Abstract
Background: Anaemia and undernutrition remain a significant public health problem in low and middle-income countries (LMICs), particularly affecting under-five children. In Tanzania, the prevalence of anaemia and undernutrition in under-five children is still high; however, less is known about the prevalence and predictors of these conditions in rural areas. Therefore, the current cross-sectional study presents the prevalence and determinants of anaemia and undernutrition among 457 children aged 6–24 months in the Babati and Hanang districts of Tanzania. Method: Haemoglobin concentration was assessed through capillary blood samples. Anaemia was classified according to WHO 2011 guidelines using a cut-off of <11.0 g/dL for children under five, while the WHO 2006 growth indicators were used to classify the nutritional status (i.e., stunting, wasting and underweight). Results: The results from this study show that 32%, 32%, 20% and 4% of children aged 6–24 months were anaemic, stunted, underweight and wasted, respectively, while only 33% had an adequate minimum dietary diversity (MDD). In addition, the child’s age (13–24 months) was significantly associated with anaemia (AOR: 2.1 95% CI 1.4, 3.1), stunting (AOR:17.4 95% CI 10.3, 29.4) and underweight (AOR: 15.9 95% CI 7.9, 32.0). Moreover, male children were three times more likely to be wasted (AOR: 3.5 95% CI 1.1, 10.9) than their female counterparts. Anaemia and stunting were the most prevalent nutritional disorders among 6–24-month-old children in the Hanang and Babati districts. Moreover, age (13–24 months) was found to be the common predictor for anaemia, stunting and underweight. Conclusion: The observed association between age and anaemia, as well as undernutrition, suggest that age may be an essential factor when designing nutrition-related programs in similar rural settings.
1. Introduction
Anaemia is a disorder associated with a low count of red blood cells and haemoglobin. Haemoglobin comprises a simple protein called globin, and an iron called haem; therefore, a low iron status can lead to reduced haemoglobin levels and result in anaemia. This is supported by the World Health Organization (WHO), which reports that more than 50% of anaemia cases are caused by iron deficiency [1]. In LMICs, anaemia mainly affects women of reproductive age (15–49 years), pregnant women and children under five years [2]. Globally, anaemia cases stand at 42% in children under five [2], which is lower compared to the prevalence of anaemia (60%) in sub-Saharan Africa [3]. Undernutrition is assessed in a variety of ways; wasting is defined as low weight for length (WLZ), stunting is low length for age (LAZ), and underweight is low weight for age (WAZ), categorized as below −2 standard deviation from the median [4]. A Global Nutrition Organization highlighted that within Africa, 32% of children were stunted and 5% were wasted in East Africa; meanwhile, the total regional prevalence for stunting was 30% and that for wasting was 6% [5].
Anaemia in children under five can be caused by a low maternal iron status, the consumption of plant-based complementary foods with low bioavailable iron, malaria infection, and gastrointestinal disorders such as diarrhoea, which might affect iron absorption in the body [6,7,8]. These factors are also linked to undernutrition in children under five years. Thus, the reduced dietary intake of nutrient-rich foods, infections, and gastrointestinal disorders, i.e., diarrhoea, might lead to wasting, stunting and underweight in young children [9,10,11]. Anaemia, stunting, wasting and underweight are caused largely by the poor dietary intake of protein, energy, fat, and micronutrient-rich foods [12,13].
The WHO defines adequate minimum dietary diversity (MDD) as the consumption of five out of eight food groups on the previous day for children aged 6–24 months [14]. However, meeting the MDD has been a challenge, especially in LMICs, where most children under five consume less than five food groups in a day [15,16,17]. The reason for this might be due to the poor socio-economic status of the household, which reduces the purchasing power of nutrient-dense foods [16]. Moreover, a lack of nutrition knowledge regarding the appropriateness of complementary feeding practices among mothers and caregivers and seasonality affect the availability of certain types of foods [18,19,20]. Dietary diversity can be linked to nutritional status, as shown in a study performed in 32 Sub-Saharan African countries [16]. The study found that 6–23-month-old children who met the MDD had a 12%, 17%, and 13% reduced risk of being stunted, underweight, and wasted, respectively, compared to the ones with inadequate dietary diversity [16].
Anaemia, wasting, stunting and underweight in children can lead to a loss of appetite and diminished neural and cognitive development, which may negatively affect a child’s academic performance [21,22]. Additionally, these undernutrition disorders lead to low immunity, which increases the chances of getting diseases and infections. As a result, it affects the child’s dietary intake and nutrient metabolism [23,24,25]. Recent national data from Tanzania show that stunting stands at 30%, wasting at 3%, underweight at 12% and anaemia at 59% in children under five [17].
However, there is a scarcity of data on the nutritional status of children in rural areas like the Babati and Hanang districts since most of the data are regional and national. Therefore, this present study sought to assess the prevalence and determinants of anaemia, wasting, stunting, and underweight among 6–24-month-old children living in the Babati and Hanang districts. These districts are unique in that most residents are agro-pastoralists, i.e., graze animals and cultivate crops, leading to a distinct and unique dietary pattern. In addition, the current study is part of a bigger study on aflatoxin exposure [26] in which the Babati and Hanang districts were purposively selected as they are among the districts with high maize production in Tanzania, and maize is one of the foods that is highly susceptible to aflatoxin contamination [27,28,29].
2. Materials and Methods
2.1. Study Area, Design and Participants Recruitment
Babati and Hanang are among the six districts in the Manyara region, Tanzania. The Manyara region is in the Northern zone of Tanzania, within the latitude of 04°10′ S and longitude of 34°15′ S, with a total area of 17,190 sq m. The health centres were randomly selected to represent other centres in the respective districts.
A cross-sectional study was conducted among mother–child pairs of children aged 6–24 months from October to November 2022. Participants were recruited from the Reproductive and Child Health Clinics (RCHs), including the mobile clinics in each selected ward. Upon reaching the health facility, systematic random sampling was conducted to select the prospective participants using clinic cards. The potential participants were informed about the study and invited to join. Participants willing to participate were assessed for their eligibility, with the criteria including children aged between 6 and 24 months and children who were not sick three days before and on the interview day. The child’s sickness was confirmed by asking the mother/caregiver and the health practitioner before enrolment of the study participants.
2.2. Sample Size
Since the current study was part of a larger aflatoxin project, the sample size was calculated based on findings from a previous aflatoxin study conducted in Haydom Ward, Manyara region, due to the limited availability of studies from the Babati and Hanang districts.
The sample size was determined using the Kothari formula [30]: n = [(Z2 × P(1 − P))/d2]; here, P was the estimated prevalence of aflatoxin exposure (72%) among children under 36 months in Haydom, Mbulu District, Manyara region [31]. The sample size calculation used a 95% confidence level (Z = 1.96), 4% absolute precision (d = 0.04), and 80% statistical power. Based on these parameters, a sample size of 485 participants was proposed. Ultimately, 457 mother–child pairs participated in the study (Figure 1). In cases where a mother had more than one child aged 6–24 months, one child was randomly selected.
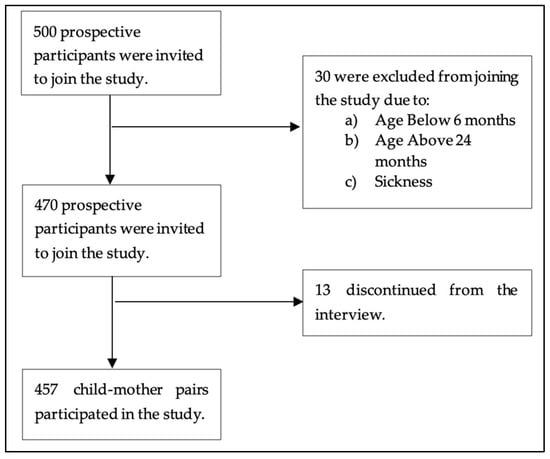
Figure 1.
Schematic diagram showing participant recruitment and sample size.
2.3. Assessment of Anthropometry, Anaemia and Dietary Diversity
Experienced research assistants with Human Nutrition backgrounds and two nurses from each RCH were recruited to collect anthropometric data such as the children’s length and weight, measure their haemoglobin level, and assess their dietary intake.
2.3.1. Anthropometry Assessment
The length of the children was measured to the nearest 0.1 cm using a length board (210 Seca, Hamburg, Germany). Each length was taken with the child lying down, face up, on the wooden length board with five major body points touching the length board. Weight was measured to the nearest 0.1 kg and was taken in light clothing using a weighing scale (874 Seca, Hamburg, Germany). For both weight and length, measurements were taken in triplicate, and the mean of each measurement was calculated and recorded as a final measurement. The WAZ, LAZ, and WLZ growth indices were determined by using ENA for SMART software 2020 (version: Jan/11); meanwhile, the children with WAZ, LAZ and WLZ below −2 standard deviation of the median were classified as underweight, stunted, and wasted, respectively. Moreover, children between with ≤−2 SD and ≥−3 SD of the median were classified as moderately underweight, stunted, or wasted, while those with <−3 SD were classified as severely underweight, stunted, or wasted [4].
2.3.2. Anaemia Diagnosis
Haemoglobin assessment was conducted in the field using a portable HemoCue®Hb 201+ machine (manufactured by HemoCue AB Company in Ängelholm, Sweden) which was validated before use. Two to three drops of blood were put in the microcuvette of the HemoCue®Hb 201+, and the haemoglobin readings were recorded in a few seconds. The measurements were performed in triplicate, and the mean of each measurement was calculated and recorded as the final measurement. The current study considered the cut-off points of a haemoglobin concentration of ≥11 g/dL, 10–10.9 g/dL, 7–9.9 g/dL and <7 g/dL as normal, mild, moderate and severe anaemia, respectively [1]. Mothers were immediately informed of their children’s haemoglobin test results. Children found to have severe anaemia were referred to paediatricians at the respective district hospitals for further evaluation and appropriate intervention, which could include blood transfusion or nutritional supplementation.
2.3.3. Dietary Intake Assessment
The mothers and caregivers of children aged 6–24 months responded to a validated food frequency questionnaire (FFQ) [32]. From these, the child’s dietary diversity was calculated by assessing the intake of eight food groups in the past 24 h based on WHO guidelines [32]. The eight food groups included Group 1: Cereal, grain, roots, and tubers; Group 2: Breast milk; Group 3: Legumes and nuts; Group 4: Dairy products; Group 5: Flesh foods; Group 6: Eggs; Group 7: Vitamin A-rich fruits and vegetables; and Group 8: fruits and vegetables. For example, when a mother reported giving the child porridge made of maize flour or sorghum in the past 24 h, the consumed food was placed in group 1, or when a mother gave her child cow’s milk, this response was placed in group 4. Thereafter, adequate minimum dietary diversity was attained if a child consumed five or more groups out of the eight food groups and inadequate dietary diversity was attained if a child consumed below five food groups [14].
2.4. Data Analysis
The current study assumed that anaemia and undernutrition in children under five persist even in districts with high food production. To assess the factors that could have contributed to this, the dependent variables used in this study were anaemia, stunting, wasting, and underweight. The child’s age in months, gender, the number of children under the age of five the mother had, food groups, and MDD were considered as the independent variables.
Data were analyzed using Statistical Packages for Social Science (SPSS) Version 28.0. The original data were recorded in Excel and transferred to the SPSS software. Descriptive statistics were presented in terms of the frequency and percentage of the socio-demographic characteristics of the child and mother, MDD, stunting, wasting, underweight, and anaemia in children. Unadjusted and adjusted logistic regression evaluated the factors associated with stunting, underweight, wasting, and anaemia. The adjusted logistic regression model included all variables that showed a significant association in the unadjusted logistic regression analysis.
2.5. Ethical Considerations
This study was conducted according to the guidelines in the Declaration of Helsinki. All procedures involving human subjects were approved by the [Tanzania National Institute for Medical Research; NIMR/R.8a/Vol.IX/4077]. Written and verbal informed consent was obtained from all subjects. Verbal consent was witnessed and formally recorded.
3. Results
3.1. Socio-Demographic Characteristics
As shown in Table 1, most study participants were from the Babati District, likely due to higher birth rates in Babati compared to the Hanang District. Participants were evenly distributed by sex, with most children aged between 6 and 12 months. Most mothers were between 18 and 29 years old, married, and had completed at least primary school education. Additionally, the majority of mothers reported exclusively breastfeeding their children for the first six months and continued breastfeeding for up to two years.

Table 1.
Socio-demographic characteristics of the study participants (mother-child dyads).
3.2. Prevalence of Stunting, Wasting, Underweight and Anaemia Among 6–24 Months Old Children
The findings from this study indicate that 32%, 4%, 20% and 32% of children aged 6–24 months were stunted, wasted, underweight and anaemic, respectively. Figure 2 presents the distribution of overall, mild, moderate and severe forms of these conditions.
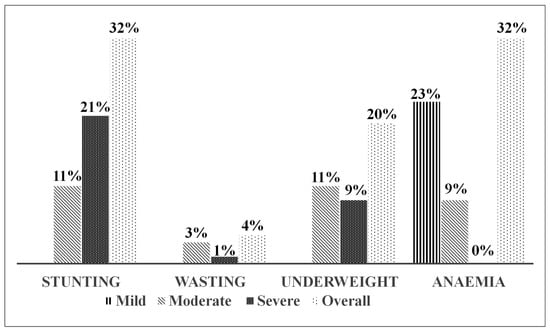
Figure 2.
Percentage of mild, moderate and severe undernutrition and anaemia among children aged 6–24 months.
3.3. Food Group Consumption Amongst 6–24 Months Old Children in Hanang and Babati Districts
Among the eight food groups used to calculate MDD in children, the cereal, grains, roots and tubers group was the most consumed group. In contrast, the egg group was the least consumed food group, as shown in Figure 3. Regarding fruit and vegetable intake, the Babati district consumed more fruits and vegetables and vitamin A-rich fruits and vegetables than the Hanang district, as shown in Figure 3. Meanwhile, only 33% of our study participants had attained the MDD.
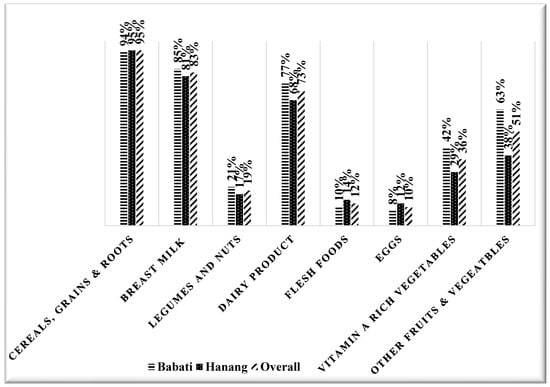
Figure 3.
Percentage of dietary intake of different food groups among children aged 6–24 months per districts and overall.
3.4. Factors Associated with Stunting, Underweight, Wasting and Anaemia Among 6–24 Months Old Children in Babati and Hanang Districts in Unadjusted Odds Ratio
In the unadjusted logistic regression model, as shown in Table 2, factors such as a child being aged between 13 and 24 months (COR: 15.8 95% CI 9.5, 26.3) and a mother having more than three under-five children (COR: 3.4 95% CI 1.7, 6.9) increased the odds of the child being stunted. Meanwhile, the intake of cereals, grains, roots and tubers (COR: 0.3 95% CI 0.1, 0.8), legumes and nuts (COR: 0.4 95% CI 0.2, 0.8), dairy products (COR: 0.5 95% CI 0.3, 0.8) and vitamin A-rich fruits and vegetables (COR: 0.56 95% CI 0.3–0.8) reduced the odds of being stunted. Moreover, a child being aged between 13 and 24 months (COR: 15.7 95% CI 7.8, 31.5) and a mother having more than three under-five children (COR: 2.2 95% CI 1.0, 4.5) increased the odds of the child being underweight, while the intake of dairy products (COR: 0.5 95% CI 0.3, 0.8) and vitamin A-rich fruits and vegetables (COR: 0.5 95% CI 0.3, 0.89) decreased the odds of children being underweight. Being a male child (COR: 3.4 95% CI 1.1, 10.6) rather than a female child increased the odds of being wasted by three times. Children aged 13–24 months (COR: 2.2 95% CI 1.5, 3.3) were two times more likely to be anaemic compared to the younger children (6–12 months). Other factors such as the MDD, intake of fresh foods, eggs and other fruits and vegetables were not associated with stunting, underweight, wasting or anaemia.

Table 2.
Factors associated with stunting, underweight, wasting and anaemia by unadjusted odds ratio.
3.5. Factors Associated with Stunting, Underweight, Wasting and Anaemia Among 6–24 Months Old Children in Babati and Hanang Districts in Adjusted Odds Ratio
In the adjusted logistic regression model, we found that children aged between 13 and 23 months had a higher risk of being stunted (AOR: 17.4 95% CI 10.3, 29.4), under-weight (AOR: 15.9 95% CI 7.9, 32.0) and anaemic (AOR: 2.1 95% CI 1.4, 3.1) than younger children (6–12 months). In terms of gender, a male child was three times more likely to be wasted (AOR: 3.5 95% CI 1.1, 10.9) than their female counterparts, highlighting a significant gender disparity that requires immediate attention. Moreover, the intake of cereals, grains, roots and tubers (AOR: 0.2 95% CI 0.1, 0.8), and legumes (AOR: 0.3 95% CI 0.2, 0.6) reduced the odds of being stunted. However, no other factors such as the number of children and the intake of dairy products and vitamin A-rich fruits and vegetables were found to be associated with anaemia, stunting, underweight or wasting (Table 3).

Table 3.
Factors associated with stunting, underweight, wasting and anaemia by adjusted odds ratio.
4. Discussion
The present study aimed to assess the prevalence and factors associated with anaemia and undernutrition among children aged 6–24 months in the Hanang and Babati districts of the Manyara region, Tanzania. In this study, we found that one-third of children were stunted and anaemic, with age in months (13–24 months) being the common predictor for anaemia, stunting and underweight.
Regarding dietary intake, cereals, grains, roots, and tubers was the most commonly consumed food group. These findings are consistent with two studies conducted in Tanzania [33,34], which reported cereals, roots, and tubers as the most consumed food group and that primarily used in the complementary foods of younger children (aged 6–24 months). Inadequate MDD was evident in most study participants (67%). These findings are consistent with those reported in the Tanzania Demographic Health Survey (TDHS-MIS), which found that most children aged 6–23 months (88%) had inadequate MDD [17]. Similarly, other studies in Tanzania found inadequate MDD among children under five [15,35]. The inadequate MDD and high intake of the cereal food group might be due to the traditional use of cereal-based complementary foods for young children in many Tanzanian communities [33,36,37,38]. In addition, the low socio-economic status of the Manyara residents may reduce their purchasing ability to buy food from other food groups (i.e., vegetables, legumes, nuts, etc.), apart from what they mainly produce as agro-pastoralists (maize and dairy foods) [15].
The prevalence of stunting (32%), wasting (4%), underweight (19%) and anaemia (32%) reported in this study aligns with the TDHS-MIS of 2022, which presents a national prevalence of 30% for stunting, 3% for wasting, 12% for underweight and 59% for anaemia among children under five years [17]. The lower prevalence of anaemia reported in this study might be attributed to seasonality, as the current study was conducted during the rainy season (November), which typically increases the availability, accessibility and affordability of vegetables [39,40]. Consequently, food prices drop with increased supply, leading to increased dietary diversification, which might have reduced the anaemia cases in the current study [15].
Interestingly, the current study found that male children had higher odds of being wasted than their female counterparts. This was consistent with other Tanzanian studies that found that female children have lower odds of being wasted than their male counterparts [17,41,42]. This can be explained by the fact that male children tend to be more playful than female children, resulting in higher energy expenditure compared to female children [9,43,44,45]. In addition, most male children tend to play outside of their home environment, which exposes them to different environmental risks and increases their chances of infections, further exacerbating the risk of wasting [42,46,47].
Stunting was more prevalent in older children (13–23 months), which is in line with other studies in Tanzania [17,41]. These results can be explained by the fact that stunting is more evident towards the end of the first 24 months in children. This signifies the repeated poor intake of food or recurrent infection at a younger age, which is evident later in life [48,49,50]. Moreover, children aged 13 to 24 months showed a higher likelihood of being underweight compared to their younger counterparts. This finding is supported by two studies conducted in Tanzania, which reported an increase in underweight cases as children grow older [17,51]. This may be attributed to increased physical activity and movement during this age, which require more energy, while mothers tend to focus their feeding practices on their younger children [42,51].
In adjusted logistic regression, the current study found that the intake of cereals grains, roots and tubers, as well as legumes and nuts, significantly decreased the odds of being stunted. These results align with a study performed in Tanzania, which found that the increased consumption of legumes, nuts, and carbohydrate-rich foods was associated with a reduced risk of stunting in children [52]. The consumption of protein-rich foods such as cow’s milk, legumes, and nuts may stimulate the production of Insulin-like Growth Factor 1 (IGF-1) [53]. When IGF-1 is stimulated, it promotes longitudinal bone growth and skeletal maturation, which can lead to an increase in height [53]. Moreover, the consumption of carbohydrate-rich foods (i.e., grains, roots and tubers) plays a crucial role in providing energy and supporting growth in young children, thereby facilitating growth and reducing stunting [54].
Another interesting finding was seen in the effect of age on anaemia; thus, older children (ages 13–24 months) were found to be more anaemic than younger children (ages 6–12 months). This aligns with findings from a study conducted in Tanzania [40]. The higher prevalence of anaemia in older children may be linked to their increased iron requirements as they grow [55]. Additionally, participants reported using complementary foods that were plant-based and contained low bioavailable iron (Fe3+) and phytates (iron inhibitors) [56], leading to a persistent reduction in iron intake, which becomes evident later in life.
While different categories of anaemia were assessed, no severe cases were observed. Most children presented with mild anaemia, indicating a likely chronic deficiency linked to limited sources of iron-rich or bioavailable iron, such as plant-based complementary foods. Similarly, undernutrition, particularly underweight and wasting, was primarily moderate rather than severe. However, a higher proportion of children had severe stunting compared to the other forms of undernutrition, highlighting persistent, long-term inadequacies in dietary quality rather than acute food insecurity. These findings align with the dietary patterns of agro-pastoralist communities, where consumption is primarily cereal-based and lacks diversity [57]. While this cross-sectional study does not evaluate the effectiveness of interventions, it highlights the importance of future research and programming in similar rural settings to consider context-specific approaches such as community-based nutrition education using locally available foods, seasonal diet planning, and/or food fortification. These strategies, tailored to the specific needs of each community, could significantly improve dietary quality and reduce the burden of nutritional deficiencies.
Strengths and limitations: One of the strengths of this study is its comprehensive reporting of nutritional status, including the prevalence of anaemia, stunting, underweight and wasting in children, specifically in the Babati and Hanang districts, as these results can be generalized to the respective districts. However, the current study is limited by the use of FFQ and MDD to assess dietary quality, which may have missed the quantity of food consumed, which is an essential component in evaluating dietary practices among children under five. Another limitation is the use of a cross-sectional study design, which restricted data collection to a single month and, therefore, did not account for seasonal variations in food consumption. Although the current study was well communicated to the community through local announcements and sensitization efforts, the study was conducted in RCH clinics within the hospital or dispensaries, which might have missed children who did not attend RCH clinics. Though the prevalence of malaria infection among children in the Manyara region is less than 1% [17], the current study did not directly assess infections such as malaria and worm infestations, which are known confounders of anaemia and undernutrition. To minimize potential confounding, we assessed whether children had accessed key health services within the three months before the interview. Specifically, we confirmed that participants had received deworming tablets to reduce the risk of worm infections, routine immunizations, and vitamin A supplementation. While infections were not directly measured, these preventive measures likely helped reduce their potential impact on our findings.
5. Conclusions
Anaemia and stunting were identified as the most prevalent forms of undernutrition among children aged 6–24 months in the Babati and Hanang districts. These conditions were significantly associated with an older age in children (13–24 months). Future nutrition programs in these areas may benefit from prioritizing strategies that directly address the determinants identified in the current study.
Author Contributions
N.M., designed the research, developed data collection tools, collected data, performed statistical analysis, interpreted results, developed the first draft and revised all manuscript versions. H.D.M., designed the study, reviewed the data collection tools, assisted in data collection, interpreted data, and critically reviewed the manuscript. N.K., S.M., C.I.A. and Y.Y.G., reviewed data collection tools, interpreted results and reviewed all the manuscript drafts. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no funding, but the APC was funded by the L’Oreal-UNESCO For Women in Science Young Talents Award for the Sub-Saharan Africa Programme, 2023.
Institutional Review Board Statement
This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects/patients were approved by the Institutional Review Board of the TANZANIA NATIONAL INSTITUTE FOR MEDICAL RESEARCH (Protocol code NIMR/R.8a/Vol.IX/4077, 3 August 2022) for studies involving humans.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors on request.
Acknowledgments
This was not a sponsored study; however, we acknowledge all the participants who joined our study and the nurses and nutritionists who helped us during data collection. Furthermore, we extend our gratitude to the District Commissioner and District Medical Officer for the Babati District and Hanang District for their support and guidance during data collection.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| HB | Haemoglobin |
| IGF-1 | Insulin-like growth factor 1 |
| LAZ | Length for Age |
| MDD | Minimum Dietary Diversity |
| RCH | Reproductive Child Health |
| SPSS | Statistical Package for Social Science |
| WAZ | Weight for Age |
| WLZ | Weight for Length |
| WHO | World Health Organization |
References
- World Health Organization. Haemoglobin Concentrations for the Diagnosis of Anaemia and Assessment of Severity. 2011. Available online: https://apps.who.int/iris/bitstream/handle/10665/85839/WHO_NMH_NHD_MNM_11.1_eng.pdf?ua=1 (accessed on 3 May 2023).
- World Health Organization. Health Topics: Anaemia. Available online: https://www.who.int/health-topics/anaemia#tab=tab_1 (accessed on 10 April 2023).
- WHO. Global Anaemia Estimates, 2021 Edition. Available online: https://www.who.int/data/gho/data/themes/topics/anaemia_in_women_and_children#:~:text=In%202019%2C%20global%20anaemia%20prevlence%20was%2039.8%25%20(95%25,UI%2056.6%25%2C%2063.7%25) (accessed on 12 April 2023).
- World Health Organization. WHO Anthro Survey Analyzer (2019). Available online: https://cdn.who.int/media/docs/default-source/child-growth/child-growth-standards/software/anthro-survey-analyser-quickguide.pdf?sfvrsn=dc7ddc6f_6 (accessed on 11 April 2023).
- Global Nutrition Report. Country Nutrition Profiles, United Republic of Tanzania. 2020. Available online: https://globalnutritionreport.org/resources/nutrition-profiles/africa/eastern-africa/united-republic-tanzania/ (accessed on 11 April 2023).
- Kejo, D.; Mosha, T.C.E.; Petrucka, P.; Kimanya, M.E. Prevalence and predictors of undernutrition among underfive children in Arusha District, Tanzania. Food Sci. Nutr. 2018, 6, 2264–2274. [Google Scholar] [CrossRef] [PubMed]
- Kebede, D.; Getaneh, F.; Endalamaw, K.; Belay, T.; Fenta, A. Prevalence of anemia and its associated factors among under-five age children in Shanan gibe hospital, Southwest Ethiopia. BMC Pediatr. 2021, 21, 542. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Gade, S.; Kalambe, M.; Gawande, U. Iron Deficiency Anemia in Pregnancy. ECS Trans. 2022, 107, 15777. [Google Scholar] [CrossRef]
- Akombi, J.B.; Agho, K.E.; Hall, J.J.; Wali, N.; Renzaho, A.M.N.; Merom, D. Stunting, Wasting and Underweight in Sub-Saharan Africa: A Systematic Review. Int. J. Environ. Res. Public Health 2017, 14, 863. [Google Scholar] [CrossRef]
- Gosdin, L.; Martorell, R.; Bartolini, R.M.; Mehta, R.; Srikantiah, S.; Young, M.F. The co-occurrence of anemia and stunting in young children. Matern. Child Nutr. 2018, 14, e12597. [Google Scholar] [CrossRef]
- Woodruff, B.A.; Wirth, J.P.; Rohner, F. Determinants of Stunting, Wasting and Anemia in Guinean Preschool-Age Children: An Analysis of DHS Data from 1992, 2005 and 2012. Food Nutr. Bull. 2018, 39, 39–53. [Google Scholar] [CrossRef]
- Meshram, I.I.; Neeraja, G.; Longvah, T. Vitamin A Deficiency, Anemia and Nutritional Status of under 5-Year Children from Northeast India. Indian J. Community Med. 2021, 46, 673–679. [Google Scholar] [CrossRef]
- Gaston, R.T.; Habyarimana, F.; Ramroop, S. Joint modelling of anemia and stunting in children less than five years of age in Lesotho: A cross-sectional case study. BMC Public Health 2022, 22, 285. [Google Scholar] [CrossRef]
- World Health Organization; United National International Children’s Emergency Fund. Indicators for Assessing Infant and Young Child Feeding Practices: Definition and Measurement Methods. 2021. Available online: https://iris.who.int/bitstream/handle/10665/340706/9789240018389-eng.pdf?sequence=1 (accessed on 3 May 2024).
- Hanselman, B.; Ambikapathi, R.; Mduma, E.; Svensen, E.; Caulfield, L.E.; Patil, C.L. Associations of land, cattle and food security with infant feeding practices among a rural population living in Manyara, Tanzania. BMC Public Health 2018, 18, 159. [Google Scholar] [CrossRef]
- Aboagye, R.G.; Seidu, A.A.; Ahinkorah, B.O.; Arthur-Holmes, F.; Cadri, A.; Dadzie, L.K.; Hagan, J.E., Jr.; Eyawo, O.; Yaya, S. Dietary Diversity and Undernutrition in Children Aged 6–23 Months in Sub-Saharan Africa. Nutrients 2021, 13, 3431. [Google Scholar] [CrossRef]
- Tanzania Demographic and Health Survey and Malaria Indicator Survey (TDHS-MIS). 2022. Available online: https://dhsprogram.com/pubs/pdf/PR144/PPR144.pdf (accessed on 10 February 2024).
- Gassara, G.; Chen, J. Household Food Insecurity, Dietary Diversity and Stunting in Sub-Saharan Africa: A Systematic Review. Nutrients 2021, 13, 4401. [Google Scholar] [CrossRef] [PubMed]
- Lencha, F.M.; Zaza, Z.J.; Digesa, L.E.; Mulatu, A.T. Minimum dietary diversity and associated factors among children under the age of five attending public health facilities in Wolaita Soddo town, Southern Ethiopia, 2021: A cross-sectional study. BMC Public Health 2022, 22, 2368. [Google Scholar] [CrossRef] [PubMed]
- Kang, Y.; Ganganaboina, S.; Fang, T.; Tran, A.; Suzuki, A.; Son, J.; Roh, K. Land access, livelihoods, and dietary diversity in a fragile setting in northern Uganda. Front. Sustain. Food Syst. 2023, 7, 178386. [Google Scholar] [CrossRef]
- Martins, V.J.B.; Florencio, T.M.; Grillo, L.P.; Franco, M.C.; Martins, P.A.; Clemente, A.P.G.; Santos, C.D.; de Fatima, A.; Vieira, M.; Sawaya, A.L. Long-Lasting Effects of Undernutrition. Int. J. Environ. Res. Public Health 2021, 8, 1817–1846. [Google Scholar] [CrossRef]
- Beula, N.V.; Premraj, C.F. Effects of Malnutrition—A Social Perspective. Res. Humanit. Soc. Sci. 2017, 7, 191–196. [Google Scholar]
- Melku, M.; Asrie, F.; Shiferaw, E.; Woldu, B.; Yihunew, Y.; Asmelash, D.; Enawgaw, B. Knowledge, Attitude and Practice Regarding Blood Donation among Graduating Undergraduate Health Science Students at the University of Gondar, Northwest Ethiopia. Ethiop. J. Health Sci. 2018, 28, 582. [Google Scholar] [CrossRef]
- Govender, I.; Rangiah, S.; Kaswa, R.; Nzaumvila, D. Malnutrition in children under the age of 5 years in a primary health care setting. S. Afr. Fam. Pract. 2021, 63, 5337. [Google Scholar] [CrossRef]
- Matiysiak, M. Anemia in Children: A pediatrician’s view. Acta Haematol. Pol. 2021, 52, 402–405. [Google Scholar] [CrossRef]
- Mshanga, N.; Kassim, N.; Sonto, S.; Martin, H.; Pirani, M.; Moore, S.; Auma, C.I.; Kimanya, M.; Gong, Y.Y. A Cross-sectional Association between Serum Aflatoxin and Micronutrient Status among Children aged 6–24 months in Rural Tanzania. MCN J. 2025, submitted. [Google Scholar]
- Tanzania Ministry of Agriculture; Food Security and Cooperatives. National Sample Census of Agriculture 2007/2008 Small Holder Agriculture—Regional Report—Manyara Region. 2012. Available online: https://www.fao.org/fileadmin/templates/ess/ess_test_folder/World_Census_Agriculture/Country_info_2010/Eliman_New_uploads/REP1_TZA_ENG_VOLII_2007-08.pdf (accessed on 28 April 2023).
- Mutungi, C.; Makindara, J.; Magoma, R.; Affognon, H. Postharvest Losses in Africa—Analytical Review and Synthesis: The Case of Tanzania; Technical Report: 1–114; African Insect Science for Food and Health: Nairobi, Kenya, 2012. [Google Scholar]
- Tanzania Ministry of Agriculture. 2016/17 Annual Agriculture Sample Survey Initial Report. Available online: https://www.nbs.go.tz/nbs/takwimu/Agriculture/2016-17_AASS%20Report%20_Final.pdf (accessed on 28 April 2023).
- Kothari, C.R. Research Methodology: Methods and Techniques; New Age International: New Delhi, India, 2004. [Google Scholar]
- Chen, C.; Mitchell, N.J.; Gratz, J.; Houpt, E.R.; Gong, Y.; Egner, P.A.; Groopman, J.D.; Riley, R.T.; Showker, J.L.; Svensen, E.; et al. Exposure to aflatoxin and fumonisin in children at risk for growth impairment in rural Tanzania. Environ. Int. 2018, 115, 29–37. [Google Scholar] [CrossRef]
- Food and Agriculture Organization. Guidelines for Measuring Household and Individual Dietary Diversity. 2010. Available online: https://www.fao.org/3/i1983e/i1983e00.pdf (accessed on 10 March 2024).
- Mollay, C.; Kassim, N.; Stoltzfus, R.; Kimanya, M. Complementary feeding in Kongwa, Tanzania: Findings to inform a mycotoxin mitigation trail. Matern. Child Nutr. 2021, 17, e13188. [Google Scholar] [CrossRef] [PubMed]
- Gichohi-Wainaina, W.N.; Kimanya, M.; Muzanila, Y.C.; Kumwenda, N.C.; Msere, H.; Rashidi, M.; Mponda, O.; Okori, P. Aflatoxin Contamination, Exposure among Rural Smallholder Farming Tanzanian Mothers and Associations with Growth among Their Children. Toxins 2023, 15, 257. [Google Scholar] [CrossRef] [PubMed]
- Ochieng, J.; Afari-Sefa, V.; Lukumay, P.J.; Dubois, T. Determinants of dietary diversity and the potential role of men in improving household nutrition in Tanzania. PLoS ONE 2017, 12, e0189022. [Google Scholar] [CrossRef] [PubMed]
- Kulwa, K.B.M.; Mamiro, P.S.; Kimanya, M.E.; Mziray, R.; Kolsteren, P.W. Feeding practices and nutrient content of complementary meals in rural central Tanzania: Implications for dietary adequacy and nutritional status. BMC Pediatr. 2015, 15, 171. [Google Scholar] [CrossRef]
- Vitta, B.S.; Benjamin, M.; Pries, A.M.; Champeny, M.; Zehner, E.; Huffman, S.L. Infant and young child feeding practices among children under 2 years of age and maternal exposure to infant and young child feeding messages and promotions in Dar es Salaam, Tanzania. Matern. Child Nutr. 2016, 12, 77–90. [Google Scholar] [CrossRef]
- Kinabo, J.L.; Mwanri, A.W.; Mamiro, P.S.; Kulwa, K.; Bundala, N.H.; Picado, J.; Msuya, J.; Ntwenya, J.; Nombo, A.; Mzimbiri, R.; et al. Infant and young child feeding practices on Unguja Island in Zanzibar, Tanzania: A ProPAN based analysis. Tanzan. J. Health Res. 2017, 19, 1–9. [Google Scholar] [CrossRef]
- Ntwenya, J.E.; Kinabo, J.; Msuya, J.; Mamiro, P.; Majili, Z.S. Dietary patterns and household food insecurity in rural populations of Kilosa district, Tanzania. PLoS ONE 2015, 10, e0126038. [Google Scholar] [CrossRef]
- Sunguya, B.F.; Zhu, S.; Paulo, L.S.; Ntoga, B.; Abdallah, F.; Assey, V.; Mpembeni, R.; Huang, J. Regional Disparities in the Decline of Anemia and Remaining Challenges among Children in Tanzania: Analyses of the Tanzania Demographic and Health Survey 2004–2015. Int. J. Environ. Res. Public Health 2020, 17, 3492. [Google Scholar] [CrossRef]
- Mgongo, M.; Chotta, N.A.S.; Hashim, T.H.; Uriyo, J.G.; Damian, D.J.; Stray-Pedersen, B.; Msuya, S.E.; Wandel, M.; Vangen, S. Underweight, Stunting and Wasting among Children in Kilimanjaro Region, Tanzania; a Population-Based Cross-Sectional Study. Int. J. Environ. Res. Public Health 2017, 14, 509. [Google Scholar] [CrossRef]
- McDonald, C.M.; Kupka, R.; Manji, K.P.; Okuma, J.; Bosch, R.J.; Aboud, S.; Kisenge, R.; Spiegelman, D.; Fawzi, W.W.; Duggan, C.P. Predictors of stunting, wasting and underweight among Tanzanian children born to HIV-infected women. Eur. J. Clin. Nutr. 2012, 66, 1265–1276. [Google Scholar] [CrossRef]
- Thurstans, S.; Opondo, C.; Seal, A.; Wells, J.; Khara, T.; Dolan, C.; Briend, A.; Myatt, M.; Garenne, M.; Sear, R.; et al. Boys are more likely to be undernourished than girls: A systematic review and meta-analysis of sex differences in undernutrition. BMJ Glob. Health 2020, 5, e004030. [Google Scholar] [CrossRef] [PubMed]
- Thurstans, S.; Opondo, C.; Seal, A.; Wells, J.; Khara, T.; Dolan, C.; Briend, A.; Myatt, M.; Garenne, M.; Sear, R.; et al. Understanding Sex Differences in Childhood Undernutrition: A Narrative Review. Nutrients 2022, 14, 948. [Google Scholar] [CrossRef] [PubMed]
- Mboya, I.B.; Mamseri, R.; Leyaro, B.J.; George, J.; Msuya, S.E.; Mgongo, M. Prevalence and factors associated with anemia among children under five years of age in Rombo district, Kilimanjaro region, Northern Tanzania. F1000res. 2020, 9, 1102. [Google Scholar] [CrossRef] [PubMed]
- Gewa, C.A.; Yandell, N. Undernutrition among Kenyan children: Contribution of child, maternal and household factors. Public Health Nutr. 2012, 15, 1029–1038. [Google Scholar] [CrossRef]
- WHO. Addressing Sex and Gender in Epidemic-Prone Infectious Diseases, WHO, Geneva, Switzerland. 2007. Available online: https://iris.who.int/bitstream/handle/10665/43644/9789241595346_eng.pdf (accessed on 10 March 2024).
- Elisaria, E.; Kuwawenaruwa, A.; Nkuba, E. Malnutrition and stunting in Tanzania Trends and Policies. Thrive, Oxford Policy Management. 2024. Available online: https://thrivechildevidence.org/resource-centre/malnutrition-and-stunting-in-tanzania-trends-and-policies/ (accessed on 20 May 2025).
- Mohhamed, T.M.; Nyaruhucha, C.N. Household and Community Factors Affecting Nutritional Status of Under-five Children (6–59 months) in Gairo District Using Composite Index of Anthropometric Failure. Tanzan. J. Sci. 2023, 49, 76–85. [Google Scholar] [CrossRef]
- Yisak, H.; Gobena, T.; Mesfin, F. Prevalence and risk factors for under nutrition among children under five at Haramaya district, Eastern Ethiopia. BMC Pediatr. 2015, 15, 212. [Google Scholar] [CrossRef]
- Moshi, C.C.; Sebastian, P.J.; Mushumbusi, D.G.; Azizi, K.A.; Meghji, W.P.; Kitunda, M.E.; Kasankala, L.M. Determinants of underweight among children aged 0–23 months in Tanzania. Food Sci. Nutr. 2022, 10, 1167–1174. [Google Scholar] [CrossRef]
- Khamis, A.G.; Mwanri, A.W.; Ntwenya, J.E.; Kreppel, K. The influence of dietary diversity on the nutritional status of children between 6 and 23 months of age in Tanzania. BMC Pediatr. 2019, 19, 518. [Google Scholar] [CrossRef]
- Givens, D.I. Milk Symposium review. The importance of milk and dairy foods in the diets of infants, adolescents, pregnant women, adults and the elderly. J. Dairy Sci. 2020, 103, 9681–9699. [Google Scholar] [CrossRef]
- Stephen, A.; Alles, M.; de Graaf, C.; Fleith, M.; Hadjilucas, E.; Isaacs, E.; Maffeis, C.; Zeinstra, G.; Matthys, C.; Gil, A. The role and requirements of digestible dietary carbohydrates in infants and toddlers. Eur. J. Clin. Nutr. 2012, 66, 765–779. [Google Scholar] [CrossRef]
- Chaparro, C.M. Setting the Stage for Child Health and Development: Prevention of Iron Deficiency in Early Infancy. J. Nutr. 2008, 138, 2529–2533. [Google Scholar] [CrossRef] [PubMed]
- Cook, J.D.; Reddy, M.B.; Burri, J.; Juillerat, M.A.; Hurrell, R.F. The influence of different cereal grains on iron absorption from infant cereal foods. Am. J. Clin. Nutr. 1997, 65, 964–969. [Google Scholar] [CrossRef] [PubMed]
- Adongo, A.O.; Matofari, J.W.; Mbuthia, E. Dietary diversity among children aged 6–59 months from settled pastoral communities in Marsabit County, Kenya. Afr. J. Food Agric. Nutr. Dev. 2024, 24, 26554–26582. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).