Analysis of Missed Skeletal Injuries Detected Using Whole-Body Bone Scan Applied to Trauma Patients: A Case–Control Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Population
2.2. Trauma Team Deployment
2.3. Admission Route
2.4. WBBS
2.5. Statistical Analysis
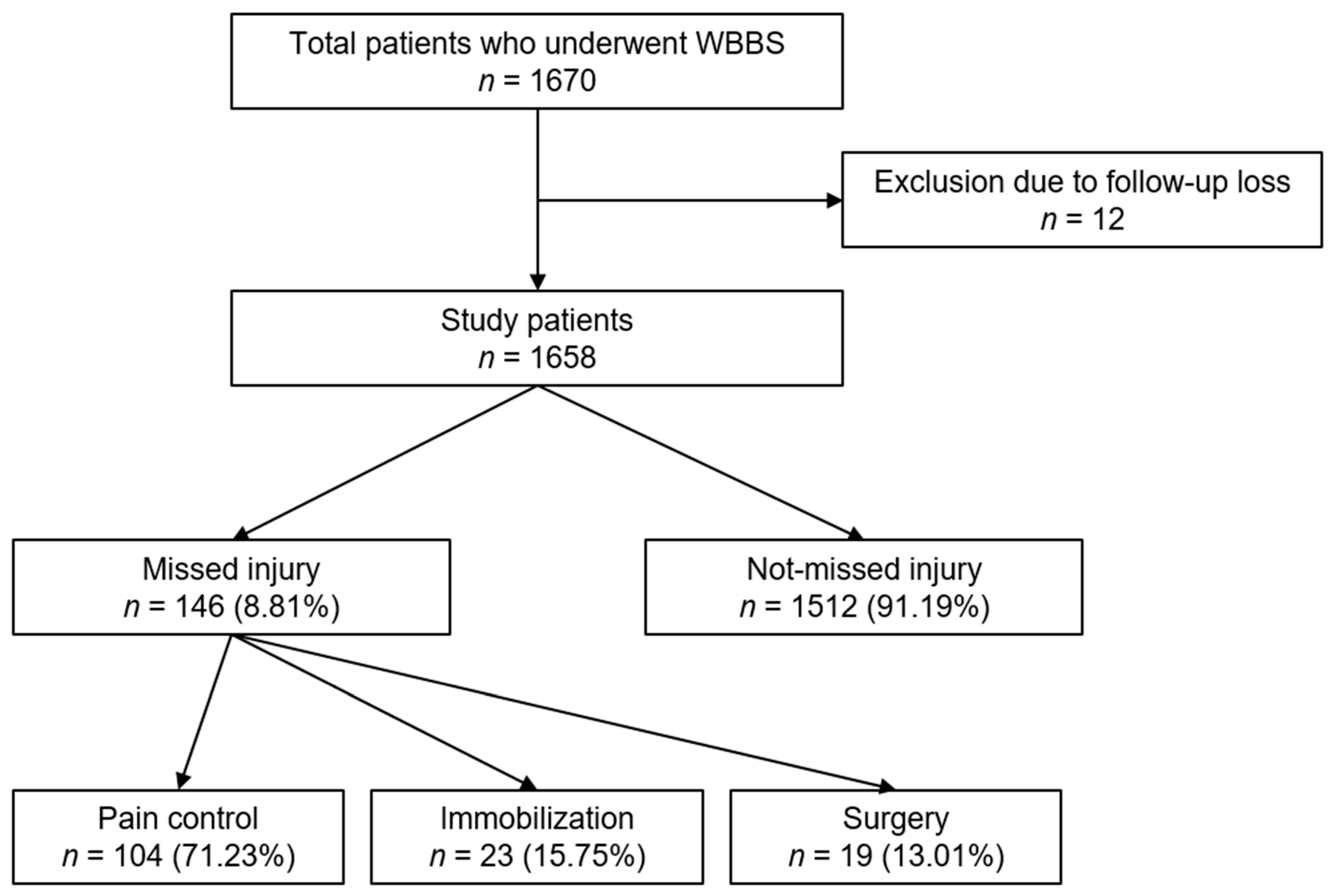
3. Results
3.1. General and Clinical Characteristics
3.2. Site of Detected Fracture and Treatment
3.3. Risk of Missing Skeletal Injuries in Patients with Multiple Traumas According to Clinical Characteristics
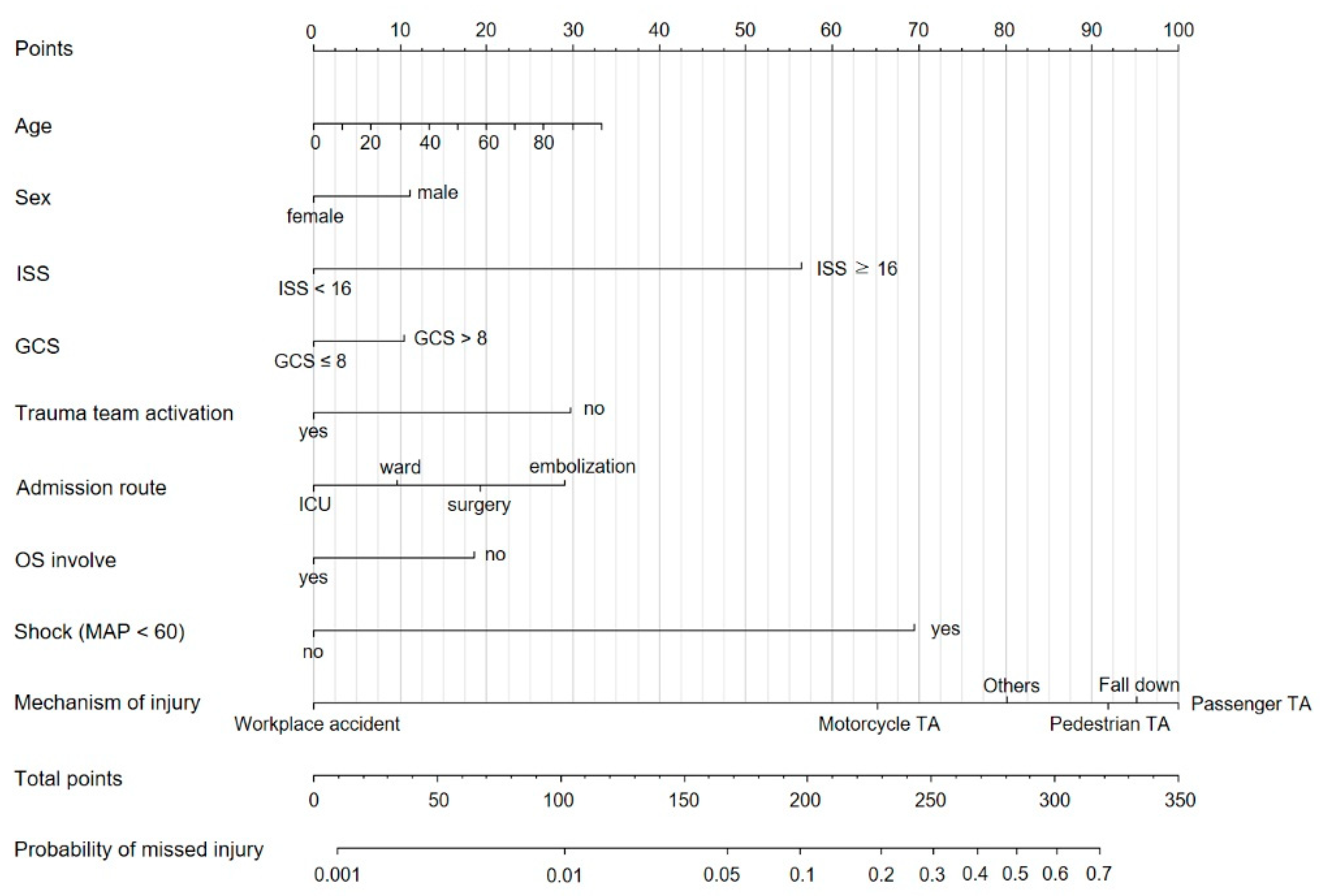
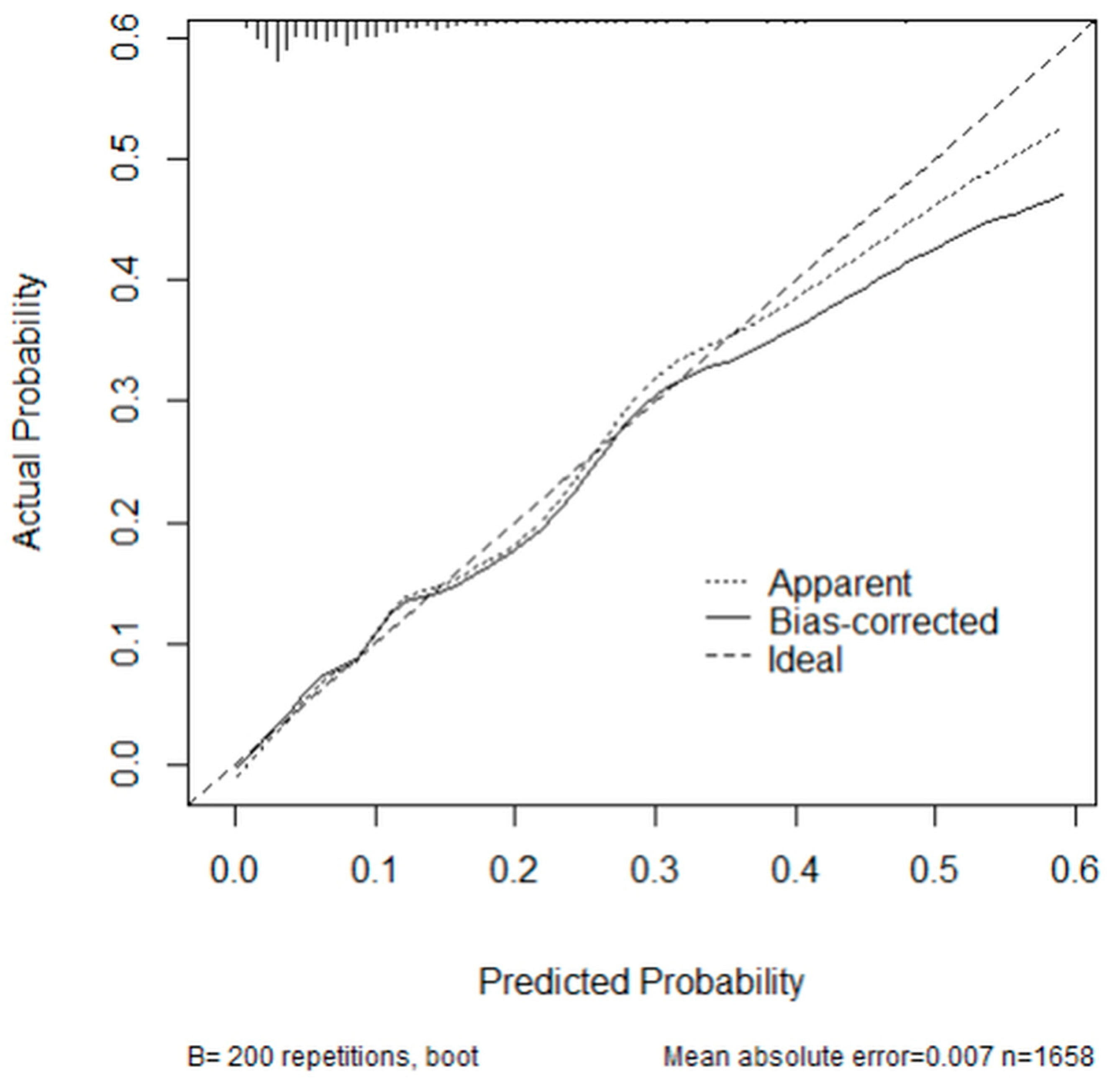
3.4. Nomogram for the Probability of Missing a Skeletal Injury
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Galvagno, S.M., Jr.; Nahmias, J.T.; Young, D.A. Advanced Trauma Life Support((R)) Update 2019: Management and Applications for Adults and Special Populations. Anesthesiol. Clin. 2019, 37, 13–32. [Google Scholar] [CrossRef]
- Enderson, B.L.; Reath, D.B.; Meadors, J.; Dallas, W.; DeBoo, J.M.; Maull, K.I. The tertiary trauma survey: A prospective study of missed injury. J. Trauma 1990, 30, 666–669; discussion 9–70. [Google Scholar] [CrossRef] [PubMed]
- Jeong, H.Y.; Kim, I.-K.; Choi, S.H.; Lee, C.; Ju, M.K. Whole Body Bone Scan for Detecting Missed Bone Injuries in Multiple Trauma Patients. J. Acute Care Surg. 2017, 7, 56–60. [Google Scholar] [CrossRef]
- Pfeifer, R.; Pape, H.C. Missed injuries in trauma patients: A literature review. Patient Saf. Surg. 2008, 2, 20. [Google Scholar] [CrossRef] [PubMed]
- Tammelin, E.; Handolin, L.; Soderlund, T. Missed Injuries in Polytrauma Patients after Trauma Tertiary Survey in Trauma Intensive Care Unit. Scand. J. Surg. 2016, 105, 241–247. [Google Scholar] [CrossRef] [PubMed]
- Pinto, A.; Berritto, D.; Russo, A.; Riccitiello, F.; Caruso, M.; Belfiore, M.P.; Papapietro, V.R.; Carotti, M.; Pinto, F.; Giovagnoni, A.; et al. Traumatic fractures in adults: Missed diagnosis on plain radiographs in the Emergency Department. Acta Biomed. 2018, 89, 111–123. [Google Scholar]
- Tsubaki, F.; Kurata, S.; Nagata, S.; Fujimoto, K.; Abe, T. Clinical spectrum and diagnostic pitfalls of multiple abnormal uptakes on bone scintigraphy. Jpn. J. Radiol. 2016, 34, 771–778. [Google Scholar] [CrossRef]
- Lee, K.J.; Jung, K.; Kim, J.; Kwon, J. Bone scan as a screening test for missed fractures in severely injured patients. Orthop. Traumatol. Surg. Res. 2014, 100, 953–957. [Google Scholar] [CrossRef][Green Version]
- Yang, D.C.; Ratani, R.S.; Mittal, P.K.; Chua, R.S.; Pate, S.M. Radionuclide three-phase whole-body bone imaging. Clin. Nucl. Med. 2002, 27, 419–426. [Google Scholar] [CrossRef]
- Kim, M.; Hong, T.H.; Cho, H.J. Validity of bone scans to detect missed injury in patients with major trauma. Ulus. Travma. Acil. Cerrahi. Derg. 2019, 25, 183–187. [Google Scholar] [CrossRef]
- Lee, J.C.; Hennessy, A.D.; Khafagi, F.A. Bone scans. Aust. Fam. Physician 2012, 41, 689–692. [Google Scholar] [PubMed]
- Lin, H.H.; Chou, P.H.; Wang, S.T.; Yu, J.K.; Chang, M.C.; Liu, C.L. Determination of the painful level in osteoporotic vertebral fractures--Retrospective comparison between plain film, bone scan, and magnetic resonance imaging. J. Chin. Med. Assoc. 2015, 78, 714–718. [Google Scholar] [CrossRef] [PubMed]
- Sirmali, M.; Turut, H.; Topcu, S.; Gulhan, E.; Yazici, U.; Kaya, S.; Taştepe, I. A comprehensive analysis of traumatic rib fractures: Morbidity, mortality and management. Eur. J. Cardiothorac. Surg. 2003, 24, 133–138. [Google Scholar] [CrossRef]
- Schmoekel, N.; Berguson, J.; Stassinopoulos, J.; Karamanos, E.; Patton, J.; Johnson, J.L. Rib fractures in the elderly: Physiology trumps anatomy. Trauma Surg. Acute Care Open 2019, 4, e000257. [Google Scholar] [CrossRef]
- El-Menyar, A.; Al-Thani, H.; Jabbour, G.; Wahlen, B.M.; Asim, M.; Abdelrahman, H.; Nabir, S.; Al-Jogol, H.; Mahmood, I.; El-Faramawy, A.; et al. Traumatic sternal injury in patients with rib fracture: A single-center experience. Int. J. Crit. Illn. Inj. Sci. 2019, 9, 75–81. [Google Scholar] [CrossRef]
- Undurraga Perl, V.J.; Johnson, C.; Kelley, S.; Woods, P.; Martin, K.; Zonies, D. Missed injuries in combat casualties: Lessons from Iraq and Afghanistan. Injury 2019, 50, 1138–1142. [Google Scholar] [CrossRef]
- Giannakopoulos, G.; Saltzherr, T.; Beenen, L.; Reitsma, J.; Bloemers, F.; Goslings, J.; Bakker, F. Missed injuries during the initial assessment in a cohort of 1124 level-1 trauma patients. Injury 2012, 43, 1517–1521. [Google Scholar] [CrossRef] [PubMed]
- Yi, F.; Zhonghua, S.; Yuhai, W.; Jirong, D.; Xuejian, C. Missed injury in patients with severe traumatic brain injury complicated by multiple trauma. Turk. Neurosurg. 2013, 23, 198–201. [Google Scholar] [CrossRef]
- Choi, P.M.; Yu, J.; Keller, M.S. Missed injuries and unplanned readmissions in pediatric trauma patients. J. Pediatr. Surg. 2017, 52, 382–385. [Google Scholar] [CrossRef]
- Podolnick, J.D.; Donovan, D.S.; Atanda, A.W., Jr. Incidence of Delayed Diagnosis of Orthopaedic Injury in Pediatric Trauma Patients. J. Orthop. Trauma 2017, 31, e281–e287. [Google Scholar] [CrossRef]
- Smith, B.P.; Goldberg, A.J.; Gaughan, J.P.; Seamon, M.J. A comparison of Injury Severity Score and New Injury Severity Score after penetrating trauma: A prospective analysis. J. Trauma Acute Care Surg. 2015, 79, 269–274. [Google Scholar] [CrossRef]
- Baker, S.P.; O’Neill, B.; Haddon, W., Jr.; Long, W.B. The injury severity score: A method for describing patients with multiple injuries and evaluating emergency care. J. Trauma 1974, 14, 187–196. [Google Scholar] [CrossRef] [PubMed]
- Fitschen-Oestern, S.; Lippross, S.; Lefering, R.; Besch, L.; Klüter, T.; Schenzer-Hoffmann, E.; Seekamp, A.; Dgu, T. Missed foot fractures in multiple trauma patients. BMC Musculoskelet. Disord. 2019, 20, 121. [Google Scholar] [CrossRef] [PubMed]
- Furnival, R.A.; Woodward, G.A.; Schunk, J.E. Delayed diagnosis of injury in pediatric trauma. Pediatrics 1996, 98, 56–62. [Google Scholar] [CrossRef]
- Hensgens, R.L.; El Moumni, M.; IJpma, F.F.A.; Harbers, J.S.; Duis, K.T.; Wendt, K.W.; Govaert, G.A. High delayed and missed injury rate after inter-hospital transfer of severely injured trauma patients. Eur. J. Trauma Emerg. Surg. 2019, 46, 1367–1374. [Google Scholar] [CrossRef] [PubMed]
- Keijzers, G.B.; Campbell, D.; Hooper, J.; Bost, N.; Crilly, J.; Steele, M.C.; Del Mar, C.; Geeraedts, L.M.G. A prospective evaluation of missed injuries in trauma patients, before and after formalising the trauma tertiary survey. World J. Surg. 2014, 38, 222–232. [Google Scholar] [CrossRef]
- Zamboni, C.; Yonamine, A.M.; Faria, C.E.N.; Filho, M.A.M.; Christian, R.W.; Mercadante, M.T. Tertiary survey in trauma patients: Avoiding neglected injuries. Injury 2014, 45, S14–S17. [Google Scholar] [CrossRef] [PubMed]
| Total (n = 1658) | Missed Injury (n = 146) | Not-Missed Injury (n = 1512) | p-Value | |
|---|---|---|---|---|
| Gender | 0.269 | |||
| Male | 1160 (69.96) | 108 (73.97) | 1052 (69.58) | |
| Female | 498 (30.04) | 38 (26.03) | 460 (30.42) | |
| Age (mean ± SD) | 57.06 ± 18.17 | 58.47 ± 15.40 | 56.93 ± 18.41 | 0.260 |
| Admission department | 0.069 | |||
| NS | 1062 (64.05) | 100 (68.49) | 962 (63.62) | |
| GS | 261 (15.74) | 29 (19.86) | 232 (15.34) | |
| TS | 204 (12.30) | 9 (6.16) | 195 (12.90) | |
| OS | 123 (7.42) | 8 (5.48) | 115 (7.61) | |
| Others | 8 (0.48) | - | 8 (0.53) | |
| ISS | <0.001 | |||
| ISS < 16 | 861 (51.93) | 37 (25.34) | 824 (54.40) | |
| ISS ≥ 16 | 797 (48.07) | 109 (74.66) | 688 (45.50) | |
| GCS | 0.090 | |||
| GCS ≤ 8 | 1487 (89.69) | 125 (85.62) | 1362 (90.08) | |
| GCS > 8 | 171 (10.31) | 21 (14.38) | 150 (9.92) | |
| Duration a (day) | 10.68 ± 4.10 | 10.58 ± 5.09 | 9.59 ± 4.36 | 0.396 |
| Admission route | <0.001 | |||
| ICU | 681 (41.07) | 52 (35.62) | 629 (41.60) | |
| Ward | 635 (38.30) | 45 (30.82) | 590 (39.02) | |
| Surgery | 331 (19.96) | 46 (31.51) | 285 (18.85) | |
| Embolization | 11 (0.66) | 3 (2.05) | 8 (0.53) | |
| Trauma team deployment | 0.321 | |||
| Yes | 1194 (72.01) | 100 (68.49) | 1094 (72.35) | |
| No | 464 (27.99) | 46 (31.51) | 418 (27.65) | |
| OS involvement | 0.004 | |||
| Yes | 1100 (66.34) | 81 (55.48) | 1019 (67.39) | |
| No | 558 (33.66) | 65 (44.52) | 493 (32.61) | |
| Shock b | <0.001 | |||
| Yes | 82 (4.95) | 29 (19.86) | 53 (3.51) | |
| No | 1576 (95.05) | 117 (80.14) | 1459 (96.49) | |
| Mechanism of injury | 0.107 | |||
| Passenger TA | 570 (36.14) | 57 (40.71) | 513 (35.70) | |
| Motorcycle TA | 15 (0.95) | 2 (1.43) | 13 (0.90) | |
| Pedestrian TA | 255 (16.17) | 21 (15.00) | 234 (16.28) | |
| Workplace accident | 76 (4.82) | 1 (0.71) | 75 (5.22) | |
| Fall | 286 (18.14) | 31 (22.14) | 255 (17.75) | |
| Others c | 375 (23.78) | 28 (20.00) | 347 (24.15) |
| Site of Detected Injury | Total (n = 146) | Treatment (n = 146) | ||
|---|---|---|---|---|
| Pain Control (n = 104) | Immobilization (n = 23) | Surgery (n = 19) | ||
| Face | ||||
| Mandible | 1 (0.68) | - | - | 1 (5.26) |
| Chest | ||||
| Rib | 84 (57.53) | 84 (80.77) | - | - |
| Sternum | 2 (1.37 | 2 (1.92) | - | - |
| Upper extremity | ||||
| Clavicle | 11 (7.53) | 4 (3.84) | 2 (8.70) | 5 (26.32) |
| Scapula | 9 (6.16) | 2 (1.92) | 6 (26.09) | 1 (5.26) |
| Humerus | 1 (0.68) | - | - | 1 (5.26) |
| Radius | 2 (1.37) | 1 (0.96) | 1 (4.35) | - |
| Hand | 10 (6.85) | 2 (1.92) | - | 8 (42.11) |
| Lower extremity | ||||
| Pelvis | 1 (0.68) | 1 (0.96) | - | - |
| Ankle | 4 (2.74) | - | 3 (13.04) | 1 (5.26) |
| Tibia | 4 (2.74) | 1 (0.96) | 2 (8.70) | 1 (5.26) |
| Fibula | 8 (5.48) | 1 (0.96) | 6 (26.09) | 1 (5.26) |
| Foot | 5 (3.42) | 4 (3.84) | 1 (4.35) | |
| Spine | ||||
| T-spine | 2 (1.37) | - | 2 (8.70) | - |
| L-spine | 2 (1.37) | 2 (1.92) | - | - |
| Univariate | Multivariable | |||
|---|---|---|---|---|
| Odds Ratio (95% CI) | p-Value | Odds Ratio (95% CI) | p-Value | |
| Gender | ||||
| Female | reference | reference | ||
| Male | 1.24 (0.85–1.83) | 0.269 | 1.25 (0.82–1.91) | 0.304 |
| Age | 1.01 (1.00–1.01) | 0.329 | 1.01 (1.00–1.02) | 0.110 |
| Admission department | ||||
| OS | reference | |||
| NS | 1.49 (0.71–3.15) | 0.979 | ||
| GS | 1.80 (0.80–4.06) | 0.977 | ||
| TS | 0.66 (0.25–1.77) | 0.985 | ||
| Others | NA | NA | ||
| ISS | ||||
| ISS < 16 | reference | reference | ||
| ISS ≥ 16 | 3.53 (2.40–5.19) | <0.001 | 3.98 (2.47–6.41) | <0.001 |
| GCS | ||||
| GCS ≤ 8 | reference | reference | ||
| GCS > 8 | 1.53 (0.93–2.50) | 0.093 | 1.25 (0.69–2.26) | 0.471 |
| Duration a (day) | 1.00 (0.99–1.01) | 0.479 | ||
| Admission route | ||||
| ICU | reference | reference | ||
| Ward | 0.92 (0.61–1.40) | 0.724 | 1.53 (0.92–2.55) | 0.115 |
| Surgery | 1.95 (1.28–2.97) | 0.001 | 1.77 (1.11–2.85) | 0.026 |
| Embolization | 4.54 (1.17–17.63) | 0.022 | 1.98 (0.35–11.38) | 0.440 |
| Trauma team deployment | ||||
| Yes | reference | reference | ||
| No | 1.20 (0.83–1.74) | 0.322 | 2.30 (1.18–4.49) | 0.015 |
| OS involvement | ||||
| Yes | reference | reference | ||
| No | 1.66 (1.18–2.34) | 0.004 | 1.46 (0.86–2.47) | 0.160 |
| Shock b | ||||
| No | reference | reference | ||
| Yes | 6.82 (4.18–11.14) | <0.001 | 5.90 (3.26–10.68) | <0.001 |
| Mechanism of injury | ||||
| Passenger TA | reference | reference | ||
| Motorcycle TA | 1.39 (0.31–6.29) | 0.289 | 0.40 (0.08–2.08) | 0.167 |
| Pedestrian TA | 0.81 (0.48–1.36) | 0.580 | 0.81 (0.47–1.41) | 0.391 |
| Workplace accident | 0.12 (0.01–0.88) | 0.040 | 0.08 (0.01–0.61) | 0.002 |
| Fall | 1.09 (0.69–1.74) | 0.085 | 0.89 (0.54–1.46) | 0.716 |
| Others c | 0.73 (0.45–1.17) | 0.846 | 0.61 (0.35–1.06) | 0.096 |
| Hosmer and Lemeshow Goodness-of-Fit test | 0.240 | |||
| C-statistics | 0.766 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chung, J.S.; An, S.; Gong, S.C.; Jung, P.Y. Analysis of Missed Skeletal Injuries Detected Using Whole-Body Bone Scan Applied to Trauma Patients: A Case–Control Study. Diagnostics 2023, 13, 1879. https://doi.org/10.3390/diagnostics13111879
Chung JS, An S, Gong SC, Jung PY. Analysis of Missed Skeletal Injuries Detected Using Whole-Body Bone Scan Applied to Trauma Patients: A Case–Control Study. Diagnostics. 2023; 13(11):1879. https://doi.org/10.3390/diagnostics13111879
Chicago/Turabian StyleChung, Jae Sik, Sanghyun An, Seong Chan Gong, and Pil Young Jung. 2023. "Analysis of Missed Skeletal Injuries Detected Using Whole-Body Bone Scan Applied to Trauma Patients: A Case–Control Study" Diagnostics 13, no. 11: 1879. https://doi.org/10.3390/diagnostics13111879
APA StyleChung, J. S., An, S., Gong, S. C., & Jung, P. Y. (2023). Analysis of Missed Skeletal Injuries Detected Using Whole-Body Bone Scan Applied to Trauma Patients: A Case–Control Study. Diagnostics, 13(11), 1879. https://doi.org/10.3390/diagnostics13111879






