Abstract
Background: To compare the diagnostic characteristics between arterial phase imaging versus portal venous phase imaging, applying polychromatic T3D images and low keV virtual monochromatic images using a 1st generation photon-counting CT detector, of CT in patients with hepatocellular carcinoma (HCC). Methods: Consecutive patients with HCC, with a clinical indication for CT imaging, were prospectively enrolled. Virtual monoenergetic images (VMI) were reconstructed at 40 to 70 keV for the PCD-CT. Two independent, blinded radiologists counted all hepatic lesions and quantified their size. The lesion-to-background ratio was quantified for both phases. SNR and CNR were determined for T3D and low VMI images; non-parametric statistics were used. Results: Among 49 oncologic patients (mean age 66.9 ± 11.2 years, eight females), HCC was detected in both arterial and portal venous scans. The signal-to-noise ratio, the CNR liver-to-muscle, the CNR tumor-to-liver, and CNR tumor-to-muscle were 6.58 ± 2.86, 1.40 ± 0.42, 1.13 ± 0.49, and 1.53 ± 0.76 in the arterial phase and 5.93 ± 2.97, 1.73 ± 0.38, 0.79 ± 0.30, and 1.36 ± 0.60 in the portal venous phase with PCD-CT, respectively. There was no significant difference in SNR between the arterial and portal venous phases, including between “T3D” and low keV images (p > 0.05). CNRtumor-to-liver differed significantly between arterial and portal venous contrast phases (p < 0.005) for both “T3D” and all reconstructed keV levels. CNRliver-to-muscle and CNRtumor-to-muscle did not differ in either the arterial or portal venous contrast phases. CNRtumor-to-liver increased in the arterial contrast phase with lower keV in addition to SD. In the portal venous contrast phase, CNRtumor-to-liver decreased with lower keV; whereas, CNRtumor-to-muscle increased with lower keV in both arterial and portal venous contrast phases. CTDI and DLP mean values for the arterial upper abdomen phase were 9.03 ± 3.59 and 275 ± 133, respectively. CTDI and DLP mean values for the abdominal portal venous phase were 8.75 ± 2.99 and 448 ± 157 with PCD-CT, respectively. No statistically significant differences were found concerning the inter-reader agreement for any of the (calculated) keV levels in either the arterial or portal-venous contrast phases. Conclusions: The arterial contrast phase imaging provides higher lesion-to-background ratios of HCC lesions using a PCD-CT; especially, at 40 keV. However, the difference was not subjectively perceived as significant.
1. Introduction
Dual-phase or even three-phase contrast-enhanced liver CT examination protocols have already been recommended decades ago in order to more accurately detect primary or secondary lesions—smaller, hyper-vascularized in particular—otherwise expected to be missed in the portal venous contrast phase (pv-phase); the latter, being the most frequently used contrast phase in abdominal imaging (“FDA Public Health Notification: Reducing Radiation Risk from Computed Tomography for Pediatric and Small Adult Patients,” 2002; Huda et al., 2000; Kalra et al., 2004; McCollough et al., 2006; Papadakis et al., 2007) [1,2,3,4,5]. This knowledge still has its plausibility, but it was propagated mainly in earlier times while using less performant CT scanners (slower table speed, longer reconstruction times, longer detector cooling time, etc.). Nevertheless, some malignant tumors such as hepatocellular carcinomas, neuroendocrine tumors, sarcomas, and even some of the most frequent malignancies such as breast, lung or GI, and GU malignant neoplasm may enhance early so that the contrast blush fades away seconds after hampering lesion detection if only pv-phases are used (Higashigaito et al., 2022; Hsieh et al., 2021; Rajendran et al., 2022; Tabatabaei et al., 2020; Wichmann et al., 2017) [6,7,8,9,10]. In the last ten years, with the advent of dual-energy CT detectors, lesion detection was generally improved by using virtual monoenergetic images with lower keV (virtual mono-contrast) images (Shuman et al., 2014a; Yamada et al., 2014) [11,12]. Besides, known physiological differences in liver and liver lesion perfusion are still expected; which, depend on the blood supply to both tissues (via the hepatic artery or the portal vein, or both), their microarchitecture, size of the extravascular, interstitial space, tumor flow characteristics and such that are protocol-dependent (contrast agent volume, contrast medium concentration, flow, volume of saline chaser, circulation time, etc.), differences in the attenuation, and delineation between the lesion and the liver parenchyma. However, they have to be enhanced by improving tissue contrast. In addition to liver lesion imaging, multiple dual-energy—and virtual monoenergetic image reconstruction—applications exist in the literature. Examples of applications here include imaging of the coronary arteries, detection of intra-abdominal hemorrhage, and CT angiography of the carotid and intracerebral vessels [13,14,15,16,17,18].
With the advent of the photon-counting detector CT, each individual X-ray that passes through the patient’s body is directly converted by incoming photons into electronic signals proportional to their deposited energy being immune to electronic noise [19,20,21,22,23]. The count rate is not affected by electronic noise. These properties have the potential for more accurate lesion delineation and increased tissue contrast. Moreover, using low keV for the generation of virtual mono-contrast images, enhancement characteristics (peripheral vs. central, diffuse vs. focal, heterogeneity of microvasculature) are expected to be further enhanced improving the detection of focal hepatic lesions.
Encouraged by these assumptions, we initiated a prospective comparative (arterial vs. portal venous) study in patients with follow-up for hepatocellular carcinomas, with the intention to compare the sensitivity of portal venous monophasic polychromatic T3D PCD-CT images with those of a combined arterial and portal venous dual-phase contrast-enhanced PCD-CT examinational protocol for the detection of hepatocellular carcinomas in the liver, and additionally, to assess the eventual benefit of complementary virtual mono-contrast 40–70 KeV reformates over the primarily generated T3D images. For this purpose, we evaluated differences in terms of SNR, CNR, as well as an inter-reader agreement for all images generated.
2. Materials and Methods
2.1. Subjects
Our institutional review board approved this prospective data evaluation, which was assigned the approval number 696/2021B01. Participants gave written informed consent. Between October 2021 and July 2022, a total of 49 consecutive patients with known hepatocellular carcinoma, who were referred for staging or treatment monitoring to our radiology department and who had standardized previous CT exams or MRI exams to confirm the HCC suspicious lesions at our institution, were enrolled.
2.2. CT-Examinational Protocol on PCD-CT
*Arterial phase: scans were all acquired on a 1st generation photon-counting detector CT with quantum imaging (NAEOTOM Alpha, Siemens Healthineers, Forchheim, Germany) equipped with two photon-counting detectors. The following examinational protocol was used: 120 KvP, eff. mAs 144, quantum iterative reconstruction factor 2 (QIR 2), level 145, slice thickness 3 mm, focal spot 0.8/1.2, kernel Br40f, single collimation width 0.4 mm, total collimation width 57.6 mm, table speed 92 cm/s, table feed/rotation 46, and spiral pitch factor 0.8.
*Portal venous phase: 120 KvP, eff. mAs 148, quantum iterative reconstruction factor 2 (QIR 2), level 145, slice thickness 3 mm, focal spot 0.8/1.2, kernel Br40f, single collimation width 0.4 mm, total collimation width 57.6 mm, table speed 92 cm/s, table feed/rotation 46, and spiral pitch factor 0.8.
2.3. Contrast Agent Protocol
The contrast medium protocol included intravenous administration of 1.2 mL/kg/BW (IMERON 350 mg iodine/mL [BRACCO Imaging, Konstanz, Germany]) at a flow rate of 2 mL/s via antecubital vein followed by a saline flush of 50 mL NaCl at 2.5 mL/s for both phases and in all patients. Contrast material was administered by using a dual-head pump injector (CT motion XD 8000, Ulrich Medical, Ulm, Germany). The delay between contrast agent injection and the scan was 30 s for the arterial phase and 65 s for the portal venous phase for PCD-CT.
2.4. Image Reconstructions
PCD-CT was performed at 120 kVp in QuantumPlus mode (obtaining full spectral information) and polychromatic T3D images were generated. Slice thickness was 3 mm for both series; single slice collimation was 0.4 mm. The kernel was set at Br40f for both phases with quantum iterative reconstruction factor 2 (QIR 2). The spiral pitch factor was 0.8. Virtual monoenergetic images (VMI) were reconstructed at 40 to 70 keV for the PCD-CT (Figure 1).
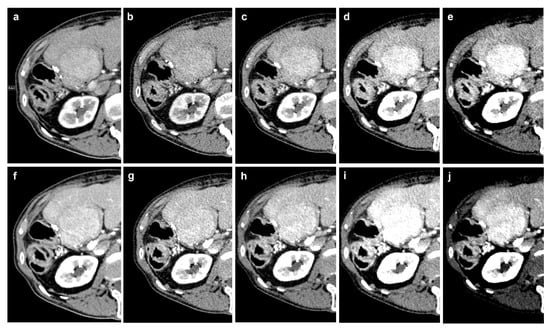
Figure 1.
Example of the different reconstructions in an HCC lesion: (a–e): arterial phase imaging (T3D, 70 keV, 60 keV, 50 keV, 40 keV); (f–j) portal venous imaging (T3D, 70 keV, 60 keV, 50 keV, 40 keV).
2.5. Subjective Image Analysis
VMI arterial and portal venous abdominal CT images were read in consensus by two radiologists with 5 and 4 years of experience in abdominal imaging. Images were randomly analyzed (arterial and portal venous, timely apart from each other) with freely adjustable window settings. Subjective image contrast and image noise were evaluated by using a five-point Likert scale: 1, excellent image quality; 2, good image quality; 3, fair but comprised image quality; 4, poor image quality; 5, non-diagnostic. Disagreements were resolved during a final consensus round.
2.6. Objective Image Analysis
All lesions were counted and registered. The maximum diameter was measured. In each patient, round or oval ROIs were manually placed twice within the liver (ROI size, 100–200 mm2), once within the lesion (40–100 mm2), once within the portal vein (30–60 mm2), and twice within the psoas muscle (40–100 mm2) depending on their size.
2.7. Quantitative Evaluation of Image Quality and Noise
In every patient, one index lesion was defined and considered for the following calculations. Signal-to-noise ratios (SNR) of the liver lesions were calculated as follows: SNR = (HUROI)/SDROIliver. The contrast-to-noise ratio (CNR) for the liver-to-muscle, tumor-to-liver, and tumor-to-muscle ratios was calculated as follows: CNRliver-to-muscle = (mean HU of ROIliver/mean HU of ROImuscle); CNRtumor-to-liver = (mean HU of ROIlesion/mean HU of ROIliver); CNRtumor-to-muscle = (mean HU of ROIlesion/mean HU of ROImuscle).
Image noise was defined as the standard deviation (SD) of the psoas muscle (SDmuscle). All ratios were performed between 40 and 70 keV at the arterial and portal venous phases in PCD-CT and for the T3D images at the arterial and portal venous phases.
2.8. Radiation Metrics
In all patients, the volumetric CT dose index (CTDIvol) and dose-length product (DLP) were documented from the dose report; which, was automatically stored in the picture archiving and communication system. Subsequently, the absolute values were compared between both contrast phases.
2.9. Statistical Analysis
Data analysis was performed using IBM SPSS Statistics for Windows, Version 26.0 (IBM Corp., Armonk, NY, USA). The level of significance was set at α = 0.05. Continuous variables are provided as mean ± standard deviation (95% confidence interval). Normal data distribution was assessed by applying the Shapiro–Wilk test. In the case of normal distribution, the variables of the two groups were compared according to the t-test for pairs. The Wilcoxon signed-rank paired test was used if data were not normally distributed. Comparison between the different keV levels of the PCD-CT was compared with the Friedman test, followed by post hoc Dunn–Bonferroni tests with alpha correction to analyze differences between the subgroups, if necessary.
3. Results
3.1. Patient Characteristics
A total of 49 patients (41 male, 66.9 ± 11.2 years) were included. Of them, 94% (n = 46) had a previous MRI for validation of the liver lesions with a mean time difference of 4.6 months (SD ± 3.4 months) (Table 1). The remaining three had only a multiphase dual-source CT (DSCT).

Table 1.
Patient characteristics.
3.2. Clinical Evaluation
Overall, between one and >10 hepatic HCC lesions were found in patients in the current study using PCD-CT. There was no statistically significant difference between arterial and portal venous contrast phases in detecting tumor manifestations (see Table 2); none of the arterialized liver lesions were missed in the portal venous contrast phase. The arterial contrast phase showed no clinical benefit in terms of the detectability of hepatocellular carcinoma manifestations.

Table 2.
The number of delineable lesions in the arterial and portal venous contrast phases, sorted by number.
3.3. Arterial vs. Portal Venous Contrast Phase
In terms of objective image quality, we found that the “liver-to-muscle” contrast-to-noise ratio and the “tumor-to-liver” CNR differed significantly between arterial and portal venous contrast phases in PCD-CT (p < 0.005). The signal-to-noise and contrast-to-noise ratios of “tumor-to-muscle” did not differ significantly (p = 0.416 and 0.366, respectively, see Table 3).

Table 3.
SNR and CNR of low-energy threshold images (T3D). SNR: signal-to-noise ratio; CNR: contrast-to-noise ratio; art-phase: arterial upper abdomen phase; pv-phase: portal venous abdominal phase.
Evaluation of Calculated Low keV Images
In terms of the signal-to-noise ratio, there was no statistically significant difference between “T3D” and the respective (low) keV levels; neither for arterial nor portal venous (p > 0.05, see Figure 2 and Table 4). In addition, the “liver-to-muscle” contrast-to-noise ratio, the “tumor-to-liver” CNR, and the “tumor-to-muscle” CNR did not differ with regard to SNR in either the arterial or portal venous contrast phases. The “liver-to-muscle” CNR increased in both arterial and portal venous contrast phases; whereas, the keV decreased while the standard deviation increased. There were statistically significant differences in terms of the CNRtumor-to-liver when comparing arterial to portal venous phases through all reconstructions (T3D to 40 keV, see Table 5). Image noise, which was determined using the standard deviation of the psoas muscle, did not differ between arterial and portal venous contrast phases (Table 6).
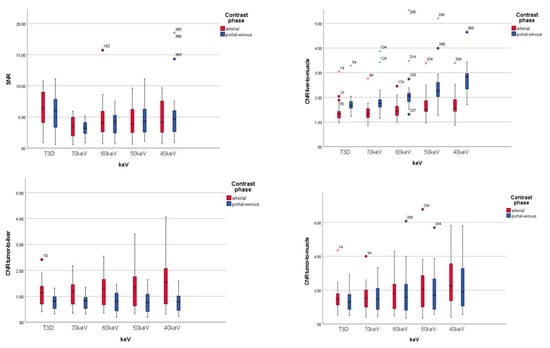
Figure 2.
Comparison of different keV levels in terms of SNR and CNR.

Table 4.
Comparison of SNR of arterial and portal venous phases.

Table 5.
Comparison of CNRtumor-to-liver of arterial and portal venous phases.

Table 6.
Image noise (standard deviation of the psoas muscle).
The “tumor-to-liver” CNR increased in the arterial contrast phase with a lower keV whereas, the standard deviation increased sharply. With respect to the portal venous contrast phase, “tumor-to-liver” CNR decreased when the keV value was decreased.
The “tumor-to-muscle” CNR increased when the keV value was reduced for both arterial and portal venous contrast phases.
The Friedmann test revealed a value of <0.001 with regard to the SNR of both the arterial and portal venous reconstructions; thus, the central tendencies differ with regard to SNR. We found a statistically significant difference between T3D and 70 keV after Bonferroni alpha correction in both arterial and portal venous contrast phases (Table 7 and Table 8).

Table 7.
Comparison of arterial SNR between T3D and low keV images.

Table 8.
Comparison of portal venous SNR between T3D and low keV images.
In terms of the arterial contrast phase CNRliver-to-muscle, we only found a statistically significant difference in the comparison of T3D and 40 keV after Bonferroni alpha correction (Table 9).

Table 9.
Comparison of arterial CNRliver-to-muscle between T3D and low keV images.
In terms of the portal venous contrast phase CNRliver-to-muscle, we found statistically significant differences in the comparison of T3D and 60/50/40 keV as well as 70 keV and 50/40 keV after Bonferroni alpha correction (Table 10).

Table 10.
Comparison of portal venous CNRliver-to-muscle between T3D and low keV images.
We did not find any statistically significant differences in terms of arterial or portal-venous CNRtumor-to-liver (Table 11 and Table 12).

Table 11.
Comparison of arterial CNRtumor-to-liver between T3D and low keV images.

Table 12.
Comparison of portal venous CNRtumor-to-liver between T3D and low keV images.
Additionally, we did not find any statistically significant differences in terms of arterial CNRtumor-to-muscle (Table 13).

Table 13.
Comparison of arterial CNRtumor-to-muscle between T3D and low keV images.
After Bonferroni alpha correction, we found statistically significant differences comparing T3D and 50/40 keV as well as comparing 70 keV with 40 keV (Table 14).

Table 14.
Comparison of portal venous CNRtumor-to-muscle between T3D and low keV images.
3.4. Inter-Reader Evaluation of Low keV Images and Contrast Phase
Regarding agreement between readers, no statistically significant differences were found. There was no significant difference between the two readers for any of the (calculated) keV levels in either the arterial or portal venous contrast phases (Table 15).

Table 15.
Data are presented as median qualitative image analysis scores; data in parentheses are interquartile ranges.
3.5. Dose Evaluation
For PCD-CT, performing an additional arterial upper abdominal phase to the standard portal venous abdominal phase results in a 51% increase in the computed tomography dose index (CTDI) and a 38% increase in the dose-length product (DLP) (Table 16, Figure 3 and Figure 4).

Table 16.
Art-phase: arterial upper abdomen phase; pv-phase: portal venous abdominal phase (including also the pelvic region); CTDI: computed tomography dose index; DLP: dose-length product; SD: standard deviation.
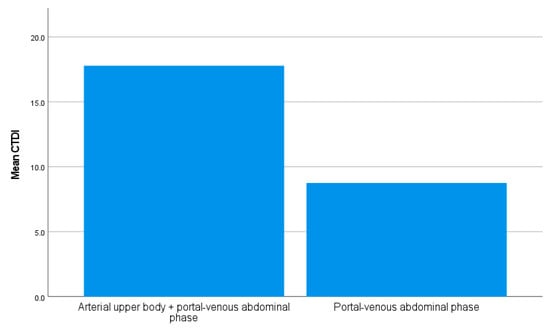
Figure 3.
The mean computed tomography dose index (CTDI) can be reduced by 51% if the arterial contrast phase is omitted.
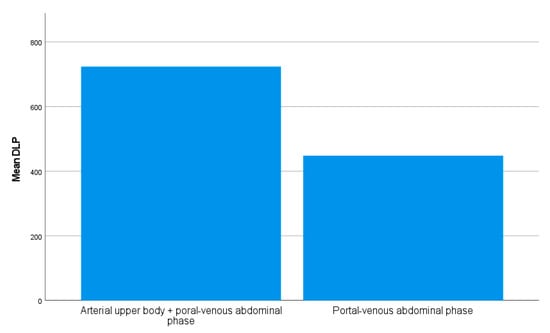
Figure 4.
The mean dose-length product (DLP) can be reduced by 38% if the arterial contrast phase is omitted or even more if the pelvic region is not included in the examination area.
4. Discussion
According to our results, the portal venous contrast phase, performed on a 1st generation PCD-CT in patients with hepatocellular carcinomas, yielded similar results with the arterial contrast phase; thus, holding potential for the reduction in radiation dose. Interestingly, the use of virtual monochromatic 40–70 keV images also did not really outperform the results of polychromatic T3D images, which potentially makes redundant the time-consuming post-processing of different sets of VMI. Hence, we found no significant difference in SNR between the arterial and portal venous phases, including between “T3D” and low keV images. Notably, the tumor-to-liver CNR was found to be significantly different between the arterial and portal venous contrast phases, but not between polychromatic “T3D” and low keV VMI. Expectedly, we found an increase in tumor-to-liver CNR, but also in SD in the arterial contrast phase at lower keV; whereas in the portal venous contrast phase, the tumor-to-liver CNR decreased at lower keV and concomitantly, the tumor-to-muscle CNR increased at lower keV in both arterial and portal venous contrast phases. This is in line with previously published results concerning image CNR [6]. There was no significant difference in SNR in the arterial contrast phase between T3D and low keV VMI, unlike in the portal venous contrast phase at 40 keV. The other keV levels yielded no significant difference over T3D.
Notably, the inter-reader agreement was good for most of the image readings. For this study, we used a standardized biphasic contrast-enhanced liver protocol where the applied energy as well as all other examinational parameters were kept comparable between the two phases. The arterial phase started at 30 s, whereas the portal venous phase started at 65 s. All liver lesions (100.0%) were detected in both the arterial phase and the portal venous phase by a mean lesion size of 4.2 ± 2.3 cm.
In this given clinical setting, the rationale for multiphasic contrast CT protocols is to improve the detection of hyper-vascular liver lesions; this topic has been intensively debated in the last two decades, advocating the role of an additional arterial contrast phase in patients presenting hyper-vascular tumors. Knowingly, the liver is supplied with blood from the portal vein to 70–80%; whereas, the bile ducts are supplied with blood from the hepatic artery. Most hepatic tumors are either exclusively or preponderantly supplied with arterial blood. Defining lesion conspicuity as the difference between lesion enhancement and parenchymal enhancement underlines the role of multiphasic studies. Based on this knowledge, timely separation of the dual blood supply would have the benefit of a higher lesion-to-liver ratio in the arterial phase, eventually coupled with a lower lesion-to-liver ratio in the portal venous phase. However, angiographic studies have shown that the portal venous phase already begins 5–6 s after contrast material injection in the celiac or splenic artery. This data suggest that with slower scanners, as used in the past, the arterial dominant phase already included some portal venous “contamination” affecting the results [24]. Frederick et al. suggest that the arterial phase is completed in 44 s, and that therefore, the detection of hyper-vascular lesions could be compromised if image acquisition lasts longer [24]. However, Winkler et al. could not find any additional liver metastases from malignant melanoma in their cohort comparing the arterial (40 s delay) with the portal venous contrast phase (70 s delay) [25]. These authors described a higher challenge in the detection of benign, primarily hepatic, lesions like adenoma and focal nodular hyperplasia; presumably, due to their greater histologic resemblance with the liver parenchyma. Mitsuzaki et al. reported improvement in the detection of smaller hepatocellular carcinomas by performing an additional arterial phase [26]. However, in their study, these authors reported a time-to-peak in the aorta of 36 s, and 90 s for the liver. With more rapid scanners, these delay times are expected to be significantly shorter, and the protocol used in our study comprised a shorter delay time for the portal venous phase (65 s) which corresponds to a late capillary/early portal venous enhancement phase. For hyper-vascular tumors, the lesion-to-liver ratio is expected to fall significantly from the arterial phase to the portal venous phase, eventually becoming negative in the latter.
In recent years, with the increasing use of dual-energy technology, the optimization of tissue contrast became possible by using virtual mono-contrast images obtained at low keV [27,28]. In a similar approach, the use of a frequency-selective nonlinear blending algorithm significantly improved tissue contrast [29]. The approval of a 1st generation photon-counting detector CT has given an additional impetus to assess its strengths and limits resulting from the more efficient exploitation of the spectral information. Eliminating electronic noise, the PCD-CT increases lesion delineation, and by means of reading virtual mono-contrast images at lower keV, also increases the tissue contrast that is supposed to be beneficial for lesion depiction. Hence, using technological advancement, requirements that are considered mandatory such as multiphasic contrast protocols could be disputed again.
At this point, the emerging CT technique called photon-counting detector CT could be used for the purpose of dose reduction by maintaining image quality. The main difference between a conventional energy-integrating detector CT and a PCD-CT is that the former uses indirect conversion technology, with a layer of scintillators converting X-ray photons into visible light which are consequently detected by a photodiode and converted into electronic signals, whereas the latter directedly converses X-ray photons into electron–hole pairs by using a semiconductor detector material with a better electron yield. Electronic noise is usually detected as a low-amplitude signal, and thus by setting the low-energy threshold to be slightly higher than the energy level associated with the electronic noise signal amplitude, electronic noise can be excluded readily from the measured count data.
Low-energy threshold images (referred to as T3D by the manufacturer) were developed as a surrogate of classical polychromatic 120 KVP images including photon energies from 20 keV to 120 keV. The way in which these polychromatic energies are weighed increases image contrast, which proved superior to classical 120 KVP; which again, seems to explain, in addition, the lesser impact of low keV images over T3D in our study compared to previous reports [11,30,31].
Our study has some limitations. First, it is just a preliminary study as our series does not have enough subjects for a vast statistical evaluation. Second, the standard of care, which in this case was MRI and CT follow-up, was performed within a time window that theoretically might have changed the number of lesions detectable by CT as compared to MRI. Third, this study does not intend to question the benefit of multiphasic imaging protocols generally. For many clinical questions, e.g., while dealing with the assessment of treatment response or for characterization of certain tumor entities, multiphasic protocols still have their justifications. Nevertheless, a reevaluation of established examinational protocols should be taken into consideration given that image quality is rapidly improving.
In summary, the additional arterial contrast phase showed a better contrast ratio for the lesion-to-background ratio compared to the portal venous contrast phase. Especially at 40 keV, the arterial phase showed the best results for the detection of hyper-arterialized HCC lesions. However, these objective findings were not confirmed by the subjective reading of the radiologists. In light of currently tighter regulations with respect to patient dose, these preliminary results should prompt larger studies aimed at the optimization of CT examinational protocols in the era of PCD-CT.
Author Contributions
Methodology, J.W.; Validation, M.F.F.; Resources, F.T.; Writing–original draft, A.E., M.H. and F.H.; Writing–review & editing, K.N., N.V., S.O.S. and F.B. All authors have read and agreed to the published version of the manuscript.
Funding
The support from the Open Access Publication Fund of the University of Tübingen.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board of the university hospital of Tuebingen (696/2021BO1, 8 December 2021).
Informed Consent Statement
Patient consent was waived due to the retrospective nature of this study.
Data Availability Statement
Data is contained within the article.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
CNR: contrast-to-noise ratio; studies: volumetric CT dose index; DLP: dose-length product; DSCT: dual-source CT; PCD-CT: photon-counting detector CT; SNR: signal-to-noise ratio.
References
- Kalra, M.K.; Maher, M.M.; Toth, T.L.; Hamberg, L.M.; Blake, M.A.; Shepard, J.-A.; Saini, S. Strategies for CT Radiation Dose Optimization. Radiology 2004, 230, 619–628. [Google Scholar] [CrossRef]
- McCollough, C.H.; Bruesewitz, M.R.; Kofler, J.M. CT Dose Reduction and Dose Management Tools: Overview of Available Options. RadioGraphics 2006, 26, 503–512. [Google Scholar] [CrossRef] [PubMed]
- Papadakis, A.E.; Perisinakis, K.; Damilakis, J. Angular on-line tube current modulation in multidetector CT examinations of children and adults: The influence of different scanning parameters on dose reduction. Med. Phys. 2007, 34, 2864–2874. [Google Scholar] [CrossRef]
- Food and Drug Administration. FDA public health notification: Reducing radiation risk from computed tomography for pediatric and small adult patients. Pediatr. Radiol. 2002, 32, 314–316. [Google Scholar] [CrossRef] [PubMed]
- Huda, W.; Scalzetti, E.M.; Levin, G. Technique Factors and Image Quality as Functions of Patient Weight at Abdominal CT. Radiology 2000, 217, 430–435. [Google Scholar] [CrossRef]
- Higashigaito, K.; Euler, A.; Eberhard, M.; Flohr, T.G.; Schmidt, B.; Alkadhi, H. Contrast-Enhanced Abdominal CT with Clinical Photon-Counting Detector CT: Assessment of Image Quality and Comparison with Energy-Integrating Detector CT. Acad. Radiol. 2021, 29, 689–697. [Google Scholar] [CrossRef]
- Rajendran, K.; Petersilka, M.; Henning, A.; Shanblatt, E.R.; Schmidt, B.; Flohr, T.G.; Ferrero, A.; Baffour, F.; Diehn, F.E.; Yu, L.; et al. First Clinical Photon-counting Detector CT System: Technical Evaluation. Radiology 2022, 303, 130–138. [Google Scholar] [CrossRef]
- Wichmann, J.L.; Hardie, A.D.; Schoepf, U.J.; Felmly, L.M.; Perry, J.D.; Varga-Szemes, A.; Mangold, S.; Caruso, D.; Canstein, C.; Vogl, T.J.; et al. Single- and dual-energy CT of the abdomen: Comparison of radiation dose and image quality of 2nd and 3rd generation dual-source CT. Eur. Radiol. 2017, 27, 642–650. [Google Scholar] [CrossRef]
- Tabatabaei, S.M.H.; Talari, H.; Gholamrezanezhad, A.; Farhood, B.; Rahimi, H.; Razzaghi, R.; Mehri, N.; Rajebi, H. A low-dose chest CT protocol for the diagnosis of COVID-19 pneumonia: A prospective study. Emerg. Radiol. 2020, 27, 607–615. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, S.S.; Leng, S.; Rajendran, K.; Tao, S.; McCollough, C.H. Photon Counting CT: Clinical Applications and Future Developments. IEEE Trans. Radiat. Plasma Med. Sci. 2020, 5, 441–452. [Google Scholar] [CrossRef]
- Shuman, W.P.; Green, D.E.; Busey, J.M.; Mitsumori, L.M.; Choi, E.; Koprowicz, K.M.; Kanal, K.M. Dual-Energy Liver CT: Effect of Monochromatic Imaging on Lesion Detection, Conspicuity, and Contrast-to-Noise Ratio of Hypervascular Lesions on Late Arterial Phase. AJR Am. J. Roentgenol. 2014, 203, 601–606. [Google Scholar] [CrossRef]
- Yamada, Y.; Jinzaki, M.; Hosokawa, T.; Tanami, Y.; Abe, T.; Kuribayashi, S. Abdominal CT: An intra-individual comparison between virtual monochromatic spectral and polychromatic 120-kVp images obtained during the same examination. Eur. J. Radiol. 2014, 83, 1715–1722. [Google Scholar] [CrossRef]
- Cicero, G.; Ascenti, G.; Albrecht, M.H.; Blandino, A.; Cavallaro, M.; D’angelo, T.; Carerj, M.L.; Vogl, T.J.; Mazziotti, S. Extra-abdominal dual-energy CT applications: A comprehensive overview. Radiol. Med. 2020, 125, 384–397. [Google Scholar] [CrossRef] [PubMed]
- Leithner, D.; Mahmoudi, S.; Wichmann, J.L.; Martin, S.S.; Lenga, L.; Albrecht, M.H.; Booz, C.; Arendt, C.T.; Beeres, M.; D’Angelo, T.; et al. Evaluation of virtual monoenergetic imaging algorithms for dual-energy carotid and intracerebral CT angiography: Effects on image quality, artefacts and diagnostic performance for the detection of stenosis. Eur. J. Radiol. 2018, 99, 111–117. [Google Scholar] [CrossRef]
- Martin, S.S.; Wichmann, J.L.; Scholtz, J.-E.; Leithner, D.; D’angelo, T.; Weyer, H.; Booz, C.; Lenga, L.; Vogl, T.J.; Albrecht, M.H. Noise-Optimized Virtual Monoenergetic Dual-Energy CT Improves Diagnostic Accuracy for the Detection of Active Arterial Bleeding of the Abdomen. J. Vasc. Interv. Radiol. 2017, 28, 1257–1266. [Google Scholar] [CrossRef]
- Lenga, L.; Albrecht, M.H.; Othman, A.E.; Martin, S.S.; Leithner, D.; D’Angelo, T.; Arendt, C.; Scholtz, J.E.; De Cecco, C.N.; Schoepf, U.J.; et al. Monoenergetic Dual-energy Computed Tomographic Imaging: Cardiothoracic Applications. J. Thorac. Imaging 2017, 32, 151–158. [Google Scholar] [CrossRef] [PubMed]
- Arendt, C.T.; Czwikla, R.; Lenga, L.; Wichmann, J.L.; Albrecht, M.H.; Booz, C.; Martin, S.S.; Leithner, D.; Tischendorf, P.; Blandino, A.; et al. Improved coronary artery contrast enhancement using noise-optimised virtual monoenergetic imaging from dual-source dual-energy computed tomography. Eur. J. Radiol. 2019, 122, 108666. [Google Scholar] [CrossRef]
- D’Angelo, T.; Cicero, G.; Mazziotti, S.; Ascenti, G.; Albrecht, M.H.; Martin, S.S.; Othman, A.E.; Vogl, T.J.; Wichmann, J.L. Dual energy computed tomography virtual monoenergetic imaging: Technique and clinical applications. Br. J. Radiol. 2019, 92, 20180546. [Google Scholar] [CrossRef] [PubMed]
- Leng, S.; Bruesewitz, M.; Tao, S.; Rajendran, K.; Halaweish, A.F.; Campeau, N.G.; Fletcher, J.G.; McCollough, C.H. Photon-counting Detector CT: System Design and Clinical Applications of an Emerging Technology. RadioGraphics 2019, 39, 729–743. [Google Scholar] [CrossRef]
- Voelker, R. Advanced CT Technology Counts Photons to Produce Sharper Images. JAMA 2021, 326, 1667. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, B.; Flohr, T. Principles and applications of dual source CT. Phys. Med. 2020, 79, 36–46. [Google Scholar] [CrossRef] [PubMed]
- Flohr, T.; Petersilka, M.; Henning, A.; Ulzheimer, S.; Ferda, J.; Schmidt, B. Photon-counting CT review. Phys. Med. 2020, 79, 126–136. [Google Scholar] [CrossRef]
- Willemink, M.J.; Persson, M.; Pourmorteza, A.; Pelc, N.J.; Fleischmann, D. Photon-counting CT: Technical Principles and Clinical Prospects. Radiology 2018, 289, 293–312. [Google Scholar] [CrossRef] [PubMed]
- Frederick, M.G.; McElaney, B.L.; Singer, A.; Park, K.S.; Paulson, E.K.; McGee, S.G.; Nelson, R.C. Timing of parenchymal enhancement on dual-phase dynamic helical CT of the liver: How long does the hepatic arterial phase predominate? AJR Am. J. Roentgenol. 1996, 166, 1305–1310. [Google Scholar] [CrossRef]
- Winkler, N.; Rezvani, M.; Heilbrun, M.; Shaaban, A. Utility of dual phase liver CT for metastatic melanoma staging and surveillance. Eur. J. Radiol. 2013, 82, 2189–2193. [Google Scholar] [CrossRef]
- Mitsuzaki, K.; Yamashita, Y.; Ogata, I.; Nishiharu, T.; Urata, J.; Takahashi, M. Multiple-phase helical CT of the liver for detecting small hepatomas in patients with liver cirrhosis: Contrast-injection protocol and optimal timing. AJR Am. J. Roentgenol. 1996, 167, 753–757. [Google Scholar] [CrossRef]
- Hokamp, N.G.; Höink, A.J.; Doerner, J.; Jordan, D.W.; Pahn, G.; Persigehl, T.; Maintz, D.; Haneder, S. Assessment of arterially hyper-enhancing liver lesions using virtual monoenergetic images from spectral detector CT: Phantom and patient experience. Abdom. Radiol. 2018, 43, 2066–2074. [Google Scholar] [CrossRef] [PubMed]
- Lenga, L.; Lange, M.; Arendt, C.T.; Booz, C.; Yel, I.; Bodelle, B.; D’Angelo, T.; Hammerstingl, R.M.; Huizinga, N.A.; Vogl, T.J.; et al. Measurement Reliability and Diagnostic Accuracy of Virtual Monoenergetic Dual-Energy CT in Patients with Colorectal Liver Metastases. Acad. Radiol. 2019, 27, e168–e175. [Google Scholar] [CrossRef]
- Bongers, M.N.; Bier, G.; Marcus, R.; Ditt, H.; Kloth, C.; Schabel, C.; Nikolaou, K.; Horger, M. Image Quality of a Novel Frequency Selective Nonlinear Blending Algorithm: An Ex Vivo Phantom Study in Comparison to Single-Energy Acquisitions and Dual-Energy Acquisitions With Monoenergetic Reconstructions. Investig. Radiol. 2016, 51, 647–654. [Google Scholar] [CrossRef] [PubMed]
- Reimer, R.P.; Hokamp, N.G.; Efferoth, A.F.; Krauskopf, A.; Zopfs, D.; Kröger, J.R.; Persigehl, T.; Maintz, D.; Bunck, A.C. Virtual monoenergetic images from spectral detector computed tomography facilitate washout assessment in arterially hyper-enhancing liver lesions. Eur. Radiol. 2021, 31, 3468–3477. [Google Scholar] [CrossRef]
- Husarik, D.B.; Gordic, S.; Desbiolles, L.; Krauss, B.; Leschka, S.; Wildermuth, S.; Alkadhi, H. Advanced virtual monoenergetic computed tomography of hyperattenuating and hypoattenuating liver lesions: Ex-vivo and patient experience in various body sizes. Investig. Radiol. 2015, 50, 695–702. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).