Health, Psychological Distress, and Functioning During the COVID-19 Pandemic Among Danish Adults with and Without a Preexisting Mental Illness
Abstract
1. Introduction
2. Methods
2.1. Setting
2.2. Data
2.3. Measures
2.4. Weight
2.5. Statistical Analysis
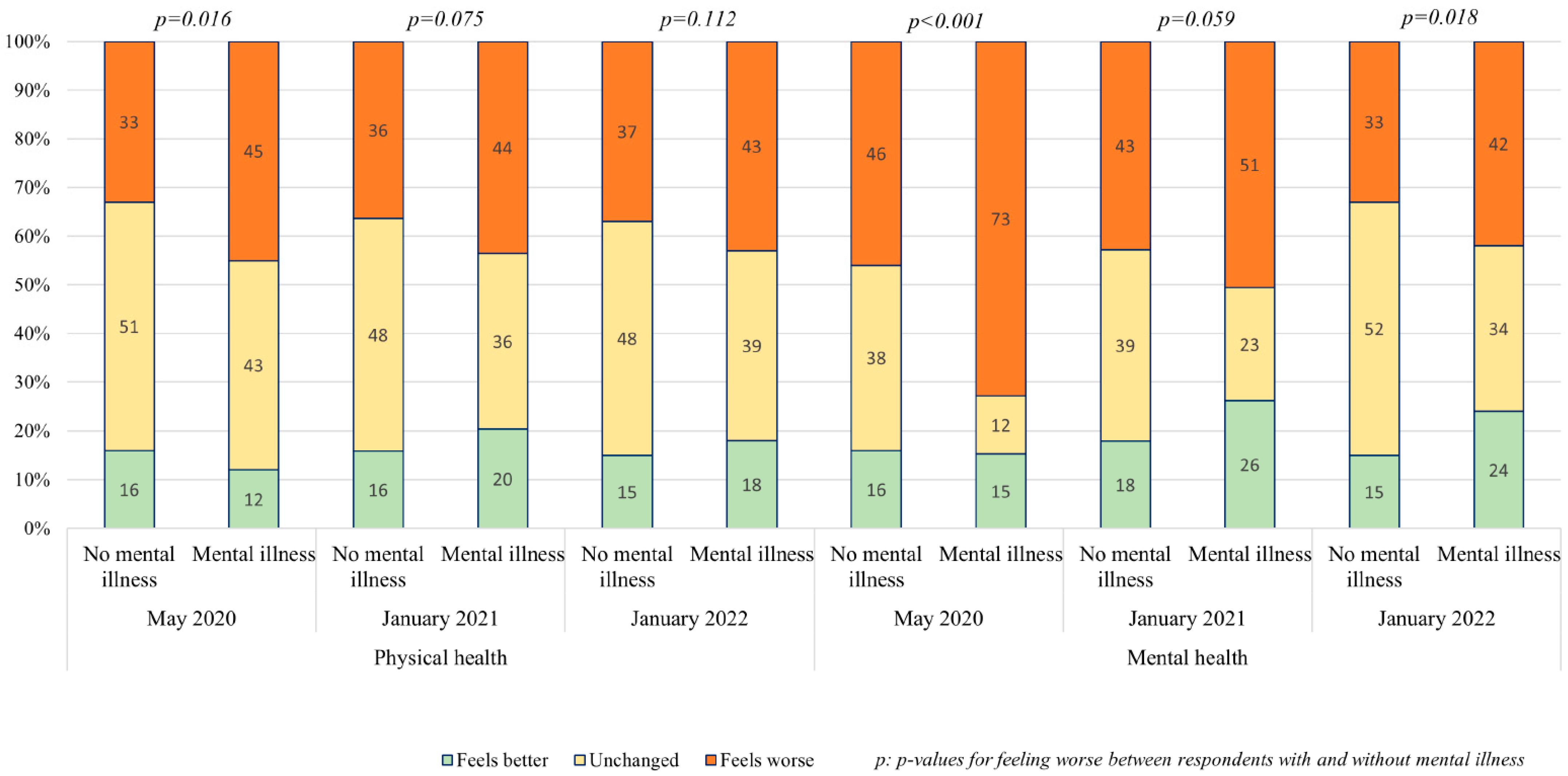
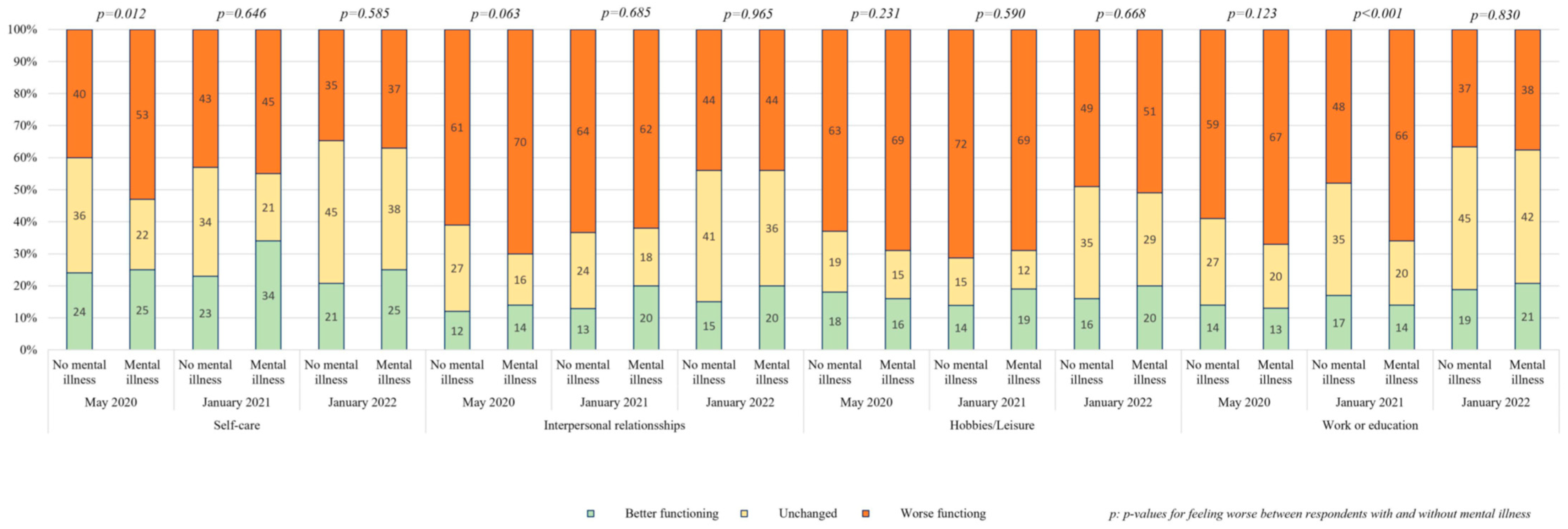
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Solmi, M.; Estradé, A.; Thompson, T.; Agorastos, A.; Radua, J.; Cortese, S.; Dragioti, E.; Leisch, F.; Vancampfort, D.; Thygesen, L.C.; et al. The Collaborative Outcomes study on Health and Functioning during Infection Times in Adults (COH-FIT-Adults): Design and methods of an international online survey targeting physical and mental health effects of the COVID-19 pandemic. J. Affect. Disord. 2021, 299, 393–407. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, N.; Barnett, P.; Greenburgh, A.; Pemovska, T.; Stefanidou, T.; Lyons, N.; Ikhtabi, S.; Talwar, S.; Francis, E.R.; Harris, S.M.; et al. Mental health in Europe during the COVID-19 pandemic: A systematic review. Lancet Psychiatry 2023, 10, 537–556. [Google Scholar] [CrossRef] [PubMed]
- Covid-19 Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 2021, 398, 1700–1712. [Google Scholar] [CrossRef] [PubMed]
- Salanti, G.; Peter, N.; Tonia, M.T.; Holloway, M.A.; White, I.R.; Darwish, L.; Low, N.; Egger, M.; Haas, A.D.; Fazel, S.; et al. The impact of the COVID-19 pandemic and associated control measures on mental health of the general population. Ann. Intern. Med. 2022, 175, 11. [Google Scholar] [CrossRef] [PubMed]
- Cénat, J.M.; Farahi, S.M.M.M.; Dalexis, R.D.; Darius, W.P.; Bekarkhanechi, F.M.; Poisson, H.; Broussard, C.; Ukwu, G.; Auguste, E.; Nguyen, D.D.; et al. The global evolution of mental health problems during the COVID.19 pandemic: A systematic review and meta-analysis of longitudinal studies. J. Affect. Disord. 2022, 315, 70–95. [Google Scholar] [CrossRef] [PubMed]
- Hossain, M.; Tasnim, S.; Sultana, A.; Faizah, F.; Mazumder, H.; Zou, L.; McKyer, E.L.J.; Ahmed, H.U.; Ma, P. Epidemiology of mental health problems in COVID-19: A review. F1000Research 2020, 9, 636–652. [Google Scholar] [CrossRef] [PubMed]
- Nam, S.-H.; Nam, J.-H.; Kwon, C.-Y. Comparison of the Mental Health Impact of COVID-19 on vulnerable and non-vulnerable groups: A systematic review and meta-analysis of observational studies. Int. J. Environ. Res. Public Health 2021, 18, 10830. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Wu, Y.; Fan, S.; Santo, T.D.; Li, L.; Jiang, X.; Li, K.; Wang, Y.; Tasleem, A.; Krishnan, A.; et al. Comparison of mental health symptoms before and during the covid-19 pandemic: Evidence from a systematic review and meta-analysis of 134 cohorts. BMJ 2023, 380, e074224. [Google Scholar] [CrossRef] [PubMed]
- Kunzler, A.M.; Lindner, S.; Röthke, N.; Schäfer, S.K.; Metzendorf, M.-I.; Sachkova, A.; Müller-Eberstein, R.; Klinger, C.; Burns, J.; Coenen, M.; et al. Mental health impact of early stages of the COVID-19 pandemic on individuals with pre-existing mental disorders: A systematic review of longitudinal research. Int. J. Environ. Res. Public Health 2023, 20, 948. [Google Scholar] [CrossRef] [PubMed]
- Murphy, L.; Markey, K.; O’ Donnell, C.; Moloney, M.; Doody, O. The impact of the COVID-19 pandemic and its related restrictions on people with pre-existent mental health conditions: A scoping review. Arch. Psychiatr. Nurs. 2021, 35, 375–394. [Google Scholar] [CrossRef] [PubMed]
- Tsamakis, K.; Tsiptsios, D.; Ouranidis, A.; Mueller, C.; Schizas, D.; Terniotis, C.; Nikolakakis, N.; Tyros, G.; Kympouropoulos, S.; Lazaris, A.; et al. COVID-19 and its consequences on mental health (Review). Exp. Ther. Med. 2021, 21, 244. [Google Scholar] [CrossRef] [PubMed]
- Torres, Z.; Oliver, A.; Fernandez, I. Older adults’ mental health during the COVID-19 pandemic: The association with social networks. Soc. Netw. 2024, 78, 164–172. [Google Scholar] [CrossRef]
- Solmi, M.; Thompson, T.; Estradé, A.; Agorastos, A.; Radua, J.; Cortese, S.; Dragioti, E.; Vancampfort, D.; Thygesen, L.C.; Aschauer, H.; et al. Global and risk-group stratified well-being and mental health during the COVID-19 pandemic in adults: Results from the international COH-FIT Study. Psychiatry Res. 2024, 342, 115972. [Google Scholar] [CrossRef] [PubMed]
- Solmi, M.; Thompson, T.; Cortese, S.; Estradé, A.; Agorastos, A.; Radua, J.; Dragioti, E.; Vancampfort, D.; Thygesen, L.C.; Aschauer, H.; et al. Collaborative outcomes study on health and functioning during infection times (COH-FIT): Insights on modifiable and non-modifiable risk and protective factors for wellbeing and mental health during the COVID-19 pandemic from multivariable and network analyses. Eur. Neuropsychopharmacol. 2025, 90, 1–15. [Google Scholar] [PubMed]
- Sørensen, T.T.; Okholm, G.T.; Vendsborg, P.; Nordentoft, M.; Correll, C.U.; Solmi, M.; Thompson, T.; Estradé, A.; Thygesen, L.C. Suicidal ideation across three waves of the COVID-19 pandemic in Denmark—Identifying vulnerable subgroups using COH-FIT data. J. Affect Disord. 2025, 389, 119656. [Google Scholar] [CrossRef] [PubMed]
- Simione, L.; Vagni, M.; Moiarano, T.; Giostra, V.; Pajardi, D. How implicit attitudes towards vaccination affect vaccine hesitancy and behaviour: Developing and validating the V-IRAP. Int. Environ. Res. Public Health 2022, 19, 4205. [Google Scholar] [CrossRef] [PubMed]
- Falbová, D.; Kovalčíková, V.; Beňuš, R.; Vorobeľová, L. Long-term consequences of COVID-19 on mental and physical health in young adults. Cent. Eur. J. Public Health 2024, 32, 219–224. [Google Scholar] [CrossRef] [PubMed]
- Solmi, M.; Thompson, T.; Estradé, A.; Agorastos, A.; Radua, J.; Cortese, S.; Dragioti, E.; Leisch, F.; Vancampfort, D.; Thygesen, L.C.; et al. Validation of the Collaborative Outcomes study on Health and Functioning during Infection Times (COH-FIT) questionnaire for adults. J. Affect. Disord. 2023, 326, 249–261. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, M.T.; Andersen, T.O.; Clotworthy, A.; Jensen, A.K.; Strandberg-Larsen, K.; Rod, N.H.; Varga, T.V. Time trends in mental health indicators during the initial 16 months of the COVID-19 pandemic in Denmark. BMC Psychiatry 2022, 22, 25. [Google Scholar] [CrossRef] [PubMed]
- Thygesen, L.C.; Møller, S.P.; Ersbøll, A.K.; Santini, Z.I.; Dahl Nielsen, M.B.; Grønbæk, M.K.; Ekholm, O. Decreasing mental well-being during the COVID-19 pandemic: A longitudinal study among Danes before and during the pandemic. J. Psychiatr. Res. 2021, 144, 151–157. [Google Scholar] [CrossRef] [PubMed]

| May 2020 a (n = 3134) n (%) | May 2020 b (n = 3078) n (%) | January 2021 (n = 1170) n (%) | January 2022 (n = 1174) n (%) | |
|---|---|---|---|---|
| Sociodemographic characteristics | ||||
| Sex | ||||
| Men | 496 (16) | 1445 (47) | 560 (48) | 526 (45) |
| Women | 2638 (84) | 1634 (53) | 610 (52) | 648 (55) |
| Age | ||||
| 18–29 years | 384 (12) | 874 (28) | 333 (28) | 320 (27) |
| 30–39 years | 465 (15) | 417 (14) | 180 (15) | 191 (16) |
| 40–49 years | 677 (22) | 548 (18) | 204 (17) | 197 (17) |
| 50–59 years | 805 (26) | 530 (17) | 199 (17) | 217 (18) |
| 60–69 years | 590 (19) | 556 (18) | 202 (17) | 203 (17) |
| 70+ years | 213 (7) | 153 (5) | 52 (4) | 46 (4) |
| Mean age (min; max) | 49 (18;84) | 44 (18;84) | 43 (18;76) | 43 (18;86) |
| Educational level | ||||
| None/primary education | 217 (7) | 874 (28) | 361 (31) | 216 (18) |
| High school/vocational school | 230 (7) | 1079 (35) | 407 (35) | 327 (28) |
| College/university degree/PhD | 2687 (86) | 1126 (37) | 402 (34) | 631 (54) |
| Occupation | ||||
| Not working | 1243 (40) | 711 (23) | 263 (22) | 194 (17) |
| Not working in health care | 1303 (41) | 2081 (68) | 802 (69) | 837 (71) |
| Working in health care | 574 (18) | 258 (8) | 104 (9) | 142 (12) |
| Missing | 14 (1) | 28 (1) | 1 (0) | 1 (0) |
| Health and wellbeing | ||||
| Mental illness | ||||
| No mental illness | 1629 (52) | 1480 (48) | 956 (82) | 946 (80) |
| At least one mental illness | 1322 (42) | 1344 (44) | 172 (15) | 194 (17) |
| Missing | 183 (6) | 254 (8) | 42 (3) | 34 (3) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vendsborg, P.; Jarlstrup, N.S.; Hoffmann, S.H.; Nordentoft, M.; Correll, C.U.; Solmi, M.; Thompson, T.; Estradé, A.; Sørensen, T.T.; Thygesen, L.C. Health, Psychological Distress, and Functioning During the COVID-19 Pandemic Among Danish Adults with and Without a Preexisting Mental Illness. Int. J. Environ. Res. Public Health 2025, 22, 1260. https://doi.org/10.3390/ijerph22081260
Vendsborg P, Jarlstrup NS, Hoffmann SH, Nordentoft M, Correll CU, Solmi M, Thompson T, Estradé A, Sørensen TT, Thygesen LC. Health, Psychological Distress, and Functioning During the COVID-19 Pandemic Among Danish Adults with and Without a Preexisting Mental Illness. International Journal of Environmental Research and Public Health. 2025; 22(8):1260. https://doi.org/10.3390/ijerph22081260
Chicago/Turabian StyleVendsborg, Per, Nanna Schneekloth Jarlstrup, Sofie H. Hoffmann, Merete Nordentoft, Christoph U. Correll, Marco Solmi, Trevor Thompson, Andrés Estradé, Trine Toft Sørensen, and Lau Caspar Thygesen. 2025. "Health, Psychological Distress, and Functioning During the COVID-19 Pandemic Among Danish Adults with and Without a Preexisting Mental Illness" International Journal of Environmental Research and Public Health 22, no. 8: 1260. https://doi.org/10.3390/ijerph22081260
APA StyleVendsborg, P., Jarlstrup, N. S., Hoffmann, S. H., Nordentoft, M., Correll, C. U., Solmi, M., Thompson, T., Estradé, A., Sørensen, T. T., & Thygesen, L. C. (2025). Health, Psychological Distress, and Functioning During the COVID-19 Pandemic Among Danish Adults with and Without a Preexisting Mental Illness. International Journal of Environmental Research and Public Health, 22(8), 1260. https://doi.org/10.3390/ijerph22081260







