Abstract
Posttraumatic carotid-cavernous fistula is a very rare complication that can occur in patients with craniomaxillofacial trauma. Symptoms involve headache, diplopia, ptosis of the upper lid, conjunctival chemosis, pulsating exophthalmos, and ophthalmoplegia. Diagnosis can be challenging because various pathologic entities can present with similar symptoms such as superior orbital fissure syndrome, orbital apex syndrome, retrobulbar hematoma, and cavernous sinus syndrome. However, accurate and early diagnosis is of utmost importance because treatment delay may lead to blindness or permanent neurologic deficits. In this article, a case of posttraumatic carotid-cavernous fistula that was twice misdiagnosed is presented.
Posttraumatic intracranial aneurysms are mainly related to perforating injuries and fractures of the cerebral and facial cranium and less frequently to iatrogenic causes such as otorhinolaryngological and maxillofacial operations [,]. They comprise less than 1% of all intracranial aneurysms despite the relatively high frequency of craniomaxillofacial trauma []. The first case of posttraumatic intracranial aneurysm was reported in 1829 by Smith who refers to a young patient who sustained trauma to the left temporal area and ultimately developed a middle meningeal artery aneurysm []. Posttraumatic carotid-cavernous fistula (CCF) occurs in 0.2 to 0.3% of patients with craniomaxillofacial trauma []. CCF is basically an abnormal communication that is created between the intracavernous portion of the internal carotid artery and the venous sinuses that comprise the cavernous sinus. The mechanism of its creation is related to the blood shunt which develops because of the pressure gradient between the high arterial pressure of the internal carotid artery and the low venous pressure of the cavernous sinus. This shunt results in increased pressure not only in the cavernous sinus but also in the structures that are normally drained by the cavernous sinus such as the orbits.
In this case report, a case of posttraumatic CCF that was twice misdiagnosed is presented.
1. Case Report
A 31-year-old man was admitted to Oral and Maxillofacial Clinic, Papanikolaou General Hospital, Thessaloniki. The patient was involved in a bicycle accident 2 days before his admission. The patient presented with gross facial swelling, flattening of the nasal dorsum, left periorbital ecchymosis, bilateral subconjunctival hemorrhage, and mild left exophthalmos. Clinical and radiographic examination revealed a fracture of the left zygomatic complex associated with hypoesthesia of the left infraorbital and supraorbital region, nasal fractures, and a mandibular fracture located on the right mandibular body. Ophthalmic examination revealed no pathologic signs. The patient had normal visual acuity (6/6 vision) and ocular motility. Diplopia was not detected. Fundus examination revealed no signs of pathology and intraocular pressure was measured 13 mm Hg, which is considered normal. Pupils were equal in size and reacted normally to light and accommodation.
On the 3rd day of hospitalization, the patient suddenly developed diplopia, left ophthalmoplegia especially at lateral gaze and dilatation of the left pupil. These findings suggested the diagnosis of superior orbital fissure syndrome (Figure 1). It was therefore assumed that these symptoms would probably improve spontaneously after the operation.
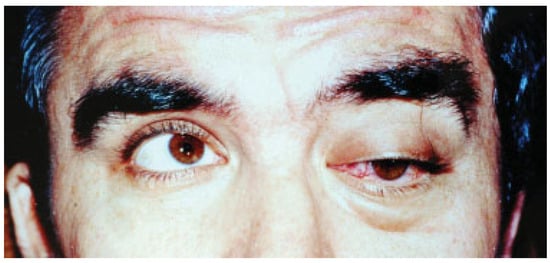
Figure 1.
Photograph of the patient presenting with marked left exophthalmos and left ophthalmoplegia. At that time, it was assumed that the patient suffered from superior orbital fissure syndrome.
On the 8th day, the patient was operated under general anesthesia. The operation involved intermaxillary fixation, reduction, and two-point fixation of the left zygomatic complex fracture and exploration of the fracture line of the orbital floor to release the contents of the orbital cavity that were entrapped. Finally, a piece of lyophilized dura was inserted on the orbital floor to prevent recurrence. No operation-related complications occurred postoperatively. However, left ophthalmoplegia and diplopia persisted with no improvement and on the 7th postoperative day (15th day of hospitalization) the patient was discharged.
Two weeks later, the patient presented for follow-up with marked improvement of eye movement, although diplopia was still present. Visual acuity (6/6 vision) and intraocular pressure (15 mm Hg) were still within normal limits. The patient was subsequently followed up every week. No change of the situation was observed during the following 3 weeks.
On the 21st postoperative day (31st postinjury day), the patient presented with marked left exophthalmos, periorbital swelling and ecchymosis, ptosis of the upper eyelid, ocular pain, nausea, and vomiting. The condition was diagnosed as periorbital cellulitis and double intravenous antibiotic therapy was initiated (Figure 2). Computerized tomography (CT) of the left orbit disclosed a mild inflammatory reaction around the miniplate in the infraorbital rim and in the region of the orbital floor. CT also revealed the presence of dilation of the upper ophthalmic vein but this finding was not further evaluated at that time (Figure 3). The clinical presentation of the patient was attributed to infection of foreign materials that were placed during the operation and therefore the plate and the lyophilized dura were removed.
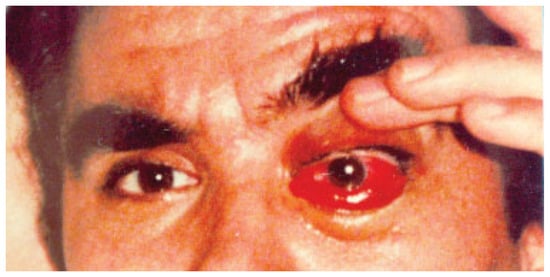
Figure 2.
Photograph of the patient presenting with periorbital and conjunctival swelling and chemosis. Ophthalmoplegia especially at lateral gaze persisted. This condition was again misdiagnosed as orbital cellulites.
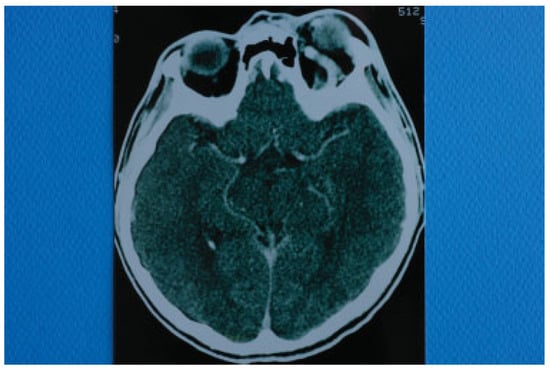
Figure 3.
Computed tomography of the skull taken with intravenous contrast medium. Dilation of left superior ophthalmic vein is depicted.
Two days after the removal of the foreign materials, there was a dramatic deterioration of the patient’s clinical presentation with intense ocular pain, worsening of exophthalmos, nausea, and vomiting. The patient also complained of “strange sounds in the cranium like water tapping.” Clinical examination revealed a systolic thrill on palpation of the left eye and a systolic wheeze on auscultation of the left frontal and temporal area. Measurement of intraocular pressure was subsequently performed and an intraocular pressure of 13 mm Hg in the right and 24 mm Hg in the left eye were recorded. Visual acuity was measured 5/6 vision and fundus examination revealed venous dilatation without further pathologic signs. The finding of intensive dilation of the left upper ophthalmic vein in the primary computed tomography was reevaluated and a posttraumatic CCF was suspected and included in the differential diagnosis. A new CT of the left orbit was ordered which revealed a threefold dilation of the cavernous sinus (Figure 4). The digital subtraction angiography (DSA) confirmed the diagnosis of CCF as it revealed a dilation of the cavernous sinus, a blood shunt between the lumen of the internal carotid artery and the cavity of the cavernous sinus, and a dilation of the upper ophthalmic vein (Figure 5).
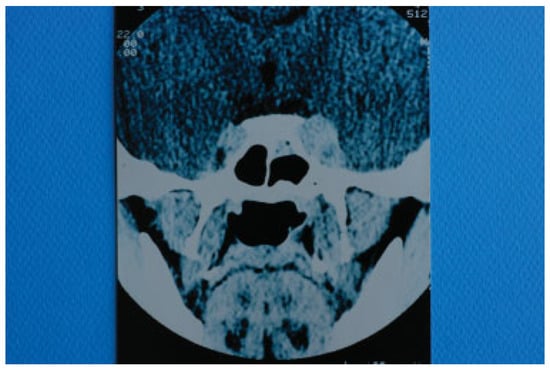
Figure 4.
Computed tomography of the base of the skull illustrating a threefold dilation of the left cavernous sinus.
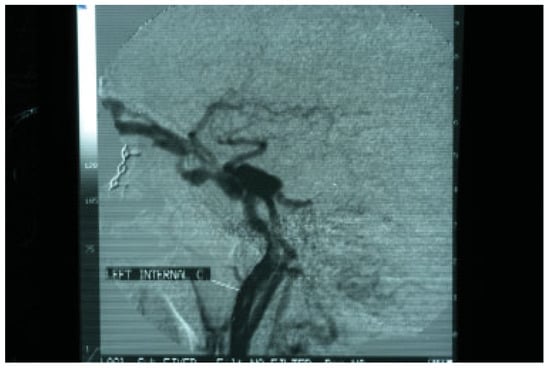
Figure 5.
Digital subtraction angiography (DSA) confirming the presence of a carotid cavernous fistula. A marked dilation of draining vessels can also be observed.
The patient was referred to a specialized center where a successful endovascular occlusion of the fistula with detachable balloon via transarterial cannulation took place. Three months later, all symptoms subsided and no permanent neurologic deficit was detected.
2. Discussion
Depending on histology and pathophysiology, intracranial aneurysms are divided into true aneurysms, pseudoaneurysms, and mixed aneurysms. In true aneurysms, there is intimal, internal elastic lamina, and media disruption with preservation of the adventitia whereas in pseudoaneurysms the entire arterial wall is disrupted. In pseudoaneurysms, the primary hemorrhage caused by the arterial wall disruption is gradually limited by cerebral parenchyma and the formation of blood clot. Subsequently, fibrinous remodeling takes place resulting in pseudoaneurysm formation. Finally, in mixed aneurysms, there is a posttraumatic disruption of a true aneurysm []. Posttraumatic intracranial aneurysms are most frequently pseudoaneurysms and usually develop in peripheral brain vessels and in the vessels of the skull base. Post-traumatic aneurysms of the skull base may involve the petrous, cavernous, or supraclinoidal part of the internal carotid artery. Whenever there is an abnormal communication between the cavernous segment of the internal carotid artery and the cavernous sinus with a blood shunt, a CCF has developed []. According to the classification system proposed by Barrow et al in 1985 (Table 1), posttraumatic CCFs are classified predominantly as type A aneurysms because usually there is a direct communication between the lumen of internal carotid artery and the sinusoids that comprise the cavernous sinus. The intracavernous segment of the internal carotid artery is bounded by strong dural attachments at its entrance into the cavernous sinus and also at its exit from it. These attachments that keep the artery fixed at two points may be responsible for possible rupture of the wall of the vessel when a sudden acceleration–deceleration force is applied. The vessel may also be lacerated by bony spicules from fractures of the anterior clinoid processes and the orbital roof []. CCFs that belong to types B, C, and D usually develop spontaneously and are characterized by communication between dural branches of the internal or external carotid artery and the cavernous sinus []. In very rare circumstances, these types of fistulae result from trauma []. In the case presented here, a pseudoaneurysm of the cavernous portion of the internal carotid artery developed following a bicycle accident.

Table 1.
Classification of carotid-cavernous fistulas according to Barrow et al [].
The time interval between the time of injury and the onset of symptoms may vary from hours to years, but in 90% of cases, the symptoms appear within 2 to 3 weeks after injury [,]. In the case presented, symptoms of the aneurysm appeared early probably at presentation but were not well estimated and the diagnosis was actually confirmed 6 weeks after injury.
The clinical picture is explained by the sudden increase of the blood pressure in the cavernous sinus that leads to impaired drainage of structures that are normally drained by cavernous sinuses and increased pressure on structures that traverse the sinuses []. The cavernous sinuses are paired structures that are composed of multiple venous sinusoids. They receive blood from superior and inferior ophthalmic veins, pterygoid plexus, sphenoparietal sinuses, and superficial cerebral veins. Through these blood filled spaces pass the internal carotid artery and cranial nerves III (oculomotor), IV (trochlear), V1 (ophthalmic division of trigeminal nerve), V2 (the maxillary division of the trigeminal nerve), and VI (abducens). All these cranial nerves, except from VI, pass through the lateral wall of the sinus, while the cranial nerve VI passes through the middle of the sinus alongside the internal carotid artery.
The symptoms include headache, diplopia, ptosis of the upper lid, conjunctival chemosis, pulsating exophthalmos, and ophthalmoplegia [,]. Ophthalmoplegia is usually detected at lateral gaze because of the vicinity of cranial nerve VI to the internal carotid artery, but the patient may also present with total ophthalmoplegia because of paresis of cranial nerves III, IV, and VI []. Ophthalmoplegia is usually accompanied by sensory disorders of the supraorbital and infraorbital nerves because of paresis of the ophthalmic and maxillary division of trigeminal nerve such as in the case presented here. This finding was not adequately evaluated during the first clinical examination. CCF may manifest itself either with ipsilateral miosis when the sympathetic fibers that travel along the internal carotid artery are transected or with ipsilateral mydriasis when the parasympathetic fibers that travel with cranial nerve III are predominantly affected as in our case [,]. The patient may also complain of sphygmic and wheezing sounds in the head. The bruit stops or improves with digital compression of the ipsilateral carotid artery. Moreover, the rupture of the aneurysm into the cavernous sinus causes a blood shunt producing systolic wheeze on auscultation of the frontal, temporal, and orbital area. Prevention of venous orbital drainage to the cavernous sinus causes intensive periorbital edema []. A common and very impressive sign is pulsating exophthalmos which is the result of arterial flow into the orbital veins that results in sphygmic down and lateral displacement of the globe []. Exophthalmos is usually accompanied by severe pain and loss of visual acuity caused mainly by thrombosis of the superior ophthalmic vein. If the patient is not treated, an increase of the venous pressure in retinal capillaries may result in hyaloid hemorrhage and blindness [].
In our case, the internal carotid artery aneurysm ruptured to the cavernous sinus on the 5th week after injury (21th postoperative and 31th postinjury day). Sensory disorders of the supraorbital and infraorbital nerves were present at initial presentation, but they were not adequately evaluated. Symptoms and signs of the CCF were identical to those referred in the literature such as diplopia, ophthalmoplegia, pupil dilation, exophthalmos, periorbital swelling, conjunctival chemosis, ptosis of the upper eyelid, ocular pain, nausea and vomiting, “strange sounds in the cranium like water tapping,” systolic wheeze on auscultation of the left frontal and temporal area and systolic thrill on palpation of the left eye.
The suspicion for the formation or rupture of a posttraumatic intracranial aneurysm of the intracavernous segment of the internal carotid artery is set by the clinical findings and is confirmed with further imaging assessment. The method of choice is four-vessel DSA, because it provides information on the location and size of the aneurysm or fistula [,]. Standard CT of the brain is usually performed at admission and may reveal signs of aneurysm or CCF formation such as ophthalmic vein dilation, basilar skull fractures, bony spicules, or herniation of the cavernous sinus into the sphenoid sinus [].
Differential diagnosis is difficult because various pathologic entities present with similar symptoms. It includes the superior orbital fissure syndrome, orbital apex syndrome, retrobulbar hematoma, and cavernous sinus syndrome [] (Table 2). In fact, the superior orbital fissure, the orbital apex, and the cavernous sinus are contiguous anatomical structures that may be affected by similar causes such as traumatic, inflammatory, neoplastic, and vascular (Figure 6 and Figure 7). Consequently, a broad category of diseases can cause the so-called superior orbital syndrome or the orbital apex syndrome or the cavernous sinus syndrome. Posttraumatic CCF is basically a vascular cause of the cavernous sinus syndrome. The symptoms of all the earlier-mentioned syndromes are similar because almost the same cranial nerves are involved, but there are some differences that help establishing the exact diagnosis. In the case of the superior orbital fissure syndrome, the patient may present with ophthalmoplegia, diplopia, hypesthesia in the distribution of V1, upper lid ptosis, exophthalmos and fixation, and dilatation of the pupil. If the orbital apex (orbital apex syndrome) is also involved, visual loss is also added to the clinical picture. If the cavernous sinus is involved (cavernous sinus syndrome), the clinical manifestations may involve the features of the superior orbital fissure syndrome with the added involvement of the maxillary branch of trigeminal nerve (V2) and oculosympathetic fibers []. When the cavernous sinus syndrome is caused by a CCF, all these symptoms may be present. Moreover, pulsatile exophthalmos is usually present, a clear systolic wheeze is typically heard on auscultation of the orbital region, the patient usually complains of “strange noises in the head” and the intraocular pressure may be elevated. When these symptoms and signs are present in a patient with a history of craniomaxillofacial trauma, post- traumatic CCF must be suspected. In the case presented, diagnosis of posttraumatic carotid aneurysm initially and CCF later was difficult for two reasons. The first reason was the associated facial fractures of the zygomatic complex, nasal bones, and orbital floor which cause similar findings and led to the first false diagnosis of posttraumatic superior orbital fissure syndrome. Second, the osteosynthetic and alloplastic material that were used around the left eye led to the other false diagnosis of postoperative infection-orbital cellulitis. The persistent clinical signs and their deterioration despite removal of foreign materials and intravenous antibiotics led to the right diagnosis of CCF. However, a high index of suspicion and a deep knowledge of this pathologic entity would probably lead to the right diagnosis from the beginning, if auscultation of the orbital region had been performed.

Table 2.
Differential diagnosis of superior orbital fissure syndrome, orbital apex syndrome, cavernous sinus syndrome, retrobulbar hematoma, and carotid-cavernous fistula.
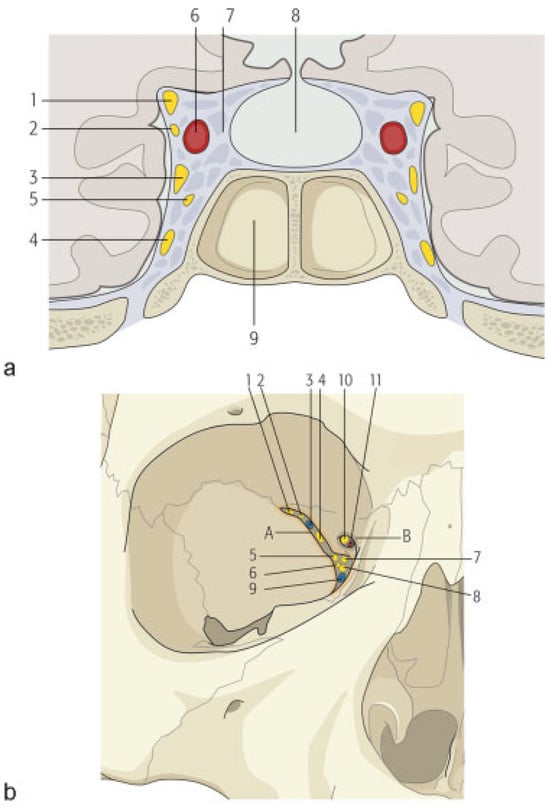
Figure 6.
(a) Schematic drawing showing which structures pass through the cavernous sinus and are consequently affected in case of cavernous sinus syndrome or carotidcavernous fistula (1) oculomotor nerve, (2) trochlear nerve, (3) ophthalmic division of trigeminal nerve, (4) maxillary division of trigeminal nerve, (5) abducens nerve, (6) internal carotid artery, (7) cavernous sinus, (8) pituitary, and (9) sinus sphenoidalis. (b) Schematic drawing showing the superior orbital fissure and the optic foramen together with the structures that pass through each of them. In case of a fracture that involves the superior orbital fissure, structures that pass through the fissure into the orbit are usually affected. If the optic foramen is also involved, the patient also suffers from loss of visual acuity due to mechanical compression of the optic nerve or the central ophthalmic artery. (1) lacrimal nerve, (2) frontal nerve, (3) superior ophthalmic vein, (4) trochlear nerve, (5) oculomotor nerve superior branch, (6) abducens nerve, (7) nasociliary nerve, (8) oculomotor nerve inferior branch, (9) inferior ophthalmic vein, (10) optic nerve, (11) ophthalmic artery, (A) superior orbital fissure, (B) optic foramen.
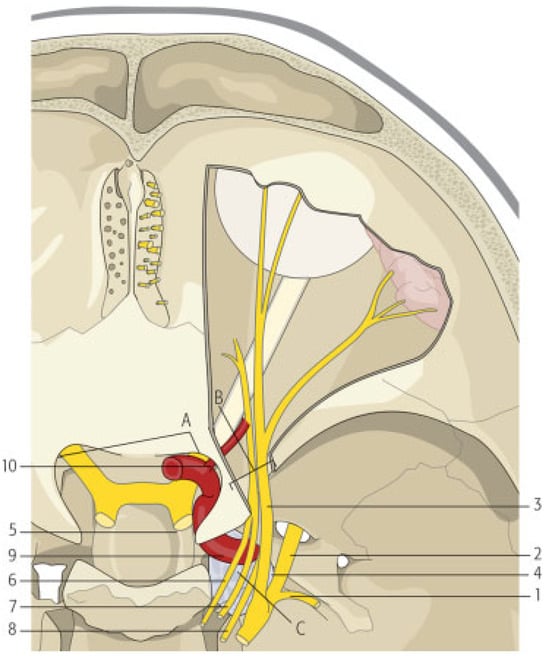
Figure 7.
Schematic drawing showing the anatomic continuity of the cavernous sinus, the orbital apex, and the superior orbital fissure. Posttraumatically, each of these structures may be involved with similar clinical manifestations. Cranial nerves III, IV, VI, and V1 pass through both the cavernous sinus and the superior orbital fissure to enter the orbit. This is the reason why diplopia, ophthalmoplegia, ptosis of the upper lid, mydriasis, and frontal sensory loss are common manifestations. Maxillary division of the trigeminal nerve passes through the cavernous sinus but not through the superior orbital fissure. (It exits the cranium through foramen rotundum). This is the reason why sensory loss of infraorbital area, nose, and upper lip is not a symptom of superior orbital fissure syndrome. Sympathetic fibers travel with the internal carotid artery which does not pass through the superior orbital fissure and this is the reason why if miosis and Horner syndrome is clinically detected, one should suspect cavernous sinus syndrome or carotid-cavernous fistula. (1) Mandibular division of trigeminal nerve, (2) maxillary division of trigeminal nerve, (3) cav- ernous sinus, (4) optic nerve, (5) internal carotid artery traveling through cavernous sinus, (6) oculomotor nerve, (7) trochlear nerve, (8) abducens nerve, (9) ophthalmic division of trigeminal nerve, (10) ophthalmic artery exiting through optic foramen, (A) optic foramen, (B) superior orbital fissure, and (C) cavernous sinus.
A variety of techniques have been proposed for treatment of posttraumatic carotid aneurysms or fistulas. Direct surgical exposure to achieve obliteration of the fistula with muscle or/ and distal carotid ligation has been widely advocated before the evolution of endovascular surgery [,]. Carotid ligation results in decrease of the intracranial carotid pressure with gradual healing of the aneurysmal wall of the vessel, formation of collateral circulation, and pressure restoration to the original levels. Today, surgical exposure is advocated only when catheterization techniques fail because of high risk of ischemic complications []. With the advent of endovascular interventional radiology, new techniques developed that are usually performed in special centers by well-trained staff. The most popular technique is the insertion of a detachable balloon into the fistula either via catheterization of the carotid or femoral artery or via catheterization of the superior ophthalmic vein [,,]. If it is impossible to pass a balloon through a narrow fistula opening, embolization using coils may also prove useful []. Spontaneous cure of a small percentage of aneurysms is also reported [].
Although treatment of the aneurysm is not usually urgent and can be performed in a scheduled manner, there are three situations that must be recognized and urgently treated. The first one is an increase in intraocular pressure which exceeds 40 mm Hg, because the risk of blindness in such situations is very high. The second one is the radiographic sign of cavernous sinus herniation into the sphenoid sinus because of the high risk of uncontrollable epistaxis, and the third one is the development of acute hemiplegia, when there is not another identifiable cause. In this case, acute hemiplegia is the result of brain hypoperfusion because the fistula “steals” large quantities of blood from the brain (“steal” phenomenon) [,].
In conclusion, a posttraumatic CCF is a very rare complication of craniomaxillofacial trauma. Diagnosis requires a high index of suspicion because the clinical picture is often attributed to trauma and treatment delays. Such fistulas must be addressed by well-trained neurosurgeons to avoid permanent neurological damage or loss of vision. In the case presented here, misdiagnosis led to rupture of the aneurysm with deterioration of the clinical picture. Fortunately, the patient fully recovered with no permanent neurological damage.
References
- Lanigan, D.T.; Tubman, D.E. Carotid-cavernous sinus fistula following Le Fort I osteotomy. J. Oral Maxillofac. Surg. 1987, 45, 969–975. [Google Scholar] [CrossRef] [PubMed]
- Jones, G.M.; Ross, J.W. Carotico-cavernous fistula presenting as a late complication of facial trauma. Br. J. Oral Maxillofac. Surg. 1989, 27, 481–486. [Google Scholar] [CrossRef] [PubMed]
- Kumar, M.; Kitchen, N.D. Infective and traumatic aneurysms. Neurosurg. Clin. N. Am. 1998, 9, 577–586. [Google Scholar] [CrossRef]
- Smith, S. On the difficulties attending the diagnosis of aneurysm being a contribution to surgical diagnosis and to medical jurisprudence. Am. J. Med. Sci. 1829, 4, 237. [Google Scholar]
- Arseni, C.; Ghiţescu, M.; Cristescu, A.; Mihăilă, G.; Drăguţoiu, E. Traumatic carotido—Cavernous fistulas. Psychiatr. Neurol. Neurochir. 1970, 73, 237–242. [Google Scholar]
- Hu, W.Y.; Hudon, M. Traumatic carotid-cavernous fistula. Can. J. Neurol. Sci. 2000, 27, 71–72. [Google Scholar]
- Barrow, D.L.; Spector, R.H.; Braun, I.F.; Landman, J.A.; Tindall, S.C.; Tindall, G.T. Classification and treatment of spontaneous carotid-cavernous sinus fistulas. J. Neurosurg. 1985, 62, 248–256. [Google Scholar] [CrossRef]
- Fu, Y.; Ohata, K.; Tsuyuguchi, N.; Hara, M. Direct surgery for posttraumatic carotid-cavernous fistula as a result of an intradural pseudoaneurysm: Case report. Neurosurgery 2002, 51, 1071–1073. [Google Scholar]
- Chae, S.W.; Kang, H.J.; Lee, H.M.; Hwang, S.J. Tinnitus caused by traumatic posterior auricular artery—Internal jugular vein fistula. J. Laryngol. Otol. 2001, 115, 313–315. [Google Scholar] [CrossRef]
- Iida, K.; Kurisu, K.; Arita, K.; et al. Critical cerebral ischemia revealed by magnetic resonance imaging in a traumatic carotid-cavernous fistula without high-risk patterns on angiograms: A case report. J. Trauma 2002, 53, 109–111. [Google Scholar] [CrossRef]
- Jimenez, D.F.; Gibbs, S.R. Carotid-cavernous sinus fistulae in craniofacial trauma: Classification and treatment. J. Craniomaxillofac. Trauma 1995, 1, 7–15. [Google Scholar] [PubMed]
- Niamtu, J., III.; Campbell, R.L. Carotid cavernous fistula. J. Oral Maxillofac. Surg. 1982, 40, 52–56. [Google Scholar] [CrossRef]
- Dubov, W.E.; Bach, J.R. Delayed presentation of a carotid-cavernous sinus fistula in a patient with traumatic brain injury. Am. J. Phys. Med. Rehabil. 1991, 70, 178–180. [Google Scholar] [CrossRef] [PubMed]
- Keltner, J.L.; Satterfield, D.; Dublin, A.B.; Lee, B.C. Dural and carotid cavernous sinus fistulas. Diagnosis, management, and complications. Ophthalmology 1987, 94, 1585–1600. [Google Scholar] [CrossRef]
- Ahn, J.Y.; Lee, B.H.; Joo, J.Y. Stent-assisted Guglielmi detachable coils embolisation for the treatment of a traumatic carotid cavernous fistula. J. Clin. Neurosci. 2003, 10, 96–98. [Google Scholar] [CrossRef]
- Uehara, T.; Tabuchi, M.; Kawaguchi, T.; Mori, E. Spontaneous dural carotid cavernous sinus fistula presenting isolated ophthalmoplegia: Evaluation with MR angiography. Neurology 1998, 50, 814–816. [Google Scholar] [CrossRef]
- Fattahi, T.T.; Brandt, M.T.; Jenkins, W.S.; Steinberg, B. Traumatic carotidcavernous fistula: Pathophysiology and treatment. J. Craniofac. Surg. 2003, 14, 240–246. [Google Scholar] [CrossRef]
- Yeh, S.; Foroozan, R. Orbital apex syndrome. Curr. Opin. Ophthalmol. 2004, 15, 490–498. [Google Scholar] [CrossRef] [PubMed]
- Yonas, H.; Dujovny, M. “True” traumatic aneurysm of the intracranial internal carotid artery: Case report. Neurosurgery 1980, 7, 499–502. [Google Scholar] [CrossRef]
- Nishijima, M.; Iwai, R.; Horie, Y.; Oka, N.; Takaku, A. Spontaneous occlusion of traumatic carotid cavernous fistula after orbital venography. Surg. Neurol. 1985, 23, 489–492. [Google Scholar] [CrossRef]
- Fleischer, A.S.; Guthkelch, A.N. Management of high cervical-intra- cranial internal carotid artery traumatic aneurysms. J. Trauma 1987, 27, 330–332. [Google Scholar] [CrossRef] [PubMed]
- Flandroy, P.; Lenelle, J.; Collignon, J.; Stevenaert, A. Carotid cavernous fistula associated with Fogarty catheter angioplasty. AJNR Am. J. Neuroradiol. 1988, 9, 1242. [Google Scholar] [PubMed]
- Newton, T.H.; Hoyt, W.F. Dural arteriovenous shunts in the region of the cavernous sinus. Neuroradiology 1970, 1, 71–81. [Google Scholar] [CrossRef]
© 2014 by the author. The Author(s) 2014.