Abstract
In recent years, the medical industry has rapidly modernized, incorporating technology to aid in accelerating and simplifying procedures for better accuracy. This technology is becoming more interconnected to create a larger network known as the Internet of Medical Things (IoMT) that can combat the pandemic’s spread. In other words, IoMT emphasizes health applications while maintaining the core concept of the Internet of Things (IoT). The further spread of Coronavirus Disease-2019 (COVID-19) can be halted by employing it. Consequently, this paper uses the Systematic Literature Review (SLR) methodology to evaluate recently published articles in the IoMT domain during the COVID-19 era. Between 2019 and 2022, we analyzed 41 studies. An analysis of the evaluation criteria reveals that the delay factor comprises 38% of the evaluation criteria, the highest percentage because a low-delay IoMT device has a quick response time between the time a request is made and the time a response is received. Moreover, the performance factor accounts for 22%, the accuracy factor accounts for 28%, the security factor for 6%, and the cost factor for 6%. Finally, we concentrate on open issues and future research challenges in IoMT during the COVID-19 era.
1. Introduction
Our living environments are increasingly becoming covered with sensors embedded in common objects. As a result of IoT technology, they are smoothly integrated into the internet network and can run autonomously without any manual effort required [1]. Currently, the IoT plays a significant role in a wide range of industries. The IoT has had a considerable impact on the healthcare industry. For example, the IoT has revolutionized people’s lives by tracking their health in real-time. IoT devices are more valuable because they are less expensive and can diagnose diseases faster.
Digital tools and technology, specifically IoT, have played an important role in combating COVID-19. The COVID-19 pandemic has had a significant impact on the IoT ecosystem. As a result of the COVID-19 pandemic, IoT-inspired frameworks and solutions got a much-needed reality check. The authorities used IoT technologies such as remote monitoring to control and contain COVID-19 [2]. All governments are combating the virus while seeking a cost-effective solution. They were using technology to teach people how the virus spreads and preventative measures can be more effective in educating people. IoT can assist in preventing the spread of this pandemic despite other technologies such as artificial intelligence, machine learning, cloud computing, and robots [3].
IoT and similar technologies may be beneficial in decreasing COVID-19 pandemics. A brief review of several potential sources of several technological approaches used to cope with the COVID-19 pandemic’s effects [4]. COVID-19 might be controlled with the use of an IoT-based architecture. In addition, a list of IoT sensors and their application domains existed. In a second demonstration, the article mentioned a possible IoT architecture for preventing the spread of COVID-19 [5].
COVID-19’s impact on the global economy has been emphasized. Thus, the conversation has shifted to using new technologies such as IoT, drones, AI, blockchain, and 5G to reduce the impact of the COVID-19 pandemic. Until a treatment for this disease is found, these technologies will be mainly responsible for managing and limiting its damage [6].
According to review studies in the field of IoMT in the era of COVID-19, the main contributions of our paper are:
- To mention and discuss upcoming research ideas and unresolved concerns based on the SLR method.
- Furthermore, we design a taxonomy for categorizing various aspects of IoMT in the era of COVID-19.
- Then, we present research questions (RQs) about the IoMT in the era of COVID-19 and answer them.
The following sections comprise this paper: Section 2 offers outlines of related work and a review of the concept. Section 3 describes the study’s objective and provides more information on selecting relevant work and categorizing the content. In Section 4, several analytical comparisons of previous research studies are presented. Section 5 discusses the present state of challenges and promising future research directions. Section 6 is the conclusion.
2. Related Work and Review of the Concept
2.1. Related Work
This section summarizes the related studies on IoMT in the era of COVID-19.
Yousif et al. [2] reviewed major IoT solutions influencing COVID-19 during the epidemic, including healthcare, contact tracing, and transportation. In addition, they discussed the difficulties and possibilities for IoT infrastructure approaches in the immediate post-COVID-19 period, as well as privacy and security problems. New standards and codes of conduct for mass adaptability will be explored. In particular, prospective research approaches for IoT applications would improve performance with retained privacy and security and allow broader adaptability by the general public. The paper’s major advantage is that it provides information on related studies.
Singh et al. [7] researched, debated, and emphasized the overall use of the IoT concept to combat the COVID-19 epidemic. They selected and reviewed twelve key uses of the IoT by researchers, academics, and scientists who were finally obliged to develop production methods to fight or combat this epidemic. However, the research lacks a taxonomy and explanation of the applications it focuses on and an illustration of related work.
Ndiaye et al. [8] showed sensor-based E-health in managing global epidemics. A worldwide viral epidemic also impacted the development of IoT networks. Social approval and protection of information exchange for IoT management systems are required to fight a worldwide epidemic. The study’s main weakness is that the taxonomy of the research was not proposed.
Dong et al. [1] showed how the IoT might be integrated into the pandemic prevention and treatment system. IoT fog-cloud technology was demonstrated, which may be utilized for COVID-19 epidemic prediction, investigations, significant discrepancies, and monitoring of SARS-CoV-2 mutations. Additionally, they studied and evaluated the provincial literature on these five treatments to show the possibilities of IoT in fighting the current COVID-19 epidemic or future infectious disease outbreaks.
Kumar et al. [9] examined the role of IoT in revolutionizing the medical area by providing accessible and practical medical services to the human race. Then, they analyzed the importance of IoT in smart hospitals, its significance in dealing with epidemics, and several designs that may identify unanticipated events utilizing multiple sensors and display the information gathered on the LED display. Observational findings have confirmed their hypothetical claims.
Kamal et al. [10] analyzed COVID-19-related IoT apps for their present state, implementation, operational problems, and prospective prospects to limit the epidemic further. In addition, an IoT implementation study was conducted, in which internal and external variables were considered.
Shamsabadi et al. [11] determined the use and capabilities of IoT and digital health in COVID-19 pandemic management. This comprehensive evaluation was carried out by browsing web databases. To list the paper’s drawbacks, we can point out that there is no taxonomy of classifications, and they do not refer to any key evaluation factor or IoT roles in COVID-19; instead, they just compare articles.
The associated survey studies on IoT in the era of COVID-19 concerns are summarized in Table 1.

Table 1.
Relevant studies of IoT in the era of COVID-19.
With proper consideration of our study domain, we present a complete literature review to address the following gaps:
- Most existing studies do not provide any taxonomy for IoMT in the COVID-19 era.
- The technique of research selection was not apparent in most of the reviewed articles.
- Several research types fail to mention IoMT factors or metrics in the COVID-19 era.
2.2. Review of Concept
2.2.1. IoMT’s Benefits in the Health Sector
Compared to the past decades, the growth of technology in health and medicine has decreased. The emergence of IoMT is one of the most essential and efficient medical advancements. IoT and health are made up of smart objects or devices that can connect to the IoT. These devices may utilize cloud connectivity to gather data and send it to a network to achieve a purpose. IoT devices may be found everywhere, from the industrial supply chain to autonomous cars, but health is one of the essential IoT applications [12,13,14].
Connected devices and the IoMT can provide considerable benefits to the healthcare industry, listed below:
- Chronic disease remote monitoring devices.
- Improving, diagnosing, and treating patients.
- It increases patient safety and medication management.
- Improvements in long-term disease treatment.
- Lower expenses.
IoT and health are both growing in popularity. The healthcare industry is currently confronted with various difficulties that can be solved using linked medical equipment and the IoT. IoMT has the potential to improve patient care, improve healthcare outcomes, and lower overall costs. The health business needs the IoMT seriously [15,16,17].
2.2.2. IoMT Applications in the Health Sector
As shown in Figure 1, IoMT focuses on health applications and, of course, the realization of crucial aspects in this field while keeping the essential concept of the IoT, which is the connectivity of all things around us to the Internet. Anything linked to human health or health systems can lead to the supply of a new service or product in the health field through network communication in the field of IoT. The IoMT is a collection of medical gadgets that link to the internal network of health systems and specialists. A person’s health information is kept in an Internet database and made available to the appropriate organization or persons, such as physicians, nurses, or the World Health Organization, using IOMT. Of course, smart medical apparel and health assessment components are not the only examples of IoT in health; smart cards in place of insurance booklets may also be included in this category. As an interdisciplinary knowledge base, the IoT has guided the creation and expansion of other sciences. The IoT and smart health are two main concepts that have seen significant growth in recent years. The IoT’s importance in society’s health has grown as smart gadgets’ applications in enhancing people’s health have grown. Public trust in the IoT has improved as disease management and timely medicine administration has improved [14,18,19].
Figure 1.
Internet of Medical Things.
The IoT is employed in a variety of medical sectors, and is most commonly utilized in the following medical fields:
- Patient-care systems that remotely can be accessed.
- Emergency notification systems.
- Exercise regimens.
- Drug management.
- Chronic illness management.
- Control of the elderly.
Smart health tools have advanced significantly in recent years. Electronic health devices use a variety of sensors to try to keep track of people’s health. Ordinary people, athletes, and patients all use these health tools. In today’s hospitals, the IoT has improved the well-being of both patients and medical employees. Regarding the doctor’s digital presence via the IoT, it is not uncommon for a doctor to be on leave and unable to be present in a delicate scenario when the presence of a doctor is essential. Using the IoT, the physician may quickly monitor the patient’s status from afar and provide essential patient care instructions to other hospital staff. Many medical volunteers in underserved communities cannot also attend medical seminars and courses in big hospitals. Volunteers will be able to offer distant medical training classes utilizing IoT communication techniques at this time. The status of certain hospitalized patients necessitates that their vital signs be checked often and at short intervals. IoT sensors can be employed and recorded in the patient’s electronic file at this time. These sensors will monitor the patient’s vital signs regularly and provide the necessary information to the doctor, greatly assisting in increasing the pace of care for critically ill patients. Athletes who must continually monitor their health information owing to the nature of their sport might utilize these sensors to be notified of their health condition at short intervals [3,4,16].
2.2.3. IoMT in the COVID-19 Era
The IoT has long been a part of our daily lives. Smart homes, smart transportation, smart industries, and various commercial, infrastructural, and military applications are examples of this use. The COVID-19 virus is not the first worldwide epidemic in history but the first of its type in the technological era. The coronavirus has spread around the world at a time when new technology can assist governments in preventing and curing its spread. IoT technology is quite effective and has played a critical role in containing this dangerous pathogen. This technology has been successful in various domains, including health, industry, education, government, and others. As shown in Figure 2, the subject of health and therapy has been one of the most essential and vital action areas for this technology [2,3,13]. The breakout of COVID-19 has ushered in a new era of technology and knowledge.
Moreover, during the COVID-19 epidemic, the IoMT played a critical role in assisting the healthcare system control incorrectly infected patients via interconnected networks and equipment. The IoMT is a network of interconnected technologies that can help prevent the spread of infectious illnesses by offering an early warning system thanks to developments in data processing and extensive connectivity. It should not be difficult for a country, particularly China, to implement such technology [1,8,10].
Figure 2.
Main IoT rolls in the COVID-19 era.
The IoMT can limit the spread of COVID-19 and might be utilized to avert such problems. As the coronavirus has transformed how many businesses think about how illness spreads, the IoT is anticipated to monitor various behaviors to ensure that health and safety rules are followed to avoid coronary heart disease. Thanks to the IoT and specifically engineered sensors, it will be able to identify whether individuals on public transit are taking important actions to prevent contagious illnesses shortly. Privacy regulations must, of course, be taken into account. The IoT has been utilized to manage emergencies in many nations as the disease has grown and expanded. Many nations, for example, have installed sophisticated body temperature measuring devices at the entrances to most public locations, such as train stations. Drones are also employed in some countries to monitor public compliance with quarantine restrictions and the wearing of masks by the general population. The IoT’s function in COVID-19 varies based on the geographical location, the country’s infrastructure, and available facilities. The IoT may be beneficial in different parts of the city, and if there is a lot of traffic in one place, report it to the appropriate organization or center. In reality, strategically installing cameras across the city makes it feasible to record all traffic without using human resources. One of the most critical functions of the IoT in COVID-19 is to identify people who do not adhere to health rules, such as not wearing a mask. Using artificial intelligence and image processing technologies, cameras connected to the IoT can be deployed at airports, businesses, city centers, and other locations to identify people without masks. There will be no need for manpower, and everyone who does not wear a mask will be photographed and punished. One of the aspects of sustainable development in countries is paying attention to health. In addition to COVID-19, IoT technology offers applications in this sector that deserve further attention [2,4,12].
2.2.4. Challenges of IoMT Use in Medicine and Patient Care
The IoMT has the potential to alter healthcare systems throughout the world drastically. However, there are still issues and concerns with employing the IoMT in medicine and patient care, with some of the more significant ones highlighted below.
- Privacy Protection of patients.
Privacy has long been a major concern. Patients require assurance that their personal information is kept confidential since physicians deal with it. Regrettably, the IoMT may be able to access this information and obtain access to the healthcare ecosystem, which is why it is critical to keep patients safe from hackers.
- Accidental failures and errors.
A little flaw in an IoMT-based health monitoring system might have major ramifications. No technology can eliminate the possibility of failure. As a result, it is critical to think about every element while developing programs and manufacturing IoT devices in the medical industry.
- Malware on the Internet.
The Internet is full of viruses in today’s world, which may infect any operating system and IoMT applications in the healthcare area. Installing effective antivirus and firewalls, on the other hand, will protect IoT software.
- No encryption on information.
Customizing the system with encryption is another method for securing patient information on IoT devices. This capability can guard against illegal access to systems. Unfortunately, not all of these systems can encrypt or have extremely weak encryption, allowing anybody to access them.
2.2.5. SIoT in the COVID-19 Era
Incorporating social networking ideas into the IoT has led to the Social Internet of Things (SIoT) paradigm, which asserts that objects can form social relationships independently of their owners, with the advantage of enhancing network scalability in information discovery. Increasing the number of devices people can use to access the Internet is one of the main benefits of social media marketing. The IoT presents marketers with a distinctive and creative opportunity to engage customers in novel ways. Social networks help the IoT ecosystem’s information exchange by facilitating faster communication between online-connected devices. An increase in engagement results in stronger relationships. These strong ties could benefit the promotion and sale of other products. The IoT will strengthen the weaknesses of social media marketing [20,21]. With the proper information management and application of knowledge from the extensive IoT network, smart equipment will be able to create a micro-community, grow, and evolve under the demands of the audience. IoT will be included in social networks once everything is intelligent. Despite its claims to enhance human existence, the IoT has raised many questions for social media designers. The SIoT algorithm seeks to differentiate between two levels: social beings and intelligent things. Regarding privacy, SIoT allows for creating social networks for individual objects, and people can access both SIoT and conventional social networks. It is important to work to make social objects a reality because using intelligent objects without allowing them to interact with people cannot be very useful [20,21,22].
Even years after the coronavirus pandemic, the new coronavirus remains a public health threat. Communication within groups and between individuals has broken down due to the emphasis on social distance. Social isolation may have slowed the spread of the coronavirus, but it has also increased COVID-19’s psychological burden and caused various other problems. Those who live alone find it challenging to deal with this situation because they lack a social support system. While the scientific community continues to work tirelessly to develop effective treatments and safety protocols for it, psychologists and mental health professionals are utilizing superior psychological investment to build mental protection against any potential threat and to address the increase in psychological issues caused by this viral infection. This assumes even greater significance given that the psychological effects of the illness on individuals, families, and communities will last for a very long time, even if the COVID-19 pandemic danger is eliminated with the development of a workable vaccine or therapy [22,23,24].
In light of the widespread global restrictions on in-person gatherings and activities, internet technology and social media networks have become society’s saviors. Many large-scale events have recently been held online, SIoT has been used in previously unheard-of ways to interact and communicate with friends, family, and society, and relevant academic and administrative tasks have all gone digital. Therefore, it is crucial to consider how social media and contemporary media have helped people connect and their communities and how this feeling of belonging has benefited their health [21].
The physicochemical characteristics of the viruses and the SIoT, which regulates the pattern of interpersonal interaction, are two factors that impact the spread of infection. Humans are not the only hosts for viral agents. They actively interact with others, spreading infections to those more or less foreseeable from a social perspective and everyone else. Although it is widely acknowledged that the characteristics of viral transmission networks significantly influence the scope and circumstances of epidemics, there has not been much research or data on COVID-19 and implementing evidence-based policies is challenging. One of the problems transmission networks face is social distance. Social distance programs encourage or mandate less contact between all members of the community, despite the entire transmission network having local information that unnecessarily aids in the spread of illness. As a thorough scientific investigation does not back it, this advice may be less effective or successful [21,22,23].
3. Research Selection Method
This section provides an overview of the IoT in the era of the COVID-19 classification method based on the SLR process, including research questions, database selection, and search terms.
The following exploration string was developed after considering the alternatives and other synonyms of the major essential components:
(“Internet of Things” OR “IoT”) AND (“COVID-19”) AND (“survey” OR “review” OR “overview” OR “challenges”)
Due to the importance of the selected topic and other factors, such as the lack of a comprehensive article on the topic of “IoT in the era of COVID-19,” the following Research Questions (RQ) will be addressed as part of this SLR study.
- RQ1:
- What are the roles of IoMT in the control and prevention of COVID-19?
- RQ2:
- What are the evaluation criteria in the domains of IoMT in COVID-19?
- RQ3:
- What are the effects of IoMT on COVID-19 concerns?
- RQ4:
- What are the important applications of IoMT for the COVID-19 pandemic?
- RQ5:
- What are the future research challenges and open issues of IoMT in COVID-19?
In addition, the inclusion criteria mentioned below are considered when selecting the final studies:
- Research articles.
- Articles available online after 2019.
- Articles in the field of IoT and COVID-19.
- Articles whose titles contain the terms IoT and COVID-19.
Moreover, the exclusion criteria mentioned below are considered when selecting the final studies:
- Non-English articles.
- Articles not in the field of IoT and COVID-19.
- Review articles.
Finally, 41 studies were chosen for evaluation and analysis. Figure 3 shows the number of papers published from 2019 until May 2022 published by top scientific publishers, including Elsevier, IEEE, Springer, John Wiley, Taylor and Francis, MDPI, and others on journal citations.
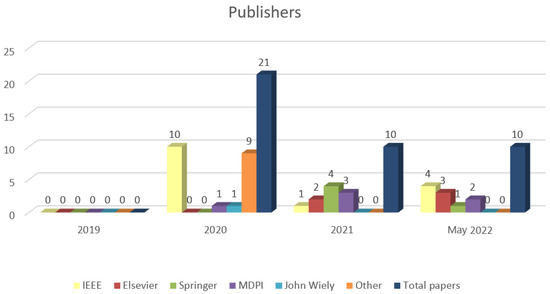
Figure 3.
Distribution of research papers by publisher.
Based on a systematic review, our work aims to give an overview of current efforts and achievements in the field of IoT in the era of COVID-19 and propose open topics for future research in this field. The research strategy’s five stages are shown in Figure 4.
A comprehensive taxonomy of the IoT in COVID-19, covering security, IoT systems engineering, algorithms, architecture and infrastructure, and IoT applications, is shown in Figure 5. In the next step, we break each aspect down into its sub-aspects.
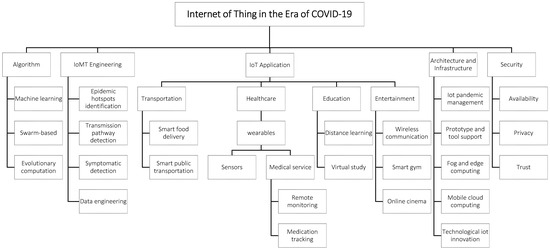
Figure 5.
The taxonomy of IoT in the era of COVID-19.
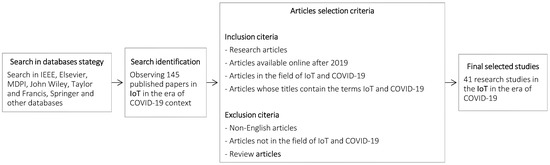
Figure 4.
Research study selection criteria and assessment chart.
4. Organization of IoMT in the Era of COVID-19
As part of the SLR process, this section provides a technical overview of the selected IoMT in the COVID-19 era for current research.
The taxonomy for IoT in the COVID-19 era categorizes existing works in the specified field based on the study chosen. Each item is classified by IoMT engineering, algorithm, architecture and infrastructure, IoMT application, and security. We review each study in terms of its major background and the advantages and disadvantages of each study’s findings.
4.1. Algorithm
Most studies provide a new COVID-19 diagnostic model based on the IoMT employing algorithms, particularly machine learning-based methods. For instance, machine learning-based methods may accurately identify COVID-19 from computed tomography images by examining radiological characteristics.
Table 2 illustrates the classification of the listed articles of the algorithm category of IoMT in the COVID-19 era. The following determines the most important contexts in the algorithm category:
- Machine learning.
- Swarm-based.
- Evolutionary computation.
In addition, the evaluation criteria for this categorization are shown in Table 3. Mobility, performance, accuracy, time, and signal value are the evaluation criteria for the algorithm category.

Table 3.
Evaluation criteria in the algorithm category.

Table 2.
Reviewed studies in the algorithm classification.
Table 2.
Reviewed studies in the algorithm classification.
| Research | Main Scope | Benefit | Drawback | Simulation/Implementation |
|---|---|---|---|---|
| Yacchirema et al. [25] | An IoT-based system for safer mobility in the COVID-19 area | More accurate | No detail mentioned | Implementation |
| Abdulkareem et al. [26] | An IoT-based system to diagnose COVID-19 using machine learning algorithms | -Better performance -Reduce the workload -Reduce the mortality rate | Simulation | |
| Shalabi et al. [27] | COVID-19 symptoms monitoring mechanism | Better performance | Not enough detail | Implementation /Simulation using C++ |
| Ukhalkar et al. [28] | An IoT-enabled and machine learning-based model for early predicting the COVID-19 test | - | -No simulation, no Implementation -Not mention the impacts clearly | No Implementation/No simulation |
| Mukhtar et al. [29] | An IoT framework to screen coronavirus | -No simulation, no Implementation -Not experiment with the idea | No Implementation/No simulation | |
| Yang et al. [30] | Prevention and Control of COVID-19 | Effectiveness | Systems hardware complexity | No Implementation/No simulation |
Yacchirema et al. [25] proposed an IoT-based system for safer mobility in the era of COVID-19. An IoT, fog, and cloud solution-integrated layered architecture was used to monitor and regulate the social distance between individuals in real-time and the capacity of shared interior spaces. It has been done by employing machine learning algorithms to recognize people’s whereabouts. Data collected from a portable IoT device has been used to train and assess these models. The disadvantage of the paper is that it did not mention details, and the advantage is that it improved the accuracy.
Abdulkareem et al. [26] presented an IoT model that used machine learning algorithms to diagnose COVID-19 patients in smart hospitals. Their machine learning model was developed and assessed using laboratory datasets. There were three primary methodological scenarios for COVID-19 diagnosis, including original and normalized datasets and feature selection. The advantages of the proposed model are better performance, reduced workload, and reduced mortality rate.
Shalabi et al. [27] presented the COVID-19 Symptoms Monitoring Mechanism (CSMM), based on IoT technology and wireless sensor networks, and intended to monitor patients, particularly the elderly, who suffer from chronic immune disorder deficiencies during their quarantine. Due to this, it is more likely to diagnose major diseases. The method was based on remote patient data monitoring and was successful. Better performance is the advantage of the presented design.
Ukhalkar et al. [28] suggested a prospective model for predicting the COVID-19 test early using symptoms. With the Smart Voice Recorder and the Bluetooth Thermometer in this model, input sounds of coughing were captured. It is possible to estimate COVID-19 susceptibility based on symptoms using classifiers such as random forest trees and decision tree classifiers. This suggested model will minimize human intervention and the usage of testing equipment for most affected populations. The main drawbacks of the paper are that no simulation or implementation approaches were used in the study, and it does not mention the impacts of the model.
Mukhtar et al. [29] suggested a framework for remote virus screening using standards-based practices. Sensors are integrated into a wearable gadget that anyone may wear to determine whether they are healthy or not in a few seconds. The framework called for testing on a large population. The data gained via testing may be utilized for advanced analytics such as epidemic prediction and prevention, population segmenting, and assisting the government and decision-makers in taking necessary steps. The disadvantage of the paper is that no simulation or implementation was used.
Yang et al. [30] emphasized the IoT’s potential for internal COVID-19 infection prevention and control. The suggested scheduling system could prevent people from congregating in certain regions. A navigation system with a density control approach and global route planning capabilities is implemented using K-Nearest Neighbor and introduces a tool for creating an internal positioning system. They constructed an iBeacon network and employed a fingerprint-based approach for real-time location. The results of the experiments suggest that the positioning system is feasible. In addition, a risk assessment model for an enclosed space has been developed. It may be incorporated into a government-sponsored macro data prevention and control system, which aids in developing a complete and systematic COVID-19 prevention and control mechanism.
4.2. IoMT Engineering
COVID-19 for the economy and people has been an inconvenience. While some sectors have been affected due to COVID-19, some special fields, such as IoMT engineering, witnessed a leap. Over the next few years, the vast IoT systems will be connected. This increase in the number of IoT systems used will also significantly increase IoT businesses. A job in IoT could have good wages because of the increase in demand, but the volunteers will need combinatorial skills to ensure an IoT hopeful career.
Table 4 illustrates the classification of the listed articles in IoMT engineering. The following determines the most important contexts in the IoMT engineering category:
- Epidemic hotspots identification.
- Transmission pathway detection.
- Symptomatic detection.
- Data engineering.
The evaluation criteria of this classification are shown in Table 5.

Table 5.
Evaluation criteria in the IoT systems engineering category.

Table 4.
Reviewed studies in the IoT systems engineering classification.
Table 4.
Reviewed studies in the IoT systems engineering classification.
| Research | Main Scope | Benefit | Drawback | Simulation/Implementation |
|---|---|---|---|---|
| Akinola et al. [31] | Superstrate antenna for satellite cynosure | -Better performance -Provide a long-time sustainable solution | - | Simulation |
| Ashraf et al. [32] | Use of IoT-Edge technologies to identify and monitor contagion | - | -Not any simulation or implementation -Not mentioned the apparent impact of the proposed framework | No Implementation/No simulation |
| Priambodo et al. [33] | Monitoring self-isolation patients of COVID-19 with the IoT technology | Better visibility on monitoring | -Not enough detail mentioned about the work | Implementation |
| Misra et al. [34] | Safety-aware IoT navigation tool to find safe routes for traveling | Reduce the distance | -Not focus on real-time traffic and speed control. | Implementation |
| Rana et al. [35] | Secure IoT communication systems for the transport and storage of COVID-19 data | Reduce the time | - | Implementation |
| Le et al. [36] | IoT-enabled depthwise separable convolution neural network for diagnosing COVID-19 | Better performance | - | Implementation |
| Cacovean et al. [37] | An IoT system for diagnosing COVID-19 patients | - | -Not presenting any detailed analysis -Not mentioned the apparent impact of the proposed framework | Implementation |
| Akhund et al. [38] | IoT-based low-cost robotic agent for a patient with a physical disability affected by the COVID-19 virus | Effectiveness | -Not presenting any statistical analysis | Implementation |
| Bashir et al. [39] | IoT-Based COVID-19 system for COVID-19 applications | Effectiveness | Restricting the scope of the check to only the given area | Simulation |
| Jung et al. [40] | An IoT-based platform for monitoring and tracking COVID-19-related person | -Reduce latency -Scalability | - | Simulation/Implementation |
| Bhardwaj et al. [41] | Health Monitoring System | Effectiveness | -High delay -Less secure data | Implementation |
| Saranya et al. [42] | Health Monitoring System | -High performance in monitoring patients -Better accuracy -Better scalability | - | Implementation |
Akinola et al. [31] suggested a superstrate for a rectangular micro-strip antenna. A 3D electromagnetic computer simulation package was used to model the proposed antenna, simulate it using a frequency-domain solver, and verify it using a time-domain solver. The advantages of the suggested antenna are better performance and the ability to provide a long-term sustainable solution for combating the COVID-19 epidemic.
Ashraf et al. [32] proposed a wearable smart gadget surveillance system for remote monitoring, prior warning, temperature, heartbeat rate, and cardiac conditions to detect sick or suspicious individuals. The proposed architecture provided a continuously updated pattern of the communication chain of COVID-19-infected people that could spread throughout their national community. The paper’s important drawbacks are that no simulation or implementation approaches were used in the study, not to mention the apparent impact of the proposed framework.
Priambodo et al. [33] created a healthcare system based on IoT and wireless body sensor networks and a gateway that can be utilized for data collection and transmission. An open-source Elastic search Logstash Kibana (ELK) stack is used for logging and indexing massive incoming data streams so that medical staff may study and display measurement results of patients and their location on a dashboard. They may monitor the patient’s status and take preventive measures if necessary. The proposed system’s advantage is better monitoring visibility, but the disadvantage is that there is not enough detail about the system.
Misra et al. [34] described developing a safe navigation system based on Q-learning that minimizes travel over categorized hotspots in a road network. Input from commuters was used to determine a safe route for travel and punished zones to create a reward function for the reinforcement learning model and showed that the system was convergent in all situations. An IoT-based architecture integrating cloud and fog computing was also proposed. The main advantage of the paper is reducing the distance. It does not focus on real-time traffic and speed control.
Rana et al. [35] developed secure communication networks to transport and store pandemic data. For instance, the COVID-19 framework was built and verified by considering COVID-19 states. A new IoT-based secure communication system was suggested for providing a central control center with information on local observations. A signal processing method was implemented that is best for the task at hand to forecast the COVID-19 model. Reducing the time is the proposed model’s benefit.
Le et al. [36] proposed an IoT-enabled depth-wise separable convolution neural network (DWS-CNN) for COVID-19 diagnosis and classification. The suggested method used a deep support vector machine. The IoT devices collected patient data and sent them to a cloud server during the data gathering step. In addition, the method was used to eliminate noise from the picture. The proposed method was then used to replace the default convolution for automated feature extraction, replacing the default convolution. Finally, the binary and multiple class labels of COVID-19 were determined using the proposed method. Better performance was the advantage of the proposed method.
Cacovean et al. [37] proposed that a centralized IoT system for diagnosing COVID-19 patients and managing their medical data would be beneficial if adopted by governments. This experiment was conducted on a sample of 300 individuals. Wearables gadgets are assigned to them, and they must wear them for a week during the day. The data are received every 60 min in real-time. These wearables were outfitted with temperature, heart rate, and GPS sensors to identify users inside or outside of a viral outbreak. The main disadvantages of this study are that it does not present any detailed analysis, nor does it mention the apparent impact of the proposed framework.
Akhund et al. [38] illustrated a virus-affected person with a physical disability using a wireless gesture control robot. As a result, the system will benefit the disabled and those infected with a virus. This robot can help wherever other people are terrified of being near people infected by a virus. The device can be used with a wheelchair to allow them to go from one location to another. Not presenting any statistical analysis is the drawback, but robots’ effectiveness is the advantage of the paper’s idea.
Bashir et al. [39] developed a low-cost IoT-enabled system based on the standard operating procedure (SOP) in COVID-19 applications. It counts the number of individuals entering and leaving an area, maintains physical distance, measures body temperature, and notifies attendees and managers of security breaches. It consisted of numerous sensor nodes communicating with a central server through a network cable. To ensure compliance, real-time monitoring and planning were all possible for the information saved on the server. No personal information was stored in the system, nor was there a way to determine who attended the meeting. The lack of a developed system restricts the scope of real-time monitoring to only the given area.
Jung et al. [40] proposed a public platform based on Software-Defined Networking Controllers to monitor and record information for COVID-19-related individuals and provide real-time information disclosure services to global centers for disease control. The platform was designed to ensure secrecy and authentication services by offering users a unique secret key. To mention the benefits of the proposed platform, we can point to reducing latency and providing scalability.
Using IoT technology, Bhardwaj et al. [41] created a complex medical monitoring system that monitors a patient’s blood pressure, heartbeat, oxygen level, and temperature. This method is advantageous in rural areas or cities and towns where neighborhood medical centers can communicate with urban hospitals regarding their patients’ health. The IoT system will notify the doctor or physician if patient health changes occur outside standard levels. This IoT-based health monitoring device makes collecting real-time data simple for doctors. The system can control the settings regularly since high-speed Internet access is available. Furthermore, the cloud platform enables data storage and recall of past measurements. Individuals can be identified and treated early with this technique.
Saranya et al. [42] designed and produced an IoT monitoring system that does not require the use of the cloud. The system comprises unobtrusive sensors, a data collection device, a microcontroller, a Wi-Fi module, a web server, and a web or mobile application. This design shows a system for monitoring and identifying the severity of coronavirus in patients by employing a variety of unobtrusive sensors to assess disease-specific vital factors such as heart rate, temperature, oxygen level, and pulse rate, which are the key symptoms of coronavirus. A microcontroller and a Wi-Fi module translate patient data from the sensor to the cloud server in real-time via the HTTP protocol. According to an experimental investigation, the suggested structures successfully monitor the severity of respiration in patients. Finally, the correctness and scalability of the architectural performance are verified.
4.3. Architecture and Infrastructure
Medical devices and software are connected to a health technology infrastructure through the IoMT, which uses communications systems. The IoMT includes portable smart displays, smart wearables, and other sophisticated tools for tracking your health state. Based on the complexity of healthcare systems, managing hundreds of medical devices diversely linked to the Internet is essential to upholding the highest level of constancy. Researchers are creating smart healthcare architectures and frameworks for deploying, coordinating, and developing intelligent IoMT services.
Table 6 shows the listed articles of IoT’s architecture and infrastructure category in the COVID-19 era. The primary contexts in the architecture and infrastructure category are based on the following:
- IoT pandemic management.
- Prototype and tool support.
- Fog and edge computing.
- Mobile cloud computing.
- Technological IoT innovation.
Moreover, Table 7 displays the evaluation criteria of this classification.

Table 7.
Evaluation criteria in the architecture and infrastructure category.

Table 6.
Reviewed studies in the architecture and infrastructure classification.
Table 6.
Reviewed studies in the architecture and infrastructure classification.
| Research | Main Scope | Benefit | Drawback | Simulation/Implementation |
|---|---|---|---|---|
| Kolhar et al. [43] | A platform for face detection during COVID-19 city lockdown | Good performance | - | Simulation |
| Roy et al. [44] | A framework for contact and infection tracking for COVID-19 | Effective utilization of the scarce resources | Not supported on a large scale | Simulation using Python. |
| Poongodi et al. [45] | An IoT-based architecture for detecting the COVID-19 infection | Effectiveness | Not enough detail | Simulation using Python. |
| Rajasekar et al. [46] | An IoT-based tracking model for identifying prospective contacts for COVID-19 | -High effectiveness -Low cost | - | No Implementation/No simulation |
| Kumar et al. [47] | Blockchain–IoT-enabled pharmaceutical supply chain for COVID-19 | -Improve the visibility -Improve transparency -Improve privacy -Reduce the chances of infections | No simulation, no Implementation | No Implementation/No simulation |
| Pandey et al. [48] | Ensuring elderly well-being during COVID-19 using the IoT | - | - | No Implementation/No simulation |
| Kallel et al. [49] | An architecture based on IoT-fog-cloud for smart systems | Effectiveness | Implementation | |
| Ramallo-González et al. [50] | An IoT platform for health data gathering and the fight against the COVID-19 pandemic | - | No detail mentioned | No Implementation/No simulation |
| Lavric et al. [51] | IoT concepts in the Context of the COVID-19 Pandemic | -Improve monitoring capabilities -Better scalability | - | Implementation |
| Mohammedqasim et al. [52] | COVID-19 detection with IoT sensor | High accuracy | - | Implementation |
| Roy et al. [53] | IoMT for early prediction of COVID-19 | Effectiveness | The results of the proposed model need to be guaranteed | Simulation |
| Leila et al. [54] | Patient Health Monitoring System | -Lower cost -Lower energy | - | No Implementation/No simulation |
Kolhar et al. [43] proposed an IoT-based biometric face detection platform for cities under lockdown during COVID-19 outbreaks in a decentralized manner. Their platform utilizes a three-layered edge computing architecture to limit the public’s movement. They used a multi-task cascading deep learning framework to detect faces. On benchmarking datasets, including FDDB and WIDER FACE, they compared the face detection approach to the current state-of-the-art algorithms. Good performance is the benefit of their proposed platform.
Roy et al. [44] developed a novel IoT-based contact and infection tracking framework, notably integrating symptom-based detection. The capacity of this system to combine real-time symptom information with verified COVID-19 cases offered a rapid and efficient means of tracking the illness’s spread, ultimately benefiting the effective utilization of precious resources. The large-scale system’s lack of support is the drawback of their provided framework.
Poongodi et al. [45] provided a powerful health-based IoT system that may enhance COVID-19 management and produce higher outcomes with given resources. The simulation results indicate that the suggested method for infection detection was effective and reliable. Not mentioning enough details is the main disadvantage of the paper, but effectiveness is its advantage.
Rajasekar et al. [46] developed an IoT-based automated tracking approach to identify prospective contacts using RFID tags and mobile phones that function as readers. This would track down those who have crossed the border without knowing those accused of doing so. A 100-percent quarantine of all conceivable primary and secondary contacts would be achievable, with administrative authorities monitoring them. We can point to the approach’s high effectiveness and low cost, not to mention its benefits.
Kumar et al. [47] presented the Blockchain-IoT that enabled the pharmaceutical supply chain. Stakeholders’ confidence will be maintained with the aid of the created framework. It would increase medical necessity and data visibility, openness, and privacy, and reduce the risk of infection by implementing technology to limit the direct participation of employees. COVID-19 may be effectively controlled and managed with the help of this framework.
Pandey et al. [48] assembled a model for elder care in the event of a disaster. The model allows for delivering essential things to the elderly on-demand and guarantees that the client receives the right assistance when needed. In this way, the elderly person’s privacy was protected.
Kallel et al. [49] proposed a modification to IoT-aware business process modeling. The suggested model considered heterogeneous IoT and non-IoT resources, resource capabilities, and quality of service limitations. Their model uses a new IoT-fog-cloud architecture that supports distributed interlayer communication, real-time stream processing, and multi-application execution within a multitenancy architecture. The proposed model uses single sign-on techniques to ensure data integrity within a multitenancy architecture. Effectiveness is the main advantage of the presented model.
Ramallo-González et al. [50] presented an IoT-based integrated solution, CIoTVID, which can act as an opportunistic agent for health data gathering in the fight against the COVID-19 pandemic. The platform consisted of four layers: data collection, data aggregation, machine intelligence, and services. The data aggregation layer was essential in this solution since the data coming from medical devices have an entirely different character than electronic sensors. Individuals, politicians, and clinics might benefit from the platform’s ability to adapt to diverse data and large data volumes. The disadvantage of this study is that it does not go into detail.
Lavric et al. [51] designed, developed, and implemented an integrated COVID-19 patient management system based on the LoRaWAN communication infrastructure. Their system has several advantages over similar solutions, including remotely monitoring symptoms and health of isolated or quarantined individuals without requiring any external interaction with the patient. Two isolated people were observed for the duration of the normal quarantine period to test the proposed system’s performance. They highlighted the suggested solution’s excellent scalability, which can monitor a large number of patients at the same time owing to the LoRaWAN communication protocol. Governments can effectively deploy this method to improve monitoring capabilities while saving lives.
Mohammedqasim et al. [52] developed an in-depth learning optimization system that can deal with imbalanced datasets to enhance patient categorization. The balancing problem is solved using an artificial minority sampling approach, and the most effective features are determined using a recursive feature reduction procedure. The data are separated into training and experimental sets to verify all models once it has been balanced and features extracted. The experimental prediction results demonstrate that the models are stable and compatible with the data, resulting in maximum accuracy. Finally, proposed approaches for dealing with data bias and obtaining high classification accuracy for COVID-19 patients are discussed. The outcomes of this study might help healthcare organizations prioritize assets more effectively.
Roy et al. [53] presented the idea of transfer models for predicting COVID-19 in patients’ chest X-ray pictures early. The dataset for this study came from the Kaggle repository, divided into two classes: COVID-19 Positive and COVID-19 Negative. The suggested model had the best accuracy and the fewest false positive predictions in the experimental sample. This can aid in the early detection of COVID-19 by doctors and technicians. A patient’s health may be tracked remotely via Internet-connected gadgets, often known as the IoMT.
Leila et al. [54] developed an intelligent approach for tracking COVID-19 patients’ health. It is an IoT architecture for monitoring the health of hospitalized patients whose conditions necessitate widespread surveillance. The device combines a portable IoT node with a remote monitoring application that collects clinical data such as temperature and oxygen saturation, among other things, depending on the scenario. The IoT system component creates a local subsystem for the patient, and the robot connects to the Internet to transfer data to a cloud server. The information is delivered to a secure location for long-term storage, which is utilized for real-time monitoring and statistics that the hospital will require in the future.
4.4. IoMT Application
IoMT has been implemented in several areas with other techniques to prevent the spread of COVID-19 and boost effectiveness by lowering the disease’s number of deaths. Research demonstrates that by integrating security measures with this technology, safe IoMT applications may be used. Additionally, the development of new IoMT technologies combined with blockchain, big data, and artificial intelligence offers more useable options.
Table 8 illustrates the classification of the listed articles in the IoMT application category in the COVID-19 era. The main scopes in the IoMT application category are based on the following:
- Transportation.
- Healthcare.
- Education.
- Entertainment.

Table 8.
Reviewed studies in the IoT application classification.
Table 8.
Reviewed studies in the IoT application classification.
| Research | Main Scope | Benefit | Drawback | Simulation/Implementation |
|---|---|---|---|---|
| Ahanger et al. [55] | An IoT–fog–cloud-based system for predicting COVID19 outbreaks | -Accuracy in classification -Better performance -More reliability | Did not investigate the development of a system that produces energy | Simulation |
| Stolojescu-Crisan et al. [56] | An IoT-based intelligent application for avoiding contact with various objects | Management of various appliances and sensors is possible with this application. | -Did not take into account keeping track of the air humidity -Did not take advantage of the thermal cameras to detect fever | Implementation by Raspberry Pi |
| Mohammed et al. [57] | An IoT diagnosis system for detecting COVID-19 | Effectiveness | Long delay | Simulation using Proteus Circuit |
| Bharathi et al. [58] | Smart system for COVID-19 using IoT | Better performance | Additional smart ideas are required for the proposed model | Simulation |
| Paganelli et al. [59] | Remote monitoring of COVID-19 | -Increasing flexibility -Security | -No Implementation or simulation -Did not consider energy consumption | No Implementation/No simulation |
| Saha et al. [60] | Oxygen Saturation Monitoring | High accuracy | Less adaptability | Implementation |
| Yelure et al. [61] | Remote monitoring of Covid-19 | Effectiveness | Additional sensors and functionalities can be added to the suggested model. | Implementation |
Moreover, Table 9 displays the evaluation criteria of this classification.

Table 9.
Evaluation criteria in the IoT Application category.
Ahanger et al. [55] provided an effective method of early detection and prediction of COVID-19. The suggested structure consists of COVID-19 data gathering, classification, mining and extraction, and COVID-19 prediction and decision modeling. The degree of membership was calculated using a temporal recurrent neural network to estimate the geographic region accurately. In addition, an approach was developed to aid in the perception of the suggested model’s feasibility. Their proposed method’s advantages are classification accuracy, better performance, and more reliability.
Stolojescu-Crisan et al. [56] presented an IoT-based method for avoiding contact with various objects and surfaces. They suggest a framework for efficiently connecting smart devices, providing intelligence that assists in automating many daily operations in offices. A smartphone application enables users to control various appliances and sensors.
Mohammed et al. [57] proposed a method to automatically identify the coronavirus from a thermal picture with little human intervention by utilizing a thermal imaging device mounted on a smart helmet. The thermal camera technology was integrated into the smart helmet and combined with IoT technology to provide real-time monitoring of the screening process. The proposed device can also display the pedestrian’s personal information and automatically take their temperature. Effectiveness is the benefit of the proposed method.
Bharathi et al. [58] suggested a concept for future IoT-based pharmaceutical services frameworks connected to general frameworks that screen particular diseases. Several wearables and non-intrusive sensors were exhibited and discussed, focusing on those monitoring basic indications, circulatory strain, and blood oxygen levels. The appropriateness of exchange standards for human services applications was then evaluated. We can point to better performance, not to mention the advantage of the provided framework.
Paganelli et al. [59] presented an IoT-based approach for remote monitoring of COVID-19 admitted patients at home that fulfills the major needs of identification, interoperability, network dynamics, context, reliability, and privacy. As remote monitoring of patients at home, especially during an epidemic, might pose challenges for safe and ethical data collection, our design includes a content management module to ensure transparency and ensure the data’s security. In addition, the research developed techniques to support an adjustable scoring system and adaptation in wearable devices to improve healthcare usefulness and expert adoption.
Saha et al. [60] demonstrated a methodology for monitoring oxygen levels and determining the severity and likelihood of a COVID-19 patient. The framework may also safeguard patient privacy and classify severity. This approach is unique in combining oxygen saturation with the IoT architecture to detect COVID-19, which has never been done before. The oximeter results are combined to produce a specific warning, and a possible categorization is carried out. The chin block delay and overall reaction, as well as throughput, detection, and intensity, are all factors in determining the outcome. This research, in the framework of the IoT, reveals a practical and substantial answer to the world’s present health threat.
Yelure et al. [61] designed a prototype using wearable IoT sensors and a trained deep learning algorithm for monitoring COVID-19 patients. Using different assessment criteria, we conducted a comparison study of CNN and DNN for cough detection. Our findings were also compared to prior research. It may be inferred that a band based on IoT and AI can always follow self-isolated or quarantined COVID-19 patients. The band system was created to track the oxygen level, temperature, pulse rate, and coughing of patients with COVID-19. The band system may collect data from various sensors and send them to physicians or healthcare professionals through Wi-Fi to keep track of the patient’s status. Patients may transmit health updates to doctors without visiting them using this technology. This will prevent COVID-19 patients from coming into contact with the outside world, lowering the chance of the virus spreading and easing the strain on the healthcare system.
4.5. Security
Medical consumers’ insufficient security knowledge exacerbates existing issues and may encourage attacks that endanger patients’ lives. As a result, guaranteeing the IoMT’s security and privacy has become an important problem that needs additional research and solution. It cannot be managed, monitored, or controlled if security cannot be evaluated. Security has also seen significant improvements due to the fast and global adoption of IoMT, which has led to significant applications and technological advancements.
Table 10 depicts the classification of the articles mentioned within the security category of IoMT in the COVID-19 era. The most significant main scopes in the security category are based on the following:
- Availability.
- Privacy.
- Trust.
Moreover, Table 11 displays the evaluation criteria of this classification.

Table 11.
Evaluation criteria in the security category.

Table 10.
Reviewed studies in the security classification.
Table 10.
Reviewed studies in the security classification.
| Research | Main Scope | Benefit | Drawback | Simulation/Implementation |
|---|---|---|---|---|
| Masud et al. [62] | A secure protocol to allow network devices to authenticate the user’s validity in IoMT | -Ensures data privacy -Integrity -More security | - | Implementation |
| Yongjun et al. [63] | A prediction model based on KNN and BPN | -Prediction ability -Fault tolerance ability -High accuracy -High efficiency -Small mean square error | - | Implementation |
| Al-Turjman et al. [64] | An IoMT framework for privacy-preserving | Better performance efficiency | Not focus on mobility environment | Simulation |
| Alam et al. [65] | IoT Framework for online detecting COVID-19 patients | Flexibility | -Not mentioned enough detail of the proposed framework -No implementation of simulation methods using | No Implementation/No simulation |
Masud et al. [62] developed a lightweight and physically secure protocol to allow network devices to authenticate the user’s validity and sensor node before setting up a session key for communication. Thanks to the suggested protocol, the IoMT networks are protected by authentication, secrecy, integrity, and anonymity. In defense against physical assaults, the suggested protocol uses fewer resources and is better for IoT-based medical network applications.
Yongjun et al. [63] presented a novel algorithm called KNN-BP based on the combination of K-Nearest Neighbor (KNN) and Back Propagation Neural Network (BPN). As a first step, the KNN-BP algorithm can detect sensor data. Results are filtered once the prediction has been finished. While the KNN technique has better data consistency than the standard BPN, it also increases the accuracy of the prediction model. The advantages of this technique include its excellent efficiency and minimal mean square error, and there is a significant improvement in the accuracy and efficiency of IoT using the KNN-BP algorithm. The security of the IoT network has been ensured.
Al-Turjman et al. [64] created an environmentally friendly framework that respects privacy. As a result, energy efficiency stabilizes the network performance using Kruskal’s algorithm and the cipher blockchain. Simulated results show that the proposed framework outperforms existing methods. Better performance and efficiency are the advantages of the proposed framework.
Alam et al. [65] created a framework for COVID-19 patients to detect health problems and diagnoses online. Smartphones can track COVID-19 patients reliably. Infectious patients’ conditions can be improved by installing mobile apps on smart devices, reducing time and costs, and enhancing patient performance. Technology such as IoT and blockchain was used to suggest a four-layer design. Flexibility is the benefit of this framework.
5. Discussion and Comparison
The method for analyzing the selected papers in IoMT in the COVID-19 era was described in previous sections. In addition, we categorized and compared the articles based on several factors, including the main scope, simulation/implementation, benefits, drawbacks, evaluation criteria, and so on. This section provides statistical and comparative information on the IoMT in the era of COVID-19 categories.
We found that 41% of the studies had implemented their proposed idea, whereas 27% of the publications employed simulation approaches to assess their new idea. As simulation platforms, we can refer to Python and Proteus. In addition, 27% of the articles did not employ any implementation or simulation, whereas 5% employed both simulation and implementation approaches, as illustrated in Figure 6.
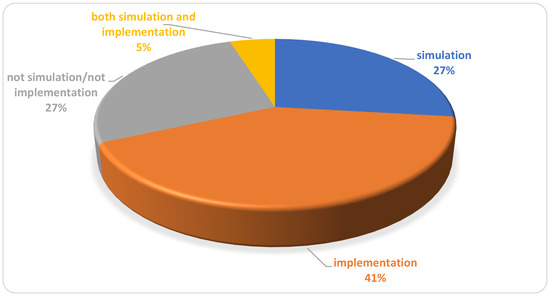
Figure 6.
Percentage of the presented evaluation environments.
The following analytical answers are presented in response to the RQs of Section 2:
RQ1: What are the roles of IoMT in the control and prevention of COVID-19?
The requirement to use IoMT technology during critical periods will pique the interest of inventors, scientists, and developers in IoMT technology, possibly resulting in remarkable growth in the post-COVID era. IoT was mainly associated with larger-scale concepts, such as smart cities and vehicles [2,3].
In this question, the role of IoMT will be discussed in COVID-19 as follows:
- (a)
- Monitoring and screening using IoMT
It might be a highly effective approach to preventing COVID-19 outbreaks. When individuals walk in public areas, drones monitor their body temperatures to see if anyone is suspicious. When individuals maintain social distancing, monitoring can provide reliable information. It can also be used to identify any dense gatherings, which will allow the authorities to take appropriate action. Wireless sensors, facial recognition, and artificial intelligence can all be helpful in this regard. IoMT may be used to improve screening methods [32,33].
- (b) Delivery
Even when restaurants and grocery shops are closed, the IoT can assist in supplying the basics in a user’s place. Users can purchase online via web pages and smartphone applications, and numerous suggestions have been made to utilize robots or drone deliveries to confined individuals to maintain social distance. COVID-19 will be followed by a growth in the home automation sector. It allows us to automate the delivery of products from restaurants and grocery shops by deploying many drones. Benefits include the elimination of the need for a human intermediary and the need for paper-based transactions [66].
- (c) Sanitization
For this pandemic, it is crucial to consider that we need a clean environment. IoMT can improve the government’s efficiency, regularity, and reliability of sanitization efforts. Setting up autonomous drones and cleaning systems that regularly sanitize and record which regions need sanitization is possible. It is not always feasible to sterilize our bodies after touching every object or piece of clothing. Even using a “Self-Sanitizing Suit” can help decrease the problem to a certain level to prevent coronavirus transmission through our clothing. We need an automatic anti-coronavirus suit. The sanitization liquid will be pumped into the suit on a timer. As the product would be in high demand during the COVID-19 era, an effort must be made to reduce its price so everyone can use it [67].
- (d) Digital diagnostics
Advanced digital diagnostics and IoMT connections are useful when combating a worldwide pandemic. Potential paradigm shifts for COVID-19 include digital diagnostics and IoMT connectivity. Many companies have integrated IoT solutions to improve operational activities, develop digital capabilities, and differentiate products and services. So, a variety of IoT devices are utilized to track health data. A smart thermometer replaces regular thermometers with smart thermometers that capture valuable data to protect communities better and share valuable data with health professionals [68].
- (e) Work from home and IoT
Corporate remote working has grown commonplace since the pandemic, and it will only become more frequent in the future. You have more flexibility and may spend less time commuting from your home. IoT sensors and networks enable this, and employment has become more appealing to prospective employees [69].
- (f) E-commerce and IoT
In the constructed environment, COVID-19 has had a significant influence. Due to strict lockout procedures, a substantial reduction in human circulation in buildings has led to bankruptcy. In the context of the pandemic, malls are being transformed into warehouses, mostly due to the expansion of e-commerce. Wholesalers and merchants had difficulty keeping track of inventories during the shutdown because of supply chain network disruptions created by the outbreak. As a result of the IoT, users now have access to more transparent and faster services [69].
RQ2: What are the evaluation criteria in the domains of IoMT in COVID-19?
The evaluation criteria of IoMT in the era of COVID-19 are compared in Figure 7. The statistical percentage of the evaluation criteria proves that the delay factor has a high percentage of the IoT in the COVID-19 era at 38%, the performance has 22%, accuracy has 28%, security has 6%, and cost has 6%.
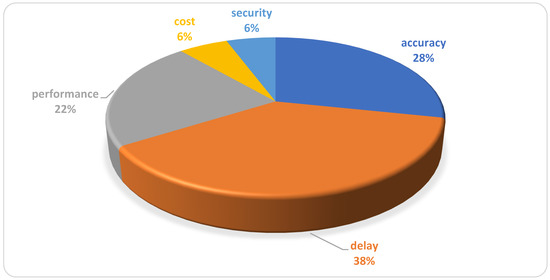
Figure 7.
Evaluation criteria of IoT in the era of COVID-19.
According to the evaluation criteria of the reviewed articles used to evaluate their proposed models, five factors were the most repeated: delay, accuracy, performance, cost, and security, respectively. Among them, the delay is the most frequent, which shows the importance of this factor in evaluating proposed methods in the field of IoMT in COVID-19. Real-time performance is an essential feature for IoMT. Particularly in the COVID-19 era, a low-delay IoMT device has a quick turnaround between when a request is submitted and when the answer returns. Since reducing reaction time is essential for realizing the full potential of the IoMT, researchers are constantly working to achieve this goal. More and more groups are using IoMT data to make decisions in real-time. The data can be useless if there is a long delay. Any IoMT application with a low delay is more likely to provide the most up-to-date data, enabling users to make better-informed decisions. Any application involving autonomous mobility must have low-delay IoMT.
RQ3: What are the effects of COVID-19 on IoMT?
COVID-19 has profoundly affected society, the economy, and innovation and will continue to do so. Effects of COVID-19 on IoT are mentioned in detail in Table 12.

Table 12.
Effects of COVID-19 on IoT.
RQ4: What are the important applications of IoMT for the COVID-19 pandemic?
- (a)
- Healthcare
Due to concerns about contamination in hospitals, there has been a significant decrease in on-site referrals for recurrent care. There has also been a reported desire to monitor non-extreme COVID-19 patients continuously, either at their quarantine sites at home or in committed quarantine locations. As a result, the pandemic has created incentives to innovate and improve or develop new remotely delivered healthcare services [7,37,70].
Some healthcare applications are listed below:
- Body temperature monitoring.
- Remote health monitoring.
- Breathing monitoring.
- Wearable sensor.
- Medication tracking.
- Blood oxygen monitoring.
- (b)
- Education and communication
COVID-19 has resulted in a rise in distance learning and social media usage for educational and communication reasons. Furthermore, the learning process is performed online.
Some education and communication applications are listed below:
- Distance learning.
- Distance communication.
- Virtual studies.
- (c)
- Transportation
Reducing human presence in cars and transportation infrastructure is widely accepted in intelligent transportation systems and COVID-19 standards. On the other hand, the cause of the decreased human presence is quite different. Intelligent transportation systems try to improve transportation services by replacing human handling and supervision with new technology. COVID-19 intends to minimize overcrowding in transportation because an overcrowded bus or train increases the likelihood of infection [71].
Some transportation applications are listed below:
- Public transportation monitoring.
- Intelligent transportation system.
- Smart vehicle.
- Traffic management.
RQ5: What are the future research challenges and open issues of IoMT in COVID-19?
- (a)
- Machine learning
Machine learning and developing a lightweight encryption scheme for distributed storage are the two areas where scientific researchers interested in IoT-based social insurance stand to make the most remarkable improvements. There is no end-to-end framework for specific or general goals that includes all segments in this area: wearable sensors, short- and long-extend correspondences, cloud-based capacity, and machine learning. Growing such a system would be a great accomplishment in IoMT-based medical services and should be a top priority for industry experts [58].Scalability
The integration of technologies to improve the performance of various systems will be the foundation of research in the future. Identifying various barriers and facilitators for adopting an integrated framework in The Public Service Commission would also give helpful information to a strategic planner for better technology adoption. Scalability is still a key challenge for integrating diverse technologies, and it requires the attention of research groups to tackle the implementation problem [47].
- (b) Lack of data
The researchers discovered that not much data are accessible in open data sources linked to the COVID-19 pandemic. It is predicted that more datasets will be available for usage on systems in the coming days. The lack of electronic health records, medical staff, and administrative resources in many developing nations prevents the implementation of the proposed systems. Ideally, the study may be expanded to include more people in better settings in the future post-COVID-19 [29,48,50].
- (c) Flexibility
With COVID-19 being the most important problem, flexibility should be considered because remote monitoring systems should easily be connected to other systems and use existing resources to improve patient safety and provide additional support [71]. Various nations must use flexible manufacturing methods to produce required medical equipment quickly [49,69].
- (d) Transportation
The transportation, logistics, and accommodation industries have all been badly affected by the COVID-19 outbreak. The future solutions will be traceable and transparent logistics, data-driven and self-adaptive decision-making, IoT tracking and monitoring data development, and effective ways to communicate with travelers [69].
6. Conclusions
In this paper, we presented an SLR-based methodology on the IoMT in the COVID-19 era domain based on the observation of 145 papers published between 2019 and 2022. We selected and examined 41 publications to address our five RQs. We showed that in recent years, IoMT has arisen as a key study issue, as COVID-19 has begun a new era. We designed a comprehensive taxonomy and categorized our research reviews into five categories: IoMT engineering, algorithm, architecture and infrastructure, IoMT application, and security. We also looked at this field’s most common evaluation criteria and reviewed and discussed open works and future research. We discovered that most publications had implemented their suggested model as an experimental finding. Delay was considered to be the most significant evaluation factor in this field, according to the examination of the evaluation criteria. Due to the growing number of studies conducted in this field, it will not be easy to verify that all studies have been covered by 2022 when this document is completed.
Author Contributions
Methodology, visualization, validation, writing—original draft, preparation, data curation, A.H.; conceptualization, investigation, writing—review and editing, supervision, A.M.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
There is no conflict of interest.
References
- Dong, Y.; Yao, Y.-D. IoT platform for COVID-19 prevention and control: A survey. IEEE Access 2021, 9, 49929–49941. [Google Scholar] [CrossRef] [PubMed]
- Yousif, M.; Hewage, C.; Nawaf, L. IoT Technologies during and beyond COVID-19: A Comprehensive Review. Future Internet 2021, 13, 105. [Google Scholar] [CrossRef]
- Chaurasia, R.K.; Mishra, R.; Mishra, R.G. The Road Map and Role of Internet of Things (IoT) in COVID-19 pandemic Scenario. Open Transp. J. 2021, 15, 11–15. [Google Scholar]
- Abubakari, M.S. The Internet of Things (IoT) as an Emerging Technological Solution for the COVID-19 pandemic Mitigation: An Overview. In Journal of Physics: Conference Series; IOP Publishing: Bristol, UK, 2021; Volume 1737, p. 012003. [Google Scholar]
- Kumar, K.; Kumar, N.; Shah, R. Role of IoT to avoid spreading of COVID-19. Int. J. Intell. Netw. 2020, 1, 32–35. [Google Scholar] [CrossRef]
- Chamola, V.; Hassija, V.; Gupta, V.; Guizani, M. A comprehensive review of the COVID-19 pandemic and the role of IoT, drones, AI, blockchain, and 5G in managing its impact. IEEE Access 2020, 8, 90225–90265. [Google Scholar] [CrossRef]
- Singh, R.P.; Javaid, M.; Haleem, A.; Suman, R. Internet of things (IoT) applications to fight against COVID-19 pandemic. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 521–524. [Google Scholar] [CrossRef]
- Ndiaye, M.; Oyewobi, S.S.; Abu-Mahfouz, A.M.; Hancke, G.P.; Kurien, A.M.; Djouani, K. IoT in the wake of COVID-19: A survey on contributions, challenges and evolution. IEEE Access 2020, 8, 186821–186839. [Google Scholar] [CrossRef]
- Kumar, M.; Nayar, N.; Mehta, G.; Sharma, A. Application of IoT in Current pandemic of COVID-19. In IOP Conference Series: Materials Science and Engineering; IOP Publishing: Bristol, UK, 2021; Volume 1022, p. 012063. [Google Scholar]
- Kamal, M.; Aljohani, A.; Alanazi, E. IoT meets COVID-19: Status, Challenges, and Opportunities. arXiv 2020, arXiv:2007.12268. [Google Scholar]
- Shamsabadi, A.; Pashaei, Z.; Karimi, A.; Mirzapour, P.; Qaderi, K.; Marhamati, M.; Barzegary, A.; Fakhfouri, A.; Mehraeen, E.; SeyedAlinaghi, S.; et al. Internet of things in the management of chronic diseases during the COVID-19 pandemic: A systematic review. Health Sci. Rep. 2022, 5, e557. [Google Scholar] [CrossRef]
- Javaid, M.; Khan, I.H. Internet of Things (IoT) enabled healthcare helps to take the challenges of COVID-19 Pandemic. J. Oral Biol. Craniofacial Res. 2021, 11, 209–214. [Google Scholar] [CrossRef]
- Chandrayan, S.S.; Suman, S.; Mazumder, T. IoT for COVID-19: A descriptive viewpoint. In Impact of AI and Data Science in Response to Coronavirus Pandemic; Springer: Singapore, 2021; pp. 193–208. [Google Scholar]
- Sharma, A.B.; Nagajayanthi, A.; Kumar, C.; Dinakaran, S. IoT-Based COVID-19 Patient Monitor with Alert System. In Futuristic Communication and Network Technologies; Springer: Singapore, 2022; pp. 1019–1027. [Google Scholar]
- Jahmunah, V.; Sudarshan, V.K.; Oh, S.L.; Gururajan, R.; Gururajan, R.; Zhou, X.; Tao, X.; Faust, O.; Ciaccio, E.J.; Ng, K.H.; et al. Future IoT tools for COVID-19 contact tracing and prediction: A review of the state-of-the-science. Int. J. Imaging Syst. Technol. 2021, 31, 455–471. [Google Scholar] [CrossRef] [PubMed]
- Meraj, M.; Singh, S.P.; Johri, P.; Quasim, M.T. An investigation on infectious disease patterns using Internet of Things (IoT). In Proceedings of the 2020 International Conference on Smart Technologies in Computing, Electrical and Electronics ICSTCEE), Bengaluru, India, 9–10 October 2020; IEEE: New York, NY, USA, 2020; pp. 599–604. [Google Scholar]
- Meraj, M.; Alvi, S.A.M.; Quasim, M.T.; Haidar, S.W. A critical review of detection and prediction of infectious disease using IOT sensors. In Proceedings of the 2021 Second International Conference on Electronics and Sustainable Communication Systems (ICESC), Coimbatore, India, 4–6 August 2021; IEEE: New York, NY, USA, 2021; pp. 679–684. [Google Scholar]
- Razdan, S.; Sharma, S. Internet of Medical Things IoMT, Overview, Emerging Technologies, and Case Studies. IETE Tech. Rev. 2021, 1–14. [Google Scholar] [CrossRef]
- Jain, S.; Nehra, M.; Kumar, R.; Dilbaghi, N.; Hu, T.; Kumar, S.; Kaushik, A.; Li, C. Internet of medical things (IoMT)—Integrated biosensors for point-of-care testing of infectious diseases. Biosens. Bioelectron. 2021, 179, 113074. [Google Scholar] [CrossRef] [PubMed]
- Mazhar, M.S.; Saleem, Y.; Almogren, A.; Arshad, J.; Jaffery, M.H.; Rehman, A.U.; Shafiq, M.; Hamam, H. Forensic Analysis on Internet of Things (IoT) Device Using Machine-to-Machine (M2M) Framework. Electronics 2022, 11, 1126. [Google Scholar] [CrossRef]
- Rehman, A.; Paul, A.; Ahmad, A. A query based information search in an individual’s small world of social internet of things. Comput. Commun. 2020, 163, 176–185. [Google Scholar] [CrossRef]
- Fan, Z.; Jamil, M.; Sadiq, M.T.; Huang, X.; Yu, X. Exploiting multiple optimizers with transfer learning techniques for the identification of COVID-19 patients. J. Healthc. Eng. 2020, 2020, 8889412. [Google Scholar] [CrossRef]
- Rehman, A.U.; Tariq, R.; Rehman, A.; Paul, A. Collapse of Online Social Networks: Structural Evaluation, Open Challenges, and Proposed Solutions. In Proceedings of the 2020 IEEE Globecom Workshops GC Wkshps, Taipei, Taiwan, 7–11 December 2020; IEEE: New York, NY, USA, 2020; pp. 1–6. [Google Scholar]
- Ahmad, R.W.; Salah, K.; Jayaraman, R.; Yaqoob, I.; Ellahham, S.; Omar, M. Blockchain and COVID-19 pandemic: Applications and challenges. IEEE TechRxiv 2020. [Google Scholar] [CrossRef]
- Yacchirema, D.; Chura, A. SafeMobility: An IoT-based System for safer mobility using machine learning in the age of COVID-19. Procedia Comput. Sci. 2021, 184, 524–531. [Google Scholar] [CrossRef]
- Abdulkareem, K.H.; Mohammed, M.A.; Salim, A.; Arif, M.; Geman, O.; Gupta, D.; Khanna, A. Realizing an effective COVID-19 diagnosis system based on machine learning and IoT in smart hospital environment. IEEE Internet Things J. 2021, 8, 15919–15928. [Google Scholar] [CrossRef]
- Shalabi, M. COVID-19 Symptoms Monitoring Mechanism using Internet of Things and Wireless Sensor Networks. IJCSNS 2020, 20, 16. [Google Scholar]
- Ukhalkar, P. Machine learning-based IoT-enabled perspective model for prediction of COVID-19 test in early stage. Mach. Learn. 2020, 29, 2599–2604. [Google Scholar]
- Mukhtar, H.; Rubaiee, S.; Krichen, M.; Alroobaea, R. An IoT Framework for Screening of COVID-19 Using Real-Time Data from Wearable Sensors. Int. J. Environ. Res. Public Health 2021, 18, 4022. [Google Scholar] [CrossRef]
- Yang, C.; Wang, W.; Li, F.; Yang, D. An IoT-Based COVID-19 Prevention and Control System for Enclosed Spaces. Future Internet 2022, 14, 40. [Google Scholar] [CrossRef]
- Akinola, A.; Singh, G.; Hashimu, I.; Prabhat, T.; Nissanov, U. FSS superstrate antenna for satellite cynosure on IoT to combat COVID-19 pandemic. Sens. Int. 2021, 2, 100090. [Google Scholar] [CrossRef]
- Ashraf, M.U.; Hannan, A.; Cheema, S.M.; Ali, Z.; Alofi, A. Detection and tracking contagion using IoT-edge technologies: Confronting COVID-19 pandemic. In Proceedings of the 2020 International Conference on Electrical, Communication, and Computer Engineering ICECCE, Istanbul, Turkey, 12–13 June 2020; IEEE: New York, NY, USA, 2020; pp. 1–6. [Google Scholar]
- Priambodo, R.; Kadarina, T.M. Monitoring self-isolation patient of COVID-19 with Internet of Things. In Proceedings of the 2020 IEEE International Conference on Communication, Networks and Satellite (Comnetsat), Batam, Indonesia, 17–18 December 2020; IEEE: New York, NY, USA, 2020; pp. 87–91. [Google Scholar]
- Misra, S.; Deb, P.K.; Koppala, N.; Mukherjee, A.; Mao, S. S-Nav: Safety-Aware IoT Navigation Tool for Avoiding COVID-19 Hotspots. IEEE Internet Things J. 2020, 8, 6975–6982. [Google Scholar] [CrossRef]
- Rana, M.M.; Abdelhadi, A.; Ahmed, M.R.U.; Ali, A. Secure IoT communication systems for prediction of COVID-19 outbreak: An optimal signal processing algorithm. In Proceedings of the 2020 Third International Conference on Smart Systems and Inventive Technology (ICSSIT), Tirunelveli, India, 20–22 August 2020; IEEE: New York, NY, USA, 2020; pp. 135–139. [Google Scholar]
- Le, D.N.; Parvathy, V.S.; Gupta, D.; Khanna, A.; Rodrigues, J.J.P.C.; Shankar, K. IoT enabled depthwise separable convolution neural network with deep support vector machine for COVID-19 diagnosis and classification. Int. J. Mach. Learn. Cybern. 2021, 12, 3235–3248. [Google Scholar] [CrossRef]
- Cacovean, D.; Ioana, I.; Nitulescu, G. IoT system in diagnosis of COVID-19 patients. Inform. Econ. 2020, 24, 75–89. [Google Scholar] [CrossRef]
- Akhund, T.M.N.U.; Jyoty, W.B.; Siddik, M.A.B.; Newaz, N.T.; al Wahid, S.K.A.; Sarker, M.M. IoT based low-cost robotic agent design for disabled and COVID-19 virus affected people. In Proceedings of the 2020 Fourth World Conference on Smart Trends in Systems, Security and Sustainability (WorldS4), London, UK, 17–28 July 2020; IEEE: New York, NY, USA, 2020; pp. 23–26. [Google Scholar]
- Bashir, A.; Izhar, U.; Jones, C. IoT-based COVID-19 SOP compliance and monitoring system for businesses and public offices. In Engineering Proceedings; Multidisciplinary Digital Publishing Institute: Basel, Switzerland, 2020; Volume 2, p. 14. [Google Scholar]
- Jung, Y.; Agulto, R. A Public Platform for Virtual IoT-Based Monitoring and Tracking of COVID-19. Electronics 2020, 10, 12. [Google Scholar] [CrossRef]
- Bhardwaj, V.; Joshi, R.; Gaur, A.M. IoT-Based Smart Health Monitoring System for COVID-19. SN Comput. Sci. 2022, 3, 1–11. [Google Scholar] [CrossRef]
- Saranya, G.; Dineshkumar, N.; Hariprasath, A.S.; Jeevanantham, G. Design of IoT Enabled Cloud Assisted Health Monitoring System for Covid-19 Patients. In Proceedings of the 2022 Second International Conference on Artificial Intelligence and Smart Energy (ICAIS), Coimbatore, India, 23–25 February 2022; IEEE: New York, NY, USA, 2022; pp. 1227–1232. [Google Scholar]
- Kolhar, M.; Al-Turjman, F.; Alameen, A.; Abualhaj, M.M. A three layered decentralized IoT biometric architecture for city lockdown during COVID-19 outbreak. IEEE Access 2020, 8, 163608–163617. [Google Scholar] [CrossRef]
- Roy, A.; Kumbhar, F.H.; Dhillon, H.S.; Saxena, N.; Shin, S.Y.; Singh, S. Efficient monitoring and contact tracing for COVID-19: A smart IoT-based framework. IEEE Internet Things Mag. 2020, 3, 17–23. [Google Scholar] [CrossRef]
- Poongodi, M.; Nguyen, T.N.; Hamdi, M.; Cengiz, K. A Measurement Approach Using Smart-IoT Based Architecture for Detecting the COVID-19. Neural Process. Lett. 2021. [Google Scholar] [CrossRef] [PubMed]
- Rajasekar, S.J.S. An enhanced IoT based tracing and tracking model for COVID-19 cases. SN Comput. Sci. 2021, 2, 1–4. [Google Scholar]
- Kumar, S.; Pundir, A.K. Blockchain—Internet of things (IoT) Enabled Pharmaceutical Supply Chain for COVID-19. In Proceedings of the NA International Conference on Industrial Engineering and Operations Management Detroit, Detroit, MI, USA, 10–14 August 2020. [Google Scholar]
- Pandey, P.; Litoriya, R. Ensuring Elderly Well-Being During COVID-19 by Using the Internet of Things. Disaster Med. Public Health Prep. 2020, 16, 763–766. [Google Scholar] [CrossRef]
- Kallel, A.; Rekik, M.; Khemakhem, M. IoT-fog-cloud based architecture for smart systems: Prototypes of autism and COVID-19 monitoring systems. Softw. Pract. Exp. 2021, 51, 91–116. [Google Scholar] [CrossRef]
- Ramallo-González, A.P.; González-Vidal, A.; Skarmeta, A.F. CIoTVID: Towards an Open IoT-Platform for Infective pandemic Diseases such as COVID-19. Sensors 2021, 21, 484. [Google Scholar] [CrossRef] [PubMed]
- Lavric, A.; Petrariu, A.I.; Mutescu, P.; Coca, E.; Popa, V. IoT Concept in the Context of the COVID-19 Pandemic: A Multi-Sensor Application Design. Sensors 2022, 22, 503. [Google Scholar] [CrossRef] [PubMed]
- Mohammedqasim, H.; Ata, O. Real-time data of COVID-19 detection with IoT sensor tracking using artificial neural network. Comput. Electr. Eng. 2022, 100, 107971. [Google Scholar] [CrossRef]
- Roy, P.K.; Kumar, A. Internet of Medical Things for early prediction of COVID-19 using ensemble transfer learning. Comput. Electr. Eng. 2022, 101, 108018. [Google Scholar] [CrossRef]
- Leila, E.A.; Othman, S.B.; Sakli, H. IoT Based Patient Health Monitoring System to Combat COVID-19 Pandemic. In Proceedings of the 2022 2nd International Conference on Computing and Information Technology (ICCIT), Tabuk, Saudi Arabia, 25–27 January 2022; IEEE: New York, NY, USA, 2022; pp. 144–147. [Google Scholar]
- Ahanger, T.A.; Tariq, U.; Nusir, M.; Aldaej, A.; Ullah, I.; Sulman, A. A novel IoT–fog–cloud-based healthcare system for monitoring and predicting COVID-19 outspread. J. Supercomput. 2021, 78, 1783–1806. [Google Scholar] [CrossRef]
- Stolojescu-Crisan, C.; Butunoi, B.-P.; Crisan, C. IoT based intelligent building applications in the context of COVID-19 pandemic. In Proceedings of the 2020 International Symposium on Electronics and Telecommunications (ISETC), Timisoara, Romania, 5–6 November 2020; IEEE: New York, NY, USA, 2020; pp. 1–4. [Google Scholar]
- Mohammed, M.N.; Halim Syamsudin, S.; Al-Zubaidi, R.R.; Sairah, A.K.; Yusuf, E. Novel COVID-19 detection and diagnosis system using IoT based smart helmet. Int. J. Psychosoc. Rehabil. 2020, 24, 2296–2303. [Google Scholar]
- Bharathi, N.; Sriramya, P. Smart healthcare system for COVID-19 using internet of things. J. Crit. Rev. 2020, 7, 1697–1702. [Google Scholar]
- Paganelli, A.I.; Velmovitsky, P.E.; Miranda, P.; Branco, A.; Alencar, P.; Cowan, D.; Endler, M.; Morita, P.P. A conceptual IoT-based early-warning architecture for remote monitoring of COVID-19 patients in wards and at home. IoT 2022, 18, 100399. [Google Scholar] [CrossRef]
- Saha, R.; Kumar, G.; Kumar, N.; Kim, T.; Devgun, T.; Thomas, R.; Barnawi, A. Internet-of-Things Framework for Oxygen Saturation Monitoring in COVID-19 Environment. IEEE IoT J. 2021, 9, 3631–3641. [Google Scholar] [CrossRef] [PubMed]
- Yelure, B.S.; Deokule, N.S.; Mane, S.S.; Bhosale, M.V.; Chavan, A.B.; Satpute, C.V. Remote monitoring of Covid-19 patients using IoT and AI. In Proceedings of the 2022 Second International Conference on Artificial Intelligence and Smart Energy (ICAIS), Coimbatore, India, 23–25 February 2022; IEEE: New York, NY, USA, 2022; pp. 73–80. [Google Scholar]
- Masud, M.; Gaba, G.S.; Alqahtani, S.; Muhammad, G.; Gupta, B.B.; Kumar, P.; Ghoneim, A. A lightweight and robust secure key establishment protocol for internet of medical things in COVID-19 patients care. IEEE Internet Things J. 2020, 8, 15694–15703. [Google Scholar] [CrossRef]
- Yongjun, T. Security design and application of Internet of things based on asymmetric encryption algorithm and neural network for COVID-19. J. Intell. Fuzzy Syst. 2020. [Google Scholar] [CrossRef]
- Al-Turjman, F.; Deebak, B.D. Privacy-aware energy-efficient framework using the internet of medical things for COVID-19. IEEE Internet Things Mag. 2020, 3, 64–68. [Google Scholar] [CrossRef]
- Alam, T. Internet of things and blockchain-based framework for Coronavirus (COVID-19) disease. SSRN 2020. [Google Scholar] [CrossRef]
- Siddiqui, S.; Shakir, M.Z.; Khan, A.A.; Dey, I. Internet of Things (IoT) Enabled Architecture for Social Distancing During pandemic. Front. Commun. Netw. 2021, 2, 6. [Google Scholar] [CrossRef]
- Sadhu, A.; Raj, Y.; Chatterjee, S. IoT based corona preventive polycoat with automatic sanitization system. In Journal of Physics: Conference Series; IOP Publishing: Bristol, UK, 2021; Volume 1797, p. 012043. [Google Scholar]
- Mukati, N.; Namdev, N.; Dilip, R.; Hemalatha, N.; Dhiman, V.; Sahu, B. Healthcare assistance to COVID-19 patient using internet of things (IoT) enabled technologies. Mater. Today Proc. 2021. [Google Scholar] [CrossRef]
- Umair, M.; Cheema, M.A.; Cheema, O.; Li, H.; Lu, H. Impact of COVID-19 on IoT Adoption in Healthcare, Smart Homes, Smart Buildings, Smart Cities, Transportation and Industrial IoT. Sensors 2021, 21, 3838. [Google Scholar] [CrossRef] [PubMed]
- Behar, J.A.; Liu, C.; Kotzen, K.; Tsutsui, K.; Corino, V.D.A.; Singh, J.; Pimentel, M.A.F.; Warrick, P.; Zaunseder, S.; Andreotti, F.; et al. Remote health diagnosis and monitoring in the time of COVID-19. Physiol. Meas. 2020, 41, 10TR01. [Google Scholar] [CrossRef] [PubMed]
- Wiseman, Y. Intelligent Transportation Systems along with the COVID-19 pandemic will Significantly Change the Transportation Market. Open Transp. J. 2021, 15, 11–15. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).