1. Introduction
Recent advances on the molecular aspects of gastric cancer (GC) have provided invaluable knowledge that led to the identification of new actionable targets and therapies [
1]. Targeted treatments and immunotherapies are mainly offered to advanced cancer patients and have, so far, minimally improved GC prognosis, justifying why GC ranks as the third leading cause of cancer-related deaths worldwide [
2]. Gastric tumors with high mutation load, microsatellite instability (MSI) or positive for Epstein–Barr viral infection are potentially immunogenic, and thus amenable for immunotherapy based on checkpoint inhibitors (e.g., anti- PD-1/PD-L1) [
3,
4]. Finding additional contexts for immuno-related therapies is an opportunity that is worth investigating further.
Regulatory T cells (Tregs) are CD4
+ T cells characterized by the surface expression of IL2Rα, and nuclear expression of the transcription factor FoxP3. Tregs are endowed with immunosuppressive activity that enforces peripheral tolerance and maintains immunological homeostasis [
5]. However, in cancer, the immunosuppressive environment promoted by Tregs withholds the antitumor immune response, hence promoting tumor progression and dissemination [
6,
7]. In GC patients, peripheral blood and tumor-infiltrating lymphocytes are enriched in Tregs [
8,
9,
10,
11,
12], which associates with increased tumor stage, poor prognosis and reduced patient survival [
13,
14,
15,
16,
17]. Nevertheless, other studies have shown that tumor infiltrating Tregs may also be associated with favorable prognosis, specifically in patients carrying tumors from the cardia or with MSI [
18,
19,
20]. Hence, the role of Tregs in GC progression remains poorly understood and highly controversial. Further, it is also unexplored in GC whether Tregs may promote tumor progression via non-immunological mechanisms, as described in other cancer models [
21,
22]. Thus, we sought to explore the contribution of Tregs in GCs with distinct histology, and whether Tregs can directly impact tumor cells to promote GC progression.
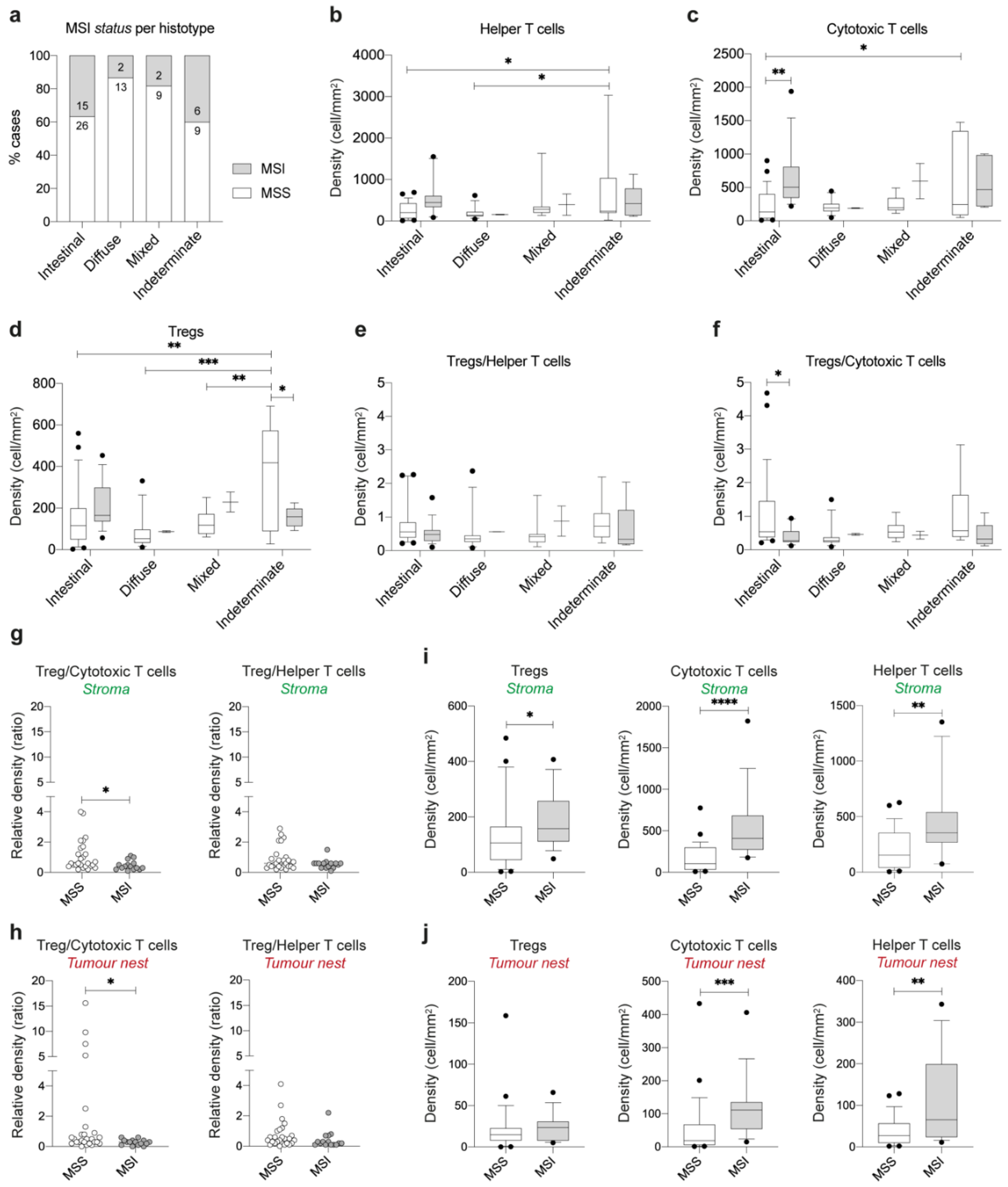
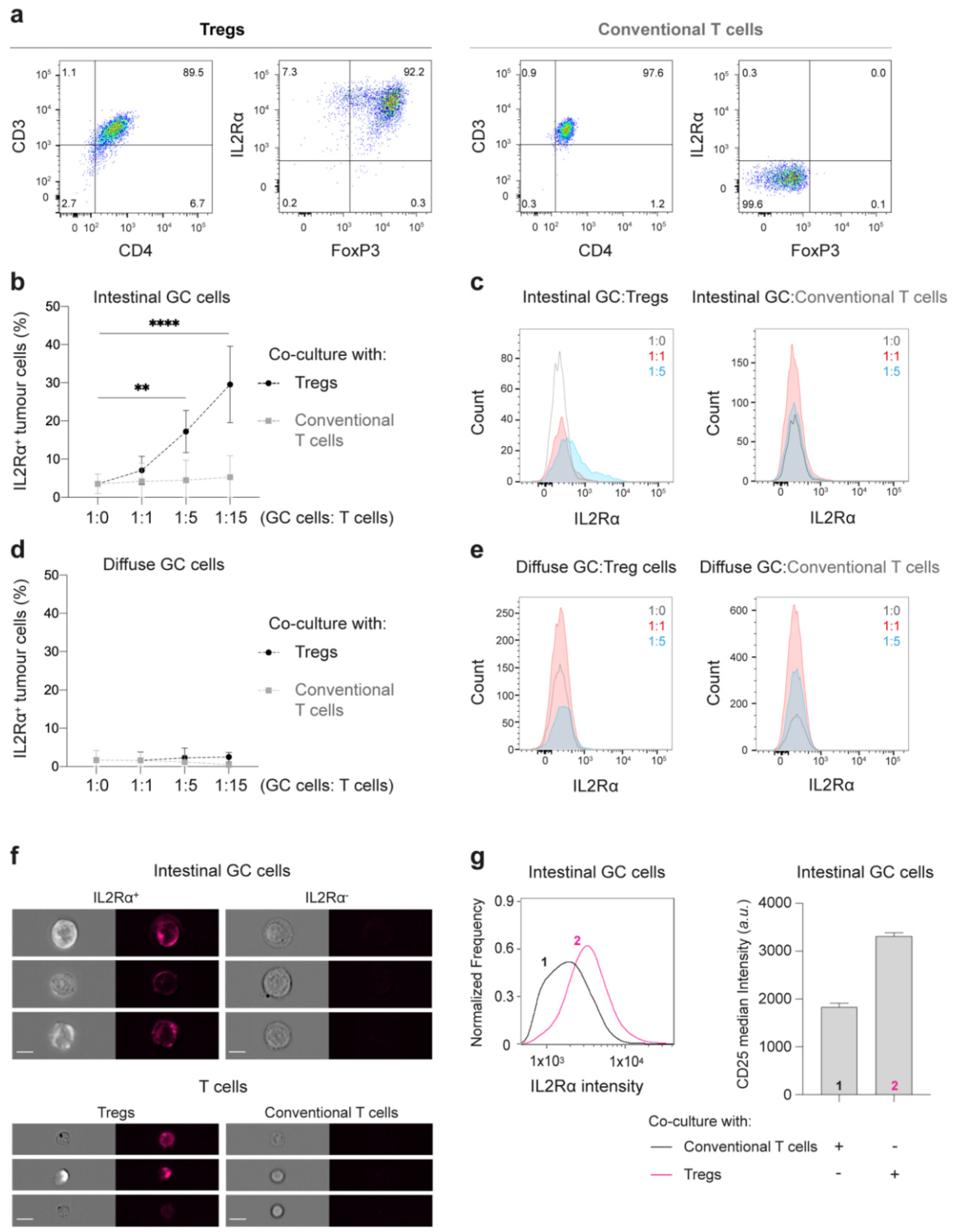
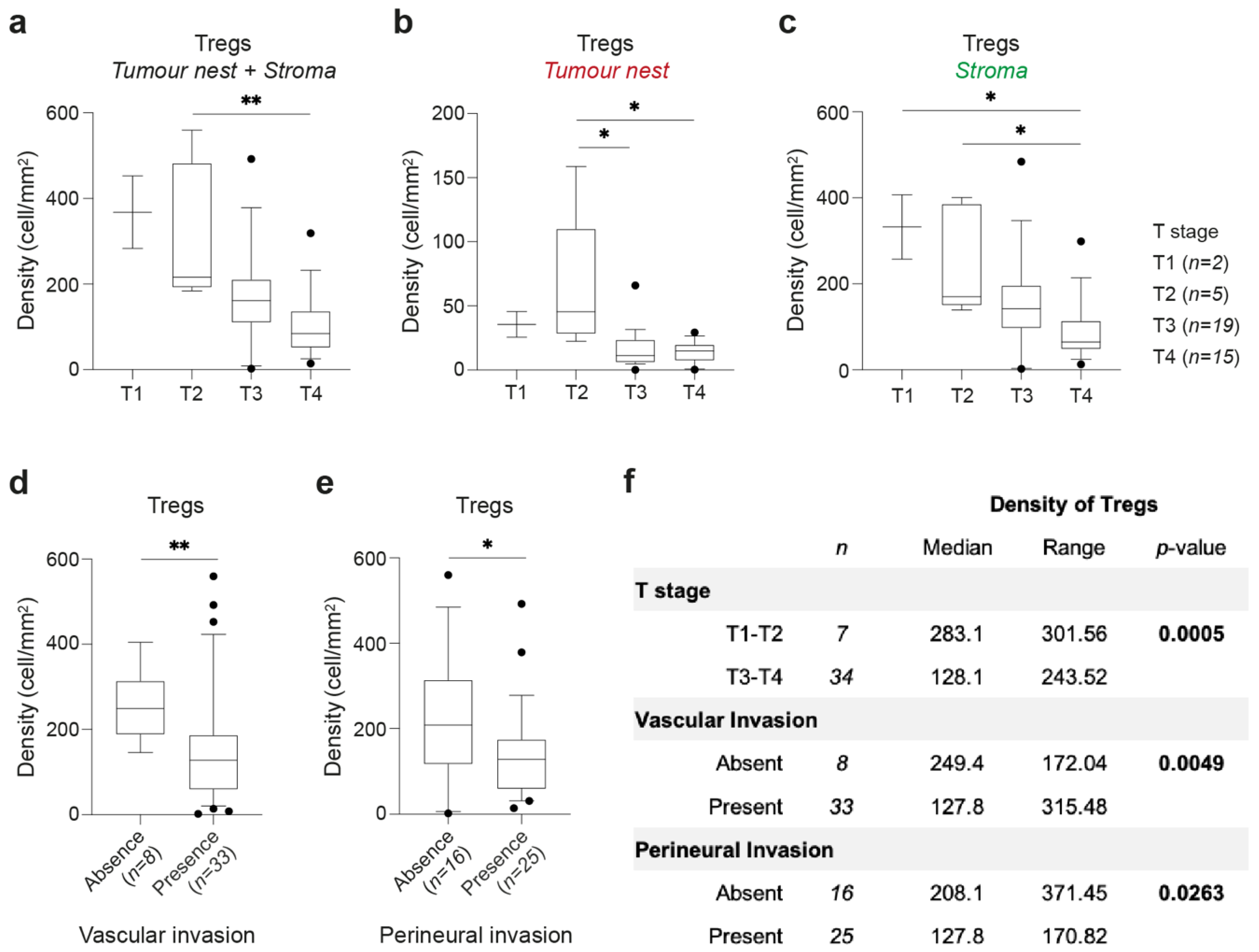
To address this, we integrated the results of T cell immunophenotyping analysis with clinicopathological features of 82 GC patients. This analysis unveiled an enrichment of Tregs specifically in intestinal- and indeterminate-type GC, as compared to diffuse-type GC. Furthermore, our data suggests that a population of Tregs is present at the tumor nest of intestinal-type GC independently of the prevalence of effector T cells. Given these results, and to understand whether Tregs may actively modulate the phenotype of tumor cells, we established and explored 3D co-cultures of Tregs with intestinal- or diffuse-type GC cell lines. We found that Tregs actively infiltrate intestinal-type GC spheroids. Upon co-culture with Tregs, intestinal-type GC cells acquire expression of IL2Rα at the cell membrane, have increased activation of MAPK signaling pathway and spheroid growth. Furthermore, we found an enrichment of Tregs in early-stage intestinal-type GC, and in the absence of vascular and perineural invasion.
Altogether, our data suggests a direct effect of Tregs on tumor cells that may be particularly important in early stages of intestinal-type GC progression.
3. Discussion
In this study, we combined single-cell immunophenotyping of GC samples, clinicopathological data, and 3D in vitro co-culture cell models to propose a tumor-promoting, non-immunosuppressive role of Tregs in GC progression (
Figure 7). According to our findings, intestinal-type GCs are enriched in Tregs that preferentially accumulate during the initial steps of tumor progression. Additionally, our in vitro results suggest that Tregs may promote proliferation of intestinal-type GC cells by inducing membranous expression of IL2Rα in tumor cells, which associated with MAPK pathway activation and cell proliferation. Together, these results led us to hypothesize that Tregs that successfully infiltrate the tumor nest of intestinal-type GCs may directly contribute to their well-known proliferative behavior.
Despite growing evidence of Treg enrichment in GC microenvironment, the role of Tregs in GC remains poorly understood. Studies showing that Tregs are already increased in non-neoplastic lesions, such as gastritis and peptic ulcers [
25,
26], suggest that Treg accumulation may be a consequence of inflammation and occurs before GC initiation. These findings have initially fostered our hypothesis that Tregs might differently contribute to the neoplastic development of tumors arising in distinct inflammatory contexts. To investigate this and considering recent data on the importance of studying the immunophenotype of GC [
27,
28], we performed a single-cell spatial analysis of the immune landscape of gastric tumors with distinct histology. Our results showed that among the T cell populations analyzed, Tregs were enriched in intestinal-type and indeterminate-type GC, which are often associated to chronic inflammation, in comparison to diffuse-type GC. This association of Tregs with inflammatory environments supports the proposed mechanisms of Treg accumulation in GC tumors based on CCL17/CCL22-mediated recruitment of Tregs or TGF-β-mediated conversion of conventional T cells into Tregs [
29,
30,
31]. Another similarity between intestinal-type and indeterminate-type GCs was the increased proportion of MSI cases, which could elicit stronger anti-tumor immune responses [
32]. Indeterminate-type MSS GCs showed elevated, though highly variable, T cell numbers that likely recapitulate the heterogenous nature of these tumors. Interestingly, in intestinal-type GCs, we observed an unbalanced ratio of Tregs and cytotoxic T cells, comparing MSS and MSI tumors. Such findings were more evident at the tumor nest of MSS tumors, where the number of Tregs was higher than the number of cytotoxic T cells. This excess of Tregs at the tumor nest fostered the hypothesis of a direct crosstalk between Tregs and intestinal-type tumor cells. Hence, we established direct co-cultures of T cells and 3D GC spheroids recapitulating the histological properties of intestinal- and diffuse-type GC [
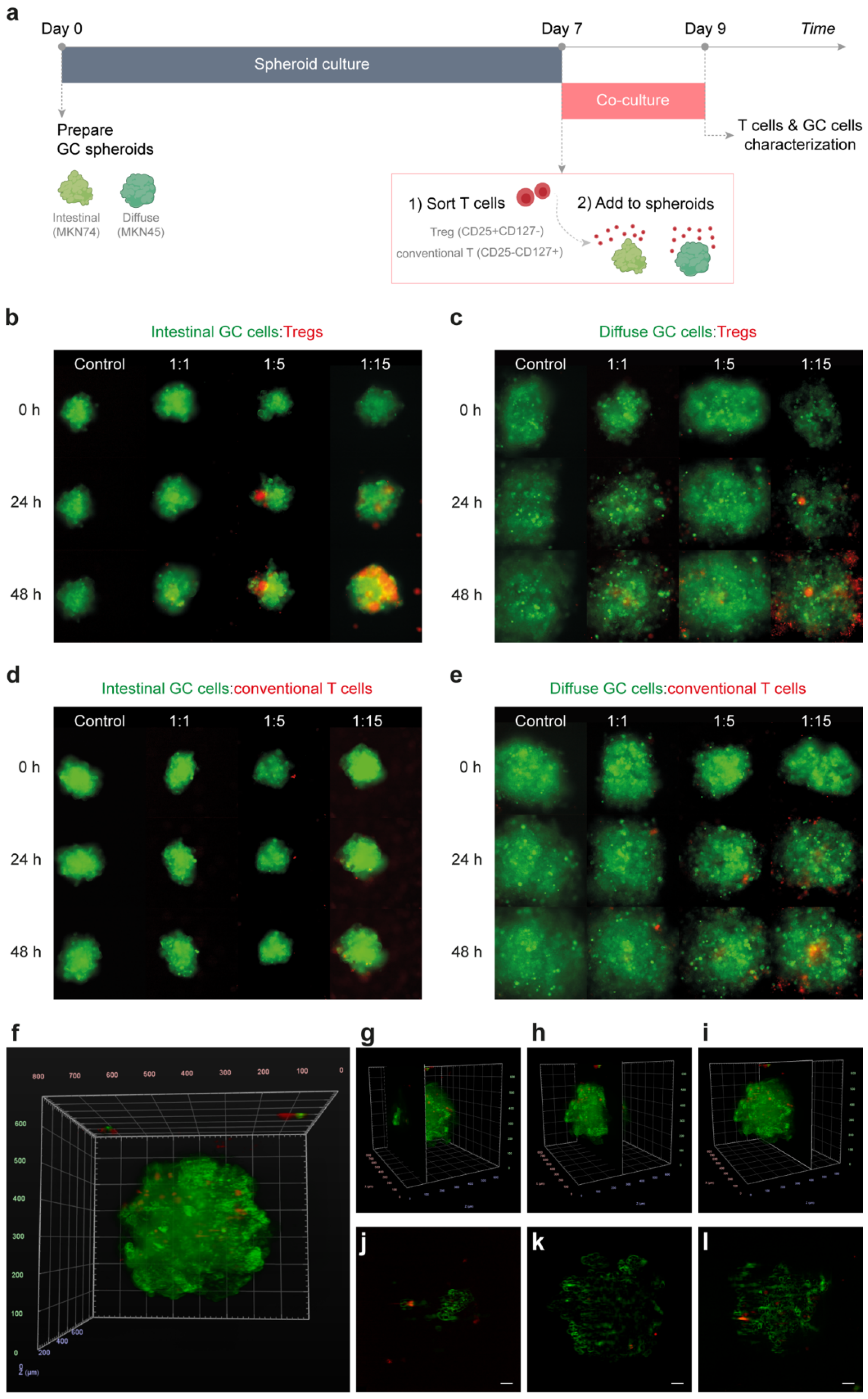
33]. This valuable tool allowed us to assess specific and active spheroid infiltration by T cells. As tumors can remodel their microenvironment, modulating Tregs’ phenotype or even converting conventional T cells into Tregs [
7], we prepared co-cultures with T cells isolated from healthy donors, presumably without prior contact with tumor cells. We demonstrated that only a small fraction of Tregs infiltrates GC spheroids, even if high numbers of Tregs are added to the culture. Our 3D co-culture system not only closely mimics tumors from GC patients, but also their microenvironment context: (1) Treg density is higher outside than inside GC spheroids, which resembles the high T cell density at the GC stroma comparing to tumor nest; (2) Tregs, but not conventional T cells, infiltrate GC spheroids, recapitulating the increased Treg numbers observed in the tumor nest; (3) Tregs preferentially infiltrate intestinal-type GC spheroids, mimicking the histological differences observed between intestinal- and diffuse-type GC. Noteworthy is also the fact that intestinal-type GC spheroids display stronger homotypic cell-to-cell adhesion than diffuse spheroids [
33], which would hamper Treg infiltration. Nevertheless, we also recognize the limitations to this approach. In this study, Tregs, but not conventional T cells, were stimulated with anti-CD3/anti-CD28 beads to maintain cell activation. A missing control of activated conventional CD4+ T cells is a significant limitation of this study as it would have allowed us to directly assess whether the observed effect is Treg-specific or driven by the stimulation of cells. Further studies should include additional and more relevant biological controls. Moreover, our co-culture system represents a simplistic representation of the in vivo scenario that should be further integrated with patient-derived xenografts or relevant in vivo models.
Our study suggests that the interaction between Tregs and tumor cells may have functional consequences, as intestinal-type cells acquire IL2Rα expression at the cell membrane, have stimulation of MAPK signaling pathway and increased spheroid growth. To our knowledge, this is the first study reporting IL2Rα de novo expression in epithelial tumor cells, which may hold important implications for the design of novel therapeutic strategies. Thus, it is critical to further understand the mechanisms that lead to IL2Rα expression in tumor cells and its molecular consequences. Our data suggests that IL2Rα is not passively transferred from Tregs to tumor cells, as tumor cells do not acquire other membrane Treg markers nor the cell tracer that was used to stain Tregs. Moreover, the conditioned medium of the Treg-intestinal tumor cell co-cultures was not sufficient to induce IL2Rα expression in other intestinal-type GC cells. Thus, it is unlikely that Treg-derived soluble factors or extracellular vesicles could actively foster or transfer IL2Rα to tumor cells. We expect that further studies focused on direct cell-cell interactions between Tregs and tumor cells, will enlighten the mechanisms underlying IL2Rα expression in tumor cells. Furthermore, it will be important to understand whether IL2Rα expression in tumor cells may also be induced by other activated T cell populations, as in this study conventional T cells were not activated.
In immune cells, IL2Rα is known to bind IL2 and form heterodimers with the β- (CD122) and γc- (CD132) chains of the IL2 receptor, to activate downstream signaling transduction [
23,
24]. Hence, it would be important to address whether IL2Rα-tumor cells additionally express CD122 and CD132, and are responsive to IL2 signals. These experiments are crucial to determine the molecular effects of Tregs in tumor cells that should be further validated in tissue samples. Although the results presented in this study suggest a novel and unexpected interaction between Tregs and tumor cells, the associated experimental limitations stress the need for further investigations to confirm the proposed hypothesis. Such experiments would require (1) the inactivation of IL2Rα and its downstream targets in tumor cells upon co-culture with Tregs; (2) a larger approach such as RNA sequencing or proteomics analysis on IL2Rα
+ tumor cells to fully disclose the signaling pathways activated by IL2Rα expression; and (3) a quantitative demonstration that spheroid growth was due to enhanced tumor cell proliferation. This thorough analysis would provide key molecular targets that could be further validated in patient-derived samples.
A deeper understanding on why, and under which circumstances, Tregs may induce expression of IL2Rα in tumor cells, may greatly impact the therapeutic strategies for intestinal-type GC patients and others presenting tumors with similar behavior. This knowledge may also shed light on the contrasting effects of IL2-based tumor therapies [
34]. Our results suggest that, under specific tumor contexts, therapies based on IL2 administration may favor tumor growth instead of just promoting immune T cell proliferation and survival. Additionally, tumor cells expressing IL2Rα at the membrane may compete with effector T cells for IL2, a tumor immune evasion strategy that, until now, was solely attributed to Tregs [
7]. Finally, innovative tumor therapies may arise directly from knowing that the initial steps of tumor growth may be dependent/potentiated by IL2Rα-mediated signaling. Strategies targeting IL2Rα [
35] can be specifically directed to epithelial cells, which may reduce the secondary effects from unspecific targeting of Tregs.
4. Materials and Methods
4.1. Patient Data
Tissue samples were obtained retrospectively from 82 GC patients who underwent gastric surgery with curative intent at Centro Hospitalar Universitário São João (CHUSJ; Porto, Portugal). Clinicopathological features were collected from medical and pathological records for further analysis (
Supplementary Table S1). Formalin-fixed paraffin-embedded (FFPE) specimens from 41 intestinal-type, 15 diffuse-type, 11 mixed-type, and 15 indeterminate-type GC tumors, according to Laurén histological classification, were included. For each case, the H&E-stained section used for histological classification was sequential to the one used for immunophenotyping analysis, to allow the association between the T cell immune profiling and tissue histological features. All cases were staged according to the eighth edition of the American Joint Committee on Cancer (AJCC) staging system. None of the patients included in this study was treated with neoadjuvant chemotherapy nor chemo-radiation therapy. The study was approved by the CHUSJ Ethics Committee (protocol 78/13).
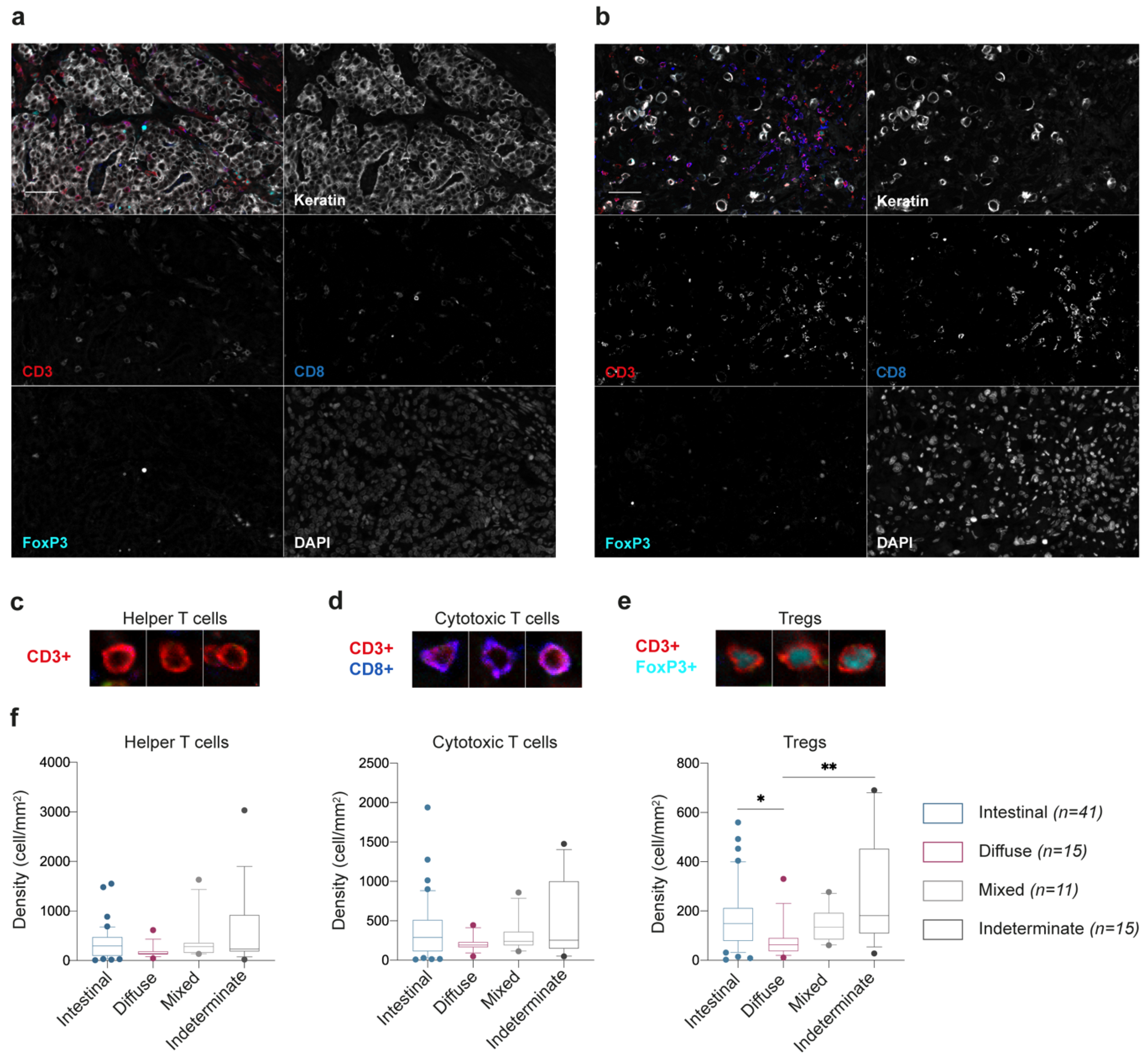
4.2. Immunofluorescence Staining, Image Acquisition, and Analysis
T cell immunophenotyping of GC samples was performed using a seven-target immunofluorescence detection protocol on single FFPE tissue sections, following a previously described combination of tyramide signal amplification (TSA) with direct and indirect immunostaining [
36]. Briefly, after an initial deparaffinisation of 4-µm tissue sections with xylene and washing with ethanol, endogenous peroxidase was inactivated by blocking with 0.3% hydrogen peroxide in methanol (20 min; Merck Millipore, Burlington, MA, USA) and heat-induced antigen retrieval was performed with Tris-EDTA buffer (10 mM/1 mM, pH 9.0, 10 min). After cooling, slides were incubated with Superblock solution (30 min; Thermo Fisher Scientific, Waltham, MA, USA) to block non-specific binding. For TSA, slides were incubated with anti-PD-1 antibody (D4W2J, 1:2000 dilution, 60 min; Cell Signalling Technology, Danvers, MA, USA), followed by incubation with poly-horseradish peroxidase solution (30 min; Immunologic, Duiven, The Netherlands) and with Opal 520 reagent (1:100 dilution, 60 min; Perkin Elmer, Waltham, MA, USA). Before proceeding to the indirect immunofluorescence step, microwave-induced antibody stripping was achieved by incubating slides in citrate buffer (10 mM, pH 6.0) at 90 W for 15 min. For the two-step immunofluorescence detection, slides were incubated with anti-FoxP3 (236A/E7, 1:25 dilution; Thermo Fisher Scientific), anti-CD8 (4B11, 1:50 dilution; Dako, Glostrup, Denmark) and anti-CD103 (EPR4166 2, 1:100 dilution; Abcam, Cambridge, UK) primary antibodies overnight, and with corresponding conjugated secondary antibodies (CF and Alexa Fluor dyes; Sigma–Aldrich, Saint Louis, MO, USA, and Thermo Fisher Scientific, respectively) for 60 min. Direct conjugated antibodies anti-CD3-AF594 (EP447E; Abcam) and anti-keratin-AF546 (AE1/AE3 and C11; Thermo Fisher Scientific and Cell Signalling Technology) were incubated for 5 h, after which slides were incubated with DAPI (1 µM) for nuclear staining and mounted using Prolong™ gold antifade reagent (Cell Signalling Technology). Further details on the antibodies used can be found in
Supplementary Table S2.
A complete scan of the slides was obtained using Vectra 3.0 Automated Quantitative Pathology Imaging System (4× magnification; Perkin Elmer) after which three regions of interest at the tumor core and another three at the invasive front were scanned with 20× magnification (1340 × 1000 µm images). Single-marker immunostainings were used to create the spectral libraries at the InForm Cell Analysis software (Perkin Elmer;
Supplementary Figure S8A). DAPI/keratin staining was used to segment images into tumor nest and stroma (
Supplementary Figure S8B). For cell segmentation, DAPI staining was used to segment nuclei, while CD3/CD8 staining was used to detect cell membrane (
Supplementary Figure S8C). The resulting cells were analyzed based on the following phenotypes (
Supplementary Figure S8D): (1) T helper cells, which were CD3
+CD8
-FoxP3
- cells; (2) CD8 T cells, CD3
+CD8
+; (3) and Treg cells that were CD3
+FoxP3
+ but CD8
-. We have also analyzed the expression of CD103 (resident T cells) and PD-1 (activated cells) within these phenotypes (
Supplementary Figure S8E). This data was not included in the main manuscript; however, it is available in
Supplementary File S1. Cells expressing cytokeratin were excluded when building T cell profiles. For each of the previous steps (i.e., tissue segmentation, cell segmentation, and immunophenotyping), the InForm Cell Analysis software was manually trained before automated classification. Cell density (cells/mm
2) was calculated by normalizing the cell counts by the tissue area of a given image.
4.3. Gastric Cancer 3D Cell Culture
Human GC cell lines MKN74 and MKN45 (intestinal- and diffuse-type GC, respectively; Japanese Collection of Research Bioresources Cell Bank) were seeded on 3D CoSeedis matrices (1 × 10
5 cells/mL; abc biopply, Solothurn, Switzerland), as previously described [
33], and cultured in RPMI 1640 medium (Thermo Fisher Scientific) supplemented with 10% fetal bovine serum (FBS; Biowest, Nuaillé, France) and 1% penicillin-streptomycin (PS; Thermo Fisher Scientific), at 37 °C in 5% CO
2 humidified atmosphere, for 7 days to allow spheroid formation before co-culture with T cells.
4.4. Preparation of Treg and Conventional T Cell Enriched Samples
Human T cells were freshly isolated from anonymized healthy donor buffy coats, provided by Instituto Português do Sangue e da Transplantação (Porto, Portugal). The isolation of immune cells from healthy blood donors was approved by the CHUSJ Ethics Committee (protocol 90/19) after each donor informed consent collection. Blood samples were diluted (1:3) in 2% FBS/PBS, layered on top of Histopaque
®-1077 (Sigma-Aldrich, St. Louis, MO, USA), on SepMate
TM tubes (Stemcell Technologies, Vancouver, BC, Canada), and centrifuged at 1200×
g (10 min, with the brake on). Resulting peripheral blood mononuclear cells (PBMCs) were enriched for CD4
+ T cells using MojoSort
TM Human CD4 T Cell Isolation Kit (BioLegend, San Diego, CA, USA). According to the manufacturer instructions, PBMCs were filtered through a 70-µm cell strainer and incubated with CD4 magnetic Nanobeads (20 min, on ice). CD4+ T cells were separated and washed in 2% FBS/PBS using a DynaMag™-15 magnet (Thermo Fisher Scientific). Thereafter, CD4
+ T cells were incubated with fluorescent conjugated antibodies anti-CD3-PE (OKT3, 1:400 dilution; Thermo Fisher Scientific), anti-CD4-FITC (OKT4, 1:400 dilution; Thermo Fisher Scientific), anti- IL2Rα-PE/Cy7 (BC96, 1:25 dilution; Thermo Fisher Scientific) and anti-CD127 APC/Cy7 (eBioRDR5, 1:50 dilution; Thermo Fisher Scientific) for 30 min. Fluorescence-activated cell sorting (FACS) of Tregs (CD3
+CD4
+CD127
−IL2Rα
+) and conventional T cells (CD3
+CD4
+CD127
+IL2Rα
−) was performed on FACSAriaII flow cytometer (BD Biosciences). Further details on the antibodies used can be found in
Supplementary Table S2.
4.5. Co-Culture of GC Spheroids and T Cells
For the co-culture of GC spheroids and T cells, MKN74 (intestinal-type) and MKN45 (diffuse-type) GC spheroids were transferred to round-bottom 96-well plates, and Tregs/conventional T cells were added to the culture media at 1:1, 1:5, and 1:15 (GC cell:T cell) ratios. Co-cultures were maintained in RPMI 1640 with 25 mM HEPES (Lonza, Basel, Switzerland) supplemented with 10% FBS, 1% PS, 1% Sodium pyruvate (Sigma-Aldrich) and recombinant human IL-2 (10 ng/mL; PeproTech, London, UK). Treg cultures were further supplemented with anti-CD3/anti-CD28 MACSiBead (0.5 beads/T cell; T Cell Activation Kit, Miltenyi Biotec, Bergisch Gladbach, Germany). As a control, MKN74/MKN45 single cultures (1:0; GC cell:T cell) were maintained in the same conditions as co-cultures. For all co-culture experiments (
Figure 3,
Figure 4 and
Figure 5), a minimal number of 6 independent T cells donors, collected and analyzed in at least 3 independent days are represented.
4.6. Live Cell Imaging
To monitor T cell infiltration into tumor spheroids, MKN74 and MKN45 cell lines stably expressing mEmerald were used to form the GC spheroids, and sorted Tregs and conventional T cells were stained with CellTrace™ Far Red (CTFR) Cell Proliferation Kit (20 min, 37 °C; Thermo Fisher Scientific) before co-culture. First, co-cultures were imaged using an automated fluorescence widefield HCS microscope (IN Cell Analyzer 2000; GE Healthcare, Chicago, IL, USA), equipped with a Plan-Fluor Nikon 20×/0.45 objective lens and a large-chip CCD camera (CoolSNAP K4). Emerald-GC spheroids were acquired in the FITC channel (Excitation/Emission: 490/ 525 nm; Exposure: 50 ms) and T cells in the Cy5 channel (Excitation/Emission: 645/705 nm; Exposure: 30 ms). Images were acquired at every 2 h for 60 h, under temperature-controlled conditions.
To further confirm Treg (CTFR) infiltration into intestinal-type GC spheroids (MKN74-Emerald), spheroids were transferred to a fluorinated ethylene propylene (FEP) microtube and imaged with a custom-built Digital Scanner Laser Light Sheet microscope (LSFM) equipped with a Nikon Plan-Fluor 10x/0.3 water-immersion objective lens in illumination and detection plans. The fluorescence signals of the Emerald-MKN74 spheroids and CTFR-Tregs were recorded using a Hamamatsu Orca-Flash 4.0 V3 camera, after sample excitation with a 488 (1.0 mW) and 640 nm (1.0 mW) laser lines, respectively, with a 525/50 nm bandpass (BP) emission filter for emerald-spheroids and a 700/75 nm BP emission filter for CTFR-Tregs. The co-culture was imaged at three timepoints (16 h, 24 h, and 48 h) from four angles (90° rotation) every 16 min. Each view consists of multiple slices 1 µm apart covering the entire spheroid. Image reconstruction was performed using the arivis Vision4D v3.1.4 (arivis AG, Rostock, Germany).
4.7. Immunophenotype by Conventional and Imaging Flow Cytometry Analysis
After 48 h of co-culture, conditioned media and spheroids were collected to analyze the phenotype of Tregs and conventional T cells. Before co-culture with GC spheroids, Tregs and conventional T cells were stained using CellTrace™ Violet (CTV) Cell Proliferation Kit (20 min, 37 °C; Thermo Fisher Scientific), to allow further evaluation of T cell proliferation and to separate T cells (CTV+) from GC cells (CTV-) in the flow cytometry analysis. To prepare single-cell suspensions, spheroids were dissociated using 0.5% Trypsin-EDTA (5 min, 37 °C; Thermo Fisher Scientific). Both T cells and GC cells were stained with anti-CD3-PE, anti-CD4-FITC, and anti-IL2Rα-PE/Cy7, as previously mentioned, and with Fixable Viability Dye eFluor™780 (1:1000 dilution; Thermo Fisher Scientific) to assess cell viability. Intracellular staining of FoxP3 was performed using the Foxp3/Transcription Factor Staining Buffer Set (Thermo Fisher Scientific), following manufacturer’s instructions. Briefly, cells were fixed with Fixation/Permeabilization Buffer (30 min; Thermo Fisher Scientific), blocked with human IgG (1 mg/mL, 15 min; Sigma-Aldrich) and stained with anti-FoxP3-APC (1:15, 30 min; Thermo Fisher Scientific). Data acquisition was performed on an LSRFortessa cytometer (Becton, Dickinson & Company, Franklin Lakes, NJ, USA) and analyzed using FlowJo v10 software (Becton, Dickinson & Company) following the gating strategy explained on
Supplementary Figure S3A.
Imaging flow cytometry was performed on single-cell suspensions derived from co-cultures of MKN74-GC spheroids with Tregs/conventional T cells and stained with anti-IL2Rα-PE/Cy7 antibody. Data was acquired on an imaging flow cytometer (ImageStreamX; Amnis Corporation, Seattle, WA, USA) equipped with INSPIRE software. Samples were excited with a 488 nm argon laser, and for each event, bright-field cell images were acquired (40× magnification) on channel 1, while IL2Rα signal was detected on channel 6 (Excitation/Emission: 496/774 nm). Laser power was not modified throughout the sample acquisition. Data analysis was performed using the IDEAS software (Amnis Corporation). Further details on the antibodies used can be found in
Supplementary Table S2.
4.8. Recovery of IL2Rα+ GC Cells and Western Blot Analysis
To analyze the effect of IL2Rα expression specifically on intestinal-type GC cells, MKN74-GC cells were stained with CellTrace™ Yellow (CTY) Cell Proliferation Kit (Thermo Fisher Scientific) before grown as spheroids, while Tregs and conventional T cells were stained with CellTrace™ Far Red (CTFR) Cell Proliferation Kit (Thermo Fisher Scientific) before co-culture. As previously, after co-culture, spheroids were dissociated, and the resulting single-cell suspension was stained with anti-IL2Rα-PE/Cy7 antibody. MKN74-GC cells (CTY+) positive or negative for IL2Rα were sorted on the FACSAria II flow cytometer (Becton, Dickinson & Company) and collected to FBS. According to the number of sorted cells, samples were resuspended in proportional volumes of radioimmunoprecipitation assay buffer (RIPA buffer) supplemented with protease and phosphatase inhibitors (Thermo Fisher Scientific) and cell lysis was allowed for 30 min, on ice. To enhance protein recovery, lysates were sonicated twice (10 s, 20×, 50%) before centrifugation at 14,000 rpm (15 min, 4 °C) to recover cleared lysates. Equal amounts of protein lysate (25 µL) from each biological replicate were subjected to Western blotting. Primary antibodies targeting phospho-Stat3 (Tyr705, D3A7; Cell Signalling Technology), Stat3 (124 h6; Cell Signalling Technology), phospho-Akt (Ser473, D9E; Cell Signalling Technology), Akt (Cell Signalling Technology), phospho-p44/42 MAPK (phospho-ERK1/2, Thr202/Tyr204; Cell Signalling Technology), p44/42 MAPK (ERK1/2; Cell Signalling Technology), and GAPDH (1E6D9; ProteinTech, Rosemont, IL, USA) were used, as well as corresponding ECLTM anti-mouse and anti-rabbit IgG horseradish peroxidase-conjugated secondary antibodies (GE Healthcare). Detected signals were quantified using Quantity One
® Basic software (Bio-Rad, Hercules, CA, USA). Unprocessed scans of Western blots are provided in
Supplementary Figure S9. Additional information on the antibodies used is detailed in
Supplementary Table S2.
4.9. Ki-67 Staining on GC-Spheroids
To investigate GC-spheroid proliferation after co-culture, spheroids were fixed with 2% paraformaldehyde (overnight; Merck, Darmstadt, Germany), stained with Gill’s hematoxylin (10 min; Bio-Optica, Milan, Italy) and injected within a drop of 2.4% low melting point agarose (50 °C; Lonza). After gelling (10 min at room temperature followed by 20 min on ice), the agarose structures were included in paraffin blocks and then sectioned into 3-µm slides. Antigen retrieval was performed using citrate buffer (10 mM, pH 6.0, at 98 °C, 40 min; Abcam). Endogenous peroxidase activity was blocked using 0.3% hydrogen peroxidase solution (20 min; Sigma-Aldrich) followed by incubation with anti-Ki-67 antibody (SP6, 1:200 dilution, 90 min; Thermo Fisher Scientific). After washing, slides were incubated with REAL EnVision Detection System (Dako) substrate buffer (30 min) and with DAB Chromogen (10 min).