Efficacy of Helicobacter pylori Eradication Based on Rabeprazole–Bismuth–Tetracycline–Tinidazole Regimen in Vietnamese Patients with Duodenal Ulcers
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Materials
2.1.1. Selection criteria
2.1.2. Exclusion Criteria
2.2. Study Methods
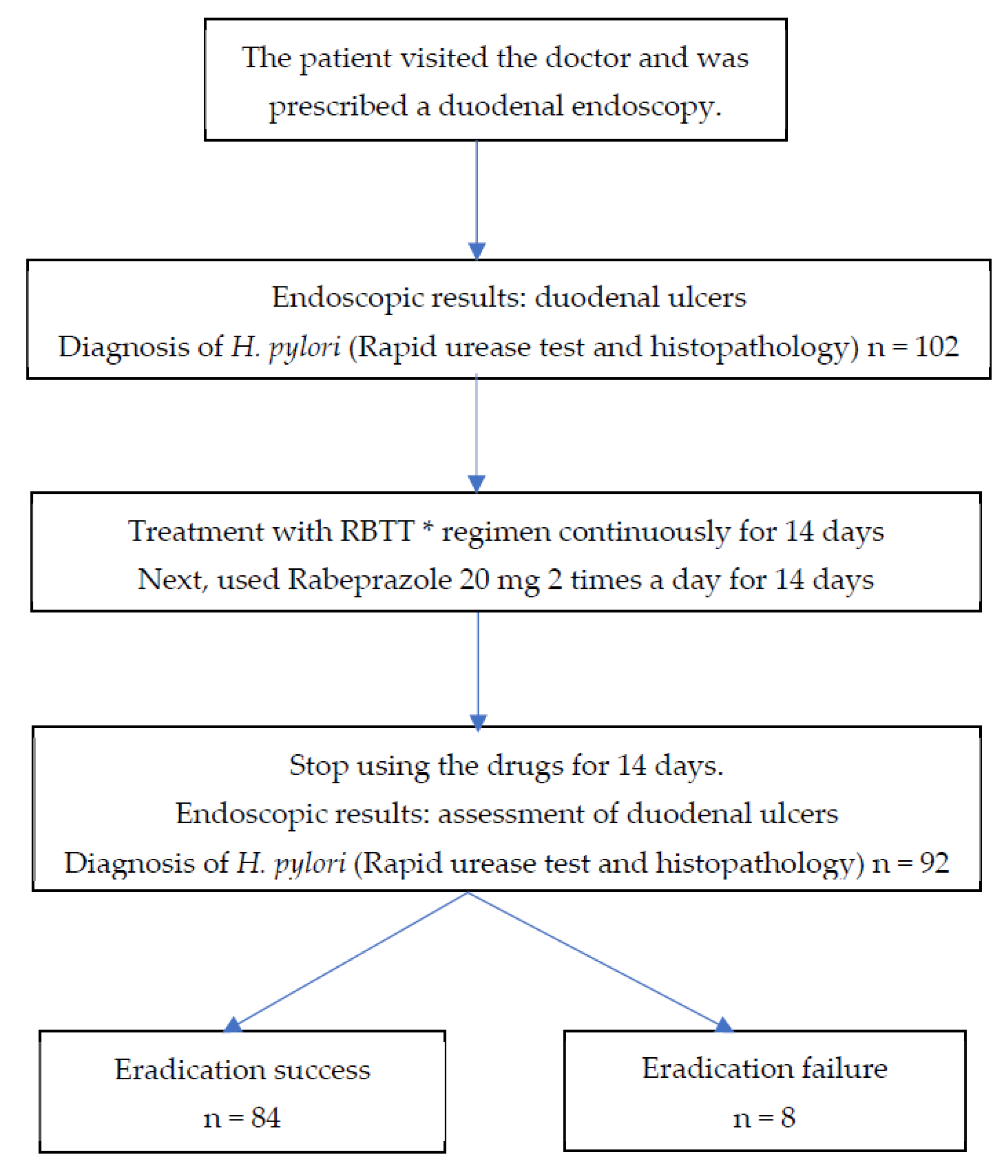
2.2.1. Study Design
2.2.2. Sample Size
- Z21-α/2: confidence coefficient with 95% reliability (1.96).
- d: absolute error (5–10%).
- P: the rate of first successful H. pylori eradication therapy.
2.2.3. Study Facilities
2.2.4. Implementation Steps
- (1)
- Patient reception and clinical examination: The doctor examined the patient, noted the clinical signs, and prescribed an endoscopy. Clinical symptoms: epigastric pain, epigastric burning, hunger pain, burping, nausea, vomiting. The severity of clinical symptoms was assessed using the GSRS scale (Gastrointestinal Symptoms Rating Scale) [14]. Smoking habits were assessed according to the U.S. Centers for Disease Control and Prevention in 2009 [15]. Alcohol consumption was rated according to the AUDIT-C alcohol use disorder screening questionnaire (The Alcohol Use Disorders Identification Test Consumption) by Bradley K.A [16].
- (2)
- Duodenal gastroscopy
- (3)
- Urease test diagnosed Helicobacter pylori
- (4)
- Gastric mucosal histopathology test diagnosed Helicobacter pylori
- (5)
- Treatment of duodenal ulcers contaminated with Helicobacter pylori (Table 1).
- (6)
- Assessment of the efficacy of treating duodenal ulcers with H. pylori infection
- (7)
- Processing and analyzing data
3. Results
3.1. Patients’ Characteristics in the Study
3.2. Results of Helicobacter pylori Eradication Therapy
3.3. Side Effects
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Graham, D.Y. History of Helicobacter pylori, duodenal ulcer, gastric ulcer and gastric cancer. World J. Gastroenterol. 2014, 20, 5191–5204. [Google Scholar] [CrossRef] [PubMed]
- Zamani, M.; Ebrahimtabar, F.; Zamani, V.; Miller, W.H.; Alizadeh-Navaei, R.; Shokri-Shirvani, J.; Derakhshan, M.H. Systematic review with meta-analysis: The worldwide prevalence of Helicobacter pylori infection. Aliment. Pharm. Ther. 2018, 4, 868–876. [Google Scholar] [CrossRef] [PubMed]
- Malfertheiner, P.; Megraud, F.; O’Morain, C.; Bazzoli, F.; El-Omar, E.; Graham, D.; Kuipers, E.J. Current concepts in the management of Helicobacter pylori infection: The Maastricht III Consensus Report. Gut 2007, 56, 772–781. [Google Scholar] [CrossRef] [PubMed]
- Onal, I.K.; Gokcan, H.; Benzer, E.; Bilir, G.; Oztas, E. What is the impact of Helicobacter pylori density on the success of eradication therapy: A clinico-histopathological study. Clin. Res. Hepatol. Gastroenterol. 2013, 37, 642–646. [Google Scholar] [CrossRef]
- Nam, C.B.; Khien, V.V.; Hoan, Q.P.; Nhuong, X.D.; Giang, T.D.; Loan, T.N. Efficacy of Helicobacter Pylori eradication therapy with PCA, PTMB, PLA. Viet. Nam. Gastroenterol. Assoc. 2016, 45, 2851–2854. [Google Scholar]
- Malfertheiner, P.; Megraud, F.; Rokkas, T.; Gisbert, J.P.; Liou, J.M.; Schulz, C.; El-Omar, E.M. Management of Helicobacter pylori infection: The Maastricht VI/Florence consensus report. Gut 2022, 71, 1724–1762. [Google Scholar] [CrossRef]
- Savoldi, A.; Carrara, E.; Graham, D.Y.; Conti, M.; Tacconelli, E. Prevalence of Antibiotic Resistance in Helicobacter pylori: A Systematic Review and Meta-analysis in World Health Organization Regions. Gastroenterology 2018, 155, 1372–1382. [Google Scholar] [CrossRef]
- The Vietnam Association of Gastroenterology. Recommendation and Diagnosis of H. Pylori Treatment in Vietnam; Medical Publishing House: Hanoi, Vietnam, 2013. [Google Scholar]
- Svensson, M.; Ström, M.; Nilsson, M.; Sörberg, M.; Nilsson, L.E. Pharmacodynamic effects of nitroimidazoles alone and in combination with clarithromycin on Helicobacter pylori. Antimicrob. Agents Chemother. 2002, 47, 2244–2248. [Google Scholar] [CrossRef]
- Abbas, S.Z.; Abbas, A.B.; Crawshaw, A.; Shaw, S.; English, J.; McGovern, D.; Dalton, H.R. Diagnosis and eradication of Helicobacter pylori in patients with duodenal ulceration in the community. J. Pak. Med. Assoc. 2003, 53, 90–94. [Google Scholar]
- Berrutti, M.; Pellicano, R.; Astegiano, M.; Smedile, A.; Saracco, G.; Morgando, A.; Rizzetto, M. Helicobacter pylori eradication: Metronidazole or tinidazole? Data from Turin, Italy. Minerva Gastroenterol. Dietol. 2008, 54, 355–358. [Google Scholar]
- Rinaldi, V.; Zullo, A.; De Francesco, V.; Hassan, C.; Winn, S.; Stoppino, V.; Attili, A.F. Helicobacter pylori eradication with proton pump inhibitor-based triple therapies and re-treatment with ranitidine bismuth citrate-based triple therapy. Aliment. Pharm. Ther. 1999, 13, 163–168. [Google Scholar] [CrossRef] [PubMed]
- Kuo, C.H.; Wang, S.S.; Hsu, W.H.; Kuo, F.C.; Weng, B.C.; Li, C.J.; Wu, D.C. rabeprazole can overcome the impact of CYP2C19 polymorphism on quadruple therapy. Helicobacter 2010, 15, 265–272. [Google Scholar] [CrossRef] [PubMed]
- Svedlund, J.; Sjödin, I.; Dotevall, G. GSRS—A clinical rating scale for gastrointestinal symptoms in patients with irritable bowel syndrome and peptic ulcer disease. Dig. Dis. Sci. 1988, 33, 129–134. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention (CDC). State-specific secondhand smoke exposure and current cigarette smoking among adults—United States, 2008. MMWR Morb. Mortal. Wkly Rep. 2009, 58, 1232–1235. [Google Scholar]
- Bradley, K.A.; DeBenedetti, A.F.; Volk, R.J.; Williams, E.C.; Frank, D.; Kivlahan, D.R. AUDIT-C as a brief screen for alcohol misuse in primary care. Alcohol. Clin. Exp. Res. 2007, 31, 1208–1217. [Google Scholar] [CrossRef]
- Dixon, M.F.; Genta, R.M.; Yardley, J.H.; Correa, P. Classification and grading of gastritis. The updated Sydney System. International Workshop on the Histopathology of Gastritis, Houston 1994. Am. J. Surg. Pathol. 1996, 20, 1161–1181. [Google Scholar] [CrossRef]
- Xie, Y.; Zhu, Z.; Wang, J.; Zhang, L.; Zhang, Z.; Lu, H.; Zeng, Z.; Chen, S.; Liu, D.; Lv, N. Ten-Day Quadruple Therapy Comprising Low-Dose Rabeprazole, Bismuth, Amoxicillin, and Tetracycline Is an Effective and Safe First-Line Treatment for Helicobacter pylori Infection in a Population with High Antibiotic Resistance: A Prospective, Multicenter, Randomized, Parallel-Controlled Clinical Trial in China. Antimicrob. Agents Chemother. 2018, 62, e00432-18. [Google Scholar]
- Sapmaz, F.; Kalkan, I.H.; Atasoy, P.; Basyigit, S.; Guliter, S. A Non-Inferiority Study: Modified Dual Therapy Consisting Higher Doses of Rabeprazole Is as Successful as Standard Quadruple Therapy in Eradication of Helicobacter pylori. Am. J. Ther. 2017, 24, e393–e398. [Google Scholar] [CrossRef]
- Wu, M.C.; Wang, Y.K. Adding Bismuth to Rabeprazole-Based First-Line Triple Therapy Does Not Improve the Eradication of Helicobacter pylori. Gastroenterol. Res. Pract. 2017, 5320180. [Google Scholar] [CrossRef]
- Kefeli, A.; Basyigit, S.; Yeniova, A.O.; Kefeli, T.T.; Aslan, M.; Tanas, O. Comparison of three different regimens against Helicobacter pylori as a first-line treatment: A randomized clinical trial. Bosn. J. Basic Med. Sci. 2016, 16, 52–57. [Google Scholar] [CrossRef]
- Gu, L.; Li, S.; He, Y. Bismuth, rabeprazole, amoxicillin, and doxycycline as first-line Helicobacter pylori therapy in clinical practice: A pilot study. Helicobacter 2019, 24, e12594. [Google Scholar] [CrossRef] [PubMed]
- Bang, C.S.; Lim, H.; Jeong, H.M. Amoxicillin or tetracycline in bismuth-containing quadruple therapy as first-line treatment for Helicobacter pylori infection. Gut Microbes 2020, 11, 1314–1323. [Google Scholar] [CrossRef]
- Van Khien, V.; Thang, D.M.; Hai, T.M.; Duat, N.Q.; Khanh, P.H.; Ha, D.T.; Binh, T.T.; Dung, H.D.Q.; Trang, T.T.H.; Yamaoka, Y. Chronic Helicobacter pylori gastritis: The eradiation efficacy of the Bismuth-containing quadruple regimen (EMBT). Viet. Nam. Gastroenterol. Assoc. 2016, 45, 2862–2870. [Google Scholar]
- Huy, T.V. Efficacy of modified Bismuth quardruple therapy (RBMA) as first-line therapy for eradication of Helicobacter Pylori in patients with chronic gastritis. J. Med. Pharm. -Hue Univ. Med. Pharm. 2019, 2, 28–32. [Google Scholar]
- Tuong, T.T.K. The eradication rate of levofloxacin containing quadruple therapy for the first-line treatment of Helicobacter Pylori. Vietnam. Med. J. 2020, 3, 23–26. [Google Scholar]
- Oh, J.H.; Dong, M.S.; Choi, M.G.; Yoo, H.W.; Lee, S.B.; Park, Y.I.; Chung, I.S. Effects of CYP2C19 and MDR1 genotype on the eradication rate of Helicobacter pylori infection by triple therapy with pantoprazole, amoxycillin and clarithromycin. J. Gastroenterol. Hepatol. 2009, 24, 294–298. [Google Scholar] [CrossRef]
- Kang, J.M.; Kim, N.; Lee, D.H.; Park, Y.S.; Kim, J.S.; Chang, I.J.; Song, I.S.; Jung, H.C. Effect of the CYP2C19 polymorphism on the eradication rate of Helicobacter pylori infection by 7-day triple therapy with regular proton pump inhibitor dosage. J. Gastroenterol. Hepatol. 2008, 23, 1287–1291. [Google Scholar] [CrossRef]
- Furuta, T.; Shirai, N.; Xiao, F.; El-Omar, E.M.; Rabkin, C.S.; Sugimura, H.; Ishizaki, T.; Ohashi, K. Polymorphism of interleukin-1beta affects the eradication rates of Helicobacter pylori by triple therapy. Clin. Gastroenterol. Hepatol. 2004, 2, 22–30. [Google Scholar] [CrossRef]
- Furuta, T.; Sugimoto, M.; Shirai, N.; Matsushita, F.; Nakajima, H.; Kumagai, J.; Senoo, K.; Kodaira, C.; Nishino, M.; Yamade, M.; et al. Effect of MDR1 C3435T polymorphism on cure rates of Helicobacter pylori infection by triple therapy with lansoprazole, amoxicillin and clarithromycin in relation to CYP 2C19 genotypes and 23S rRNA genotypes of H. pylori. Aliment. Pharm. Ther. 2007, 26, 693–703. [Google Scholar] [CrossRef]
- Kuo, C.H.; Hsu, P.I.; Kuo, F.C.; Wang, S.S.; Hu, H.M.; Liu, C.J.; Chuah, S.K.; Chen, Y.H.; Hsieh, M.C.; Wu, D.C.; et al. Comparison of 10 day bismuth quadruple therapy with high-dose metronidazole or levofloxacin for second-line Helicobacter pylori therapy: A randomized controlled trial. J. Antimicrob. Chemother. 2013, 68, 222–228. [Google Scholar] [CrossRef]
- Zhang, Y.W.; Hu, W.L.; Cai, Y.; Zheng, W.F.; Du, Q.; Kim, J.J.; Kao, J.Y.; Dai, N.; Si, J.M. Outcomes of furazolidone- and amoxicillin-based quadruple therapy for Helicobacter pylori infection and predictors of failed eradication. World J. Gastroenterol. 2018, 24, 4596–4605. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, S.A.; Al-lela, O.Q.; Hussein, N.R.; Hajany, R.S.; Alduhoky, L.S. Clarithromycin versus Levofloxacin-Based Regimens for Helicobacter Pylori Eradication in the Kurdistan Region of Iraq: A Randomized Clinical Trial. Gastroenterol. Insights 2019, 10, 8256. [Google Scholar] [CrossRef]
- Ghazvini, K.; Kamali, H.; Hosseininasab-nodoushan, S.A.; Keikha, M. The CYP2C19 polymorphisms effects on H. pylori cure rate in proton pump inhibitor-based therapeutic regimens: An updated meta-analysis. Gene Rep. 2021, 25, 101340. [Google Scholar] [CrossRef]
| Rabeprazole (Pariet) 20 mg | |||
| Breakfast: a.c/ 1 tablet | Lunch: a.c 30–60 mins/ 1 tablet | Dinner: none | Bedtime: none |
| Bismuth (Trymo) 120 mg | |||
| Breakfast: a.c 30 mins/ 1 tablet | Lunch: a.c 30 mins/ 1 tablet | Dinner: a.c 30 mins/ 1 tablet | Bedtime: a.c 15 mins/ 1 tablet |
| Tetracycline 500 mg | |||
| Breakfast: p.c 30 mins/ 1 tablet | Lunch: p.c 30 mins/ 1 tablet | Dinner: p.c 30 mins/ 1 tablet | Bedtime: a.c 15 mins/ 1 tablet |
| Tinidazole 500 mg | |||
| Breakfast: p.c/ 1 tablet | Lunch: p.c 30 mins/ 1 tablet | Dinner: none | Bedtime: none |
| Demographic Characteristics | Frequency (n = 102) | Rate (%) |
|---|---|---|
| Sex | ||
| Male | 79 | 77.5 |
| Female | 23 | 22.5 |
| Age | ||
| Mean age | 43.8 ± 13.9 | |
| <30 years | 16 | 15.7 |
| 30-59 years | 73 | 71.6 |
| Weight (kg) | ||
| Mean weight | 59.7 ± 8.5 | |
| Smoking | ||
| Yes | 40 | 49 |
| No | 52 | 51 |
| Alcohol | ||
| Yes | 59 | 57.8 |
| No | 43 | 42.2 |
| Symptoms | ||
| Epigastric pain | 96 | 94.1 |
| Epigastric burning | 61 | 59.8 |
| Burping | 63 | 61.8 |
| Hunger pain | 93 | 91.2 |
| Nausea, vomiting | 21 | 20.6 |
| At least one symptom | 102 | 100 |
| Quantity of ulcers | ||
| 1 | 86 | 84.3 |
| ≥2 | 16 | 15.7 |
| Size of ulcers | ||
| <10mm | 66 | 64.7 |
| ≥10mm | 36 | 35.3 |
| H. pylori bacterial density | ||
| Mild | 57 | 55.9 |
| Medium | 34 | 33.3 |
| Severe | 11 | 10.8 |
| Factor | Result | |||
|---|---|---|---|---|
| Success | Failure | |||
| n | % | n | % | |
| H. pylori (PP) | 84 | 91.3 | 8 | 8.7 |
| H. pylori (ITT) | 84 | 82.4 | 18 | 17.6 |
| H. pylori in males | 72 | 96.0 | 3 | 4.0 |
| H. pylori in females | 12 | 70.6 | 5 | 29.4 |
| Duodenal ulcers | 89 | 96.7 | 3 | 3.3 |
| Clinical signs | 75 | 81.5 | 17 | 18.5 |
| Factor | n | Eradication | p | OR, 95% Cl | |
|---|---|---|---|---|---|
| Success | Failure | ||||
| Age group | |||||
| <60 | 82 | 75 (91.5) | 7 (8.5) | 1.00 | 1.19, 0.13–10.81 |
| ≥60 | 10 | 9 (90.0) | 1 (9.0) | ||
| Gender | |||||
| Male | 75 | 72 (96.0) | 3 (4.0) | <0.01 | 10.00, 2.10–47.41 |
| Female | 17 | 12 (70.6) | 5 (29.4) | ||
| Density of H. pylori | |||||
| Mild | 51 | 48 (94.1) | 3 (5.9) | 0.45 | 2.22, 0.49–9.11 |
| Medium, severe | 41 | 36 (87.8) | 5 (12.2) | ||
| Alcohol | |||||
| Yes | 57 | 52 (91.2) | 5 (8.8) | 1.00 | 0.97, 0.21–4.35 |
| No | 35 | 33 (91.4) | 3 (8.6) | ||
| Smoking | |||||
| Yes | 49 | 44 (89.8) | 5 (10.2) | 0.71 | 0.66, 0.14–2.94 |
| No | 43 | 40 (93.0) | 3 (7.0) | ||
| Factor | OR | 95% Cl | p |
|---|---|---|---|
| Age: ≥60 | 3.05 | 0.20–46.14 | 0.41 |
| Sex: female | 19.12 | 2.83–128.93 | <0.01 |
| Density of H. pylori: medium and severe | 3.19 | 0.58–19.77 | 0.17 |
| Alcohol: yes | 1.68 | 0.12–22.56 | 0.69 |
| Smoking: yes | 2.0 | 0.15–26.82 | 0.59 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nguyen, L.T.; Nguyen, V.B.; Tran, T.V.; Duong, H.Q.; Le, L.T.T.; Phuong, M.H.T.; Nguyen, T. Efficacy of Helicobacter pylori Eradication Based on Rabeprazole–Bismuth–Tetracycline–Tinidazole Regimen in Vietnamese Patients with Duodenal Ulcers. Gastroenterol. Insights 2022, 13, 365-376. https://doi.org/10.3390/gastroent13040036
Nguyen LT, Nguyen VB, Tran TV, Duong HQ, Le LTT, Phuong MHT, Nguyen T. Efficacy of Helicobacter pylori Eradication Based on Rabeprazole–Bismuth–Tetracycline–Tinidazole Regimen in Vietnamese Patients with Duodenal Ulcers. Gastroenterology Insights. 2022; 13(4):365-376. https://doi.org/10.3390/gastroent13040036
Chicago/Turabian StyleNguyen, Liem Thanh, Vuong Ba Nguyen, Tu Viet Tran, Huy Quang Duong, Loan Thi Thuy Le, Mai Huynh Truc Phuong, and Thang Nguyen. 2022. "Efficacy of Helicobacter pylori Eradication Based on Rabeprazole–Bismuth–Tetracycline–Tinidazole Regimen in Vietnamese Patients with Duodenal Ulcers" Gastroenterology Insights 13, no. 4: 365-376. https://doi.org/10.3390/gastroent13040036
APA StyleNguyen, L. T., Nguyen, V. B., Tran, T. V., Duong, H. Q., Le, L. T. T., Phuong, M. H. T., & Nguyen, T. (2022). Efficacy of Helicobacter pylori Eradication Based on Rabeprazole–Bismuth–Tetracycline–Tinidazole Regimen in Vietnamese Patients with Duodenal Ulcers. Gastroenterology Insights, 13(4), 365-376. https://doi.org/10.3390/gastroent13040036






