Abstract
Background: Women who experience intimate partner violence (IPV) have a higher likelihood of experiencing detrimental physical, psychological and sexual and reproductive health (SRH) outcomes. However, a gap remains in published literature on SRH interventions available to women experiencing IPV. Methods: A scoping review was undertaken to examine: What is the nature of sexual and reproductive healthcare interventions provided to women experiencing IPV? Five databases (APA PsycInfo, CINAHL Complete, Informit, PubMed and Scopus) were searched on 9 October 2023 for peer-reviewed systematic reviews or primary research published from 1 January 2004–present. The search was repeated on 11 June 2025 to ensure recency of studies. Two researchers independently screened studies at title and abstract, and full-text levels. The two searches yielded a total of 10,844 studies, of which nine were included in the review. Results: Due to the heterogenous nature of the studies, thematic analysis was undertaken with four themes being identified: Outcomes of interventions; Positive impact of personalised and patient-centred care; Professionals’ knowledge, education and training as a facilitator; and Barriers to effective IPV intervention implementation in healthcare. SRH interventions available to women who experienced IPV can empower survivors, improve access to care, and enhance service quality. Conclusions: Evidence-based models of care that are intersectional, trauma-informed and integrated into SRH and IPV services are critical to ensure future work supports women of differing backgrounds who have experienced IPV. Future research should include evaluating effectiveness of interventions, identifying and addressing systemic barriers, and supporting underrepresented groups.
1. Background/Introduction
Violence against women is a global healthcare issue resulting in preventable morbidity and mortality [1]. It is well understood that women who experience violence, particularly from an intimate partner, are more likely to experience detrimental physical and psychological health outcomes. In addition to unintended pregnancies and poor mental health, these women are at increased risk of experiencing sexually transmitted infections (STIs), endometriosis, infertility, and miscarriage [1,2]. Despite this evidence, there is paucity of literature focused on the nature of sexual and reproductive health (SRH) interventions provided to women who are exposed to intimate partner violence (IPV).
Although women experiencing IPV have a pronounced need for healthcare, the existing literature indicates that healthcare for exposed women is fragmented, with barriers to access common [3,4]. There is also evidence to suggest that some women choose not to disclose their abuse, with perceived stigma leading women to fear judgement from healthcare providers, which may in turn delay or prevent women from seeking healthcare [3,5,6,7,8]. Additionally, women may be more likely to report past IPV experiences to their healthcare providers when compared to recent or current abuse [9], which impedes the provision of appropriate and timely healthcare interventions. These challenges can result in the misdiagnosis and/or mistreatment of health issues associated with IPV, including associated sexual and reproductive issues [10,11].
Challenges may also present due to the current disconnect between psychosocial and primary care providers for women experiencing IPV. The healthcare needs of women experiencing IPV are often categorised as either psychological (e.g., counselling or social support services) or physical (e.g., emergency department care for physical injuries/ailments), with limited overlap between the two [12,13]. This limited cross-talk between primary care providers and social support services prevents the transfer of relevant health information from one provider to another [4,14], and thus, may hinder appropriate treatment. Moreover, primary care providers that respond to the acute physical health needs of women experiencing violence or abuse (e.g., nurses), often have low awareness of IPV as a health issue and may be unfamiliar with appropriate referral pathways and services [15], especially for the most marginalised and vulnerable survivor populations [16].
Compounding to these barriers, sexual and reproductive healthcare can also be neglected or poorly implemented because discussion surrounding sexual activity concerns can be misunderstood or make health professionals feel uncomfortable, particularly in the absence of appropriate knowledge and/or training [17,18]. It is also worth acknowledging the often stressful and high-stakes nature of working within a healthcare setting, where providers may be time poor, working within an overburdened healthcare system, and have multiple patients simultaneously requiring care. Health worker burnout and compassion fatigue are well documented phenomena (e.g., [19,20,21]) and may manifest as a reduced level of patient care or prioritisation of only the most acute or obvious health concerns. Thus, an additional challenge for women experiencing sexual and/or reproductive ill health due to IPV may be a de-prioritisation of these health concerns by health professionals outside of a family planning environment [22]. Given these barriers, reproductive healthcare providers are uniquely placed to recognise and assist women of differing backgrounds experiencing IPV [23]. To identify current gaps in the treatment options, this scoping review was undertaken to understand the nature of sexual and reproductive healthcare interventions available to women exposed to IPV.
2. Materials and Methods
The scoping review was guided by the five-step systematic framework developed by Arksey and O’Malley [24], including the extension developed by Levac et al. [25]. This approach was selected due to the exploratory nature of the research question, the anticipated heterogeneity of study designs and outcomes, and the need to map the breadth of existing evidence rather than assess intervention effectiveness. A scoping review methodology is well-suited to identifying key concepts, types of evidence, and gaps in the literature, thereby aligning with the objective of comprehensively describing SRH interventions for women experiencing IPV.
Within this context, the framework outlines five key steps for conducting a scoping review: (1) Developing the review question; (2) Finding studies; (3) Study selection; (4) Data synthesis; and (5) Data collation, summary and reporting. A search was undertaken on the PROSPERO website to assess whether any existing protocols or reviews had been published on this topic, with no results found. The protocol was not registered or published. The review is reported using the Preferred Reporting Items for Systematic reviews with extension for Scoping Reviews (PRISMA-ScR) checklist [26] (Supplementary Material S1).
2.1. Review Question
The question guiding this scoping review was what is the nature of sexual and reproductive healthcare interventions provided to women experiencing IPV?
2.2. Search Strategy
A search strategy was developed with guidance from an experienced University healthcare librarian. A broad range of databases were selected to ensure breadth and depth of previously published literature, including APA PsycInfo, CINAHL, Informit, PubMed and Scopus. The search was undertaken on 9 October 2023 and updated on 11 June 2025. Search terms, and eligibility criteria were developed from the review question’s concepts. The search terms, inclusion and exclusion criteria and full search strategy for each database are included in Supplementary Material S2.
2.3. Eligibility Criteria
Articles were included if they were peer-reviewed systematic reviews or primary research. The date range of 1 January 2004 onwards was selected due to publication of the first international reproductive health strategy, inclusive of sexual health, and the recognition of the impact of IPV on women’s SRH in this year [27]. Inclusion criteria encompassed interventions focused on sexual and/or reproductive healthcare for women who had experienced IPV. For studies that were focused on violence against women, findings specific to IPV were extracted, including studies within reviews. Woman was defined as cisgender, as identified in each individual study. Studies had to be published in English due to lack of sufficient funding for translation services. Lastly, grey literature was excluded to preserve methodological rigor, and to ensure greater reliability and transparency, particularly in the context of sensitive health interventions.
2.4. Screening Procedure
Studies identified through database searches were imported into EndNote. Duplicates were removed and studies were then imported into Covidence. Two members of the research team individually assessed each study at the title and abstract, and full-text levels for eligibility. Screening was completed by four research team members (LE, DT, LR, RJ). The research team met before and during each screening stage and any disagreements were resolved using a fifth researcher (MH).
2.5. Quality Assessment
Quality appraisal for quantitative and qualitative studies was completed using the Mixed Methods Appraisal Tool (MMAT) [28], and the Joanna Briggs Institute (JBI) Checklist for Systematic Reviews and Research Syntheses was used for the literature and systematic reviews [29]. Overall, the methodological quality of included studies was mixed. Most met core criteria related to research clarity and appropriate data collection, though several had unclear reporting on appraisal processes and potential bias. These variations should be considered when interpreting the findings (Supplementary Material S3). In accordance with scoping review methodology, variations in quality were noted; however, they did not determine inclusion or interpretation. As such, no studies were excluded based on quality [24,25].
2.6. Data Charting and Analysis
Data extraction was completed in Covidence using a data extraction form developed by the research team. The items within the form were iteratively developed to include study characteristics (including the aim, design, participant inclusion and exclusion criteria and total number of participants), participant demographics, type of violence and identification strategy and details about the intervention (including the intervention type, location and referral) and main findings. Two research team members individually performed data extraction for each study (total of three research team members completed data extraction: LE, DT, RJ).
Analysis and synthesis of the study findings included descriptive synthesis due to the limited availability and heterogeneity of quantitative data that precluded the use of meta-analysis, which was also outside of the scope of this review [30]. As such, thematic analysis was undertaken within the context of the review question and any implications for future research, policy and/or practice [31,32,33]. Thematic analysis was undertaken independently by two researchers (LE and DT) allowing for generation and defining of themes. A revised six-step guide was flexibly applied to capture the “uniting idea” for each theme [32].
2.7. Ethics Approval
This review synthesises data from previously published studies, therefore no ethical approval was required.
3. Results
The five database searches on 9 October 2023 resulted in a total of 7947 records. Following screening, 146 records met eligibility for review at full-text level, of which 138 were excluded. The most common reasons for exclusion included, a lack of an intervention, insufficient detail about the intervention, interventions not focused on sexual and reproductive healthcare, studies not exclusively focused on women, incorrect population cohort, non-peer-reviewed sources, or protocol papers (Figure 1). Eight remaining records were included in the review. The repeated search on 11 June 2025 identified one additional paper to be included. A total of nine papers were included in the final analyses. See Figure 1 for studies included and excluded with rationale at each stage.
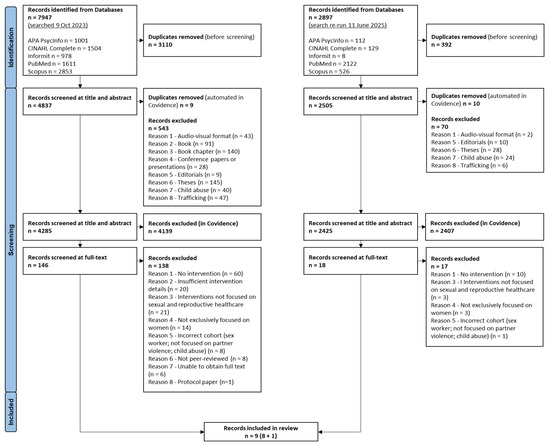
Figure 1.
PRISMA diagram.
3.1. Study Characteristics
Three studies provided comparative analyses of interventions using randomised or cluster controls [34,35,36], three were systematic reviews [37,38,39], two were qualitative studies [40,41] and one study utilised a mixed-method approach [42]. Most studies originated from the United States of America (USA) (n = 6), followed by India (n = 1), Kenya (n = 1), and one focusing on multiple countries. Publication dates ranged from 2011 and 2024. Participant numbers ranged from 72 [41] to 12,078 [37]. An overview of study characteristics including aim, design, study inclusion and exclusion criteria, main findings and number of participants is detailed in Table 1.

Table 1.
Study characteristics.
The focus of the studies included implementing interventions into differing services, outcomes of interventions and possible barriers/facilitators of these interventions [34,35,36,40,41,42], and synthesis of evidence to explore interventions and outcomes in reproductive and sexual health to address violence against women [37,38,39]. When reported, the sociodemographic information varied greatly between studies. Detailed sociodemographic, relationship and intervention information are provided in Table 2, including study intervention details.

Table 2.
Study intervention details.
3.2. Identified Themes
Four themes were identified within the literature (Figure 2). The first theme was Outcomes of interventions which discusses survivors being able to access peer support and gain a feeling of empowerment and control, and the ability for healthcare workers to provide individualised care. The second theme, Positive impact of personalised and patient-centred care details the results of these interventions, bringing about positive change and feelings of safety, respect, and being heard, thus being able to start the healing process. Professionals’ knowledge, education and training as a facilitator was the third theme. This theme included the impact of education and training of healthcare professionals being able to implement interventions and supports, with increased knowledge and understanding enabling greater intervention implementation. The final theme, Barriers to effective IPV intervention implementation in healthcare, discussed barriers to intervention implementation with influencing factors from consumers, healthcare providers and organisational perspectives. Each of these themes are detailed separately.
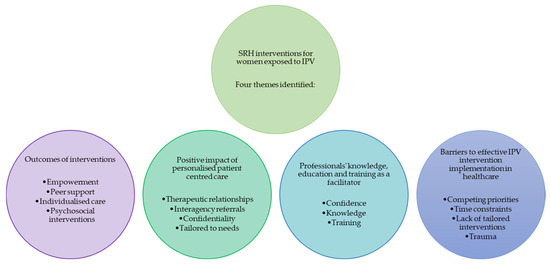
Figure 2.
Diagram of identified themes.
3.3. Outcomes of Interventions
The studies provided comprehensive insights regarding the various interventions aimed at supporting survivors of IPV, where there is a particular focus on empowerment, peer support, individualised care, and focused psychosocial interventions [39,40,42]. These approaches to care have shown significant outcomes in enhancing the wellbeing and recovery of survivors, such as personal safety, physical health, mental health, and improved quality of life [34,36,38,39,42]. Empowerment was a critical outcome of these interventions, which involved helping survivors regain control over their lives and decisions through skill-building, safety planning, trauma-informed education, and linkage to supportive services tailored to their individual needs. For example, in one study, survivors reported a sense of relief and increased confidence after participating in empowerment-focused interventions. This empowerment was further reinforced by providing information and resources, enabling individuals to make informed decisions about their health and safety [38].
Peer support was identified as another vital feature, with it creating a sense of community and understanding among survivors [35,37]. Participants felt more comfortable and supported when they could share their experiences with others who had similar experiences. Peer support groups also facilitated a sense of belonging and validation, which were essential for emotional recovery. The shared experiences within these groups fostered a supportive environment where survivors could openly discuss their challenges and triumphs [35].
Individualised care and focused psychosocial interventions were also highlighted as significant outcomes. Individualised care involved tailoring interventions to meet the specific needs of each survivor, considering their unique experiences and circumstances [37,38]. This personalised approach ensured that survivors receive the most relevant and effective support. For example, focused psychosocial interventions, such as counselling and therapy, were effective in addressing the psychological impacts of abuse [37,38,39]. The literature indicated that such interventions have been effective in reducing symptoms of trauma, anxiety, and depression among survivors [38]. By providing a safe space for survivors to process their experiences and emotions, these interventions play a crucial role in their overall recovery and wellbeing [38].
3.4. Positive Impact of Personalised and Patient-Centred Care
Several positive impacts of therapeutic relationships with healthcare providers and interagency referrals or connections were present in the context of care for survivors of violence. The empathetic approach of healthcare providers, who displayed sensitivity and supportive demeanour, helped the survivors feel more confident and active in their treatment process [42]. Therapeutic relationships fostered a sense of control and empowerment, which was indicated to be crucial for individuals who had experienced IPV including reproductive coercion (RC) [38].
Another positive impact was the role of interagency referrals and connections in providing comprehensive care [36,37,41]. The literature illustrated how effective collaboration between different agencies, such as healthcare providers, sexual health clinics, and advocacy services, can enhance the support system and care for survivors [40]. For instance, the involvement of Sexual Violence Advocates provided additional layers of support [40]. These interagency connections ensured that survivors received not only medical care but also emotional and legal support, which are essential for holistic care. The ability to refer patients to specialised services and ensure follow-up care significantly improved the overall quality of care and support available to survivors [38].
The literature also highlighted the importance of confidentiality in building trust and encouraging survivors to seek help [42]. Many women expressed concerns about confidentiality, fearing that their experiences might be disclosed without their consent. Reinforcing the confidentiality of the services provided and ensuring that survivors’ identities were protected helped alleviate these fears [36]. This assurance of confidentiality was particularly important for those who were hesitant to seek help due to the stigma associated with attending sexual health clinics. By addressing these concerns, healthcare providers were able to create a safe and supportive environment that encouraged more survivors to come forward and access the services they needed [36,42].
Lastly, the positive impact of personalised and patient-centred care was evident in the women’s feedback. The ability to tailor the care to meet individual needs, such as allowing patients to leave the service at any point or come back for follow-up appointments, was highly valued. This flexibility and responsiveness to the patients’ comfort levels and preferences played a crucial role in their healing process [42]. This specialised care provides longer consultation times and a more in-depth understanding of the survivors’ experiences and was shown to be instrumental in helping women feel respected, safe, and ready to begin their healing journey [42]. Further, approaches within some included studies highlight culturally tailored approaches including specific priority sub-groups (e.g., Black, Hispanic, Spanish-speaking participants; [38], [35] and [34], respectively); and evidence of community-led or community embedded aspects of the intervention (e.g., community engagement [37] community resources [38]).
3.5. Professionals’ Knowledge, Education and Training as a Facilitator
Multiple studies demonstrated that healthcare professionals’ knowledge, education, and/or training in SRH significantly influenced the implementation and effectiveness of IPV interventions [39,41,42]. Specifically, elements such as safety planning, skill building, psychoeducation, and counselling were identified as critical for improving outcomes in diverse populations [39]. These studies also highlighted healthcare professionals’ increased confidence and knowledge through education and training are linked to better adherence and implementation outcomes [34,36,41,42]. For example, the Kenyan study [36] focused on addressing IPV and RC in reproductive counselling among female family planning patients, found that training healthcare providers in contraceptive counselling related to IPV and RC led to higher contraceptive uptake, greater awareness of IPV services, and a reduction in attitudes justifying RC among female participants [36].
Similarly, an IPV and RC trauma-informed assessment and education intervention in family planning clinics found that women who received the intervention felt more confident in their providers’ responses to IPV and perceived care [42]. Of the 37% of women in this study who had experienced lifetime physical or sexual IPV, over half also experienced RC (68%). Providers reported that the intervention helped them direct care, conduct assessments and screenings, and feel more comfortable with sensitive conversations [42].
In addition, another two studies in the USA found that an IPV and RC intervention decreased pregnancy coercion among women who received the intervention and made them more likely to end unhealthy relationships with the healthcare providers reporting greater confidence in discussing IPV and RC due to increased training and knowledge [34,41]. These findings are similar to others [40], who reported training of personnel better equipped staff to discuss reproductive health and harm reduction strategies for and among women in the USA.
In addition, two of the three reviews also highlighted the importance of training, knowledge, and education for healthcare providers in the context of interventions and care provision [37,39]. One systematic review [38] also emphasised the importance of clinician expertise and experience in achieving positive outcomes for IPV interventions. For example, a review of multicomponent interventions addressing safety and health risks among Black women in the USA, found that clinician expertise was crucial for the success of these interventions, although success was not measured [38]. Additionally, healthcare provider knowledge and training were found to influence provider readiness and confidence in delivering care, particularly in low- and middle-income countries [37]. Considering these studies’ contexts with women from low- and middle-income countries around the world, Black female survivors of violence in the USA, and women survivors in India, a significant finding was that none of the three studies explored the role intersectional-informed IPV interventions and care provisions may have on the healthcare providers’ knowledge, education and training as a facilitator.
3.6. Barriers to Effective IPV Intervention Implementation in Healthcare
Included studies identified several barriers related to both healthcare provider and systemic issues that impact the implementation and outcomes of interventions. While education and training of healthcare providers positively influence intervention implementation and outcomes, they can also be identified as a barrier. For example, readiness at both the individual and organisational level, including attitudes towards violence against women among employees, were barriers to intervention implementation and outcomes [37]. In evaluating the feasibility of integrating reproductive health services into IPV and sexual violence programs through healthcare provider training, ref. [40] found that institutional priorities acted as a barrier to the implementation of health services within IPV/sexual violence programs. Another study identified lack of time, and uncertainty among health professionals regarding an appropriate time to raise issues of IPV [41].
One significant barrier highlighted within healthcare provider education and training were the lack of tailored interventions addressing specific needs. A tailored reproductive empowerment contraception counselling intervention significantly increased contraceptive use and awareness of IPV services among patients in Kenya [36]. This finding highlights the importance of specialised training for healthcare providers to improve outcomes. Without such personally [36] and culturally [34,35] tailored interventions, healthcare providers may lack the necessary knowledge and skills to effectively support patients, leading to suboptimal care.
Time constraints and conflicting priorities were also demonstrated to pose significant barriers to effective healthcare provider training and education [41]. Literature highlighted the impact of trauma on both women and providers [38,41]. For women, past trauma can make it difficult to engage with healthcare services, especially if they fear re-traumatisation or judgment. The fear of recalling traumatic events, shame, and fear of welfare can deter women from seeking help or fully disclosing their experiences [41]. For healthcare providers, dealing with trauma cases was highlighted as emotionally taxing, leading to burnout and compassion fatigue [38,41]. This emotional burden can affect healthcare providers’ ability to provide empathetic and effective care.
4. Discussion
Due to the continued vast unmet and unaddressed healthcare needs for women who have experienced IPV, particularly in relation to SRH care, this scoping review sought to explore and synthesise the SRH interventions provided to women exposed to IPV on an international scale. Findings from this review highlight a variety of facilitators and barriers to effective IPV intervention implementation in healthcare. This included interventions enabling survivors to access peer support and gain feelings of control and empowerment, and healthcare professionals having greater capacity to provide individualised care [35,37,38,39,40,42]. The findings also identified the positive impact the IPV interventions had on the survivors, bringing about positive change where being heard, feeling safe and respected allowed for the healing process to commence [36,42].
Identified interventions regarding SRH included a range of approaches targeting both healthcare providers and women who have experienced IPV. The main foci were training or education for healthcare providers (e.g., IPV, RC), and education or specialised clinics/supports (e.g., SRH, IPV) for women receiving care [34,36,39,40,41,42]. Additionally, a meaningful subset of studies (more than half) included multiple components of these interventions [34,37,38,39,42]. Further, the current studies identified a variety of interventions provided to women who have experienced IPV, including support groups/clinics focused on IPV and/or reproductive health, education for healthcare providers and women, and interventions targeting priority sub-groups (e.g., Hispanic women or Black women) [35,37,38]. The interventions did not focus on routine screening and assessment for IPV, but focused on training, education, and specialised support. Significantly, the relevant knowledge, education and training-focused studies [37,38,39] overlooked the importance of considering intersectionality and intersectional-informed IPV interventions and care provision on the healthcare providers’ knowledge, education and training; central to women survivors of violence part of multiply marginalised and vulnerable communities [16,48].
Consistent with previous research, interventions that were provided in varied modalities also demonstrated how IPV and SRH can be integrated within existing models of care. This enabled greater feasibility, cost-effectiveness, more seamless access by service users, and protection of privacy/confidentiality for women under the guise of accessing ‘usual’ healthcare [49,50], including within more discrete primary care settings [51]. Further, findings suggest that attempts at integration of IPV with SRH services, and vice versa, can serve as a viable means for providing more coordinated approaches to prevention, screening and specialised supports. Such endeavours offer a more holistic approach to ensuring continuity of care for issues that highly inter-relate (i.e., IPV and SRH). This contrasts with what has historically occurred when supporting women presenting with either of these concerns in isolation. The integration of IPV and SRH services serves to counteract traditional health vs. welfare sector silos [40].
Given the broad and exploratory nature of this scoping review, and without specific a priori research questions, consistent with scoping review approaches, the findings are synthesised in relation to the emergent themes. These themes relate to SRH interventions provided to women who have experienced IPV surrounding barriers, facilitators, outcomes of interventions and positive impacts of interventions reported by survivors, which were identified through this review. Consistent with this approach, previous research has demonstrated the value in exploring barriers and facilitators as an early phase in growing an empirical literature base and to guide future rigour in intervention delivery and evaluation (see [52]).
4.1. Outcomes of Interventions
Empirical evidence highlights the positive impact of interventions seeking to improve the social support and mental health of women survivors who are exposed to IPV, such as reduction in experience of IPV or reduction in partner aggression [53]. The identified studies demonstrated how sexual and reproductive healthcare interventions, which focus on empowerment, helped women survivors of IPV to increase their level of confidence. It enabled them to make informed decisions about their safety and health through the provision of information and resources for example [38]. Other research [54], also found improved mental health outcomes in the women survivors of IPV engaging in interventions focusing on empowerment.
Closely aligned, the studies in this review also stressed how psychosocial interventions such as therapy and counselling addressed the psychological and mental health effects of IPV. This included reducing signs of anxiety, depression and trauma among women survivors, including overall recovery and wellbeing [37,38]. As highlighted within the literature ([55,56]), counselling plays a vital role in the recovery of women exposed to and surviving IPV; however, perpetrators are equally in need of counselling to effectively break cycles of IPV within and across generations [55].
When peer-support was part of the intervention, women IPV survivors expressed feeling more comfortable and supported in sharing their experiences, in turn creating a supportive environment [35]. As outlined elsewhere, peer-support plays a vital role in the context of IPV service provision and is conceptualised as a holistic alternative to ‘traditional’ forms of IPV interventions such as personal growth, including that of the peer-support worker [57]. However, the peer-support model has also been presented with challenges, such as lack of role clarity for peer-support workers, and scepticism towards peer-support workers from credentialed professionals [58].
Parallel to this, the identified articles within this scoping review stressed the importance for IPV interventions to be tailored to the unique needs, experiences and circumstances of the women survivors to ensure relevance and efficacy, including socio-economic status, ethnicity, and cultural and linguistic backgrounds [37,38]. The aspect of tailoring IPV interventions to the needs of the survivors, and intersectionality-informed, have been explored elsewhere linked to housing and homeless [59], social contexts and cultural needs of the women survivors [60,61], and included being sensitive and affirming to the survivor’s sexual orientation [62,63].
4.2. Positive Impact of Personalised and Patient-Centred Care
Consistent with previous published literature, findings from this review highlight the importance and value that women place on service providers taking humanistic [64], trauma-informed [65], and client-centred [66] approaches when supporting them. These factors are even more important when working with women who are experiencing heightened levels of and multiple forms of vulnerability, including intersectionality, risk and stigma and help to strengthen rapport and facilitate health service engagement, particularly in highly sensitive and stigmatised topics of IPV and SRH [67,68].
Echoing the findings of the current study, the importance of inter-agency collaboration, cross-referral and advocacy are critical ingredients to effectively engage with and support women who have experienced IPV with SRH options and decision making. The following recommendations have been suggested to enhance the feasibility and benefits of such IPV/SRH collaborations, and include formal partnership agreements, cross-training opportunities for staff, and standardised referral protocols [40]. Further recommendations include policy change to sustain such partnerships, which can be enabled through staff training and greater funding [69].
One additional and paramount consideration illuminated in this study, which enabled trust and help seeking for women who have experienced IPV, was the vital role of felt and actual privacy/confidentiality. This is consistent with literature purporting confidentiality as essential for engagement and intervention to be possible [70], particularly due to the psychological effects of IPV and coercive control and the safety concerns for victim-survivors [71,72].
4.3. Facilitators
Findings from the current study lend support for the value and benefit of education and training to enhance healthcare providers’ knowledge and confidence, particularly in topics of heightened sensitivity, stigma and risk (e.g., IPV, SRH) taking an intersectional trauma-informed approach [16]. This enhanced knowledge and confidence by healthcare providers has been demonstrated to lead to more effective implementation of IPV and SRH interventions and potentially better client outcomes (see Zachor et al., 2018 [73]). However, results in a 2021 systematic review demonstrate some inconsistent findings, in part, due to the heterogeneity of studies [74]. Consistent with previous research, there are distinct benefits of ensuring an IPV workforce is better equipped to provide education and referral options for SRH, and in turn for clinicians in SRH to better screen for IPV and provide appropriate referrals for specialised IPV support and advocacy services [73]. A recent integrative literature review [75] has also recommended the need for dedicated funding for responding to IPV training and emphasised the importance of continuing professional development. Future healthcare professional training in the combined SRH and IPV space would also benefit from interdisciplinary approaches tailored to cultural and linguistic needs when supporting members of key priority groups (see [76]), in tandem with community-led approaches [77,78], to maximise potential uptake, relevancy and impact.
4.4. Barriers
Healthcare providers often exhibit hesitancy in screening for IPV due to a variety of factors. Despite receiving training, some midwives, nurses, and other healthcare professionals remain reluctant to consistently implement routine inquiries embedded within IPV interventions [79]. This hesitancy can stem from personal discomfort, fear of offending patients, or uncertainty about how to handle disclosures of IPV effectively.
Another significant barrier to the effective implementation of IPV interventions was time constraints. Healthcare providers often struggle to find the appropriate time to raise issues of IPV during consultations, especially when there are multiple presenting concerns that need to be addressed. The need to prioritise other urgent health issues can lead to the de-prioritisation of IPV-related matters. Literature has highlighted [41] that lack of time and the challenge of integrating IPV screening into already busy schedules are common hindrances. This indicates a systemic issue within healthcare settings where the structure and demands of clinical practice do not align well with the needs of IPV screening and intervention. Innovative solutions, such as integrating IPV screening into routine health assessments or using digital tools to streamline the process, could be explored to mitigate these time constraints [80]. At the institutional level, several barriers can impede the effective implementation of IPV interventions. For example, research found [40] that institutional priorities often hindered the integration of reproductive health services into IPV programs. As such, these insights highlight the importance of institutional commitment and the need for standardised, evidence-based protocols to ensure consistent and effective care.
Trauma and burnout also play a critical role in hindering effective intervention implementation. Both women experiencing IPV and healthcare providers can be affected by trauma, which poses additional barriers to effective intervention implementation. Past trauma can make it difficult for women to engage with healthcare services, especially if they fear re-traumatisation or judgment [41]. The fear of recalling traumatic events, feelings of shame, and concerns about welfare can deter women from seeking help or fully disclosing their experiences [41]. Healthcare providers dealing with trauma cases can experience emotional exhaustion, leading to burnout and compassion fatigue [81]. This emotional burden can affect their ability to provide empathetic and effective care. Literature has highlighted ([38,41]) dealing with trauma cases is emotionally taxing for providers, which can impact their performance and wellbeing. Addressing these issues requires a dual approach, which encompasses providing trauma-informed care and support for patients and ensuring that healthcare providers have access to resources and support to manage their own emotional wellbeing. As such, training in trauma-informed care, regular debriefing sessions, and access to mental health resources for providers remains essential.
4.5. Strengths
This review spanned multiple countries and distilled evidence on what works for women and the mechanisms through which positive benefit can be achieved. These mechanisms provide evidence on how healthcare providers can address service fragmentation and disconnect in a way that minimises stigma and empower women of differing vulnerable backgrounds who experience invisibility or marginalisation within healthcare systems [16]. The findings offer significant potential for replicating effective strategies to improve outcomes and close health service gaps. The findings could guide the development of SRH and IPV best practice guidelines for sexual health and other health services. Such guidelines could support the development of “no wrong door” approaches that would identify and support affected individuals, regardless of their point of access. Sexual health “first aid” training could be provided across sectors to raise awareness of this important issue among IPV survivors and aid in earlier identification and linking in of women for support, and ensuring services are accessible for women.
4.6. Limitations and Future Research Directions
There are several limitations to the current scoping review. Firstly, while peer-review ensured rigour, the focus on peer-reviewed and English only potentially narrowed the scope of the findings [82] and limits geographical diversity and generalisability. This restriction of language may have excluded relevant interventions published in other languages, thereby impacting the comprehensiveness and global applicability of the findings. This concentration of research based in the USA may reflect strong funding and established SRH-IPV integration models within that context; however, it raises concerns about transferability to other cultural and healthcare contexts. Also, the varied methodological approaches and lack of heterogeneity and specificity across studies prevented statistical comparisons. The poor specificity of detail in many of the articles, such as lack of detail on who committed the sexual or domestic violence and the relationship(s) to the women means it is possible that studies on violence that were excluded may have also included IPV but were excluded from the review due to minimal reporting. Thirdly, we considered women as a holistic group, and did not specifically distinguish sub-groups. Future research and reviews should explicitly include or report on trans women to ensure their experiences are represented. Similarly, cultural, linguistic, ethnic, and spiritual diversity was not always reported in the studies, meaning it was not possible to explicitly foreground these important contextual factors in SRH interventions for IPV survivors, nor the extent to which interventions were community-led and appropriately culturally tailored. Finally, this review primarily examined SRH interventions for women experiencing IPV but did not consider the nature of their relationship configurations—such as heterosexual, same-sex, polyamorous, or other forms. These limit understandings of how relationship dynamics may influence access to and experiences with care, and collectively highlight key areas for future research, staff training and health promotion efforts.
5. Conclusions
There are a variety of SRH interventions available to women who are exposed to IPV, highlighting their potential to empower survivors, improve access to care, and enhance service quality. Interventions that were intersectional, trauma-informed and client-centred were especially effective in fostering trust and engagement. However, gaps remain, including limited representation of diverse populations, relationship types, and community-led initiatives. More research is needed to guide evidence-based SRH care for women affected by IPV. Future research should focus on evaluating intervention effectiveness, addressing systemic barriers such as provider burnout and institutional constraints, and exploring underrepresented groups and grassroots efforts. Collaborative partnerships and sustainable funding are essential to support these initiatives. Developing holistic, evidence-based models of care that integrate SRH and IPV services is a critical next step. Broader societal change is also needed to challenge gendered power dynamics and improve women’s agency in accessing care. Together, these efforts can build a more inclusive and responsive healthcare system for all women affected by IPV.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph22091377/s1, Supplementary Material S1 PRISMA-ScR Checklist, Supplementary Material S2 Search terms, inclusion and exclusion criteria and database searches, Supplementary Material S3 Included studies’ quality appraisal.
Author Contributions
Conceptualization, L.E.; methodology, L.E.; validation, L.E., D.T., L.R. and R.M.J.; formal analysis, L.E., D.T., L.R. and R.M.J.; investigation, L.E., D.T., L.R. and R.M.J.; writing—original draft preparation, L.E., D.T., L.R., B.L., A.B.M., A.B. and R.M.J.; writing—review and editing, L.E., D.T., L.R., B.L., A.B.M., A.B., M.H. and R.M.J.; supervision, L.E.; funding acquisition, L.E. All authors have read and agreed to the published version of the manuscript.
Funding
Funding from the University of Southern Queensland’s Centre for Health Research supported this work.
Data Availability Statement
The original contributions presented in this study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- World Health Organisation. Violence Against Women Prevalence Estimates 2018: Global, Regional and National Prevalence Estimates for Intimate Partner Violence Against Women and Global and Regional Prevalence Estimates for Non-Partner Sexual Violence Against Women; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- East, L.; Terry, D.; Viljoen, B.; Hutchinson, M. Intimate partner violence and sexual and reproductive health outcomes of women: An Australian population cohort study. Sex. Reprod. Healthc. 2025, 44, 101100. [Google Scholar] [CrossRef]
- Papas, L.; Hollingdrake, O.; Currie, J. Social determinant factors and access to health care for women experiencing domestic and family violence: Qualitative synthesis. J. Adv. Nurs. 2023, 79, 1633–1649. [Google Scholar] [CrossRef]
- Wilson, K.S.; Silberberg, M.R.; Brown, A.J.; Yaggy, S.D. Health needs and barriers to healthcare of women who have experienced intimate partner violence. J. Women’s Health 2007, 16, 1485–1498. [Google Scholar] [CrossRef]
- Dichter, M.E.; Makaroun, L.; Tuepker, A.; True, G.; Montgomery, A.E.; Iverson, K. Middle-aged women’s experiences of intimate partner violence screening and disclosure: “It’s a private matter. It’s an embarrassing situation”. J. Gen. Intern. Med. 2020, 35, 2655–2661. [Google Scholar] [CrossRef] [PubMed]
- Mackenzie, M.; Gannon, M.; Stanley, N.; Cosgrove, K.; Feder, G. ‘You certainly don’t go back to the doctor once you’ve been told, “I’ll never understand women like you.”’ Seeking candidacy and structural competency in the dynamics of domestic abuse disclosure. Sociol. Health Illn. 2019, 41, 1159–1174. [Google Scholar] [CrossRef] [PubMed]
- Murray, C.E.; Crowe, A.; Overstreet, N.M. Sources and components of stigma experienced by survivors of intimate partner violence. J. Interpers. Violence 2018, 33, 515–536. [Google Scholar] [CrossRef] [PubMed]
- Fanslow, J.L.; Robinson, E.M. Physical injuries resulting from intimate partner violence and disclosure to healthcare providers: Results from a New Zealand population-based study. Inj. Prev. 2011, 17, 37–42. [Google Scholar] [CrossRef]
- Higgins, D.; Manhire, K.; Marshall, B. Prevalence of intimate partner violence disclosed during routine screening in a large general practice. J. Prim. Health Care 2015, 7, 102–108. [Google Scholar] [CrossRef][Green Version]
- Lichtenstein, B. Domestic violence in barriers to health care for HIV-positive women. AIDS Patient Care STDs 2006, 20, 122–132. [Google Scholar] [CrossRef]
- Akyüz, A.; Yavan, T.; Şahiner, G.; Kılıç, A. Domestic violence and woman’s reproductive health: A review of the literature. Aggress. Violent Behav. 2012, 17, 514–518. [Google Scholar] [CrossRef]
- Greene, M.C.; Bencomo, C.; Rees, S.; Ventevogel, P.; Likindikoki, S.; Nemiro, A.; Bonz, A.; Mbwambo, J.K.; Tol, W.A.; McGovern, T.M. Multilevel determinants of integrated service delivery for intimate partner violence and mental health in humanitarian settings. Int. J. Environ. Res. Public Health 2021, 18, 12484. [Google Scholar] [CrossRef]
- Tower, M.; Mcmurray, A.; Rowe, J.; Wallis, M. Domestic violence, health and health care: Women’s accounts of their experiences. Contemp. Nurse 2006, 21, 186–198. [Google Scholar] [CrossRef]
- Keeling, J.; Fisher, C. Health professionals’ responses to women’s disclosure of domestic violence. J. Interpers. Violence 2015, 30, 2363–2378. [Google Scholar] [CrossRef] [PubMed]
- Hollingdrake, O.; Saadi, N.; Alban Cruz, A.; Currie, J. Qualitative study of the perspectives of women with lived experience of domestic and family violence on accessing healthcare. J. Adv. Nurs. 2023, 79, 1353–1366. [Google Scholar] [CrossRef] [PubMed]
- Kulkarni, S. Intersectional Trauma-Informed Intimate Partner Violence (IPV) Services: Narrowing the Gap between IPV Service Delivery and Survivor Needs. J. Fam. Violence 2019, 34, 55–64. [Google Scholar] [CrossRef]
- East, L.; Hutchinson, M. Sexual violence matters: Nurses must respond. J. Adv. Nurs. 2023, 79, e10–e11. [Google Scholar] [CrossRef]
- Davidson, N.; Hammarberg, K.; Romero, L.; Fisher, J. Access to preventive sexual and reproductive health care for women from refugee-like backgrounds: A systematic review. BMC Public Health 2022, 22, 403. [Google Scholar] [CrossRef]
- Nolte, A.G.; Downing, C.; Temane, A.; Hastings-Tolsma, M. Compassion fatigue in nurses: A metasynthesis. J. Clin. Nurs. 2017, 26, 4364–4378. [Google Scholar] [CrossRef]
- Woo, T.; Ho, R.; Tang, A.; Tam, W. Global prevalence of burnout symptoms among nurses: A systematic review and meta-analysis. J. Psychiatr. Res. 2020, 123, 9–20. [Google Scholar] [CrossRef]
- Xie, W.; Chen, L.; Feng, F.; Okoli, C.T.; Tang, P.; Zeng, L.; Jin, M.; Zhang, Y.; Wang, J. The prevalence of com-passion satisfaction and compassion fatigue among nurses: A systematic review and meta-analysis. Int. J. Nurs. Stud. 2021, 120, 103973. [Google Scholar] [CrossRef]
- Hudspeth, N.; Cameron, J.; Baloch, S.; Tarzia, L.; Hegarty, K. Health practitioners’ perceptions of structural barriers to the identification of intimate partner abuse: A qualitative meta-synthesis. BMC Health Serv. Res. 2022, 22, 96. [Google Scholar] [CrossRef]
- Fanslow, J. Intimate partner violence and women’s reproductive health. Obstet. Gynaecol. Reprod. Med. 2017, 27, 148–157. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping studies: Advancing the methodology. Implement. Sci. 2010, 5, 69. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Annu. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- World Health Organisation. Reproductive Health Strategy: To Accelerate Progress Towards the Attainment of International Development Goals and Targets; World Health Organization: Geneva, Switzerland, 2004. [Google Scholar]
- Hong, Q.N.; Fàbregues, S.; Bartlett, G.; Boardman, F.; Cargo, M.; Dagenais, P.; Gagnon, M.P.; Griffiths, F.; Nicolau, B.; O’Cathain, A.; et al. Mixed Methods Appraisal Tool (MMAT). Educ. Inf. 2018, 34, 285–291. [Google Scholar] [CrossRef]
- Joanna Briggs Institute. Checklist for Systematic Reviews and Research Syntheses; Joanna Briggs Institute: Adelaide, Australia, 2017. [Google Scholar]
- Cook, D.A. Systematic and Nonsystematic Reviews: Choosing an Approach. In Healthcare Simulation Research: A Practical Guide; Nestel, D., Hui, J., Kunkler, K., Scerbo, M.W., Calhoun, A.W., Eds.; Springer International Publishing: Cham, Switzerland, 2019; pp. 55–60. [Google Scholar]
- Braun, V.; Clarke, V. Thematic Analysis. In APA Handbook of Research Methods in Psychology; Cooper, H., Ed.; APA Books: Washington, DC, USA, 2012; pp. 57–71. [Google Scholar]
- Braun, V.; Clarke, V. Reflecting on reflexive thematic analysis. Qual. Res. Sport Exerc. Health 2019, 11, 589–597. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Successful Qualitative Research: A Practical Guide for Beginners; Sage: London, UK, 2013. [Google Scholar]
- Miller, E.; Decker, M.R.; McCauley, H.L.; Tancredi, D.J.; Levenson, R.R.; Waldman, J.; Schoenwald, P.; Silverman, J.G. A family planning clinic partner violence intervention to reduce risk associated with reproductive coercion. Contraception 2011, 83, 274–280. [Google Scholar] [CrossRef]
- Mitrani, V.B.; McCabe, B.E.; Gonzalez-Guarda, R.M.; Florom-Smith, A.; Peragallo, N. Participation in SEPA, a sexual and relational health intervention for Hispanic women. West. J. Nurs. Res. 2013, 35, 849–866. [Google Scholar] [CrossRef]
- Uysal, J.; Boyce, S.C.; Undie, C.C.; Liambila, W.; Wendoh, S.; Pearson, E.; Johns, N.E.; Silverman, J.G. Effects of a clinic-based reproductive empowerment intervention on proximal outcomes of contraceptive use, self-efficacy, attitudes, and awareness and use of survivor services: A cluster-controlled trial in Nairobi, Kenya. Sex. Reprod. Health Matters 2023, 31, 2227371. [Google Scholar] [CrossRef]
- Lewis, N.V.; Munas, M.; Colombini, M.; d’Oliveira, A.F.; Pereira, S.; Shrestha, S.; Rajapakse, T.; Shaheen, A.; Rishal, P.; Alkaiyat, A.; et al. Interventions in sexual and reproductive health services addressing violence against women in low-income and middle-income countries: A mixed-methods systematic review. BMJ Open 2022, 12, e051924. [Google Scholar] [CrossRef]
- Sabri, B.; Gielen, A. Integrated Multicomponent Interventions for Safety and Health Risks Among Black Female Survivors of Violence: A Systematic Review. Trauma Violence Abus. 2019, 20, 720–731. [Google Scholar] [CrossRef]
- Sabri, B.; Mani, S.S.; Kaduluri, V.P.S. Integrated domestic violence and reproductive health interventions in India: A systematic review. Reprod. Health 2024, 21, 94. [Google Scholar] [CrossRef]
- Gmelin, T.; Raible, C.A.; Dick, R.; Kukke, S.; Miller, E. Integrating Reproductive Health Services Into Intimate Partner and Sexual Violence Victim Service Programs. Violence Against Women 2018, 24, 1557–1569. [Google Scholar] [CrossRef]
- Miller, E.; McCauley, H.L.; Decker, M.R.; Levenson, R.; Zelazny, S.; Jones, K.A.; Anderson, H.; Silverman, J.G. Implementation of a Family Planning Clinic-Based Partner Violence and Reproductive Coercion Intervention: Provider and Patient Perspectives. Perspect. Sex. Reprod. Health 2017, 49, 85–93. [Google Scholar] [CrossRef]
- Decker, M.R.; Flessa, S.; Pillai, R.V.; Dick, R.N.; Quam, J.; Cheng, D.; McDonald-Mosley, R.; Alexander, K.A.; Holliday, C.N.; Miller, E. Implementing Trauma-Informed Partner Violence Assessment in Family Planning Clinics. J. Women’s Health 2017, 26, 957–965. [Google Scholar] [CrossRef] [PubMed]
- Kiely, M.; El-Mohandes, A.A.E.; El-Khorazaty, M.N.; Gantz, M.G. An integrated intervention to reduce intimate partner violence in pregnancy: A randomized controlled trial. Obstet. Gynecol. 2010, 115, 273–283. [Google Scholar] [CrossRef] [PubMed]
- Arora, S.; Deosthali, P.B.; Rege, S. Effectiveness of a counselling intervention implemented in antenatal setting for pregnant women facing domestic violence: A pre-experimental study. BJOG Int. J. Obstet. Gynaecol. 2019, 126, 50–57. [Google Scholar] [CrossRef] [PubMed]
- Nair, S.; Donta, B.; Shahina, B. Intervention to reduce partner violence and enhance contraceptive use among women in a low-income community in Mumbai, India. Indian Soc. Study Reprod. Fertil. Newsl. 2020, 25, 50–56. [Google Scholar]
- Raj, A.; Saggurti, N.; Battala, M.; Nair, S.; Dasgupta, A.; Naik, D.D.; Abramovitz, D.; Silverman, J.G.; Balaiah, D. Randomized controlled trial to test the RHANI Wives HIV intervention for women in India at risk for HIV from husbands. AIDS Behav. 2013, 17, 3066–3080. [Google Scholar] [CrossRef]
- Saggurti, N.; Nair, S.; Silverman, J.G.; Naik, D.D.; Battala, M.; Dasgupta, A.; Balaiah, D.; Raj, A. Impact of the RHANI Wives intervention on marital conflict and sexual coercion. Int. J. Gynaecol. Obstet. 2014, 126, 18–22. [Google Scholar] [CrossRef]
- Williams, K.; Harb, M.; Satyen, L.; Davies, M. s-CAPE trauma recovery program: The need for a holistic, trauma- and violence-informed domestic violence framework. Front. Glob. Women’s Health 2024, 5, 1404599. [Google Scholar] [CrossRef]
- Gold, L.; Norman, R.; Devine, A.; Feder, G.; Taft, A.J.; Hegarty, K.L. Cost-Effectiveness of Health Care Interventions to Address Intimate Partner Violence: What Do We Know and What Else Should We Look for? Violence Against Women 2011, 17, 389–403. [Google Scholar] [CrossRef]
- Nanda, P.; Tandon, S.; Khanna, A. Virtual and essential—Adolescent SRHR in the time of COVID-19. Sex. Reprod. Health Matters 2020, 28, 1831136. [Google Scholar] [CrossRef]
- Thompson, E.L.; Fulda, K.G.; Grace, J.; Galvin, A.M.; Spence, E.E. The Implementation of an Interpersonal Violence Screening Program in Primary Care Settings: Lessons Learned. Health Promot. Pract. 2022, 23, 640–649. [Google Scholar] [CrossRef]
- Abu-Odah, H.; Said, N.B.; Nair, S.C.; Allsop, M.J.; Currow, D.C.; Salah, M.S.; Hamad, B.A.; Elessi, K.; Alkhatib, A.; ElMokhallalati, Y.; et al. Identifying barriers and facilitators of translating research evidence into clinical practice: A systematic review of reviews. Health Soc. Care Community 2022, 30, e3265–e3276. [Google Scholar] [CrossRef] [PubMed]
- Ogbe, E.; Harmon, S.; Van den Bergh, R.; Degomme, O. A systematic review of intimate partner violence interventions focused on improving social support and/mental health outcomes of survivors. PLoS ONE 2020, 15, e0235177. [Google Scholar] [CrossRef]
- Tiwari, A.; Fong, D.Y.T.; Yuen, K.H.; Yuk, H.; Pang, P.; Humphreys, J.; Bullock, L. Effect of an Advocacy Intervention on Mental Health in Chinese Women Survivors of Intimate Partner Violence: A Randomized Controlled Trial. JAMA 2010, 304, 536–543. [Google Scholar] [CrossRef] [PubMed]
- Tutty, L. Chapter Sixteen: Identifying, Assessing, and Counselling Male Intimate Partner Violence Perpetrators and Abused Women. In Cruel but Not Unusual: Violence in Families in Canada; Alaggia, R., Vine, C., Eds.; Wilfrid Laurier University Press: Waterloo, ON, Canada, 2022; pp. 519–552. [Google Scholar]
- O’Doherty, L.; Taket, A.; Valpied, J.; Hegarty, K. Receiving care for intimate partner violence in primary care: Barriers and enablers for women participating in the weave randomised controlled trial. Soc. Sci. Med. 2016, 160, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Osborn, M.; Ball, T.; Rajah, V. Peer Support Work in the Context of Intimate Partner Violence: A Scoping Review. Trauma Violence Abus. 2024, 25, 4261–4276. [Google Scholar] [CrossRef]
- Gregory, A.; Johnson, E.; Feder, G.; Campbell, J.; Konya, J.; Perôt, C. Perceptions of Peer Support for Victim-Survivors of Sexual Violence and Abuse: An Exploratory Study With Key Stakeholders. J. Interpers. Violence 2022, 37, NP14036–NP14065. [Google Scholar] [CrossRef]
- Yakubovich, A.R.; Bartsch, A.; Metheny, N.; Gesink, D.; O’Campo, P. Housing interventions for women experiencing intimate partner violence: A systematic review. Lancet Public Health 2022, 7, e23–e35. [Google Scholar] [CrossRef] [PubMed]
- Goddard-Eckrich, D.; Henry, B.F.; Sardana, S.; Thomas, B.V.; Richer, A.; Hunt, T.; Chang, M.; Johnson, K.; Gilbert, L. Evidence of Help-Seeking Behaviors Among Black Women Under Community Supervision in New York City: A Plea for Culturally Tailored Intimate Partner Violence Interventions. Women’s Health Rep. 2022, 3, 867. [Google Scholar] [CrossRef] [PubMed]
- Lirios, A.; Mullens, A.B.; Daken, K.; Moran, C.; Gu, Z.; Assefa, Y.; Dean, J.A. Sexual and reproductive health literacy of culturally and linguistically diverse young people in Australia: A systematic review. Cult. Health Sex. 2024, 26, 790–807. [Google Scholar] [CrossRef] [PubMed]
- Gray, R.; Walker, T.; Hamer, J.; Broady, T.; Kean, J.; Ling, J.; Bear, B. Developing LGBTQ Programs for Perpetrators and Victims/Survivors of Domestic and Family Violence (Research Report Octeber 2020); Australia’s National Research Organisation for Women’s Safety: Sydney, NSW, Australia, 2020. [Google Scholar]
- Burke, C.; Dunlea, R.R. The Prosecution of Same-Sex Intimate Partner Violence Cases. J. Interpers. Violence 2025. [Google Scholar] [CrossRef]
- Peters, S.M. Demedicalizing the aftermath of sexual assault: Toward a radical humanistic approach. J. Humanist. Psychol. 2021, 61, 939–961. [Google Scholar] [CrossRef]
- Wathen, C.N.; Mantler, T. Trauma- and Violence-Informed Care: Orienting Intimate Partner Violence Interventions to Equity. Curr. Epidemiol. Rep. 2022, 9, 233–244. [Google Scholar] [CrossRef]
- Wyatt, B.J. Growing Forward: Best-Practice(s) in Client-Centred Service(s) for Those Experiencing and Using Intimate Partner Violence; University of Regina: Regina, SK, Canada, 2019. [Google Scholar]
- Bohren, M.A.; Vazquez Corona, M.; Odiase, O.J.; Wilson, A.N.; Sudhinaraset, M.; Diamond-Smith, N.; Berryman, J.; Tunçalp, Ö.; Afulani, P.A. Strategies to reduce stigma and discrimination in sexual and reproductive healthcare settings: A mixed-methods systematic review. PLOS Glob. Public Health 2022, 2, e0000582. [Google Scholar] [CrossRef]
- Murvartian, L.; Matías-García, J.A.; Saavedra-Macías, F.J.; Crowe, A. A Systematic Review of Public Stigmatization Toward Women Victims of Intimate Partner Violence in Low- and Middle-Income Countries. Trauma Violence Abus. 2024, 25, 1349–1364. [Google Scholar] [CrossRef]
- Scott, S.E.; Risser, L.; Miller-Walfish, S.; Marjavi, A.; Ali, A.; Segebrecht, J.; Branch, T.; Dawson, S.; Miller, E. Policy and Systems Change in Intimate Partner Violence and Human Trafficking: Evaluation of a Federal Cross-Sector Initiative. J. Women’s Health 2023, 32, 779–786. [Google Scholar] [CrossRef]
- O’Connor-Terry, C.; Burton, D.; Gowda, T.; Laing, A.; Chang, J.C. Challenges of seeking reproductive health care in people experiencing intimate partner violence. J. Interpers. Violence 2022, 37, NP5167–NP5186. [Google Scholar] [CrossRef]
- Kazmerski, T.; McCauley, H.L.; Jones, K.; Borrero, S.; Silverman, J.G.; Decker, M.R.; Tancredi, D.; Miller, E. Use of reproductive and sexual health services among female family planning clinic clients exposed to partner violence and reproductive coercion. Matern. Child Health J. 2015, 19, 1490–1496. [Google Scholar] [CrossRef]
- Mullens, A.B.; Duyker, J.; Brownlow, C.; Lemoire, J.; Daken, K.; Gow, J. Point-of-care testing (POCT) for HIV/STI targeting MSM in regional Australia at community ‘beat’ locations. BMC Health Serv. Res. 2019, 19, 93. [Google Scholar] [CrossRef]
- Zachor, H.; Chang, J.C.; Zelazny, S.; Jones, K.A.; Miller, E. Training reproductive health providers to talk about intimate partner violence and reproductive coercion: An exploratory study. Health Educ. Res. 2018, 33, 175–185. [Google Scholar] [CrossRef]
- Kalra, N.; Hooker, L.; Reisenhofer, S.; Di Tanna, G.L.; García-Moreno, C. Training healthcare providers to respond to intimate partner violence against women. Cochrane Database Syst. Rev. 2021, 5, CD012423. [Google Scholar] [CrossRef] [PubMed]
- Ambikile, J.S.; Leshabari, S.; Ohnishi, M. Curricular Limitations and Recommendations for Training Health Care Providers to Respond to Intimate Partner Violence: An Integrative Literature Review. Trauma Violence Abus. 2022, 23, 1262–1269. [Google Scholar] [CrossRef] [PubMed]
- Moya, E.M.; Chávez-Baray, S.M.; Martínez, O.; Aguirre-Polanco, A. Exploring intimate partner violence and sexual health needs in the southwestern united states: Perspectives from health and human services workers. Health Soc. Work. 2016, 41, e29–e37. [Google Scholar] [CrossRef]
- Awolaran, O.; OlaOlorun, F.M. A community-based intervention to challenge attitudes towards intimate partner violence: Results from a randomised community trial in rural South-West Nigeria. Rural Remote Health 2025, 25, 9269. [Google Scholar] [CrossRef]
- Tohit, N.F.M.; Rashid, S.A.Z.A.; Fakuradzi, W.F.S.W.A.; Zaidi, N.A.A.; Haque, M. Exploring pathways from community involvement to empowerment in sexual and reproductive health: A public health perspective. Adv. Hum. Biol. 2024, 14, 296–307. [Google Scholar] [CrossRef]
- Ying Ying, C.; Hairi, N.N.; Othman, S. Tools for Assessing Healthcare Providers’ Readiness to Respond to Intimate Partner Violence: A Systematic Review. J. Fam. Violence 2024, 39, 759–782. [Google Scholar] [CrossRef]
- Portnoy, G.A.; Colon, R.; Gross, G.M.; Adams, L.J.; Bastian, L.A.; Iverson, K.M. Patient and provider barriers, facilitators, and implementation preferences of intimate partner violence perpetration screening. BMC Health Serv. Res. 2020, 20, 746. [Google Scholar] [CrossRef]
- Sinclair, S.; Raffin-Bouchal, S.; Venturato, L.; Mijovic-Kondejewski, J.; Smith-MacDonald, L. Compassion fatigue: A meta-narrative review of the healthcare literature. Int. J. Nurs. Stud. 2017, 69, 9–24. [Google Scholar] [CrossRef]
- Munn, Z.; Pollock, D.; Khalil, H.; Alexander, L.; Mclnerney, P.; Godfrey, C.; Peters, M.; Tricco, A. What are scoping reviews? Providing a formal definition of scoping reviews as a type of evidence synthesis. JBI Evid. Synth. 2022, 20, 950–952. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).