Abstract
eHealth has transformed transplantation care by enhancing communication between patients and clinics, supporting self-management, and improving adherence to medical advice. However, existing research on eHealth in transplantation remains fragmented, lacking a comprehensive understanding of its diverse users, associated benefits and challenges, and key considerations for intervention development. This systematic review, conducted following the PRISMA guidelines, analyzed the literature on eHealth in transplantation published between 2018 and September 2023 across multiple databases. A total of 60 studies were included, highlighting benefits such as improved patient engagement, accessibility, empowerment, and cost-efficiency. Three primary categories of barriers were identified: knowledge and access barriers, usability and implementation challenges, and trust issues. Additionally, patient-centered design and readiness were found to be crucial factors in developing effective eHealth solutions. These findings underscore the need for tailored, patient-centric interventions to maximize the potential of eHealth in transplantation care. Moreover, the success of eHealth interventions in transplantation is increasingly dependent on robust networking infrastructure, cloud-based telemedicine systems, and secure data-sharing platforms. These technologies facilitate real-time communication between transplant teams and patients, ensuring continuous care and monitoring.
Keywords:
eHealth; transplantation; utilization; integration; user type; barriers; benefits; development process 1. Introduction
‘eHealth’ refers to the use of digital technologies and electronic communication tools in the healthcare industry to improve healthcare delivery, patient outcomes, and accessibility [1]. Around the world, the landscape of eHealth is witnessing rapid advancements and adoption. The World Health Organization reported that national mobile health interventions are present within 83% of member states, 58% have implemented successful eHealth strategies, and 78% have enacted laws safeguarding electronic patient data [2]. The COVID-19 pandemic has accelerated the adoption of telemedicine, telehealth, and virtual health, highlighting the importance of remote healthcare solutions. Research has shown that 58% of countries have used telemedicine since the pandemic began [3]. While the terms ‘telemedicine’ and ‘telehealth’ have historically been used to describe remote healthcare services, recent literature and practices have shifted towards using the term ‘virtual health’ [4,5,6,7]. For consistency and to reflect these emerging trends, this paper adopts ‘virtual health’ as the preferred term for digital health interventions in transplantation care. It is important to note that ‘virtual health’ encompasses telemedicine, telehealth, and related digital tools, and these terms are often used interchangeably in literature. As such, the studies referenced in this paper may use ‘telehealth’ or ‘telemedicine,’ and these terms will be retained when citing specific research. Additionally, innovations in artificial intelligence (AI)-driven diagnostics, personalized medicine, and data analytics are revolutionizing global healthcare delivery, providing more efficient, patient-centered approaches [8]. For transplantation care, the successful integration of virtual health relies on digital communication networks that enable remote patient monitoring, virtual consultations, and access to electronic health records (EHRs) across healthcare settings. The growing use of Internet of Medical Things (IoMT) devices, cloud computing, and blockchain for health data security has significantly enhanced real-time data exchange and patient engagement [9,10]. Furthermore, 5G-enabled virtual health and AI-assisted platforms provide low-latency remote monitoring and decision support in transplantation care [11].
Although eHealth has demonstrated benefits across several domains of healthcare—including pediatric, trauma, and cancer care [4,5,6]—transplantation care involves a uniquely complex and longitudinal treatment pathway. Patients require ongoing evaluation, multidisciplinary coordination, and lifelong follow-up, which can be greatly enhanced through digital health solutions [7,8,9,10,11,12,13,14,15,16,17,18]. eHealth technologies address critical needs in this domain by reducing barriers to care, improving medication adherence, and enabling remote monitoring—particularly important for immunocompromised patients [12,13]. Moreover, the success of transplantation outcomes depends on secure, timely communication and integrated health information systems, areas where digital innovations such as telemedicine, cloud platforms, and blockchain technologies offer substantial value [8,11,14,15]. These specific needs highlight the necessity for a focused investigation into the role and efficacy of eHealth within transplantation care.
eHealth has been applied to several types of healthcare services, including pediatric care [12], cancer care [13], trauma care [16], and transplantation [17]. Scholars argue the critical role of eHealth in transplantation as it has significantly enhanced patient care, optimized organ allocation, and improved post-transplant outcomes [17]. Through virtual health and remote monitoring technologies, eHealth facilitates pre-transplant evaluations, enabling healthcare providers to assess potential recipients remotely, thereby reducing geographical barriers and expediting the evaluation process [18]. Moreover, eHealth solutions enable real-time communication between transplant teams, allowing seamless collaboration among specialists regardless of location. During the post-transplantation process, remote monitoring tools aid in tracking patient progress, vital signs, and medication adherence, fostering timely interventions and reducing the need for frequent in-person visits, especially critical in the early stages of recovery [17].
Overall, eHealth innovations significantly improve transplant care by optimizing workflows, enhancing communication, and ensuring personalized, continuous care for transplant recipients. However, according to Duettmann and colleagues [19], existing eHealth in transplantation studies are fragmented. Duettmann and colleagues [19] reviewed eHealth innovations in transplantation, highlighting their potential to improve workflows, communication, and personalized care. However, their analysis revealed a fragmentation in the field—a lack of integration and consistency across studies. Transplant types and eHealth adoption vary significantly due to the unique needs and challenges associated with different organ transplants. For example, kidney transplant recipients often require long-term remote monitoring for renal function [20], while lung transplant patients may need continuous monitoring of frailty status and pulmonary function using wearable technology [21]. Unlike general chronic disease management, transplantation involves medication adherence, frequent follow-ups, and a heightened risk of complications, making tailored eHealth solutions crucial [22,23]. Additionally, factors such as the level of digital health literacy, trust in technology, and concerns about data security impact adoption differently across transplant populations [22,24]. Understanding these contextual differences ensures that eHealth interventions are designed to meet the specific needs of transplant recipients, leading to better engagement, adherence, and health outcomes. These studies employed diverse eHealth interventions, such as ‘telehealth’ for remote healthcare services and patient education [12,25] and ‘telemedicine’ for virtual clinician–patient consultations and medication-related clinic visits [18,26]. While providing valuable insights, the existing review falls short of offering a cohesive synthesis of findings or addressing contextual differences in eHealth adoption.
For this reason, to develop a comprehensive understanding of the advantages and barriers posed by eHealth in transplantation, and to delineate future research paths, it is essential to analyze and synthesize the collective body of relevant studies [27]. Therefore, this study aims to systematically review prior studies to identify the factors that have been investigated for their impact on the utilization and incorporation of eHealth in transplant care. Furthermore, it seeks to formulate an integrated framework on the application of eHealth for transplantation purposes. Given the fragmentation in existing research, as highlighted by [19], this study aims to address the lack of cohesion and consistency by offering a more comprehensive and integrated analysis of eHealth applications across different transplant types. By doing so, it will help identify the key factors influencing the adoption of eHealth in transplantation and guide the development of more tailored and effective digital health strategies. To guide this systematic review and synthesize insights from the literature, we formulated the following research questions prior to data extraction and analysis:
- What evidence exists regarding the effectiveness of specific eHealth tools (e.g., virtual health, health apps, wearables) in improving health outcomes for transplant patients?
- Who are the primary user groups of eHealth devices in the transplantation context, and how do their needs and experiences differ?
- What are the predominant barriers hindering the widespread adoption of digital health tools among different user groups (e.g., patients, healthcare providers)?
- What are the key benefits of eHealth tools for pre- and post-transplant care?
- What are the critical factors to consider in designing and implementing eHealth interventions for transplant patients?
2. Methods
2.1. Data Sources and Search Strategies
This systematic review followed the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines [28]. The first step of this process was using the research questions to help shape and develop a search strategy to capture all related and eligible papers in the targeted database. In this case, the following keywords were identified: “eHealth”, “digital health”, “telehealth”, “health informatics”, “electronic health”, “mHealth”, “mobile health”, and “transplant”. A systematic search of the literature on eHealth in transplants was conducted through the databases of Business Source Complete, PubMed, IEEE Xplore, JSTOR, Scopus, SpringerLink, ClinicalKey, ScienceDirect, Wiley Online Library, OVID, and Web of Science. The search was conducted within the databases by selecting eHealth-related terms using an OR operator (e.g., “eHealth OR electronic health OR digital health” OR “telehealth” OR “mhealth” [Title/Abstract]) and using the Boolean operator “AND” to search the keyword transplant simultaneously. The review focuses on articles published from 2018 onward to ensure the inclusion of the most recent and relevant findings. This timeframe reflects the rapid evolution of eHealth technologies, such as virtual health, digital tools, and their increasing integration into transplant care practices. Since technology and healthcare delivery methods have advanced significantly in recent years, studies published before 2018 may not adequately capture the current state of eHealth applications, their capabilities, or emerging challenges. The initial search was conducted between September and October 2023 and yielded a total of 30,996 publications.
2.2. Eligibility Criteria and Selection of Studies
We searched for systematic literature reviews where the intervention was any digital health tool for transplantation purposes. Studies were included if they were
- Peer-reviewed articles;
- Empirical studies using primary or secondary data;
- Published in English (due to the team’s inability to translate articles);
- Studies published between 2018 and September 2023.
Exclusion criteria were
- Non-English studies;
- Secondary research and conceptual papers (e.g., review studies that incorporated theoretical studies or opinions as primary sources of evidence);
- Non-peer reviewed papers;
- Papers older than 2018;
- Full text not available;
- Search terms not found in the abstract;
- Books, PhD and Masters theses, and conference abstracts.
We screened titles and abstracts applying the criteria above. Articles identified throughout the search strategy were collected in a Microsoft Excel spreadsheet. The duplicated articles were excluded through filters, cell formulas, and manual checks. After reviewing the full texts of the remaining papers, both reviewers completed the selection process. We checked the justifications for the excluded studies. All discrepancies were addressed through discussion, seeking agreement from both reviewers (IF and FH) to mitigate potential selection bias.
2.3. Data Extraction
A pre-defined Microsoft Excel spreadsheet was used to code the eligible articles and collect the extracted data. The following data were extracted for each selected article: author(s)/year, objective of study, study design/methodology, type of transplant, health technology, participants, number of participants, country, and main findings.
3. Results
After removing articles that met the inclusion and exclusion criteria, a total of 30,764 articles were removed. The next step was identifying and removing duplicates, which meant 44 duplicate records were removed. The next step was screening the remaining 232 articles for its relevance. In total, 110 articles were removed as they were not relevant for the purpose of this study, which meant 122 articles remained for the next step. Then, we retrieved the full-text articles for the identified relevant studies. The full paper of 33 articles could not be retrieved, which meant 89 articles remained for the eligibility phase to assess the eligibility of the studies to be included in the systematic review. In this phase, the full-text articles were assessed to determine whether they met the eligibility criteria. After reviewing the full texts of the remaining papers, we completed the selection process. All discrepancies were addressed through discussion, seeking agreement from both reviewers to mitigate potential selection bias. To ensure a comprehensive review, a manual search in relevant journals was conducted, and a supplementary search in Web of Science identified five additional studies that met the inclusion criteria. Therefore, a total of 60 articles were included in this literature review. An overview of all selected studies is presented in Table 1, with the first author, year of publication, name of journal/conference, and the type of digital health (more details of these articles are presented in Table A1, Appendix A). Figure 1 presents the flowchart, which illustrates the selection process for the articles included in this systematic literature review.

Table 1.
List of selected studies by type of digital health and human–technology interaction.
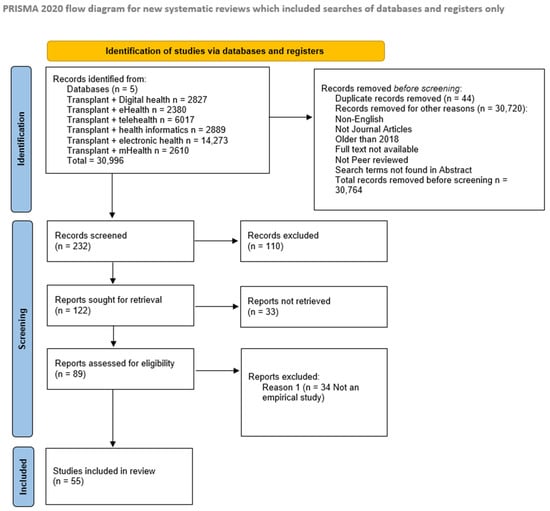
Figure 1.
PRISMA flow chart of the systematic review on the eHealth interventions for transplantation purposes.
3.1. End-User Communication and Interaction with Technology
As shown in Table 1, the interaction between end-users, including patients, their families, healthcare practitioners, and pharmacists, with technology plays a critical role in transplant patient care. Patients and their families primarily utilize mobile health applications and telehealth platforms to track vital health information, manage medication adherence, and maintain communication with healthcare providers [20,22,29]. These technologies empower patients to take an active role in managing their health, with features such as medication reminders and health alerts [30]. Pharmacists and healthcare practitioners, in turn, leverage these digital tools to remotely monitor patients’ medication, health metrics, and overall well-being, ensuring continuous care post-discharge [10,31,32,33]. Additionally, the use of AI-driven tools allows healthcare providers to predict long-term risks, such as graft failure, enabling early intervention [34]. The integration of these technologies fosters improved communication, enhances patient self-management, and supports efficient care coordination, particularly for patients in rural or remote areas [35,36].
3.2. Characteristics of Included Study
Out of 60 studies, 38 (63%) of them used quantitative methods, 9 (15%) studies used qualitative methods, and 13 (22%) applied a mixed-methods approach. In terms of the transplant context, 15 (25%) studies covered the use of digital tools in multi-organ transplant; 20 (33%) of them studied the role of digital health tools in kidney transplant; 6 (10%) studies investigated the role of digital health tools for heart transplants. Most studies, 40 (67%), have been conducted in America; 10 (17%) studies in Europe; 9 (15%) of them in Asia-Pacific; only 1 (2%) study in the Middle East. In terms of participants, 46 (77%) studies were conducted among patients as the users of the digital health devices; 4 (6%) of them were among family members; 10 (17%) of them among care providers, as shown in Table 2.

Table 2.
Characteristics of included studies.
3.3. Descriptive Overview
Paired word cloud analysis refers to the technique of comparing two or more word clouds side by side [74]. This approach helps identify similarities and differences in word frequency, sentiment, or themes across various datasets [74]. The paired word cloud analysis was applied over the abstracts and titles to identify recurring concepts/themes within the selected studies. The analysis from the title word cloud depicts the words that have been used often: (a) health with 12 repetitions, (b) mobile with ten repetitions, (c) technology with eight repetitions, (d) kidney transplant recipients with seven repetitions, and (e) transplant with six repetitions. The analysis from the abstract word cloud depicts the words that have been used often: (a) transplant with 160 repetitions, (b) patients with 148 repetitions, (c) telehealth with 74 repetitions, (d) technology with 34 repetitions, and (e) mobile with 32 repetitions.
The high repetition of technology and transplantation indicates the strong connection between the two concepts. The strong connection between “technology and transplant” is evident from the consistent and prominent repetition of these terms across both titles and abstracts. This pattern underscores the centrality of technology as a recurring theme in the research and its critical role in improving transplantation care and outcomes. Given the consistent focus on these interconnected themes, the purpose of this study is to investigate the role technology (eHealth) plays in transplantation. This focus on technology’s integration into transplantation care is grounded in a comprehensive review of the existing literature and relevant studies, ensuring that the research is impartial and based on a broad range of perspectives. By examining various technological approaches and their application to transplantation, this study remains objective and trustworthy in its findings. Another term that was highly repetitive was kidney transplant recipients, which highlights the importance of studying the different types of transplants. Another noteworthy connection is the high repetition of telehealth and mobile, which highlights the importance of investigating the types of digital health interventions used. Figure 2 shows the word cloud on selected studies’ article titles and selected studies’ abstract.

Figure 2.
Frequent words in title and frequent words in Abstracts.
3.4. Extracted Themes
Based on the extracted themes from the selected studies, we developed a conceptual framework to present the critical factors of using digital health by different stakeholders for transplantation (as shown in Figure 3), such as the involved users of the digital health (e.g., caregivers), the barriers to using digital health for transplant (e.g., knowledge and access barriers), benefits of using digital health for transplant (e.g., improved patient care), the development process of digital health for transplant (e.g., patient-centered) and the type of used digital health for transplant purposes (e.g., mobile health).
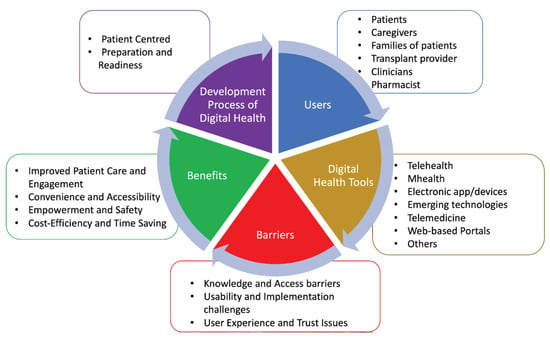
Figure 3.
Conceptual framework on the use of digital health for transplant.
3.4.1. Users
The majority of studies (46 out of 60) focused on patients as the users of digital health devices, while in four studies, caregivers and families of the patients were the users of these devices. In three studies, transplant pharmacists were the users of these devices. In one study, transplant providers were the users of these devices, and in another study, clinicians were the users of these devices.
3.4.2. Process of Development of Digital Health Tools
Five studies have outlined the process of developing digital health interventions for transplantation use. Patient-centered and preparation and readiness are the common themes that studies have identified as being important factors in the process of developing digital health [10,37].
3.4.3. Benefits of Using Digital Health Tools
Out of 60 analyzed studies, 37 studies have identified various benefits of using health devices for transplantation purposes. These findings have been grouped into four main categories: (1) improving patient care and engagement, (2) convenience and accessibility, (3) empowerment and safety, and (4) cost-efficiency and time-saving.
3.4.4. Barriers of Using Digital Health Tools
Out of 60 studies, nine of them have explored challenges and barriers to using digital health technologies and interventions for transplant purposes. These findings have been grouped into three main categories including (1) knowledge and access barriers, (2) usability and implementation challenges, and (3) user experience and trust issues. Regarding the knowledge and access barriers towards using digital health devices, six of the analyzed studies have highlighted the underlying reasons behind these barriers such as poor IT literacy and health literacy (HL), socio-economic factors and language barriers, and poor IT acceptance. In particular, poor IT acceptance was commonly observed among older adults and individuals from lower socio-economic backgrounds [38,39]. These groups often struggle with adapting to new technologies due to a lack of familiarity, insufficient training, and a general reluctance to engage with digital tools. Devices used in the studies varied widely, including computers, smartphones, and tablets [40,41,42,43]. The level of competency in using these devices differed greatly among patients, with many patients requiring additional training or support to navigate these tools effectively [22,24,39,44,45]. Additionally, concerns regarding data security and distrust of technology were noted as significant factors discouraging adoption, leading to lower engagement with digital health solutions despite their potential benefits [24,38]. It is also crucial to note that patients’ access to digital devices and IT connections—whether self-owned or provided by the healthcare system—can significantly affect their ability to engage with these tools.
Regarding the usability and implementation challenges with using digital health tools, five of the analyzed studies highlighted the root causes behind these barriers such as manual and continuous data entry, poor decisions because of inaccurate data from the patient’s end, lack of professional support, poor dissemination of digital intervention, and costs. Six analyzed studies emphasized the underlying reasons behind the user experience and trust issues associated with utilizing digital health tools. These challenges encompassed issues such as privacy and security concerns, lack of human connection, and outdated/inconsistent information.
3.4.5. Different Types of eHealth Tools
Out of 60 studies, 22 studies investigated mHealth, 19 studies investigated telehealth, 10 studies looked at electronic apps/devices (e.g., digital health home spirometry, electronic mental health screening), three studies used web-based portals, two studies used emerging technologies (e.g., AI, wearables), two studies looked at telemedicine, and two studies used other forms of tech (e.g., health information technology and interactive health technology). A summary of the extracted themes, key indicators, and related references is presented in Table 3.

Table 3.
Summary of Main Extracted Themes and Related References.
The analyzed studies showed that telehealth and mHealth applications enhance patient engagement and accessibility, but their effectiveness depends on high-speed internet connectivity, cloud-based health information systems, and secure communication networks. Some studies highlighted that digital health tools, such as virtual consultations and real-time remote monitoring, require robust networking infrastructures to ensure data security, interoperability, and low-latency transmission [15,16,26].
3.4.6. The Role of Networking and Communication in eHealth for Transplantation
The effectiveness of eHealth interventions in transplantation depends on networking infrastructure and secure digital communication systems. Cloud computing allows for seamless integration of patient records across transplant centers, while IoMT-enabled devices enhance continuous patient monitoring through secure data exchange [10,25]. Moreover, blockchain-based data security has emerged as a crucial aspect of ensuring privacy in digital health applications for transplant recipients [15]. The introduction of 5G-enabled telehealth has transformed post-transplant care by enabling real-time, low-latency remote monitoring, allowing healthcare professionals to track patients’ vital signs and intervene quickly in case of complications or rejection [21]. The speed and reliability of 5G, combined with edge computing, enhance data processing and emergency response times, ensuring timely care. Networked eHealth solutions further improve coordination by enabling transplant teams to access electronic health records (EHRs) across different locations, ensuring specialists have up-to-date information for informed decision-making [24]. As digital health adoption grows, securing patient data is essential. Encrypted cloud-based transplant databases provide a secure platform for storing and sharing medical records and protecting against cyber threats while ensuring compliance with privacy regulations. By integrating 5G, eHealth solutions, and secure cloud computing, digital health technologies enhance post-transplant care, improving efficiency, security, and patient outcomes [9].
4. Discussion
This systematic literature review addresses an important gap by reviewing the studies elucidating the utilization of eHealth devices in the context of transplant care. This review encompasses 60 articles, which collectively explore diverse facets, including different types of users engaging with digital health within the realm of transplant care, the barriers and benefits associated with digital health tools, and the process of developing digital health. Predominantly, the existing literature in this domain focused on the implementation of eHealth in transplantation; therefore, this review addresses the gap by demonstrating the multifaceted aspects entailed in the utilization and integration of eHealth in transplant care that received less attention in the literature. By systematically analyzing and interpreting findings from multiple studies, this review was able to highlight patterns, themes, and underexplored areas that contribute to a more holistic understanding. However, it is important to acknowledge that the insights presented in this review are based on secondary data from the included studies. While this approach is valuable for identifying trends and gaps, conducting empirical research would provide an opportunity to directly engage with eHealth users and stakeholders in transplantation care, offering richer, firsthand insights into their experiences, needs, and challenges. Future studies could build on the findings of this review by undertaking qualitative or mixed-methods research to address these areas in greater depth.
In terms of the users of eHealth tools, this study identified two main groups of eHealth users: (1) patients, caregivers, and families [30,37,40,73]; (2) transplant providers, clinicians, and pharmacists [10,11,23,26,34,46,47]. The findings indicate that both groups of users are connected through the shared goal of providing and receiving health care services for transplant purposes. Health devices facilitate the seamless exchange of information between patients/families and healthcare providers [40,46]. Patients can provide real-time health status and symptoms data, enabling healthcare providers to make informed decisions [39,51,52]. Health Information Technology (HIT) plays a crucial role in supporting these interactions by ensuring the integration of patient data across various touchpoints in the transplant journey [15,24]. Interoperable electronic health records (EHRs) are essential for managing patient history, donor–recipient compatibility data, medication adherence, and post-transplant monitoring [15,47]. Digital platforms further enhance engagement by enabling virtual health for follow-up care, patient portals for medication adherence tracking, and remote monitoring systems to detect early signs of organ rejection or complications [33,47]. Given that transplant patients often have comorbid conditions such as diabetes, hypertension, or infections, HIT must also support comprehensive care by incorporating these diagnoses into treatment plans and facilitating collaboration between specialties [18,47].
While most eHealth tools are designed as a single domain [37,40,48] through shared platforms, both parties can coordinate care more effectively. For instance, patients can schedule appointments, track medications, and share relevant data with healthcare providers, leading to more personalized and timely care [41,44,46,48]. While most eHealth tools are designed for a single domain [37,40,48], shared platforms allow both patients and providers to coordinate care more effectively. Patients can schedule appointments, track medications, and share relevant data with healthcare providers, leading to more personalized and timely care [41,44,46,48]. At the same time, HIT strengthens provider decision-making through real-time access to laboratory results, decision support tools for organ allocation and rejection risk assessment, and predictive analytics for graft survival. Secure data-sharing frameworks between transplant centers, laboratories, and specialists enhance continuity of care and reduce transplant-related risks. By enabling data-driven decision-making and improving communication, HIT fosters a holistic approach to transplant care, ultimately optimizing patient outcomes. Beyond improving provider coordination, health tools also empower patients by providing them with resources to participate actively in their care. Meanwhile, healthcare providers can use these tools to engage patients in self-management, monitor their progress remotely, and inform their decisions regarding patient health. Integrating digital health tools for patient and provider-centric purposes fosters a holistic approach to transplant care, enhancing communication, efficiency, and overall patient outcomes. By leveraging shared platforms, healthcare providers can make informed decisions such as altering medication dosages, treatment plans, and interventions based on the data provided by patients through health devices [31,47].
Regarding the barriers to using eHealth, this study identified three categories of barriers, including (1) knowledge and access barriers [22,24,39,44,70,75,76], (2) usability and implementation challenges [22,39,44,45], and (3) user experience and trust issues [9,24,38]. These three categories indicate interconnectedness and highlight a chain reaction, where problems within one category will induce problems in another. In the case of knowledge and access barriers, poor IT literacy can exacerbate usability challenges [44]. For instance, patients who are unfamiliar with digital tools may struggle to navigate platforms for scheduling appointments or tracking medications, leading to frustration and reluctance to use the tools. Similarly, if users need more understanding or training on how to use devices/software, usability challenges become more prominent [39]. Limited access to adequate resources, such as appropriate internet connection, can hinder the successful use and integration of digital tools [38,52].
Furthermore, negative user experiences can reinforce knowledge barriers. If someone has a bad experience with technology, they might be less inclined to invest time learning about it or exploring its capabilities. Difficulties in using technology directly impact user experience [39]. For example, complex interfaces or functionalities often result in poor user experiences, which can trigger trust issues. A common example of this could be when a patient encounters an overly complicated health app that fails to track their data correctly, leading them to question the reliability of the platform. Trust issues, particularly concerning privacy and data security, can discourage users from fully engaging with eHealth tools [38]. Users might be concerned about the confidentiality of their health information or fear their data could be misused, which can lead to their reluctance in using certain devices or platforms [9]. These trust issues can undermine user engagement, thus compounding the barriers to successful technology adoption.
Addressing one category of barriers involves considering and mitigating aspects from the other categories. For instance, improving user experience might involve simplifying usability, addressing knowledge gaps through education or training, and fostering trust by enhancing security measures. Ultimately, overcoming barriers to digital devices requires a holistic approach that considers the interconnected nature of these challenges and seeks comprehensive solutions to improve technology adoption and usage. By considering these interrelated barriers, stakeholders can develop tailored interventions and strategies that enhance user engagement, improve clinical workflows, and ultimately enhance patient care and outcomes.
In terms of benefits that eHealth provides to users, this study identified four categories of benefits associated with using health devices for transplantation pre- and post-care, including (1) improvement in patient care and engagements [17,18,26,29,30,32,41,49,52,54,55,69,72], (2) convenience and accessibility [17,22,35,56,59,61], (3) empowerment and safety [22,33,52,55], and (4) cost-efficiency and time-saving [35,56,59,64,65]. These four categories indicate interconnectedness and highlight areas that influence and generate impact in one another. Empowered patients are more engaged in their care, leading to better adherence to treatment plans and improved outcomes [58]. When patients feel empowered with a suitable health device, they will take a more proactive approach to their health [39,58]. Remote monitoring and accessibility reduce the need for in-person visits, lowering healthcare costs and saving time for patients and transplant providers [12,24]. Feeling empowered and safe using health devices increases the willingness of individuals to adopt and use them [59]. This, in turn, improves accessibility to healthcare services, especially for those who might face barriers to traditional healthcare access [10]. One critical factor affecting the effectiveness of eHealth solutions in transplantation is the underlying digital communication infrastructure. Networking and communication play a crucial role at every stage of the transplant process, from pre-transplant evaluation to post-transplant monitoring and long-term follow-up care [18,36]. Before transplantation, effective networking between transplant centers and donor registries is essential for organ allocation, ensuring that organs are matched efficiently based on real-time patient data and compatibility criteria [77]. During the transplant process, seamless communication between multidisciplinary teams, including transplant surgeons, nephrologists, hepatologists, and coordinators, is necessary to optimize surgical planning and resource allocation [77]. Post-transplant, continuous digital communication enables real-time monitoring of transplant recipients, facilitating early detection of complications such as organ rejection or infections [33,47]. For example, networked Internet of Medical Things (IoMT) devices transmit patient vitals directly to healthcare providers, ensuring timely interventions [10,15,18]. Long-term, networking enhances remote patient engagement, allowing transplant recipients to consult specialists from different locations and access digital health resources for medication adherence and lifestyle management [9,53,57]. The need for networking becomes even more critical in regions with limited transplant facilities, as digital communication helps bridge geographical barriers, improving equity in access to transplant care [35]. Several studies in this review indicate that real-time telehealth monitoring, EHRs, and AI-driven analytics rely on cloud-based data systems and high-speed networks. The integration of 5G, IoMT devices, and blockchain security has the potential to improve data security, remote accessibility, and telehealth service reliability [10,15,18].
Regarding the development process of eHealth interventions, this study identified two crucial factors in developing the process of digital health, which are (1) patient-centered [12,37,70] and (2) preparation and readiness [37,73]. A patient-centered approach in the development of eHealth tools emphasizes the need to ensure that health devices, as well as transplant providers, clinicians, and pharmacists, are all aligned with patient needs. This approach requires eHealth tool developers to prioritize patient-specific needs in the design of health devices [12,37]. For instance, personalizing features on digital tools ensures that patients feel actively involved in their care, tailoring their experience to their specific needs and preferences [12,37]. A key consideration in the effectiveness of digital health systems for transplant patients is whether they align with patient needs. While platforms like MyChart provide access to health records, lab results, and appointment scheduling, they may not fully address patients’ deeper concerns, such as understanding the significance of their medical data and its impact on their long-term health [60]. Patients require more than just access to information [60]. They need contextualized insights that guide their decision-making and improve adherence to post-transplant care plans. AI-driven tools have the potential to enhance patient engagement by providing personalized explanations of medical data, predicting potential health risks, and offering real-time guidance based on trends in their health records [34]. For instance, AI-powered decision-support systems could help transplant recipients interpret fluctuations in biomarkers, medication side effects, or early signs of organ rejection. By bridging the gap between raw data access and meaningful health literacy, these tools can foster greater patient confidence and encourage active participation in their post-transplant care. Future research should explore patient perspectives on digital health tools to determine specific gaps in existing systems and assess whether AI-driven solutions could enhance patient understanding, engagement, and overall health outcomes.
Additionally, addressing attitudes toward Health Information Technology (HIT) and ensuring the credibility of the information provided builds trust—an essential component for patient engagement [12,37]. Preparation and readiness are two interrelated factors crucial for the successful adoption of eHealth tools in transplantation care. Preparation involves understanding the context in which digital tools will be used, considering factors like user capabilities, technological infrastructure, and barriers to access. Studies have highlighted that patient hesitance often stems from a lack of familiarity or knowledge about these tools [30,37], emphasizing the importance of addressing user capabilities to ensure effective tool usage. Readiness, on the other hand, pertains to both patients and healthcare systems being equipped to adopt and utilize these tools. This includes ensuring that patients have the necessary IT literacy and are open to technology [39,44]. Moreover, the credibility of digital health tools is vital for readiness; without trust, patients may hesitate to adopt them [10,31]. Both factors must be addressed in tandem, as neglecting either can limit the effectiveness of eHealth tools.
These two factors, patient-centered design, preparation, and readiness, are deeply interdependent. A patient-centered approach not only influences the design of the tools but also shapes the preparation phase by highlighting the need for health devices, providers, and healthcare systems to align with patient needs. eHealth tool developers must ensure that digital devices support those needs, while patient preparation and readiness depend on whether the tools meet their requirements and expectations. Therefore, a lack of focus on any of these aspects would limit the effectiveness of eHealth devices.
Regarding evidence of the efficacy of different eHealth devices, multiple studies have demonstrated measurable and positive impacts of different eHealth devices on individuals’ health. The majority of the studies that utilized telehealth, revealed the positive impact telehealth had on patients, such as reduced time and costs as well as improved access to care [35,56,59,64,65]. Moreover, the use of telemedicine also demonstrated positive outcomes for patients, which was highlighted by one study that improved access to pharmacy care and improved the accuracy of medication lists [26]. The majority of the studies that implemented mHealth identified the positive impact mHealth had on patients post-transplantation, with reduced complications and hospitalizations [22,29,30,41]. The majority of the studies that used electronic apps/devices demonstrated positive improvement in patient outcomes, such as reduced infections and improvement in the self-management of symptoms [10,54,61]. Only a few previous studies focused on the use of emerging technologies, such as artificial intelligence (AI) and wearables, discussing the positive outcomes for patients, such as helping with clinician decision-making and encouraging physical activity to improve overall health; e.g., [34]. This highlights the gap in studies on the role of emerging technologies in transplantation care. Although the findings suggest that eHealth technologies have the potential to significantly improve patient outcomes and enhance the delivery of care in transplantation settings, there is a need for continued research and innovation to explore the full potential of emerging technologies, address existing gaps in the literature, and optimize transplant care delivery, ultimately advancing the field of eHealth in transplantation care.
A variety of digital health technologies are utilized across different types of transplants, with some overlap in their applications. While all transplant types benefit from telehealth and mobile health applications, certain technologies were more commonly associated with specific organ transplants in the selected studies. For example, electronic health records (EHRs) were widely used in kidney, liver, pancreas, heart, and lung transplants [15,47,48], while artificial intelligence (iBox) has been specifically applied in kidney transplantation [34], whereas digital health home spirometry interventions and telemedicine were more commonly associated with lung transplants [18,26]. Additionally, electronic mental health screening was predominantly used in heart transplantation, reflecting the specific psychological challenges faced by these patients [61]. For younger patients, mobile health applications were more frequently used in heart, kidney, liver, and blood and marrow transplants, supporting both their clinical and emotional needs [40,56]. These distinct patterns underscore the importance of developing digital health solutions that are finely tuned to the specific challenges faced by transplant recipients depending on their organ type.
The findings from this systematic review offer valuable insights that extend beyond transplantation care, contributing to a broader, generalizable knowledge base in healthcare. The integration of eHealth tools in transplant care highlights key principles that can be applied to other clinical settings, particularly in managing complex, long-term conditions. For instance, the use of interoperable electronic health records (EHRs) to centralize patient data and improve care coordination is a practice that can enhance patient outcomes across various specialties, from chronic disease management to general healthcare. Additionally, the emphasis on patient-centered care in the development of eHealth devices, as demonstrated in transplantation, underscores the importance of tailoring healthcare tools to individual patient needs, which is crucial in diverse medical contexts. The barriers and benefits identified in the use of digital health tools also offer broader lessons for healthcare systems globally. Overcoming challenges like digital literacy and trust issues and leveraging tools for patient engagement and remote monitoring can be applied to various disease areas, improving the accessibility and efficiency of care. Finally, the multidisciplinary collaboration in transplant teams, exemplified by the shared use of health technologies among patients, clinicians, and providers, reinforces the value of interdisciplinary coordination, which is a principle that can be generalized to other healthcare models, leading to more holistic, integrated patient care.
Limitations and Future Research
This study has a few limitations which should be considered. Firstly, this research draws upon data gathered from prior studies investigating the use of eHealth in transplantation. Since this study does not involve primary data collection, it is susceptible to inheriting the limitations and validity issues of the studies used as sources. However, to address this limitation, as a part of the exclusion criteria, only empirical studies were included in the literature review process. Secondly, this study relied on preceding journal articles and restricted data sources. This decision was made to ensure the reliability and academic rigor of the findings, as peer-reviewed studies are subject to stringent evaluation processes. However, with advancements in technology, eHealth is constantly changing and improving, meaning there is a considerable body of literature on the subject that may exist outside of traditional academic journals and databases, including online materials and commercial publications.
Although this review presents a variety of eHealth tools and implementation strategies, we recognize the need to evaluate which approaches are more effective in specific transplantation contexts. Telehealth and mHealth solutions emerged as the most frequently used and widely studied, often showing consistent benefits in improving medication adherence, accessibility, and patient engagement, particularly during post-transplant recovery [14,40,56]. In contrast, AI-based tools and wearables, while promising, are still in early-stage development with limited empirical evidence supporting their effectiveness. Moreover, mHealth tools that integrated personalized feedback and in-app support features were more effective in promoting self-management than those providing static information. These observations suggest that while a range of approaches exist, those that support real-time interaction, tailored content, and seamless integration into clinical workflows offer greater promise for adoption and long-term use in transplant care.
Despite excluding such sources, the findings presented within this study are still relevant as it utilizes studies from peer-reviewed, well-established journals and databases commonly used for previous systematic reviews. Future research could address these gaps by integrating insights from grey literature, industry publications, and non-English studies, providing a more comprehensive perspective on eHealth adoption and advancements in transplantation care.
One notable limitation of this study is the potential age bias inherent in the reviewed literature. Most of the selected studies (n = 22) focused on mHealth, a domain that is more accessible and appealing to younger users who tend to use mobile devices more frequently than older individuals. Consequently, the findings may not accurately reflect the digital health engagement of older transplant recipients, who might rely more on other forms of digital technology, such as desktop computers, or may be less inclined to adopt emerging mobile applications. This age bias suggests that the observed trends in eHealth usage may be disproportionately influenced by the habits of younger patients. Future research should investigate digital health interventions across a broader age spectrum to ensure that the diverse needs and preferences of all transplant recipients are adequately captured. Such studies could help develop more inclusive eHealth strategies that promote patient empowerment and self-management for both younger and older populations. Another gap identified was the lack of studies in countries that had high rates of transplantation. Countries that have high rates of transplantation could hold a wealth of information that can be used globally to improve patient care and outcomes for transplantation. Therefore, future research should further expand to different countries. Moreover, studies within this review involved different samples of studies from different countries. Some studies did not report the ethnicities of participants (eHealth users) within their sample, which means some groups of people may not be well represented. Therefore, findings may not accurately represent the needs and responses of under-reported ethnic groups. Future studies should aim to enhance the inclusivity and representativeness of participant samples to contribute to a more robust and generalizable knowledge base within the context of transplantation.
Lastly, many studies focused on mHealth (n = 22) and telehealth (n = 19) as digital interventions for transplantation. Emerging digital interventions (e.g., AI, virtual reality, augmented reality, wearables) did not receive much attention. Considering the growth and importance of these emerging technologies for further improving patient care, and outcomes and streamlining healthcare processes in innovative ways, it is suggested that future studies investigate emerging eHealth interventions and measure their impact to help health facilities deploy the most beneficial solution to improve patient outcomes.
5. Conclusions
eHealth is transforming the field of transplantation, offering many benefits for both patients and healthcare providers. Its impact spans the entire transplant journey, from pre-transplant assessment to post-transplant care and ongoing long-term management. However, there are barriers that prevent the implementation and use of eHealth. Therefore, it is important to better understand the pivotal role of eHealth in the landscape of transplantation. Therefore, this study systematically reviewed prior studies to identify the factors that have been investigated for their impact on the utilization and incorporation of eHealth in transplant care. Furthermore, based on 60 selected articles, this study formulated an integrated framework for the application of eHealth for transplantation purposes. The developed framework integrated multiple facets of using eHealth in transplantation, including (1) barriers to using digital health devices, (2) benefits of using health devices, (3) the process of developing digital health, and (4) users of digital health. Finally, this study identified future prospects of eHealth in translation, such as the use of emerging technologies like AI and wearables to improve patient outcomes. The increasing adoption of eHealth solutions in transplantation is closely tied to advancements in healthcare networking and digital communication. As internet-based platforms continue to evolve, real-time telehealth, cloud-based patient records, and AI-driven analytics will play an even greater role in enhancing transplant care delivery and patient outcomes.
Author Contributions
Author I.F. was responsible for the initial conduction of the systematic review; Author F.H. reviewed the literature and assessed the quality of the included studies and justification of excluded studies; I.F. synthesized the literature according to the decided methodology and wrote a first draft of the manuscript; F.H. revised the draft and contributed to the final version. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
No new data were created or analyzed in this study.
Conflicts of Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Appendix A

Table A1.
Selected Studies for this Systematic Literature Review.
Table A1.
Selected Studies for this Systematic Literature Review.
| Author(s)/Year | Objective of Study | Study Design/Methodology | Type of Transplant | Health Technology | Participants | Number of Participants | Country | Main Findings | |
|---|---|---|---|---|---|---|---|---|---|
| [9] | Kimiafar et al., 2019 | Create a tool for evaluating privacy issues in a web-based liver transplantation registry (WLTR) and gauge patient perspectives on the WLTR’s privacy aspects. | Mixed methods—quantitative and qualitative | Organ—liver | Web-based portal (registry) | Patients | 81 | Iran | System designers and developers need to create privacy policies aligning with the registry program’s goals and user needs to safeguard patient information. |
| [10] | Handler et al., 2023 | Examine healthcare providers’ views on the characteristics of digital health interventions. | Qualitative, thematic analysis | Organ | Electronic app/devices (Digital Health Program) | Providers | 13 | Canada | Providers saw digital health interventions as a potential complement to current physical activity counselling, forming an innovative strategy to tackle identified barriers in solid organ transplant recipients’ participation in physical activity. |
| [11] | La hoz et al., 2021 | Assess the effectiveness of an electronic health record-based registry and its data extraction tools for clinical research in solid organ transplantation. | Quantitative | Organ—heart, kidney, liver, lung, multiorgan | Electronic app/devices (electronic health record) | Patients | 917 | US | Our study demonstrates the value of an electronic health record-based registry and automated extraction tools for clinical research in solid organ transplantation. A bloodstream infection (BSI) diminishes the 1-year survival of solid organ transplant recipients. |
| [12] | Deboni et al., 2020 | Detail the creation and execution of telehealth for monitoring renal transplant and peritoneal dialysis patients amid the COVID-19 pandemic. | Quantitative—descriptive study | Organ | Telehealth | Patients | 960 | Brazil | Outlines the creation and use of telehealth in monitoring renal transplant and peritoneal dialysis patients amid the COVID-19 pandemic. |
| [14] | Chang et al., 2021 | Assessing the viability and efficiency of remotely monitoring kidney transplant patients. | Quantitative | Organ—kidney | Telehealth | Patients | 2 | US | Our early findings show RPM’s feasibility and effectiveness post-transplant, broadening care through remote models. This is particularly crucial now, enabling close monitoring of COVID-19-positive transplant patients in home isolation. |
| [15] | Forbes et al., 2018 | Compare the expenses between patients initially evaluated via telehealth and those assessed in-person throughout the evaluation process. | Quantitative | Organ | Telehealth | Patients | 302 | US | Amid the rising prevalence of telemedicine applications, we share our encounter using telehealth for initial kidney transplant waitlist evaluations, showcasing reduced costs and time, potentially enhancing transplantation accessibility. |
| [17] | Hatzikiriakidis et al., 2022 | Investigate how the COVID-19 pandemic affected the daily lives of young LTx recipients, examining the relationship between immunosuppression and the virus. | Qualitative | Organ—lung | Telehealth | Patients | 11 | Australia | Adolescent LTx recipients face poorer post-transplant outcomes than adults, leading to lower survival rates. Strategies informed by youth could enhance healthcare during public health crises, including (1) empowering youth in shaping their healthcare; (2) tailoring care programs; (3) implementing video-based telehealth when in-person care is not available; (4) offering in-person care for socially vulnerable youth lacking private, secure spaces for telehealth; (5) utilizing technology to improve health literacy, care, and psychosocial support; and (6) ensuring consistent clinicians to build trusting relationships. |
| [18] | Holderried et al., 2021 | Assessed the utilization and promise of contemporary ICT in solid organ transplant recipients. | Quantitative—questionnaire | Solid organ transplants—kidney, liver, pancreas, or combined | Telemedicine | Patient | 234 | Germany | Most SOT recipients widely embrace modern ICT for health purposes. Integrating eHealth more extensively has the potential to enhance comprehensive care, regardless of the transplanted organ. Successful implementation of eHealth technologies in cross-sectoral care will require research on online physician–patient communication, data security, safety, and the quality of care. |
| [20] | Reber et al., 2018 | Identify RTRs favoring and benefiting from mobile technologies like smartphones, potentially suited for mHealth interventions. | Quantitative | Organ—renal | mHealth | Patients | 109 | Germany | Young adult patients may benefit considerably from mobile health strategies. Additionally, a higher education level and typical cognitive function support an inclination toward mobile technology. These factors should be considered in crafting mHealth interventions for RTRs. Further research on potential barriers and desired technological features is crucial to tailor apps to patients’ requirements for effective mHealth interventions. |
| [21] | Duarte-Rojo et al., 2022 | Create a technique to gauge the step length of LT candidates, enabling the remote acquisition of the 6 min walk test (6MWT) distance using a personal activity tracker (PAT). | Quantitative | Organ—liver | Emerging technologies (Wearables) | Patient | 137 | US | We devised a technique to measure the 6MWT distance remotely using a PAT. This innovative method introduces the potential for conducting telemedicine-based PAT-6MWT to track the frailty status of LT candidates. |
| [22] | Eno et al., 2018 | Evaluate living kidney donors’ views and beliefs regarding mHealth for follow-up purposes. | Quantitative—survey | Organ—kidney | mHealth | Patient | 100 | US | In general, smartphone ownership was prevalent (94 out of 100, 94.0%), and among smartphone users surveyed, 79% (74 out of 94) believed that using an mHealth tool for their required follow-up would be helpful. There were no notable differences by age, gender, or race. These findings imply that patients could gain from an mHealth tool for living donor follow-up. |
| [23] | Hensler et al., 2018 | A pharmacist-led dose optimization program using electronic health records (EHRs) was created. A retrospective study was performed to assess if there was a reduced occurrence of CMV infection and ganciclovir-resistant infections after the intervention. | Quantitative | Organ—kidney, liver, and pancreas kidney | Electronic app/devices (electronic health record) | Patients | 566 | US | A pharmacist-led valganciclovir dose optimization program using EHR was linked to decreased CMV infections. |
| [24] | Tang et al., 2020 | Detail the viewpoints and encounters with eHealth within kidney transplant recipients. | Qualitative | Organ—kidney | Electronic app/devices (eHealth) | Patients | 30 | Australia | Recipients recognized eHealth’s potential for aiding healthcare and self-care but faced tech navigation issues and worried about privacy and misinformation. User-friendly, tailored, and secure eHealth systems could enhance satisfaction and outcomes. |
| [25] | Barnett et al., 2021 | Investigate liver transplant recipients’ experiences with a 12-week telehealth lifestyle program and evaluate the feasibility of this innovative service. | Qualitative | Organ—liver | Telehealth | Patients | 19 | Australia | A telehealth lifestyle program, administered by dietitians and exercise physiologists, is a viable alternative to in-person care for liver transplant recipients. There is a necessity to expand and innovate routine service delivery beyond face-to-face consultations. |
| [26] | Park et al., 2021 | Detail the establishment of a CT transplant pharmacist role in an LTR virtual clinic and outline the clinical interventions and medication errors discovered by the pharmacists amid COVID-19. | Quantitative | Organ—lung | Telemedicine | Transplant pharmacists and patients | Two Pharmacists and 157 Lung Transplant Patients | US | Introducing CT transplant pharmacist telehealth sessions could boost patient access to pharmacy care and enhance medication list accuracy. Most errors showed significant severity and service value. Further study is required to assess this service’s impact on patient outcomes and cost-effectiveness. |
| [29] | Erez et al., 2023 | Assess the viability and acceptance of a home urinalysis kit paired with a smartphone app. | Quantitative | Organ—kidney | mHealth | Patients | 103 | US | The Healthy.io home urine testing app garnered significantly higher satisfaction from patients and caregivers compared to current methods, indicating substantial potential to improve patient-centred care. |
| [30] | Lerret et al., 2022 | Outline the viability, acceptance, and initial effectiveness of an mHealth family self-management intervention (myFAMI) aimed at enhancing coping post-discharge, family quality of life, self-efficacy, family self-management, and healthcare resource utilization. | Quantitative | Organ—pediatric heart, kidney and liver | mHealth | Patient families | 46 | US | The intervention was positively accepted and showed promise for future post-discharge programs for families of pediatric transplant recipients. |
| [31] | Gonzales et al., 2022 | Outline the occurrence and nature of interventions in a pharmacist-led, mobile health-based approach for KTX recipients, and its effect on patient risk levels. | Quantitative | Organ—kidney | mHealth | Patient | 68 | US | A pharmacist-led mHealth intervention could increase chances for diverse interventions and lower risk levels in KTX recipients. |
| [32] | Khalil et al., 2022 | Evaluate transplant pharmacists’ encounters with telehealth amid the COVID-19 pandemic. | Quantitative | Organ—heart, lung, liver, intestine, kidney, pancreas | Telehealth | Pharmacists of Transplant patients | 45 | US | COVID-19 prompted widespread telehealth adoption, aiding in maintaining care continuity. While pharmacists expected reduced future use, most preferred ongoing telehealth utilization in their practice. |
| [33] | Mussetti et al., 2021 | Assess the application of a telehealth platform in monitoring HCT patients within the initial two weeks post-discharge. | Quantitative | Hematopoietic cell transplantation | Telehealth | Patients | 12 | Spain | This study demonstrated the feasibility of using telehealth in the early post-transplant phase, offering benefits to physicians and patients in the medical and psychological realms. However, technological challenges persist, particularly for older adult patients. Simplified technologies could enhance the future utilization of telehealth systems in this context. |
| [34] | Divard et al., 2022 | Assess transplant physicians’ capability to forecast long-term allograft failure and compare their predictions to a validated artificial intelligence (AI) algorithm. | Quantitative | Organ—kidney | Emerging technologies (Artificial Intelligence (iBox)) | Patients and Physicians | 400 | France | The study highlights physicians’ generally limited accuracy in predicting long-term graft failure, contrasting with the superior performance of iBox. It advocates for a companion tool to aid physicians in prognosis and clinical decision-making. |
| [35] | Sidhu et al., 2019 | Assess the effects of telehealth versus face-to-face follow-up on lung transplant recipients. | Quantitative | Organ—lung | Telehealth | Patients | 204 | Canada | Telehealth proves safe and effective for specific transplant recipients, improving care access and lessening time and financial strain, particularly for patients distant from primary transplant centres. |
| [36] | Gunn et al., 2021 | Uncover the social, emotional, psychological, spiritual, informational, and practical challenges faced by organ transplant recipients and their caregivers in regional areas, and explore ways to enhance support services for this demographic. | Qualitative | Organ—liver, lung, kidney, heart | Telehealth | Patients | 22 | Australia | Inventive approaches are needed to provide specialized transplant information and psychosocial support to rural transplant recipients, their caregivers, employers, and local health professionals. These strategies, delivered through telehealth, phone, social media, or websites, should be tailored based on preferences and the extent of required support. |
| [37] | Bangerter et al., 2022 | Utilize a human-centred design to create a high-fidelity prototype of a HIT-enabled psychoeducational tool for HSCT caregivers. | Mixed methods—literature review, visualization, design evaluation | Hematopoietic stem cell transplant | Others (Health Information Technology) | Caregivers | 63 | US | This study combines healthcare delivery research and human-centred design to create tech-supported aid for HSCT caregivers. It presents a design approach for a HIT-enabled psychoeducational prototype, aiding the development of future eHealth innovations for HSCT optimization. |
| [38] | Eno et al., 2019 | Create an mHealth platform tailored to gather and report follow-up data from Living Kidney Donors after donation. | Qualitative | Organ—kidney | mHealth | Transplant providers | 21 | US | Transplant providers believe mHealth could enhance LKD follow-up and aid centres in meeting reporting requirements. Yet, creating a secure, user-friendly, and affordable system remains a challenge. |
| [39] | O’Brien et al., 2018 | Outline demographics, usage, obstacles, and views on mobile app utilization for self-care management among adult kidney transplant recipients. | Quantitative—questionnaire/survey | Organ—kidney | mHealth | Patients | 123 | US | Results hint at a possible link between using mHealth apps and reduced hospitalizations post-kidney transplantation. |
| [40] | Adib et al., 2022 | Create a smartphone-driven app framework aimed at offering connected health management solutions and assisting family members of pediatric transplant recipients. | Qualitative—action research methodology | Pediatric—organ | mHealth | Family members of patients | US | Outlines a successful mHealth app development process by combining theory-based nursing interventions with AR methodology in computer science. Emphasizing efficiency-enhancing factors facilitated seamless app navigation and data collection. Enables the evaluation of acceptability, usefulness, and usability for similar future studies. | |
| [41] | Gomis-Pastor et al., 2020 | Detail the execution of the mHeart model and highlight key facilitators in designing an mHealth approach. | Mixed methods | Organ—heart | mHealth | Patients | 135 | Spain | The versatile mHeart model can be adapted to various clinical and research settings, encouraging cardiology health providers to devise innovative approaches for managing complex treatments and multiple health issues within healthcare systems. Both professionals and patients show readiness to embrace such innovative mHealth programs. The highlighted facilitators and strategies were crucial for successfully implementing this new holistic, theory-based mHealth strategy. |
| [42] | Vanhoof et al., 2018 | To (a) choose an IHT platform for a self-management aid, (b) gauge transplant patients’ readiness to utilize IHT for self-management support, and (c) examine transplant patients’ opinions regarding potential IHT functions. | Quantitative—descriptive study | Organ—heart, lung, liver, kidney | Others (Interactive Health Technology) | Patients | 122 | Belgium | Studying transplant patients’ ICT ownership and usage revealed that computers and the internet, not smartphones, are the optimal platforms for self-management interventions. Though patients are generally receptive to IHT, considering patient acceptance factors and their preferred IHT features is crucial in further IHT development. This initial step in human-centered design is pivotal for designers creating or utilizing IHTs. |
| [43] | Wang et al., 2019 | Investigates the potential for customization considering patients’ medical status and health literacy. | Mixed methods | Organ—kidney | Web-based portal (self-management support system) | Patients | 49 | Netherlands | Data indicate that when creating an SMSS, the communication approach should align with patients’ experiences and medical conditions. |
| [44] | Oliveira et al., 2023 | Assessing the adoption of a kidney health app among kidney transplant recipients | Quantitative | Organ—kidney | mHealth | Patients | 225 | Brazil | The kidney transplant recipient segment in the Renal Health app intrigued the younger demographic but demonstrated low engagement over the monitored months. These outcomes provide valuable insights into implementing mHealth tech in kidney transplantation. |
| [45] | Keating et al., 2020 | Assessing the agreement and reliability of clinician-measured versus patient self-measured clinical and functional assessments in remote home-based monitoring via telehealth. | Quantitative | Organ—liver | Telehealth | Patients | 18 | Australia | In general, liver transplant recipients (LTRs) can reliably self-assess clinical and functional measures at home. Yet, there was considerable individual variability in accuracy and agreement, with no functional assessment meeting acceptable limits relative to MCIDs over 80% of the time. |
| [46] | Xu-Stettner et al., 2023 | Highlight the significance of treatment choices made by transplant pharmacists concerning telehealth versus in-person clinic visits. | Quantitative—descriptive comparative evaluation | Organ—liver | Telehealth | Providers/pharmacists of transplant patients | 28 | US | Transplant pharmacists can offer similarly crucial recommendations via telehealth as they do during in-clinic visits, considering both the total and critical treatment decisions. |
| [47] | Morken et al., 2023 | We investigated the obstacles and aids to Survivorship Care Plan (SCP) utilization among HSCT survivors and their clinicians. | Quantitative—survey | Hematopoietic stem cell | Electronic app/devices (electronic health record) | Patients and clinicians | 27 Patients and 18 Clinicians | US—Wisconsin | While previous efforts focused on barriers to SCP creation, our study delved into factors impacting SCP utilization. Identifying barriers and aids for SCP use among HSCT survivors and clinicians enables the creation of optimized SCP templates and clinical processes, potentially improving outcomes for these survivors. |
| [48] | Kelly et al., 2019 | Detail the execution of a five-session group intervention aimed at enhancing medication adherence in adolescent transplant recipients using home-based telemedicine. | Quantitative | Organ—kidney, livery, heart | Telehealth | Patients | 33 | US | We investigate the hurdles in establishing a home-based group, offer practical solutions tailored for adolescents, and suggest ways to equip clinicians for potential obstacles when implementing a telehealth group with youth. |
| [49] | Killian et al., 2022 | Explored the feasibility and acceptance of an asynchronous mHealth application for directly observed therapy (DOT) among adolescent heart transplant recipients. | Quantitative—pilot study and survey | Organ—heart | mHealth | Patients | 10 | US | This pilot study yields promising indications about the feasibility, acceptability, and potential impact of DOT for adolescent heart transplant recipients. Further randomized studies are needed to validate these findings. |
| [50] | Odisho et al., 2023 | Created a digital health intervention employing Bluetooth-enabled home spirometers for real-world monitoring of lung transplantation complications. | Quantitative | Organ—lung | Electronic app/devices (digital health home spirometry intervention) | Patients | 371 | US | Our innovative EHR-integrated home spirometry intervention, utilizing automated chat, garnered high acceptance, provided dependable graft function assessments, and offered automated feedback and education, resulting in reasonably high adherence rates. Notably, in-person onboarding improved engagement and adherence. Subsequent research will explore the impact of remote care monitoring on the early detection of lung transplant complications. |
| [51] | O’Brien et al., 2022 | Detail insights gained from training a research team and educating kidney transplant recipients on mHealth technology through a virtual format. | Quantitative | Organ—kidney | mHealth | Patients | 20 | US | Results indicate that time, educational resources, and employing verbal, written, and visual information are crucial when executing a virtual research study. |
| [52] | Gomis-Pastor et al., 2021 | Assess if an mHealth approach outperforms standard care in enhancing adherence and patients’ experiences among heart transplant recipients. | Quantitative and qualitative | Organ—heart | mHealth | Patients | 134 | Spain | Our study found that the mHealth approach notably enhanced medication adherence and patient confidence in their medication routines among HTx recipients. The mHeart mobile app proved to be a viable tool for delivering personalized, long-term interventions to improve assessed objectives in this population. |
| [53] | Killian et al., 2023 | Examine the type and extent of in-app communication between adolescent heart transplant recipients and nursing staff during an asynchronous mobile video directly observed therapy intervention. | Mixed methods—content analysis. creating codes and using thematic analysis | Organ—heart | mHealth | Patients | 10 | US | The research highlighted the feasibility and advantages of the two-way communication features in the directly observed therapy intervention, boosting engagement and enhancing medication adherence among adolescent heart transplant patients. Ongoing research and clinical emphasis on patient engagement and meaningful interpersonal communication could facilitate integrating this intervention into standard care at pediatric transplant centres. |
| [54] | Sayegh et al., 2022 | Assess the suitability and viability of a short mobile health (mHealth) intervention and its influence on medication adherence in Adolescent and Young Adult (AYA) liver transplant recipients. | Mixed methods | Organ—liver | mHealth | Patients | 35 | US | The findings indicate that sending text messages to patients regarding positive health markers was well-received and could potentially enhance self-management of illness in AYA individuals with refinement. |
| [55] | Vaughn et al., 2020 | To examine the viability of incorporating mHealth tech for monitoring symptom data in PBMT patients and assess the study’s structure, assessments, and protocols. | Qualitative | Pediatric blood and marrow transplant | mHealth | Patients | 7 | US | Gathering frequent, long-term symptom data from kids and showing mobile tech acceptance indicates its feasibility. Our results also show how these technologies help gather symptom data for better understanding and devising symptom management strategies. |
| [56] | Hickman et al., 2021 | Explored the viability of a 12-week telehealth lifestyle intervention for liver transplant recipients. | Quantitative | Organ—liver | Telehealth | Patients | 7 | Australia | A telehealth-based cardio-protective lifestyle intervention is viable for liver transplant recipients and could enhance access to specialized care for supporting metabolic health post-transplant. |
| [57] | Pollockm et al., 2023 | Assess if the MyKidneyCoach app enhanced patient activation, engagement, and dietary habits in a diverse kidney transplant (KT) population. | Quantitative | Organ—kidney | mHealth | Patients | 9 | US | MyKidneyCoach had high user acceptance and minimal dropout, with enhancements seen in patient-reported outcomes. Both Black and non-Black users showed better self-management skills, indicating a potential in reducing healthcare disparities in KT. |
| [58] | Delman et al., 2021 | Reporting the University of Cincinnati Medical Centre response to the COVID-19 pandemic | Quantitative | Organ—liver | Telehealth | Patients | 344 | US | During the COVID-19 period, performing orthotopic liver transplants safely and successfully is achievable without jeopardizing results. This is achieved by enhancing telehealth usage, conducting rapid COVID-19 tests, and implementing comprehensive protocols for handling immunosuppressed patients. |
| [59] | John et al., 2020 | Studied the impact of telehealth on the liver transplant assessment. | Quantitative | Organ—liver | Telehealth | Patients | 465 | US | Telehealth significantly shortens the time from referral to the initial hepatologist evaluation and placement on the liver transplant waitlist, especially for patients with lower MELD scores. However, it does not affect the time to transplantation or pretransplant mortality. Further research, especially outside the Veterans Administration Health System, is required to validate telehealth as a safe and efficient means to broaden access for patients undergoing liver transplant evaluations. |
| [60] | Anton et al., 2021 | Assess the viability of employing electronic mental health screenings in pediatric heart failure and transplant clinics. | Quantitative—surveys | Organ—Heart | Electronic app/devices (Electronic Mental Health Screening) | Patients | 119 | US | Findings indicate the viability of electronic mental health screening during cardiology clinic visits, offering valuable mental health insights. |
| [61] | Andrew et al., 2020 | Assessing the use of telehealth within the routine follow-up of renal transplant patients. | Quantitative | Organ—Liver | Telehealth | Patients | Australia | A telehealth model of care for routine follow-up of renal transplant recipients was successful in reducing travel costs and time for regional patients. | |
| [62] | Fleming et al., 2021 | Assess a pharmacist-led telehealth intervention using mHealth (TRANSAFE Rx study) aimed at enhancing medication safety. | Quantitative | Organ—kidney | mHealth | Patients | 68 | US | A link was found between the active trial intervention and improved tacrolimus IPV. Given the consistent link between high tacrolimus IPV and negative allograft outcomes, our findings suggest that employing multi-dimensional technologies could enhance clinical results. However, further prospective studies are needed to confirm the changeability of tacrolimus IPV and the effects of reducing it on long-term clinical outcomes. |
| [63] | Gomis-Pastor et al., 2023 | Evaluating if mHeart lowers complication rates and healthcare resource utilization, considering its correlation with patient adherence. | Quantitative | Organ—heart | mHealth | Patients | 134 | Spain | The mHeart approach notably decreased post-transplant complications and medical attention requirements in HTx recipients. Adherence status influences the need for medical care. |
| [64] | Forbes et al., 2018 | Assess the impact of telehealth within the transplant waitlist evaluation process | Quantitative | Organ—kidney | Telehealth | Care Providers | US | Implementation of telehealth, including web-based referrals and videoconference, improved timeliness to kidney transplant waitlist evaluation. | |
| [65] | Huuskes et al., 2021 | Detailed kidney transplant recipients’ views on telehealth advantages, obstacles, and potential risks. | Quantitative and qualitative | Organ—kidney | Telehealth | Patients | 34 | Australia | Telehealth offers convenience, reduces time and financial burdens, and lessens the overall treatment load. Post-pandemic, it should be accessible through trusted nephrologists and include resources to assist patients in preparing for appointments. |
| [66] | Maroney et al., 2021 | Examine eHealth literacy in kidney transplant (KT) and liver transplant (LT) recipients, and explore its correlation with the use of web-based patient portals. | Quantitative—surveys | Organ—kidney and Lung | Web-based portal (patient portal) | Patients | 288 | US—Atlanta | Kidney and liver transplant recipients who regularly use patient portals exhibit high eHealth literacy, suggesting the benefit of promoting regular usage to enhance post-transplant health and medication adherence. |
| [67] | Mathur et al., 2021 | Explored views of solid organ transplant (SOT) recipients on physical activity and their preferences for features in digital health tools. | Quantitative and qualitative | Organ—liver, heart, lung, kidney, pancreas | mHealth | Patients | 21 | Canada | Solid organ transplant (SOT) recipients outlined preferred features for a digital health tool, potentially informing the design of future applications supporting physical activity in this group. |
| [68] | O’Brien et al., 2020 | Investigated kidney transplant recipients’ opinions on the utility of mHealth apps and identified crucial features they find valuable in these applications. | Qualitative | Organ—kidney | mHealth | Patients | 20 | US | Further research is necessary to determine the most effective consumer-oriented mHealth app for kidney transplant recipients’ self-care. Interestingly, participants had limited discussions with their healthcare providers regarding the use of mHealth apps for self-care tracking. |
| [69] | Schmidt et al., 2021 | Evaluating the use of EHR for kidney transplant recipients | Mixed methods | Kidney | Electronic health record | Providers | Germany | Integrated electronic health record and research database for kidney transplant recipients that combines automated and manual data entry to enable efficient clinical care and research. | |
| [70] | Tang et al., 2023 | Assess the perspectives, factors and patterns of eHealth use in Kidney Transplant recipients | Mixed methods | Kidney | Electronic devices/app (eHealth) | Patients | Australia | Study found that the burden of technology hindered eHealth adoption among transplant patients. Participants felt overwhelmed by the large volume of online information, making it difficult to filter and trust eHealth resources. Many struggled to decipher complex medical content, leading to confusion and reluctance to use eHealth for self-management. Additionally, technical challenges, such as navigation difficulties and hardware issues, further discouraged engagement, especially among those who lacked confidence in their digital skills. | |
| [71] | Thiessen et al., 2020 | An observational review of the abdominal transplant program at the University of California. | Quantitative—descriptive study | Organ—kidney, liver, pancreas | Telehealth | Transplant Clinic | US | Each transplant program is distinct, necessitating a tailored approach to sustain crucial transplantation services. The authors’ experience highlights specific areas needing attention in these programs, offering potential solutions applicable to ensure ongoing transplantation during the COVID-19 era. | |
| [72] | Zmaili et al., 2022 | Assessing Takotsubo cardiomyopathy in orthotopic liver transplant recipients | Quantitative | Organ—liver | Electronic health record | Patients | US | Takotsubo cardiomyopathy is significantly more likely to occur in orthotopic liver transplant recipients, especially in older, Caucasian, female patients with cardiac arrhythmias. | |
| [73] | Skeens et al., 2022 | Evaluate the practicality and usability of a mHealth app (BMT4me) aimed at enhancing adherence to immunosuppressant medication and monitoring symptoms in children after HSCT. | Mixed methods—qualitative and quantitative | Hematopoietic stem cell transplant | mHealth | Caregivers of Pediatric Patients | 15 | US | This protocol outlines a mixed-methods study focusing on developing and deploying a smartphone app for caregivers of children undergoing HSCT. The app aims to enhance immunosuppressant adherence and symptom monitoring post-discharge. Study results will guide further app refinement and assess the feasibility of a pilot randomized controlled trial assessing its impact on clinical outcomes. |
References
- Senbach, G. What is e-health? J. Med. Internet Res. 2001, 3, e20. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Global Diffusion of eHealth: Making Universal Health Coverage Achievable: Report of the Third Global Survey on eHealth; WHO: Geneva, Switzerland, 2016; Available online: https://iris.who.int/bitstream/handle/10665/252529/9789241511780-eng.pdf?sequence=1 (accessed on 15 September 2023).
- European Parliament. The Rise of Digital Health Technologies During the Pandemic. 2021. Available online: https://www.europarl.europa.eu/RegData/etudes/BRIE/2021/690548/EPRS_BRI(2021)690548_EN.pdf (accessed on 15 September 2023).
- Castor, C.; Lindkvist, R.M.; Hallström, I.K.; Holmberg, R. Health Care Professionals’ Experiences and Views of eHealth in Pediatric Care: Qualitative Interview Study Applying a Theoretical Framework for Implementation. JMIR Pediatr. Parent. 2023, 6, e47663. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Schrader, D.; Boelman, C.; Huh, L.; Connolly, M.B. Rapid Implementation of Virtual Health in a Pediatric Neurology Practice During COVID-19. Can. J. Neurol. Sci. J. Can. Sci. Neurol. 2021, 48, 575–577. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Borycki, E.M.; Kushniruk, A.W. Connecting the World of Healthcare Virtually: A Scoping Review on Virtual Care Delivery. Healthcare 2021, 9, 1325. [Google Scholar] [CrossRef]
- Lee, K.C.S.; Breznen, B.; Ukhova, A.; Martin, S.S.; Koehler, F. Virtual healthcare solutions in heart failure: A literature review. Front. Cardiovasc. Med. 2023, 10, 1231000. [Google Scholar] [CrossRef]
- Shaheen, M.Y. Applications of Artificial Intelligence (AI) in healthcare: A review. Sci. Prepr. 2021. [CrossRef]
- Kimiafar, K.; Yazdipour, A.B.; Hoseini, B.; Sarbaz, M. Development and implementation of an instrument to assess privacy challenges of a web-based liver transplantation registry. Electron. Physician 2019, 11, 7441–7449. [Google Scholar] [CrossRef]
- Handler, L.; Jaloul, P.; Clancy, J.; Cuypers, B.; Muir, J.; Hemphill, J.; Janaudis-Ferreira, T.; Gottesman, C.; Wickerson, L.; Lovas, M.; et al. A qualitative study of the Perspectives of Healthcare Professionals on Features of Digital Health Interventions to Support Physical Activity in Solid Organ Transplant Recipients. Prog. Transplant. 2023, 33, 43–49. [Google Scholar] [CrossRef]
- La Hoz, R.M.; Liu, T.; Xie, D.; Adams-Huet, B.; Willett, D.L.; Haley, R.W.; Greenberg, D.E. The use of automated data extraction tools to develop a solid organ transplant registry: Proof of concept study of bloodstream infections. J. Infect. 2021, 82, 41–47. [Google Scholar] [CrossRef]
- Deboni, L.M.; Neermann, E.M.V.; Calice-Silva, V.; Hanauer, M.A.; Moreira, A.; Ambrósio, A.; Guterres, D.B.; Vieira, M.A.; Nerbass, F.B. Development and implementation of telehealth for peritoneal dialysis and kidney transplant patients monitoring during the COVID-19 pandemic. Braz. J. Nephrol. 2020, 43, 422–428. [Google Scholar] [CrossRef]
- Doyle-Lindrud, S. State of eHealth in cancer care: Review of the benefits and limitations of ehealth tools. Clin. J. Oncol. Nurs. 2020, 24, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.H.; Sritharan, S.; Schmitt, K.; Patel, S.; Crew, R.J.; Tsapepas, D.S. Home care delivery and remote patient monitoring of kidney transplant recipients during COVID-19 pandemic. Prog. Transplant. 2021, 31, 381–384. [Google Scholar] [CrossRef] [PubMed]
- Forbes, R.C.; Rybacki, D.B.; Johnson, T.B.; Hannah-Gillis, A.; Shaffer, D.; Hale, D.A. A cost comparison for telehealth utilization in the kidney transplant waitlist evaluation process. Transplantation 2018, 102, 279–283. [Google Scholar] [CrossRef] [PubMed]
- Bakker, A.; Riper, H.; Olff, M. E-health applications in the field of traumatic stress. Eur. J. Psychotraumatol. 2020, 11, 1762317. [Google Scholar] [CrossRef]
- Hatzikiriakidis, K.; West, S.; Ayton, D.; Morris, H.; Martin, R.S.; Paraskeva, M. When immunosuppression and COVID-19 intersect: An exploratory qualitative study of young lung transplant recipient perceptions of daily life during a pandemic. Pediatr. Transplant. 2022, 26, e14281. [Google Scholar] [CrossRef]
- Holderried, M.; Hoeper, A.; Holderried, F.; Heyne, N.; Nadalin, S.; Unger, O.; Ernst, C.; Guthoff, M. Attitude and potential benefits of modern information and communication technology use and telemedicine in cross-sectoral solid organ transplant care. Sci. Rep. 2021, 11, 9037. [Google Scholar] [CrossRef]
- Duettmann, W.; Naik, M.G.; Zukunft, B.; Osmonodja, B.; Bachmann, F.; Choi, M.; Roller, R.; Mayrdorfer, M.; Halleck, F.; Schmidt, D.; et al. eHealth in transplantation. Transpl. Int. 2021, 34, 16–26. [Google Scholar] [CrossRef]
- Reber, S.; Scheel, S.; Stoessel, L.; Schieber, K.; Jank, S.; Lüker, C.; Vitinius, F.; Grundmann, F.; Eckardt, K.-U.; Prokosch, H.-U.; et al. Mobile technology affinity in renal transplant recipients. Transplant. Proc. 2018, 50, 92–98. [Google Scholar] [CrossRef]
- Duarte-Rojo, A.; Brown, R.A.; Bloomer, P.M.; Duarte, M.N.; Grubbs, R.K.; Hernaez, R. A Telemedicine Alternative to the 6-Minute Walk Test Using Personal Activity Trackers in Liver Transplant Candidates. Transplant. Direct 2022, 8, e1347. [Google Scholar] [CrossRef]
- Eno, A.K.; Thomas, A.G.; Ruck, J.M.; Rasmussen, S.E.V.P.; Halpern, S.E.; Waldram, M.M.; Muzaale, A.D.; Purnell, T.S.; Massie, A.B.; Wang, J.M.G.; et al. Assessing the attitudes and perceptions regarding the use of mobile health technologies for living kidney donor follow-up: Survey study. JMIR mHealth uHealth 2018, 6, e11192. [Google Scholar] [CrossRef]
- Hensler, D.; Richardson, C.L.; Brown, J.; Tseng, C.; DeCamp, P.J.; Yang, A.; Pawlowski, A.; Ho, B.; Ison, M.G. Impact of electronic health record-based, pharmacist-driven valganciclovir dose optimization in solid organ transplant recipients. Transpl. Infect. Dis. 2018, 20, e12849. [Google Scholar] [CrossRef] [PubMed]
- Tang, J.; James, L.; Howell, M.; Tong, A.; Wong, G. eHealth interventions for solid organ transplant recipients: A systematic review and meta-analysis of randomized controlled trials. Transplantation 2020, 104, e224–e235. [Google Scholar] [CrossRef]
- Barnett, A.; Campbell, K.L.; Mayr, H.L.; Keating, S.E.; Macdonald, G.A.; Hickman, I.J. Liver transplant recipients’ experiences and perspectives of a telehealth-delivered lifestyle programme: A qualitative study. J. Telemed. Telecare 2021, 27, 590–598. [Google Scholar] [CrossRef]
- Park, L.; Kim, J.H.; Waldman, G.; Marks, C.R.; Clark, J.E. Impact analysis of virtual ambulatory transplant pharmacists during COVID-19. J. Am. Coll. Clin. Pharm. 2021, 4, 978–987. [Google Scholar] [CrossRef] [PubMed]
- Lame, G. Systematic Literature Reviews: An Introduction. Proc. Des. Soc. Int. Conf. Eng. Des. 2019, 1, 1633–1642. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2020, 151, 264–269. [Google Scholar] [CrossRef]
- Erez, D.L.; Derwick, H.; Furth, S.; Ballester, L.; Omuemu, S.; Adiri, Y.; Mink, J.; Denburg, M. Dipping at home: Is it better, easier, and more convenient? A feasibility and acceptability study of a novel home urinalysis using a smartphone application. Pediatr. Nephrol. 2023, 38, 139–143. [Google Scholar] [CrossRef]
- Lerret, S.M.; Schiffman, R.; White-Traut, R.; Medoff-Cooper, B.; Ahamed, S.I.; Adib, R.; Liegl, M.; Alonso, E.; Mavis, A.; Jensen, K.; et al. Feasibility and acceptability of a mHealth self-management intervention for pediatric transplant families. West. J. Nurs. Res. 2022, 44, 955–965. [Google Scholar] [CrossRef]
- Gonzales, H.M.; Fleming, J.N.; Gebregziabher, M.; Posadas Salas, M.A.; McGillicuddy, J.W.; Taber, D.J. A critical analysis of the specific pharmacist interventions and risk assessments during the 12-month TRANSAFE Rx randomized controlled trial. Ann. Pharmacother. 2022, 56, 685–690. [Google Scholar] [CrossRef]
- Khalil, K.; Tsapepas, D.; West-Thielke, P. Transplant pharmacists’ experience with telehealth during the COVID-19 pandemic. J. Pharm. Pract. 2022, 37, 307–310. [Google Scholar] [CrossRef]
- Mussetti, A.; Salas, M.Q.; Condom, M.; Antonio, M.; Ochoa, C.; Ivan, I.; Torre, D.J.R.L.; Linares, G.S.; Ansoleaga, B.; Patiño-Gutierrez, B.; et al. Use of telehealth for domiciliary follow-up after hematopoietic cell transplantation during the COVID-19 pandemic: Prospective pilot study. J. Med. Internet Res. Form. Res. 2021, 5, e26121. [Google Scholar] [CrossRef] [PubMed]
- Divard, G.; Raynaud, M.; Tatapudi, V.S.; Abdalla, B.; Bailly, E.; Assayag, M.; Binois, Y.; Cohen, R.; Zhang, H.; Ulloa, C.; et al. Comparison of artificial intelligence and human-based prediction and stratification of the risk of long-term kidney allograft failure. Commun. Med. 2022, 2, 150. [Google Scholar] [CrossRef] [PubMed]
- Sidhu, A.; Chaparro, C.; Chow, C.W.; Davies, M.; Singer, L.G. Outcomes of telehealth care for lung transplant recipients. Clin. Transplant. 2019, 33, e13580. [Google Scholar] [CrossRef] [PubMed]
- Gunn, K.M.; Skrabal Ross, X.; McLoughlin, M.; McDonald, S.; Olver, I. The psychosocial experiences and supportive care preferences of organ transplant recipients and their carers who live in regional Australia. Aust. J. Rural. Health 2021, 29, 92–105. [Google Scholar] [CrossRef]
- Bangerter, L.R.; Looze, M.; Barry, B.; Harder, K.; Griffin, J.; Dezutter, M.; Khera, N.; Ailawadhi, S.; Schaepe, K.; Fischer, K. A hybrid method of healthcare delivery research and human-centered design to develop technology-enabled support for caregivers of hematopoietic stem cell transplant recipients. Support. Care Cancer 2022, 30, 227–235. [Google Scholar] [CrossRef]
- Eno, A.L.; Rucj, J.M.; Rasmussen, S.E.V.P.; Waldram, M.M.; Thomas, A.G.; Purnell, T.S.; Wang, J.M.G.; Massie, A.B.; Almmary, F.A.; Cooper, L.M.; et al. Perspectives on implementing mobile health technology for living kidney donor follow-up: In-depth interviews with transplant providers. Clin. Transplant. 2019, 33, e13637. [Google Scholar] [CrossRef]
- O’Brien, T.; Russell, C.L.; Tan, A.; Washington, M.; Hathaway, D. An exploratory correlational study in the use of mobile technology among adult kidney transplant recipients. Prog. Transplant. 2018, 28, 368–375. [Google Scholar] [CrossRef]
- Adib, R.; Das, D.; Ahamed, S.I.; Lerret, S.M. An mHealth app-based self-management intervention for family members of pediatric transplant recipients (myFAMI): Framework design and development study. JMIR Nurs. 2022, 5, e32785. [Google Scholar] [CrossRef]
- Gomis-Pastor, M.; Mirabet, S.; Roig, E.; Brossa, V.; Lopez, L.; Ros, S.; Mas Malagarriga, N.; Mangues, M. Improving patients’ experience and medication adherence after heart transplant using a multilevel eHealth intervention: The mHealth clinical trial. Transplantion 2020, 104, S578–S579. [Google Scholar] [CrossRef]
- Vanhoof, J.; Vandenberghe, B.; Geerts, D.; Philippaerts, P.; De Maziere, P.; Dabs, D.A.; De Geest, S.; Dobbels, F. Technology experience of solid organ transplant patients and their overall willingness to use interactive health technology. J. Nurs. Scholarsh. 2018, 50, 151–162. [Google Scholar] [CrossRef]
- Wang, W.; van Lint, C.L.; Brinkman, W.P.; Rövekamp, T.J.; van Dijk, S.; van der Boog, P.; Neerincx, M.A. Guided or factual computer support for kidney patients with different experience levels and medical health situations: Preferences and usage. Health Technol. 2019, 9, 329–342. [Google Scholar] [CrossRef]
- Oliveira, J.G.R.D.; Sanders-Pinheiro, H.; Freitas Filho, R.A.D.; Vasconcelos Filho, J.E.; Askari, M.; Silva Júnior, G.B.D. Evaluation of the use of a Renal Health application by kidney transplant recipients. Rev. Lat. Am. Enferm. 2023, 31, e3822. [Google Scholar] [CrossRef] [PubMed]
- Keating, S.E.; Barnett, A.; Croci, I.; Hannigan, A.; Elvin-Walsh, L.; Coombes, J.S.; Campbell, K.L.; Macdonald, G.A.; Hickman, I.J. Agreement and reliability of clinician-in-clinic versus patient-at-home clinical and functional assessments: Implications for telehealth services. Arch. Rehabil. Res. Clin. Transl. 2020, 2, 100066. [Google Scholar] [CrossRef] [PubMed]
- Xu-Stettner, J.; Thompson, A.N.; Fitzgerald, L.J.; Licari, T.; McMurry, K.A.; Tischer, S. Comparison of Transplant Pharmacist Treatment Decisions Between Telehealth and Clinic Visits. Prog. Transplant. 2023, 33, 156–161. [Google Scholar] [CrossRef]
- Morken, C.; Tevaarwek, A.J.; Jukett, M.B.; Swiecichowski, A.K.; Haine, J.E.; Zhang, X.; Williams, Z.T.; Norslien, K.; Campbell, B.; Wassenaar, T.; et al. Barriers and facilitators to the use of survivorship care plans by hematopoietic stem cell transplant survivors and clinicians. Support. Care Cancer 2022, 30, 1323–1330. [Google Scholar] [CrossRef]
- Kelly, S.L.; Steinberg, E.A.; Suplee, A.; Upshaw, N.C.; Campbell, K.R.; Thomas, J.F.; Buchanan, C.L. Implementing a home-based telehealth group adherence intervention with adolescent transplant recipients. Telemed. e-Health 2019, 25, 1040–1048. [Google Scholar] [CrossRef]
- Killian, M.O.; Clifford, S.; Lustria, M.L.A.; Skivington, G.L.; Gupta, D. Directly observed therapy to promote medication adherence in adolescent heart transplant recipients. Pediatr. Transplant. 2022, 26, e14288. [Google Scholar] [CrossRef]
- Odisho, A.Y.; Liu, A.W.; Maiorano, A.R.; Bigazzi, M.O.A.; Medina, E.; Leard, L.E.; Shah, R.; Venado, A.; Perez, A.; Golden, J.; et al. Design and implementation of a digital health home spirometry intervention for remote monitoring of lung transplant function. J. Heart Lung Transplant. 2023, 42, 828–837. [Google Scholar] [CrossRef]
- O’Brien, T. Lessons Learned for Training a Research Team and Teaching Kidney Transplant Recipients How to Use a Mobile Health Technology for Dietary Intake and Physical Activity via a Virtual Platform. Nephrol. Nurs. J. 2022, 49, 527–530. [Google Scholar] [CrossRef]
- Gomis-Pastor, M.; Perez, S.M.; Minguell, E.R.; Loidi, V.B.; Lopez, L.L.; Abarca, S.R.; Tugas, E.G.; Mas-Malagarriga, N.; Bafalluy, M.A.M. Mobile health to improve adherence and patient experience in heart transplantation recipients: The mHeart trial. Healthcare 2021, 9, 463. [Google Scholar] [CrossRef]
- Killian, M.O.; Schelbe, L.; Lustria, M.L.A.; Watkivs, M.; Gupta, D. Engaging Adolescent Heart Transplant Recipients Through In-App Messaging During Mobile Health Intervention. Prog. Transplant. 2023, 33, 229–235. [Google Scholar] [CrossRef] [PubMed]
- Sayegh, C.; Im, D.; Moss, I.K.; Urquiza, R.; Patel, S.; Thomas, D.W. Randomized pilot trial of praise text messages to improve medication adherence among adolescents and young adults with liver transplants. Pediatr. Transplant. 2022, 26, e14361. [Google Scholar] [CrossRef] [PubMed]
- Vaughn, J.; Gollarahalli, S.; Shaw, R.J.; Docherty, S.; Yang, Q.; Malhotra, C.; Summers-Gockerman, E.; Shah, N. Mobile health technology for pediatric symptom monitoring: A feasibility study. Nurs. Res. 2020, 69, 142–148. [Google Scholar] [CrossRef]
- Hickman, I.J.; Hannigan, A.K.; Johnson, H.E.; Elvin-Walsh, L.; Mayr, H.L.; Staudacher, H.M.; Barnett, A.; Stoney, R.; Salisbury, C.; Jarrett, M.; et al. Telehealth-delivered, cardioprotective diet and exercise program for liver transplant recipients: A randomized feasibility study. Transplant. Direct 2021, 7, e667. [Google Scholar] [CrossRef]
- Pollockm, M.D.; Stauffer, N.; Lee, H.; Chow, S.; Satoru, I.; Moats, L.; Swan-Nesbit, S.; Li, Y.; Roberts, J.K.; Ellis, M.J.; et al. MyKidneyCoach, patient activation, and clinical outcomes in diverse kidney transplant recipients: A randomized control pilot trial. Transplant. Direct 2023, 9, e1462. [Google Scholar] [CrossRef]
- Delman, A.M.; Turner, K.M.; Jones, C.R.; Vaysburg, D.M.; Silski, L.S.; King, C.; Luckett, K.; Safdar, K.; Quillin, R.C.; Shah, S.A. Keeping the lights on: Telehealth, testing, and 6-month outcomes for orthotopic liver transplantation during the COVID-19 pandemic. Surgery 2021, 169, 1519–1524. [Google Scholar] [CrossRef]
- John, B.V.; Love, E.; Dahman, B.; Kurbanova, N.; Konjeti, V.R.; Sundaram, L.T.; Deng, Y.; Aubuchon, S.; Heuman, D.; Bajaj, J.S.; et al. Use of telehealth expedites evaluation and listing of patients referred for liver transplantation. Clin. Gastroenterol. Hepatol. 2020, 18, 1822–1830. [Google Scholar] [CrossRef]
- Anton, C.M.; Drake, M.B.; Butts, R.J.; Cao, T.; Rezaeizadeh, A.; Trivedi, M.H.; Triplett, K.N. Electronic mental health screening in a pediatric heart failure and transplant clinic. J. Clin. Psychol. Med. Settings 2021, 28, 815–825. [Google Scholar] [CrossRef]
- Andrew, N.; Barraclough, K.A.; Long, K.; Barraclough, K.A.; Fazio, T.N.; Holt, S.; Kanhutu, K.; Hughes, P.D. Telehealth model of care for routine follow up of renal transplant recipients in a tertiary centre: A case study. J. Telemed. Telecare 2020, 26, 232–238. [Google Scholar] [CrossRef]
- Fleming, J.N.; Gebregziabher, M.; Posadas, A.; Su, Z.; McGillicuddy, J.W.; Taber, D.J. Impact of a pharmacist-led, mHealth-based intervention on tacrolimus trough variability in kidney transplant recipients: A report from the TRANSAFE Rx randomized controlled trial. Am. J. Health-Syst. Pharm. 2021, 78, 1287–1293. [Google Scholar] [CrossRef]
- Gomis-Pastor, M.; Mirabet Perez, S.; De Dios Lopez, A.; Brossa Loidi, V.; Lopez Lopez, L.; Pelegrin Cruz, R.; Mangues Bafalluy, M.A. Does an eHealth Intervention Reduce Complications and Healthcare Resources? A mHeart Single-Center Randomized-Controlled Trial. J. Cardiovasc. Dev. Dis. 2023, 10, 77. [Google Scholar] [CrossRef] [PubMed]
- Forbes, R.C.; Broman, K.K.; Johnson, T.B.; Forbes, R.C.; Johnson, T.B.; Rybacki, D.B.; Hannah Gillis, A.E.; Hagemann Williams, M.; Shaffer, D.; Feurer, I.D.; et al. Implementation of telehealth is associated with improved timeliness to kidney transplant waitlist evaluation. J. Telemed. Telecare 2018, 24, 485–491. [Google Scholar] [CrossRef] [PubMed]
- Huuskes, B.M.; Scholes-Robertson, N.; Guha, C.; Baumgart, A.; Wong, G.; Kanellis, J.; Chadban, S.; Barraclough, K.A.; Viecelli, A.K.; Hawley, C.M.; et al. Kidney transplant recipient perspectives on telehealth during the COVID-19 pandemic. Transpl. Int. 2021, 34, 1517–1529. [Google Scholar] [CrossRef] [PubMed]
- Maroney, K.; Curtis, L.M.; Opsasnick, L.; Smith, K.D.; Eifler, M.R.; Moore, A.; Wedd, A.; Wolf, M.S.; Patzer, R.E. eHealth literacy and web-based patient portal usage among kidney and liver transplant recipients. Clin. Transplant. 2021, 35, e14184. [Google Scholar] [CrossRef] [PubMed]
- Mathur, S.; Janaudis-Ferreira, T.; Hemphill, J.; Cafazzo, J.A.; Hart, D.; Holdsworth, S.; Lovas, M.; Wickerson, L. User-centered design features for digital health applications to support physical activity behaviors in solid organ transplant recipients: A qualitative study. Clin. Transplant. 2021, 35, e14472. [Google Scholar] [CrossRef]
- O’Brien, T.; Rosenthal, A. Preferred Features in Mobile Health Applications for Kidney Transplant Recipients: A Qualitative Approach. Nephrol. Nurs. J. 2020, 47, 529–536. [Google Scholar] [CrossRef]
- Schmidt, D.; Osmanodja, B.; Pfefferkorn, M.; Graf, V.; Raschke, D.; Duettmann, W.; Naik, M.G.; Gethmann, C.J.; Mayrdorfer, M.; Halleck, F.; et al. TBase—An Integrated Electronic Health Record and Research Database for Kidney Transplant Recipients. J. Vis. Exp. 2021, 170, e61971. [Google Scholar] [CrossRef]
- Tang, J.; Howell, M.; Lee, V.W.; Guha, C.; Dominello, A.; Roger, S.; Keung, K.; Teixeira-Pinto, A.; Tong, A.; Wong, G. Patients’ Perspectives, Factors, and Patterns of eHealth Use in Kidney Transplant Recipients. Kidney Int. Rep. 2023, 8, 727–736. [Google Scholar] [CrossRef]
- Thiessen, C.; Wisel, S.A.; Yamaguchi, S.; Dietch, Z.C.; Feng, S.; Freise, C.E. Rapid modification of workflows and fellow staffing at a single transplant center to address the COVID-19 crisis. Transplant. Proc. 2020, 52, 2596–2600. [Google Scholar] [CrossRef]
- Zmaili, M.; Alzubi, J.; Alkhayyat, M.; Cohen, J.; Alkharabsheh, S.; Rana, M.; Alvarez, P.A.; Mansoor, E.; Xu, B. Takotsubo cardiomyopathy in orthotopic liver transplant recipients: A cohort study using multi-center pooled electronic health record data. World J. Hepatol. 2022, 14, 400–410. [Google Scholar] [CrossRef]
- Skeens, M.; Sezgin, E.; Stevens, J.; Landier, W.; Pai, A.; Gerhardt, C. An mHealth App to Promote Adherence to Immunosuppressant Medication and Track Symptoms in Children After Hematopoietic Stem Cell Transplant: Protocol for a Mixed Methods Usability Study. J. Med. Internet Res. Res. Protoc. 2022, 11, e39098. [Google Scholar] [CrossRef] [PubMed]
- DePaolo, C.A.; Wilkinson, K. Get Your Head into the Clouds: Using Word Clouds for Analyzing Qualitative Assessment Data. TechTrends 2014, 58, 38–44. [Google Scholar] [CrossRef]
- Niehm, L.S.; Tyner, K.; Shelley, M.C.; Fitzgerald, M.A. Technology adoption in small family-owned businesses: Accessibility, perceived advantage, and information technology literacy. J. Fam. Econ. Issues 2010, 31, 498–515. [Google Scholar] [CrossRef]
- Shelley, M.; Thrane, L.; Shulman, S.; Lang, E.; Beisser, S.; Larson, T.; Mutiti, J. Digital citizenship: Parameters of the digital divide. Soc. Sci. Comput. Rev. 2004, 22, 256–269. [Google Scholar] [CrossRef]
- Matthews, A.K.; Min, Y.J.; Akufo, J.; Burke, L.; Dodd, D.; Donenberg, G. Barriers to Using a Patient Portal Among Low-income Patient Populations: A Qualitative Descriptive Study. J. Health Care Poor Underserved 2023, 34, 863–883. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).