Abstract
We present the case of a 26-year-old, otherwise healthy female patient who attended dermatology outpatient clinic due to a reddish, asymptomatic plaque located on the midline of the tongue. Dermoscopic examination revealed an area of small, atrophic filiform papillae. Based on clinical and dermoscopic features, median rhomboid glossitis (MRG) was suspected. Histopathological analysis confirmed the diagnosis.
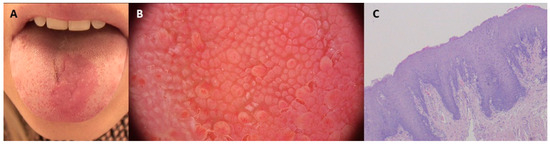
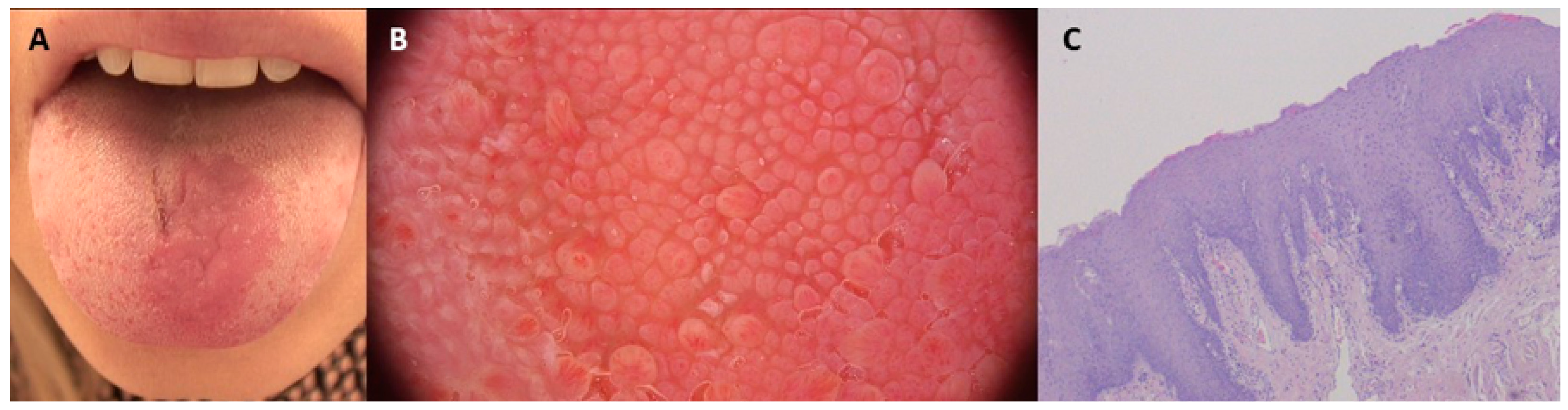
Figure 1.
A 26-year-old otherwise-healthy woman presented with an asymptomatic, well-demarcated erythematous area on the dorsum of the tongue (A). On dermoscopy, we observed an area in which small, atrophic filiform papillae were observed, different from the normal surrounding tissue (FotoFinder, Vexia Medicam 800 HD; magnification 20×) (B). Based on the clinical and dermoscopic presentation, median rhomboid glossitis (MRG) was suspected. Both direct examination and culture were negative. Microscopically, stratified squamous epithelium flattened on the surface with some acanthosis, without visible cellular atypia, and sparse lymphocytic infiltrates in the adjacent lamina propria, were observed with surrounding tissue of normal appearance. Histopathological evaluation confirmed the diagnosis of MRG (C). According to data from the literature, the prevalence of MRG ranges from 0.01% to approximately 2.4%, with adult cohorts accounting for between 0.5% and 1%. The prevalence in children is notably lower, at around 0.14% [1,2,3]. MRG typically manifests as a reddish, flat, rhomboid macule or plaque located medially on the dorsum of the tongue. In most cases it is diagnosed based on the clinical presentation. Less commonly it may present as a tumor or in a paramedial location, in which cases it may pose diagnostic difficulties. Differential diagnosis includes atrophic candidiasis, iron deficiency anemia, vitamin B12 deficiency anemia, hemangioma, pyogenic granuloma, Kaposi sarcoma, squamous cell carcinoma, erythroplakia, amyloidosis, or a granular cell tumor [4,5]. The etiology of MRG is not completely understood. Some authors consider this entity to be a subtype of oral candidiasis, while others have suggested an embryological, inflammatory, or autoimmune origin. In the presented case the results of mycological examination and culture were negative (but false negative results cannot be excluded). MRG is associated with good prognosis. In most cases it is asymptomatic, and thus requires no treatment [4]. Coexistence of a corresponding inflammatory area on the palate called candidal infection of the tongue and non-specific inflammation of the palate (CIT-NIP) requires the exclusion of immunodeficiency [5]. Reports in the literature concerning the significance of dermoscopy in the diagnosis of tongue diseases are scant [6,7,8]. The sensitivity and specificity of our observations remain to be elucidated in future studies.
Figure 1.
A 26-year-old otherwise-healthy woman presented with an asymptomatic, well-demarcated erythematous area on the dorsum of the tongue (A). On dermoscopy, we observed an area in which small, atrophic filiform papillae were observed, different from the normal surrounding tissue (FotoFinder, Vexia Medicam 800 HD; magnification 20×) (B). Based on the clinical and dermoscopic presentation, median rhomboid glossitis (MRG) was suspected. Both direct examination and culture were negative. Microscopically, stratified squamous epithelium flattened on the surface with some acanthosis, without visible cellular atypia, and sparse lymphocytic infiltrates in the adjacent lamina propria, were observed with surrounding tissue of normal appearance. Histopathological evaluation confirmed the diagnosis of MRG (C). According to data from the literature, the prevalence of MRG ranges from 0.01% to approximately 2.4%, with adult cohorts accounting for between 0.5% and 1%. The prevalence in children is notably lower, at around 0.14% [1,2,3]. MRG typically manifests as a reddish, flat, rhomboid macule or plaque located medially on the dorsum of the tongue. In most cases it is diagnosed based on the clinical presentation. Less commonly it may present as a tumor or in a paramedial location, in which cases it may pose diagnostic difficulties. Differential diagnosis includes atrophic candidiasis, iron deficiency anemia, vitamin B12 deficiency anemia, hemangioma, pyogenic granuloma, Kaposi sarcoma, squamous cell carcinoma, erythroplakia, amyloidosis, or a granular cell tumor [4,5]. The etiology of MRG is not completely understood. Some authors consider this entity to be a subtype of oral candidiasis, while others have suggested an embryological, inflammatory, or autoimmune origin. In the presented case the results of mycological examination and culture were negative (but false negative results cannot be excluded). MRG is associated with good prognosis. In most cases it is asymptomatic, and thus requires no treatment [4]. Coexistence of a corresponding inflammatory area on the palate called candidal infection of the tongue and non-specific inflammation of the palate (CIT-NIP) requires the exclusion of immunodeficiency [5]. Reports in the literature concerning the significance of dermoscopy in the diagnosis of tongue diseases are scant [6,7,8]. The sensitivity and specificity of our observations remain to be elucidated in future studies.
Author Contributions
M.S. (Martyna Sławińska)—Conceptualization, data curation, writing—original draft preparation; W.B.—histopathological figures preparation & review; B.Z.—writing—review & editing, submission of manuscript; M.S. (Michał Sobjanek)—investigation & supervision. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not Applicable.
Informed Consent Statement
Verbal consent has been obtained from the patient to publish this paper. The rationale for utilizing verbal consent is that the patient was lost from the follow-up, and contact with the patient to provide the written consent at the time of writing the paper was not possible.
Data Availability Statement
Not Applicable. No new data were created or analyzed in this study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Yarom, N.; Cantony, U.; Gorsky, M. Prevalence of fissured tongue, geographic tongue and median rhomboid glossitis among Israeli adults of different ethnic origins. Dermatology 2004, 209, 88–94. [Google Scholar] [CrossRef] [PubMed]
- Gawre, S.R.; Sonar, P.R.; Reche, A.; Tiwari, A.V.; Arya, A.; Singh, A. Median Rhomboid Glossitis: A Case Study. Cureus 2024, 16, e6118. [Google Scholar] [CrossRef] [PubMed]
- Redman, R.S. Prevalence of geographic tongue, fissured tongue, median rhomboid glossitis, and hairy tongue among 3,611 Minnesota schoolchildren. Oral. Surg. Oral. Med. Oral. Pathol. 1970, 30, 390–395. [Google Scholar] [CrossRef] [PubMed]
- Rogers, R.S.; Bruce, A. The tongue in clinical diagnosis. J. Eur. Acad. Dermatol. Venereol. 2004, 18, 254–259. [Google Scholar] [CrossRef] [PubMed]
- Lago-Méndez, L.; Blanco-Carrión, A.; Diniz-Freitas, M.; Gándara-Vila, P.; García-García, A.; Gándara-Rey, J.M. Rhomboid glossitis in atypical location: Case report and differential diagnosis. Med. Oral. Patol. Oral. Cir. Bucal 2005, 10, 123–127. [Google Scholar] [PubMed]
- Jha, A.K.; Zeeshan, M.D.; Jha Amar, A.K. Mucoscopy in lingual varicosities. Dermatol. Pract. Concept. 2018, 8, 54–55. [Google Scholar] [CrossRef] [PubMed]
- Sonthalia, S.; Varma, S.; Jha, A.K.; Jakhar, D.; Kaliyadan, F. Case Report: Dermoscopic features of oral lichen planus—The evolution of mucoscopy. F1000Res 2018, 7, 284. [Google Scholar] [CrossRef] [PubMed]
- Rather, S.; Shah, A.A.; Shah, F.Y.; Bhat, M.A.; Reyaz, S.; Hassan, I. Dermoscopy of Oral Mucosal Lesions: Experience from a Tertiary Care Center in North India and Review of Literature. Indian Dermatol. Online J. 2022, 13, 346–360. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
