Abstract
Nonbacterial thrombotic endocarditis is a rare form of noninfectious endocarditis with a very high rate of embolic complications. We present the case of a 74-year-old male with known metastatic biliary adenocarcinoma, who presented with acute ST-elevation myocardial infarction due to thrombotic occlusion of the right coronary artery in the context of a mitral and aortic valve marantic endocarditis.
Case report
A 74-year-old male with metastatic biliary adenocarcinoma was admitted directly to our coronary catheter laboratory because of an inferior ST-elevation myocardial infarction (STEMI) (Figure 1). The patient received loading doses of 500 mg aspirin, 60 mg prasugrel and 5000 IU nonfractionated heparin during prehospital care. The coronary angiogram showed a thrombotic occlusion of the distal segment of the right coronary artery but otherwise normal coronaries (Figure 2). The thrombus was aspirated with an Export Advance catheter; there was no underlying plaque and no stent was implanted. Antiplatelet therapy was interrupted, and therapeutic anticoagulation with nonfractionated heparin was initiated despite thrombocytopenia (75,000/mm3) and anaemia (haemoglobin 71 g/l), because a cardioembolic origin was suspected. Transthoracic echocardiography (TTE) revealed a dilated left ventricle with severely reduced ejection fraction (LVEF) of 30%. Vegetations were observed on both aortic and mitral valves (Figure 3), leading to severe aortic regurgitation and mitral regurgitation. There was no patent foramen ovale. The diagnosis of marantic endocarditis was made since the patient was afebrile, laboratory parameters did not show significant inflammation (C-reactive protein, leucocyte count), multiple blood cultures were negative (including polymerase chainreaction [PCR] tests for Coxiella, Brucella and Legionella) after several weeks, and there was clear underlying cancer. Although there was no neurological deficit, we performed a brain magnetic resonance imaging, which showed three, probably acute, ischaemic lesions (Figure 4) with a small haemorrhagic transformation. Anticoagulation was interrupted and upon his wish, the patient was discharged home with palliative care.
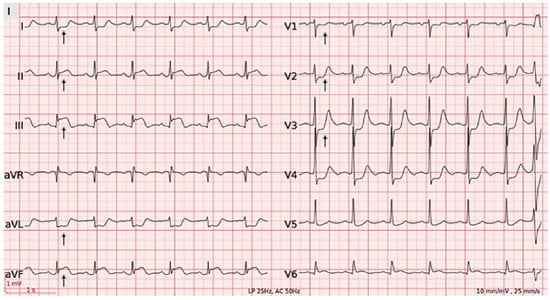
Figure 1.
ECG demonstrating normal sinus rhythm, normal axis, non specific intraventricular conduction delay, ST-segment elevation in II, III, aVF, ST depression in DI, aVL, V1–V3.
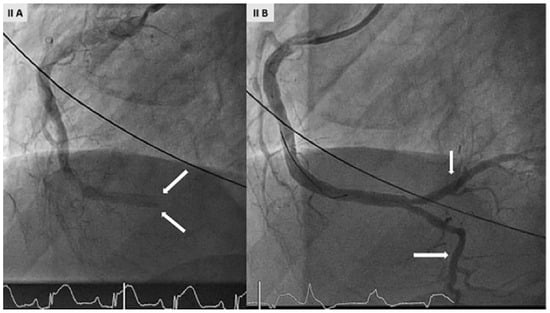
Figure 2.
(A) Coronary angiogram demonstrating an acute thrombotic occlusion of the distal segment of the right coronary artery (RCA) but otherwise normal coronaries. (B) good result with TIMI-3 flow in RCA after thrombectomy with an Export Advance catheter.
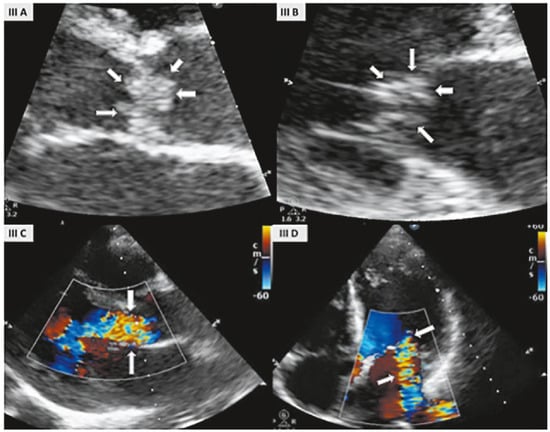
Figure 3.
Transthoracic echocardiography (TTE) parasternal long axis view with zoom showing large vegetations on both aortic (A) and mitral valve (B). Parasternal long axis view showing a severe aortic regurgitation (C); apical four chamber view showing dilated left atrium and left ventricle with severe mitral regurgitation (D).
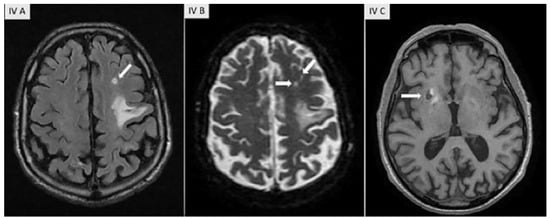
Figure 4.
Brain MRI-T2 flair, diffusion and T1 sequences demonstrating multiple both acute and old lesions compatible with emboli and one of them (in the right lenticular nucleus with haemorrhagic transformation).
Discussion
Nonbacterial thrombotic endocarditis (NBTE), also referred to as marantic, Libman-Sacks or verrucous endocarditis, is a rare form of noninfectious endocarditis with an estimated incidence of 0.9–1.6% on autopsy series [1]. This condition usually occurs in patients with advanced malignancy, mainly adenocarcinomas (pancreas, lung, colon, ovary, biliary and prostate) or systemic lupus erythematosus [2,3]. Inflammatory conditions such as antiphospholipid syndrome, rheumatic heart disease, rheumatoid arthritis, sepsis and burns are less common aetiologies.
The spectrum of lesions is broad, ranging from microscopic aggregates to large vegetations, predominantly on the aortic and mitral valves [1]. The vegetations seen in NBTE consist of platelet thrombi interwoven with strands of fibrin, immune complexes and mononuclear cells [4] and have a high risk of embolisation [5]. Thus, the major clinical manifestations of NTBE result from systemic embolisation, including cerebral and coronary, rather than valvular dysfunction [6,7,8]. When confronted with myocardial infarction in unusual settings, one should consider endocarditis as an embolic source [9].
Our patient was directly transferred to the catheter laboratory, bypassing the emergency department. Both the catheter laboratory personnel and interventional cardiologists were unaware of his detailed oncological history. However, this would probably not have changed the decision to go ahead with angiography. An embolic occlusion was suspected from the anatomy and absence of coronary artery disease. The next crucial step was thus to exclude a cardioembolic source, such as thrombus, intracardiac mass or vegetation, and patent foramen ovale.
There are, unfortunately, no echocardiographic criteria, whether transthoracic or transoesophageal, able to reliably distinguish bacterial from nonbacterial endocarditis [10,11]. A rigorous microbiological workup including several (at least three) sets of blood cultures is mandatory. The absence of typical and atypical organisms, negative PCR, and negative serology for Coxiella burnetii, Legionella spp., and Brucella spp. help support the diagnosis of NBTE [12]. Additional workup should include investigations for hypercoagulable states (lupus anticoagulant, antiphospholipid antibodies) and appropriate cancer screening [3,13].
In our case, although NBTE endocarditis was quickly suspected, given the comorbidities and echocardiographic findings, the patient was nonetheless given high-dose amoxicillin clavulanic acid until completion of the infectious disease workup, and subsequent negative blood cultures.
The management of NBTE consists of treating the underlying condition, with indefinite therapeutic anticoagulation due to the prothrombotic pathogenesis of the vegetation, its fragile nature and the high incidence of recurrent embolisation [2,14]. The risk of haemorrhagic transformation after stroke is high, so that brain computed tomography is recommended before initiation of the treatment to rule out intracranial haemorrhage. Therapeutic dose subcutaneous low molecular weight heparin or intravenous unfractionated heparin should be used rather than an anti-vitamin K inhibitor or a direct thrombin / factor Xa inhibitor. The indications for surgery in NBTE are the same as for infective endocarditis (large mobile vegetation, valvular dysfunction or recurrent embolic events despite anticoagulation), but surgery is performed only in selected cases where the risk is weighed against the benefits in patients who often have reduced life-expectancies from their underlying condition [3,15]. Regular clinical follow-up including repeat transthoracic echocardiography within the first 3 weeks, and every 3 months thereafter should be considered [3,5]. The overall prognosis is worse than for bacterial endocarditis, with high levels of morbidity due to neurocognitive dysfunction, death from recurrent embolisation and the underlying disease [5].
This case highlights several challenges, including the management of life-threatening situations in patients with advanced malignancies and shared decisionmaking, the risk benefit issues and complications of anticoagulation in patients with stroke due to a thrombotic mass, and the crucial role of interdisciplinary care.
Conflicts of Interest
No financial support and no other potential conflict of interest relevant to this article was reported.
References
- Lopez, J.A.; Ross, R.S.; Fishbein, M.C.; Siegel, R.J. Non bacterial thrombotic endocarditis: A review. Am Heart J. 1987, 113, 773–784. [Google Scholar] [CrossRef] [PubMed]
- El-Shami, K.; Griffiths, E.; Streiff, M. Non bacterial thrombotic endocarditis in cancer patients: Pathogenesis, diagnosis and treatment. Oncologist. 2007, 12, 518–523. [Google Scholar] [CrossRef] [PubMed]
- Roldan, C.A.; Shively, B.K.; Crawford, M.H. An echocardiographic study of valvular heart disease associated with systemic lupus erythematosus. N Engl J Med. 1996, 335, 1424–1430. [Google Scholar] [CrossRef] [PubMed]
- Eiken, P.W.; Edwards, W.D.; Tazelaar, H.D.; McBane, R.D.; Zehr, K.J. Surgical pathology of non bacterial thrombotic endocarditis in 30 patients, 1985–2000. Mayo Clinic Proc. 2001, 76, 1204–1212. [Google Scholar] [CrossRef] [PubMed]
- Roldan, C.A.; Sibbit, W.L., Jr.; Qualls, C.R.; Jung, R.E.; Greene, E.R.; Gasparovic, C.M.; et al. Libman-Sacks endocarditis and embolic cerebrovascular disease. JACC Cardiovasc Imaging. 2013, 6, 973–983. [Google Scholar] [CrossRef] [PubMed]
- Borowski, A.; Ghodsizad, A.; Cohnen, M.; Gams, E. Recurrent embolism in the course of marantic endocarditis. Ann Thorac Surg. 2005, 79, 2145–2147. [Google Scholar] [CrossRef] [PubMed]
- Graus, F.; Rogers, L.R.; Posner, J.B. Cerebrovascular complications in patients with cancer. Medicine (Baltimore) 1985, 64, 16–35. [Google Scholar] [CrossRef] [PubMed]
- Tiong, I.S.; William, M.J.; Perez, D.J. Non bacterial thrombotic endocarditis with ST-elevation myocardial infarction treated with percutaneous coronary aspiration thrombectomy. Heart Lung Circ. 2013, 22, 386–389. [Google Scholar] [CrossRef] [PubMed]
- Arroyo, D.; Cook, S.; Hayoz, D.; Togni, M. “The plug and the bug” – a case of coronary embolism in bacterial endocarditis. Cardiovascular Medicine. 2014, 17, 24–26. [Google Scholar]
- De Bruijn, S.F.; Agema, W.R.; Lammers, G.J.; van der Wall, E.E.; Wolterbeek, R.; Holman ERet, a.l. Transesophageal echocardiography is superior to transthoracic echocardiography in management of patients of any age with transient ischemic attack or stroke. Stroke. 2006, 37, 2531–2534. [Google Scholar] [CrossRef] [PubMed]
- Dutta, T.; Karas, M.G.; Segal, A.Z.; Kizer, J.R. Yield of transoesophageal echocardiography for non bacterial thrombotic endocarditis and other cardiac sources of embolism in cancer patients with cerebral ischemia. Am J Cardiol. 2006, 97, 894–898. [Google Scholar] [CrossRef] [PubMed]
- Habib, G.; Lancelotti, P.; Antunes, M.J.; Bongiorni, M.G.; Casalta, J.P.; Del Zotti, F.; et al. 2015 ESC guidelines for the management of infective endocarditis. The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Eur Heart J. 2015, 36, 3075–3128. [Google Scholar] [CrossRef] [PubMed]
- Hughson, M.D.; McCarty, G.A.; Sholer, C.M.; Brumback, R.A. Thrombotic cerebral arteriopathy in patients with the antiphospholipid syndrome. Mod Pathol. 1993, 6, 644–653. [Google Scholar] [PubMed]
- Whitlock, R.P.; Sun, J.C.; Fremes, S.E.; Rubens, F.D.; Teoh, K.H. Antithrombotic and thrombolytic therapy for valvular disease: Antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Prcatice Guidelines. Chest. 2012, 141 (Suppl. 2), e576S–e600S. [Google Scholar] [CrossRef] [PubMed]
- Rabinstein, A.A.; Giovanelli, C.; Romano, J.G.; Koch, S.; Forteza, A.M.; Ricci, M. Surgical treatment of non bacterial thrombotic endocarditis presenting with stroke. J Neurol. 2005, 252, 352. [Google Scholar] [CrossRef] [PubMed]
© 2018 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.