Abstract
The mandible is an important component of the orofacial skeleton, and resection of part of the mandible as part of head and neck oncological procedures can have dramatic impact on both function and cosmesis. In this article, we describe a new technique in the resection osteotomy and flap fixation that improves the stability and aesthetic outcome of the reconstruction. The mandibular resection is performed utilizing a horizontal osteotomy above the mandibular angle on one side and a stepped body or angled osteotomy on the other side. Our technique is unique as it allows flexibility in adjusting the chin point projection to give the best possible aesthetic outcome; it allows more bone-to-bone contact, which increases the stability; it reduces rotation; and it allows for use of miniplate fixation, facilitating future rehabilitation with implants. We have been using this technique with great success in our hospital, and we recommend its use for its improved flexibility, stability, and aesthetic outcome.
The mandible is an important component of the orofacial skeleton, and resection of part of the mandible as part of head and neck oncological procedures can have dramatic impact on both function and cosmesis.
It has been two decades since Hidalgo [1] reported the use of fibular flaps with 100% bone survival. Since then, various studies [2,3,4,5] have reported the reliability and safety of using free fibular transfers.
In this article, we describe a new technique in the resection osteotomy and flap fixation, which improves the stability and aesthetic outcome of the reconstruction.
Technique
The flap is raised in the usual way, before the pedicle is released, using a silicone template as a guide; osteotomies are made in the osseous part of the flap without shortening of the proximal or distal ends of the flap.
The mandibular resection is performed utilizing a horizontal osteotomy (Figure 1) above the mandibular angle on one side and a stepped body or angle osteotomy on the other side (Figure 2). A silicone template is created to the shape and dimension of the resected mandibular segment. The template is used as a guide to osteotomize the fibula at the donor site to reproduce the middle symphyseal segment of the mandible without shortening the fibula. The flap is then transferred to the recipient site and oriented so that one end will fit in the stepped osteotomy in a key and lock fashion (Figure 3) and the other end of the flap will overlap with the horizontal mandibular osteotomy (Figure 4), allowing room for adjustment in the anterior posterior direction to achieve the desired chin point projection (Figure 5). When the desired projection is achieved—guided by the silicone template—both ends of the flap are marked with a sterile pencil and trimmed using the saw; then miniplates are used to fix the flap in place (Figure 6).
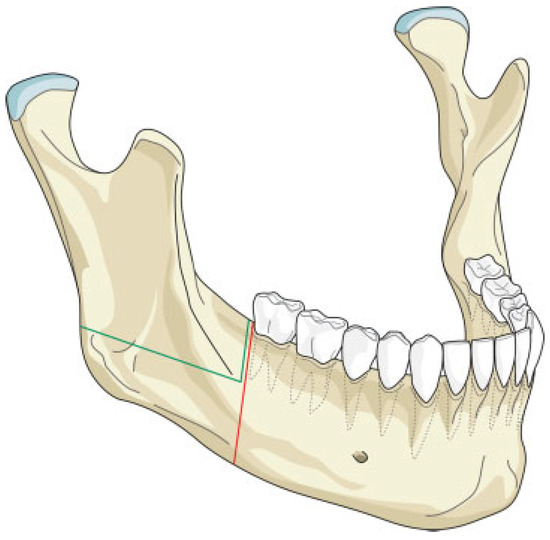
Figure 1.
Illustration of the horizontal osteotomy cuts (green lines). The red lines represent the conventional osteotomy cuts without the modification.
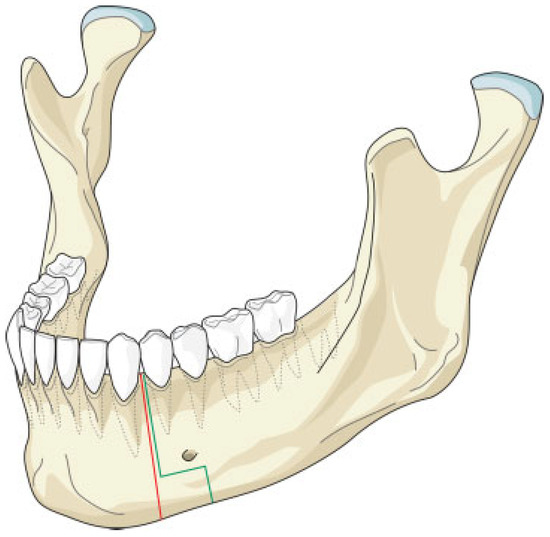
Figure 2.
Illustration of the stepped osteotomy cuts (black lines). The red lines represent the conventional osteotomy cuts without the modification.
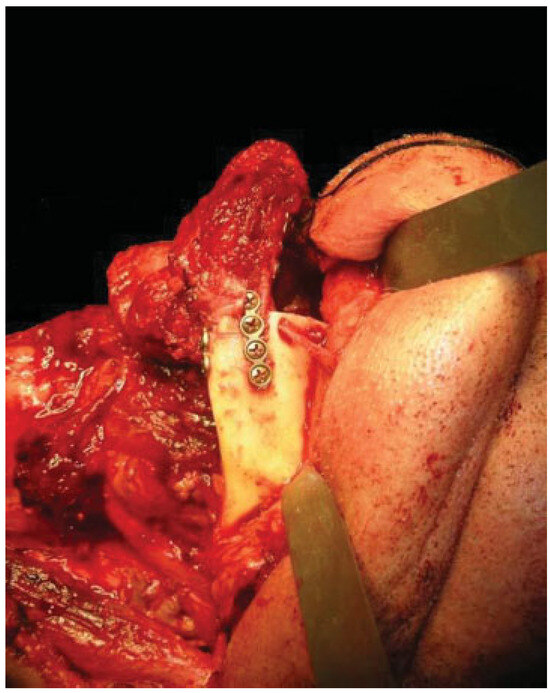
Figure 3.
Fibular flap fitting in key and lock fashion into the stepped mandibular osteotomy.
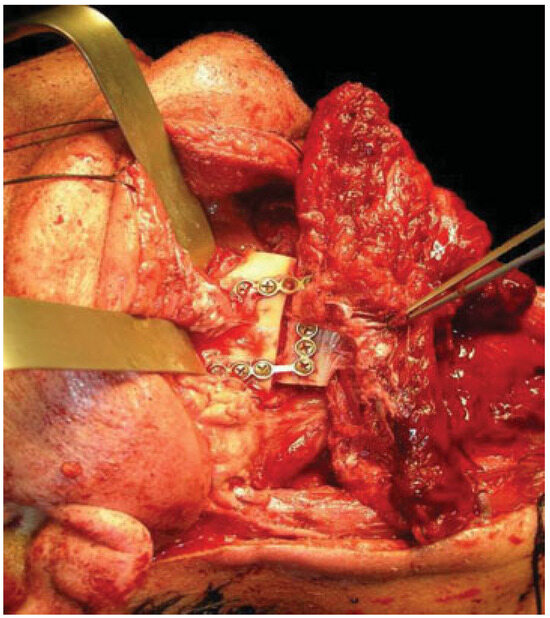
Figure 4.
Fibular flap overlapping with horizontal mandibular osteotomy allowing for anteroposterior adjustment.
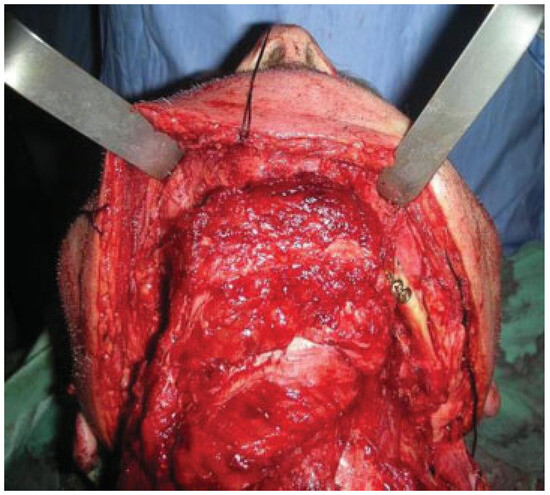
Figure 5.
Desired chin point projection achieved by anteroposterior adjustment of the flap.
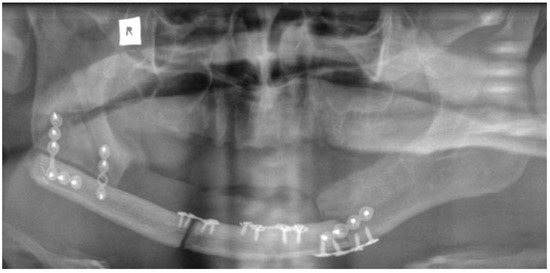
Figure 6.
An orthopantomogram showing the fibula flap in place with the horizontal and stepped osteotomy technique.
Discussion
Several techniques [6] and variations [7] in flap design and fixation have been described to improve the functional and aesthetic outcome of fibular flap reconstruction of the mandible.
Our technique is unique as it allows flexibility in adjusting the chin point projection to give the best possible aesthetic outcome. Trimming of the flap ends is performed at the recipient site to reduce the risk of short flap, but should this happen, the overlap at the horizontal osteotomy side will allow for compensation (Figure 4). Moreover, the greater surface contact area at the horizontal osteotomy side together with the key and lock fitting at the stepped osteotomy side (Figure 3) increase the stability of the flap and reduce the risk of rotation, hence allowing the use of miniplates for fixation; this in return allows room for placing more than one plate on each side, adding to the stability. The use of miniplates for fixation also facilitates the placement of implants in future rehabilitation.
We have been using this technique with great success at Royal Derby Hospital, and we recommend it for its improved flexibility, stability, and aesthetic outcome.
References
- Hidalgo, D.A. Fibula free flap: a new method of mandible reconstruction. Plast Reconstr Surg 1989, 84, 71–79. [Google Scholar] [PubMed]
- Shpitzer, T.; Neligan, P.C.; Gullane, P.J.; et al. Oromandibular reconstruction with the fibular free flap. Analysis of 50 consecutive flaps. Arch Otolaryngol Head Neck Surg 1997, 123, 939–944. [Google Scholar] [CrossRef] [PubMed]
- Peled, M.; El-Naaj, I.A.; Lipin, Y.; Ardekian, L. The use of free fibular flap for functional mandibular reconstruction. J Oral Maxillofac Surg 2005, 63, 220–224. [Google Scholar] [CrossRef] [PubMed]
- Belt, P.J.; Dickinson, I.C.; Theile, D.R.B. Vascularised free fibular flap in bone resection and reconstruction. Br J Plast Surg 2005, 58, 425–430. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Kim, M.J.; Kim, J.W. Mandibular reconstruction with free vascularized fibular flap. J Craniomaxillofac Surg 1995, 23, 20–26. [Google Scholar] [PubMed]
- Ruhin, B.; Menard, P.; Ceccaldi, J.; Dichamp, J.; Bertrand, J.C. Double-barrel fibular free flap for mandibular reconstruction: beneficial alternative for dentalimplanted rehabilitation (5 cases). Rev Stomatol Chir Maxillofac 2006, 107, 338–344; discussion 345–346. [Google Scholar] [CrossRef] [PubMed]
- Baker, N.J. Modification of the skin incision to allow versatility in placement of the skin paddle when raising a fibular osteocutaneous flap. Br J Oral Maxillofac Surg 2005, 43, 535–536. [Google Scholar] [CrossRef] [PubMed]
© 2011 by the author. The Author(s) 2011.