Abstract
Coronary vasospasm is often considered a rather benign condition. But one needs to take into account that they can trigger severe myocardial ischaemia causing ventricular arrhythmias and sudden cardiac arrest. Introduction of effective treatments, including calcium channel blockers are key. But individual response to various calcium channel blockers may differ.
Case description
History of presentation
A 54-year-old male was transferred to our hospital by air transportation after surviving a sudden cardiac arrest (SCA) secondary to ventricular fibrillation (VF) during breakfast. Besides arterial hypertension, he was previously healthy, but had lately noticed recurrent chest discomfort (“pressure-like” pain), which occasionally occurred at rest and during exertion.
Upon loss of consciousness, cardiopulmonary resuscitation had been immediately started by his family members and continued by the emergency medical service, who defibrillated the patient three times for VF. After return of spontaneous circulation, the initial electrocardiogram (ECG) indicated sinus rhythm with ST-segment elevations in leads V2–V4, highlighted in Figure 1. Consequently, the patient was transferred to our regional tertiary centre for an urgent coronary angiogram.
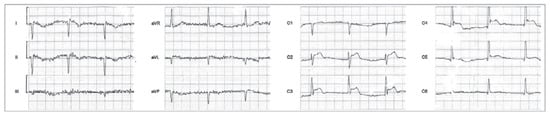
Figure 1.
Pre-hospital ECG after return of spontaneous circulation with ST-segment elevation in leads V2–V4.
Management
On arrival at our hospital, the patient was awake, and the ECG no longer indicated any acute abnormalities. The urgen coronary angiogram was unremarkable except for mild atherosclerosis (normal coronary blood flow, no angiographic evidence for thrombus or plaque rupture) (Figure 2). In addition, left ventriculography indicated moderate left ventricular dysfunction (ejection fraction 40%) with diffuse hypokinesia. The patient was admitted to our intensive care unit (ICU). Shortly after admission to the ICU, he started complaining of rapidly worsening chest discomfort, which was accompanied by recurrent ST-segment elevations in the anterior leads, as shown in Figure 3a. Sublingual nitroglycerine administration promptly improved both symptoms and the ECG changes (Figure 3b). Nevertheless, he developed a recurrent episode of VF secondary to early premature ventricular contractions (Figure 3c). This was immediately terminated by defibrillation at 200 joules.
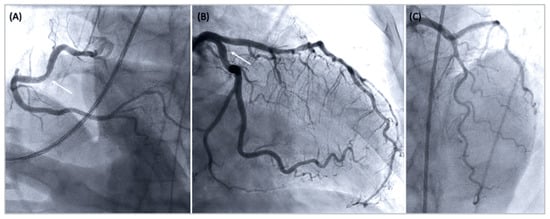
Figure 2.
Coronary angiogram indicating mild coronary atheromatosis (arrow): (A) right coronary artery – left anterior oblique cranial projection, (B) left circumflex – right anterior oblique caudal view, and (C) left anterior descending artery – cranial projection.
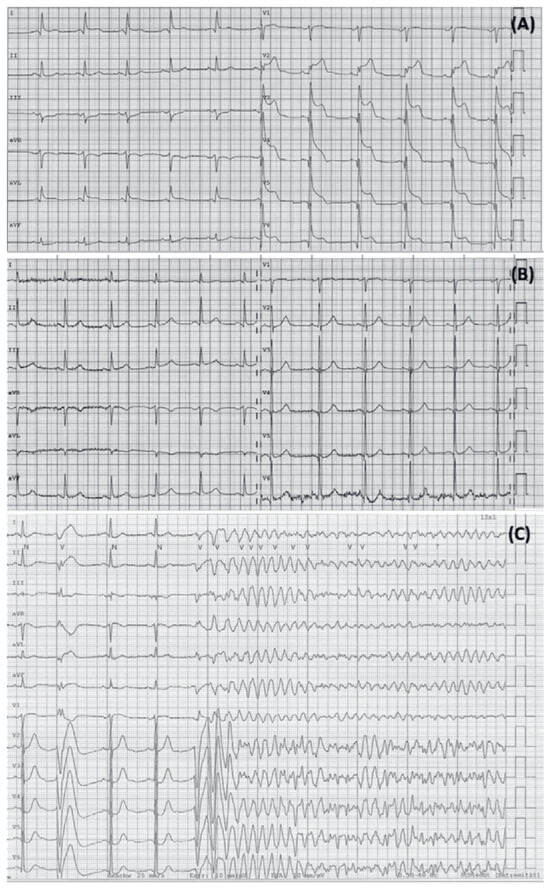
Figure 3.
ECGs after ICU admission: (A) Initial ECG indicating ST-segment elevation (accompanied by chest pain), (B) normal ECG during a pain-free period, and (C) Renewed ventricular fibrillation after episode of chest pain on ICU.
Since obstructive coronary artery disease had been excluded and we had no overt evidence of relevant cardiomyopathy, we primarily assumed Prinzmetal’s angina with coronary spasm inducing severe ischaemia and VF. Consequently, the patient was started on verapamil. Nevertheless, we ordered cardiac magnetic resonance tomography, which did not reveal any evidence of myocardial fibrosis, active myocarditis or any specific cardiomyopathy. Of note, the patient’s medical history and clinical evaluation did not reveal any typical triggers of vasospasm, including current smoking, recent alcohol consumption or abuse of amphetamines or cocaine.
After surviving SCA secondary to presumed coronary vasospasm, the decision was made to place an implantable cardiac defibrillator (ICD). Moreover, our patient did not show any further ischaemic symptoms or arrhythmias after initiation of the calcium channel blocker therapy. He recovered very well and was ultimately discharged after 9 days in hospital. Prior to discharge, an echocardiogram highlighted normalisation of the left ventricular function (EF 56%). Also, verapamil was switched to amlodipine with the expectation of fewer drug related side effects and better long-term tolerance.
Follow-up
A few days after discharge, while being assessed for cardiac rehabilitation, the patient reported recurrent chest discomfort at rest. A treadmill test had to be aborted because of angina and significant ST-segment elevation, displayed in Figure 4, which were immediately responsive to nitroglycerine. Consequently, amlodipine was replaced by verapamil again and our patient has remained asymptomatic ever since. The latest follow-up examination (12 months later) showed a normal treadmill test and biventricular function on echocardiography, and no arrhythmias in the ICD interrogation.
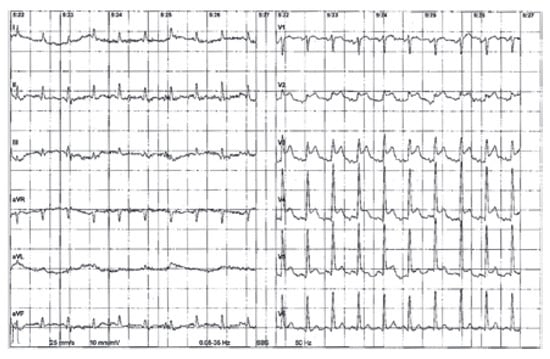
Figure 4.
ECG recorded during follow up treadmill test.
Discussion
We describe a rare case of a male patient who survived SCA secondary to a severe form of coronary vasospasm, which additionally showed a different therapy response to various calcium channel blockers.
In Western countries, SCA still represents one of the leading causes of death among adults. Coronary artery disease and cardiomyopathies are the most common underlying causes, whereas SCA secondary to coronary vasospasm appears to be a rare, but possibly underrecognised entity. Of note, a recent French study identified coronary vasospasm as the responsible mechanism in 2% of all SCA survivors investigated, with 9.7% of the affected patients already known to suffer from coronary vasospasm or vasospastic angina [].
The classic manifestation of vasospastic angina, which is characterised by a spontaneous, focal spasm of a major epicardial coronary artery, consequent resting angina, ST-segment elevation in the corresponding ECG leads and prompt relief after nitrate administration, was first described by Myron Prinzmetal as “a variant form of angina pectoris” in 1959 [,]. Nowadays the clinical picture of vasospastic angina is understood to be a broader phenomenon, which also includes distally pronounced diffuse vasospasm usually associated with ST-segment depression [,]. In contrast to classic angina pectoris, which results from a fixed atherosclerotic stenosis of a epicardial coronary artery, in patients with vasospastic angina the angina threshold is varying during daytime (with a peak during the night and in the early morning in many cases). Accordingly, there is no clear association between the cardiac oxygen demand – which, for example, is influenced by physical activity or emotional stress – and the occurrence of chest painIn contrast to classic angina, which often derives from obstructive atherosclerotic disease involving epicardial coronary arteries, the angina threshold varies during the daytime among patients with vasospastic angina with a peak seen during late nighttime and the early morning hours in many cases. Accordingly, there is no clear association between cardiac oxygen demand – which, for example, is influenced by physical activity or emotional stress – and the occurrence of chest pain in vasospastic angina []. Depending on the duration and the scale of myocardial ischaemia, coronary vasospasm not only causes angina, but can lead to myocardial infarction, life-threatening arrhythmias, atrioventricular block and SCA [].
The factors that contribute to the development of coronary vasospasm remain incompletely understood. It is presumed that individual and genetically determined response to potential triggers (e.g., alcohol, cocaine, catecholamines, acetylcholine, smoking) and the presence of precipitating factors (e.g., inflammation, vascular smooth muscle cell hyperreactivity, endothelial dysfunction) play an important role [,].
According to the diagnostic criteria recently published by the Coronary Vasomotion Disorders International Study Group (COVADIS) [], the diagnosis of a vasospastic angina can be made in the event of typical clinical symptoms, accompanying ischaemic ECG changes and/or angiographic documentation of coronary vasospasm (Table 1). However, it is paramount to rule out alternative entities, which may mimic the patterns of coronary vasospasm, including for instance small vessel coronary artery disease, embolic myocardial infarction, myopericarditis and takotsubo cardiomyopathy.

Table 1.
Diagnostic criteria for vasospastic angina according to COVADIS [].
Besides eradication of possible triggers, management of coronary vasospasm generally includes medical therapy with vasodilators. Acute vasospastic attacks may respond well to nitroglycerine, whereas calcium channel blockers are the drugs of choice for long-term prophylaxis [,,]. Furthermore, in patients with recurrent ventricular arrhythmias and SCA due to coronary vasospasm, an ICD may need to be evaluated []. Although calcium channel blockers have been shown to reduce anginal attacks and major adverse cardiac events in patients with coronary vasospasm [,,,], knowledge about the effectiveness of different forms of calcium channel blockers (dihydropyridines, phenylalkylamines and benzothiazepines) remains scarce. In this context, our case suggests that the intraindividual response to various calcium channel blockers can differ and that less selective calcium channel blockers with more systemic effects, such as the phenylalkylamine verapamil or the benzothiazepine diltiazem, may be more effective inpatients with persistent or life-threatening vasospastic attacks [,,]. This may be attributable not only to their differing vasodilatative properties, but also to their negative chronotropic and inotropic effects.
Conclusions
Although coronary vasospasm is often considered a rather benign condition, they can trigger severe myocardial ischaemia, which ultimately results in ventricular arrhythmias and SCA. This was illustrated by our case vignette. Therefore, early identification of this condition and introduction of effective management strategies, including elimination of potential triggers and vasodilatory drugs, are key. In this context, we moreover highlight that the response to various calcium channel blockers may differ between patients. This is important, since there appears to be a general opinion that the various calcium channel blockers might be equally efficacious in the treatment of vasospastic angina. Nevertheless, more studies evaluating optimal medical management, including the role of various calcium channel blockers, in patients with coronary vasospasm are needed.
Funding
There was no funding for this manuscript.
Acknowledgments
The authors wish to express their thank to our patient, who gave us permission to publish this case.
References
- Waldmann, V.; Bougouin, W.; Karam, N.; Narayanan, K.; Sharifzadehgan, A.; Spaulding, C.; et al. Paris-Sudden Death Expertise Center (Paris-SDEC) Investigators. Coronary Vasospasm-Related Sudden Cardiac Arrest in the Community. J Am Coll Cardiol. 2018, 72, 814–815. [Google Scholar] [CrossRef] [PubMed]
- Prinzmetal, M.; Kennamer, R.; Merliss, R.; Wada, T.; Bor, N. Angina pectoris. I. A variant form of angina pectoris; preliminary report. Am J Med. 1959, 27, 375–388. [Google Scholar] [CrossRef] [PubMed]
- Matta, A.; Bouisset, F.; Lhermusier, T.; Campelo-Parada, F.; Elbaz, M.; Carrié, D.; et al. Coronary Artery Spasm: new Insights. J Interv Cardiol. 2020, 58, 94586. [Google Scholar] [CrossRef] [PubMed]
- Montalescot, G.; Sechtem, U.; Achenbach, S.; Andreotti, F.; Arden, C.; Budaj, A.; et al. Document Reviewers. 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J. 2013, 34, 2949–3003. [Google Scholar] [CrossRef] [PubMed]
- Song, J.K. Coronary Artery Vasospasm. Korean Circ J. 2018, 48, 767–777. [Google Scholar] [CrossRef] [PubMed]
- Picard, F.; Sayah, N.; Spagnoli, V.; Adjedj, J.; Varenne, O. Vasospastic angina: A literature review of current evidence. Arch Cardiovasc Dis. 2019, 112, 44–55. [Google Scholar] [CrossRef] [PubMed]
- Beltrame, J.F.; Crea, F.; Kaski, J.C.; Ogawa, H.; Ong, P.; Sechtem, U.; et al. Coronary Vasomotion Disorders International Study Group (COVADIS). International standardization of diagnostic criteria for vasospastic angina. Eur Heart J. 2017, 38, 2565–2568. [Google Scholar] [PubMed]
- Baek, S.H. Class differences in calcium-channel blockers in vasospastic angina. Circ. J. Off. J. Jpn. Circ. Soc. 2010, 74, 1806–1807. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rodríguez-Mañero, M.; Oloriz, T.; le Polain de Waroux, J.B.; Burri, H.; Kreidieh, B.; de Asmundis, C.; et al. Long-term prognosis of patients with life-threatening ventricular arrhythmias induced by coronary artery spasm. Europace. 2018, 20, 851–858. [Google Scholar] [CrossRef] [PubMed]
© 2021 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.