A Triple Oral Combination of Bendamustine, Acalabrutinib, and Venetoclax Demonstrates Efficacy Against Mantle Cell Lymphoma In Vitro and In Vivo
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Cell Culture
2.2. Reagents
2.3. [3-(4,5-Dimethylthiazol-2-yl)-5-(3-carboxymethoxyphenyl)-2-(4-sulfophenyl)-2H-tetrazolium] (MTS) Assays
2.4. Annexin-PI Assays
2.5. In Vivo Tumor Models
2.6. Bioluminescence Imaging
2.7. Statistical Analysis
3. Results
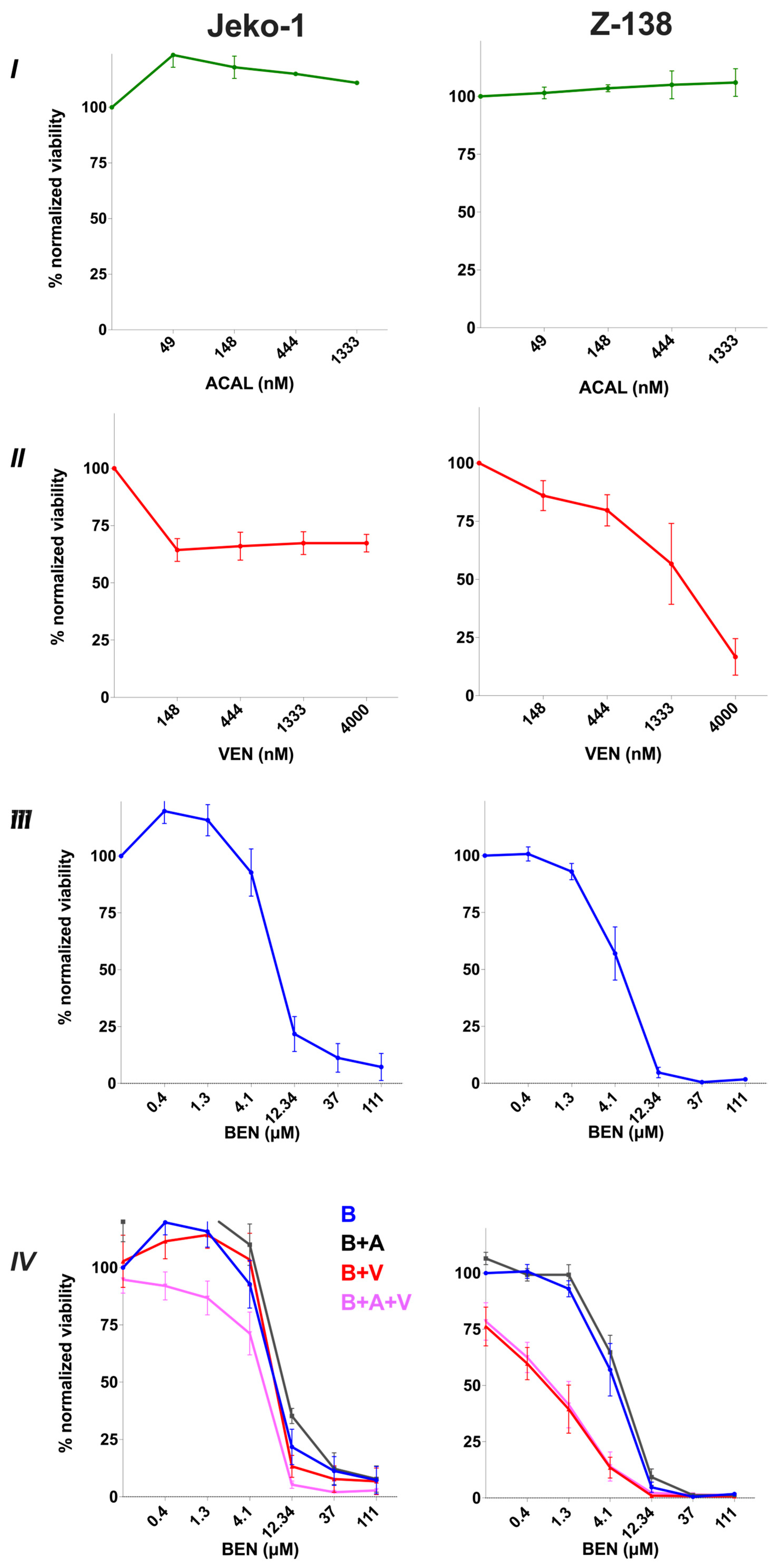
3.1. Sensitivity of MCL Cell Lines to Bendamustine, Venetoclax and Acalabrutinib Monotherapies and Combination Therapies In Vitro
3.2. Bendamustine Combined with Venetoclax +/− Acalabrutinib Increases Apoptosis and Cell Death
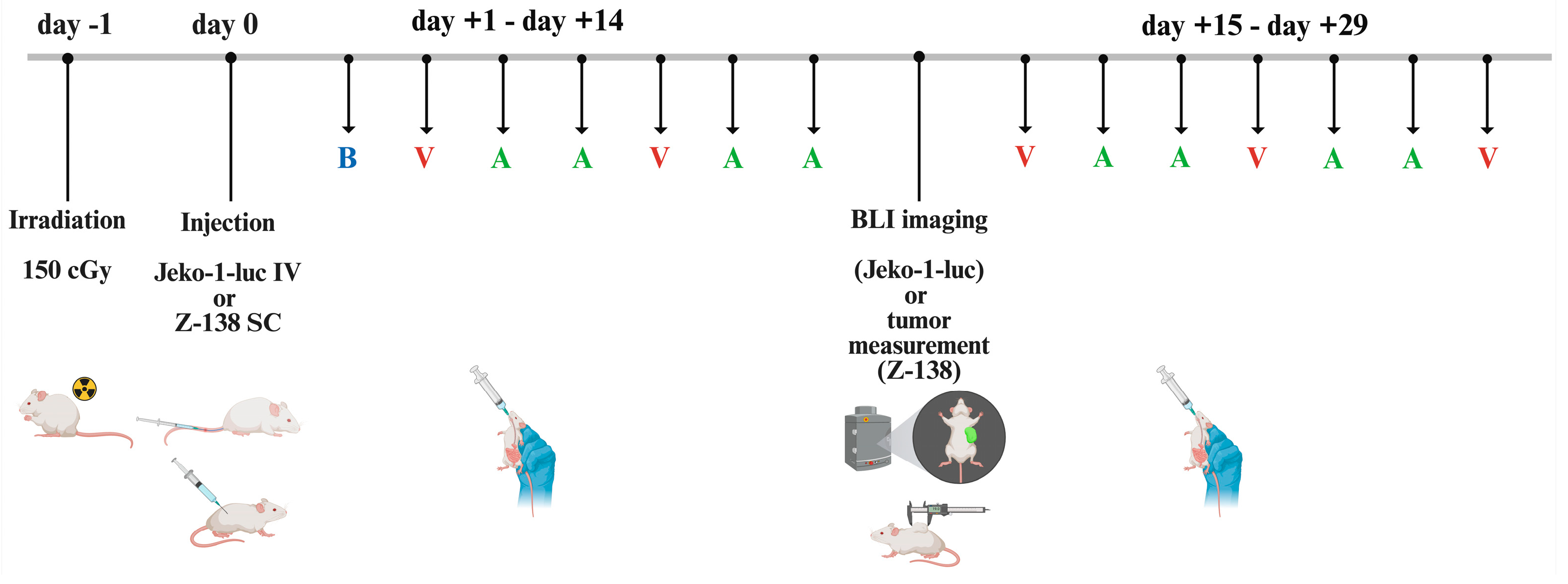
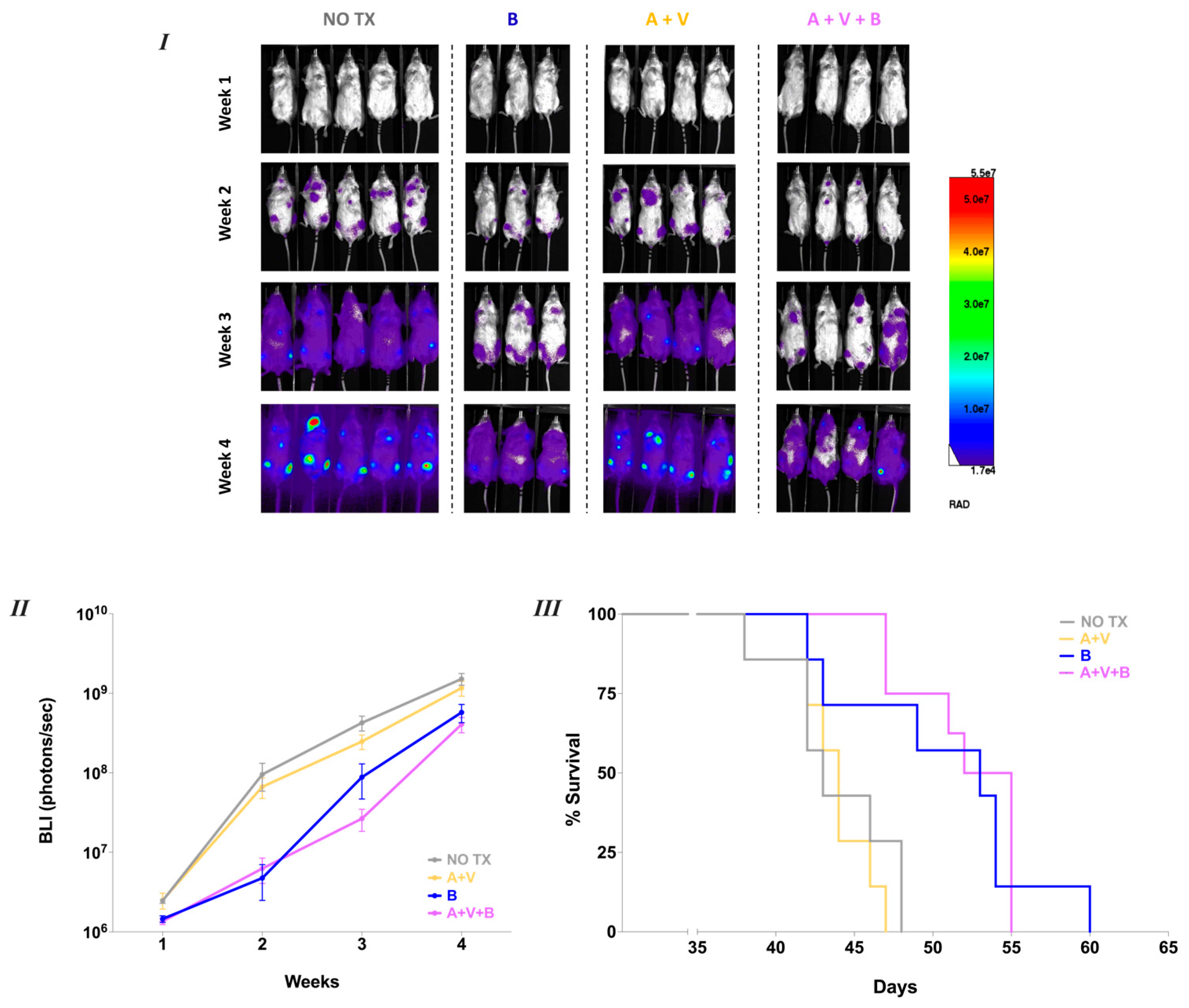
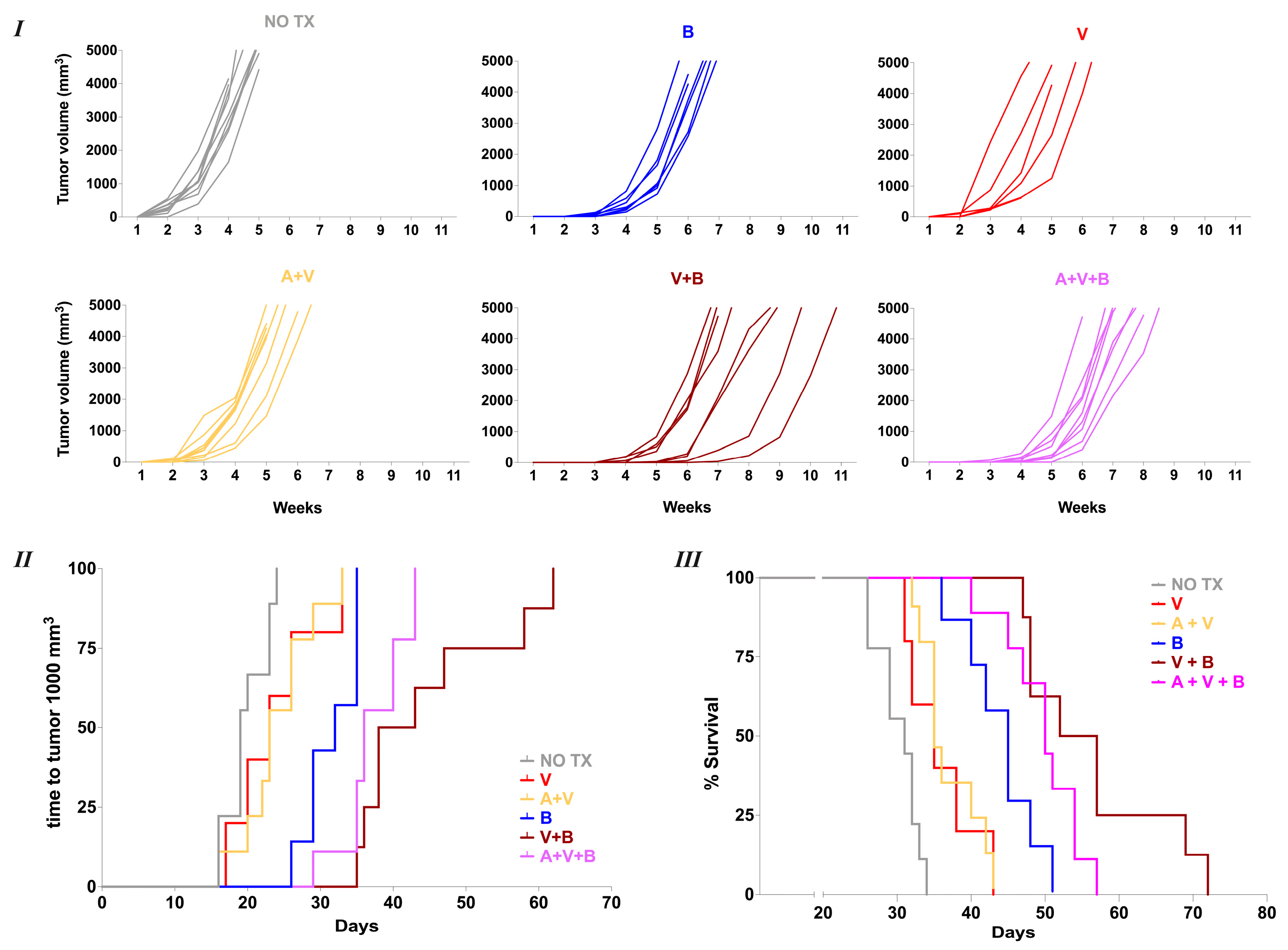
3.3. Oral Bendamustine Significantly Improves Survival in MCL-Bearing Mice Alone or in Combination with Venetoclax
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BEN | Bendamustine |
| ACAL | Acalabrutinib |
| VEN | Venetoclax |
| MCL | Mantle-cell lymphoma |
| R/R | Relapsed/Refractory |
| BTKi | Bruton’s tyrosine kinase inhibitor |
| RTX | Rituximab |
| Bcl-2 | B-cell lymphoma 2 |
| DMSO | Dimethylsulfoxide |
| IC50 | Half max inhibitory concentration |
| PI | Propidium iodide |
| Bcl-xL | B-cell lymphoma-extra large |
| MCL-1 | Myeloid cell leukemia 1 |
| Cmax | Maximum plasma concentration |
| IBR | Ibrutinib |
| OS | Overall survival |
| ORR | Overall response rate |
| PFS | Progression-free survival |
| CR | Complete Response |
| SEM | Standard error of the means |
| PBS | Phosphate buffer saline |
| ANOVA | Analysis of variance |
| BLI | Bioluminescence imaging |
| μM | Micromolar |
| nM | Nanomolar |
| IV | Intravenous |
| SC | Subcutaneous |
| PO | Per os |
| Cgy | Centigray |
| CIT | Chemoimmunotherapy |
| CI | Confidence interval |
| HEPES | 4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid |
| RPMI 1640 | Roswell Park Memorial Institute |
| PEG | Polyethylene glycol |
| NSG mice | (NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ) mice |
| Phosal50-PG | Phosphatidylcholine in propylene glycol, content ≥ 50.0% |
References
- Silkenstedt, E.; Dreyling, M. Mantle cell lymphoma-Update on molecular biology, prognostication and treatment approaches. Hematol. Oncol. 2023, 41 (Suppl. 1), 36–42. [Google Scholar] [CrossRef] [PubMed]
- Jain, P.; Wang, M.L. Mantle cell lymphoma in 2022-A comprehensive update on molecular pathogenesis, risk stratification, clinical approach, and current and novel treatments. Am. J. Hematol. 2022, 97, 638–656. [Google Scholar] [CrossRef] [PubMed]
- Lu, T.; Zhang, J.; McCracken, J.M.; Young, K.H. Recent advances in genomics and therapeutics in mantle cell lymphoma. Cancer Treat. Rev. 2024, 122, 102651. [Google Scholar] [CrossRef]
- Leoni, L.M.; Hartley, J.A. Mechanism of action: The unique pattern of bendamustine-induced cytotoxicity. Semin. Hematol. 2011, 48 (Suppl. 1), S12–S23. [Google Scholar] [CrossRef] [PubMed]
- Rummel, M.J.; Niederle, N.; Maschmeyer, G.; Banat, G.A.; von Grünhagen, U.; Losem, C.; Kofahl-Krause, D.; Heil, G.; Welslau, M.; Balser, C.; et al. Bendamustine plus rituximab versus CHOP plus rituximab as first-line treatment for patients with indolent and mantle-cell lymphomas: An open-label, multicentre, randomised, phase 3 non-inferiority trial. Lancet 2013, 381, 1203–1210. [Google Scholar] [CrossRef]
- Flinn, I.W.; Van Der Jagt, R.; Kahl, B.; Wood, P.; Hawkins, T.; MacDonald, D.; Simpson, D.; Kolibaba, K.; Issa, S.; Chang, J.; et al. First-Line Treatment of Patients with Indolent Non-Hodgkin Lymphoma or Mantle-Cell Lymphoma with Bendamustine Plus Rituximab Versus R-CHOP or R-CVP: Results of the BRIGHT 5-Year Follow-Up Study. J. Clin. Oncol. 2019, 37, 984–991. [Google Scholar] [CrossRef]
- Yi, J.H.; Kim, S.J.; Lee, J.O.; Lee, G.W.; Kwak, J.Y.; Eom, H.S.; Jo, J.C.; Choi, Y.S.; Oh, S.Y.; Kim, W.S. Bendamustine Plus Rituximab for Mantle Cell Lymphoma: A Korean, Multicenter Retrospective Analysis. Anticancer Res. 2022, 42, 6083–6089. [Google Scholar] [CrossRef]
- García-Noblejas, A.; Martínez Chamorro, C.; Navarro Matilla, B.; Da Silva Rodriguez, C.; González-Lopez, T.J.; Oña Navarrete, R.; Ramírez Sánchez, M.J.; Martínez Barranco, P.; Sánchez Blanco, J.J.; Nicolás, C.; et al. Bendamustine as salvage treatment for patients with relapsed or refractory mantle cell lymphoma patients: A retrospective study of the Spanish experience. Ann. Hematol. 2014, 93, 1551–1558. [Google Scholar] [CrossRef]
- Eyre, T.A.; Cheah, C.Y.; Wang, M.L. Therapeutic options for relapsed/refractory mantle cell lymphoma. Blood 2022, 139, 666–677. [Google Scholar] [CrossRef]
- Silkenstedt, E.; Dreyling, M. Treatment of Relapsed/Refractory MCL. Blood 2024, 145, 673–682. [Google Scholar] [CrossRef]
- Kumar, S.A.; Gao, J.; Patel, S.A. The shifting therapeutic paradigm for relapsed/refractory mantle cell lymphoma. Leuk. Res. 2023, 134, 107385. [Google Scholar] [CrossRef]
- Sharman, J.; Kabadi, S.M.; Clark, J.; Andorsky, D. Treatment patterns and outcomes among mantle cell lymphoma patients treated with ibrutinib in the United States: A retrospective electronic medical record database and chart review study. Br. J. Haematol. 2021, 192, 737–746. [Google Scholar] [CrossRef]
- Wu, J.; Zhang, M.; Liu, D. Acalabrutinib (ACP-196): A selective second-generation BTK inhibitor. J. Hematol. Oncol. 2016, 9, 21. [Google Scholar] [CrossRef]
- Wang, M.; Rule, S.; Zinzani, P.L.; Goy, A.; Casasnovas, O.; Smith, S.D.; Damaj, G.; Doorduijn, J.; Lamy, T.; Morschhauser, F.; et al. Acalabrutinib in relapsed or refractory mantle cell lymphoma (ACE-LY-004): A single-arm, multicentre, phase 2 trial. Lancet 2018, 391, 659–667. [Google Scholar] [CrossRef]
- Wang, M.; Rule, S.; Zinzani, P.L.; Goy, A.; Casasnovas, O.; Smith, S.D.; Damaj, G.; Doorduijn, J.K.; Lamy, T.; Morschhauser, F.; et al. Durable response with single agent acalabrutinib in patients with relapsed or refractory mantle cell lymphoma. Leukemia 2019, 33, 2762–2766. [Google Scholar] [CrossRef]
- Le Gouill, S.; Długosz-Danecka, M.; Rule, S.; Zinzani, P.L.; Goy, A.; Smith, S.D.; Doorduijn, J.K.; Panizo, C.; Shah, B.D.; Davies, A.J.; et al. Final results and overall survival data from a phase II study of acalabrutinib monotherapy in patients with relapsed/refractory mantle cell lymphoma, including those with poor prognostic factors. Haematologica 2024, 109, 343–350. [Google Scholar] [CrossRef]
- Wang, M.; Salek, D.; Belada, D.; Song, Y.; Jurczak, W.; Kahl, B.S.; Paludo, J.; Chu, M.P.; Kryachok, I.; Fogliatto, L.; et al. Acalabrutinib Plus Bendamustine-Rituximab in Untreated Mantle Cell Lymphoma. J. Clin. Oncol. 2025. ahead of print. [Google Scholar] [CrossRef]
- Adams, J.M.; Cory, S. The BCL-2 arbiters of apoptosis and their growing role as cancer targets. Cell Death Differ. 2018, 25, 27–36. [Google Scholar] [CrossRef]
- Davids, M.S.; Roberts, A.W.; Seymour, J.F.; Pagel, J.M.; Kahl, B.S.; Wierda, W.G.; Puvvada, S.; Kipps, T.J.; Anderson, M.A.; Salem, A.H.; et al. Phase I First-in-Human Study of Venetoclax in Patients with Relapsed or Refractory Non-Hodgkin Lymphoma. J. Clin. Oncol. 2017, 35, 826–833. [Google Scholar] [CrossRef]
- Jiang, H.; Lwin, T.; Zhao, X.; Ren, Y.; Li, G.; Moscinski, L.; Shah, B.; Tao, J. Venetoclax as a single agent and in combination with PI3K-MTOR1/2 kinase inhibitors against ibrutinib sensitive and resistant mantle cell lymphoma. Br. J. Haematol. 2019, 184, 298–302. [Google Scholar] [CrossRef]
- Tam, C.S.; Anderson, M.A.; Pott, C.; Agarwal, R.; Handunnetti, S.; Hicks, R.J.; Burbury, K.; Turner, G.; Di Iulio, J.; Bressel, M.; et al. Ibrutinib plus Venetoclax for the Treatment of Mantle-Cell Lymphoma. N. Engl. J. Med. 2018, 378, 1211–1223. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Robak, T.; Maddocks, K.J.; Phillips, T.; Smith, S.D.; Gallinson, D.; Calvo, R.; Wun, C.C.; Munugalavadla, V.; Jurczak, W. Acalabrutinib plus venetoclax and rituximab in treatment-naive mantle cell lymphoma: 2-year safety and efficacy analysis. Blood Adv. 2024, 8, 4539–4548. [Google Scholar] [CrossRef] [PubMed]
- Kim, A.I.; Armand, P.; Ryan, C.E.; Redd, R.A.; Forsyth, M.; Mai, J.; Pazienza, S.; Bresnahan, C.; Kats, V.M.; Abdulkarim, S.; et al. Preliminary Efficacy and Safety of a Phase 1/2 Study of Acalabrutinib, Venetoclax, and Obinutuzumab in Patients with Relapsed/Refractory and Previously Untreated Mantle Cell Lymphoma (MAVO). Blood 2024, 144 (Suppl. 1), 4408. [Google Scholar] [CrossRef]
- Grieve, C.; Joseph, A.; Drullinsky, P.; Zelenetz, A.D.; Hamlin, P.; Kumar, A. Phase I study of bendamustine, rituximab, ibrutinib, and venetoclax in relapsed, refractory mantle cell lymphoma. Leuk. Lymphoma 2024, 65, 235–241. [Google Scholar] [CrossRef]
- Ryan, C.E.; Armand, P.; LaCasce, A.S. Frontline management of mantle cell lymphoma. Blood 2025, 145, 663–672. [Google Scholar] [CrossRef]
- Liewer, S.; Huddleston, A.N. Oral targeted therapies: Managing drug interactions, enhancing adherence and optimizing medication safety in lymphoma patients. Expert Rev. Anticancer Ther. 2015, 15, 453–464. [Google Scholar] [CrossRef]
- Cracchiolo, M.J.; Davis, L.; Matiatos, A.P.; Davini, D.W.; Husnain, M.; Simpson, R.J.; Voudouris, V.; Katsanis, E. Comparable efficacy of oral bendamustine versus intravenous administration in treating hematologic malignancies. Cancer Chemother. Pharmacol. 2024, 94, 361–372. [Google Scholar] [CrossRef]
- Yao, T.; Ding, J.; Sharma, S.; Li, Y.; Xu, Q.; Ma, P. Assessment of ethnic differences in pharmacokinetics and clinical responses of acalabrutinib between Chinese and White patients with B-cell malignancies. Br. J. Clin. Pharmacol. 2025, 1–12. [Google Scholar] [CrossRef]
- Owen, J.S.; Melhem, M.; Passarell, J.A.; D’Andrea, D.; Darwish, M.; Kahl, B. Bendamustine pharmacokinetic profile and exposure-response relationships in patients with indolent non-Hodgkin’s lymphoma. Cancer Chemother. Pharmacol. 2010, 66, 1039–1049. [Google Scholar] [CrossRef]
- Yang, X.; Mei, C.; He, X.; He, L.; Lu, X.; Tong, H.; Lou, Y. Quantification of Venetoclax for Therapeutic Drug Monitoring in Chinese Acute Myeloid Leukemia Patients by a Validated UPLC-MS/MS Method. Molecules 2022, 27, 1607. [Google Scholar] [CrossRef]
- Byrd, J.C.; Harrington, B.; O’Brien, S.; Jones, J.A.; Schuh, A.; Devereux, S.; Chaves, J.; Wierda, W.G.; Awan, F.T.; Brown, J.R.; et al. Acalabrutinib (ACP-196) in Relapsed Chronic Lymphocytic Leukemia. N. Engl. J. Med. 2016, 374, 323–332. [Google Scholar] [CrossRef] [PubMed]
- Salem, A.H.; Menon, R.M. Clinical pharmacokinetics and pharmacodynamics of venetoclax, a selective B-cell lymphoma-2 inhibitor. Clin. Transl. Sci. 2024, 17, e13807. [Google Scholar] [CrossRef] [PubMed]
- Lalic, H.; Aurer, I.; Batinic, D.; Visnjic, D.; Smoljo, T.; Babic, A. Bendamustine: A review of pharmacology, clinical use and immunological effects (Review). Oncol. Rep. 2022, 47, 114. [Google Scholar] [CrossRef] [PubMed]
- Telford, C.; Kabadi, S.M.; Abhyankar, S.; Song, J.; Signorovitch, J.; Zhao, J.; Yao, Z. Matching-adjusted Indirect Comparisons of the Efficacy and Safety of Acalabrutinib Versus Other Targeted Therapies in Relapsed/Refractory Mantle Cell Lymphoma. Clin. Ther. 2019, 41, 2357–2379. [Google Scholar] [CrossRef]
- Nakhoda, S.; Vistarop, A.; Wang, Y.L. Resistance to Bruton tyrosine kinase inhibition in chronic lymphocytic leukaemia and non-Hodgkin lymphoma. Br. J. Haematol. 2023, 200, 137–149. [Google Scholar] [CrossRef]
- Zhao, X.; Lwin, T.; Silva, A.; Shah, B.; Tao, J.; Fang, B.; Zhang, L.; Fu, K.; Bi, C.; Li, J.; et al. Unification of de novo and acquired ibrutinib resistance in mantle cell lymphoma. Nat. Commun. 2017, 8, 14920. [Google Scholar] [CrossRef]
- Stephens, D.M.; Byrd, J.C. Resistance to Bruton tyrosine kinase inhibitors: The Achilles heel of their success story in lymphoid malignancies. Blood 2021, 138, 1099–1109. [Google Scholar] [CrossRef]
- Liu, Z.; Liu, J.; Zhang, T.; Li, L.; Zhang, S.; Jia, H.; Xia, Y.; Shi, M.; Zhang, J.; Yue, S.; et al. Distinct BTK inhibitors differentially induce apoptosis but similarly suppress chemotaxis and lipid accumulation in mantle cell lymphoma. BMC Cancer 2021, 21, 732. [Google Scholar] [CrossRef]
- Lantermans, H.C.; Ma, F.; Kuil, A.; van Kesteren, S.; Yasinoglu, S.; Yang, G.; Buhrlage, S.J.; Wang, J.; Gray, N.S.; Kersten, M.J.; et al. The dual HCK/BTK inhibitor KIN-8194 impairs growth and integrin-mediated adhesion of BTKi-resistant mantle cell lymphoma. Leukemia 2024, 38, 1570–1580. [Google Scholar] [CrossRef]
- Medeiros, L.J.; Estrov, Z.; Rassidakis, G.Z. Z-138 cell line was derived from a patient with blastoid variant mantle cell lymphoma. Leuk. Res. 2006, 30, 497–501. [Google Scholar] [CrossRef]
- Amin, H.M.; McDonnell, T.J.; Medeiros, L.J.; Rassidakis, G.Z.; Leventaki, V.; O’Connor, S.L.; Keating, M.J.; Lai, R. Characterization of 4 mantle cell lymphoma cell lines. Arch. Pathol. Lab. Med. 2003, 127, 424–431. [Google Scholar] [CrossRef] [PubMed]
- Jeon, H.J.; Kim, C.W.; Yoshino, T.; Akagi, T. Establishment and characterization of a mantle cell lymphoma cell line. Br. J. Haematol. 1998, 102, 1323–1326. [Google Scholar] [CrossRef] [PubMed]
- Davids, M.S.; Roberts, A.W.; Kenkre, V.P.; Wierda, W.G.; Kumar, A.; Kipps, T.J.; Boyer, M.; Salem, A.H.; Pesko, J.C.; Arzt, J.A.; et al. Long-term Follow-up of Patients with Relapsed or Refractory Non-Hodgkin Lymphoma Treated with Venetoclax in a Phase I, First-in-Human Study. Clin. Cancer Res. 2021, 27, 4690–4695. [Google Scholar] [CrossRef] [PubMed]
- Sawalha, Y.; Goyal, S.; Switchenko, J.M.; Romancik, J.T.; Kamdar, M.; Greenwell, I.B.; Hess, B.T.; Isaac, K.M.; Portell, C.A.; Mejia Garcia, A.; et al. A multicenter analysis of the outcomes with venetoclax in patients with relapsed mantle cell lymphoma. Blood Adv. 2023, 7, 2983–2993. [Google Scholar] [CrossRef]
- Chiron, D.; Dousset, C.; Brosseau, C.; Touzeau, C.; Maïga, S.; Moreau, P.; Pellat-Deceunynck, C.; Le Gouill, S.; Amiot, M. Biological rational for sequential targeting of Bruton tyrosine kinase and Bcl-2 to overcome CD40-induced ABT-199 resistance in mantle cell lymphoma. Oncotarget 2015, 6, 8750–8759. [Google Scholar] [CrossRef]
- Prukova, D.; Andera, L.; Nahacka, Z.; Karolova, J.; Svaton, M.; Klanova, M.; Havranek, O.; Soukup, J.; Svobodova, K.; Zemanova, Z.; et al. Cotargeting of BCL2 with Venetoclax and MCL1 with S63845 Is Synthetically Lethal In Vivo in Relapsed Mantle Cell Lymphoma. Clin. Cancer Res. 2019, 25, 4455–4465. [Google Scholar] [CrossRef]
- Dolnikova, A.; Kazantsev, D.; Klanova, M.; Pokorna, E.; Sovilj, D.; Kelemen, C.D.; Tuskova, L.; Hoferkova, E.; Mraz, M.; Helman, K.; et al. Blockage of BCL-XL overcomes venetoclax resistance across BCL2+ lymphoid malignancies irrespective of BIM status. Blood Adv. 2024, 8, 3532–3543. [Google Scholar] [CrossRef]
- Brown-Burke, F.; Hwang, I.; Sloan, S.; Hinterschied, C.; Helmig-Mason, J.; Long, M.; Chan, W.K.; Prouty, A.; Chung, J.H.; Zhang, Y.; et al. PRMT5 inhibition drives therapeutic vulnerability to combination treatment with BCL-2 inhibition in mantle cell lymphoma. Blood Adv. 2023, 7, 6211–6224. [Google Scholar] [CrossRef]
- Cosenza, M.; Sacchi, S.; Pozzi, S. Preclinical Efficacy and Biological Effects of Venetoclax and Ixazomib in Combination in Lymphoma Cells. Blood 2020, 136, 37–38. [Google Scholar] [CrossRef]
- Zhao, S.; Kanagal-Shamanna, R.; Navsaria, L.; Ok, C.Y.; Zhang, S.; Nomie, K.; Han, G.; Hao, D.; Hill, H.A.; Jiang, C.; et al. Efficacy of venetoclax in high-risk relapsed mantle cell lymphoma (MCL)—Outcomes and mutation profile from venetoclax resistant MCL paatients. Am. J. Hematol. 2020, 95, 623–629. [Google Scholar] [CrossRef]
- Hagiwara, K.; Tokunaga, T.; Iida, H.; Nagai, H. Synergistic Cytotoxicity of Bendamustine and the BTK Inhibitor in a Mantle Cell Lymphoma Cell Line. Anticancer Res. 2015, 35, 6679–6684. [Google Scholar] [PubMed]
- Wang, M.L.; Jurczak, W.; Jerkeman, M.; Trotman, J.; Zinzani, P.L.; Belada, D.; Boccomini, C.; Flinn, I.W.; Giri, P.; Goy, A.; et al. Ibrutinib plus Bendamustine and Rituximab in Untreated Mantle-Cell Lymphoma. N. Engl. J. Med. 2022, 386, 2482–2494. [Google Scholar] [CrossRef] [PubMed]
- Phillips, T.J.; Smith, S.D.; Jurczak, W.; Robak, T.; Stevens, D.; Farber, C.M.; Pagel, J.M.; Maddocks, K.J.; Flinn, I.W.; Jedrzejczak, W.W.; et al. Safety and efficacy of acalabrutinib plus bendamustine and rituximab in patients with treatment-naive or relapsed/refractory mantle cell lymphoma: Phase Ib trial. Haematologica 2020, 132, 4144. [Google Scholar] [CrossRef] [PubMed]
- Banna, G.L.; Collovà, E.; Gebbia, V.; Lipari, H.; Giuffrida, P.; Cavallaro, S.; Condorelli, R.; Buscarino, C.; Tralongo, P.; Ferraù, F. Anticancer oral therapy: Emerging related issues. Cancer Treat. Rev. 2010, 36, 595–605. [Google Scholar] [CrossRef]
- Lonardi, S.; Bortolami, A.; Stefani, M.; Monfardini, S. Oral Anticancer Drugs in the Elderly. Drugs Aging 2007, 24, 395–410. [Google Scholar] [CrossRef]
- Romancik, J.T.; Cohen, J.B. Management of Older Adults with Mantle Cell Lymphoma. Drugs Aging 2020, 37, 469–481. [Google Scholar] [CrossRef]
- Dillmon, M.S.; Kennedy, E.B.; Anderson, M.K.; Brodersen, M.; Cohen, H.; D′Amato, S.L.; Davis, P.; Doshi, G.; Genschaw, S.; Makhoul, I.; et al. Patient-Centered Standards for Medically Integrated Dispensing: ASCO/NCODA Standards. J. Clin. Oncol. 2020, 38, 633–644. [Google Scholar] [CrossRef]
- Wang, H.; Shi, H.; Wang, Y.; Wang, N.; Li, Y.; Yang, Q.; Li, Y.; Liu, C.; Zan, Y.; Feng, S.; et al. Potentially Hazardous Drug-Drug Interactions Associated with Oral Antineoplastic Agents Prescribed in Chinese Tertiary Care Teaching Hospital Settings: A Multicenter Cross-Sectional Study. Front. Pharmacol. 2022, 13, 808848. [Google Scholar] [CrossRef]
- Itoh, K.; Igarashi, T.; Irisawa, H.; Aotsuka, N.; Masuda, S.; Utsu, Y.; Tsujimura, H.; Tsukasaki, K.; Wakita, H. Randomized phase II study of a bendamustine monotherapy schedule for relapsed or refractory low-grade B-cell non-Hodgkin lymphoma or mantle cell lymphoma (RABBIT-14). Leuk. Lymphoma 2018, 59, 1606–1613. [Google Scholar] [CrossRef]
- Ohmachi, K.; Ando, K.; Ogura, M.; Uchida, T.; Itoh, K.; Kubota, N.; Ishizawa, K.; Yamamoto, J.; Watanabe, T.; Uike, N.; et al. Multicenter phase II study of bendamustine for relapsed or refractory indolent B-cell non-Hodgkin lymphoma and mantle cell lymphoma. Cancer Sci. 2010, 101, 2059–2064. [Google Scholar] [CrossRef]
- Souers, A.J.; Leverson, J.D.; Boghaert, E.R.; Ackler, S.L.; Catron, N.D.; Chen, J.; Dayton, B.D.; Ding, H.; Enschede, S.H.; Fairbrother, W.J.; et al. ABT-199, a potent and selective BCL-2 inhibitor, achieves antitumor activity while sparing platelets. Nat. Med. 2013, 19, 202–208. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Filioglou, D.; Santa-Cruz, N.; Leite, G.S.F.; Davini, D.W.; Cracchiolo, M.J.; Baker, F.L.; Husnain, M.; Simpson, R.J.; Voudouris, V.; Katsanis, E. A Triple Oral Combination of Bendamustine, Acalabrutinib, and Venetoclax Demonstrates Efficacy Against Mantle Cell Lymphoma In Vitro and In Vivo. Cancers 2025, 17, 1889. https://doi.org/10.3390/cancers17111889
Filioglou D, Santa-Cruz N, Leite GSF, Davini DW, Cracchiolo MJ, Baker FL, Husnain M, Simpson RJ, Voudouris V, Katsanis E. A Triple Oral Combination of Bendamustine, Acalabrutinib, and Venetoclax Demonstrates Efficacy Against Mantle Cell Lymphoma In Vitro and In Vivo. Cancers. 2025; 17(11):1889. https://doi.org/10.3390/cancers17111889
Chicago/Turabian StyleFilioglou, Dimitrios, Nina Santa-Cruz, Geovana S. F. Leite, Dan W. Davini, Megan J. Cracchiolo, Forrest L. Baker, Muhammad Husnain, Richard J. Simpson, Vasilios Voudouris, and Emmanuel Katsanis. 2025. "A Triple Oral Combination of Bendamustine, Acalabrutinib, and Venetoclax Demonstrates Efficacy Against Mantle Cell Lymphoma In Vitro and In Vivo" Cancers 17, no. 11: 1889. https://doi.org/10.3390/cancers17111889
APA StyleFilioglou, D., Santa-Cruz, N., Leite, G. S. F., Davini, D. W., Cracchiolo, M. J., Baker, F. L., Husnain, M., Simpson, R. J., Voudouris, V., & Katsanis, E. (2025). A Triple Oral Combination of Bendamustine, Acalabrutinib, and Venetoclax Demonstrates Efficacy Against Mantle Cell Lymphoma In Vitro and In Vivo. Cancers, 17(11), 1889. https://doi.org/10.3390/cancers17111889






