Case Report
We report on a 15-year-old and apparently healthy boy, who was in search of work. He was planning to become an apprentice for train track building in the Swiss Railway company. As usual in Switzerland, the boy had a checkup performed by the Railway company doctor. His main clinical finding was a moderate hypertension measured at the right arm (142/ 88 mm Hg) and at the left arm (134/98 mm Hg).
Furthermore, in this tall patient (181 cm, 68 kg), a 2⁄6-systolic murmur was audible at the mid portion of the left sternal border. The patient was therefore referred to a cardiological examination including echocardiography, to identify the cause of the murmur.
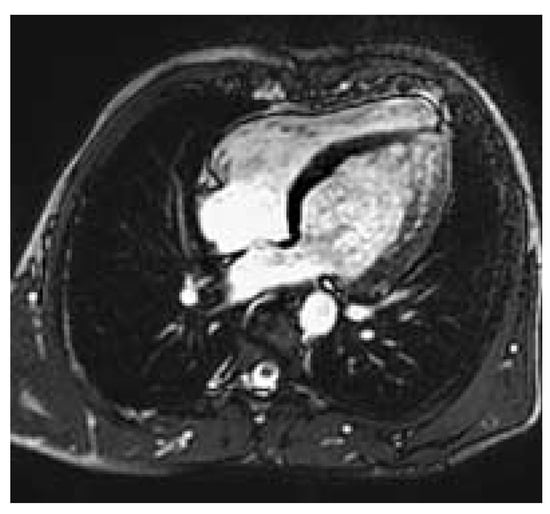
Figure 1.
Left ventricle with apical thinning and apical / periapical trabeculations.
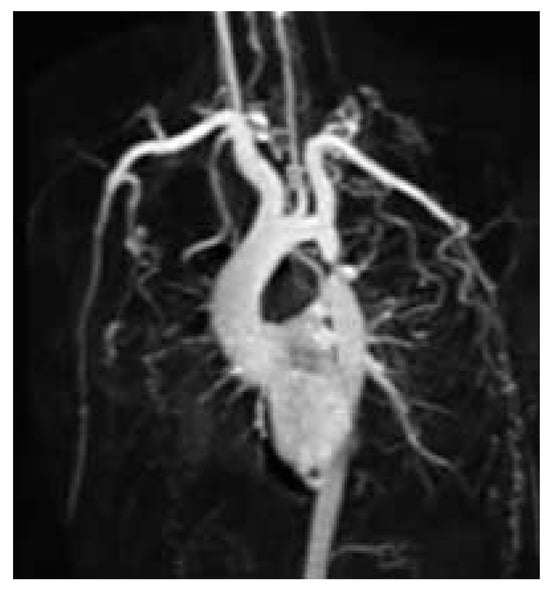
Figure 2.
Severe postductal coarctation with poststenotic saccular aneurysm and extensive collateral formation (CMR 3D contrast enhanced acquisition).
The chest radiograph showed no abnormality. The ECG at rest did not show left ventricular hypertrophy nor any other abnormality. However, on clinical examination, there was no palpable pulse in the lower extremities. The echocardiogram revealed the expected stenosis of the descending aorta with a peak gradient of 62 mm Hg. The left ventricle was not dilated (60 mm), but showed apical thinning (4.4 mm) and trabeculations with local hypokinesia. There was no valvular abnormality such as eg a bicuspid aortic valve, but a slight aortic root dilation (40 mm) was detected.
A cardiovascular magnetic resonance study (CMR) was performed at our institution in order to assess the exact location, the degree and severity of the aortic stenosis and to rule out associated congenital anomalies. CMR showed a normal left ventricular mass (181 g, 95.3 g/m2, [normal: 91 ± 11 g/m2]), a moderately reduced left ventricular ejection fraction of 37.6%, a diffuse, apically pronounced hypokinesia with apical trabeculations (fig. 1), and no late contrast enhancement. In CMR, the aortic root was slightly dilatated (40 mm), the ascending aorta was normal but the aortic arch was slightly hypoplastic. The proximal part of the descending aorta showed a severe postductal stenosis (fig. 2) of 28 mm in length, a small poststenotic saccular aneurysm (confirmed by surgery, fig. 3), and an extensive collateral vascular system through the subclavian, scapular, internal thoracic, and intercostal arteries. The origin and proximal course of the coronary arteries as well as the pulmonary venous return were normal.

Figure 3.
Specimen removed by operation showing the poststenotic saccular aneurysm.
The patient underwent successful surgical treatment by insertion of a short graft interponation. Postoperatively, the patient recovered without any complications. Three months after the surgical intervention, the echocardiogram showed an only slightly elevated peak pressure gradient of 34 mm Hg due to the hypoplastic aortic arch but no blood pressure difference between the upper and lower limbs any more.
Discussion
Postductal aortic stenosis is a typical narrowing of the aortic lumen with an incidence of 1:6000 live births. It may occur in patients with Turner’s syndrome, and may be associated with a ventricular septal defect, the Shone syndrome, and cerebral aneurysms in the circle of Willisi. The most frequent form is the postductal one (98%).
Early detection of this malformation is crucial. In patients operated before age 14, the 20-year survival of postductal coarctation after operation is 91%, after the age of 14 only 79% []. The major causes of death are aortic rupture and cerebral hemorrhage.
In unusual presentation as in our case including virtual absence of symptoms, an only mild hypertension, a normal ECG at rest, and a normal chest radiograph, the diagnosis is difficult and can be easily missed. However, the absence of the pulse in the lower limbs reveals the “pulseless disease”. The additional findings in our patient included a left ventricular dysfunction, apical thinning and increased trabeculations, which may, however, also be due to an unknown coincidence with a form of cardiomyopathy, to hypertension, or due to an association of the coarctation with non compacted myocardium. This latter association has been published in a series of 12 patients with ventricular noncompaction [].
In summary, surgery is the preferred method in severe coarctation, especially when signs of aortic wall weakness, a postductal saccular aneurysm, and a dilatation of the aortic root are already present. Percutaneous dilatation is effective solely in mild coarctation and in recurrent coarctation following surgical repair. In severe coarctation percutaneous dilatation remains controversial because of the risk of incomplete relief of obstruction or aneurysm formation []. Furthermore, in subjects with a hypoplastic aortic arch associated with coarctation, as in our patient, percutaneous intervention is not a feasible approach [].
References
- Cohen, M.; Fuster, V.; Steele, P.M.; Driscoll, D.; McGoon, D.C. Coarctation of the aorta. Long-term follow-up and prediction of outcome after surgical correction. Circulation 1989, 80, 840–845. [Google Scholar] [CrossRef] [PubMed]
- Ozkutlu, S.; Ayabakan, C.; Celiker, A.; Elshershari, H. Noncompaction of ventricular myocardium: a study of twelve patients. J Am Soc Echocardiogr 2002, 15, 1523–1528. [Google Scholar] [CrossRef] [PubMed]
- Gibbs, J.L. Congenital heart disease: interventional catheterization. Opening up I: the ventricular outflow tracts and great arteries. Heart 2000, 83, 111–115. [Google Scholar] [CrossRef] [PubMed]
- Eberli, F. Therapie angeborener und erworbener Herzklappenfehler. Was geht heute perkutan? Cardiovasc 2005, 2, 23–27. [Google Scholar]
© 2005 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.