Simple Summary
Complications after major surgery for gastrointestinal cancers are common. Physiotherapists are frequently employed by hospitals to treat patients, with interventions aimed at minimising complications and improving recovery after surgery. At present, the most effective physiotherapy interventions for this patient population are unknown. It is unclear if providing physiotherapy confers additional benefit compared to no treatment. Additionally, it is unknown if the timing of physiotherapy interventions, preoperatively, perioperatively or postoperatively, impacts outcomes. Currently, no systematic review has specifically examined the efficacy of physiotherapy in the gastrointestinal cancer surgery population. This systematic review will evaluate and synthesise the evidence, examining the effects of perioperative physiotherapy interventions delivered with a prophylactic intent on postoperative outcomes.
Abstract
Background/Objectives: Major surgery for gastrointestinal cancer carries a 50% risk of postoperative complications. Physiotherapists commonly provide interventions to patients undergoing gastrointestinal surgery for cancer with the intent of preventing complications and improving recovery. However, the evidence is unclear if physiotherapy is effective compared to providing no physiotherapy, nor if timing of service delivery during the perioperative pathway influences outcomes. The objective of this review is to evaluate and synthesise the evidence examining the effects of perioperative physiotherapy interventions delivered with prophylactic intent on postoperative outcomes compared to no treatment or early mobilisation alone. Methods: A protocol was prospectively registered with PROSPERO and a systematic review performed of four databases. Randomised controlled trials examining prophylactic physiotherapy interventions in adults undergoing gastrointestinal surgery for cancer were eligible for inclusion. Results: Nine publications from eight randomised controlled trials were included with a total sample of 1418 participants. Due to inconsistent reporting of other perioperative complications, meta-analysis of the effect of physiotherapy was only possible specific to postoperative pulmonary complications (PPCs). This found an estimated 59% reduction in risk with exposure to physiotherapy interventions (RR 0.41, 95%CI 0.23 to 0.73, p < 0.001). Sub-group analysis demonstrated that timing of delivery may be important, with physiotherapy delivered only in the preoperative phase or combined with a postoperative service significantly reducing PPC risk (RR 0.32, 95%CI 0.17 to 0.60, p < 0.001) and hospital length of stay (MD–1.4 days, 95%CI −2.24 to −0.58, p = 0.01), whilst the effect of postoperative physiotherapy alone was less certain. Conclusions: Preoperative-alone and perioperative physiotherapy is likely to minimise the risk of PPCs in patients undergoing gastrointestinal surgery for cancer. This challenges current traditional paradigms of providing physiotherapy only in the postoperative phase of surgery. A review with broader scope and component network analysis is required to confirm this.
1. Introduction
Surgery is often necessary for the curative management of colorectal, upper gastrointestinal and hepatobiliary cancers. Major gastrointestinal surgery does not come without risk, with up to 50% of patients suffering a postoperative complication [1,2], which are associated with poorer outcomes, prolonged recovery for patients [3] and significant financial ramifications for the health service [4]. Understandably, the implementation of strategies to prevent postoperative complications are strongly advised [1].
Physiotherapists are commonly employed by hospitals in high-income countries to preoperatively assist patients to prepare for surgery [5] and postoperatively to aid a patient’s physical recovery and to prevent postoperative complications [6], with a particular focus on postoperative pulmonary complications (PPC) [6]. The most effective physiotherapeutic methods for preventing complications after abdominal surgery remain uncertain [7,8], predominantly due to a lack of clarity on whether additional physiotherapy interventions provide further benefit to early postoperative mobilisation alone [8]. Additionally, effect differences according to the timing of physiotherapy interventions; given either preoperatively, postoperatively, or perioperatively is not clearly understood.
The most recent systematic reviews specifically exploring physiotherapy interventions in the abdominal surgery population were published in 2006 [9,10]. Since 2006, new randomised controlled trials (RCTs) have been published that would not have been considered in these reviews. Importantly, neither of these systematic reviews were specific to the gastrointestinal cancer surgery population. Considering the large worldwide volume of gastrointestinal cancer surgery and the ubiquitous provision of physiotherapy services to these patients in high-income countries, it is essential that the evidence specific to physiotherapy in the gastrointestinal cancer surgery population is explored. Additionally, performing an updated systematic review will allow the adoption of modern statistical analysis techniques that were not available for earlier reviews.
This systematic review will evaluate and synthesise the evidence for perioperative physiotherapy interventions delivered with a prophylactic intent to effect postoperative outcomes when compared to a no-treatment control, or usual care of early mobilisation alone, in adults undergoing gastrointestinal surgery for cancer. The primary outcome will be PPCs with a sub-group analysis of effect due to timing of physiotherapy interventions. Impacts to other outcomes including medical and surgical complications, acute length of stay, functional outcomes, all-cause mortality and adverse events attributable to physiotherapy will also be explored.
2. Materials and Methods
2.1. Protocol and Registration
The protocol for this systematic review and meta-analysis was prepared in line with the Preferred Reporting Items for Systematic Review Protocols (PRISMA 2020) [11] and prospectively registered with the International Prospective Register of Systematic Reviews (PROPSERO CRD42024578131). There were no deviations to the published protocol.
2.2. Study Eligibility Criteria
Studies eligible for inclusion needed to have met the following criteria (Table 1).

Table 1.
Study inclusion criteria.
2.2.1. Design
Randomised controlled, pseudo-randomised and cluster randomised trials.
2.2.2. Participants
Due to the specific focus of this review on the major gastrointestinal cancer surgery population, studies were only eligible for inclusion if they enrolled participants aged 18 years and over of whom no less than 50% were undergoing major gastrointestinal surgery for cancer. Major gastrointestinal surgery for cancer was defined as surgery via any type of intra-peritoneal incision (e.g., open, laparoscopic, minimally invasive) to the abdomen, involving luminal resection or resection of a whole, or part of a, solid organ within the gastrointestinal tract and requiring general anaesthetic and a minimum overnight stay in hospital [6,12]. For this review, oesophagectomy was classified as gastrointestinal surgery.
2.2.3. Interventions
Perioperative physiotherapy techniques/treatments with the intent of minimising the deleterious impacts of anaesthesia and major surgery [6,13] including but are not limited to PPCs, postoperative ileus, wound infection and deep vein thrombosis. Physiotherapy techniques include interventions delivered preoperatively to enhance a patient’s knowledge of their risk of a PPC, training on breathing exercises, and targeted respiratory muscle strengthening [5]. Postoperative interventions include lung expansion techniques, such as coached deep breathing exercises or incentive spirometry and targeted therapeutic physical activity [6]. For the purposes of this review, interventions had to be delivered with the intent of prophylaxis against postoperative complications not in response to signs of deterioration or a diagnosis of a complication.
Prehabilitation consisting of multi-modal or whole-body exercise in the gastrointestinal surgery population delivered with the aim of enhancing preparedness for surgery and reducing postoperative complications were not included in this systematic review as numerous systematic reviews summarising the evidence of this multimodal intervention on postoperative complications have been conducted [6]. Non-invasive ventilation (NIV) was also specifically excluded due to recent systematic reviews in the abdominal surgery population [14].
Interventions for this systematic review included the following:
- (i)
- Patient education and training to perform self-directed breathing exercises;
- (ii)
- Coached/supervised breathing exercises, without augmentation with a device;
- (iii)
- Respiratory muscle training;
- (iv)
- Positive expiratory pressure therapy;
- (v)
- Incentive spirometry;
- (vi)
- Postoperative supervised/assisted mobilisation and physical activity;
- (vii)
- Combinations of above.
The time point of therapy was recorded: preoperative only, postoperative only or perioperative. Eligible interventions were required to be delivered by physiotherapists (including exercise therapists, and respiratory therapists). This restriction was chosen as physiotherapists are the predominant profession providing these interventions in high-income countries. Physiotherapists are also specifically trained in the provision of these interventions with minimum competency standard thresholds and credentialing as part of entry level tertiary qualifications. This provides some quality assurance of the interventions delivered in included trials minimising the possible influence of unknown or low quality treatment fidelity on outcomes. Interventions delivered by a Therapy Assistant under explicit instruction from the physiotherapist were also included as this also is reflective of current practice in many hospitals.
2.2.4. Comparator
A true no-treatment control (i.e., absence of any physiotherapy treatment) or usual care. Usual care in high-income country health care systems includes a culture of routine early mobilisation out of bed for patients post major surgery and the general encouragement of breathing exercise but not the provision of specific coaching for breathing exercises or the use of devices such as incentive spirometers [6,15]. Studies were excluded if the comparator involved participants receiving any type of active physiotherapy interventions beyond this definition.
2.2.5. Outcomes
The primary outcome for this systematic review was the incidence of a PPC within the acute hospital stay including: composite PPC diagnostic tools [16], atelectasis as diagnosed from radiographic imaging or lung ultrasound, pneumonia (any diagnostic construct), acute respiratory failure (any diagnostic construct), or acute hypoxemia (arterial blood gases, pulse oximetry) [17]. Secondary outcomes are any type of reported in-hospital medical or surgical complication, functional recovery measures, length of hospital stay, 30 day mortality and health related quality of life. Measures of adherence to delivered interventions and any adverse events associated with the intervention will also be collected.
2.2.6. Exclusion Criteria
A study was excluded if:
- -
- It was in a language other than English and a reliable translation could not be obtained.
- -
- More than 50% of participants had a surgical procedure for an indication other than cancer (i.e., bariatric surgery or cholecystectomy) or where the surgery did not involve the gastrointestinal tract (i.e., gynaecological or urological).
- -
- Participants had a diagnosis of a PPC on entry into trial.
- -
- It compared interventions to other active interventions, unless a sub-category comparing an active intervention to a suitable control could be extracted.
- -
- The intervention was part of a multimodal package of care and the independent effect of the physiotherapy intervention could not be determined, e.g., Enhanced Recovery After Surgery or fast-track pathways.
- -
- The intervention was prehabilitation of whole-body strength and/or conditioning
- -
- The intervention was NIV.
For further details of inclusion and exclusion criteria, see Table S1 in the Supplementary Material.
2.3. Search Strategy
The search strategy was developed by the primary author (SW) in consultation with a medical librarian experienced in the development of health-related systematic review search strategies. Study investigators peer-reviewed the draft search strategy which then underwent piloting and validity refinement. The search string was developed for MEDLINE and modified appropriately for other databases (Table S2, Supplementary Material, for full search strategy and MESH terms). No language or publication date restrictions were applied.
2.4. Information Sources
A systematic search was undertaken in MEDLINE via PubMed, Wed of Science, CINAHL Complete via EBSCO Host and COCHRANE Central on 21 and 22 August 2024. Reference lists of full-text articles selected for inclusion were screened for additional citations not captured in the original search strategy.
2.5. Study Selection
All identified records were imported into Covidence [18] where duplicates and ineligible studies were removed by automation tools then manually checked (SW). Two reviewers (SW and SM) independently conducted all stages of study review and selection. Search results were screened by title and abstract, with clearly ineligible articles excluded. All remaining articles underwent full-text review for eligibility against the inclusion criteria. A third party (IB) reviewed circumstances where consensus was not reached between the two reviewers, with their decision considered final. Study flow through the screening and selection process was captured in a PRISMA flow chart (see Figure 1). Explanations for article exclusion following full-text review are recorded (Table S3, Supplementary Material).
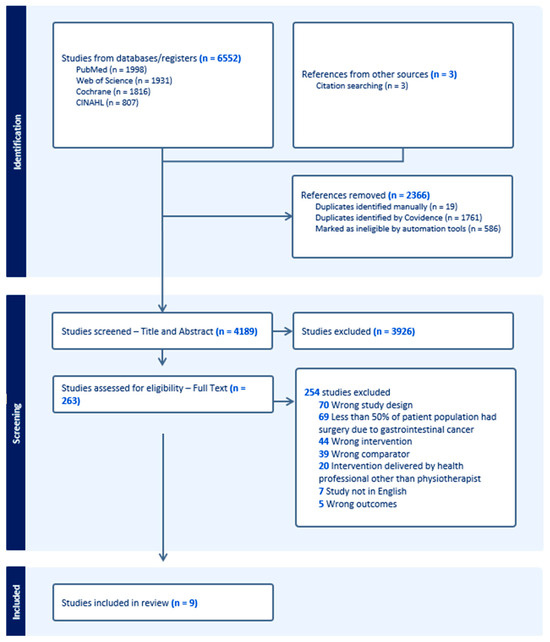
Figure 1.
PRISMA flow chart of included and excluded studies within this systematic review and meta-analysis.
2.6. Data Collection Process
Data were extracted from selected studies independently by two reviewers (SW and SM) using a standardised form. Disagreements on data extraction were addressed through a cooperative review of the original source, with any unresolved conflicts managed by a third party (IB). Where data in the published study were unclear, the primary author attempted to contact the corresponding author via email to request further information.
2.7. Data Items
Data extracted included the following:
- -
- Study details (author, year published, title, journal, country of recruitment).
- -
- Methods (design, randomization, blinding, number of study arms).
- -
- Participants (numbers recruited, demographics).
- -
- Intervention and comparator details.
- -
- For dichotomous outcome measures, the number of participants in each group meeting the outcome.
- -
- For continuous outcomes, the mean and variance for each group. When mean and variance were not reported in the original article, these were calculated from the raw data using Cochrane methods [19].
2.8. Risk of Bias
Three reviewers (SW, RM and JW) independently appraised each included study for methodological quality and risk of bias (RoB 2.0; www.riskofbias.info/ (accessed on 28 October 2024) [20]. Any disagreements were resolved by consensus, with referral if necessary to a fourth assessor (IB). The risk of bias scoring was not an eligibility criterion for this systematic review.
2.9. Data Synthesis
Extracted data were synthesised using descriptive statistics and, where possible, meta-analyses were conducted. Pooled data were analysed for the effect of physiotherapy compared to a control of no physiotherapy or usual care of early mobilisation alone on the rate of PPCs (the primary outcome). Where a study had more than one intervention arm and both arms complied with the inclusion criteria, data were amalgamated into a single intervention group for meta-analysis [19]. Sensitivity analyses were conducted on the primary outcome to determine (a) the effect of removing data from studies with a high risk of bias, and (b) the effect of physiotherapy on different PPC diagnostic constructs.
Sub-group analyses for the effect of physiotherapy intervention delivery timing (preoperative, postoperative, perioperative) on the primary outcome were performed. Where data were available, secondary analyses were performed for the effect of physiotherapy on all-cause surgical and medical complications and the acute hospital stay.
Where meta-analysis was conducted, data were pooled using commercially available software [21] with Mantel–Haenszel (MH) random-effects modelling and graphically represented. Heterogeneity of the true effect size within included studies was assessed using the 95% prediction interval (PI) rather than the I2 statistic [22]. The I2 statistic provides information about the proportion of variance in observed effects due to variance in the true effect rather than sampling error and does not provide information about how much effect sizes may vary between studies [22,23]. If the PI demonstrates that the effect size is consistent across studies, the impact of the intervention will be similar for all relevant populations. Should the PI demonstrate that the effect size varies substantially, inferences can be made as to whether the effect is always beneficial but with differing degrees of effect (trivial to moderate to large) or even that the effect may be beneficial in some instances and potentially not beneficial in others [23]. By employing the PI, insights can be gained into the clinical interpretation of heterogeneity by estimating the true treatment effects that can be expected in the treatment of future patients [24].
Dichotomous outcomes were calculated using risk ratios (RR) and 95% confidence intervals (95%CI). Continuous outcomes were calculated as mean differences (MD) when data were on a uniform scale and standardised mean differences (SMD) with 95%CI when data were on a different scale.
3. Results
3.1. Search Results
Systematic searches produced a total of 6555 records (Figure 1). After duplicate removal and screening of titles and abstracts, 263 records proceeded to full-text screening with 254 excluded. Of excluded studies, 69 were deemed ineligible as the surgery was not due to gastrointestinal cancer. An additional 39 studies were excluded because an active control was used as the comparator (i.e., incentive spirometry was compared to coached deep breathing exercises). Twenty studies were excluded as the intervention was delivered by a health professional other than a physiotherapist (see Table S3, Supplementary Material, for detailed description of exclusion reasons). After exclusions, nine publications from eight RCTs met the inclusion criteria (Table 2) [25,26,27,28,29,30,31,32,33].

Table 2.
Characteristics of included studies.
3.2. Study Characteristics
The nine included publications had sample sizes ranging from 41 to 441 participants. A total of 1418 participants were randomised into intervention or control groups. Loss-to-follow up was low, with primary outcome data available from 732 intervention group participants and 638 control group participants (combined 1370/1418 (97%)). Two studies involved a four-arm design where three different interventions were each compared with a no-treatment control [27,30]. The six other studies compared a single intervention arm with a control. There was one multicentre international study (Australian and New Zealand) reporting different outcomes over two publications [25,26]. The others were single-centre trials conducted in Sweden, Brazil, China, the Republic of Korea, India and the United Kingdom. Characteristics of the included studies can be seen in Table 2.
3.3. Risk of Bias
Methodological limitations and overall risk of bias was determined to be low for three studies [25,28,31] and moderate in three studies [29,30,32]. Two studies were assessed as high risk of bias [27,33], with possible outcome reporting limitations [27,33] and imbalanced randomization [33]. For example, 28% of controls had oesophageal cancer compared to 4% of intervention participants and 40% of the control group had stomach cancer compared to 24% of the intervention group in the study published by Singh et al. [33]. See Table S4, Supplementary Material, for the risk of bias figure.
3.4. Participants
Participants were, on average, 62 years old (SD 16) and there was an equal representation of the sexes (52.5% (703/1338) male). One study restricted recruitment to only those at high risk of developing PPCs [28] whilst, conversely, one study excluded participants with pre-existing respiratory disease [33]. All other studies included all patients generally listed for gastrointestinal surgery [25,26,27,29,30,31,32] with a majority of participants having an American Society of Anesthesiologists (ASA) score of 1 or 2 (971/1338 (73%)). Seven studies included a variety of gastrointestinal surgery procedures [25,26,27,28,29,30,33], whilst two focused on colorectal surgery [31,32]. Participant characteristics for all included studies can be seen in Table 2.
3.5. Interventions
3.5.1. Preoperative Alone
Three studies provided preoperative physiotherapy alone. Two provided a single education and training session (15–30 min) where patients were taught breathing exercises and instructed to start these independently on waking from their anaesthetic after surgery [25,29]. The other provided training in preoperative breathing exercises, augmented with either an incentive spirometer or respiratory muscle trainer, to be completed independently prior to surgery twice daily for a minimum of two weeks before surgery [27]. Refer to Table 3 for detailed intervention characteristics of the included studies that provided preoperative physiotherapy alone.

Table 3.
Intervention characteristics of included studies.
3.5.2. Postoperative Alone
Three studies investigated postoperative physiotherapy. One provided intensive daily coached breathing exercise sessions for a minimum of ten sessions across the first four postoperative days [28]. Another provided three coached breathing exercise sessions per day with or without incentive spirometers for the first five postoperative days [30]. The final study provided twice-daily 15 min whole-body exercise sessions from the first postoperative day until hospital discharge [31]. Table 3 provides intervention characteristics for included studies that provided postoperative physiotherapy alone.
3.5.3. Perioperative (Both Preoperative and Postoperative Interventions)
One study admitted patients to hospital five days before surgery where thrice daily education and coached breathing exercises and positive expiratory pressure blowing therapy was supervised with these therapies continuing for four days following surgery [32]. The final study provided outpatient preoperative supervised breathing exercises and incentive spirometry for 30 min twice daily for up to five days which continued postoperatively in hospital for an unspecified period [33]. Detailed intervention characteristics of the included studies that explored perioperative interventions can be found in Table 3.
3.6. Comparators
Four studies had a control group where participants were not provided with any physiotherapy [27,29,30,31]. In two studies, participants, including those in the control, were provided with a standardised postoperative ambulation protocol delivered by physiotherapists [25,26,28] whilst two studies provided a control of general encouragement of mobilisation but did not specify who provided this [32,33]. Table 3 provides details of the comparator for each included study.
3.7. Adherence to Intervention
Two studies reported participant adherence to physiotherapy interventions. One study recorded that the intervention group performed significantly more breathing and coughing exercises [28] and the other reported excellent adherence (85%) to prescribed physical exercise sessions [31]. Table 3 highlights adherence to interventions for each included study.
3.8. PPC Outcomes
Outcomes and the time point measured are found in Table 2. Two studies reported PPCs using composite diagnostic tools [25,28], whilst four reported PPCs as total incidence from a composite of different respiratory diagnoses [27,30,32,33]. The effect of physiotherapy on pneumonia was reported in four studies [25,29,32,33], two studies [25,32] reported acute respiratory failure, two reported hypoxaemia [26,29] and three reported atelectasis [26,32,33].
3.9. Effect of Physiotherapy Interventions on Primary Outcome
PPC
Seven of eight studies [25,27,28,29,30,32,33] measured the incidence of PPCs in a physiotherapy intervention group compared to no physiotherapy or early mobilisation alone and were included in the meta-analysis. The aggregated data from these existing studies suggest that exposure to a respiratory focused physiotherapy intervention is likely to result in an estimated 59% reduction in the risk of PPCs with 95% probability that the true effect is between a 27% to 77% reduction in risk (RR 0.41, 95%CI 0.23 to 0.73, p < 0.001). However, as existing studies vary significantly in effect direction, the calculated PI of 0.09 to 1.91 indicates there is a 95% probability that future studies in this field could be either positive or negative in effect (see Figure 2).
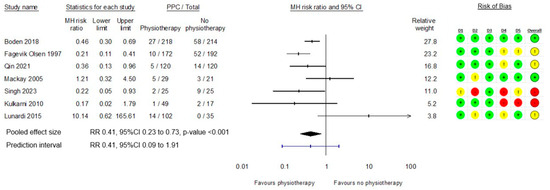
Figure 2.
Meta-analysis of effect of physiotherapy on PPCs with risk of bias grading [25,27,28,29,30,32,33].
A sensitivity analysis was undertaken for the primary outcome excluding studies assessed at high risk of bias [27,33]. Removing these two studies from the analysis did not change the mean estimate of the effect of the intervention. However, the certainty of a clinically meaningful difference in PPC risk is lessened with the 95% confidence interval including the possibility of as little as a 3% reduction in PPC risk with exposure to a physiotherapy intervention (RR 0.48, 95%CI 0.24 to 0.97, p = 0.04, 95% PI 0.05 to 4.35).
Sensitivity analyses of the effects of physiotherapy on alternate PPC diagnostic constructs found a certain reduction in pneumonia risk (RR 0.37, 95%CI 0.21 to 0.63, p < 0.001), However, the effect of physiotherapy on acute respiratory failure (RR 0.40, 95%CI 0.15 to 1.07, p = 0.07), atelectasis (RR 0.52, 95%CI 0.24 to 1.11, p = 0.09) and acute hypoxemia (RR = 0.26, 95%CI 0.02 to4.36, p = 0.32) is less certain (Figure 3a).
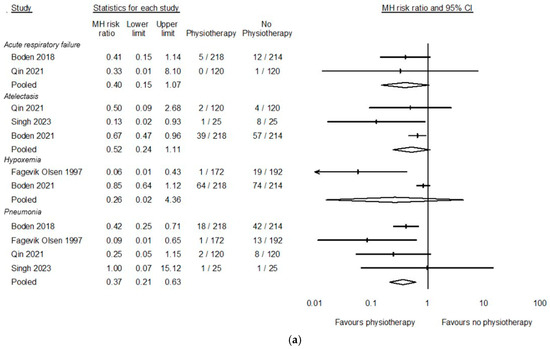
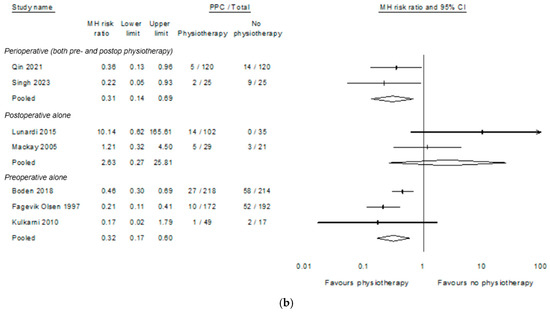
Figure 3.
(a). Sensitivity analysis of effect of physiotherapy on different PPC diagnostic constructs [25,26,29,32,33]; (b). Sub-group analysis of the effect of time of delivery of physiotherapy on PPCs [25,27,28,29,30,32,33].
A sub-group analysis was performed to explore if the timing of physiotherapy delivery influenced the primary outcome. Interventions delivered preoperatively (RR 0.44, 95%CI 0.29 to 0.67, p < 0.001) and perioperatively (RR 0.25, 95%CI 0.15 to 0.41, p < 0.001) may lead to a probable reduction in PPC risk, whereas interventions delivered only in the postoperative phase may be unlikely to effect PPC risk (RR 2.41, 95%CI 0.34 to 17.03, p = 0.38). See Figure 3b.
3.10. Effect of Physiotherapy Interventions on Secondary Outcomes
3.10.1. All-Cause Complications
Due to significant heterogeneity amongst the classification and reporting of postoperative complications across the included studies, it was not possible to conduct a meta-analysis of the effect of physiotherapy on surgical complications separately to medical complications. For this review these outcomes were aggregated to all-cause complications. For specific details regarding the data extracted and aggregated from each included study for all-cause complications, please see Table S5, Supplementary Materials. Although the effect estimate favours physiotherapy interventions to reduce the risk of all-cause postoperative complications, the probability of a null effect has not been excluded (RR 0.87, 95%CI 0.71 to 1.05, p = 0.15, Figure 4).
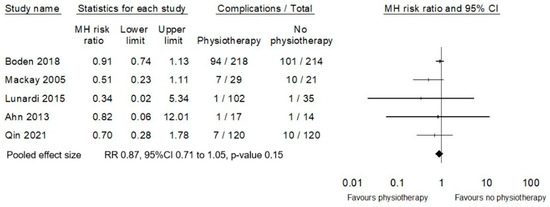
Figure 4.
Meta-analysis of effect of physiotherapy on all-cause complications (excluding PPC) [25,28,30,31,32].
3.10.2. Hospital Length of Stay
Pooled data from seven studies reporting hospital stay [25,28,29,30,31,32,33] suggest an estimated reduction in a day less in hospital for participants provided with physiotherapy (MD–1.4 days, 95%CI −2.24 to −0.58, p = 0.01, Figure 5). Sub-group analyses according to timing of the physiotherapy intervention finds that the extent of this benefit may be influenced by the timing of physiotherapy delivery, with perioperative physiotherapy indicating a more beneficial effect on length of stay than postoperative physiotherapy alone.
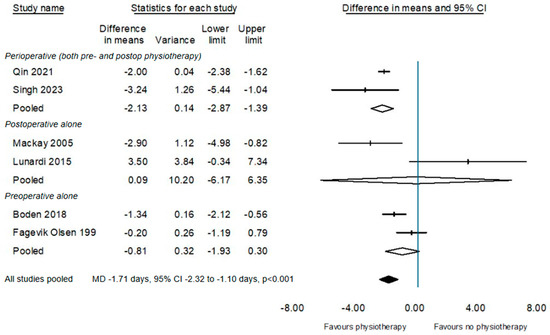
Figure 5.
Sub-group of the effect of physiotherapy on acute hospital length of stay according to timing of delivery of physiotherapy intervention [25,28,29,30,32,33].
3.10.3. Functional Outcomes
Due to significant heterogeneity in the assessment of functional outcomes, a meta-analysis was not possible. Of the three studies that reported functional outcomes, none reported a significant difference between groups [25,28,31].
3.10.4. All-Cause Mortality
Pooled data from three studies reporting in-hospital all-cause mortality [25,28,30] did not detect an effect favouring physiotherapy (RR 1.01, 95%CI 0.30 to 3.40).
3.10.5. Quality of Life
No study reported HRQoL within the first 30 days post-surgery.
3.10.6. Adverse Events
There were no adverse events reported to be directly associated with physiotherapy interventions [25,31].
4. Discussion
This systematic review and meta-analysis aggregated data from eight RCTs that investigated physiotherapy interventions to prevent postoperative complications and improve recovery following major gastrointestinal surgery for cancer. This is the first systematic review to consider the effect of physiotherapy compared to providing no physiotherapy or postoperative early mobilisation alone in this specific cancer surgery population. The meta-analysis of pooled data finds that physiotherapy is likely to be effective in halving the risk of a patient developing a PPC, including pneumonia, and in reducing acute hospital length of stay by one to two days. These data also suggest that these effects are most likely to be achieved if physiotherapy is delivered in both the pre- and postoperative phases of gastrointestinal surgery, with the benefits of a postoperative-alone physiotherapy service uncertain.
This new meta-analysis aligns with earlier systematic reviews exploring physiotherapy for the prevention of PPCs in patients undergoing abdominal surgery. Two previous meta-analyses concluded that prophylactic respiratory physiotherapy is likely to be effective in reducing PPCs [7,9]. Two other meta-analyses that report greater uncertainty about the effect of physiotherapy may be limited as both specifically excluded preoperative physiotherapy interventions [8,10].
High-quality RCTs assessing the effectiveness of preoperative education and deep breathing exercise training in this patient population have consistently reported positive effects [25,27,34,35]. At present, the evidence appears to support the provision of preoperative interventions including physiotherapy education and training [34], inspiratory muscle training [36], and prehabilitation as the most effective way of preventing PPCs [37]. Data from our study support these previous studies, suggesting that the timing of prophylactic interventions influences the risk of PPCs, with preoperative physiotherapy likely to reduce the risk of PPCs after gastrointestinal surgery for cancer and with the effects of postoperative physiotherapy alone uncertain. This may directly challenge traditional paradigms of care where hospitals in high-income countries predominantly only provide physiotherapy postoperatively [38,39,40].
From a clinical perspective, postoperative physiotherapy alone may not be sufficient to prevent postoperative complications in this patient population and preoperative physiotherapy appears to have greater effect in reductions in complications such as PPCs. However, the limited number of studies investigating physiotherapy for patients having major gastrointestinal surgery for cancer and the inconsistent effect direction mean that currently, there are not enough data to provide firm recommendations for practice change in this area. A meta-analysis with greater scope is required before any practice recommendations can be made for postoperative physiotherapy, and therefore, the authors currently advise that clinicians maintain the status quo of current physiotherapy service delivery with regard to postoperative physiotherapy.
The initial intent of this review was to analyse a broad range of physiotherapy interventions for patients having gastrointestinal surgery for cancer; however, following the application of stringent predetermined inclusion criteria, only nine publications from eight RCTs were eligible for inclusion. There were several considerations guiding the application of stringent inclusion criteria for this review. Most abdominal surgery RCTs define patient populations via incision type or location [6] rather than by indication for surgery. Consequently, 69 RCTs were excluded because it could not be established that at least 50% of patients had specifically undergone gastrointestinal surgery for cancer. Studies of multimodal Enhanced Recovery After Surgery (ERAS) programmes aimed at reducing an array of postoperative complications and enhancing outcomes [15,41] added complexity to the screening process. Due to the multi-modal, multi-professional nature of the ERAS interventions, effects of the physiotherapy intervention could not be independently determined, deeming these studies ineligible.
Specifying the comparator to be a true no-treatment control or clearly defined usual care of early mobilisation further restricted study eligibility with 39 clinical trials excluded on this basis. Many RCTs exploring the efficacy of physiotherapy interventions employ a direct comparison of one active intervention compared to one or more other active interventions. Whilst this methodology resolves how effective one intervention is compared to another, it does not resolve whether an intervention provides any additional benefit compared to no treatment or standardised usual care [19]. Given the current uncertainty regarding whether additional physiotherapy beyond usual care confers greater benefits in the broader abdominal surgery population, it was necessary to include only studies that met the comparator eligibility criteria.
Only interventions specifically delivered by physiotherapists (or equivalent) were included in this review, resulting in a further 20 studies being excluded. Although respiratory exercises and postoperative therapeutic rehabilitation may be delivered by health professionals other than physiotherapists (or equivalent), these interventions are commonly considered a primary defined role of physiotherapists working within the multidisciplinary hospital teams caring for this patient population in high-income countries. Furthermore, physiotherapists undergo specific training in the provision of these interventions as part of minimum core competency thresholds to achieve entry level tertiary qualifications. The quality and standardisation of respiratory and rehabilitation interventions delivered by other health professions is uncertain. To ensure that the results of this systematic review were unlikely to be influenced by questions of treatment fidelity and quality of the interventions, studies were restricted to only those where the interventions were provided or prescribed by qualified registered physiotherapists.
In the studies included in this current review, reporting of interventions and outcomes lacked clarity and consistency, at times affecting the data that could be extracted for analysis. Only two studies reported on adverse events attributed to physiotherapy intervention as a possible outcome [25,26,31]. Future trials could be improved by clearer detailed reporting of intervention dosage and patient adherence and this may allow better insights into feasibility of interventions for clinical practice and acceptability of interventions to clients [42]. It is recommended that all future RCTs prospectively collect and report on data regarding both the benefits and harms of health interventions [43]. Heterogenous outcome measures, especially for functional outcomes, impacted how findings were reported and whether these findings could be combined for meta-analysis. The use of standardised outcome measures in perioperative medicine is required to facilitate more accurate meta-analyses and reduce research waste [44,45]. Future RCTs should carefully consider these factors when selecting and reporting on appropriate outcomes measures.
The findings of this current meta-analysis may be limited by the small number of included studies and, consequentially, uncertainty in effect size estimates restricting the ability to make specific practice-related recommendations. Unanswered questions remain in this patient population including uncertainty regarding efficacy of postoperative mobilisation and efficacy of coached postoperative breathing exercises. High quality RCTs with appropriate comparators are required to advance understanding in this area of practice. Additional research is necessary to further validate the observed effects of preoperative physiotherapy, to strengthen confidence in making change of practice recommendations. Employing broader eligibility criteria by including clinical trials testing respiratory and whole-body exercise interventions delivered by any type of health care provider and in participants having all-cause abdominal surgery, not just for cancer, would have resulted in an additional 89 studies being included for data pooling. This additional data may have allowed for more definitive conclusions.
Future reviews in this field would be advised to expand eligibility criteria as outlined, particularly regarding interventions delivered by any health care provider and utilise sensitivity analyses to elicit whether intervention efficacy is influenced by the health discipline who provides that care. Moving forwards, a review of broader scope and with component network analysis [46] will assist with addressing remaining questions in this field of practice.
5. Conclusions
This systematic review contributes to previous findings supporting the hypothesis that prophylactic physiotherapy interventions may minimise the risk of PPCs after major surgery. This current review finds that the size of this effect specifically for patients having gastrointestinal surgery for cancer could be a large and significant reduction in risk of between 27% and 77% compared to patients who do not receive any type of physiotherapy or early mobilisation alone. These findings should be interpreted with caution given the low number of eligible studies and the heterogeneity of the included studies. The strength of the existing body of literature regarding preoperative physiotherapy indicates that preoperative physiotherapy should be implemented in this patient population. However, completion of a broader network meta-analysis is essential prior to considering any recommendations for practice changes in the delivery of postoperative physiotherapy. Until further evidence is available, clinicians who currently provide postoperative physiotherapy to patients undergoing major gastrointestinal cancer surgery are advised to maintain the status quo of their service delivery.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/cancers17040676/s1, Table S1: detailed inclusion and exclusion criteria; Table S2: Medline via PubMed Search Strategy; Table S3: Explanations for article exclusion following full-text review; Table S4: Cochrane Risk of Bias Assessment; Table S5: Classification of data extracted for all-cause complications per study. References [25,26,27,28,29,30,31,32,33] are mentioned in the supplementary materials.
Author Contributions
S.W. and I.B. are the principal investigators and conceived the systematic review. S.W., I.B., R.M. and K.J.H. were involved in the design of the study. I.B. and S.W. designed the data analysis plan and undertook data analysis. S.M. was involved in all stages of screening for eligible studies and data extraction. J.L.W. provided critical input and supervision for risk of bias screening. S.W. wrote the original draft manuscript. I.B. and J.R. provided critical review and editing of the manuscript. All authors have provided critical input and contributed important intellectual content regarding the design and methods of this study. All authors have read and agreed to the published version of the manuscript.
Funding
S.W. is supported by a University of Tasmania PhD scholarship. I.B. is supported by a National Health and Medical Research Council Investigator Grant 2022/GNT2016947.
Acknowledgments
The authors would like to acknowledge the expertise of University of Tasmania Research Librarian, Michaela Venn, for her assistance with the development of the search strategies for this systematic review.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| PPC | Postoperative pulmonary complication |
| ASA | American Society of Anaesthesiologists |
| RCT | Randomised controlled trial |
| HRQoL | Health related quality of life |
References
- van Kooten, R.T.; Bahadoer, R.R.; Peeters, K.; Hoeksema, J.H.L.; Steyerberg, E.W.; Hartgrink, H.H.; van de Velde, C.J.H.; Wouters, M.; Tollenaar, R. Preoperative Risk Factors for Major Postoperative Complications after Complex Gastrointestinal Cancer Surgery: A Systematic Review. Eur. J. Surg. Oncol. 2021, 47, 3049–3058. [Google Scholar] [CrossRef]
- Busweiler, L.; Henneman, D.; Dikken, J.; Fiocco, M.; van Berge Henegouwen, M.; Wijnhoven, B.; van Hillegersberg, R.; Rosman, C.; Wouters, M.; van Sandick, J. Failure-to-Rescue in Patients Undergoing Surgery for Esophageal or Gastric Cancer. Eur. J. Surg. Oncol. 2017, 43, 1962–1969. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.; Wang, J.; Chen, K.; Kang, M.; Zhang, H.; Jin, X.; Lin, L.; Chen, J. Relationship between Postoperative Complications and the Prognosis of Gastric Carcinoma Patients Who Underwent Surgical Resection: A Systematic Review and Meta-Analysis. Cancer Control 2021, 28, 10732748211011955. [Google Scholar] [CrossRef] [PubMed]
- Louis, M.; Johnston, S.A.; Churilov, L.; Ma, R.; Christophi, C.; Weinberg, L. Financial Burden of Postoperative Complications Following Colonic Resection: A Systematic Review. Medicine 2021, 100, e26546. [Google Scholar] [CrossRef] [PubMed]
- Boden, I.; Denehy, L. Respiratory Prehabilitation for the Prevention of Postoperative Pulmonary Complications after Major Surgery. Curr. Anesthesiol. Rep. 2022, 12, 44–58. [Google Scholar] [CrossRef]
- Boden, I. Physiotherapy Management of Major Abdominal Surgery. J. Physiother. 2024, 70, 170–180. [Google Scholar] [CrossRef] [PubMed]
- Odor, P.M.; Bampoe, S.; Gilhooly, D.; Creagh-Brown, B.; Moonesinghe, S.R. Perioperative Interventions for Prevention of Postoperative Pulmonary Complications: Systematic Review and Meta-Analysis. BMJ Br. Med. J. 2020, 368, m540. [Google Scholar] [CrossRef] [PubMed]
- Kokotovic, D.; Berkfors, A.; Gögenur, I.; Ekeloef, S.; Burcharth, J. The Effect of Postoperative Respiratory and Mobilization Interventions on Postoperative Complications Following Abdominal Surgery: A Systematic Review and Meta-Analysis. Eur. J. Trauma Emerg. Surg. 2021, 47, 975–990. [Google Scholar] [CrossRef]
- Lawrence, V.A.; Cornell, J.E.; Smetana, G.W.; Lawrence, V.A.; Cornell, J.E.; Smetana, G.W. Strategies to Reduce Postoperative Pulmonary Complications after Noncardiothoracic Surgery: Systematic Review for the American College of Physicians. Ann. Intern. Med. 2006, 144, 596–608. [Google Scholar] [CrossRef] [PubMed]
- Pasquina, P.; Tramèr, M.R.; Granier, J.M.; Walder, B. Respiratory Physiotherapy to Prevent Pulmonary Complications after Abdominal Surgery: A Systematic Review. Chest 2006, 130, 1887–1899. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E. The Prisma 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Courtney, A.; Clymo, J.; Dorudi, Y.; Moonesinghe, S.R.; Dorudi, S. Scoping Review: The Terminology Used to Describe Major Abdominal Surgical Procedures. World J. Surg. 2024, 48, 574–584. [Google Scholar] [CrossRef] [PubMed]
- Nijbroek, S.G.; Schultz, M.J.; Hemmes, S.N.T. Prediction of Postoperative Pulmonary Complications. Curr. Opin. Anesthesiol. 2019, 32, 443–451. [Google Scholar] [CrossRef] [PubMed]
- Lockstone, J.; Denehy, L.; Truong, D.; Whish-Wilson, G.A.; Boden, I.; Abo, S.; Parry, S.M. Prophylactic Postoperative Noninvasive Ventilation in Adults Undergoing Upper Abdominal Surgery: A Systematic Review and Meta-Analysis. Crit. Care Med. 2022, 50, 1522–1532. [Google Scholar] [CrossRef]
- Gustafsson, U.O.; Scott, M.J.; Hubner, M.; Nygren, J.; Demartines, N.; Francis, N.; Rockall, T.A.; Young-Fadok, T.M.; Hill, A.G.; Soop, M.; et al. Guidelines for Perioperative Care in Elective Colorectal Surgery: Enhanced Recovery after Surgery (Eras®) Society Recommendations: 2018. World J. Surg. 2019, 43, 659–695. [Google Scholar] [CrossRef] [PubMed]
- Abbott, T.E.F.; Fowler, A.J.; Pelosi, P.; Gama de Abreu, M.; Møller, A.M.; Canet, J.; Creagh-Brown, B.; Mythen, M.; Gin, T.; Lalu, M.M.; et al. A Systematic Review and Consensus Definitions for Standardised End-Points in Perioperative Medicine: Pulmonary Complications. Br. J. Anaesth. 2018, 120, 1066–1079. [Google Scholar] [CrossRef]
- Fernandez-Bustamante, A.; Frendl, G.; Sprung, J.; Kor, D.J.; Subramaniam, B.; Martinez Ruiz, R.; Lee, J.W.; Henderson, W.G.; Moss, A.; Mehdiratta, N.; et al. Postoperative Pulmonary Complications, Early Mortality, and Hospital Stay Following Noncardiothoracic Surgery: A Multicenter Study by the Perioperative Research Network Investigators. JAMA Surg. 2017, 152, 157–166. [Google Scholar] [CrossRef] [PubMed]
- Covidence Veritas Health Innovation. Covidence Systematic Review Software. Available online: www.covidence.org (accessed on 20 August 2024).
- Higgins, J.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions, version 6.5 (Updated August 2024); John Wiley & Sons: Chichester, UK, 2024; Available online: www.training.cochrane.org/handbook (accessed on 20 August 2024).
- Sterne, J.A.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M. Rob 2: A Revised Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Borenstein, M.; Hedges, L.; Higgins, J.; Rothstein, H. Comprehensive Meta-Analysis Version 4; Biostat: Englewood, NJ, USA, 2022. [Google Scholar]
- Borenstein, M. Research Note: In a Meta-Analysis, the I2 Index Does Not Tell Us How Much the Effect Size Varies across Studies. J. Physiother. 2020, 66, 135–139. [Google Scholar] [CrossRef] [PubMed]
- Borenstein, M. How to Understand and Report Heterogeneity in a Meta-Analysis: The Difference between I-Squared and Prediction Intervals. Integr. Med. Res. 2023, 12, 101014. [Google Scholar] [CrossRef]
- IntHout, J.; Ioannidis, J.P.A.; Rovers, M.M.; Goeman, J.J. Plea for Routinely Presenting Prediction Intervals in Meta-Analysis. BMJ Open 2016, 6, e010247. [Google Scholar] [CrossRef]
- Boden, I.; Skinner, E.H.; Browning, L.; Reeve, J.; Anderson, L.; Hill, C.; Robertson, I.K.; Story, D.; Denehy, L. Preoperative Physiotherapy for the Prevention of Respiratory Complications after Upper Abdominal Surgery: Pragmatic, Double Blinded, Multicentre Randomised Controlled Trial. BMJ 2018, 360, j5916. [Google Scholar] [CrossRef]
- Boden, I.; Reeve, J.; Robertson, I.K.; Browning, L.; Skinner, E.H.; Anderson, L.; Hill, C.; Story, D.; Denehy, L. Effects of Preoperative Physiotherapy on Signs and Symptoms of Pulmonary Collapse and Infection after Major Abdominal Surgery: Secondary Analysis of the Lippsmack-Pop Multicentre Randomised Controlled Trial. Perioper. Med. 2021, 10, 36. [Google Scholar] [CrossRef] [PubMed]
- Kulkarni, S.R.; Fletcher, E.; McConnell, A.K.; Poskitt, K.R.; Whyman, M.R. Pre-Operative Inspiratory Muscle Training Preserves Postoperative Inspiratory Muscle Strength Following Major Abdominal Surgery—A Randomised Pilot Study. Ann. R. Coll. Surg. Engl. 2010, 92, 700–707. [Google Scholar] [CrossRef]
- Mackay, M.R.; Ellis, E.; Johnston, C. Randomised Clinical Trial of Physiotherapy after Open Abdominal Surgery in High Risk Patients. Aust. J. Physiother. 2005, 51, 151–159. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Fagevik Olsén, M.; Hahn, I.; Nordgren, S.; Lönroth, H.; Lundholm, K. Randomized Controlled Trial of Prophylactic Chest Physiotherapy in Major Abdominal Surgery. Br. J. Surg. 1997, 84, 1535–1538. [Google Scholar] [CrossRef] [PubMed]
- Lunardi, A.C.; Paisani, D.M.; Silva, C.; Cano, D.P.; Tanaka, C.; Carvalho, C.R.F. Comparison of Lung Expansion Techniques on Thoracoabdominal Mechanics and Incidence of Pulmonary Complications after Upper Abdominal Surgery: A Randomized and Controlled Trial. Chest 2015, 148, 1003–1010. [Google Scholar] [CrossRef] [PubMed]
- Ahn, K.Y.; Hur, H.; Kim, D.H.; Min, J.; Jeong, D.H.; Chu, S.H.; Lee, J.W.; Ligibel, J.A.; Meyerhardt, J.A.; Jones, L.W.; et al. The Effects of Inpatient Exercise Therapy on the Length of Hospital Stay in Stages I-Iii Colon Cancer Patients: Randomized Controlled Trial. Int. J. Color. Dis. 2013, 28, 643–651. [Google Scholar] [CrossRef] [PubMed]
- Qin, P.P.; Jin, J.Y.; Wang, W.J.; Min, S. Perioperative Breathing Training to Prevent Postoperative Pulmonary Complications in Patients Undergoing Laparoscopic Colorectal Surgery: A Randomized Controlled Trial. Clin. Rehabil. 2021, 35, 692–702. [Google Scholar] [CrossRef]
- Singh, V.; Pai, S.A.; Hosmath, V. Clinical Outcome of Patients Undergoing Preoperative Chest Physiotherapy in Elective Upper Abdominal Surgeries. J. Perioper. Pract. 2023, 33, 182–189. [Google Scholar] [CrossRef] [PubMed]
- Boden, I.; Reeve, J.; Jernås, A.; Denehy, L.; Olsén, M.F. Preoperative Physiotherapy Prevents Postoperative Pulmonary Complications after Major Abdominal Surgery: A Meta-Analysis of Individual Patient Data. J. Physiother. 2024, 70, 216–223. [Google Scholar] [CrossRef] [PubMed]
- Lohiya, M.L.; Malviya, A.; Sharma, D.D.; Ram, S.; Chauhan, M.K.; Chauhan, L.S. Prophylactic Chest Physiotherapy in Major Abdominal Surgery among Elderly Patients. J. Indian. Acad. Geriatr. 2018, 14, 64–68. [Google Scholar] [CrossRef]
- Assouline, B.; Cools, E.; Schorer, R.; Kayser, B.; Elia, N.; Licker, M. Preoperative Exercise Training to Prevent Postoperative Pulmonary Complications in Adults Undergoing Major Surgery. A Systematic Review and Meta-Analysis with Trial Sequential Analysis. Ann. Am. Thorac. Soc. 2021, 18, 678–688. [Google Scholar] [CrossRef] [PubMed]
- Molenaar, C.J.L.; Minnella, E.M.; Coca-Martinez, M.; ten Cate, D.W.G.; Regis, M.; Awasthi, R.; Martínez-Palli, G.; López-Baamonde, M.; Sebio-Garcia, R.; Feo, C.V.; et al. Effect of Multimodal Prehabilitation on Reducing Postoperative Complications and Enhancing Functional Capacity Following Colorectal Cancer Surgery the Prehab Randomized Clinical Trial. JAMA Surg. 2023, 158, 572–581. [Google Scholar] [CrossRef] [PubMed]
- Patman, S.; Bartley, A.; Ferraz, A.; Bunting, C. Physiotherapy in Upper Abdominal Surgery—What Is Current Practice in Australia? Arch. Physiother. 2017, 7, 11. [Google Scholar] [CrossRef] [PubMed]
- Aldhuhoori, F.Z.; Walton, L.M.; Bairapareddy, K.C.; Amaravadi, S.K.; Alaparthi, G.K. Physiotherapy Practice for Management of Patients Undergoing Upper Abdominal Surgery in United Arab Emirates—A National Survey. J. Multidiscip. Healthc. 2021, 14, 2513–2526. [Google Scholar] [CrossRef] [PubMed]
- van Beijsterveld, C.A.; Heldens, A.F.; Bongers, B.C.; van Meeteren, N.L. Variation in Preoperative and Postoperative Physical Therapist Management of Patients Opting for Elective Abdominal Surgery. Phys. Ther. 2019, 99, 1291–1303. [Google Scholar] [CrossRef]
- Scott, M.; Baldini, G.; Fearon, K.; Feldheiser, A.; Feldman, L.; Gan, T.; Ljungqvist, O.; Lobo, D.; Rockall, T.; Schricker, T. Enhanced Recovery after Surgery (Eras) for Gastrointestinal Surgery, Part 1: Pathophysiological Considerations. Acta Anaesthesiol. Scand. 2015, 59, 1212–1231. [Google Scholar] [CrossRef] [PubMed]
- Nagpal, T.S.; Mottola, M.F.; Barakat, R.; Prapavessis, H. Adherence Is a Key Factor for Interpreting the Results of Exercise Interventions. Physiotherapy 2021, 113, 8–11. [Google Scholar] [CrossRef] [PubMed]
- Junqueira, D.R.; Zorzela, L.; Golder, S.; Loke, Y.; Gagnier, J.J.; Julious, S.A.; Li, T.; Mayo-Wilson, E.; Pham, B.; Phillips, R.; et al. Consort Harms 2022 Statement, Explanation, and Elaboration: Updated Guideline for the Reporting of Harms in Randomized Trials. J. Clin. Epidemiol. 2023, 158, 149–165. [Google Scholar] [CrossRef]
- Glasziou, P.; Chalmers, I. Research Waste Is Still a Scandal—An Essay by Paul Glasziou and Iain Chalmers. BMJ 2018, 363, k4645. [Google Scholar] [CrossRef]
- Myles, P.; Grocott, M.; Boney, O.; Moonesinghe, S.; Group, C.-S.; Myles, P.; Grocott, M.; Biccard, B.; Boney, O.; Chan, M. Standardizing End Points in Perioperative Trials: Towards a Core and Extended Outcome Set. Br. J. Anaesth. 2016, 116, 586–589. [Google Scholar] [CrossRef] [PubMed]
- Tsokani, S.; Seitidis, G.; Mavridis, D. Component Network Meta-Analysis in a Nutshell. BMJ Evid.-Based Med. 2023, 28, 183–186. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).