Abstract
Background: Leptospirosis is a zoonotic disease that is ubiquitously distributed and is classified as a re-emerging infectious disease in humans and animals. Many serovars are carried by wildlife; all of them are capable of causing illness in humans. The purpose of this study was to investigate the prevalence of Leptospirosis in wild long-tailed macaques (Macaca fascicularis) at Kosumpee Forest Park, Mahasarakham, Thailand. Methods: A cross-sectional study was conducted at the park. Blood samples were collected via saphenous vein from 30 free-ranging long-tailed macaques. All samples were tested by the microscopic agglutination test. The LipL32 gene was used to detect pathogenic Leptospira in blood samples by conventional polymerase chain reaction. Results: Screening of the 30 wild macaques showed an overall Leptospira seroreactivity of 13.33%. Three of 30 macaques reacted against Leptospira serovar Shermani and one macaque was infected with Leptospira serovar Sejroe. None of the macaques presented clinical signs of leptospirosis. None of the blood samples showed the detection of the LipL32 gene. Conclusions: The results indicate that the long-tailed macaques at Kosumpee Forest Park may act as natural reservoirs for Leptospirosis. Further, the results provide evidence-based information indicating that several pathogenic Leptospira serovars are circulating in the wild macaques in the study area.
1. Introduction
Leptospirosis is known as a major endemic bacterial zoonotic disease in Thailand. It is considered to be a neglected tropical disease in many countries, especially in tropical areas [1]. The zoonosis is caused by Gram-negative spirochetes, a spiral-shaped pathogenic bacterium called Leptospira interrogans. The pathogenic Leptospira bacteria has more than 300 diverse serovars [2]. A wide variety mammalian species can play a role as disease reservoirs and carriers that transmit the pathogen to humans and other animals. They harbor the pathogenic Leptospira spp. in renal tubules. These bacteria are shed from the animal reservoirs through their urine and contaminate the environment, usually soils and water [3]. Humans and animals may then be exposed to these pathogenic Leptospira spp. via direct contact with infected animals or through indirect contact with the contaminated water [4].
Detection of antibody titer against Leptospira spp. by the microscopic agglutination test (MAT) is the gold standard method used mainly for serodiagnosis and seroprevalence of leptospirosis in both humans and animals. Given its ability to diagnose a specificity for serogroups and serovars, this method can identify the specific circulating serovars of infected human and animal hosts from their regions [5]. In Thailand, previous reports have revealed that many pets and livestock species serve as reservoir hosts for several predominant serovars of the pathogenic Leptospira interrogans, including serovars Canicola and Bataviae [6,7] in dogs, serovars Bratislava and Pomona in pigs [8], serovar Sejroe and Ranarum in cattle [6,9], serovars Ranarum and Shermani in the bullfighting cattle [10], serovar Pyrogenes in rodents [11], and serovars Mini, Shermani, and Ranarum in sheep and goats [9]. Compared to the work with livestock, there is very little information regarding the status of leptospirosis in wildlife of Thailand, especially in long-tailed macaques (Macaca fascicularis) that often live in shared environments with humans and are considered the most frequently encountered non-human primate species in this region [12]. As such, these macaques represent a potential reservoir host for this disease and, in turn, transmit the pathogen to humans and other animals. Given the potential One Health concern, the purpose of the current study was to assess the prevalence of the Leptospira spp. serovar in a free-ranging population of long-tailed macaques at Kosumpee Forest Park (KFP), Maha Sarakham, Northeastern Thailand. This study was part of a larger, ongoing project addressing human–primate conflict and coexistence [13,14,15] and screening for macaque health [16,17] at KFP.
2. Materials and Methods
2.1. Ethics Statement
This project was conducted in accordance with the animal-use protocol approved by the Institutional Animal Care and Use Committee at Mahasarakham University (IACUC-MSU) for animal subjects research (protocol approval No. 0009/2016). All animal sample collection complied with the applicable laws of Thailand.
2.2. Sample Collection and Procedures
As detailed in our previous studies [15,17], KFP supports a free-ranging population of long-tailed macaques (approximately 850 macaques at the time of the study), distributed among five social groups [14]. KFP is located in Kosum Phisai district, about 27 km from Muang district (city area), Maha Sarakham, Northeast Thailand (Figure 1). There is extensive interaction between the macaques and the local residents and tourists, often resulting in various levels of conflict, including crop raiding, damage to buildings, and aggressive interactions.
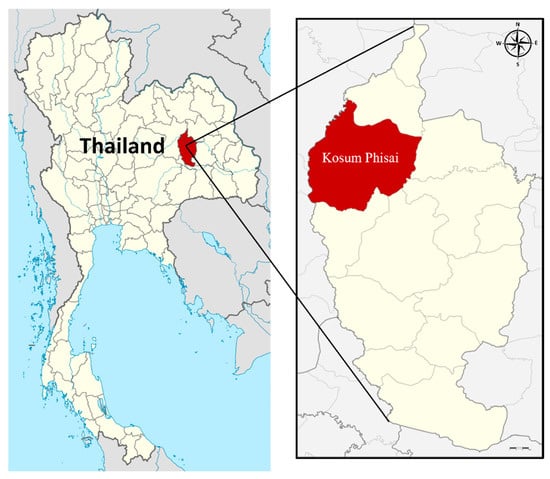
Figure 1.
Map shows Kosum Phisai district, Maha Sarakham in the northeast of Thailand, where the Kosumpee Forest Park is located. (Source: https://en.wikipedia.org/wiki/Maha_Sarakham_province, accessed on 18 September 2022).
Blood samples were collected (10–11 November 2018) from 30 randomly selected free-ranging macaques living around the KFP area during trapping for health screening. All trapping and sampling procedures were conducted by wildlife veterinary specialists from Mahasarakham University (MSU) following the protocol approved by the MSU Institutional Animal Care and Use Committee and the Thai Department of National Parks. Capture procedures, previously described by Pumipuntu and team [17], involved the use of a soft nylon mesh cage with a wooden frame, baited with groundnuts and bananas. An intramuscular injection of Tiletamine-zolazepam (Zoletil® 100 mg/mL, Virbac, Carros, France) was administered via 5 mL anesthetic blowpipes to sedate the macaques in the cage. Following anesthesia, the macaques were removed from the cage, and vital signs were monitored prior to sample collection. Blood samples (5 mL in volume) were aseptically collected via the saphenous vein from each macaque. The samples were then transferred into a sterile plain blood collection tube/red cap (BD Vacutainer, BD, Franklin Lakes, NJ, USA), placed at room temperature for 10 min and separated a serum by centrifugation at 3000 g for 15 min. The separated serum samples were transferred into 1.5 mL sterile microtube (Eppendorf, Hamburg, Germany). All blood samples were processed for DNA extraction with the QIAamp DNA mini kit (Qiagen, Valencia, CA, USA) according to the manufacturer’s instructions. All serum and DNA extraction samples were stored at −20 °C at the Veterinary Public Health Laboratory of the Faculty of Veterinary Sciences at Mahasarakham University for further assessment.
2.3. Microscopic Agglutination Test
All macaque serum samples were analyzed for the presence of Leptosipira-serovar-specific antibodies by the microscopic agglutination test (MAT) and performed according to standard methodology [18] by using a panel of 24 serovars that commonly circulate in the region, namely Pomona, Pyrogenes, Ranarum, Sarmin, Sejroe, Shermani, Tarassovi, Patoc, Canicola, Celledoni, Cynopteri, Ballum, Bataviae, Djasiman, Javanica, Louisiana, Manhao, Mini, Grippotyphosa, Australis, Autumnalis, Hebdomadis, Icterohaemorrhagiae, and Panama. All serum samples were diluted into 1:50 with phosphate-buffered solution (PBS) in a microtiter plate. Subsequently, they were serially diluted two-fold with PBS to set the dilutions to 1:100 to 1:1600. A dilution titer at 1:100 sera was considered as the level to screen the serum for positive leptospirosis.
2.4. Molecular Identification
Bacterial DNA was extracted from all blood samples using a QIAamp DNA mini kit (Qiagen, Hilden, Germany) according to the manufacturer’s instructions. The concentration and purity of DNA extractions from macaques’ blood samples were assessed with the NanoDrop 1000 Spectrophotometer (Thermo Scientific, Branchburg, NJ, USA) by measuring the wavelength at OD 260 and 280 nm, and the purity was measured by obtaining the 260/280 ratio. These DNA extractions were stored at −20 °C for further molecular analysis. All DNA samples were assessed for the LipL32 gene as a means of detecting pathogenic Leptospira bacteria.
Each PCR reaction was carried out in 25 µL, including the DNA template, Taq DNA Polymerase Master Mix (KAPA2G™ Robust HotStart ReadyMix PCR Kit, Kapa Biosystems, Wilmington, MA, USA), sterile deionized water, and 10 µmol/L of both forward and reverse primers of the LipL32 gene. Forward and reverse primers used for targeting the LipL32 gene were 45F (5′-AAG CAT TAC CGC TTG TGG TG-3′) and 286R (5′-GAA CTC CCA TTT CAG CGA TT-3′), respectively. These primers generated a fragment size of 242 base pairs of PCR product, which has been noted to provide both 100% sensitivity and specificity [19]. PCR amplification was conducted with one cycle of initial denaturation at 94 °C for 4 min. PCR amplification was then performed following 35 cycles of denaturation at 94 °C for 30 s, annealing to 53 °C for 30 s, extension at 72 °C for 1 min, and the final extension cycle at 72 °C for 5 min. PCR products underwent electrophoresis by 2% agarose gels in 1X TAE buffer that was stained with ViSafe Red Gel Stain (Vivantis, Selangor, Malaysia) at 100 V for 30 min, and visualized under ultraviolet light. The fragments were identified via VC100bp Plus DNA ladder (Vivantis, Selangor, Malaysia). Sterile water was used as a negative control, and DNA of Leptospira interrogans serovar Sejroe was used as a positive control in each running of the gel electrophoresis.
2.5. Statistical Analysis
Descriptive statistics were used to determine the prevalence of leptospirosis infection and the presence of Leptospira serovar antibodies. Their seroprevalence (percentage) with binomial exact calculation and 95% confidence intervals (CI) were calculated via a free online program (http://sampsize.sourceforge.net/iface/index.html, accessed on 7 August 2022).
3. Results
Of the 30 macaques sampled at KFP, none of the animals presented clinical signs of leptospirosis. From the MAT analysis, antibodies against Leptospira spp. were detected in four (13.33%, 95% CI: 3.76–30.72%) of the macaques. Of the four positive animals, three reacted against Leptospira serovar Shermani (10%; 95% CI: 2.11–26.53%), and one reacted against Leptospira serovar Sejroe (3.33%; 95% CI: 0.08-17.22%) as shown in Table 1. However, of the 30 blood samples analyzed by PCR, none were found to possess the LipL32 gene, which is used to indicate the presence of pathogenic Leptospira bacteria.

Table 1.
MAT and PCR results of Leptospira spp. infection of wild long-tailed macaques.
4. Discussion
Based on the detection of antibodies against Leptospira spp. that were found in the long-tailed macaques at Kosumpee Forest Park, the possibility exists that these macaques act as natural reservoir hosts for leptospirosis. Given the close contact between the macaques and local resident in this shared environment, the opportunity for cross-transmission of zoonotic pathogens presents a real concern; one that also has been noted by others [20,21]. The occurrence of Leptospira seropositivity from the long-tailed macaques in this study (13.33%) was lower than what has been found in some recent studies from other countries, including Southern, Central, and Eastern Thailand, with 48 out of 223 (21.52%) long-tailed macaques [21]; 8 out of the 12 monkeys (66.66%) from Sarawak, Malaysia [22]; 39 out of 83 wild African green monkeys (47%) on the Caribbean island of Saint Kitts, India [23]; 16 out of 52 capuchin monkeys (30.77%) from Colombia [24]; and 39 out of 50 tufted capuchin monkeys (78%) from Southeast Sao Paulo state, Brazil [25].
Regarding the MAT result, Leptospira serovar Shermani was the most prevalent serovar followed by Leptospira serovar Sejroe. This finding is concordant with a previous study that revealed that the most general serovars in humans and livestock in Thailand were Shermani, Ranarum, and Sejroe [26]. Leptospira serovars Ranarum and Shermani were also be found in long-tailed macaques inhabiting Southern, Central, and Eastern regions of Thailand, as described in a recent study [21]. Additionally, Leptospira serovar Sejroe was reported to be circulating in cattle in Maha Sarakham province [6], which represents the same general study area as this current study. Our research provides significant baseline epidemiological information that could be correlated with the occurrence of leptospirosis in both humans and animals in this study area. Moreover, this infectious disease is considered endemic and a significant public health concern in Maha Sarakham province. In fact, between 2004 and 2014, Kosum Phisai district (where our study site was located) reported the second highest number of human cases in the province [27]. Thus, there may be a possibility that various animal species, including wild macaques, could play a potential role in leptospirosis animal reservoirs at this study site, as previous research suggested [27]. It should be noted, however, that our results did not support a role of wild macaques in the transmission of the disease. The occurrence of Leptospirosis in the wild macaques in this study, however, suggests that pathogenic leptospira spp. have persisted as an important bacterial infection in the local wildlife population. Although it seems to be a common contagious bacterial pathogen with subclinical cases in the macaques sampled, its presence as a wildlife zoonotic disease, which can be transmitted to humans and other animals, presents a concern for both veterinary and public health.
The investigation of pathogenic Leptospira bacteria via PCR assay in the blood samples of subclinical long-tailed macaques explained their active infection status and were used to assess the current infection rates within their population, which were determined as potential reservoirs of leptospirosis in this area [28]. However, all of the blood samples were negative for Leptospira. This finding may be the result of the sample-collection period occurring during a time phase without asymptomatic bacteremia status of the long-tailed macaques. As such, the presence of bacteria in the blood was not detected [3]. However, the PCR results could not be used to conclude that the leptospirosis was not present in these wild macaques. Further, there is a possible explanation for negative PCR results. Research has shown that the incidence of leptospirosis shows seasonal variation, with cases of the disease increasing with rainfall intensity [29]. The lack of positive PCR results in the current study may be due to the fact that blood sampling was not conducted during the rainy season.
5. Conclusions
The purpose of the study was to assess the prevalence of Leptospira spp. serovar circulating in a population of free-ranging long-tailed macaques at Kosumpee Forest Park (KFP), Maha Sarakham, Northeastern Thailand. The results revealed the occurrence of leptospirosis in the macaques, which live in close proximity to the local community and have frequent contact with residents and tourists. The findings are crucial in terms of recognizing and identifying the dominant contagious serovars in the study area. Additionally, this evidence-based research on Leptospira serovars indicates that several pathogenic Leptospira serovars are circulating in the wild macaques in the study and might be associated with previous epidemiological data in both humans and animals in the area. As such, we emphasize the need for concern regarding leptospirosis as a potential zoonotic disease in this area. Additional research is needed to monitor the presence of pathogens in other potential animal reservoirs that could be act as leptospirosis carriers so to improve our understanding of the disease circulation in every part in the ecosystem including wildlife, domestic animals, and humans.
Author Contributions
Conceptualization, N.P.; project administration, R.C.K., A.K. and T.T.; sample collection, N.P., P.T., T.T. and A.K.; methodology, N.P., P.T. and T.T.; data analyzing, N.P. and R.C.K.; Drafted and revised the manuscript, N.P., P.K. and R.C.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research project was financially supported by Mahasarakham University (Fast Track 2021). R.C.K. and P.K.’s effort was supported in part by the National Institutes of Health (NIH) Office of Research Infrastructure Programs (ORIP) under award number P51OD010425 to the Washington National Primate Research Center, USA.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
The authors would like to thank all the staff at Kosumpee Forest Park; Pitchakorn Petcharat from Petcharat Animal Clinic; Thanyaphorn Chamnandee, Kittisak Saengthong, Suvit Pathomthanasarn, Ratchanon Kusolsongkhrokul, Papichchaya Doemlim, and Panitporn Damrongsukij from One Health Research Unit VET MSU; the Wildlife and Exotic Friends Club—MSU; and students from the Faculty of Environment and Resource Studies at MSU for their valuable advice and assistance with the sampling in the field. We are grateful to the Faculty of Veterinary Sciences at MSU for the use of its diagnostic laboratory. Finally, we are grateful to the Thailand Department of National Parks—Wildlife and Plant Conservation (DNP) and the National Research Council of Thailand for their approval (NRCT project approval to RCK—Project ID: 2016/048; “Healthy Coexistence between Human and Non-human Primates: A One Health Approach”).
Conflicts of Interest
The authors declare that they have no competing interests in this research.
References
- Narkkul, U.; Thaipadungpanit, J.; Srisawat, N.; Rudge, J.W.; Thongdee, M.; Pawarana, R.; Pan-Ngum, W. Human, animal, water source interactions and leptospirosis in Thailand. Sci. Rep. 2021, 11, 3215. [Google Scholar] [CrossRef] [PubMed]
- Picardeau, M. Virulence of the zoonotic agent of leptospirosis: Still terra incognita? Nat. Rev. Microbiol. 2017, 15, 297–307. [Google Scholar] [CrossRef] [PubMed]
- Haake, D.A.; Levett, P.N. Leptospirosis in humans. Curr. Top. Microbiol. Immunol. 2015, 387, 65–97. [Google Scholar]
- Murray, G.L. The molecular basis of Leptospiral pathogenesis. Curr. Top. Microbiol. Immunol. 2015, 387, 139–185. [Google Scholar] [PubMed]
- Goris, M.G.; Hartskeerl, R.A. Leptospirosis serodiagnosis by the microscopic agglutination test. Curr. Protoc. Microbiol. 2014, 32, 12E.5.1–12E.5.18. [Google Scholar] [CrossRef] [PubMed]
- Pumipuntu, N.; Suwannarong, K. Seroprevalence of Leptospira spp. in cattle and dogs in Mahasarakham province, Thailand. J. Health Res. 2017, 30, 223–226. [Google Scholar]
- Jittapalapong, S.; Sittisan, P.; Sakpuaram, T.; Kabeya, H.; Maruyama, S.; Inpankaew, T. Coinfection of Leptospira spp. and Toxoplasma gondii among stray dogs in Bangkok, Thailand. Southeast Asian J. Trop. Med. Public Health 2009, 40, 247–252. [Google Scholar]
- Tangkanakul, W.; Smits, H.L.; Jatanasen, S.; Ashford, D.A. Leptospirosis: An emerging health problem in Thailand. Southeast Asian J. Trop. Med. Public Health 2005, 36, 281–288. [Google Scholar]
- Suwancharoen, D.; Chaisakdanugull, Y.; Thanapongtharm, W.; Yoshida, S. Serological survey of leptospirosis in livestock in Thailand. Epidemiol. Infect. 2013, 141, 2269–2277. [Google Scholar] [CrossRef]
- Ngasaman, R.; Chanchayanon, B.; Kaewnoi, D.; Kamyingkird, K.A. Variety of Leptospira serovar distribution in bullfighting cattle in southern of Thailand. Zoonotic Dis. 2022, 2, 73–81. [Google Scholar] [CrossRef]
- Kositanont, U.; Naigowit, P.; Imvithaya, A.; Singchai, C.; Puthavathana, P. Prevalence of antibodies to Leptospira serovars in rodents and shrews trapped in low and high endemic areas in Thailand. J. Med. Assoc. Thai. 2003, 86, 136–142. [Google Scholar] [PubMed]
- Malaivijitnond, S.; Hamada, Y. Current situation and status of long tailed macaques (Macaca fascicularis) in Thailand. Nat. Hist. J. Chulalongkorn Univ. 2008, 8, 185–204. [Google Scholar]
- Grant, E.; Kyes, R.C.; Kyes, P.; Trinh, P.; Ramirez, V.; Tanee, T.; Pinloar, P.; Dangtakote, R.; Rabinowitz, P. Fecal microbiota dysbiosis in macaques and humans within a shared environment. PLoS ONE 2019, 14, e0210679. [Google Scholar]
- Kyes, R.C.; Tanee, T.; Thamsenanupap, P.; Karaket, A.; Iskandar, E.; Kyes, P. Population status of the long-tailed macaques (Macaca fascicularis) at Kosumpee Forest Park, Maha Sarakham, Thailand. Am. J. Primatol. 2018, 80, 22. [Google Scholar]
- Schurer, J.; Ramirez, V.; Kyes, P.; Tanee, T.; Patarapadungkit, N.; Thamsenanupap, P.; Trufan, S.; Grant, E.T.; Kelley, S.; Nueaitong, H.; et al. Long-tailed macaques (Macaca fascicularis) in urban landscapes: Investigating gastrointestinal parasitism and barriers for healthy co-existence in northeast Thailand. Am. J. Trop. Med. Hyg. 2019, 100, 357–364. [Google Scholar] [CrossRef] [PubMed]
- Damrongsukij, P.; Doemlim, P.; Kusolsongkhrokul, R.; Tanee, T.; Petcharat, P.; Siriporn, B.; Piratae, S.; Pumipuntu, N. One health approach of melioidosis and gastrointestinal parasitic infections from Macaca fascicularis to human at Kosumpee forest park, Maha Sarakham, Thailand. Infect. Drug Resist. 2021, 15, 2213–2223. [Google Scholar] [CrossRef] [PubMed]
- Pumipuntu, N.; Chamnandee, T.; Saengthong, K.; Pathomthanasarn, S.; Tanee, T.; Kyes, P.; Thamsenanupap, P.; Karaket, A.; Roberts, M.C.; Kyes, R.C. Investigation of methicillin-resistant Staphylococcus aureus (MRSA), methicillin-susceptible Staphylococcus aureus (MSSA) and Staphylococcus argenteus from wild long-tailed macaques (Macaca fascicularis) at Kosumpee Forest Park, Maha Sarakham, Thailand. Vet. World 2022, 15, 2693–2698. [Google Scholar]
- Faine, S.; Adler, B.; Bolin, C.; Perolat, P. Leptospira and Leptospirosis, 2nd ed.; CRC Press: Melbourne, Australia, 1999. [Google Scholar]
- Tan, C.G.; Dharmarajan, G.; Beasley, J.; Rhodes, O., Jr.; Moore, G.; Wu, C.C.; Lin, T.L. Neglected leptospirosis in raccoons (Procyon lotor) in Indiana, USA. Vet. Q. 2014, 34, 1–10. [Google Scholar] [CrossRef]
- Kaewchot, S.; Tangsudjai, S.; Sariya, L.; Mongkolphan, C.; Saechin, A.; Sariwongchan, R.; Panpeth, N.; Thongsahuan, S.; Suksai, P. Zoonotic pathogens survey in free-living long-tailed macaques in Thailand. Int. J. Vet. Sci. 2022, 10, 11–18. [Google Scholar] [CrossRef]
- Saechan, V.; Tongthainan, D.; Fungfuang, W.; Tulayakul, P.; Ieamsaard, G.; Ngasaman, R. Natural infection of leptospirosis and melioidosis in long-tailed macaques (Macaca fascicularis) in Thailand. J. Vet. Med. 2022, 84, 700–706. [Google Scholar] [CrossRef]
- Thayaparan, S.; Robertson, I.D.; Abdullah, M.T. Leptospiral agglutinins in captive and free ranging non-human primates in Sarawak, Malaysia. Vet. World. 2014, 7, 428–431. [Google Scholar] [CrossRef]
- Rajeev, S.; Bolfa, P.; Shiokawa, K.; Beierschmitt, A.; Palmour, R. Leptospira infection in African green monkeys in an endemic area: An opportunity for comparative studies in a natural environment. Pathogens 2020, 16, 474. [Google Scholar] [CrossRef] [PubMed]
- Szonyi, B.; Agudelo-Flórez, P.; Ramírez, M.; Moreno, N.; Ko, A.I. An outbreak of severe leptospirosis in capuchin (Cebus) monkeys. Vet. J. 2011, 188, 237–239. [Google Scholar] [CrossRef] [PubMed]
- Girio, R.; de Andrade-Cruvinel, T.M.; Vasconcellos, S.A.; Repetti, C.; Friolani, M.; Bueno, P.; Felix, M.; Teixeira, D.B. Serological survey and DNA screening of Leptospira spp. in free-living adult tufted capuchin monkeys (Cebus apella nigritus) in a forest reserve Southeast São Paulo State, Brazil. J. Med. Primatol. 2021, 50, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Chadsuthi, S.; Bicout, D.J.; Wiratsudakul, A.; Suwancharoen, D.; Petkanchanapong, W.; Modchang, C.; Triampo, W.; Ratanakorn, P.; Chalvet-Monfray, K. Investigation on predominant Leptospira serovars and its distribution in humans and livestock in Thailand, 2010–2015. PLoS Negl. Trop. Dis. 2017, 11, e0005228. [Google Scholar] [CrossRef]
- Viroj, J.; Claude, J.; Lajaunie, C.; Cappelle, J.; Kritiyakan, A.; Thuainan, P.; Chewnarupai, W.; Morand, S. Agro-Environmental Determinants of Leptospirosis: A Retrospective Spatiotemporal Analysis (2004–2014) in Mahasarakham Province (Thailand). Trop. Med. Infect. Dis. 2021, 6, 115. [Google Scholar] [CrossRef]
- Toyokawa, T.; Ohnishi, M.; Koizumi, N. Diagnosis of acute leptospirosis. Expert Rev. Anti-Infect. Ther. 2011, 9, 111–121. [Google Scholar] [CrossRef]
- Phosri, A. Effects of rainfall on human leptospirosis in Thailand: Evidence of multi-province study using distributed lag non-linear model. Stoch. Environ. Res. Risk Assess. 2022, 36, 4119–4132. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).