Simple Summary
Breast cancer survivors often experience multiple symptoms such as pain, fatigue, sleep disturbance, depression, anxiety, and hot flashes during endocrine therapy. This study examined the feasibility of integrating acupuncture into treatment options for symptom management among medically underserved breast cancer survivors. We randomized 62 participants into acupuncture and usual care groups. High retention and satisfaction rates indicated that acupuncture is both feasible and acceptable for this population. After 10 acupuncture sessions over 5 weeks, participants showed significant improvements in pain, fatigue, sleep disturbance, depression, and anxiety. This approach shows potential for reducing symptoms and addressing health disparities among underserved breast cancer survivors.
Abstract
Background/Objectives: Breast cancer survivors undergoing long-term endocrine therapy often experience multiple symptoms, including pain, fatigue, sleep disturbance, hot flashes, anxiety, and depression. This study explored the feasibility and acceptability of integrating acupuncture for symptom management in medically underserved breast cancer survivors. Methods: This randomized controlled trial was conducted at two clinics serving medically underserved populations. Breast cancer survivors (N = 62) were randomized to receive acupuncture (n = 31) or usual care (n = 31). The acupuncture group underwent 10 sessions over 5 weeks. Symptoms were assessed at baseline and Weeks 6 and 12. Results: The majority of participants (55%) were Black, mean age was 55.2 ± 9.3 years, and 62.9% had a household income below $55,000. Retention (90.3%), engagement (93.1%), and acceptability (92.8%) rates were high, demonstrating that integrating acupuncture into care for medically underserved breast cancer survivors is both feasible and acceptable. At Week 6, the acupuncture group showed significant reduction compared to the usual care group in pain, fatigue, sleep disturbance, depression, anxiety, and the symptom cluster score. All improvements persisted to Week 12 except for those in anxiety. Conclusions: Integrating acupuncture for symptom management in medically underserved breast cancer survivors is both feasible and acceptable. This approach offers potential benefits for reducing multiple symptoms and addressing health disparities.
1. Introduction
Breast cancer remains the most common cancer among women worldwide. An estimated 310,000 new cases of invasive breast cancer are expected to be diagnosed in the United States (U.S.) in 2024, contributing to the growing population of 4.1 million breast cancer survivors [1]. With advances in early detection and treatment, more women are surviving breast cancer. Long-term survivorship, however, often comes with a significant symptom burden [2,3]. Breast cancer survivors often experience a range of distressing symptoms, particularly during long-term endocrine therapy, which is commonly prescribed to reduce the risk of cancer recurrence [4,5]. A recent systematic review revealed that the most common symptoms breast cancer survivors report were joint pain (64%), hot flashes (75%), fatigue (80%), and sleep disturbance (50%) [6]. These symptoms can persist long after treatment ends [7], profoundly impacting breast cancer survivors’ quality of life (QOL) and ability to work [8,9]. Therefore, effective, individualized symptom management is crucial, especially during long-term endocrine therapy, as adherence to this therapy is essential for survival [4].
Acupuncture, a modality of Traditional Chinese Medicine, has emerged as a promising nonpharmacological intervention for managing multiple cancer-related symptoms [10]. Research has demonstrated its potential to reduce pain, improve sleep, reduce fatigue, and improve other cancer-related symptoms [11]. Medically underserved breast cancer survivors tend to have greater pain and greater mental health distress [12,13]. However, a review indicated that this population experiences disparities in the receipt of survivorship care plans and has substantial unmet needs with respect to their survivorship care [14]. They often face barriers to accessing comprehensive care and supportive therapies [15,16], including acupuncture. Financial constraints, cultural differences, lack of insurance coverage, and logistical challenges, such as transportation and clinic availability, often prevent medically underserved cancer survivors from benefiting fully from complementary and integrative health (CIH) therapies [17]. Expanding access to acupuncture for underserved populations is crucial to providing equitable care and addressing disparities in symptom management for breast cancer survivors [17].
In the United States, most acupuncture trials have been conducted in primarily non-Hispanic White populations, and acupuncture services are often concentrated in clinics that cater to more affluent or insured individuals [17]. To our knowledge, only a few studies have explored the integration of acupuncture into the care of patients from underserved communities, focusing mainly on chronic pain [18]. There is little research on its use for medically underserved breast cancer survivors. Addressing these gaps is critical, exploring the feasibility and acceptability of acupuncture in this population may offer a promising avenue for alleviating symptoms and improving well-being, while also informing strategies to enhance access and equity in survivorship care. In the present pilot study, the primary aim is to assess the feasibility and acceptability of integrating acupuncture for the treatment of multiple symptoms into clinics serving medically underserved breast cancer survivors. The secondary aim is to assess changes in symptom outcomes and compare these changes between the acupuncture group and the usual care group at Week 6 and Week 12.
2. Materials and Methods
2.1. Participants and Study Design
In this randomized controlled trial (RCT), early-stage breast cancer survivors were assigned to receive either a 5-week acupuncture treatment or usual care (control). Participants were recruited from the Mile Square Health Center (MSHC) Survivorship Clinic and the University of Illinois Hospital and Health Sciences (UI Health) Outpatient Care Center Oncology Clinic between January 2023 and August 2024. Both the UI Oncology Clinic and MSHC serve an underserved and diverse population. The MSHC is a federally qualified health center (FQHC), with most patients being racial and ethnic minority women and children who live at or below the poverty line and are publicly insured. This study was registered with Clinical Trials.gov (NCT05615753). Human subject approval was obtained from the University of Illinois Chicago’s Human Research Protection Office (IRB no. 2022-0353) [19]. This study was designed in accordance with the CONSORT 2010 Statement (Table S1) [20].
Eligible participants were women who (a) had histologically confirmed Stage 0, I, II, or III breast cancer; (b) were at least 18 years old; (c) had completed their primary cancer treatment (i.e., surgery, radiotherapy, chemotherapy) within 1 month prior to the start of the study and were currently being treated with endocrine therapy; (d) were able to speak and read English; and (e) self-reported experiencing pain, fatigue, sleep disturbance, depression, anxiety, and/or hot flashes in the last month. Specifically, eligible women had to report a minimum average severity rating of 3 or greater (0–10 numeric rating scale) for at least three of the six symptoms, and at least two of the symptoms had to be physical (pain, fatigue, or sleep disturbance). Participants were excluded if they (a) had metastatic breast cancer (Stage IV); (b) had a bleeding disorder (e.g., hemophilia, Von Willebrand disease, thrombocytopenia); (c) did not have time to attend the twice weekly acupuncture sessions for 5 consecutive weeks within the next few months; (d) had psychiatric or medical disorders that would affect study assessments such as dementia, Alzheimer’s disease, traumatic brain injury, stroke, or history of any neurological condition; or (e) were breastfeeding or pregnant or were planning on becoming pregnant during the study period.
2.2. Procedure
2.2.1. Recruitment
The research coordinator (RC) reviewed patients’ electronic health records (EHRs) to identify survivors who met the inclusion criteria. The RC then reached out to eligible breast cancer survivors via email and text message providing study information along with an attached flyer. Additionally, the RC informed providers when eligible survivors were scheduled for routine visits at the clinic. During these visits, providers introduced the eligible breast cancer survivors to the study using a recruitment script and the study flyer. Providers asked about survivors’ interest in participating or for permission for the RC to contact them.
2.2.2. Screening
The RC then contacted eligible survivors to provide further details about the study and conduct a more in-depth assessment to confirm their eligibility for participation The RC conducted screening interviews in the clinic waiting room or by phone with survivors who expressed an interest in participating, asking them to rate their level of pain, fatigue, sleep disturbance, depression, anxiety, and hot flashes over the past 1 month on a scale of 0–10. Those who met the eligibility criteria and agreed to participate were then asked to provide written informed consent and scheduled for the baseline (Week 0) study visit.
2.2.3. Data Collection
Participants completed all outcome assessments in REDCap [21], thus enabling a form of blinded outcomes assessment. At the baseline study visit (Week 0), the RC instructed participants on completing study questionnaires in REDCap [21] and asked them to complete the demographic and patient-reported outcomes questionnaires. Participants received email reminders to complete the study questionnaires for Weeks 6 and 12 through REDCap 2 days before the due dates. The RA checked for completed questionnaires on the due date and as needed, sent a second email reminder with a follow-up phone call to ensure that the questionnaires were completed within 3 days.
2.2.4. Randomization
After all the participants completed the baseline questionnaires in REDCap, they were randomly assigned 1:1, via REDCap’s randomization module. The allocation was stratified by age and baseline composite symptom score and followed a permuted block design.
2.3. Intervention
The acupuncture intervention involved 10 sessions delivered twice per week over a 5-week period, with at least one day separating each session. A semi-standardized protocol was used for all participants, which included (1) standardized acupuncture points aimed at managing symptoms such as pain, fatigue, sleep disturbances, depression, anxiety, and hot flashes; and (2) additional points customized to address up to three of the participant’s most painful areas (e.g., chest, fingers, shoulders, lower back, knees, hips, wrists, feet, or toes), which could be adjusted at each session. Needles were kept in place for 30 min and gently rotated before and after insertion. The acupuncture needles used were all 0.25 mm diameter x 40 mm length. Details of the acupuncture points are available in the published protocol [19]. The acupuncture intervention was conducted by three acupuncturists at the Acupuncture Research Lab of the University of Illinois Chicago College of Nursing near MSHC and UI Health.
2.4. Usual Care Group
Participants in the usual care group were given written educational resources on managing breast cancer symptoms and maintained their standard treatments (endocrine therapy) as prescribed. No additional interventions or acupuncture treatments were offered to these participants during the course of the study.
2.5. Measures
2.5.1. Demographic and Clinical Characteristics
Sociodemographic data (age, race, education, occupation, family income, household size, marital status) were collected at baseline through a questionnaire. Clinical information, such as disease stage and treatment types, was obtained from the EHR.
2.5.2. Symptoms
The PROMIS-29 (v1.0) is a 29-item, generic health assessment tool that measures multiple domains, including physical functioning, anxiety, depression, fatigue, sleep disturbance, and pain interference. Each domain comprises four items, and each item is rated on a 5-point Likert scale (from 1 to 5). It also contains an extra item to assess pain intensity, which respondents rank on a scale of 1 (“no pain”) to 10 (“worst imaginable pain”). The PROMIS-29 is a reliable measure of symptoms among cancer patients with good internal consistency and convergent validity (Cronbach’s alphas: 0.81–0.96) [22,23,24]. The PROMIS scores are reported on the T-score metric, which allows for comparison to population norms. In this scoring system, a T-score of 50 represents the mean for the general population, and each 10-point increment corresponds to one standard deviation. Higher scores reflect a greater degree of the construct or severity of the symptom being measured.
The hot flash composite score (HFCS) was calculated by multiplying the average daily frequency of hot flashes in the preceding week by the average severity rating [25]. Participants documented the frequency and intensity of hot flashes at baseline, Week 6, and Week 12 using the Daily Hot Flash Diary, rating severity on a scale from 1 (“mild”) to 4 (“very severe”). The HFCS has been established as a reliable and valid measure in previous acupuncture studies involving women with breast cancer [26].
Since the primary symptom outcome for this study is the symptom cluster, we calculated a symptom cluster composite score by averaging participants’ scores for pain, fatigue, sleep disturbance, depression, anxiety, and hot flashes.
2.5.3. Feasibility and Acceptability
Feasibility outcomes include the following:
- (a)
- Recruitment rate: calculated as the number of randomized women out of those we screened and contacted.
- (b)
- Retention rate: calculated as the number of women who completed baseline and follow-up assessments at week 6 and week 12 out of the total number of participants.
- (c)
- Engagement/adherence rate: calculated as the number of women who completed all 10 acupuncture sessions out of those randomized to the acupuncture group.
- (d)
- Fidelity: calculated as the number of times acupuncturists followed the treatment protocol and adhered to the standardized point selection guidelines.
The Protocol Acceptability Scale is a 9-item self-report measure that assesses study acceptability. It has exhibited stable test-retest reliability in prior studies [27,28]. Items are measured on a scale from 0 (negative response) to 2 (positive response), with total scores ranging from 0 to 18. Higher scores indicate greater levels of acceptability. We administered the scale to participants in the acupuncture group in Week 6 after acupuncture treatment. The study protocol was deemed to have high acceptability if 80% of participants reported a total score of ≥14.5.
To ensure the integrity and consistency of the acupuncture intervention, fidelity checks were conducted throughout the study. Fidelity was assessed across several key dimensions, including (1) adherence to the treatment protocol, (2) standardization of acupuncture point selection, and (3) consistency in session duration and frequency. Random unscheduled fidelity checks were performed approximately every 3 months. One of our investigators (J.S.) monitored the needle insertions for appropriate placement during training and fidelity checks.
2.6. Data Analysis
Demographic and clinical characteristics and symptom measures were summarized as mean (standard deviation) or count (percentage) for continuous and categorical variables, respectively. To make the HFCS comparable to the PROMIS measures, the HFCS was standardized to have a distribution of mean at 50 and standard deviation at 10, with a range from 0 to 100 (measurements that were −5 SD from the mean were set to be 0, and those 5 SD from the mean were set to be 100). Baseline comparisons between the acupuncture and control groups were conducted using the Wilcoxon rank sum test (Mann–Whitney U test) for numeric variables and Fisher’s exact test for categorical variables. Because our outcome measures were repeated measures over time, we assessed differences in changes from baseline to Week 6 and Week 12 using mixed-effect models [29]. Fixed-effect factors associated with the outcomes of interest included group assignment (acupuncture versus usual care group), time (treated as a categorical variable), and intervention × time interaction. Results are presented as between-group differences from baseline to Week 6 and Week 12 with 95% confidence intervals. The analyses were conducted using SAS 9.4 (SAS Institute, Cary, NC) [30]. All tests were two-sided, and p-values < 0.05 were considered significant.
For the feasibility testing, we aimed to detect recruitment, retention, completion, and acceptability rates using a 95% two-sided confidence interval. Assuming retention rates are within the desired range of 80% or higher, we require at least 62 breast cancer survivors to achieve a 95% confidence level (from 67.8% to 89.1%).
3. Results
3.1. Demographic and Clinical Characteristics
Sixty-two patients were randomly assigned to the acupuncture intervention (n = 31) and usual care (n = 31) groups (Figure 1). Table 1 summarizes the participants’ demographic and clinical characteristics at Week 0. Participants had an average age of 55.2 ± 9.3 years and a BMI of 31.6 kg/m2; the majority had attained at least a bachelor’s degree (51.5%) and had a household income of less than $55,000 (62.9%). The study population was diverse, with the majority (54.8%) identifying as Black or African American. All participants were diagnosed with early-stage breast cancer, with nearly half (46.8%) classified as Stage 1. All participants were receiving endocrine therapy; drug type varied, with the greatest number (35.5%) taking anastrozole. The top three pain sites were the hand joints (62.9%), the knee joints (61.3%), and the lower back (51.6%). Nearly one-third of participants (32.3%) reported antidepressant use. The most common comorbidity was high blood pressure (50.0%). There were no differences between groups on demographic or clinical characteristics at baseline.
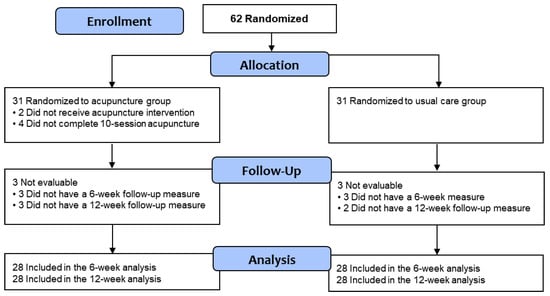
Figure 1.
CONSORT flow diagram.

Table 1.
Baseline demographic and clinical characteristics.
3.2. Feasibility
3.2.1. Recruitment and Retention
We contacted and screened 300 potential participants. Among them, 62 women were interested in participating and provided informed consent. After consent and randomization, two participants dropped out because of lack of time and illness of family members.
A total of 58 participants (93.5%) completed the Week 6 assessment, and 56 (90.3%) completed the Week 12 assessment (Figure 1). The study attrition rate was 9.7%, which was less than our target of 20%.
3.2.2. Engagement
Most participants in the acupuncture group (93.1%) completed all 10 sessions of their acupuncture treatment plan. For the four participants who missed acupuncture sessions, the primary reasons included pain, shoulder problems, illness or hospitalization, and scheduling conflicts with other appointments. These barriers highlight the health and logistical challenges breast cancer survivors face.
3.2.3. Fidelity
All three acupuncturists followed the treatment protocol and adhered to the standardized point selection guidelines. Deviations in session frequency or duration were documented after each session to maintain accuracy in data collection and intervention delivery.
3.3. Acceptability and Survivor Treatment Satisfaction
Table 2 shows the feasibility and acceptability responses. Among those who completed the Protocol Acceptability Scale for Treating Psychoneurological Symptoms with Acupuncture (n = 27), the mean acceptability score was 16.6 ± 1.4, with 92.8% of respondents rating it as acceptable (score > 14.5). This result met our criterion of an acceptability rate of 80% or more.

Table 2.
Feasibility and acceptability responses.
The satisfaction assessment survey was completed by 27 of the 31 participants who received acupuncture. All expressed that they liked acupuncture, with 63% being very satisfied with their treatment and 29.6% satisfied. Additionally, 66.7% strongly agreed that the acupuncture intervention was beneficial and worth their time. Half of the participants (50%) strongly agreed, and 23.1% agreed that acupuncture helped them manage their cancer-related symptoms.
3.4. Symptom Outcomes
There were no significant differences in the severity of pain interference, fatigue, sleep disturbance, depression, anxiety, or hot flashes between the two groups at baseline (Table 3). As shown in Table 4, compared to participants receiving usual care, participants who received acupuncture treatment had significantly greater reductions in pain, fatigue, sleep disturbance, and depression as well as in the composite score of six symptoms at both Week 6 and Week 12. Anxiety was significantly reduced in the acupuncture group compared to the control group at Week 6 only. There were no significant differences in the reduction in hot flashes between the two groups at either time point.

Table 3.
Baseline symptom severity (Week 0): comparison between the two groups.

Table 4.
Changes in symptom severity from baseline to Week 6 and Week 12: Comparison between the two groups.
4. Discussion
This study evaluated the feasibility and acceptability of a 5-week acupuncture intervention for the treatment of multiple cancer-related symptoms in medically underserved breast cancer survivors during endocrine therapy. This study is important because most prior acupuncture trials have focused on predominantly White populations, leaving a gap in knowledge of the feasibility and acceptability of this intervention among diverse and underserved groups. Participants in the acupuncture group showed significant reductions in the symptom cluster and multiple symptoms, including pain interference, fatigue, sleep disturbances, depression, and anxiety compared to those receiving usual care.
We found that the integration of acupuncture into clinics caring for medically underserved breast cancer survivors is both feasible and acceptable. The high recruitment, retention, engagement, and satisfaction rates for this study suggest there is demand for acupuncture treatment among this population. Many medically underserved breast cancer survivors voluntarily asked to participate in the study to receive acupuncture treatment. Successful recruitment is highly attributed to the referrals from oncologists, who play a pivotal role in bridging the gap between patients and CIH therapies. This emphasizes the importance of integrating oncologist referrals into recruitment strategies for future implementation studies, particularly those focusing on underserved populations. Additionally, the willingness of participants to join the study and their adherence to the treatment underscores the unmet need for acupuncture to address multiple treatment-related symptoms often experienced by breast cancer survivors. When barriers such as cost and availability are mitigated, patients are likely to engage with and benefit from acupuncture, highlighting the importance of improving access to acupuncture in medically underserved breast cancer survivors.
Several challenges encountered during the implementation of this project may offer valuable insights for future research efforts. Black women are more likely than non-Black women to be diagnosed with triple-negative breast cancer, which does not require endocrine therapy. During screening, we noticed that many breast cancer survivors who were never prescribed endocrine therapy also reported experiencing multiple symptoms (e.g., pain, fatigue, hot flashes). Future studies should broaden the inclusion criteria to extend beyond breast cancer survivors receiving endocrine therapy. Expanding the scope to include a more diverse population of breast cancer survivors will provide a more comprehensive understanding of symptom management needs across different subgroups, allowing for more inclusive and tailored interventions.
A barrier to providing acupuncture in medically underserved populations is the lack of insurance reimbursement. Our study offered free acupuncture and successfully demonstrated the feasibility of delivering care through this model. Many participants expressed a strong desire to continue receiving acupuncture after completing the study, but the out-of-pocket cost and lack of insurance reimbursement were significant barriers. To address this challenge, we have explored and will continue to pursue, various strategies to make acupuncture more affordable and accessible. In April 2023, Illinois Medicaid began covering acupuncture for chronic low back pain and breech presentation [31]. Findings from the present study provide evidence that can be used to support expanding acupuncture coverage for medically underserved breast cancer survivors. More equitable access to healthcare is needed to improve treatment options for this population.
In addition, participants in the acupuncture group showed significant reductions in multiple symptoms, including pain interference, fatigue, sleep disturbances, depression, and anxiety compared to those receiving usual care. Notably, most of these symptom improvements persisted for up to 6 weeks post-intervention, except for anxiety. Published estimates for the Minimally Important Change (MIC) for PROMIS measures do vary widely depending on the specific domain and population studied. A systematic review of MIC estimates for PROMIS measures suggests a range of 2 to 6 T-score points for a MIC [32]. In our study, most of the symptoms exhibited a clinically significant change after acupuncture based on the MIC estimates for PROMIS. In this study, acupuncture appeared to have no significant effects on hot flashes. Findings are partially consistent with previous meta-analyses [11,33,34] reporting that acupuncture significantly reduced pain, fatigue, sleep disturbances, and hot flashes compared to usual care in patients with breast cancer. One possible explanation for the inconsistent results regarding anxiety and hot flashes is our inclusion criteria: to be eligible for participation, women had to present with at least three out of six symptoms, and at least two had to be physical symptoms (such as pain, fatigue, or sleep disturbance). Consequently, some participants may not have experienced moderate or severe hot flashes or anxiety at baseline, which could have affected our ability to detect the effects of acupuncture on these two symptoms.
Our study has some limitations. First, we recruited breast cancer survivors from two clinics that primarily serve medically underserved populations in Chicago. Randomization was not stratified by clinics to control potential confounding factors. Future studies should consider stratified randomization by clinics to better control for potential confounders. Second, it is important to note that we did not include Spanish-speaking breast cancer survivors. Findings may thus not be fully representative of the broader population of medically underserved breast cancer survivors, particularly those from different linguistic, cultural, or ethnic groups. Results, therefore, may not be generalizable to other health systems or patient populations with different demographic characteristics or language needs. Future research should include multiple sites across various settings and patient populations to improve the generalizability of the findings. Third, participants with an interest in acupuncture were more likely to join and adhere, resulting in non-random attrition. This introduces selection bias and limits the generalizability of findings to the broader population of medically underserved breast cancer survivors. Future studies should consider conducting drop-out analyses to assess whether attrition is non-random. Another limitation is the usual care group did not receive special attention. Future studies should include an attention-controlled group to have 10 equally long visits without acupuncture to control for the potential effects of attention and psychosocial support. Also, long-term follow-ups in clinical studies can be challenging, and in this study, the 12-week follow-up did not completely account for potential changes in medical treatment, such as increased analgesic use, which could have influenced symptom assessments, particularly for pain. Lastly, the intervention was delivered in a nearby integrative clinic. To improve convenience and accessibility for patients, future studies should explore the feasibility of delivering acupuncture treatment within the oncology clinic or an FQHC and integrating acupuncture services into the care plan of underserved breast cancer survivors. This shift could enhance the integration of acupuncture into conventional care settings, allowing for better coordination among healthcare providers and more streamlined access for patients.
5. Conclusions
Our findings suggest that integrating acupuncture into care to manage multiple cancer-related symptoms is feasible and acceptable in outpatient clinics serving medically underserved breast cancer survivors. To further validate these results and assess their applicability across different settings and survivor populations, including non-English-speaking populations, a multi-site implementation trial is needed. Such a trial would provide a more comprehensive understanding of acupuncture’s efficacy in managing common symptoms reported by breast cancer survivors across diverse health systems and patient populations in the U.S.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/cancers17020304/s1, Table S1: CONSORT checklist.
Author Contributions
Conceptualization, H.L., A.Z.D., J.M.S., and C.L.P.; methodology, H.L., A.Z.D., J.M.S., and Z.C.; data curation, S.G. and N.L.; formal analysis, Z.C. and W.M.; writing—original draft, H.L. and H.C.; writing—review and editing, H.L., A.Z.D., J.M.S., S.G., N.L., and O.D. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the National Center for Complementary and Integrative Health (R34 AT012084 and K24 AT011995-01).
Institutional Review Board Statement
This study was approved by the University of Illinois Chicago Human Research Protection Office (2022–0353) on 27 October 2022.
Informed Consent Statement
All breast cancer survivors who participated in the study provided written informed consent for the use of their data for research purposes.
Data Availability Statement
Full trial protocol can be accessed at https://doi.org/10.1016/j.cct.2023.107387 (accessed on 17 December 2024). Participants’ survey data are available upon request to interested researchers.
Acknowledgments
The authors sincerely appreciate the time and valuable insights shared by all those who participated in and contributed to the study and thank Marnie Wiss for editing this manuscript.
Conflicts of Interest
The authors have no conflicts of interest to disclose.
References
- Tonorezos, E.; Devasia, T.; Mariotto, A.B.; Mollica, M.A.; Gallicchio, L.; Green, P.; Doose, M.; Brick, R.; Streck, B.; Reed, C.; et al. Prevalence of cancer survivors in the United States. JNCI J. Natl. Cancer Inst. 2024, 116, 1784–1790. [Google Scholar] [CrossRef]
- Mandelblatt, J.S.; Zhai, W.; Ahn, J.; Small, B.J.; Ahles, T.A.; Carroll, J.E.; Denduluri, N.; Dilawari, A.; Extermann, M.; Graham, D.; et al. Symptom burden among older breast cancer survivors: The Thinking and Living With Cancer (TLC) study. Cancer 2020, 126, 1183–1192. [Google Scholar] [CrossRef]
- Whisenant, M.S.; Williams, L.A.; Mendoza, T.; Cleeland, C.; Chen, T.H.; Fisch, M.J.; Shi, Q. Identification of Breast Cancer Survivors With High Symptom Burden. Cancer Nurs. 2022, 45, 253–261. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Lu, Z.; Qiu, J.; Luo, H.; Tang, L.; Li, Y.; Li, P. Symptom experience in endocrine therapy for breast cancer patients: A qualitative systematic review and meta-synthesis. Asia-Pac. J. Oncol. Nurs. 2023, 11, 100364. [Google Scholar] [CrossRef]
- Eliassen, F.M.; Blåfjelldal, V.; Helland, T.; Hjorth, C.F.; Hølland, K.; Lode, L.; Bertelsen, B.-E.; Janssen, E.A.M.; Mellgren, G.; Kvaløy, J.T.; et al. Importance of endocrine treatment adherence and persistence in breast cancer survivorship: A systematic review. BMC Cancer 2023, 23, 625. [Google Scholar] [CrossRef] [PubMed]
- Elshafie, S.; Trivedi, R.; Villa-Zapata, L.A.; Tackett, R.L.; Zaghloul, I.Y.; Young, H.N. Adherence, clinical benefits, and adverse effects of endocrine therapies among women with nonmetastatic breast cancer in developing countries: A systematic review and meta-analysis. Cancer 2024, 131, e35550. [Google Scholar] [CrossRef] [PubMed]
- Carmen, A.; Anne, O.; Monika, S.; Daniel, E.; Johannes, G.; Verena, M.; Michael, H.; Christine, B. Does the toxicity of endocrine therapy persist into long-term survivorship?: Patient-reported outcome results from a follow-up study beyond a 10-year-survival. Breast Cancer Res. Treat. 2023, 198, 475–485. [Google Scholar] [CrossRef]
- Alnaim, L. Health-Related Quality of Life in Women With Breast Cancer Undergoing Treatment With Hormonal Therapy–A Review Study. Eur. J. Breast Health 2022, 18, 292. [Google Scholar] [CrossRef] [PubMed]
- Bjerkeset, E.; Röhrl, K.; Schou-Bredal, I. Symptom cluster of pain, fatigue, and psychological distress in breast cancer survivors: Prevalence and characteristics. Breast Cancer Res. Treat. 2020, 180, 63–71. [Google Scholar] [CrossRef] [PubMed]
- Mao, J.J.; Ismaila, N.; Bao, T.; Barton, D.; Ben-Arye, E.; Garland, E.L.; Greenlee, H.; Leblanc, T.; Lee, R.T.; Lopez, A.M. Integrative medicine for pain management in oncology: Society for integrative oncology–ASCO guideline. J. Clin. Oncol. 2022, 40, 3998–4024. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Schlaeger, J.M.; Jang, M.K.; Lin, Y.; Park, C.; Liu, T.; Sun, M.; Doorenbos, A.Z. Acupuncture improves multiple treatment-related symptoms in breast cancer survivors: A systematic review and meta-analysis. J. Altern. Complement. Med. 2021, 27, 1084–1097. [Google Scholar] [CrossRef]
- Vallerand, A.H.; Hasenau, S.; Templin, T.; Collins-Bohler, D. Disparities between black and white patients with cancer pain: The effect of perception of control over pain. Pain Med. 2005, 6, 242–250. [Google Scholar] [CrossRef] [PubMed]
- Alcalá, H.E. Differential mental health impact of cancer across racial/ethnic groups: Findings from a population-based study in California. BMC Public Health 2014, 14, 930. [Google Scholar] [CrossRef] [PubMed]
- Tarver, W.L.; Justice, Z.; Jonnalagadda, P.; Rahurkar, S.; Obeng-Gyasi, S.; Krok-Schoen, J.L.; Petrecca, A.; Paskett, E.D. A scoping review of the evidence on survivorship care plans among minority, rural, and low-income populations. J. Cancer Surviv. 2024, 14, 930. [Google Scholar] [CrossRef] [PubMed]
- Caraballo, C.; Ndumele, C.D.; Roy, B.; Lu, Y.; Riley, C.; Herrin, J.; Krumholz, H.M. Trends in racial and ethnic disparities in barriers to timely medical care among adults in the US, 1999 to 2018. JAMA Health Forum 2022, 3, e223856. [Google Scholar] [CrossRef] [PubMed]
- Tangkiatkumjai, M.; Boardman, H.; Walker, D.-M. Potential factors that influence usage of complementary and alternative medicine worldwide: A systematic review. BMC Complement. Med. Ther. 2020, 20, 363. [Google Scholar] [CrossRef] [PubMed]
- Miller, D.W.; Roseen, E.J.; Stone, J.A.M.; Gardiner, P.; Olson, J.; Rosen, S.; Wayne, P.; Davis, R.; Coeytaux, R. Incorporating Acupuncture Into American Healthcare: Initiating a Discussion on Implementation Science, the Status of the Field, and Stakeholder Considerations. Glob. Adv. Health Med. 2021, 10, 21649561211042574. [Google Scholar] [CrossRef] [PubMed]
- Teets, R.; Nielsen, A.; Moonaz, S.; Anderson, B.J.; Mah, D.M.; Walter, E.; Milanes, M.; Jyung, H.; Soto Cossio, L.E.; Meissner, P. Group acupuncture therapy with yoga therapy for chronic neck, low back, and osteoarthritis pain in safety net settings for an underserved population: A feasibility pilot study. Glob. Adv. Integr. Med. Health 2023, 12, 27536130231202515. [Google Scholar] [CrossRef]
- Li, H.; Schlaeger, J.M.; Patil, C.L.; Danciu, O.; Chen, Z.; Lif, N.; Gao, S.; Doorenbos, A.Z. Feasibility of implementing acupuncture in medically underserved breast cancer survivors (FAB): A protocol. Contemp. Clin. Trials 2024, 136, 107387. [Google Scholar] [CrossRef]
- Schulz, K.F.; Altman, D.G.; Moher, D. CONSORT 2010 Statement: Updated guidelines for reporting parallel group randomised trials. BMJ 2010, 340, c332. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef] [PubMed]
- Deyo, R.A.; Ramsey, K.; Buckley, D.I.; Michaels, L.; Kobus, A.; Eckstrom, E.; Forro, V.; Morris, C. Performance of a Patient Reported Outcomes Measurement Information System (PROMIS) Short Form in Older Adults with Chronic Musculoskeletal Pain. Pain Med. 2015, 17, 314–324. [Google Scholar] [CrossRef] [PubMed]
- Kang, D.; Kim, Y.; Lim, J.; Yoon, J.; Kim, S.; Kang, E.; Nam, H.; Shim, S.; Lee, M.; Bok, H.; et al. Validation of the Korean Version of the Patient-Reported Outcomes Measurement Information System 29 Profile V2.1 among Cancer Survivors. Cancer Res. Treat. 2022, 54, 10–19. [Google Scholar] [CrossRef]
- Cella, D.; Choi, S.W.; Condon, D.M.; Schalet, B.; Hays, R.D.; Rothrock, N.E.; Yount, S.; Cook, K.F.; Gershon, R.C.; Amtmann, D.; et al. PROMIS(®) Adult Health Profiles: Efficient Short-Form Measures of Seven Health Domains. Value Health 2019, 22, 537–544. [Google Scholar] [CrossRef] [PubMed]
- Sloan, J.A.; Loprinzi, C.L.; Novotny, P.J.; Barton, D.L.; Lavasseur, B.I.; Windschitl, H. Methodologic Lessons Learned From Hot Flash Studies. J. Clin. Oncol. 2001, 19, 4280–4290. [Google Scholar] [CrossRef] [PubMed]
- Mao, J.J.; Bowman, M.A.; Xie, S.X.; Bruner, D.; DeMichele, A.; Farrar, J.T. Electroacupuncture versus gabapentin for hot flashes among breast cancer survivors: A randomized placebo-controlled trial. J. Clin. Oncol. 2015, 33, 3615. [Google Scholar] [CrossRef] [PubMed]
- Wilkie, D.J.; Huang, H.-Y.; Berry, D.L.; Schwartz, A.; Lin, Y.-C.; Ko, N.-Y.; Chen, A.; Gralow, J.; Lindsley, S.K.; Fitzgibbon, D. Cancer symptom control: Feasibility of a tailored, interactive computerized program for patients. Fam. Community Health 2001, 24, 48–62. [Google Scholar] [CrossRef] [PubMed]
- Wilkie, D.J.; Judge, M.K.M.; Berry, D.L.; Dell, J.; Zong, S.; Gilespie, R. Usability of a computerized PAINReportIt in the general public with pain and people with cancer pain. J. Pain Symptom Manag. 2003, 25, 213–224. [Google Scholar] [CrossRef] [PubMed]
- Laird, N.M.; Ware, J.H. Random-effects models for longitudinal data. Biometrics 1982, 38, 963–974. [Google Scholar] [CrossRef] [PubMed]
- SAS Institute. SAS Certified Professional Prep Guide: Advanced Programming Using SAS 9.4; SAS institute: Cary, NC, USA, 2019. [Google Scholar]
- Illinois Department of Healthcare and Family Services. Provider Notice: Fee-for-Service Claims—October 2023 Pricer Updates. Available online: https://hfs.illinois.gov/medicalproviders/notices/notice.prn231018a.html (accessed on 18 October 2023).
- Terwee, C.B.; Peipert, J.D.; Chapman, R.; Lai, J.S.; Terluin, B.; Cella, D.; Griffiths, P.; Mokkink, L.B. Minimal important change (MIC): A conceptual clarification and systematic review of MIC estimates of PROMIS measures. Qual. Life Res. 2021, 30, 2729–2754. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Sun, Y.; Li, D.; Liu, X.; Fang, C.; Yang, C.; Luo, T.; Lu, H.; Li, H.; Zhang, H. Acupuncture for breast cancer: A systematic review and meta-analysis of patient-reported outcomes. Front. Oncol. 2021, 11, 646315. [Google Scholar] [CrossRef] [PubMed]
- Choi, T.Y.; Ang, L.; Jun, J.H.; Alraek, T.; Birch, S.; Lu, W.; Lee, M.S. Acupuncture for Managing Cancer-Related Fatigue in Breast Cancer Patients: A Systematic Review and Meta-Analysis. Cancers 2022, 14, 4419. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).