based on their baseline BMI: underweight (BMI < 18.5), normal (18.5 ≤ BMI < 23), overweight (23 ≤ BMI < 25), and obese (25 ≤ BMI) []. Based on time (time ≤ 30, 30 < time ≤ 60, 60 < time) since stroke onset, patients were divided into three groups. The National Institutes of Health Stroke Scales (NIHSS) NIH and FMA-LL score before MSC injection were used to represent baseline stroke severity and lower limb motor function, respectively. Stroke severity was classified into three groups based on baseline NIHSS: moderate (NIHSS < 9), moderate to severe (9 ≤ NIHSS < 16), and severe (16 ≤ NIHSS) []. In addition, to assess the integrity of the affected corticospinal tract TMS of the affected motor cortex was used to measure MEPs in the paretic first dorsal interosseous muscle at rest, as described previously []. Patients were classified into two groups according to the presence of MEPs on the affected first dorsal interosseus muscle (FDI): “MEPs response” included all patients who showed MEPs in the affected FDI, whereas “no MEPs response” included patients without any MEPs in the affected FDI.
2.4. Statistical Analysis
SPSS version 27.0 (SPSS, Chicago, IL, USA) was used for all statistical analyses. Good and poor responders were compared using an independent t-test and chi-square tests for normally distributed variables and Mann–Whitney tests for nonparametric data. Univariate logistic regression was conducted to identify possible factors associated with a good response to MSC therapy and any variables with univariate association with p-values < 0.20 were considered as potentially associated with MSC therapy and thus included in a multivariate model. Multivariate logistic regression models were then developed. A p-value < 0.05 was considered statistically significant.
3. Results
3.1. Comparison between Good and Poor Responders
Twelve (33%) of the thirty-six patients receiving MSC therapy who reached the MCID of FMA-LL (≥6 points) were classified as good responders. By contrast, 24 (66.7%) patients were classified as poor responders. There was no significant difference in baseline demographics and clinical characteristics between good and poor responders in the MSC group (Table 1). The rate of good response showed a significant negative correlation with age and stroke duration (p < 0.05). In addition, obese stroke patients responded better to MSC therapy than stroke patients with normal weight (p < 0.05, Figure 1).

Table 1.
Baseline demographics and clinical characteristics of good responders and poor responders among stroke patients treated with mesenchymal stem cells.
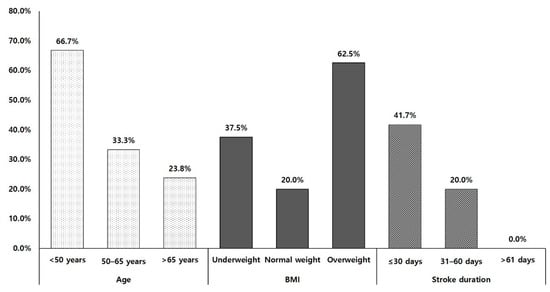
Figure 1.
Rate of good responders. BMI: body mass index.
3.2. Associated Factors Analysis
Table 2 presents the results of univariate and multivariate analyses. In univariate analysis, age, stroke duration, and MEP response were factors associated with MCID of FMA-LL. Potential relating factors with a p-value < 0.2 were then used in multivariate analysis. Age and stroke duration were significant independent factors in the multivariate analysis predicting a good response with MCID of FMA-LL (p < 0.05, Nagelkerke’s R2 of 0.547, Table 2).

Table 2.
Univariate logistic regression analysis of the association between baseline clinical features with responders in lower limb score of Fugl–Meyer assessment of patients treated with stem cells.
4. Discussion
A significant improvement in the affected lower extremity motor function without significant adverse effect was reported in the STARTING-2 trial of MSC therapy involving patients with middle cerebral artery infarction []. The two factors relating patient response to MSC therapy were age and stroke duration from onset to treatment. Therefore, these two factors could be considered in the design of MSC therapy for patients with ischemic stroke.
Several trials have been reported that intravenous autologous MSC therapy was safe and might improve motor recovery in subacute and chronic stroke patients [,,]. There was a lack of reports on the factors affecting MSC therapy, although the treatment response might vary depending on the characteristics of the patients. It is necessary to identify the factors related to MSC therapy response for enhancing therapeutic efficacy. Stroke duration was analyzed as a significant factor independent of age determining the effects of MSC therapy in stroke patients in this post hoc analysis. Neuroplasticity has been suggested as a mechanism for improving motor function in subacute stroke patients []. Many pharmacotherapy trials have also demonstrated the effect of drugs on neuroplasticity in stroke patients []. Mechanistic targets of stem cells have been known as chemokines, trophic factors, and relevant microRNAs that increased markedly in the infarcted brain during the acute stroke phase and decreased with time [,]. These mechanistic targets are also important for neuroplasticity in stroke patients []. The mechanism of the motor function enhancing the effect of MSCs might be attributed to increased neuroplasticity. Therefore, stroke duration, which is a period of high neuroplasticity after stroke, was a significant independent factor affecting MSC therapy in this study [].
In this post hoc analysis, age was one of the independent factors affecting MSC therapy among potential factors influencing motor recovery after stroke. This result might be attributed to age in predicting the prognosis of motor recovery in stroke patients []. However, age affects the MSC function of each participant. Aging has an impact on the function of stem cells because the general efficiency of most cellular and intercellular processes tends to decline with age []. In an animal study involving aging rodents, the proliferation of hypothalamic neural stem cells progressively declined in vivo and depleted eventually in aged mice []. In addition, the neurorestorative potential of MSCs may be limited in the elderly due to the limited number of bone marrow MSCs [], and the relatively low number of neural stem/progenitor cells in the human brain []. To overcome these limitations, the STARTING-2 trial used the preconditioning MSCs using each patient’s serum to achieve rejuvenation of autologous MSCs. In spite of the preconditioning MSCs, the therapeutic effects were insufficient in aged stroke patients. Further studies with younger stem cells are needed to elucidate the mechanism associated with age underlying the effects of MSC therapy [].
Stroke patients with overweight tended to be higher effective for achieving MCID of lower motor function than those with normal weight. Some previous studies have reported that obesity might be a positive influencing factor for functional outcomes after stroke [,]. This phenomenon, referred to as the obesity paradox, because obesity and overweight are well-known risk factors for the development of ischemic stroke []. The results of this study could also be considered as supporting results for the obesity paradox phenomenon in stroke patients. However, some studies have reported that there is insufficient evidence to support the obesity paradox controlling patient factors and comorbid conditions [,]. Therefore, further study will be needed to clarify the influence of obesity on the effects of MSCs therapy in stroke patients.
In this study, 33.3% of all patients who received MSCs showed MCID in their FMA-LL score. The relatively low rate may be attributed to the baseline severity of motor involvement in patients with stroke in the STARTING-2 trial. The most reliable factor predicting the prognosis of lower extremity motor function was baseline motor function in patients with subacute stroke []. Nevertheless, in this post hoc analysis, there was no relation between baseline FMA-LL and responders with MCID after MSC therapy for stroke, thereby indirectly demonstrating that MSCs were effective in improving spontaneous recovery.
This study has some limitations. First, we did not enroll patients with ischemic stroke showing mild motor involvement. Therefore, the study findings are not necessarily applicable to MSC therapy design to improve motor function in all patients with subacute stroke. Another limitation was that only patients who completed the follow-up were analyzed due to the nature of post hoc analysis. In addition, a relatively small number of patients was another limitation. Therefore, further studies with large numbers of patients diagnosed with stroke are needed.
5. Conclusions
In conclusion, younger age and a relatively short duration of stroke might be considered when individualizing MSC therapy to improve lower extremity motor function in patients with subacute stroke.
Author Contributions
W.H.C.: contribution to conception and design; acquisition of data; analysis of data; involvement in drafting the manuscript; final approval of the version to be published, J.L.: contribution to conception and design; final approval of the version to be published, J.-W.C.: acquisition of data; final approval of the version to be published, Y.-H.K. and O.Y.B.: contribution to conception and design; acquisition of data; analysis of data; revising the manuscript critically; final approval of the version to be published. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by a grant from the Korea Health Technology R&D Project, the Ministry of Health & Welfare (HI14C16240000), the Technology Innovation Program (1415174804) funded by the Ministry of Trade, Industry & Energy (MOTIE, Korea), a National Research Foundation of Korea (NRF) grant funded by the Korean government (NRF-2020R1A2C3010304 and NRF-2018R1D1A1A02086038).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of Samsung Medical Center (IRB-2011-10-047).
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A
STARTING-2 Investigators: Oh Young Bang, MD, PhD; Jong-Won Chung, MD, PhD; Suk Jae Kim, MD, MSc; Soo-Kyoung Kim, MD, PhD; Jin Soo Lee, MD, PhD; Sung-Il Sohn, MD, PhD; Yun-Hee Kim, MD, PhD; Won Hyuk Chang, MD, PhD; Jungsoo Lee, PhD; Yeon Hee Cho, MS; Ji Hee Sung, MS; Eun Hee Kim, PhD; Jeong Pyo Son, PhD; Dong Hee Kim, PhD; Eun-Hyeok Choi, MD; Sookyung Ryoo, MD; Yoon Mi Kang, MS; Yong Man Kim, PhD; Hyun Soo Kim, MD, PhD; Jun Ho Jang, MD, PhD.
References
- Braddom, R.L. Physical Medicine and Rehabilitation, 3rd ed.; Elsevier Saunders: Edinburgh, UK, 2007. [Google Scholar]
- Danielsson, A.; Willén, C.; Sunnerhagen, K.S. Physical Activity, Ambulation, and Motor Impairment Late after Stroke. Stroke Res. Treat. 2011, 2012, 1–5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burke, E.; Dobkin, B.H.; Noser, E.A.; Enney, L.A.; Cramer, S.C. Predictors and Biomarkers of Treatment Gains in a Clinical Stroke Trial Targeting the Lower Extremity. Stroke 2014, 45, 2379–2384. [Google Scholar] [CrossRef] [Green Version]
- Langhorne, P.; Bernhardt, J.; Kwakkel, G. Stroke rehabilitation. Lancet 2011, 377, 1693–1702. [Google Scholar] [CrossRef]
- Chopp, M.; Li, Y. Treatment of neural injury with marrow stromal cells. Lancet Neurol. 2002, 1, 92–100. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.S.; Hong, J.M.; Moon, G.J.; Lee, P.H.; Ahn, Y.H.; Bang, O.Y. A Long-Term Follow-Up Study of Intravenous Autologous Mesenchymal Stem Cell Transplantation in Patients With Ischemic Stroke. Stem Cells 2010, 28, 1099–1106. [Google Scholar] [CrossRef]
- Chung, J.W.; Chang, W.H.; Bang, O.Y.; Moon, G.J.; Kim, S.J.; Kim, S.K.; Lee, J.S.; Sohn, S.I.; Kim, Y.H. Efficacy and Safety of Intravenous Mesenchymal Stem Cells for Ischemic Stroke. Neurology 2021, 96, e1012–e1023. [Google Scholar] [CrossRef] [PubMed]
- Franceschini, M.; Ceravolo, M.G.; Agosti, M.; Cavallini, P.; Bonassi, S.; Dall’Armi, V.; Massucci, M.; Schifini, F.; Sale, P. Clinical relevance of action observation in upper-limb stroke rehabilitation: A possible role in recovery of functional dexterity. A ran-domized clinical trial. Neurorehabilit. Neural Repair 2012, 26, 456–462. [Google Scholar] [CrossRef] [PubMed]
- Pandian, S.; Arya, K.N.; Kumar, D. Minimal clinically important difference of the lower-extremity fugl–meyer assessment in chronic-stroke. Top. Stroke Rehabil. 2016, 23, 1–7. [Google Scholar] [CrossRef]
- Chang, W.H.; Sohn, M.K.; Lee, J.; Kim, D.Y.; Lee, S.-G.; Shin, Y.-I.; Oh, G.-J.; Lee, Y.-S.; Joo, M.C.; Han, E.Y.; et al. Predictors of functional level and quality of life at 6 months after a first-ever stroke: The KOSCO study. J. Neurol. 2016, 263, 1166–1177. [Google Scholar] [CrossRef]
- Morone, G.; Iosa, M.; Paolucci, T.; Muzzioli, L.; Paolucci, S. Relationship Between Body Mass Index and Rehabilitation Outcomes in Subacute Stroke With Dysphagia. Am. J. Phys. Med. Rehabil. 2019, 98, 608–612. [Google Scholar] [CrossRef] [PubMed]
- Stinear, C.M. Prediction of motor recovery after stroke: Advances in biomarkers. Lancet Neurol. 2017, 16, 826–836. [Google Scholar] [CrossRef] [PubMed]
- Stinear, C. Prediction of recovery of motor function after stroke. Lancet Neurol. 2010, 9, 1228–1232. [Google Scholar] [CrossRef]
- Jang, S.Y.; Shin, Y.-I.; Kim, D.Y.; Sohn, M.K.; Lee, J.; Lee, S.-G.; Oh, G.-J.; Lee, Y.-S.; Joo, M.C.; Han, E.Y.; et al. Effect of obesity on functional outcomes at 6 months post-stroke among elderly Koreans: A prospective multicentre study. BMJ Open 2015, 5, e008712. [Google Scholar] [CrossRef] [PubMed]
- Sacco, R.L.; DeRosa, J.T.; Haley, J.E.C.; Levin, B.; Ordronneau, P.; Phillips, S.J.; Rundek, T.; Snipes, R.G.; Thompson, J.L.P. Glycine antagonist in neuroprotection for patients with acute stroke: GAIN Americas: A randomized controlled trial. JAMA 2001, 285, 1719–1728. [Google Scholar] [CrossRef]
- Kim, Y.; Chang, W.; Bang, O.; Kim, S.; Park, Y.; Lee, P. Long-term effects of rTMS on motor recovery in patients after subacute stroke. J. Rehabil. Med. 2010, 42, 758–764. [Google Scholar] [CrossRef] [Green Version]
- Bang, O.Y.; Lee, J.S.; Lee, P.H.; Lee, G. Autologous mesenchymal stem cell transplantation in stroke patients. Ann. Neurol. 2005, 57, 874–882. [Google Scholar] [CrossRef]
- Savitz, S.I.; Misra, V.; Kasam, M.; Juneja, H.; Cox, C.S., Jr.; Alderman, S.; Aisiku, I.; Kar, S.; Gee, A.; Grotta, J.C. Intravenous autologous bone marrow mononuclear cells for ischemic stroke. Ann. Neurol. 2011, 70, 59–69. [Google Scholar] [CrossRef] [PubMed]
- Stinear, C.M.; Lang, C.E.; Zeiler, S.; Byblow, W.D. Advances and challenges in stroke rehabilitation. Lancet Neurol. 2020, 19, 348–360. [Google Scholar] [CrossRef]
- Viale, L.; Catoira, N.P.; Di Girolamo, G.; González, C.D. Pharmacotherapy and motor recovery after stroke. Expert Rev. Neurother. 2017, 18, 65–82. [Google Scholar] [CrossRef]
- Hill, W.D.; Hess, D.C.; Martin-Studdard, A.; Carothers, J.J.; Zheng, J.; Hale, D.; Maeda, M.; Fagan, S.C.; Carroll, J.E.; Conway, S.J. SDF-1 (CXCL12) Is Upregulated in the Ischemic Penumbra Following Stroke: Association with Bone Marrow Cell Homing to Injury. J. Neuropathol. Exp. Neurol. 2004, 63, 84–96. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bang, O.Y.; Kim, E.H.; Cha, J.M.; Moon, G.J. Adult Stem Cell Therapy for Stroke: Challenges and Progress. J. Stroke 2016, 18, 256–266. [Google Scholar] [CrossRef] [PubMed]
- Narbonne, P. The effect of age on stem cell function and utility for therapy. Cell Med. 2018, 10, 2155179018773756. [Google Scholar] [CrossRef] [Green Version]
- Romine, J.; Gao, X.; Xu, X.-M.; So, K.F.; Chen, J. The proliferation of amplifying neural progenitor cells is impaired in the aging brain and restored by the mTOR pathway activation. Neurobiol. Aging 2015, 36, 1716–1726. [Google Scholar] [CrossRef] [PubMed]
- Caplan, A.I. Why are MSCs therapeutic? New data: New insight. J. Pathol. 2009, 217, 318–324. [Google Scholar] [CrossRef] [PubMed]
- Manganas, L.N.; Zhang, X.; Li, Y.; Hazel, R.D.; Smith, S.D.; Wagshul, M.E.; Henn, F.; Benveniste, H.; Djurić, P.M.; Enikolopov, G.; et al. Magnetic Resonance Spectroscopy Identifies Neural Progenitor Cells in the Live Human Brain. Science 2007, 318, 980–985. [Google Scholar] [CrossRef] [Green Version]
- Burke, D.T.; Al-Adawi, S.; Bell, R.B.; Easley, K.; Chen, S.; Burke, D.P. Effect of Body Mass Index on Stroke Rehabilitation. Arch. Phys. Med. Rehabil. 2014, 95, 1055–1059. [Google Scholar] [CrossRef] [PubMed]
- Oesch, L.; Tatlisumak, T.; Arnold, M.; Sarikaya, H. Obesity paradox in stroke—Myth or reality? A systematic review. PLoS ONE 2017, 12, e0171334. [Google Scholar] [CrossRef]
- Kalichman, L.; Alperovitch-Najenson, D.; Treger, I. The impact of patient’s weight on post-stroke rehabilitation. Disabil. Rehabil. 2015, 38, 1684–1690. [Google Scholar] [CrossRef] [PubMed]
- Freeman, C.; Blough, A.; Rotich, D.; Curl, A.; Eickmeyer, S.M. The obesity paradox may not lead to functional gains in stroke patients undergoing acute inpatient rehabilitation. PM R. 2021. [Google Scholar] [CrossRef]
- Huang, S.-L.; Chen, B.-B.; Hsueh, I.-P.; Jeng, J.-S.; Koh, C.-L.; Hsieh, C.-L. Prediction of lower extremity motor recovery in persons with severe lower extremity paresis after stroke. Brain Inj. 2018, 32, 627–633. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).