Simple Summary
The introduction of BRAF/MEK-directed targeted therapy (TT) has significantly improved the management of patients with advanced BRAF-V600-mutant melanoma. Although resistance occurs, there is a subgroup of patients showing a complete response (CR) to TT and who maintain durable disease control. For these patients with durable CR, it is not clear whether it is safe to cease therapy. In this retrospective, multicenter study we have analyzed 37 patients who received TT and achieved a CR upon treatment. We identified 15 patients with a durable CR to TT. Overall, patients who discontinued TT (n = 26) were at higher risk of tumor progression compared to patients receiving ongoing TT. Sustained CR was however not restricted to patients with ongoing TT (n = 11) but was also found in patients who ceased TT (n = 4). Finally, our analysis indicated which patients with an initial CR might be most likely to maintain durable CR upon discontinuation of TT.
Abstract
The advent of BRAF/MEK inhibitors (BRAFi/MEKi) has significantly improved progression-free (PFS) and overall survival (OS) for patients with advanced BRAF-V600-mutant melanoma. Long-term survivors have been identified particularly among patients with a complete response (CR) to BRAF/MEK-directed targeted therapy (TT). However, it remains unclear which patients who achieved a CR maintain a durable response and whether treatment cessation might be a safe option in these patients. Therefore, this study investigated the impact of treatment cessation on the clinical course of patients with a CR upon BRAF/MEK-directed-TT. We retrospectively selected patients with BRAF-V600-mutant advanced non-resectable melanoma who had been treated with BRAFi ± MEKi therapy and achieved a CR upon treatment out of the multicentric skin cancer registry ADOReg. Data on baseline patient characteristics, duration of TT, treatment cessation, tumor progression (TP) and response to second-line treatments were collected and analyzed. Of 461 patients who received BRAF/MEK-directed TT 37 achieved a CR. TP after initial CR was observed in 22 patients (60%) mainly affecting patients who discontinued TT (n = 22/26), whereas all patients with ongoing TT (n = 11) maintained their CR. Accordingly, patients who discontinued TT had a higher risk of TP compared to patients with ongoing treatment (p < 0.001). However, our data also show that patients who received TT for more than 16 months and who discontinued TT for other reasons than TP or toxicity did not have a shorter PFS compared to patients with ongoing treatment. Response rates to second-line treatment being initiated in 21 patients, varied between 27% for immune-checkpoint inhibitors (ICI) and 60% for BRAFi/MEKi rechallenge. In summary, we identified a considerable number of patients who achieved a CR upon BRAF/MEK-directed TT in this contemporary real-world cohort of patients with BRAF-V600-mutant melanoma. Sustained PFS was not restricted to ongoing TT but was also found in patients who discontinued TT.
1. Introduction
The advent of mitogen-activated protein kinase (MAPK) pathway inhibitors [1,2,3,4,5] and immune checkpoint inhibitors (ICI) [6,7,8] has dramatically changed the treatment landscape for patients with advanced melanoma. Prior to the introduction of these classes of medication, chemotherapy represented the only treatment option for patients with advanced melanoma and disease outcomes were poor with a median overall survival (OS) of approximately 7.5 months and a 5-year survival rate of less than 10% [3,9,10]. Nearly 50% of cutaneous melanomas harbor a BRAF-V600 mutation, resulting in a constitutive activation of the MAPK pathway [11,12]. Through direct inhibition of the BRAF-V600 driver mutation via BRAF inhibitors (BRAFi) a prolonged progression-free and overall survival have been overserved [5,13]. Nevertheless, disease progression after a median progression-free survival of 6–7 months was a common theme in therapy with single-agent BRAFi [1,4]. Reactivation of the MAPK pathway, development of de novo NRAS or MEK mutations, or variant splicing of mutant BRAF-V600 are among the mechanisms associated with the development of secondary acquired resistance [14,15,16]. The combination of a BRAFi with a MEK inhibitor (MEKi) has resulted in a significantly improved PFS and OS as well as a decreased incidence of adverse events [3,17,18]. The combinations of BRAF and MEK inhibitors have demonstrated immediate anti-tumor effects, which culminate in tumor regression and symptomatic improvement. However, response durability and the degree of response differ: Emerging data from a recently published landmark analysis suggests that a subset of patients with a CR to combination BRAFi/MEKi treatment shows a profound and durable response with a 5-year overall survival rate of 71% [19,20]. In contrast, patients with stable disease (SD) as the best overall response (BOR) only have a 5-year OS rate of 16%. Overall, partial response was reported in approximately 50% of the patients, whereas complete response, on the other hand, is recorded in 3–6% of the patients [4,21].
Unlike many ICI studies, where treatment is often only continued for a finite period of time, BRAFi/MEKi studies are regularly continued indefinitely, irrespective of progression or unacceptable toxicities [22]. Although TT protocols have generally a good tolerability, adverse events can occur frequently and represent one of the main reasons for treatment discontinuation [23,24]. Taking into account the clinical impact of persisting low-grade toxicities on the patients’ quality of life and the potential risk of secondary malignancies [25,26], it remains a pending issue to determine whether BRAFi and MEKi should be continued until progression or whether it can be stopped at an earlier time point without posing a significant risk for subsequent tumor progression (TP).
In particular, it is currently unclear how long BRAFi and MEKi should be continued for patients with an initial CR and if treatment cessation might impact the clinical outcome of these patients. Investigating the clinical course of patients with an initial CR to BRAF/MEK-directed TT might further help to identify potential factors affecting the duration of response and thus optimize individual treatment strategies after CR to TT.
In the current study, we retrospectively examined a cohort of patients with BRAF-V600-mutant metastatic melanoma who were treated with BRAFi/MEKi and achieved an initial CR upon treatment. Data on the presented patient cohort were collected within the framework of the “Registery of the Arbeitsgemeinschaft Dermatologische Onkologie” (ADOReg). In order to assess the outcome of patients with CR after cessation of TT, we have compared three subgroups of patients: Patients with CR, who did continuously receive BRAF/MEK-directed TT upon CR, patients who had to discontinue TT due to TP or toxicity, and patients who did discontinue TT for other reasons, such as the personal wish of the patient or at the recommendation of the supervising physician (i.e., long-term moderate toxicities). Additionally, we aimed to identify potential factors predicting the clinical outcome of patients after treatment discontinuation, such as clinicopathological factors or the initial duration of TT. Last, we investigated the clinical response of patients who received ICI therapy as second-line treatment subsequent to TP during BRAF/MEK-directed TT. Such investigations are clinically relevant given the possibility of disease progression after cessation of BRAF/MEK-directed TT and the subsequent exigency to efficiently rechallenge tumor treatment.
2. Patients and Methods
We retrospectively analyzed all patients with BRAF-V600 advanced melanoma and CR upon BRAF-MEK-directed TT, who were included into the multicentric skin cancer registry ADOReg of the Dermatologic Cooperative Oncology Group (DeCOG) until the data cut-off (04/2020).
Data on the age at the start of TT with BRAFi and MEKi, sex, primary localization of melanoma, site of metastasis, LDH levels in serum, systemic pretreatments, duration of treatment, BOR to treatment, duration of the initial response, overall status of the patient, reasons for discontinuation, subsequent course of the disease and second-line treatment were collected. BOR was defined as complete response (CR), partial response (PR), stable disease (SD), or progressive disease (PD). PD was defined by disease recurrence at any site during observation according to standard RECIST criteria. In this retrospective analysis we included patients with advanced non-resectable melanoma (n = 2441/5231, 46.7%) who received first-line BRAF ± MEKi therapy (n = 461/5231, 8.8%) and subsequently showed a CR (n = 37/5231, 0.71%), and assessed their clinical course.
Statistical Analysis
Descriptive statistics were used to analyze the baseline characteristics of the study population. Treatment duration was calculated as the period between initial drug administration and the date of treatment discontinuation. The duration of the initial response was calculated from the date of the first administration of BRAF ± MEKi to the date of tumor progression or last follow-up. We employed Kaplan-Meier plots to illustrate median overall survival (OS) and progression-free survival (PFS) probabilities and to calculate the median OS and PFS of the investigated groups. Survival curves were compared by using the log-rank test. We performed univariate and multivariate Cox regression analysis to evaluate the impact of certain clinical baseline characteristics (e.g., sex, age, or ulceration) on OS. In order to quantify the impact on PFS and OS, we used Hazard ratios (HR) with 95% confidence intervals (CI). In all cases, two-tailed p-values were calculated and considered significant with values p < 0.05. SPSS (version 23, IBM, Ehningen, Germany), RStudio (Version 1.3.959) and GraphPad PRISM (Version 5, GraphPad Software, San Diego, CA, USA) were used for all analyses.
3. Results
3.1. Baseline Patient Characteristics
Among the 5231 melanoma patients in the ADOreg database, 2441 patients had an unresectable stage III or stage IV melanoma, and from these 461 patients (18.9%) received BRAFi ± MEKi treatment. Among patients receiving BRAF ± MEKi therapy, 37 patients (15 female, 22 male) developed a CR (8.0% of all advanced melanoma patients receiving BRAF ± MEKi therapy) and were enrolled into this retrospective study (Figure 1).
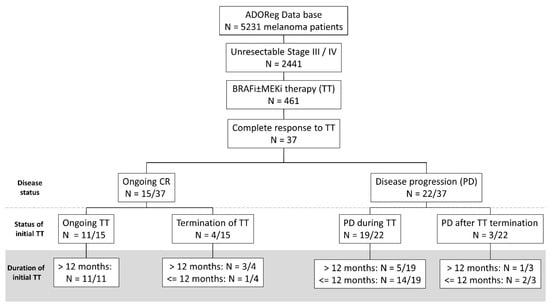
Figure 1.
Flow chart showing the selection steps of the retrospective study and the treatment outcomes of melanoma patients after an initial CR to BRAF/MEKi therapy. We included all patients with an unresectable stage III / IV melanoma receiving BRAF/MEK-inhibitor (i) therapy who showed an initial complete response (CR) (n = 37). Among these 37 patients, 40.5% experienced an ongoing CR, whereas 59.5% showed disease progression during follow-up. 11 patients who showed an ongoing CR continuously received BRAF ± MEKi therapy, whereas 4/15 patients discontinued TT previously, but yet showed an ongoing CR. Notably, most patients with an ongoing CR received initial BRAF ± MEKi therapy for a longer interval than 12 months. By contrast, patients showing a disease progression after initial CR, received BRAF ± MEKi therapy for less than 12 months and most patients experienced disease progression (PD) during BRAF ± MEKi therapy.
For this cohort showing an initial CR, the maximum observation period starting from the first application of BRAF ± MEKi therapy comprised 100 months. The mean patient age at TT initiation was 58 years (interquartile range, IQR: 33–77 years). The median primary tumor thickness was 3.2 mm (IQR: 1.33–5.00 mm). Eleven patients (29% of all patients) had an ulcerated primary tumor. All patients had confirmed BRAF-V600-mutations in their melanoma and 24 patients (64.9%) showed a BRAF-V600E-mutation. The median time interval from primary cancer diagnosis to metastasis was 15.0 months (IQR 1.5–58.0 months), with 9 patients (24.3%) showing an AJCC stage IV upon initial presentation and 5 patients (13.5%) having been diagnosed with melanoma brain metastasis (MBM) at the time of initial presentation. During the observation period, patients developed metastasis in a median of 3 different metastatic sites (range: 0–7) and 11 patients developed MBM in the course of the disease (Table 1).

Table 1.
Baseline patient characteristics.
All patients included in this retrospective study received BRAFi ± MEKi for at least one month and responded with an initial CR to TT as the BOR. All patients were naïve to systemic treatment, and TT with BRAFi ± MEKi was administered as first-line therapy. Overall, three patients received monotherapy with vemurafenib (2/37) or dabrafenib (1/37) and 34 patients received a combination of BRAFi and MEKi treatment, including five patients with encorafenib and binimetinib, 20 patients with dabrafenib and trametinib, and nine patients with cobimetinib and vemurafenib (Table 1).
3.2. Duration of BRAF/MEK Inhibitor Therapy
The median duration of TT in the entire cohort was 16 months (IQR: 6.5–28.0 months) with 11 patients still receiving the initial therapy with BRAFi± MEKi at the time of data cut-off (median treatment duration: 25.0 months). Among patients who terminated TT, the most common causes for treatment cessation were tumor progression (n = 13/26, 50%) and toxicity (n = 6/26, 23.1%). In seven patients, treatment was discontinued due to patient preference or at recommendation of the physician (in the following collectively referred to as physicians’ choice) (27%). When comparing the duration of treatment for patients who terminated BRAF ± MEKi for various reasons we observed that patients terminating TT due to toxicity received BRAF ± MEKi for the shortest time interval (median 5.5 months) compared to patients who terminated therapy due to TP (median: 10.0 months) or physicians’ choice (median: 12.0 months) (Figure 2). The median observation period after treatment cessation was 19 months (range: 0–70 months).
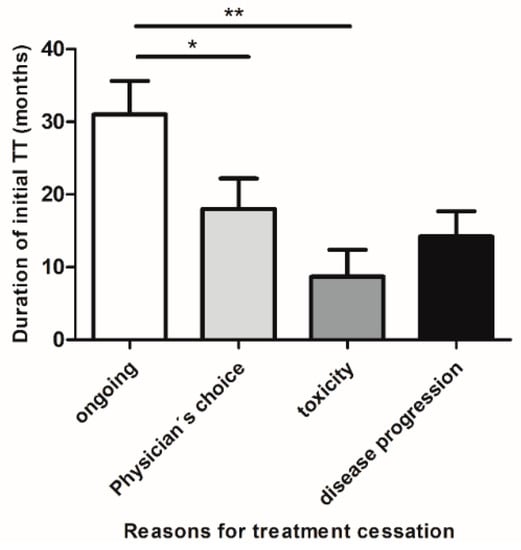
Figure 2.
Duration of BRAF/MEKi therapy in patients who obtained CR and either maintained treatment or discontinued TT for various reasons. Patients who discontinued first-line BRAF ± MEKi treatment due to treatment-associated toxicities (mean duration ± SEM: 8.7 ± 3.7 months) or due to disease progression (mean ± SEM: 14.2 ± 3.4 months), received therapy for a shorter time period compared to patients who discontinued therapy for other reasons (mean ± SEM: 18 ± 4.2 months) i.e., patient preference or at recommendation of the treating physician (collectively termed: physician’s choice). Patients with ongoing treatment had received BRAF ± MEKi therapy for the longest time period (mean ± SEM: 31 ± 4.6 months). Abbreviations: * p < 0.05; ** p < 0.005.
3.3. Treatment Duration Is Not Correlated with the Risk of TAE, But with a Longer PFS and OS
Our results revealed that 40% of patients recorded treatment-associated adverse events (TAE) of ≥CTCAE grade 1 during BRAF ± MEKi therapy including fever (11%), diarrhea (13%), or colitis (6%). Notably, the occurrence of TAE was not correlated with the duration of TT (t-test: 0.29). On the contrary, treatment-associated toxicities leading to discontinuation of therapy mainly occurred within the first 12 months of therapy (n = 5/6), thus reflecting the notion that patients terminating TT due to toxicity received BRAFi/MEKi for a shorter time period compared to patients ceasing TT for other reasons.
3.4. Factors Associated with Disease Progression and Survival upon BRAF/MEKi Treatment
Different clinical and pathological factors are associated with disease progression in the early stage of melanoma, such as ulceration or tumor thickness [27,28]. Thus, we investigated whether established prognostic factors, such as T-status, Breslow-index, ulceration, the number of metastatic tumor sites, the duration of treatment, the presence of MBM or AJCC-stage, and baseline patient characteristics (i.e., gender, age) might impact the OS in patients with complete responders upon BRAFi ± MEKi, using a multivariate Cox-Model. Here, the number of metastatic sites, and the ulceration status were found to increase the risk of disease progression upon TT, whereas the duration of initial TT was found to decrease the risk of disease progression. In accordance, we could show that patients who received BRAF ± MEKi therapy for a longer time period than 16 months had a significantly longer PFS and OS compared to patients receiving BRAF ± MEKi therapy for less than 16 months (median PFS 46 months vs. 7 months, p < 0.001, Figure 3; median OS: 77 months vs. 36 months, p = 0.037, Figure S1).
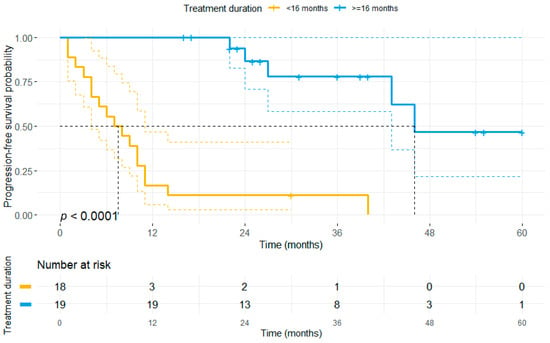
Figure 3.
The duration of first-line BRAF ± MEKi therapy correlates with progression-free survival. The patient cohort was stratified based on the median duration of first-line BRAF± MEKi treatment (16 months) in the entire study population. Patients who received first-line BRAF ± MEKi therapy for more than 16 months showed a significantly longer PFS (median: 46 months) as compared to patients receiving TT for a shorter time period (median PFS: 7 months).
3.5. Treatment Outcomes upon BRAF/MEKi Therapy
Tumor progression after initial CR to BRAF ± MEKi therapy was found in 22/37 patients and was most common in patients who had to discontinue TT in the course of the disease. 19/37 patients (54%) exhibited a relapse while under BRAFi ± MEKi treatment, whereas 3/37 patients (8.1%) relapsed after termination of BRAFi ± MEKi. Among patients who terminated BRAFi ± MEKi treatment while in CR, the median time to recurrence following treatment cessation was 1 month (mean: 10.9 months, range: 0–28 months). When excluding those patients who had to discontinue TT due to adverse events the median time from treatment cessation to relapse was 28 months (mean: 17.3 months). The median duration of treatment cessation among the 26 patients who had terminated TT was 0 months, with 20/37 patients terminating TT for less than 6 months, and 6/37 terminating TT for a longer interval than 6 months. By contrast, eleven of the 37 patients with CR (30%) received TT throughout the observation period, and all of these maintained their CR. Overall 15/37 (40.5%) patients remained progression-free throughout the observation period. The median PFS for the overall cohort, as assessed by Kaplan-Meier method, was 27 months (95% CI: 1.5–52.5 months) and median OS was 77 months (95% CI: 19.0–135.0 months).
3.6. Impact of Treatment Discontinuation
Investigating the impact of treatment discontinuation on the primary endpoints, we observed that patients who had discontinued TT (irrespective of the reasons) had a significantly shorter PFS (median PFS: 10 vs. not reached, p < 0.001, Figure 4) and OS compared to patients receiving ongoing TT (median OS: 77 months vs. not reached, p = 0.049, Figure S2).
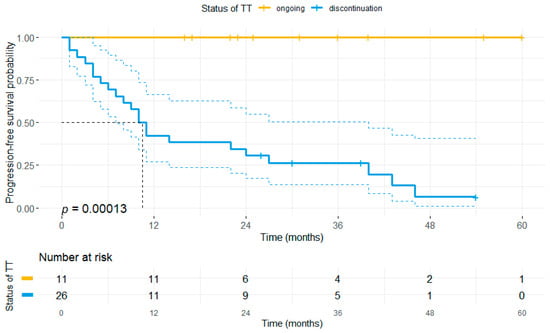
Figure 4.
Discontinuation of TT correlates with the risk of disease progression. All patients who obtained CR upon BRAF ± MEKi treatment and received therapy until data cut-off (n = 11) maintained their CR, whereas 22 of 26 patients who discontinued BRAF ± MEKi therapy at any time point during the observation period eventually relapsed. Accordingly, patients who had terminated TT showed a significantly shorter PFS (median: 10 months) compared to patients with ongoing BRAF ± MEKi therapy. Notably, patients who maintained their CR until treatment cessation showed a lower risk of tumor relapse after treatment cessation (n = 3/7) as compared to all patients ceasing TT.
Due to the strong heterogeneity in terms of treatment and outcome within this subcohort (see Table 2), we further distinguished patients according to the reasons for TT cessation or the duration of TT cessation. Here, our data revealed that 9/13 patients (69.2%) who discontinued TT for other reasons than PD experienced tumor progression after a median of 8 months, whereas 4/13 patients (30.8%) remained tumor-free. Progression-free survivors were mainly identified among patients who discontinued TT due to the wish of the patient or physicians’ choice (75%). Therefore, we compared patients who had to discontinue TT due to TAE or PD (n = 6 and n = 13) with patients who discontinued therapy for other reasons (n = 7) and patients who received ongoing TT (n = 11).

Table 2.
Patient characteristics in a subcohort of patients who discontinued TT due to reasons other than PD.
Our results unveiled, that patients who discontinued treatment either due to toxicity or PD did have a significantly shorter PFS (median PFS 3 months vs. 10 months vs. 40 months vs. not reached, p < 0.0001) compared to patients having discontinued for other reasons or receiving ongoing TT (Figure 5). Moreover, it was found that patients who discontinued therapy after previously having received TT for at least 12 months had a significantly longer PFS as compared to patients ceasing TT after a short initial BRAF/MEKi therapy (median PFS: 40 months vs. 6 months, p < 0.0001; Figure 6).
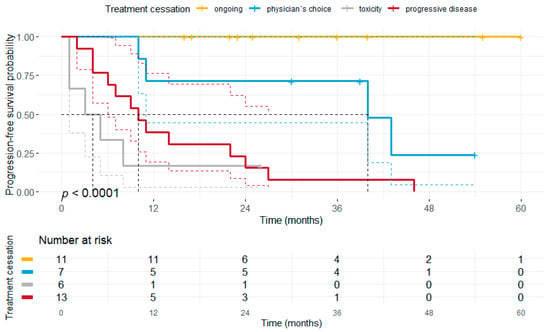
Figure 5.
Kaplan-Meier plot illustrating the progression-free survival separated by the reasons for treatment discontinuation. Patients who terminated BRAF ± MEKi therapy due to toxicity or disease progression had a significantly shorter PFS (median PFS: 3 months vs. 10 months) compared to patients with ongoing treatment (median PFS not reached, p < 0.0001) or treatment discontinuation due to other reasons (termed as physician’s choice) (median PFS: 40 months, p = 0.013).
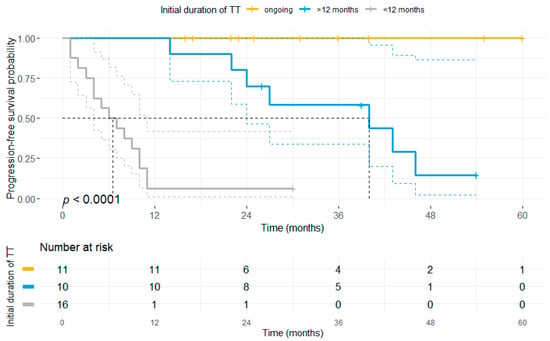
Figure 6.
Initial duration of BRAF ± MEKi therapy correlates with progression-free survival even after discontinuation of TT. The patient cohort was stratified based on the status of BRAF ± MEKi therapy (ongoing, yellow vs. discontinuation: blue and grey) and the initial duration of first-line BRAF ± MEKi treatment. Patients who received first-line BRAF ± MEKi therapy for more than 12 months prior to treatment discontinuation (blue) showed a significantly longer PFS (median: 40 months) as compared to patients receiving TT for a shorter time period (median PFS: 6 months) prior to treatment cessation.
Furthermore, we could observe that the median PFS and OS of patients who had stopped TT for a period of at least 6 months did not statistically differ from patients receiving ongoing BRAF ± MEKi therapy (median PFS 43 months vs. not reached, p < 0.001; median OS not reached in both groups, p = 0.06), whereas patients who terminated BRAF ± MEKi therapy for less than 6 months had a significantly shorter PFS and OS (median PFS: 9 months; median OS: 36 months) (Figure S3).
3.7. Duration of Response and Second-Line Treatment
Nearly 60% of patients (22/37) who initially responded with a CR to BRAFi ± MEKi treatment eventually showed TP at a later time point, requiring the application of second-line treatments that comprised either a re-induction of BRAFi ± MEKi (n = 5), initiation of ICI therapy (n = 15) or treatment with the oncolytic virus talimogen laherparepvec (n = 1) (Table 1). Among these patients receiving second-line treatments, 16 patients relapsed while under first-line BRAFi ± MEKi treatment, and 5 patients relapsed subsequent to BRAF ± MEKi termination. In patients that relapsed after discontinuation of TT, the median interval between discontinuation of first-line TT and the first administration of second-line ICI was 0 months (range: 0–13 months), whereas for patients with a re-induction of BRAF ± MEKi the median interval was 23 months (range: 0–28 months). Patients with second-line ICI received either a combination of ipilimumab (IPI) and nivolumab (Nivo) (33%) or monotherapy with Nivo (27%), IPI (13%), pembrolizumab (20%), or atezolizumab (7%). Notably, patients were less likely to respond to second-line ICI when ICI therapy was initiated subsequent to PD during BRAF ± MEKi (CR: n = 1, PR: n = none; ORR: 12.5%), as compared to patients who received ICI after discontinuation of BRAF ± MEKi for other reasons than PD (CR: n = 2, PR: n = 1; ORR: 42.8%).
Kaplan-Meier analysis including all patients receiving second-line ICI therapy revealed a median OS of 24 months and median PFS was 2 months (Figure S4). Overall, response to second-line ICI (defined as CR, PR or MR) was weak (n = 4/15; 27%) and CR could only be observed in 20% of patients (median PFS: 12 months). By contrast, three of the five patients who stopped first-line BRAFi ± MEKi, responded with a PR/CR (60%) to BRAFi ± MEKi-rechallenge, which lasted for a median of 9 months. Two of these patients remained relapse-free until the end of the observation period (median 9.5 months). Considering the widely divergent outcomes within the second-line ICI therapy and second-line TT cohorts, we hypothesized that certain clinical characteristics might help to identify patients with an increased risk of disease progression. Therefore, we performed logistic regression analysis to assess whether clinical characteristics correlate with the PFS of those two groups. In our study, we found no significant differences concerning T-stage (T2B vs. T2A), median AJCC stage at the time of initial diagnosis (IIIA vs. IIIA), median Breslow-thickness (3.6 mm vs. 3.15 mm), or the presence of tumor ulceration in the primary tumor (33% vs. 23%).
4. Discussion
The advent of immune checkpoint inhibitors (e.g., anti-PD-L1, anti-PD-1, anti-CTLA4) and the targeted inhibition of the MAPK pathway with BRAF and MEK inhibitors in BRAF-V600-mutant melanoma patients has led to profound and durable tumor responses in some patients with advanced melanoma [5,6]. Recent data suggests an overall survival of more than 5 years and a PFS >20% after 3 years in a subset of patients who have shown complete response to initial BRAF ± MEKi treatment [3]. Although patients undergoing a CR thus have a favorable survival, relapses while on treatment occur in approximately 30% of patients [29].
To date, there are no reliable clinical factors or markers which might predict the long-term response of BRAFi/MEKi after an initial CR. Hence, unlike many immunotherapy studies, the treatment in BRAF/MEKi-trials is mostly continued indefinitely. However, it has been reported that BRAF/MEKi therapy might also affect the tumor microenvironment (TME) and improve durable tumor surveillance, thus having a long-term beneficial effect. It has been shown that these long-term effects are most likely in patients with CR to TT [30]. In particular, it has been suggested by Long and colleagues, that patients with a CR and favorable baseline characteristics, such as a lower initial tumor burden, fewer metastatic tumor sites, or normal LDH-levels, may be more likely to show a stronger and more sustained response, thus driving long-term survival [19]. Nonetheless, the issue of whether TT should be continued until tumor progression or whether it can be stopped at an earlier time point without posing a significant risk of disease progression in this particular subgroup of patients remains unsolved.
In this retrospective study, we present the outcomes of a series of 37 patients who obtained CR upon BRAF ± MEK inhibition. The median duration of initial TT has been 16 months, with 11 patients still receiving therapy at the time of data cut-off. We observed that 60% of patients with an initial CR eventually showed tumor progression. Notably, disease progression has only been observed in patients who ceased BRAF ± MEKi therapy after obtaining an initial CR. Aligning with these results, median PFS and OS were significantly worse in patients who had to discontinue TT. Patients with a durable CR after treatment cessation were predominantly identified in a subcohort of patients who received initial TT for a long time period, who discontinued TT for other reasons than PD or toxicity, and who discontinued TT for a longer interval than 6 months (n = 4/6). Interestingly, baseline patient characteristics, including the median time of patient follow-up, have been similar for patients receiving ongoing TT.
These findings are consistent with previous reports investigating the outcome after treatment cessation in patients with a CR to initial BRAF ± MEKi therapy (see Table 3). These reports revealed the occurrence of long-term and progression-free survivors after discontinuation of TT. However, rates of melanoma recurrence (0–50%), median intervals to recurrence subsequent to TT discontinuation (3.0–6.6 months), and median follow-up after treatment cessation (12–19 months) showed strong variations depending on the specific trial [2,4,22,31,32,33]. Notably, all case reports reported high rates of treatment cessation due to toxicity (54%-100%), with the exception of Warburton and colleagues who excluded patients who terminated TT due to toxicity from their retrospective study [31].

Table 3.
Comparison of outcomes reported for metastatic melanoma cohorts with an initial CR to BRAFi ± MEKi therapy.
Our cohort differs from those previously published studies since we have included patients who continuously received TT and patients who ceased TT for various reasons. Therefore, we were able to compare the outcome of all these different subgroups and thus provide further insight into whether and when BRAF ± MEKi therapy can be safely discontinued in complete responders. In particular, patients included in our retrospective study received BRAF ± MEKi therapy for a relatively long time period before ceasing TT. Only two studies have reported a longer initial treatment with BRAF/MEKi [31,33]. However, patients terminating BRAF ± MEKi in this retrospective study for other reasons than PD showed a higher rate of tumor progression (69.2%) and a shorter PFS upon termination of TT, which might be explained by the longer overall observation period covered in our study [22,34,35].
In contrast to a previous report, we could further observe a strong correlation between the duration of the initial BRAF ± MEKi treatment and the maintenance of response after treatment cessation [22]. In particular, our analysis revealed that patients who received TT for a longer period than 12 months prior to treatment discontinuation had a significantly longer PFS as compared to patients with a shorter initial treatment. Therefore, we suggest that the duration of previous BRAF ± MEKi treatment might impact the strength and durability of the response after treatment discontinuation. Considering the off-target effects of BRAF/MEKi therapy, such as a paradoxical activation of CD8+ T-cells, it seems conceivable that a longer initial treatment with TT might prime anti-tumor immunity towards a more durable response even after treatment cessation [36]. However, due to the small number of patients included in our retrospective study, the clinical significance of our results certainly requires confirmation in larger prospective trials. Moreover, and consistent with previous trials, we could confirm that patients showing positive prognostic markers, such as a smaller number of metastatic tumor sites, no melanoma brain metastases and a smaller tumor burden at the time of initial diagnosis are more likely to undergo a prolonged response to BRAF ± MEKi therapy even after treatment discontinuation.
In most clinical trials with BRAF ± MEKi therapy, the main reason for discontinuation of treatment was disease progression [4,22]. In our retrospective study, disease progression has also been the main reason for treatment cessation (n = 13/22). Disease progression was largely found within the first 12 months of treatment (n = 9/13). By contrast, only two patients who had to discontinue therapy due to other reasons had shown a disease progression prior to 12 months of therapy (n = 2/7).
An important observation of our study is the correlation between the initial duration of BRAF ± MEKi therapy and sustained response durability upon discontinuation of TT. Moreover, we could show that discontinuation of TT due to disease progression (n = 13) or toxicity (n = 6) occurred at early time points after the initial administration of TT. In contrast, patients who terminated TT for other reasons had received BRAFi/MEKi for a longer period. Consistent with these findings, patients terminating BRAF/MEKi therapy for other reasons than PD or toxicity showed a significantly longer PFS and OS.
Although TT resulted in an initial CR in all patients investigated, tumor progression was observed in nearly 60% of patients, mostly affecting patients who had to discontinue TT. One common explanation for melanoma recurrence after an initial CR and subsequent discontinuation of treatment are micrometastases, which remain under cytostatic control during TT, while again proliferating upon treatment cessation [22]. However, this hypothesis might not explain the prolonged progression-free survival after treatment cessation, which has been found in some patients. In this regard, it has been suggested that BRAF/MEKi therapy—next to its cytostatic effects—might also contribute to tumor control via immunomodulatory effects, such as increasing melanoma immunogenicity, paradoxical activation of effector T cells, or reducing the infiltration of tumor-associated macrophages and myeloid-derived suppressor cells [36,37].
Our data regarding tumor progression are consistent with those of larger clinical trials. Notably, patients which have discontinued TT in this study had a higher risk of disease progression (n = 9/13) compared to a previously published study (n = 3/12) [31]. In our study tumor recurrence resulted in an alteration of the anti-tumor regiment and administration of ICI. Response to ICI in the second-line setting varies from 15.4% in case of pembrolizumab to 12% for combined IPI + Nivo treatment [38]. After DC-vaccination [39] or first-line ICI [6] response rates have been reported to be much higher (35–72%). By contrast, median PFS after progression upon combined TT has been reported to be 2.6 months for anti-PD-1 monotherapy vs. 2.0 months for a combination of anti-PD-1 and anti-CTLA-4 therapy. Objective response rates were found in 18.0% and 15.0%, respectively, whereas median OS has been found to be 8.4 months for nivolumab treatment and 7.2 months for combined Ipi + Nivo treatment [40]. Notably, these reports have included all patients receiving BRAF ± MEKi treatment.
In our study second-line ICI was administered in 15 patients subsequent to disease progression. The median interval between the initial application of first-line BRAF/MEKi therapy and the first administration of ICI was 10 months. Overall response rate (27%) and median PFS (2 months) to ICI in this second-line setting were poor as compared to ORR and median PFS in treatment-naïve patients [6]. This observation is consistent with the narrative of an aggressive melanoma progression once TT is discontinued [41]. While certain clinical factors such as the frequent appearance of MBM, a higher tumor burden, and increased levels of LDH are known factors that dampen the response to subsequent ICI [42,43] recent molecular studies have underlined the immunogenic profile of TT and its shift towards an immune inhibitory tumor microenvironment once secondary resistance occurs. This leads to a decrease in CD8+ T cell infiltration and an increase of regulatory T cells [44,45]. Furthermore, decreased PD-L1 expression levels at progress have been observed [46,47]. Hence, this shift in the TME at time of tumor progression might potentially contribute to the weak response found in patients receiving second-line ICI.
Reactivation of the MAPK signaling pathway is largely responsible for an acquired resistance against BRAF/MEKi therapy either due to emerging new spliced variants of BRAF, development NRAS mutation, or loss of feedback inhibition leading to BRAF dimerization resulting in resistance to BRAFi [48,49,50]. Nonetheless, it has been reported, that the rechallenge of BRAF ± MEKi therapy in patients who initially responded to TT is associated with a further response: Here, Valpione and coworkers have reported an objective response rate of 42% and PFS of 5 months after BRAFi rechallenge in 116 patients, which is consistent with the results of our study (ORR: 60% and PFS: 9 months) and previous publications [2,35,51]. Determining the optimal individual treatment after disease progression upon initial BRAF ± MEKi therapy might therefore be another important issue for clinical trials, as it may contribute to a better outcome and even lead to durable tumor responses in melanoma patients.
When interpreting the results of our analysis, limitations to be considered are the retrospective nature and the small cohort of patients under investigation, which may limit the significance and the accuracy to predict patients who may obtain long-term benefits of the treatment regimen. Therefore, interpretation of subgroup analysis in particular requires caution. Nonetheless, the multi-institutional approach may help overcome bias from a single-center analysis. Also, our patient collective features certain clinical characteristics that are consistent with those of larger studies.
In summary, we could provide evidence for the occurrence of patients who have maintained an initial CR even after cessation of TT. Our data indicate that patients who have initially received at least 16 months of TT, and who did not have to discontinue TT due to PD or toxicity are more likely to obtain a long-term response. The observation that treatment cessation due to toxicity is associated with a short PFS further suggests that treatment discontinuation due to toxicity should be avoided and toxicity control should be considered an important element of BRAF/MEK-directed TT not least with respect to the patients’ quality of life. The retrospective design of our study, however, does not allow for a reliable prediction of patients who will obtain long-term benefit and with no prospective data available to guide treatment decisions, stopping BRAF/MEKi therapy in CR cannot be recommended. Thus, prospective randomized clinical trials involving a tightly monitored discontinuation of TT with further translational end-points might further clarify the issue for whom it would be safe to cease treatment at which time point. Notably, recruitment and ethics of such study might be difficult since the occurrence of disease progression has been found to significantly worsen a subsequent reinduction of treatment.
Based on our data, it might however be conceivable to conduct further studies on BRAF ± MEKi treatment cessation in patients who have initially obtained a CR, show good prognostic clinical features, who have received TT for at least 16 months without showing disease relapse and who have not discontinued treatment due to PD or treatment-associated toxicities. During the first 6 months of subsequent treatment discontinuation, we further suggest a close clinical monitoring allowing for the rechallenge of BRAF± MEKi therapy in case of disease recurrence. The data presented here should assist clinicians to make informed and individualized decisions, taking into consideration the risks and chances (e.g., avoidance of cumulative side effects, paradoxical secondary malignancies) of treatment cessation, while patients that do not fit the outlined criteria should remain on treatment, as our data has unequivocally confirmed that patients who continued TT have the longest PFS and OS.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/cancers13102312/s1, Figure S1: Initial duration of BRAF/MEKi-directed targeted therapy is correlated with the overall survival in complete responders; Figure S2: Patients with an initial CR ceasing BRAF/MEKi-directed targeted therapy have a shorter overall survival; Figure S3: Patients maintaining their CR for a longer time interval after treatment cessation have a better progression-free and overall survival; Figure S4: Progression-free and overall survival in patients receiving second line ICI treatment subsequent to tumor progression during first line BRAF/MEKi treatment.
Author Contributions
Writing and editing by H.S., M.H., M.S., M.I.F., C.L. and S.G.; Methodology, software, validation, formal analysis, funding acquisition and illustration of tables and figures by M.H. and H.S.; Conceptualization: H.S., M.H. and C.L.; Project administration: C.L; Supervision by S.G. and C.L. Data acquisition: P.M., F.M., D.S., S.U., E.L., L.Z., R.H., C.P., K.K., M.W., P.T., D.N., D.D., M.K., F.Z., S.H., A.F., U.L., A.K., J.U., J.K., F.B. and C.L. All authors have read and agreed to the published version of the manuscript.
Funding
H.S. and M.H. are supported by an intramural research funding of the UMC Mainz. M.H. supported by the Clinician Scientist Fellowship “TransMed Jumpstart Program: 2019_A72” supported by the Else Kröner Fresenius Foundation.
Institutional Review Board Statement
The ADOREG registry was approved by the ethics committee of the University Duisburg-Essen (14-5921-BO), and provides real-world data from skin cancer patients of clinical centers of the DeCOG. The analysis of the anonymized retrospective data from the ADOReg registry was conducted according to the guidelines of the Declaration of Helsinki.
Informed Consent Statement
Informed consent was waived due to the anonymized collection of retrospective patient data within the ADOReg framework.
Data Availability Statement
All relevant data are within the manuscript and its supporting Tables and Figures. The retrospective data used for statistics have been collected within the framework of the ADOReg.
Conflicts of Interest
H.S., M.H., M.S., M.F., F.B., J.K., A.K., M.W. declare no conflict of interest. P.M. declares research support from Bristol Myers Squibb, Merck Sharp & Dohme and Novartis; speakers and advisory board honoraria from Amgen, Almirall Hermal, Bristol Myers Squibb, GlaxoSmithKline, Merck Sharp & Dohme, Merck Serono, Novartis, Pierre Fabre, Roche and Sanofi, and travel support from Bristol Myers Squibb, and Merck Sharp & Dohme, Novartis, Pierre Fabre, Amgen and Roche. S.H. served in advisory boards of Pierre Fabre, MSD, BMS, Novartis and Sanofi and received research project funding from BMS and Novartis outside the submitted work. D.N. served as consultant and payed referee to MSD, BMS, Novartis, Roche, Almirall Hermal, Mylan and Sanofi outside the submitted work. S.U. declares research support from Bristol Myers Squibb and Merck Serono; speakers and advisory board honoraria from Bristol Myers Squibb, Merck Sharp & Dohme, Merck Serono, Novartis and Roche, and travel support from Bristol Myers Squibb, and Merck Sharp & Dohme. D.S. declares relevant Honoria outside of this work from Roche, Novartis, Bristol-Myers Squibb, Merck Sharp & Dohme, Merck-Serono, Sanofi, Regeneron, Array, Pierre-Fabre, Pfizer, 4SC, Helsinn, Philogen, InFlarX, Amgen, SunPharma, Ultimovacs and Sandoz. E.L. served as consultant and/or has received honoraria from Amgen, Actelion, Roche, Bristol-Myers Squibb, Merck Sharp & Dohme, Novartis, Janssen, Medac, Sanofi, Sunpharma and travel support from Amgen, Merck Sharp & Dohme, Bristol-Myers Squibb, Amgen, Pierre Fabre, Sunpharma and Novartis, outside the submitted work. L.Z. declares honoria from Roche, BMS, MSD, Novartis, Pierre Fabre, consultant or advisory role honoria from BMS, Novartis, Pierre Fabre, Sunpharma, Sanofi and MSD, research funding from Novartis and travel support from BMS, Pierre Fabre, Sanofi, Amgen, Novartis and Sunpharma. U.L. declares research support from Merck Sharp & Dome; speakers and advisory board Honoria from Merck Sharp & Dome, Novartis Sun Pharma, Almirall Hemal, Sanofi and Roche outside the submitted work. A.F. served as a consultant to Roche, Novartis, MSD, BMS, Pierre-Fabre; received travel support from Roche, Novartis, BMS, Pierre-Fabre, and received speaker fees from Roche, Novartis, BMS, MSD and CeGAT, and reports institutional research grants from BMS Stiftung Immunonkologie. R.H. declares speakers and advisory board honoraria from Bristol Myers Squibb, Merck Sharp & Dohme, Novartis, Pierre Fabre, Roche and SUN-Pharma outside the submitted work. C.P. received honoraria (speaker honoraria or honoraria as a consultant) and travel support from: Novartis, BMS, Roche, Merck Serono, MSD, Celgene, AbbVie, Amgen, SUNPHARMA, Allergy Therapeutics and LEO. J.U. declares research support from Novartis, speakers and advisory board Honoria from BMS, MSD, Novartis, Pierre Fabre, Roche, Sanofi and Sun Pharma, and travel support from BMS, Medac and Sun Pharma outside the submitted work. F.M. has received travel support or/and speaker’s fees or/and advisor’s honoraria by Novartis, Roche, BMS, MSD and Pierre Fabre and research funding from Novartis and Roche. D.D. declares speakers and advisory board Honoria and/or travel support from BMS, MSD, Novartis, Pierre Fabre and Roche outside the submitted work. K.C.K. has served as consultant or/and has received Honoria from Amgen, Roche, BMS, MSD, Pierre Fabre and Novartis, and received travel support from Amgen, MSD, BMS, Pierre Fabre, Medac and Novartis. M.K. declares research support from Roche, MSD, BMS, Lilly, Sun Pharma, Novartis and lecture Honoria from MSD, BMS, Roche, Sun pharma and Novartis outside the submitted work. P.T. declares speaker’s honoraria from BMS, Novartis, MSD, Pierre-Fabre, CureVac and Roche, consultant’s honoraria from BMS, Novartis, Pierre-Fabre, Merck Serono, Sanofi und Roche and travel support from BMS, Pierre-Fabre and Roche. F.Z. declares personal fees outside the submitted work from Bristol-Myers Squibb GmbH & Co KG, Munich; MSD SHARP & DOHME GmbH, Haar; Roche Pharma AG, Grenzach-Wyhlen; GlaxoSmithKline GmbH & Co KG, Munich; Sanofi-Aventis GmbH, Berlin; Novartis Pharma GmbH, Nürnberg. S.G. declares honoraria for advisory boards, oral presentations and travel expenses from Roche, Novartis, MSD, and BMS outside the submitted work. C.L. declares speakers, advisory board honoraria and travel support from Bristol Myers Squibb, Merck Sharp and Dohme, Merck Serono, Novartis, Roche, Pierre Fabre, Sun Pharma, Kiowa Kirin, Sanofi, Biontech, Almirall Hermal outside the submitted work.
References
- Chapman, P.B.; Hauschild, A.; Robert, C.; Haanen, J.B.; Ascierto, P.; Larkin, J.; Dummer, R.; Garbe, C.; Testori, A.; Maio, M.; et al. Improved survival with vemurafenib in melanoma with BRAF V600E mutation. N. Engl. J. Med. 2011, 364, 2507–2516. [Google Scholar] [CrossRef]
- McArthur, G.A.; Chapman, P.B.; Robert, C.; Larkin, J.; Haanen, J.B.; Dummer, R.; Ribas, A.; Hogg, D.; Hamid, O.; Ascierto, P.A.; et al. Safety and efficacy of vemurafenib in BRAF(V600E) and BRAF(V600K) mutation-positive melanoma (BRIM-3): Extended follow-up of a phase 3, randomised, open-label study. Lancet Oncol. 2014, 15, 323–332. [Google Scholar] [CrossRef]
- Long, G.V.; Flaherty, K.T.; Stroyakovskiy, D.; Gogas, H.; Levchenko, E.; de Braud, F.; Larkin, J.; Garbe, C.; Jouary, T.; Hauschild, A.; et al. Dabrafenib plus trametinib versus dabrafenib monotherapy in patients with metastatic BRAF V600E/K-mutant melanoma: Long-term survival and safety analysis of a phase 3 study. Ann. Oncol. 2017, 28, 1631–1639. [Google Scholar] [CrossRef] [PubMed]
- Hauschild, A.; Grob, J.J.; Demidov, L.V.; Jouary, T.; Gutzmer, R.; Millward, M.; Rutkowski, P.; Blank, C.U.; Miller, W.H., Jr.; Kaempgen, E.; et al. Dabrafenib in BRAF-mutated metastatic melanoma: A multicentre, open-label, phase 3 randomised controlled trial. Lancet 2012, 380, 358–365. [Google Scholar] [CrossRef]
- Larkin, J.; Del Vecchio, M.; Ascierto, P.A.; Krajsova, I.; Schachter, J.; Neyns, B.; Espinosa, E.; Garbe, C.; Sileni, V.C.; Gogas, H.; et al. Vemurafenib in patients with BRAF(V600) mutated metastatic melanoma: An open-label, multicentre, safety study. Lancet Oncol. 2014, 15, 436–444. [Google Scholar] [CrossRef]
- Larkin, J.; Chiarion-Sileni, V.; Gonzalez, R.; Grob, J.J.; Rutkowski, P.; Lao, C.D.; Cowey, C.L.; Schadendorf, D.; Wagstaff, J.; Dummer, R.; et al. Five-Year Survival with Combined Nivolumab and Ipilimumab in Advanced Melanoma. N. Engl. J. Med. 2019, 381, 1535–1546. [Google Scholar] [CrossRef] [PubMed]
- Johnson, D.B.; Peng, C.; Sosman, J.A. Nivolumab in melanoma: Latest evidence and clinical potential. Ther. Adv. Med. Oncol. 2015, 7, 97–106. [Google Scholar] [CrossRef]
- Maio, M.; Grob, J.J.; Aamdal, S.; Bondarenko, I.; Robert, C.; Thomas, L.; Garbe, C.; Chiarion-Sileni, V.; Testori, A.; Chen, T.T.; et al. Five-year survival rates for treatment-naive patients with advanced melanoma who received ipilimumab plus dacarbazine in a phase III trial. J. Clin. Oncol. 2015, 33, 1191–1196. [Google Scholar] [CrossRef] [PubMed]
- Barth, A.; Wanek, L.A.; Morton, D.L. Prognostic factors in 1521 melanoma patients with distant metastases. J. Am. Coll. Surg. 1995, 181, 193–201. [Google Scholar]
- Eberlein, T.J. Prognosis of patients with advanced melanoma. J. Am. Coll. Surg. 1995, 181, 263–265. [Google Scholar]
- Davies, H.; Bignell, G.R.; Cox, C.; Stephens, P.; Edkins, S.; Clegg, S.; Teague, J.; Woffendin, H.; Garnett, M.J.; Bottomley, W.; et al. Mutations of the BRAF gene in human cancer. Nature 2002, 417, 949–954. [Google Scholar] [CrossRef]
- Ascierto, P.A.; Kirkwood, J.M.; Grob, J.J.; Simeone, E.; Grimaldi, A.M.; Maio, M.; Palmieri, G.; Testori, A.; Marincola, F.M.; Mozzillo, N. The role of BRAF V600 mutation in melanoma. J. Transl. Med. 2012, 10, 85. [Google Scholar] [CrossRef] [PubMed]
- Croce, L.; Coperchini, F.; Magri, F.; Chiovato, L.; Rotondi, M. The multifaceted anti-cancer effects of BRAF-inhibitors. Oncotarget 2019, 10, 6623–6640. [Google Scholar] [CrossRef] [PubMed]
- Shi, H.; Hong, A.; Kong, X.; Koya, R.C.; Song, C.; Moriceau, G.; Hugo, W.; Yu, C.C.; Ng, C.; Chodon, T.; et al. A novel AKT1 mutant amplifies an adaptive melanoma response to BRAF inhibition. Cancer Discov. 2014, 4, 69–79. [Google Scholar] [CrossRef]
- Vido, M.J.; Le, K.; Hartsough, E.J.; Aplin, A.E. BRAF Splice Variant Resistance to RAF Inhibitor Requires Enhanced MEK Association. Cell Rep. 2018, 25, 1501–1510.e1503. [Google Scholar] [CrossRef]
- Van Allen, E.M.; Wagle, N.; Sucker, A.; Treacy, D.J.; Johannessen, C.M.; Goetz, E.M.; Place, C.S.; Taylor-Weiner, A.; Whittaker, S.; Kryukov, G.V.; et al. The genetic landscape of clinical resistance to RAF inhibition in metastatic melanoma. Cancer Discov. 2014, 4, 94–109. [Google Scholar] [CrossRef] [PubMed]
- Ribas, A.; Daud, A.; Pavlick, A.C.; Gonzalez, R.; Lewis, K.D.; Hamid, O.; Gajewski, T.F.; Puzanov, I.; Wongchenko, M.; Rooney, I.; et al. Extended 5-Year Follow-up Results of a Phase Ib Study (BRIM7) of Vemurafenib and Cobimetinib in BRAF-Mutant Melanoma. Clin. Cancer Res. 2020, 26, 46–53. [Google Scholar] [CrossRef]
- Dummer, R.; Ascierto, P.A.; Gogas, H.J.; Arance, A.; Mandala, M.; Liszkay, G.; Garbe, C.; Schadendorf, D.; Krajsova, I.; Gutzmer, R.; et al. Encorafenib plus binimetinib versus vemurafenib or encorafenib in patients with BRAF-mutant melanoma (COLUMBUS): A multicentre, open-label, randomised phase 3 trial. Lancet Oncol. 2018, 19, 603–615. [Google Scholar] [CrossRef]
- Robert, C.; Grob, J.J.; Stroyakovskiy, D.; Karaszewska, B.; Hauschild, A.; Levchenko, E.; Chiarion Sileni, V.; Schachter, J.; Garbe, C.; Bondarenko, I.; et al. Five-Year Outcomes with Dabrafenib plus Trametinib in Metastatic Melanoma. N. Engl. J. Med. 2019, 381, 626–636. [Google Scholar] [CrossRef]
- Schummer, P.; Schilling, B.; Gesierich, A. Long-Term Outcomes in BRAF-Mutated Melanoma Treated with Combined Targeted Therapy or Immune Checkpoint Blockade: Are We Approaching a True Cure? Am. J. Clin. Dermatol. 2020, 21, 493–504. [Google Scholar] [CrossRef]
- Long, G.V.; Stroyakovskiy, D.; Gogas, H.; Levchenko, E.; de Braud, F.; Larkin, J.; Garbe, C.; Jouary, T.; Hauschild, A.; Grob, J.J.; et al. Combined BRAF and MEK inhibition versus BRAF inhibition alone in melanoma. N. Engl. J. Med. 2014, 371, 1877–1888. [Google Scholar] [CrossRef]
- Carlino, M.S.; Vanella, V.; Girgis, C.; Giannarelli, D.; Guminski, A.; Festino, L.; Kefford, R.F.; Menzies, A.M.; Long, G.V.; Ascierto, P.A. Cessation of targeted therapy after a complete response in BRAF-mutant advanced melanoma: A case series. Br. J. Cancer 2016, 115, 1280–1284. [Google Scholar] [CrossRef] [PubMed]
- Heinzerling, L.; Eigentler, T.K.; Fluck, M.; Hassel, J.C.; Heller-Schenck, D.; Leipe, J.; Pauschinger, M.; Vogel, A.; Zimmer, L.; Gutzmer, R. Tolerability of BRAF/MEK inhibitor combinations: Adverse event evaluation and management. ESMO Open 2019, 4, e000491. [Google Scholar] [CrossRef]
- Greco, A.; Safi, D.; Swami, U.; Ginader, T.; Milhem, M.; Zakharia, Y. Efficacy and Adverse Events in Metastatic Melanoma Patients Treated with Combination BRAF Plus MEK Inhibitors Versus BRAF Inhibitors: A Systematic Review. Cancers 2019, 11, 1950. [Google Scholar] [CrossRef]
- Menzies, A.M.; Kefford, R.F.; Long, G.V. Paradoxical oncogenesis: Are all BRAF inhibitors equal? Pigment Cell Melanoma Res. 2013, 26, 611–615. [Google Scholar] [CrossRef]
- Escuin-Ordinas, H.; Li, S.; Xie, M.W.; Sun, L.; Hugo, W.; Huang, R.R.; Jiao, J.; de-Faria, F.M.; Realegeno, S.; Krystofinski, P.; et al. Cutaneous wound healing through paradoxical MAPK activation by BRAF inhibitors. Nat. Commun. 2016, 7, 12348. [Google Scholar] [CrossRef]
- Cherobin, A.; Wainstein, A.J.A.; Colosimo, E.A.; Goulart, E.M.A.; Bittencourt, F.V. Prognostic factors for metastasis in cutaneous melanoma. An. Bras. Dermatol. 2018, 93, 19–26. [Google Scholar] [CrossRef]
- Kim, J.E.; Chung, B.Y.; Sim, C.Y.; Park, A.Y.; Lee, J.S.; Whang, K.U.; Park, Y.L.; Kim, H.O.; Park, C.W.; Lee, S.Y. Clinicopathologic Features and Prognostic Factors of Primary Cutaneous Melanoma: A Multicenter Study in Korea. J. Korean Med. Sci. 2019, 34, e126. [Google Scholar] [CrossRef] [PubMed]
- Menzies, A.M.; Wilmott, J.S.; Drummond, M.; Lo, S.; Lyle, M.; Chan, M.M.; Thompson, J.F.; Guminski, A.; Carlino, M.S.; Scolyer, R.A.; et al. Clinicopathologic features associated with efficacy and long-term survival in metastatic melanoma patients treated with BRAF or combined BRAF and MEK inhibitors. Cancer 2015, 121, 3826–3835. [Google Scholar] [CrossRef] [PubMed]
- Ascierto, P.A.; Ribas, A.; Larkin, J.; McArthur, G.A.; Lewis, K.D.; Hauschild, A.; Flaherty, K.T.; McKenna, E.; Zhu, Q.; Mun, Y.; et al. Impact of initial treatment and prognostic factors on postprogression survival in BRAF-mutated metastatic melanoma treated with dacarbazine or vemurafenib +/− cobimetinib: A pooled analysis of four clinical trials. J. Transl. Med. 2020, 18, 294. [Google Scholar] [CrossRef]
- Warburton, L.; Meniawy, T.M.; Calapre, L.; Pereira, M.; McEvoy, A.; Ziman, M.; Gray, E.S.; Millward, M. Stopping targeted therapy for complete responders in advanced BRAF mutant melanoma. Sci. Rep. 2020, 10, 18878. [Google Scholar] [CrossRef]
- Desvignes, C.; Abi Rached, H.; Templier, C.; Drumez, E.; Lepesant, P.; Desmedt, E.; Mortier, L. BRAF inhibitor discontinuation and rechallenge in advanced melanoma patients with a complete initial treatment response. Melanoma Res. 2017, 27, 281–287. [Google Scholar] [CrossRef] [PubMed]
- Vanhaecke, C.; Deilhes, F.; Chanal, J.; Regnier-Rosencher, E.; Boitier, F.; Boulinguez, S.; Avril, M.F.; Guégan, S.; Dupin, N.; Aractingi, S.; et al. BRAF V600 inhibitor discontinuation after complete response in advanced melanoma: A retrospective analysis of 16 patients. Br. J. Dermatol. 2017, 177, e94–e95. [Google Scholar] [CrossRef]
- Wyluda, E.J.; Cheng, J.; Schell, T.D.; Haley, J.S.; Mallon, C.; Neves, R.I.; Robertson, G.; Sivik, J.; Mackley, H.; Talamo, G.; et al. Durable complete responses off all treatment in patients with metastatic malignant melanoma after sequential immunotherapy followed by a finite course of BRAF inhibitor therapy. Cancer Biol. Ther. 2015, 16, 662–670. [Google Scholar] [CrossRef]
- Tolk, H.; Satzger, I.; Mohr, P.; Zimmer, L.; Weide, B.; Schad, S.; Gutzmer, R. Complete remission of metastatic melanoma upon BRAF inhibitor treatment—What happens after discontinuation? Melanoma Res. 2015, 25, 362–366. [Google Scholar] [CrossRef]
- Ascierto, P.A.; Dummer, R. Immunological effects of BRAF+MEK inhibition. Oncoimmunology 2018, 7, e1468955. [Google Scholar] [CrossRef]
- Kuske, M.; Westphal, D.; Wehner, R.; Schmitz, M.; Beissert, S.; Praetorius, C.; Meier, F. Immunomodulatory effects of BRAF and MEK inhibitors: Implications for Melanoma therapy. Pharmacol. Res. 2018, 136, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Dearden, H.C.; Mason, R.; Nguyen, B.; Soon, J.A.; Smith, J.L.; Randhawa, M.; Mant, A.; Warburton, L.; Lo, S.; Meniawy, T.; et al. Combined ipilimumab and nivolumab first-line and after BRAF-directed targeted therapies in advanced melanoma patients. Ann. Oncol. 2018, 29. [Google Scholar] [CrossRef]
- van Willigen, W.W.; Bloemendal, M.; Boers-Sonderen, M.J.; de Groot, J.W.B.; Koornstra, R.H.T.; van der Veldt, A.A.M.; Haanen, J.; Boudewijns, S.; Schreibelt, G.; Gerritsen, W.R.; et al. Response and survival of metastatic melanoma patients treated with immune checkpoint inhibition for recurrent disease on adjuvant dendritic cell vaccination. Oncoimmunology 2020, 9, 1738814. [Google Scholar] [CrossRef]
- Kreft, S.; Gesierich, A.; Eigentler, T.; Franklin, C.; Valpione, S.; Ugurel, S.; Utikal, J.; Haferkamp, S.; Blank, C.; Larkin, J.; et al. Efficacy of PD-1-based immunotherapy after radiologic progression on targeted therapy in stage IV melanoma. Eur. J. Cancer 2019, 116, 207–215. [Google Scholar] [CrossRef] [PubMed]
- Ascierto, P.A.; Margolin, K. Ipilimumab before BRAF inhibitor treatment may be more beneficial than vice versa for the majority of patients with advanced melanoma. Cancer 2014, 120, 1617–1619. [Google Scholar] [CrossRef]
- Ascierto, P.A.; Simeone, E.; Sileni, V.C.; Del Vecchio, M.; Marchetti, P.; Cappellini, G.C.; Ridolfi, R.; de Rosa, F.; Cognetti, F.; Ferraresi, V.; et al. Sequential treatment with ipilimumab and BRAF inhibitors in patients with metastatic melanoma: Data from the Italian cohort of the ipilimumab expanded access program. Cancer Investig. 2014, 32, 144–149. [Google Scholar] [CrossRef] [PubMed]
- Scholtens, A.; Geukes Foppen, M.H.; Blank, C.U.; van Thienen, J.V.; van Tinteren, H.; Haanen, J.B. Vemurafenib for BRAF V600 mutated advanced melanoma: Results of treatment beyond progression. Eur. J. Cancer 2015, 51, 642–652. [Google Scholar] [CrossRef] [PubMed]
- Cooper, Z.A.; Reuben, A.; Spencer, C.N.; Prieto, P.A.; Austin-Breneman, J.L.; Jiang, H.; Haymaker, C.; Gopalakrishnan, V.; Tetzlaff, M.T.; Frederick, D.T.; et al. Distinct clinical patterns and immune infiltrates are observed at time of progression on targeted therapy versus immune checkpoint blockade for melanoma. Oncoimmunology 2016, 5, e1136044. [Google Scholar] [CrossRef] [PubMed]
- Cooper, Z.A.; Juneja, V.R.; Sage, P.T.; Frederick, D.T.; Piris, A.; Mitra, D.; Lo, J.A.; Hodi, F.S.; Freeman, G.J.; Bosenberg, M.W.; et al. Response to BRAF inhibition in melanoma is enhanced when combined with immune checkpoint blockade. Cancer Immunol. Res. 2014, 2, 643–654. [Google Scholar] [CrossRef]
- Kakavand, H.; Wilmott, J.S.; Menzies, A.M.; Vilain, R.; Haydu, L.E.; Yearley, J.H.; Thompson, J.F.; Kefford, R.F.; Hersey, P.; Long, G.V.; et al. PD-L1 Expression and Tumor-Infiltrating Lymphocytes Define Different Subsets of MAPK Inhibitor-Treated Melanoma Patients. Clin. Cancer Res. 2015, 21, 3140–3148. [Google Scholar] [CrossRef]
- Massi, D.; Romano, E.; Rulli, E.; Merelli, B.; Nassini, R.; De Logu, F.; Bieche, I.; Baroni, G.; Cattaneo, L.; Xue, G.; et al. Baseline beta-catenin, programmed death-ligand 1 expression and tumour-infiltrating lymphocytes predict response and poor prognosis in BRAF inhibitor-treated melanoma patients. Eur. J. Cancer 2017, 78, 70–81. [Google Scholar] [CrossRef]
- Shi, H.; Hugo, W.; Kong, X.; Hong, A.; Koya, R.C.; Moriceau, G.; Chodon, T.; Guo, R.; Johnson, D.B.; Dahlman, K.B.; et al. Acquired resistance and clonal evolution in melanoma during BRAF inhibitor therapy. Cancer Discov. 2014, 4, 80–93. [Google Scholar] [CrossRef]
- Smith, M.P.; Brunton, H.; Rowling, E.J.; Ferguson, J.; Arozarena, I.; Miskolczi, Z.; Lee, J.L.; Girotti, M.R.; Marais, R.; Levesque, M.P.; et al. Inhibiting Drivers of Non-mutational Drug Tolerance Is a Salvage Strategy for Targeted Melanoma Therapy. Cancer Cell 2016, 29, 270–284. [Google Scholar] [CrossRef]
- Girotti, M.R.; Lopes, F.; Preece, N.; Niculescu-Duvaz, D.; Zambon, A.; Davies, L.; Whittaker, S.; Saturno, G.; Viros, A.; Pedersen, M.; et al. Paradox-breaking RAF inhibitors that also target SRC are effective in drug-resistant BRAF mutant melanoma. Cancer Cell 2015, 27, 85–96. [Google Scholar] [CrossRef]
- Valpione, S.; Carlino, M.S.; Mangana, J.; Mooradian, M.J.; McArthur, G.; Schadendorf, D.; Hauschild, A.; Menzies, A.M.; Arance, A.; Ascierto, P.A.; et al. Rechallenge with BRAF-directed treatment in metastatic melanoma: A multi-institutional retrospective study. Eur. J. Cancer 2018, 91, 116–124. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).