Abstract
Rising healthcare costs force healthcare organizations worldwide to reconsider their business strategies. Hospital managers are tasked with lowering operating costs while upholding the high quality of care, two goals perceived as contradictory by many healthcare professionals. Attempting to contribute towards reaching these goals, the study explores the digitalization of the healthcare supply chain through the adoption of enterprise resource planning (ERP) systems and its impact on hospital supply chain costs. Established technology adoption theories are synthesized to develop a research model that investigates the adoption of hospital ERP systems and its impact on supply chain cost performance. The framework is validated via structural equation modeling (SEM) with data collected from 107 Greek public hospitals. The results indicate that technological and organizational readiness, hospital size, governmental policies, and perceived benefits have a significant influence on the extent of ERP systems adoption. They also demonstrate a statistically significant association between the use of ERP systems and hospital supply chain costs. The present study highlights the influencing factors of ERP systems adoption in hospitals and provides empirical evidence on the resulting cost benefits., This implies greater urgency for hospitals to digitalize their supply chain by implementing and fully exploiting the ERP systems’ functionality in order to reach their goal of delivering quality care at a lower cost.
1. Introduction
Public healthcare spending cuts force healthcare organizations worldwide to reduce their operating costs while being required to ensure the quality of care. One of the focal points is the healthcare supply chain, which can be defined as a complex system managing the flow of products, services, and information to satisfy the needs of those who serve patients []. Supply chain costs are estimated to account for 40 to 50% of a healthcare provider’s total costs [], suggesting that supply chain performance improvement could be a major enabler for increasing the operational efficiency and reducing costs [].
While other sectors deploy various supply chain management (SCM) practices to lower their supply chain costs, the healthcare sector is clearly lagging behind []. Some scholars attribute this fact to the relative complexity of healthcare supply chains due to (1) the existence of strong national and international regulatory frameworks, (2) the difficulty of demand forecasting because of patient heterogeneity, and (3) limited SCM knowledge by pharmacists and physicians who are key decision-makers regarding the procurement of drugs []. The relatively low adoption rate of enterprise resource planning (ERP) systems that support the management of hospital supply chains might be an additional reason []. The hospital supply chain encompasses the process of procuring, manufacturing, and delivering goods and services from providers to patients, including medical and non-medical products, such as pharmaceuticals, medical devices, food, and cleaning supplies. Effective coordination and communication among various partners are essential for ensuring optimal patient care and safety. The financial flows are closely linked to the supply chain’s product and information flow, which can be effectively managed by utilizing ERP systems []. ERP systems are comprehensive software applications designed to integrate the main functional areas of an organization’s business processes and are known to impact the adoption of SCM practices significantly []. Despite their importance in making hospitals more efficient and deliver their services more promptly, research studies involving the digitalization of healthcare supply chains and ERP implementations in healthcare are sparse. For example, a study of ERP adoption cases in healthcare organizations by Poba-Nzaou et al. [] found only three empirical studies examining ERP implementation in healthcare facilities.
Within this context, the present study aims to develop a conceptual framework to investigate ERP systems adoption in healthcare settings and empirically validate their contribution towards reducing healthcare supply chain costs. To study the adoption of various technologies and innovations in general, a plethora of models and variations or combinations of these models have been suggested in the literature, such as (1) the technology–organization–environment (TOE) framework, (2) the technology acceptance model (TAM), (3) theory of planned behavior (TPB), (4) the innovation diffusion theory (IDT), (5) unified theory of acceptance and use of technology (UTAUT), and (6) the human organization and technology fit (HOT-fit). The TOE theory focuses specifically on technology acceptance and follows an integrative approach by complementing technology-oriented determinants of adoption with organizational and environmental constructs. It identifies three aspects of a firm’s context that may influence the adoption of technological innovation: (1) the technological context, which reflects both the existing IT infrastructure and IT expertise; (2) the organizational context, which relates to characteristics of the organization, such as organizational culture and size; and (3) the environmental context, which describes the framework in which an organization conducts its business, referring mainly to its business partners, its competitors and its interactions with the government.
The literature search revealed that the TOE framework could form a suitable basis for investigating the adoption of ERP systems as it has received consistent empirical support within various business sectors, including the healthcare sector [,]. However, questioning whether a single theoretical model can sufficiently examine the adoption and diffusion of various technologies in different business settings, this research aims at expanding this framework to increase its explanatory and predictive power. Therefore, a synthesized framework that combines the established theoretical lens of the TOE model with the theory of perceived benefits is proposed and expanded by a performance component. Several weaknesses identified by other scholars as part of previous technology adoption studies [] were addressed during the development of the proposed synthesized framework. The study’s research framework has distinct advantages compared to other frameworks used in the past as it (a) expands existing models through the inclusion of new constructs, (b) incorporates both organizational characteristics and personal belief components, and (c) emphasizes the extent of technology adoption, rather than treating adoption as a dichotomous (yes/no) variable.
2. Research Framework and Hypotheses Development
The resulting theoretical framework serves as a foundation that guides the understanding, explanation, and prediction of the extent of ERP systems adoption in hospitals and their impact on hospital supply chain costs. This is enabled through the inclusion of the following six dimensions: (1) technological context, (2) organizational context, (3) environmental context, (4) perceived benefits, (5) extent of ERP systems adoption, and (6) hospital supply chain costs.
2.1. Technological Context of ERP Systems Adoption in Hospitals
The technological context of the conceptual framework is represented by the hospital’s technological readiness, which comprises IT infrastructure and IT expertise [,]. IT infrastructure establishes a platform that provides the foundation for implementing ERP systems, and IT expertise entails the knowledge and skills to implement ERP systems. Research has shown that firms with sophisticated IT infrastructure and skilled IT resources have increased chances of successfully implementing technology innovations []. Accordingly, the first hypothesis is postulated:
H1.
The extent of ERP systems adoption in hospital supply chains is positively affected by technological readiness.
2.2. Organizational Context of ERP Systems Adoption in Hospitals
Various organizational factors have been suggested to impact innovation and technology adoption. One factor in many technology adoption studies is organizational readiness, which reflects an organization’s internal capability to accept new technologies []. Organizational readiness is impacted by the organization’s culture and the availability of skilled, knowledgeable, and well-trained resources regarding new technologies []. An additional aspect of organizational readiness considered crucial in many IT adoption studies is top management support and commitment, as it is necessary to ensure adequate resources and to overcome barriers and resistance to change inherent in the organization []. Therefore, the second hypothesis is formed:
H2.
The extent of ERP systems adoption in hospital supply chains is positively impacted by organizational readiness.
The organization’s size constitutes one of the most commonly researched variables in the organizational context. However, there has been some disagreement regarding the direction of the relationship. Some scholars have suggested that smaller organizations are more likely to be innovative since a smaller size translates into a higher flexibility and less bureaucracy []. More studies, however, conclude that the organization’s size positively impacts innovation [] since larger organizations are more likely to have the financial resources to invest in new technologies and absorb the associated risks [,]. Thus, the third hypothesis is proposed:
H3.
The extent of ERP systems adoption in hospital supply chains is positively affected by hospital size.
2.3. Environmental Context of ERP Systems Adoption in Hospitals
The environmental context refers to influencing factors from the external environment in which an organization conducts its business. This study will focus on two key environmental variables, considered the most important for ERP systems adoption in healthcare institutions: business partner influence and government influence. The environmental factor of competitive pressure, which is included in many TOE-based studies, was not incorporated into the model, as Greek public hospitals operate in a nonmarket environment [].
Pressure from supply chain partners and government influence constitute environmental factors that may influence an organization’s adoption of technologies. Suppliers may advocate certain technologies and suggest their adoption or even use their power and influence to pressure their business partners to do so []. Governments can provide incentives or even mandate technology adoption, especially in highly regulated sectors, such as healthcare. Hence, the fourth and fifth hypotheses are set:
H4.
The extent of ERP systems adoption in hospital supply chains is positively affected by business partner readiness.
H5.
The extent of ERP systems adoption in hospital supply chains is positively affected by government policies.
2.4. Impact of the Perceived Benefits on the Extent of ERP Systems Adoption
Perceived benefits, also referred to as “relative advantage” in classical innovation literature, relate to the anticipated advantages that ERP systems adoption can provide to the organization. Perceived benefits are associated with direct and indirect benefits, such as inventory cost reductions, improved patient safety, and quality of care, respectively. Although other studies chose to incorporate perceived benefits in their technological or organizational contexts, other scholars’ approaches were followed, such as Gibbs and Kraemer [] and Oliveira and Martins []. They treated perceived benefits as a separate construct since they represent the decision-makers’ personal beliefs rather than reflect the organization’s attributes. Thus, the sixth hypothesis is postulated:
H6.
The extent of ERP systems adoption in hospital supply chains is positively affected by perceived benefits.
2.5. Impact of ERP Systems Adoption on Hospital Supply Chain Costs
Several scholars have called for empirical evidence on the relationship between technology adoption and hospital performance []. Therefore, apart from studying the determinants of ERP systems adoption in hospitals, this research aimed to examine their impact in hospitals. Supply chain costs, encompassing costs related to the purchase, distribution, and management of supplies, are critical to improving the hospital cost performance as they account for about one-third of the operating costs of healthcare facilities []. Considering the global trends towards healthcare cost reductions and the fiscal policies aiming at public healthcare spending cuts, the focus was placed on the cost side of hospital performance. It should be noted that cost performance has to be used in concert with quality performance—including process, outcome, and patient experience—when assessing overall hospital performance. Therefore, the final hypothesis is proposed:
H7.
Hospital supply chain costs are positively affected by the extent of ERP systems adoption.
Figure 1 depicts the theoretical model with the associated hypotheses.
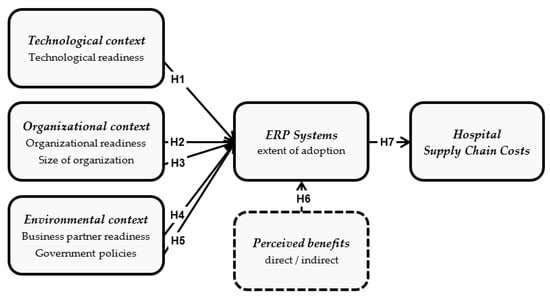
Figure 1.
Theoretical research framework.
3. Research Methodology
The theoretical underpinning of the research framework is followed by an explanation of the methodology employed to investigate the postulated hypotheses. The widely used survey research method was applied to collect the primary data needed for hypothesis testing. The scope of the study was concentrated on the Greek public healthcare sector, which provided a sufficient base considering it represents over 72% of the total Greek healthcare sector in terms of hospital bed capacity [].
The questionnaire developed to support the survey is divided into two parts. The first part relates to demographic information. The second part includes multiple items for measuring the model’s independent variables on a 5-point Likert scale (see Supplementary Materials). To increase confidence in the validity of the research findings, the hospital’s supply chain cost performance was evaluated using secondary data from a different source rather than relying on subjective estimates of the key informants. This provided a more fine-grained analysis and reduced the possibility of potential informant bias. To operationalize Greek public hospitals’ supply chain costs, the average supply chain costs per inpatient day were calculated using data from the Greek Ministry of Health’s business intelligence health portal []. Initially, the supply chain costs per patient were calculated by dividing the yearly total hospital supply chain costs by the number of hospitalized patients per year. The supply chain cost per patient is expectedly higher for hospitals treating more severe cases as they require longer lengths of patient stays; thus, this measure needed to be adjusted to be suitable for relative performance comparisons. Consequently, the average length of stay (ALOS), an indicator often used as an efficiency metric, was considered []. The supply chain cost per patient was divided by the ALOS to calculate the average supply chain cost per patient day. This was the metric used as a benchmark for the hospital’s supply chain cost performance per patient day.
Prior to final data collection, the questionnaire was piloted in three hospitals to test and examine the face validity. In most of the cases, the key informant selected was the inventory/storeroom manager (72%); in some cases, the procurement manager (22%), and in a few cases, the financial manager (6%). Due to their role as active mid-level managers of Greek public hospitals, characterized by flat hierarchical structures, they were expected to have a good understanding of the intra-organizational characteristics besides being knowledgeable about the issues under investigation. Of the 125 questionnaires handed out or sent out via email, 107 were filled out and returned, exceeding the initial expectations, as approximately 86% of the total population of public hospitals was covered.
Following the data collection, the possibility of non-response bias was investigated by examining the differences in the mean of all measured variables between early and late respondents. The rationale behind such an analysis is that late respondents are more similar to non-respondents than to early respondents []. No statistically significant differences were found, suggesting that non-response bias is not a serious issue for the study.
The objective of this study was not simply to provide a basic statistical analysis and identify individual factors and behaviors, but to uncover the causal relationships and connections among the areas of interest. To achieve this, advanced methods and techniques of statistical data analysis were necessary, specifically those related to causal analysis and the examination of multiple variables. Structural equation modeling (SEM) was chosen as the method of analysis for the study as it is a multivariate method used to test hypotheses regarding the influences among interacting variables and allows the testing of direct and indirect effects on pre-assumed causal relationships [].
4. Results
Following the collection of the data, structural equation modeling (SEM) using the AMOS 22.0 software [] was employed to analyze the data, following the two-step approach suggested by Anderson and Gerbing for the assessment of both measurement and structural components []. A confirmatory factor analysis (CFA) was applied to validate the conceptual soundness of the latent variables used in the structural model, to examine the variables and path relationships hypothesized in the study, and to further test the unidimensionality and reliability, as described by Hair et al. []. The final measurement model consists of five latent variables measured by multiple indicators. As suggested by Hair et al., the widely used absolute indices (measuring how well the hypothesized model reproduces the covariance matrix obtained from the sample data) and incremental indices (measuring how well the hypothesized model provides benefits beyond the worst-case model) were calculated, as reported in Table 1 []. Although the normed fit index (NFI), one of the incremental fit indices, is slightly below conventional levels, all other incremental indices are well above the recommended thresholds; thus, the measurement model results reflect the acceptable absolute and incremental measurement model fit, indicating unidimensionality, reliability, and model acceptability.
Then, the reliability and validity, particularly the constructs’ convergent and discriminant validity, were assessed. The reliability and the convergent validity were confirmed, as all five factors reached construct reliabilities (CRs) exceeding the generally recommended 0.70 threshold [] and (b) the average variances extracted (AVE) exceeding the suggested 0.50 threshold [], indicating that more than 50% of a factor’s variance is due to its measurement items. The discriminant validity was also supported, considering that the inter-factor correlations were less than the square root of the factor’s AVEs, as advocated by Fornell and Larcker and depicted in Table 2 [].

Table 2.
Construct reliabilities (CR), average variances extracted (AVE), and inter-factor correlations.

Table 1.
Goodness of fit measures.
Table 1.
Goodness of fit measures.
| The Goodness of Fit Indices | Recommended Value (Source) | Measurement Model Result | Structural Model Result |
|---|---|---|---|
| Absolute fit | |||
| χ2/df Chi-square/Degrees of freedom | <3.00 Jöreskog and Sörbom [] | 1.047 | 1.094 |
| GFI Goodness of Fit Index | >0.90 Jöreskog and Sörbom [] | 0.901 | 0.977 |
| AGFI Adjusted Goodness of Fit Index | >0.85 Jöreskog nd Sörbom [] | 0.851 | 0.932 |
| RMSEA Root Mean Square Error of Approximation | <0.05 Hu and Bentler [] | 0.022 | 0.031 |
| Incremental fit | |||
| IFI Incremental Fit Index | >0.95 Hu and Bentler [] | 0.993 | 0.997 |
| NFI Normed Fit Index | >0.90 Hu and Bentler [] | 0.864 | 0.948 |
| TLI (NNFI) Tucker Lewis Index | >0.95 Hu and Bentler [] | 0.990 | 0.975 |
| CFI Comparative Fit Index | >0.95 Hu and Bentler [] | 0.993 | 0.991 |
The study’s findings indicate that the analysis employed a well-explained factor structure and that the developed constructs can be used to test the conceptual model and the associated hypotheses. Following the positive assessment of the measurement model, the structural model was analyzed to test the hypotheses. Similarly to the measurement model, the previously outlined absolute and incremental indices were calculated. They all demonstrated results within the recommended ranges, as seen in Table 1. No post-hoc modifications were conducted as all calculated fit indices for the structural model indicated that the hypothesized model represents a good fit to the data.
As can be seen in Figure 2 and Table 3, support was found for hypotheses 1, 2, 3, 5, and 6, indicating that technological readiness, organizational readiness, organizational size, governmental policies, and perceived benefits have a direct positive impact on the extent of ERP systems adoption in hospital supply chains. In contrast, hypothesis 4 was not supported, suggesting that business partners do not significantly impact the extent of ERP systems adoption in hospital supply chains. Finally, hypothesis 7 was supported, indicating that the extent of ERP systems adoption in hospital supply chains has a significant direct positive impact on hospital supply chain costs. These results demonstrate the explanatory power of the research model. The r2 values show that technological readiness, organizational readiness, organizational size, governmental policies, and perceived benefits explain 44% of ERP systems adoption in hospital supply chains. In comparison, 15% of hospital supply chain costs can be attributed to ERP systems adoption. These results suggest some interesting interpretations, which will be discussed in the next section.
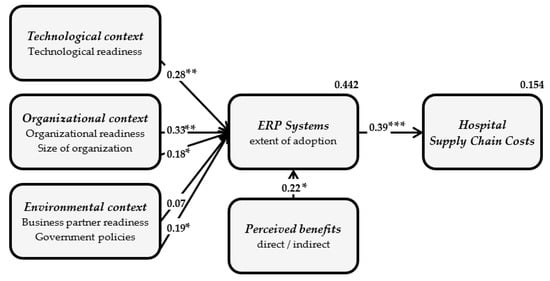
Figure 2.
Results of the hypotheses (* p < 0.05; ** p < 0.01; *** p < 0.001).

Table 3.
Results of the hypotheses.
5. Discussion
There seems to be a consensus about the added value ERP systems can have for the digitalization of healthcare organizations. However, it is mainly based on assertion rather than demonstration []. The main objective of the present study was to make this added value more explicit through performance metrics and investigate the conditions under which this added value emerges. Responding to calls for more theory-driven empirical research, the adoption of ERP systems and their impact on cost performance was examined by developing and empirically validating a conceptual framework that integrates the established theoretical lens of the TOE theory with the theory of perceived benefits. Furthermore, the framework employs a business performance lens, thus moving beyond the traditional scope of other technology adoption frameworks in order to enhance its explanatory power.
The study is foremost in exploring the business value of ERP systems in healthcare settings. The analysis results highlight the significant impact of ERP systems usage on hospital supply chain costs and confirm the core TOE technological, organizational, and environmental relationships of ERP systems adoption, thus creating an in-depth understanding of the phenomenon. These findings are of paramount importance because hospitals, as every other firm, need to show the business value derived from the application of ERP systems. The findings imply that hospitals’ rising supply chain costs, which comprise a large percentage of the total cost of care, can be counteracted by digitalizing their supply chains, by implementing and fully exploiting ERP systems. Consequently, hospital management can better justify the investment in ERP systems, which is often neglected as it competes with investment in clinical technologies. The study’s results align with previous research in the manufacturing and public services sectors, demonstrating that ERP adoption improves operational efficiency and financial performance [,]. Furthermore, by emphasizing the extent of ERP systems usage, the study encourages other researchers to look beyond the mere adoption of information technologies by digging deeper into their evolutionary process.
The study found support for several drivers of ERP systems adoption in hospital supply chains. The results imply that hospitals with established, integrated technology infrastructure and skilled IT resources are better suited for ERP systems adoption. Efforts to increase technological readiness will yield the expected results only if they are embedded within a learning and continuous improvement culture in an organization characterized by organizational readiness []. Upper management support was found to play a critical role in ERP systems adoption, suggesting managers should secure adequate financial and organizational resources, launch related initiatives, actively support the implementation projects and clear the way by removing barriers. Personnel attitude towards change is another component of organizational readiness. Therefore, hospital executives need to promote the positive impact of ERP systems on the business processes and tasks performed by the hospital’s employees, alleviate possible concerns and provide incentives to personnel actively involved in the implementation of these systems.
Moreover, findings suggest that there is no one-size-fits-all approach. Larger hospitals are more likely to adopt ERP systems and expand their depth. This finding can be attributed to economies of scale [] and the fact that larger hospitals enjoy resource advantages [], as is the case for the Greek public healthcare sector. The unique aspects of the healthcare supply chain and the uniquely complex organizational structures and characteristics that are impacted by various stakeholders with different priorities and seemingly competing interests—effective care vs. efficient operations—do not counterbalance the adoption mechanics of technological and organizational readiness. Regarding the Greek healthcare sector, the results indicate that despite the severe financial crisis and the resulting difficulties, certain public hospitals are leading the way to higher efficiency by digitalizing their supply chains through adopting ERP systems. They demonstrate that determining factors, such as knowledgeable and motivated employees, skilled IT professionals, positive attitude towards change, and supportive upper management can compensate for limited financial resources, raising the bar for less productive hospitals.
The role of the third pillar of technology adoption, the environmental context, could only be partially confirmed in the study. Governmental policies, on the one hand, play a significant role in the adoption of ERP systems as public hospitals operate in a tightly regulated sector. Governments are often willing to promote and provide incentives for adopting ERP systems to enable centralized planning, control, and reporting functions. On the other hand, the influence of business partners could not be confirmed in the study, which might be attributable to the lack of trust and collaboration between hospitals and their suppliers. The healthcare sector is known to be lagging behind other sectors in recognizing the critical contribution of suppliers to the ongoing and sustainable success of an organization []. Furthermore, the essential role of perceived direct and indirect benefits suggests that ERP systems vendors should make more significant marketing efforts to let hospitals appreciate the benefits of ERP systems adoption.
In conclusion, the provided insights on ERP systems adoption in hospitals and their demonstrated impact on hospital supply chain costs bring attention to this less explored area of research and reinforce the role of ERP systems as a strategic asset for the digitalization of the healthcare supply chain. The study’s results imply greater urgency for hospitals to digitalize their supply chain by implementing and fully exploiting ERP systems functionality to deliver quality care at a lower cost. They also provide essential policy recommendations, such as the need for hospital executives to secure adequate financial and organizational resources, provide active support, remove barriers during the implementation process, provide incentives to those involved, and promote the benefits of ERP systems to employees. It is important to note that each hospital has unique characteristics, so a tailored approach to adopting ERP systems is necessary []. Additionally, fostering a learning and continuous improvement culture is crucial for increasing technological readiness. The government, as a major public health stakeholder, top management of healthcare institutions, and the research community should engage in coordinated actions toward increasing awareness of the role of ERP systems. A greater understanding of their potential benefits and positive impact on hospital cost performance may lead to a faster and more comprehensive adoption.
6. Limitations and Future Research
While this study makes significant contributions, it comes with some limitations that offer opportunities for further research. Difficulties in gathering data for Greek hospitals cause some of these limitations, such as the exclusion of private hospital data. Their inclusion as part of a future research phase will expand the research model by allowing them to investigate competitive pressure as an additional component within the environmental context and add hospital ownership as a meaningful control variable. Moreover, a second phase will equip the study with a longitudinal dimension. Its current cross-sectional character constitutes a definite limitation, especially considering that the fit between ERP systems adoption and cost performance is a gradual process.
Furthermore, testing the model and the associated hypotheses using data collected from Greek public hospitals may limit the generalizability of the findings. The Greek public sector operates in an environment of resilient economic recession and is influenced by frequent shifts in the direction of governmental policies. Therefore, the findings should be cautiously extended to other contexts, and the research should be replicated in hospitals in other countries.
Finally, as in every research study examining relationships among variables, endogeneity and common method bias limitations cannot be ruled out completely. Potential informant bias and random errors are drawbacks common to survey research as the measures for some of the study’s constructs are subjective. Much effort was put into dealing with these issues upfront while conceptualizing the research framework and the methodology design. Additionally, potential effects were assessed as part of the post hoc data analysis by performing appropriate tests. As a result, the authors hope that a study of convincing robustness has been presented, which will spur further interest in exploring the business value of ERP systems adoption within the healthcare sector.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/su15043163/s1.
Author Contributions
Conceptualization, C.B., D.B., E.A., C.A. and D.A.; Methodology, C.B., D.B., E.A., C.A. and D.A.; Validation, C.B., D.B., E.A., C.A. and D.A.; Investigation, C.B., D.B., E.A., C.A. and D.A.; Data curation, C.B., D.B., E.A., C.A. and D.A.; Writing—original draft, C.B.; Writing—review & editing, D.B., E.A., C.A. and D.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This research did not require approval by the ethics committee of the International Hellenic University. The ethics committee of the International Hellenic University is responsible for establishing the relevant guidelines (§1 N. 4521/2018), which indicate that studies involving non-interventional research in which individuals are asked to provide information, but in which they are not the subjects of the research, do not require approval.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Hospital data not subjected to confidentiality are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Callender, C.; Grasman, S.E. Barriers and best practices for material management in the healthcare sector. Eng. Manag. J. 2010, 22, 11–19. [Google Scholar]
- Gartner Research. Healthcare Supply Chain: Management and Resilience Strategy; Gartner Research: Stamford, CT, USA, 2022. [Google Scholar]
- Pal, S.K.; Baral, M.M.; Mukherjee, S.; Venkataiah, C.; Jana, B. Analyzing the impact of supply chain innovation as a mediator for healthcare firms’ performance. Mater. Today Proc. 2022, 56, 2880–2887. [Google Scholar]
- Beaulieu, M.; Bentahar, O. Digitalization of the healthcare supply chain: A roadmap to generate benefits and effectively support healthcare delivery. Technol. Forecast. Soc. Chang. 2021, 167, 1207–1217. [Google Scholar] [CrossRef]
- Mandal, S. The influence of dynamic capabilities on hospital-supplier collaboration and hospital supply chain performance. Int. J. Oper. Prod. Manag. 2017, 37, 664–684. [Google Scholar] [CrossRef]
- HIMSS Analytics. Technology Deep Dive: Enterprise Resource Planning. Available online: https://www.himssanalytics.org/news/technology-deep-dive-enterprise-resource-planning (accessed on 17 December 2021).
- Habib, M.M.; Chowdhury, F.; Sabah, S.; Debnath, D. A Study on Hospital Supply Chain Management. Am. J. Ind. Bus. Manag. 2022, 12, 806–823. [Google Scholar]
- Ahmad, H.; Hanandeh, R.; Mustafa, H.; Alzagheer, H. The effects of ERP system implementation on the integration of Supply Chain. Uncertain Supply Chain. Manag. 2021, 9, 1099–1106. [Google Scholar]
- Poba-Nzaou, P.; Uwizeyemungu, S.; Raymond, L.; Paré, G. Motivations Underlying the Adoption of ERP Systems in Healthcare Organizations: Insights from Online Stories. Inf. Syst. Front. 2014, 16, 591–605. [Google Scholar] [CrossRef]
- Aboelmaged, M.; Hashem, G. RFID application in patient and medical asset operations management: A technology, organizational and environmental (TOE) perspective into key enablers and impediments. Int. J. Med. Inform. 2018, 118, 58–64. [Google Scholar]
- Lo, M.F.; Ng, P.M.L. Knowledge management for health care and long-term care in the technology-organization-environment context. In Chronic Illness and Long-Term Care: Breakthroughs in Research and Practice; IGI Global: Hershey, PE, USA, 2019; pp. 277–302. [Google Scholar]
- Zhu, K.; Kraemer, K.L.; Xu, S. The process of innovation assimilation by firms in different countries: A technology diffusion perspective on e-business. Manag. Sci. 2006, 52, 1557–1576. [Google Scholar] [CrossRef]
- Oliveira, T.; Martins, M.F. Understanding e-business adoption across industries in European countries. Ind. Manag. Data Syst. 2010, 110, 1337–1354. [Google Scholar]
- Lin, H.F.; Lin, S.M. Determinants of e-business diffusion: A test of the technology diffusion perspective. Technovation 2008, 28, 135–145. [Google Scholar]
- Zhen, Z.; Yousaf, Z.; Radulescu, M.; Yasir, M. Nexus of digital organizational culture, capabilities, organizational readiness, and innovation: Investigation of SMEs operating in the digital economy. Sustainability 2021, 13, 720. [Google Scholar] [CrossRef]
- Kruszyńska-Fischbach, A.; Sysko-Romańczuk, S.; Rafalik, M.; Walczak, R.; Kludacz-Alessandri, M. Organizational E-Readiness for the Digital Transformation of Primary Healthcare Providers during the COVID-19 Pandemic in Poland. J. Clin. Med. 2021, 11, 133. [Google Scholar] [CrossRef]
- Marei, A.; Daoud, L.; Ibrahim, M.; Al-Jabaly, S. Moderating role of top management support in electronic procurement usage of Jordanian firms. Manag. Sci. Lett. 2021, 11, 1121–1132. [Google Scholar]
- Mandel, M. Scale and innovation in today’s economy. In Progressive Policy Institute Policy Memo; Progressive Policy Institute: Washington, DC, USA, 2011. [Google Scholar]
- Pan, M.J.; Jang, W.Y. Determinants of the adoption of enterprise resource planning within the technology-organization-environment framework: Taiwan’s communications industry. J. Comput. Inf. Syst. 2008, 48, 94–102. [Google Scholar]
- Hsu, P.F.; Kraemer, K.L.; Dunkle, D. Determinants of e-business use in US firms. Int. J. Electron. Commer. 2006, 10, 9–45. [Google Scholar] [CrossRef]
- Mitropoulos, P.; Mitropoulos, I.; Sissouras, A. Managing for efficiency in health care: The case of Greek public hospitals. Eur. J. Health Econ. 2013, 14, 929–938. [Google Scholar] [CrossRef]
- Gibbs, J.L.; Kraemer, K.L. A cross-country investigation of the determinants of scope of e-commerce use: An institutional approach. Electron. Mark. 2004, 14, 124–137. [Google Scholar] [CrossRef]
- De Pourcq, K.; Gemmel, P.; Devis, B.; Van Ooteghem, J.; De Caluwé, T.; Trybou, J. A three-step methodology for process-oriented performance: How to enhance automated data collection in healthcare. Inform. Health Soc. Care 2019, 44, 313–325. [Google Scholar]
- Nachtmann, H.; Pohl, E. The State of Healthcare Logistics: Cost and Quality Improvement Opportunities; Center for Innovation in Healthcare Logistics, University of Arkansas: Fayetteville, NC, USA, 2009. [Google Scholar]
- ICAP. ICAP Group Healthcare Sector Report; ICAP: Andover, MA, USA, 2020. [Google Scholar]
- BI-Health. Business Intelligence Portal of National Healthcare System. Available online: http://portal.bi.moh.gov.gr/el (accessed on 29 November 2021).
- OECD. Length of Hospital Stay (Indicator). Available online: https://data.oecd.org/healthcare/length-of-hospital-stay.htm (accessed on 22 October 2021). [CrossRef]
- Lin, I.F.; Schaeffer, N.C. Using survey participants to estimate the impact of nonparticipation. Public Opin. Q. 1995, 59, 236–258. [Google Scholar] [CrossRef]
- Zhang, H. Structural equation modeling. In Models and Methods for Management Science; Springer Nature: Singapore, 2022; pp. 363–381. [Google Scholar]
- Arbuckle, J. IBM SPSS and AMOS (Version 22.0) User Guide; IBM: New York, NY, USA, 2015. [Google Scholar]
- Anderson, J.C.; Gerbing, D.W. Structural equation modeling in practice: A review and recommended two-step approach. Psychol. Bull. 1988, 103, 411–423. [Google Scholar] [CrossRef]
- Hair, J.F.; Black, W.C.; Babin, B.J.; Anderson, R.E.; Tatham, R.L. Multivariate Data Analysis; Prentice Hall: Upper Saddle River, NJ, USA, 1988; Volume 5, pp. 207–219. [Google Scholar]
- Fornell, C.; Larcker, D.F. Structural equation models with unobservable variables and measurement error. J. Mark. Res. 1981, 18, 382–388. [Google Scholar]
- Jöreskog, K.G.; Sörbom, D. LISREL 8: Structural equation modeling with the SIMPLIS command language. In Scientific Software International; Lawrence Erlbaum Associates, Inc.: Mahwah, NJ, USA, 1993. [Google Scholar]
- Hu, L.T.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. A Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Stefanou, C.J.; Revanoglou, A. ERP integration in a healthcare environment: A case study. J. Enterp. Inf. Manag. 2006, 19, 115–130. [Google Scholar] [CrossRef]
- Fernandez, D.; Zainol, Z.; Ahmad, H. The impacts of ERP systems on public sector organizations. Procedia Comput. Sci. 2017, 111, 31–36. [Google Scholar]
- Madanhire, I.; Mbohwa, C. Enterprise resource planning (ERP) in improving operational efficiency: Case study. Procedia CIRP 2016, 40, 225–229. [Google Scholar]
- Durrani, H.; Khoja, S.; Naseem, A.; Scott, R.E.; Gul, A.; Jan, R. Health needs and eHealth readiness assessment of health care organizations in Kabul and Bamyan, Afghanistan. East. Meditteranean Health J. 2012, 18, 663–670. [Google Scholar]
- Sultz, H.; Young, K. Health Care USA; Jones & Bartlett Learning: Burlington, MA, USA, 2014. [Google Scholar]
- Rogers, E.M. Diffusion of Innovations. Simon and Schuster; Free Press: New York, NY, USA, 2010. [Google Scholar]
- Gortzis, L.G. Selecting healthcare information systems provided by third-party vendors: A mind map beyond the manuals. Inform. Health Soc. Care 2010, 35, 1–9. [Google Scholar] [CrossRef]
- Damali, U.; Kocakulah, M.; Ozkul, A.S. Investigation of Cloud ERP Adoption in the Healthcare Industry Through Technology-Organization-Environment (TOE) Framework: Qualitative Study. Int. J. Healthc. Inf. Syst. Inform. 2021, 16, 1–4. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).