Dental Restorative Materials for Elderly Populations
Abstract
1. Introduction
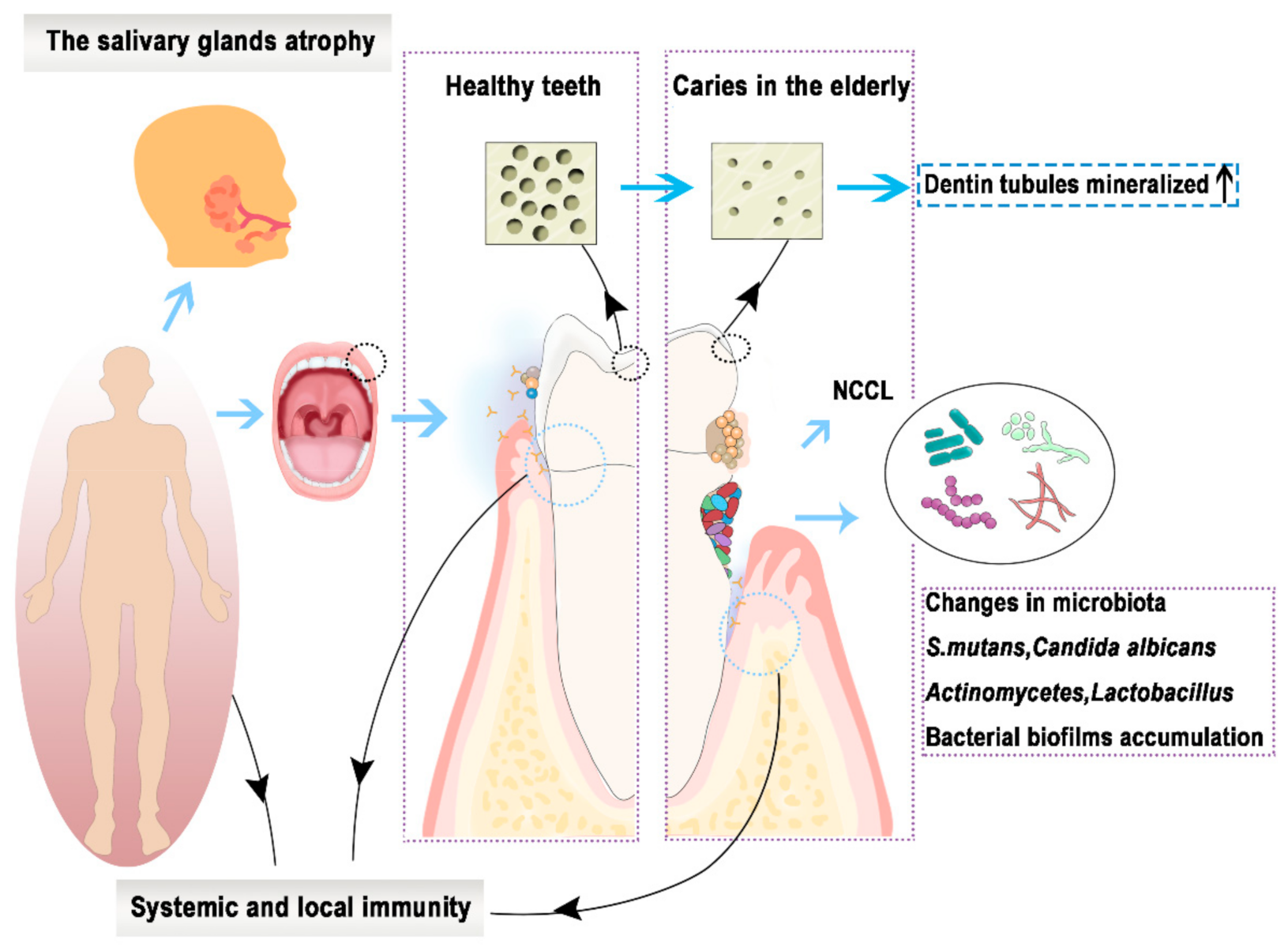
2. The Challenges of Dental Restorative Materials in the Elderly
3. Currently Available Restorative Materials for the Elderly
3.1. Amalgam
3.2. Glass Ionomer Cement
3.3. Light-Cured Composite Resin
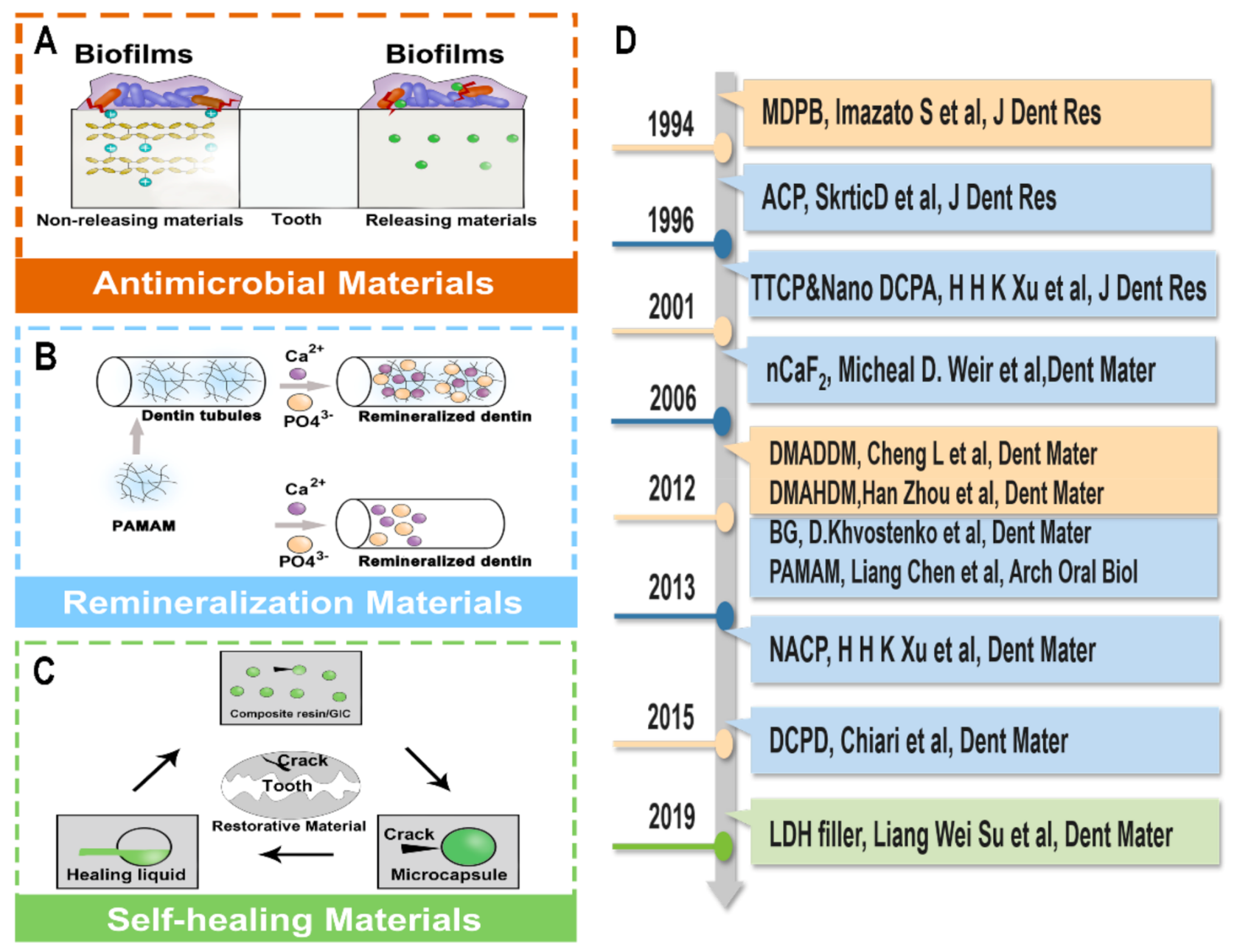
4. Novel Anticariogenic Restorative Materials
4.1. Antimicrobial Materials
4.2. Remineralization Materials
4.3. Self-Healing and Low-Shrinkage Materials
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Kassebaum, N.J.; Bernabé, E.; Dahiya, M.; Bhandari, B.; Murray, C.J.; Marcenes, W. Global burden of untreated caries: A systematic review and metaregression. J. Dent. Res. 2015, 94, 650–658. [Google Scholar] [CrossRef]
- Eke, P.I.; Wei, L.; Borgnakke, W.S.; Thornton-Evans, G.; Zhang, X.; Lu, H.; McGuire, L.C.; Genco, R.J. Periodontitis prevalence in adults ≥65 years of age, in the USA. Periodontology 2000 2016, 72, 76–95. [Google Scholar] [CrossRef]
- Fure, S. Ten-year cross-sectional and incidence study of coronal and root caries and some related factors in elderly Swedish individuals. Gerodontology 2004, 21, 130–140. [Google Scholar] [CrossRef]
- Jiang, Q.; Liu, J.; Chen, L.; Gan, N.; Yang, D. The Oral Microbiome in the Elderly with Dental Caries and Health. Front. Cell. Infect. Microbiol. 2018, 8, 442. [Google Scholar] [CrossRef]
- Diaz de Guillory, C.; Schoolfield, J.D.; Johnson, D.; Yeh, C.K.; Chen, S.; Cappelli, D.P.; Bober-Moken, I.G.; Dang, H. Co-relationships between glandular salivary flow rates and dental caries. Gerodontology 2014, 31, 210–219. [Google Scholar] [CrossRef]
- Humphrey, S.P.; Williamson, R.T. A review of saliva: Normal composition, flow, and function. J. Prosthet. Dent. 2001, 85, 162–169. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Q.; Zhou, X.; Cheng, L.; Li, M. The Adhesion and Invasion Mechanisms of Streptococci. Curr. Issues Mol. Biol. 2019, 32, 521–560. [Google Scholar] [CrossRef] [PubMed]
- Do, T.; Damé-Teixeira, N.; Naginyte, M.; Marsh, P.D. Root Surface Biofilms and Caries. Monogr. Oral Sci. 2017, 26, 26–34. [Google Scholar] [CrossRef] [PubMed]
- Zaremba, M.L.; Daniluk, T.; Rozkiewicz, D.; Cylwik-Rokicka, D.; Kierklo, A.; Tokajuk, G.; Dabrowska, E.; Pawińska, M.; Klimiuk, A.; Stokowska, W.; et al. Incidence rate of Candida species in the oral cavity of middle-aged and elderly subjects. Adv. Med Sci. 2006, 51 (Suppl. 1), 233–236. [Google Scholar] [PubMed]
- Steele, J.G.; Sheiham, A.; Marcenes, W.; Fay, N.; Walls, A.W. Clinical and behavioural risk indicators for root caries in older people. Gerodontology 2001, 18, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Zhang, X.; Cheng, L.; Xu, X.; Zhou, X.; Wu, H.; Peng, X. Signal Transduction of Streptococci by Cyclic Dinucleotide Second Messengers. Curr. Issues Mol. Biol. 2019, 32, 87–122. [Google Scholar] [CrossRef]
- Chen, H.; Zhou, X.; Ren, B.; Cheng, L. The regulation of hyphae growth in Candida albicans. Virulence 2020, 11, 337–348. [Google Scholar] [CrossRef]
- Griffin, S.O.; Griffin, P.M.; Swann, J.L.; Zlobin, N. Estimating rates of new root caries in older adults. J. Dent. Res. 2004, 83, 634–638. [Google Scholar] [CrossRef]
- Leventouri, T.; Antonakos, A.; Kyriacou, A.; Venturelli, R.; Liarokapis, E.; Perdikatsis, V. Crystal structure studies of human dental apatite as a function of age. Int. J. Biomater. 2009, 2009, 698547. [Google Scholar] [CrossRef] [PubMed]
- Heasman, P.A.; Ritchie, M.; Asuni, A.; Gavillet, E.; Simonsen, J.L.; Nyvad, B. Gingival recession and root caries in the ageing population: A critical evaluation of treatments. J. Clin. Periodontol. 2017, 44 (Suppl. 18), S178–S193. [Google Scholar] [CrossRef]
- Betancourt, D.E.; Baldion, P.A.; Castellanos, J.E. Resin-Dentin Bonding Interface: Mechanisms of Degradation and Strategies for Stabilization of the Hybrid Layer. Int. J. Biomater. 2019, 2019, 5268342. [Google Scholar] [CrossRef]
- Carvalho, T.S.; Lussi, A. Age-related morphological, histological and functional changes in teeth. J. Oral Rehabil. 2017, 44, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Mazzoni, A.; Tjäderhane, L.; Checchi, V.; Di Lenarda, R.; Salo, T.; Tay, F.R.; Pashley, D.H.; Breschi, L. Role of dentin MMPs in caries progression and bond stability. J. Dent. Res. 2015, 94, 241–251. [Google Scholar] [CrossRef] [PubMed]
- Kinney, J.H.; Nalla, R.K.; Pople, J.A.; Breunig, T.M.; Ritchie, R.O. Age-related transparent root dentin: Mineral concentration, crystallite size, and mechanical properties. Biomaterials 2005, 26, 3363–3376. [Google Scholar] [CrossRef] [PubMed]
- Ivancik, J.; Neerchal, N.K.; Romberg, E.; Arola, D. The reduction in fatigue crack growth resistance of dentin with depth. J. Dent. Res. 2011, 90, 1031–1036. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.E.; Lin, C.L.; Wang, C.H.; Cheng, C.H.; Chang, C.H. Stresses at the cervical lesion of maxillary premolar--a finite element investigation. J. Dent. 2002, 30, 283–290. [Google Scholar] [CrossRef]
- Machado, A.C.; Soares, C.J.; Reis, B.R.; Bicalho, A.A.; Raposo, L.; Soares, P.V. Stress-strain Analysis of Premolars With Non-carious Cervical Lesions: Influence of Restorative Material, Loading Direction and Mechanical Fatigue. Oper. Dent. 2017, 42, 253–265. [Google Scholar] [CrossRef]
- Valinoti, A.C.; Neves, B.G.; da Silva, E.M.; Maia, L.C. Surface degradation of composite resins by acidic medicines and pH-cycling. J. Appl. Oral Sci. Rev. Fob 2008, 16, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Leistevuo, J.; Järvinen, H.; Osterblad, M.; Leistevuo, T.; Huovinen, P.; Tenovuo, J. Resistance to mercury and antimicrobial agents in Streptococcus mutans isolates from human subjects in relation to exposure to dental amalgam fillings. Antimicrob. Agents Chemother. 2000, 44, 456–457. [Google Scholar] [CrossRef] [PubMed]
- Setcos, J.C.; Staninec, M.; Wilson, N.H. Bonding of amalgam restorations: Existing knowledge and future prospects. Oper. Dent. 2000, 25, 121–129. [Google Scholar]
- Chun, K.J.; Lee, J.Y. Comparative study of mechanical properties of dental restorative materials and dental hard tissues in compressive loads. J. Dent. Biomech. 2014, 5, 1–6. [Google Scholar] [CrossRef]
- Caplan, D.J.; Li, Y.; Wang, W.; Kang, S.; Marchini, L.; Cowen, H.J.; Yan, J. Dental Restoration Longevity among Geriatric and Special Needs Patients. Jdr Clin. Transl. Res. 2019, 4, 41–48. [Google Scholar] [CrossRef]
- Thanyavuthi, A.; Boonchai, W.; Kasemsarn, P. Amalgam Contact Allergy in Oral Lichenoid Lesions. Dermat. 2016, 27, 215–221. [Google Scholar] [CrossRef] [PubMed]
- Nakata, T.T.; Bae, K.S.; Baumgartner, J.C. Perforation repair comparing mineral trioxide aggregate and amalgam using an anaerobic bacterial leakage model. J. Endod. 1998, 24, 184–186. [Google Scholar] [CrossRef]
- Sidhu, S.K.; Nicholson, J.W. A Review of Glass-Ionomer Cements for Clinical Dentistry. J. Funct. Biomater. 2016, 7, 16. [Google Scholar] [CrossRef]
- Ullah, R.; Zafar, M.S.J.F. Oral and dental delivery of fluoride: A review. Fluoride 2015, 48, 195–204. [Google Scholar]
- Wiegand, A.; Buchalla, W.; Attin, T. Review on fluoride-releasing restorative materials—Fluoride release and uptake characteristics, antibacterial activity and influence on caries formation. Dent. Mater. 2007, 23, 343–362. [Google Scholar] [CrossRef] [PubMed]
- Bhavana, V.; Chaitanya, K.; Gandi, P.; Patil, J.; Dola, B.; Reddy, R. Evaluation of antibacterial and antifungal activity of new calcium-based cement (Biodentine) compared to MTA and glass ionomer cement. J. Conserv. Dent. 2015, 18, 44–46. [Google Scholar] [CrossRef]
- Naik, R.G.; Dodamani, A.S.; Khairnar, M.R.; Jadhav, H.C.; Deshmukh, M.A. Comparative assessment of antibacterial activity of different glass ionomer cements on cariogenic bacteria. Restor. Dent. Endod. 2016, 41, 278–282. [Google Scholar] [CrossRef] [PubMed]
- Nassar, H.M.; Platt, J.A. Fluoride Release from Two High-Viscosity Glass Ionomers after Exposure to Fluoride Slurry and Varnish. Materials 2019, 12, 3760. [Google Scholar] [CrossRef]
- Cabral, M.F.C.; Martinho, R.L.d.M.; Guedes-Neto, M.V.; Rebelo, M.A.B.; Pontes, D.G.; Cohen-Carneiro, F. Do conventional glass ionomer cements release more fluoride than resin-modified glass ionomer cements? Restor. Dent. Endod. 2015, 40, 209–215. [Google Scholar] [CrossRef]
- Kuhn, E.; Chibinski, A.C.; Reis, A.; Wambier, D.S. The role of glass ionomer cement on the remineralization of infected dentin: An in vivo study. Pediatric Dent. 2014, 36, E118–E124. [Google Scholar]
- Kim, Y.K.; Yiu, C.K.Y.; Kim, J.R.; Gu, L.; Kim, S.K.; Weller, R.N.; Pashley, D.H.; Tay, F.R. Failure of a Glass Ionomer to Remineralize Apatite-depleted Dentin. J. Dent. Res. 2010, 89, 230–235. [Google Scholar] [CrossRef]
- Bueno, L.S.; Silva, R.M.; Magalhães, A.P.R.; Navarro, M.F.L.; Pascotto, R.C.; Buzalaf, M.A.R.; Nicholson, J.W.; Sidhu, S.K.; Borges, A.F.S. Positive correlation between fluoride release and acid erosion of restorative glass-ionomer cements. Dent. Mater. 2019, 35, 135–143. [Google Scholar] [CrossRef] [PubMed]
- Najeeb, S.; Khurshid, Z.; Ghabbani, H.; Zafar, M.S.; Sefat, F.J.A.D.B. Nano glass ionomer cement: Modification for biodental applications—ScienceDirect. Adv. Dent. Biomater. 2019, 217–227. [Google Scholar] [CrossRef]
- Berzins, D.W.; Abey, S.; Costache, M.C.; Wilkie, C.A.; Roberts, H.W. Resin-modified glass-ionomer setting reaction competition. J. Dent. Res. 2010, 89, 82–86. [Google Scholar] [CrossRef]
- Nicholson, J.W.; Sidhu, S.K.; Czarnecka, B. Enhancing the Mechanical Properties of Glass-Ionomer Dental Cements: A Review. Materials 2020, 13, 2510. [Google Scholar] [CrossRef]
- Bonifácio, C.C.; Kleverlaan, C.J.; Raggio, D.P.; Werner, A.; De Carvalho, R.C.R.; Van Amerongen, W.E. Physical-mechanical properties of glass ionomer cements indicated for atraumatic restorative treatment. Aust. Dent. J. 2009, 54, 233–237. [Google Scholar] [CrossRef]
- Carlén, A.; Nikdel, K.; Wennerberg, A.; Holmberg, K.; Olsson, J. Surface characteristics and in vitro biofilm formation on glass ionomer and composite resin. Biomaterials 2001, 22, 481–487. [Google Scholar] [CrossRef]
- Montanaro, L.; Campoccia, D.; Rizzi, S.; Donati, M.E.; Breschi, L.; Prati, C.; Arciola, C.R. Evaluation of bacterial adhesion of Streptococcus mutans on dental restorative materials. Biomaterials 2004, 25, 4457–4463. [Google Scholar] [CrossRef]
- Beyth, N.; Bahir, R.; Matalon, S.; Domb, A.J.; Weiss, E.I. Streptococcus mutans biofilm changes surface-topography of resin composites. Dent. Mater. 2008, 24, 732–736. [Google Scholar] [CrossRef] [PubMed]
- Hao, Y.; Huang, X.; Zhou, X.; Li, M.; Ren, B.; Peng, X.; Cheng, L. Influence of Dental Prosthesis and Restorative Materials Interface on Oral Biofilms. Int. J. Mol. Sci. 2018, 19, 3157. [Google Scholar] [CrossRef]
- Zafar, M. Effects of Surface Pre-Reacted Glass Particles on Fluoride Release of Dental Restorative Materials. World Appl. Sci. J. 2013, 28, 457–462. [Google Scholar] [CrossRef]
- Naoum, S.; Martin, E.; Ellakwa, A. Long-term fluoride exchanges at restoration surfaces and effects on surface mechanical properties. Isrn Dent. 2013, 2013, 579039. [Google Scholar] [CrossRef] [PubMed]
- Moszner, N.; Salz, U.; Zimmermann, J. Chemical aspects of self-etching enamel-dentin adhesives: A systematic review. Dent. Mater. 2005, 21, 895–910. [Google Scholar] [CrossRef]
- Fabião, A.; Fronza, B.; Andre, C.; Cavalli, V.; Giannini, M. Microtensile dentin bond strength and interface morphology of different self-etching adhesives and universal adhesives applied in self-etching mode. J. Adhes. Sci. Technol. 2020, 1–10. [Google Scholar] [CrossRef]
- van Dijken, J.W.; Pallesen, U. Fracture frequency and longevity of fractured resin composite, polyacid-modified resin composite, and resin-modified glass ionomer cement class IV restorations: An up to 14 years of follow-up. Clin. Oral Investig. 2010, 14, 217–222. [Google Scholar] [CrossRef]
- Xie, D.; Brantley, W.A.; Culbertson, B.M.; Wang, G. Mechanical properties and microstructures of glass-ionomer cements. Dent. Mater. 2000, 16, 129–138. [Google Scholar] [CrossRef]
- Vallittu, P.K. An overview of development and status of fiber-reinforced composites as dental and medical biomaterials. Acta Biomater. Odontol. Scand. 2018, 4, 44–55. [Google Scholar] [CrossRef] [PubMed]
- Xiao, B.; Huang, Q.; Wang, Y.; Chen, H.; Long, G.J.F. A fractal model for capillary flow through a single tortuous capillary with roughened surfaces in fibrous porous media. Fractals 2021, 29, 2150017. [Google Scholar] [CrossRef]
- Garoushi, S.; Vallittu, P.K.; Lassila, L.V. Fracture toughness, compressive strength and load-bearing capacity of short glass fibre-reinforced composite resin. Chin. J. Dent. Res. Off. J. Sci. Sect. Chin. Stomatol. Assoc. 2011, 14, 15–19. [Google Scholar]
- Garoushi, S.; Gargoum, A.; Vallittu, P.K.; Lassila, L. Short fiber-reinforced composite restorations: A review of the current literature. J. Investig. Clin. Dent. 2018, 9, e12330. [Google Scholar] [CrossRef]
- Lassila, L.; Keulemans, F.; Vallittu, P.K.; Garoushi, S. Characterization of restorative short-fiber reinforced dental composites. Dent. Mater. J. 2020, 39, 992–999. [Google Scholar] [CrossRef]
- Kleverlaan, C.J.; Feilzer, A.J. Polymerization shrinkage and contraction stress of dental resin composites. Dent. Mater. 2005, 21, 1150–1157. [Google Scholar] [CrossRef]
- Feng, C.; Zhao, S.; Chu, B.; Hong-Bo, L. Resin composite shrinkage stress distribution in classI cavity of mandibular molar using 3D finite element analysis. Chin. J. Geriatr. Dent. 2009, 7, 104. [Google Scholar]
- Peutzfeldt, A. Resin composites in dentistry: The monomer systems. Eur. J. Oral Sci. 1997, 105, 97–116. [Google Scholar] [CrossRef] [PubMed]
- Mashalkar, S.; Pawar, M.G.; Kolhe, S.; Jain, D.T. Comparative evaluation of root canal disinfection by conventional method and laser: An in vivo study. Niger. J. Clin. Pract. 2014, 17, 67–74. [Google Scholar] [CrossRef]
- Zhou, X.; Huang, X.; Li, M.; Peng, X.; Cheng, L. Development and status of resin composite as dental restorative materials. J. Appl. Polym. Sci. 2019, 136, 48180. [Google Scholar] [CrossRef]
- Melo, M.A.S.; Weir, M.D.; Li, F.; Cheng, L.; Zhang, K.; Xu, H.H.K.J.R.o.A. Adhesives. Control of biofilm at the tooth-restoration bonding interface: A question for antibacterial monomers? A critical review. Rev. Adhes. Adhes. 2017, 5, 303–324. [Google Scholar] [CrossRef]
- Wang, H.; Wang, S.; Cheng, L.; Jiang, Y.; Melo, M.A.S.; Weir, M.D.; Oates, T.W.; Zhou, X.; Xu, H.H.K. Novel dental composite with capability to suppress cariogenic species and promote non-cariogenic species in oral biofilms. Mater. Sci. Eng. C Mater. Biol. Appl. 2019, 94, 587–596. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Wang, S.; Zhou, X.; Zou, Y.; Li, M.; Peng, X.; Ren, B.; Xu, H.H.K.; Weir, M.D.; Cheng, L.; et al. Short-Time Antibacterial Effects of Dimethylaminododecyl Methacrylate on Oral Multispecies Biofilm In Vitro. Biomed Res. Int. 2019, 2019, 6393470. [Google Scholar] [CrossRef]
- Cao, W.; Zhang, Y.; Wang, X.; Chen, Y.; Li, Q.; Xing, X.; Xiao, Y.; Peng, X.; Ye, Z. Development of a novel resin-based dental material with dual biocidal modes and sustained release of Ag(+) ions based on photocurable core-shell AgBr/cationic polymer nanocomposites. J. Mater. Sci. Mater. Med. 2017, 28, 103. [Google Scholar] [CrossRef]
- Cheng, L.; Weir, M.D.; Xu, H.H.; Antonucci, J.M.; Kraigsley, A.M.; Lin, N.J.; Lin-Gibson, S.; Zhou, X. Antibacterial amorphous calcium phosphate nanocomposites with a quaternary ammonium dimethacrylate and silver nanoparticles. Dent. Mater. 2012, 28, 561–572. [Google Scholar] [CrossRef]
- Chen, S.; Gururaj, S.; Xia, W.; Engqvist, H. Synthesis of Ag doped calcium phosphate particles and their antibacterial effect as additives in dental glass ionomer cements. J. Mater. Sci. Mater. Med. 2016, 27, 172. [Google Scholar] [CrossRef][Green Version]
- Breschi, L.; Mazzoni, A.; Nato, F.; Carrilho, M.; Visintini, E.; Tjäderhane, L.; Ruggeri, A., Jr.; Tay, F.R.; Dorigo Ede, S.; Pashley, D.H. Chlorhexidine stabilizes the adhesive interface: A 2-year in vitro study. Dent. Mater. 2010, 26, 320–325. [Google Scholar] [CrossRef]
- Fei, X.; Li, Y.; Weir, M.D.; Baras, B.H.; Wang, H.; Wang, S.; Sun, J.; Melo, M.A.S.; Ruan, J.; Xu, H.H.K. Novel pit and fissure sealant containing nano-CaF2 and dimethylaminohexadecyl methacrylate with double benefits of fluoride release and antibacterial function. Dent. Mater. 2020, 36, 1241–1253. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.F.; Wu, R.; Fan, Y.; Liao, S.; Wang, Y.; Wen, Z.T.; Xu, X. Antibacterial dental composites with chlorhexidine and mesoporous silica. J. Dent. Res. 2014, 93, 1283–1289. [Google Scholar] [CrossRef] [PubMed]
- Mei, M.L.; Chu, C.H.; Lo, E.C.; Samaranayake, L.P. Preventing root caries development under oral biofilm challenge in an artificial mouth. Med. Oral Patol. Oral Cir. Bucal 2013, 18, e557–e563. [Google Scholar] [CrossRef] [PubMed]
- van Strijp, A.J.; Gerardu, V.A.; Buijs, M.J.; van Loveren, C.; ten Cate, J.M. Chlorhexidine efficacy in preventing lesion formation in enamel and dentine: An in situ study. Caries Res. 2008, 42, 460–465. [Google Scholar] [CrossRef]
- Ishiguro, T.; Mayanagi, G.; Azumi, M.; Otani, H.; Fukushima, A.; Sasaki, K.; Takahashi, N. Sodium fluoride and silver diamine fluoride-coated tooth surfaces inhibit bacterial acid production at the bacteria/tooth interface. J. Dent. 2019, 84, 30–35. [Google Scholar] [CrossRef]
- Zhou, W.; Liu, S.; Zhou, X.; Hannig, M.; Rupf, S.; Feng, J.; Peng, X.; Cheng, L. Modifying Adhesive Materials to Improve the Longevity of Resinous Restorations. Int. J. Mol. Sci. 2019, 20, 723. [Google Scholar] [CrossRef]
- Liang, J.; Liu, F.; Zou, J.; Xu, H.H.K.; Han, Q.; Wang, Z.; Li, B.; Yang, B.; Ren, B.; Li, M.; et al. pH-Responsive Antibacterial Resin Adhesives for Secondary Caries Inhibition. J. Dent. Res. 2020, 99, 1368–1376. [Google Scholar] [CrossRef]
- Chen, C.; Cheng, L.; Weir, M.D.; Lin, N.J.; Lin-Gibson, S.; Zhou, X.D.; Xu, H.H. Primer containing dimethylaminododecyl methacrylate kills bacteria impregnated in human dentin blocks. Int. J. Oral Sci. 2016, 8, 239–245. [Google Scholar] [CrossRef][Green Version]
- Feng, J.; Cheng, L.; Zhou, X.; Xu, H.H.K.; Weir, M.D.; Li, Q.; Hannig, M.; Rupf, S. Effects of water aging on the mechanical and anti-biofilm properties of glass-ionomer cement containing dimethylaminododecyl methacrylate. Dent. Mater. 2019, 35, 434–443. [Google Scholar] [CrossRef]
- Cheng, L.; Zhang, K.; Zhang, N.; Melo, M.A.S.; Weir, M.D.; Zhou, X.D.; Bai, Y.X.; Reynolds, M.A.; Xu, H.H.K. Developing a New Generation of Antimicrobial and Bioactive Dental Resins. J. Dent. Res. 2017, 96, 855–863. [Google Scholar] [CrossRef]
- Wang, S.P.; Ge, Y.; Zhou, X.D.; Xu, H.H.; Weir, M.D.; Zhang, K.K.; Wang, H.H.; Hannig, M.; Rupf, S.; Li, Q.; et al. Effect of anti-biofilm glass-ionomer cement on Streptococcus mutans biofilms. Int. J. Oral Sci. 2016, 8, 76–83. [Google Scholar] [CrossRef]
- Liang, J.; Li, M.; Ren, B.; Wu, T.; Xu, H.H.K.; Liu, Y.; Peng, X.; Yang, G.; Weir, M.D.; Zhang, S.; et al. The anti-caries effects of dental adhesive resin influenced by the position of functional groups in quaternary ammonium monomers. Dent. Mater. 2018, 34, 400–411. [Google Scholar] [CrossRef]
- Han, Q.; Li, B.; Zhou, X.; Ge, Y.; Wang, S.; Li, M.; Ren, B.; Wang, H.; Zhang, K.; Xu, H.H.K.; et al. Anti-Caries Effects of Dental Adhesives Containing Quaternary Ammonium Methacrylates with Different Chain Lengths. Materials 2017, 10, 643. [Google Scholar] [CrossRef]
- Wang, S.; Wang, H.; Ren, B.; Li, X.; Wang, L.; Zhou, H.; Weir, M.D.; Zhou, X.; Masri, R.M.; Oates, T.W.; et al. Drug resistance of oral bacteria to new antibacterial dental monomer dimethylaminohexadecyl methacrylate. Sci. Rep. 2018, 8, 5509. [Google Scholar] [CrossRef]
- Jiang, Y.L.; Qiu, W.; Zhou, X.D.; Li, H.; Lu, J.Z.; Xu, H.H.; Peng, X.; Li, M.Y.; Feng, M.Y.; Cheng, L.; et al. Quaternary ammonium-induced multidrug tolerant Streptococcus mutans persisters elevate cariogenic virulence in vitro. Int. J. Oral Sci. 2017, 9, e7. [Google Scholar] [CrossRef]
- Wang, S.; Wang, H.; Ren, B.; Li, H.; Weir, M.D.; Zhou, X.; Oates, T.W.; Cheng, L.; Xu, H.H.K. Do quaternary ammonium monomers induce drug resistance in cariogenic, endodontic and periodontal bacterial species? Dent. Mater. 2017, 33, 1127–1138. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Zhou, C.; Ren, B.; Li, X.; Weir, M.D.; Masri, R.M.; Oates, T.W.; Cheng, L.; Xu, H.K.H. Formation of persisters in Streptococcus mutans biofilms induced by antibacterial dental monomer. J. Mater. Sci. Mater. Med. 2017, 28, 178. [Google Scholar] [CrossRef] [PubMed]
- Imazato, S.; Ebi, N.; Takahashi, Y.; Kaneko, T.; Ebisu, S.; Russell, R.R. Antibacterial activity of bactericide-immobilized filler for resin-based restoratives. Biomaterials 2003, 24, 3605–3609. [Google Scholar] [CrossRef]
- Murata, H.; Koepsel, R.R.; Matyjaszewski, K.; Russell, A.J. Permanent, non-leaching antibacterial surface—2: How high density cationic surfaces kill bacterial cells. Biomaterials 2007, 28, 4870–4879. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Huang, X.; Zhou, X.; Han, Q.; Zhou, W.; Liang, J.; Xu, H.H.K.; Ren, B.; Peng, X.; Weir, M.D.; et al. Anti-caries effect of resin infiltrant modified by quaternary ammonium monomers. J. Dent. 2020, 97, 103355. [Google Scholar] [CrossRef]
- Thomé, T.; Mayer, M.P.; Imazato, S.; Geraldo-Martins, V.R.; Marques, M.M. In vitro analysis of inhibitory effects of the antibacterial monomer MDPB-containing restorations on the progression of secondary root caries. J. Dent. 2009, 37, 705–711. [Google Scholar] [CrossRef]
- Zhou, W.; Zhou, X.; Huang, X.; Zhu, C.; Weir, M.D.; Melo, M.A.S.; Bonavente, A.; Lynch, C.D.; Imazato, S.; Oates, T.W.; et al. Antibacterial and remineralizing nanocomposite inhibit root caries biofilms and protect root dentin hardness at the margins. J. Dent. 2020, 97, 103344. [Google Scholar] [CrossRef] [PubMed]
- Ge, Y.; Ren, B.; Zhou, X.; Xu, H.H.K.; Wang, S.; Li, M.; Weir, M.D.; Feng, M.; Cheng, L. Novel Dental Adhesive with Biofilm-Regulating and Remineralization Capabilities. Materials 2017, 10, 26. [Google Scholar] [CrossRef] [PubMed]
- Zhang, K.; Ren, B.; Zhou, X.; Xu, H.H.; Chen, Y.; Han, Q.; Li, B.; Weir, M.D.; Li, M.; Feng, M.; et al. Effect of Antimicrobial Denture Base Resin on Multi-Species Biofilm Formation. Int. J. Mol. Sci. 2016, 17, 1033. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Zhou, Y.; Zhou, X.; Liao, B.; Xu, H.H.K.; Chu, C.H.; Cheng, L.; Ren, B. Dimethylaminododecyl methacrylate inhibits Candida albicans and oropharyngeal candidiasis in a pH-dependent manner. Appl. Microbiol. Biotechnol. 2020, 104, 3585–3595. [Google Scholar] [CrossRef]
- Chen, H.; Han, Q.; Zhou, X.; Zhang, K.; Wang, S.; Xu, H.H.K.; Weir, M.D.; Feng, M.; Li, M.; Peng, X.; et al. Heat-Polymerized Resin Containing Dimethylaminododecyl Methacrylate Inhibits Candida albicans Biofilm. Materials 2017, 10, 431. [Google Scholar] [CrossRef]
- Wu, T.; Li, B.; Zhou, X.; Hu, Y.; Zhang, H.; Huang, Y.; Xu, H.H.K.; Guo, Q.; Li, M.; Feng, M.; et al. Evaluation of Novel Anticaries Adhesive in a Secondary Caries Animal Model. Caries Res. 2018, 52, 14–21. [Google Scholar] [CrossRef]
- Xu, H.H.; Sun, L.; Weir, M.D.; Antonucci, J.M.; Takagi, S.; Chow, L.C.; Peltz, M. Nano DCPA-whisker composites with high strength and Ca and PO(4) release. J. Dent. Res. 2006, 85, 722–727. [Google Scholar] [CrossRef]
- Xu, H.H.; Weir, M.D.; Sun, L. Calcium and phosphate ion releasing composite: Effect of pH on release and mechanical properties. Dent. Mater. 2009, 25, 535–542. [Google Scholar] [CrossRef]
- Zhang, K.; Wang, S.; Zhou, C.; Cheng, L.; Gao, X.; Xie, X.; Sun, J.; Wang, H.; Weir, M.D.; Reynolds, M.A.; et al. Advanced smart biomaterials and constructs for hard tissue engineering and regeneration. Bone Res. 2018, 6, 31. [Google Scholar] [CrossRef]
- Zhang, L.; Weir, M.D.; Chow, L.C.; Antonucci, J.M.; Chen, J.; Xu, H.H. Novel rechargeable calcium phosphate dental nanocomposite. Dent. Mater. 2016, 32, 285–293. [Google Scholar] [CrossRef]
- Weir, M.D.; Ruan, J.; Zhang, N.; Chow, L.C.; Zhang, K.; Chang, X.; Bai, Y.; Xu, H.H.K. Effect of calcium phosphate nanocomposite on in vitro remineralization of human dentin lesions. Dent. Mater. 2017, 33, 1033–1044. [Google Scholar] [CrossRef]
- Al-Dulaijan, Y.A.; Cheng, L.; Weir, M.D.; Melo, M.A.S.; Liu, H.; Oates, T.W.; Wang, L.; Xu, H.H.K. Novel rechargeable calcium phosphate nanocomposite with antibacterial activity to suppress biofilm acids and dental caries. J. Dent. 2018, 72, 44–52. [Google Scholar] [CrossRef]
- Weir, M.D.; Moreau, J.L.; Levine, E.D.; Strassler, H.E.; Chow, L.C.; Xu, H.H. Nanocomposite containing CaF(2) nanoparticles: Thermal cycling, wear and long-term water-aging. Dent. Mater. 2012, 28, 642–652. [Google Scholar] [CrossRef] [PubMed]
- Wei Su, L.; Lin, D.J.; Yen Uan, J. Novel dental resin composites containing LiAl-F layered double hydroxide (LDH) filler: Fluoride release/recharge, mechanical properties, color change, and cytotoxicity. Dent. Mater. 2019, 35, 663–672. [Google Scholar] [CrossRef] [PubMed]
- Xiao, S.; Liang, K.; Weir, M.D.; Cheng, L.; Liu, H.; Zhou, X.; Ding, Y.; Xu, H.H.K. Combining Bioactive Multifunctional Dental Composite with PAMAM for Root Dentin Remineralization. Materials 2017, 10, 89. [Google Scholar] [CrossRef] [PubMed]
- Liang, K.; Wang, S.; Tao, S.; Xiao, S.; Zhou, H.; Wang, P.; Cheng, L.; Zhou, X.; Weir, M.D.; Oates, T.W.; et al. Dental remineralization via poly(amido amine) and restorative materials containing calcium phosphate nanoparticles. Int. J. Oral Sci. 2019, 11, 15. [Google Scholar] [CrossRef]
- Gao, Y.; Liang, K.; Weir, M.D.; Gao, J.; Imazato, S.; Tay, F.R.; Lynch, C.D.; Oates, T.W.; Li, J.; Xu, H.H.K. Enamel remineralization via poly(amido amine) and adhesive resin containing calcium phosphate nanoparticles. J. Dent. 2020, 92, 103262. [Google Scholar] [CrossRef]
- Tezvergil-Mutluay, A.; Seseogullari-Dirihan, R.; Feitosa, V.P.; Cama, G.; Brauer, D.S.; Sauro, S. Effects of Composites Containing Bioactive Glasses on Demineralized Dentin. J. Dent. Res. 2017, 96, 999–1005. [Google Scholar] [CrossRef]
- Huyang, G.; Debertin, A.E.; Sun, J. Design and development of self-healing dental composites. Mater. Des. 2016, 94, 295–302. [Google Scholar] [CrossRef]
- Wang, J.; Liu, Y.; Yu, J.; Sun, Y.; Xie, W. Study of POSS on the Properties of Novel Inorganic Dental Composite Resin. Polymers 2020, 12, 478. [Google Scholar] [CrossRef] [PubMed]
- Park, H.Y.; Kloxin, C.J.; Abuelyaman, A.S.; Oxman, J.D.; Bowman, C.N. Novel dental restorative materials having low polymerization shrinkage stress via stress relaxation by addition-fragmentation chain transfer. Dent. Mater. 2012, 28, 1113–1119. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Huang, Z.-M.; Zhang, C.-C.; Xue, Y.-D. Stiffness prediction of short fiber reinforced composites. Int. J. Mech. Sci. 2019, 161-162, 105068. [Google Scholar] [CrossRef]
| Antibacterial Property | Adhesive Property | Remineralization Property | Mechanical Property | Anti-Aging Property | Aesthetic Property | |
|---|---|---|---|---|---|---|
| Amalgam | + | − | − | + | + | − |
| Conventional Glass Ionomer Cement | + | + | + | − | − | − |
| High-Viscosity Glass Ionomer Cement (Ketac Molar Easymix, etc.) | + | + | + | + | − | − |
| Resin-modified Glass Ionomer Cement (Fuji II LC, etc.) | + | + | + | − | + | + |
| Conventional Light Curing Composite Resin | − | − (Without adhesive system) | − | + | − | + |
| Fluoride-releasing composite (Compomer, e.g., Dyract Extra, etc.; Giomer, e.g., Beautifil II, etc.) | Further studies are needed | − (Without adhesive system) | Further studies are needed | + | − | + |
| Short Fiber-reinforc ed composite (everX Flow, everX Posterior, etc.) | Further studies are needed | − (Without adhesive system) | Further studies are needed | + | + | + |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, Y.; Song, B.; Zhou, X.; Chen, H.; Wang, H.; Cheng, L. Dental Restorative Materials for Elderly Populations. Polymers 2021, 13, 828. https://doi.org/10.3390/polym13050828
Huang Y, Song B, Zhou X, Chen H, Wang H, Cheng L. Dental Restorative Materials for Elderly Populations. Polymers. 2021; 13(5):828. https://doi.org/10.3390/polym13050828
Chicago/Turabian StyleHuang, Yuyao, Bingqing Song, Xuedong Zhou, Hui Chen, Haohao Wang, and Lei Cheng. 2021. "Dental Restorative Materials for Elderly Populations" Polymers 13, no. 5: 828. https://doi.org/10.3390/polym13050828
APA StyleHuang, Y., Song, B., Zhou, X., Chen, H., Wang, H., & Cheng, L. (2021). Dental Restorative Materials for Elderly Populations. Polymers, 13(5), 828. https://doi.org/10.3390/polym13050828






