Determining Factors in the Implementation of Biosecurity Measures by Hospital Nurses in Piura, Peru
Abstract
1. Introduction
2. Literature Review
2.1. The Main Biosafety Measures in the Hospital Environment
2.2. Factors Influencing the Implementation of Biosafety Measures by Nurses
2.3. Scientific Support of the Research Hypotheses
3. Materials and Methods
3.1. Participants
3.2. Data Collection Instruments
3.3. Procedure and Data Analysis
4. Results
4.1. Results of the Measurement Model
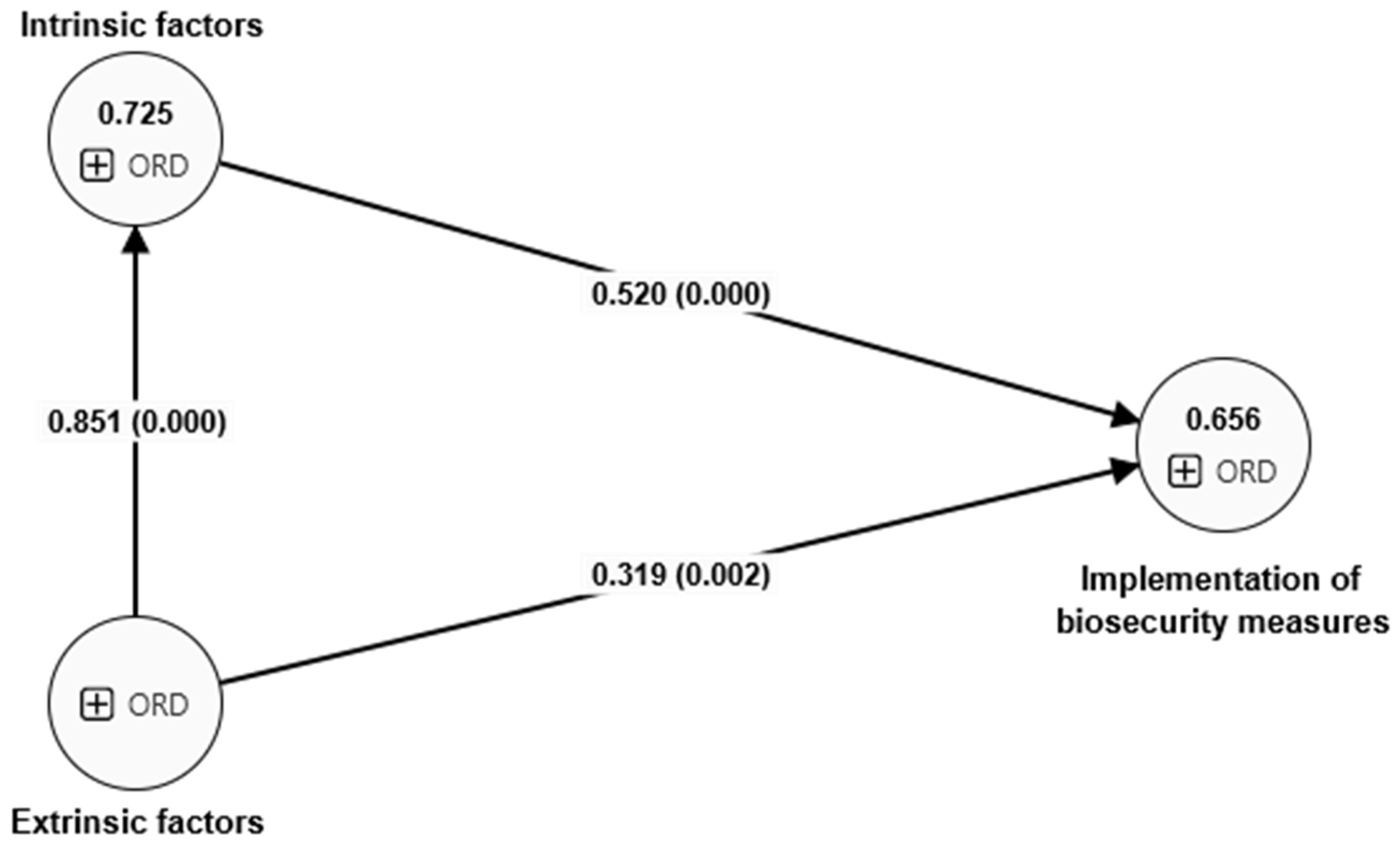
4.2. Contrasting the Research Hypotheses
5. Discussion
6. Conclusions
7. Limitations and Future Studies
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Public Involvement Statement
Guidelines and Standards Statement
Use of Artificial Intelligence
Conflicts of Interest
References
- Rajagopalan, R.; Shivamurthy, M.C. A retrospective evaluation of compliance in various surgical departments with respect to surgical antibiotic prophylaxis in a tertiary care hospital. Res. J. Pharm. Technol. 2013, 6, 749–752. [Google Scholar]
- Shalini, S.; Vidyasree, M.D.; Abiselvi, A.; Gopalakrishnan, S. Impact and effect of nosocomial infections: A review. Res. J. Pharm. Biol. Chem. Sci. 2015, 6, 947–951. [Google Scholar]
- Parsia, Y.; Tamyez, P.F. Role of hospital management on minimization risks of Nosocomial Infections. In Proceedings of the 2nd European International Conference on Industrial Engineering and Operations Management, Paris, France, 26–27 July 2018; pp. 486–487. [Google Scholar]
- Jan Muhammad, F.; Siddiqui, N.; Ali, N.; Kazmi, S.U. Analysis of Biosafety Performance in Selected Hospital Medical Laboratories in Karachi, Pakistan. Appl. Biosaf. 2018, 23, 39–46. [Google Scholar] [CrossRef][Green Version]
- Cárdenas, F.S.C. Factors associated with the application of biosafety measures taken by nursing professionals. Rev. Cuba. De Enferm. 2020, 36, 1–10. [Google Scholar]
- Bai, Y.; Zhang, F.; Lu, Y.; Ning, H.; Kang, J. Management and discussion on strengthening biosafety awareness of medical microbiology researchers. J. Med. Pest Control 2023, 39, 1011–1017. [Google Scholar] [CrossRef]
- Matosova, E.V.; Andryukov, B.G.; Bynina, M.P.; Drobot, E.I.; Lyapun, I.N. Biosafety of personnel of microbiological laboratories in the context of the Federal Law of the Russian Federation № 492-FZ of December 30, 2020 «On the biological safety of the Russian Federation». Klin. Lab. Diagn. 2022, 67, 414–422. [Google Scholar] [CrossRef]
- Seringe, É. Epidemiology and prevention of health care associated infections. La Rev. Du Prat. 2017, 67, 206–210. [Google Scholar]
- Liu, J.Y.; Dickter, J.K. Nosocomial Infections: A History of Hospital-Acquired Infections. Gastrointest. Endosc. Clin. N. Am. 2020, 30, 637–652. [Google Scholar] [CrossRef]
- Horcajada, J.P.; Padilla, B. Endemic and epidemic. Investigation of a nosocomial outbreak. Enfermedades Infecc. Y Microbiol. Clin. 2013, 31, 181–186. [Google Scholar] [CrossRef]
- Yazdani Cherati, J.; Shojaee, J.; Chaharkameh, A.; Rezai, M.S.; Khosravi, F.; Rezai, F.; Dalili, A. Incidence of nosocomial infection in selected cities according NISS software in Mazandaran province. J. Maz. Univ. Med. Sci. 2015, 24, 64–71. [Google Scholar]
- Wang, Z.; Du, M.; Cao, H.; Yao, H.; Liu, B.; Bai, Y.; Geng, H.; Jia, Z.; Liu, Y. Epidemiology and risk factors for nosocomial infections in a Chinese tertiary-care hospital: A 10-year retrospective case–control study. Infect. Dis. 2024, 56, 320–329. [Google Scholar] [CrossRef]
- Liang, J.J.; Rudnick, W.; Mitchell, R.; Brooks, J.; Bush, K.; Conly, J.; Ellison, J.; Frenette, C.; Johnston, L.; Lavallée, C.; et al. Antimicrobial use in Canadian acute-care hospitals: Findings from three national point-prevalence surveys between 2002 and 2017. Infect. Control Hosp. Epidemiol. 2022, 43, 1558–1564. [Google Scholar] [CrossRef] [PubMed]
- Wałaszek, M. The analysis of the occurrence of nosocomial infections in the neurosurgical ward in the District Hospital from 2003–2012. Przegla̧d Epidemiol. 2015, 69, 507–514. [Google Scholar]
- dos Santos Dias de Souza, G.; Pereira Coelho, H.; de Sales, D.; Kéllen, J.; Vieira Pereira, H.C.; Machado Borges, A.M.; de Alencar, V.; Morais, A. Biosafety measures in nursing care to hemodialysis patients: Integrative review. Rev. Baiana De Enferm. 2022, 36, 193–211. [Google Scholar] [CrossRef]
- Brand, C.I.; Fontana, R.T. Biosafety in the perspective of nursing staff of Intensive Care Units. Rev. Bras. De Enferm. 2014, 67, 78–84. [Google Scholar] [CrossRef][Green Version]
- da Silva, G.G.; Neto, D.L.; de Aguiar Campos, M.P.; de Mattos, M.C.; Otero, L.M. Measures for the adhesion to biosafety recommendations by the nursing team. Enferm. Glob. 2018, 17, 58–67. [Google Scholar] [CrossRef][Green Version]
- Jeréz, I.E.H.; Laza, O.U.; Álvarez, J.C.F.; Hernández, L.L. Nursing intervention in intensive care on Biosafety for the care of patients with COVID-19. Rev. Cuba. De Hematol. Inmunol. Y Hemoter. 2021, 37. [Google Scholar]
- da Silveira, S.S.; Gomes da Silva, R.M.; da Silva, M.T.; Teixeira, R.C.; Lemos Goulart, M.D.; Bezerra Góes, F.G.; Vieira Pereira Ávila, F.M.; da Costa Fernandes, A.P.; Dantas Cavalcanti, A.C.; Peclat Flores, P.V.; et al. Nursing students’ knowledge about biosafety in the hospital context during the pandemic: A qualitative approach. Online Braz. J. Nurs. 2023, 22. [Google Scholar] [CrossRef]
- Subbalakshmi, E.; Abirami, P.; Subramanian, V.; Sumitha, A.; Victor, H.K. Awareness of hand hygiene in hospital setup for infection control: Knowledge-based questionnaire for health care workers in a teaching hospital. Biomed. Pharmacol. J. 2020, 13, 1773–1779. [Google Scholar] [CrossRef]
- Rai, A.; Kothari, R.; Singh, D.P. Assessment of available technologies for hospital waste management: A need for society. In Environmental Issues Surrounding Human Overpopulation; Sustainable Infrastructure; IGI Global: Hershey, PA, USA, 2016; pp. 172–188. [Google Scholar] [CrossRef]
- Rai, A.; Kothari, R.; Singh, D.P. Assessment of available technologies for hospital waste management: A need for society. In Waste Management: Concepts, Methodologies, Tools, and Applications; IGI Global: Hershey, PA, USA, 2019; pp. 860–876. [Google Scholar] [CrossRef]
- Kumari Sharma, P.; Singhal, P. Medical waste management. In Medical Microbiology; Elsevier Health Sciences: Philadelphia, PA, USA, 2022; pp. 239–262. [Google Scholar] [CrossRef]
- Das, N.K.; Prasad, S.; Jayaram, K. A tqm approach to implementation of Handling and management of hospital waste in hospital. Asian J. Microbiol. Biotechnol. Environ. Sci. 2016, 18, 1005–1009. [Google Scholar]
- Sengodan, V.C. Segregation of biomedical waste in an South Indian tertiary care hospital. J. Nat. Sci. Biol. Med. 2014, 5, 378–382. [Google Scholar] [CrossRef]
- Forumadi, M.; Vanaei, F.; Mostafaii, G.; Ghafari, Y.; Ghobakhloo, Z.; Ghobakhloo, S. Evaluation of hospital wastes management with emphasis on genotoxic wastes in Semnan University of Medical Science’s hospitals. Int. J. Environ. Health Eng. 2023, 12, 13. [Google Scholar] [CrossRef]
- Núñez, D.V.; Sánchez, E.C.; Díaz, P.H.R.; Escobar, T.T.M. Effectiveness of guide of good practical in the hospital bioseguridad. Rev. Cuba. De Enferm. 2017, 33, 40–51. [Google Scholar]
- Toapanta Llumiquinga, Y.G.; Rivera Aguilar, T.E. Knowledge and perception of biosafety measures in nursing students. Salud Cienc. Y Tecnol. 2023, 3, 496. [Google Scholar] [CrossRef]
- Kang, P.; Kang, J.; Monsen, K.A. Nurse Information Security Policy Compliance, Information Competence, and Information Security Attitudes Predict Information Security Behavior. CIN Comput. Inform. Nurs. 2023, 41, 595–602. [Google Scholar] [CrossRef]
- da Silva, M.A.S.; de Lima, M.C.L.; Dourado, C.A.R.O.; Pinho, C.M.; Andrade, M.S. Nursing professionals’ biosafety in confronting COVID-19. Rev. Bras. De Enferm. 2022, 75, 45–56. [Google Scholar] [CrossRef]
- Lopes Joaquim, F.; Cavalcanti Valente, G.S. The relation of biosafety at the cost-effectiveness in hospitalizations: Nexus with the permanent instruction. Enferm. Glob. 2013, 12, 339–354. [Google Scholar]
- Sari, P.K.; Handayani, P.W.; Hidayanto, A.N.; Yazid, S.; Aji, R.F. Information Security Behavior in Health Information Systems: A Review of Research Trends and Antecedent Factors. Healthcare 2022, 10, 2531. [Google Scholar] [CrossRef] [PubMed]
- Bajjou, T.; Sekhsokh, Y.; Amine, I.L.; Gentry-Weeks, C. Knowledge of Biosafety Among Workers in Private and Public Clinical and Research Laboratories in Morocco. Appl. Biosaf. 2019, 24, 46–54. [Google Scholar] [CrossRef]
- Griffin, Y.; Sullivan, D.; Stray, S. Biosafety Knowledge Among Students at an Academic Medical Center: A Survey Validation by Field Professionals. Appl. Biosaf. 2017, 22, 123–129. [Google Scholar] [CrossRef][Green Version]
- Vandenplas, Y.; Simoens, S.; Van Wilder, P.; Vulto, A.G.; Huys, I. The impact of policy interventions to promote the uptake of biosimilar medicines in Belgium: A nationwide interrupted time series analysis. Health Res. Policy Syst. 2023, 21, 68. [Google Scholar] [CrossRef]
- Chen, A.J.; Ribero, R.; van Nuys, K. Provider differences in biosimilar uptake in the filgrastim market. Am. J. Manag. Care 2020, 26, 208–213. [Google Scholar] [CrossRef] [PubMed]
- Munson, E.; Bowles, E.J.; Dern, R.; Beck, E.; Podzorski, R.P.; Bateman, A.C.; Block, T.K.; Kropp, J.L.; Radke, T.; Siebers, K.; et al. Laboratory focus on improving the culture of biosafety: Statewide risk assessment of clinical laboratories that process specimens for microbiologic analysis. J. Clin. Microbiol. 2018, 56, e01569-17. [Google Scholar] [CrossRef]
- Wu, C.; Zhang, H.; Zhang, Y.; Hu, M.; Lin, Y.; He, J.; Li, S.; Zhang, Y.; Lang, H.J. The biosafety incident response competence scale for clinical nursing staff: A development and validation study. BMC Nurs. 2024, 23, 180. [Google Scholar] [CrossRef] [PubMed]
- Fornell, C.; Larcker, D.F. Evaluating structural equation models with unobservable variables and measurement error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Hair, J.F. Multivariate Data Analysis; Pearson Education Limited: Chapel Hill, NC, USA, 2009. [Google Scholar]
- Nunnally, J.; Bernstein, D.I.H. Psychometric Theory; McGraw-Hill Companies: New York, NY, USA, 1994. [Google Scholar]
- Teo, T.; Noyes, J. Explaining the intention to use technology among preservice teachers: A multigroup analysis of the Unified Theory of Acceptance and Use of Technology. Interact. Learn. Environ. 2014, 22, 51–66. [Google Scholar] [CrossRef]
- Sist, L.; Chiappinotto, S.; Messina, R.; Rucci, P.; Palese, A. The Reasons for Unfinished Nursing Care during the COVID-19 Pandemic: An Integrative Review. Nurs. Rep. 2024, 14, 753–766. [Google Scholar] [CrossRef] [PubMed]
- Toyama, N.; Hokama, C.; Takahara, M.; Toyama, Y. Associations between Difficulty in Accessing Maternal and Child Health Services and Stress Responses among Mothers Raising Young Children during the COVID-19 Pandemic in Japan. Nurs. Rep. 2024, 14, 506–515. [Google Scholar] [CrossRef]
- Ahmed, G.; Almoosa, Z.; Mohamed, D.; Rapal, J.; Minguez, O.; Abu Khurma, I.; Alnems, A.; Al Mutair, A. Healthcare Provider Attitudes toward the Newly Developed COVID-19 Vaccine: Cross-Sectional Study. Nurs. Rep. 2021, 11, 187–194. [Google Scholar] [CrossRef]
| Fi | % | |
|---|---|---|
| Gender | ||
| Male | 51 | 23.8 |
| Female | 163 | 76.16 |
| Age | ||
| 25–30 | 78 | 36.5 |
| 31–35 | 86 | 40. 2 |
| 36–40 | 22 | 10. 3 |
| 41–45 | 9 | 4.3 |
| 46–50 | 9 | 4.3 |
| 51–55 | 9 | 4.3 |
| 56–60 | 1 | 0.4 |
| Service time | ||
| Up to 1 year | 56 | 26.05 |
| Up to 2 years | 34 | 15.81 |
| Up to 3 years | 59 | 27.44 |
| Up to 4 years | 31 | 14.42 |
| More than 5 years | 35 | 16.28 |
| Items | Construct | Outer Loadings | VIF | |
|---|---|---|---|---|
| I consistently perform hand hygiene before and after patient contact. | BIOM1 <- BIOM | Implementation of biosecurity measures (BIOM) | 0.790 | 2.716 |
| I always wear appropriate personal protective equipment when needed. | BIOM10 <- BIOM | 0.766 | 2.047 | |
| I properly dispose of medical waste according to hospital guidelines. | BIOM11 <- BIOM | 0.790 | 3.146 | |
| I follow correct protocols for handling and disposing of sharp objects. | BIOM12 <- BIOM | 0.769 | 2.203 | |
| I maintain a sterile field during invasive procedures. | BIOM13 <- BIOM | 0.742 | 2.678 | |
| I regularly clean and disinfect frequently touched surfaces in my work area. | BIOM14 <- BIOM | 0.770 | 2.613 | |
| I follow isolation precautions for patients with infectious diseases. | BIOM15 <- BIOM | 0.789 | 2.091 | |
| I properly handle and store potentially infectious specimens. | BIOM16 <- BIOM | 0.808 | 3.996 | |
| I educate patients and visitors about necessary biosecurity measures. | BIOM17 <- BIOM | 0.810 | 3.164 | |
| I report any breaches in biosecurity protocols to the appropriate authority. | BIOM18 <- BIOM | 0.816 | 2.292 | |
| I participate in regular biosecurity training and updates. | BIOM19 <- BIOM | 0.764 | 2.603 | |
| I properly use and maintain biosecurity equipment (e.g., biological safety cabinets). | BIOM2 <- BIOM | 0.733 | 2.104 | |
| I follow correct procedures for decontamination of equipment and work areas. | BIOM20 <- BIOM | 0.856 | 2.859 | |
| I adhere to protocols for safe handling and transport of biological materials. | BIOM3 <- BIOM | 0.744 | 2.031 | |
| I implement proper respiratory hygiene and cough etiquette. | BIOM4 <- BIOM | 0.715 | 3.475 | |
| I use aseptic technique when performing clinical procedures. | BIOM5 <- BIOM | 0.702 | 2.502 | |
| I follow protocols for safe handling and disposal of contaminated linens. | BIOM6 <- BIOM | 0.782 | 3.246 | |
| I maintain vaccination status as recommended for healthcare workers. | BIOM7 <- BIOM | 0.885 | 2.537 | |
| I use personal protective equipment correctly and consistently. | BIOM8 <- BIOM | 0.788 | 3.095 | |
| I follow postexposure protocols in case of potential biosecurity breaches. | BIOM9 <- BIOM | 0.775 | 3.475 | |
| My workplace provides adequate personal protective equipment for biosecurity. | FEX1 -> FEX | Extrinsic factors (FEX) | 0.811 | 2.157 |
| There is continuous supervision of biosecurity practices in my hospital. | FEX2 -> FEX | 0.881 | 2.514 | |
| The hospital has clear policies and procedures for biosecurity measures. | FEX3 -> FEX | 0.864 | 2.463 | |
| My workplace offers regular training sessions on biosecurity protocols. | FEX4 -> FEX | 0.901 | 2.636 | |
| I have sufficient knowledge about biosecurity measures. | FINT1 -> FINT | Intrinsic factors (FINT) | 0.891 | 2.754 |
| I feel confident in my ability to implement biosecurity protocols. | FINT2 -> FINT | 0.808 | 2.734 | |
| I believe biosecurity measures are important for patient and staff safety. | FINT3 -> FINT | 0.861 | 2.388 | |
| I actively seek opportunities to update my biosecurity knowledge. | FINT4 -> FINT | 0.837 | 2.724 | |
| My professional experience has improved my understanding of biosecurity practices. | FINT5 -> FINT | 0.845 | 2.303 | |
| α | CR | AVE | R2 | FEX | FINT | BIOM | |
|---|---|---|---|---|---|---|---|
| FEX | 0.859 | 0.857 | 0.685 | 0.751 | |||
| FINT | 0.853 | 0.932 | 0.662 | 0.725 | 0.546 | 0.658 | |
| BIOM | 0.931 | 0.957 | 0.535 | 0.656 | 0.399 | 0.470 | 0.765 |
| Hypothesis | Path | p Value | 2.5% | 97.5% | DE | Interpretation | |
|---|---|---|---|---|---|---|---|
| H1 | FEX -> BIOM | 0.319 | 0.000 | 0.123 | 0.522 | 0.102 | Accepted |
| H2 | FINT -> BIOM | 0.520 | 0.002 | 0.305 | 0.714 | 0.105 | Accepted |
| H3 | FEX -> FINT -> BIOM | 0.443 | 0.000 | 0.265 | 0.601 | 0.086 | Accepted |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Agurto Córdova, L.M.; Espino Carrasco, D.K.; Santa Cruz Espino, B.M.; Espino Carrasco, M.; Vargas Cabrera, C.; Vásquez Cachay, R.; Dávila Valdera, L.; Valdera Benavides, E.D.; Valderrama Soto, R. Determining Factors in the Implementation of Biosecurity Measures by Hospital Nurses in Piura, Peru. Nurs. Rep. 2024, 14, 2117-2129. https://doi.org/10.3390/nursrep14030158
Agurto Córdova LM, Espino Carrasco DK, Santa Cruz Espino BM, Espino Carrasco M, Vargas Cabrera C, Vásquez Cachay R, Dávila Valdera L, Valdera Benavides ED, Valderrama Soto R. Determining Factors in the Implementation of Biosecurity Measures by Hospital Nurses in Piura, Peru. Nursing Reports. 2024; 14(3):2117-2129. https://doi.org/10.3390/nursrep14030158
Chicago/Turabian StyleAgurto Córdova, Luz Mirella, Danicsa Karina Espino Carrasco, Briseidy Massiel Santa Cruz Espino, Mayury Espino Carrasco, Cindy Vargas Cabrera, Royer Vásquez Cachay, Lady Dávila Valdera, Edson David Valdera Benavides, and Roque Valderrama Soto. 2024. "Determining Factors in the Implementation of Biosecurity Measures by Hospital Nurses in Piura, Peru" Nursing Reports 14, no. 3: 2117-2129. https://doi.org/10.3390/nursrep14030158
APA StyleAgurto Córdova, L. M., Espino Carrasco, D. K., Santa Cruz Espino, B. M., Espino Carrasco, M., Vargas Cabrera, C., Vásquez Cachay, R., Dávila Valdera, L., Valdera Benavides, E. D., & Valderrama Soto, R. (2024). Determining Factors in the Implementation of Biosecurity Measures by Hospital Nurses in Piura, Peru. Nursing Reports, 14(3), 2117-2129. https://doi.org/10.3390/nursrep14030158






