Abstract
To assess temporal changes to the risk of death in COVID-19 cases caused by the Omicron variant, we calculated age-standardized case fatality rates (CFR) in patients aged ≥40 years over nine diagnostic periods (3 January to 28 August 2022) in ten Japanese prefectures (14.8 million residents). Among 552,581 study subjects, we found that there were 1836 fatalities during the isolation period (up to 28 days from date of onset). The highest age-standardized CFR (0.85%, 95% confidence interval (CI):0.78–0.92) was observed in cases diagnosed in the second 4-week period (January 31 to February 27), after which it declined significantly up to the 6th 4-week period (0.23%, 95% CI: 0.13–0.33, May 23 to June 19). The CFR then increased again but remained at 0.39% in the eighth period (July 18 to August 28). The CFR in cases with the BA.2 or BA.5 sublineages in the age range 60–80 years was significantly lower than that with BA.1 infections (60 years: 0.19%, 0.02%, 0.053%, respectively; 70 years: 0.91%, 0.33%, 0.39%; ≥80 years: 3.78%, 1.96%, 1.81%, respectively). We conclude that the risk of death in Japanese COVID-19 patients infected with Omicron variants declined through February to mid-June 2022.
1. Introduction
Since the Omicron (B.1.1.529) variant of SARS-CoV-2 was first reported in South Africa on 24 November 2021 [1], it became widely distributed, and by late January, 2022, it was the most prevalent lineage globally, representing 85% of variant cases reported [2]. Japan also experienced a rapid replacement of the Delta variant of concern (VOC) with Omicron, reaching 94% of total newly-detected COVID19 cases by 10–16 January 2022 [3] (Figure A1).
In contrast to its strong infectivity [4,5], a number of epidemiological studies indicated that the clinical severity of infection with the Omicron VOC was lower than with the Delta VOC [6,7,8,9,10,11,12]. However, the clinical severity in the COVID-19 cases was probably influenced not only by the nature of the viral variant but also by booster vaccine coverage [6,13,14,15,16], medical accessibility, availability of novel oral antiviral treatments and life expectancy before the pre-COVID-19 era in the population. The frequency of infection by the BA.1 Omicron sublineage was overtaken by the BA.2 sublineage in April, which was subsequently replaced by BA.5 in late July, being responsible for 97% of the total newly-detected COVID19 cases between 15 and 21 August 2022 in Japan [3] (Figure A1).
These differences in viral sublineage penetration are thought to have altered the pattern of clinical severity of cases with the Omicron variant, thus affecting the case fatality rate (CFR) in the Japanese population. CFR has a very important influence on COVID-19 public health policy decision-making. Davies, M.-A. et al. compared the clinical severity of Omicron BA.4/BA.5 infection with BA.1 in South Africa and concluded that severe hospitalization or risk of death was similar for BA.4/BA.5 and BA.1 infections [17]. However, little is known about the real-world temporal changes of the CFR in cases of infection with different Omicron variants in Japan. Therefore, we aimed to assess the changing case fatality rate of COVID-19 caused by Omicron between January and August 2022 in the Japanese population.
2. Materials and Methods
2.1. Data Source
All instances of test-confirmed COVID-19 were required to be reported by the physician to the Public Health Center (a branch of local government) up until 25 September 2022, adhering to the Infectious Diseases Control Law. Most patients were diagnosed by a test for COVID-19 in an outpatient consultation or at hospital admission. Japanese hospitals test almost all patients for COVID-19 before admission for the purpose of prevention of infection spread in hospitals. Antigen tests were approved on 13 May 2020 and had been already distributed in Japan [18]. Individuals who underwent autopsy were tested. The study team collaborated with 10 prefectures (Gunma, Ibaraki, Nagano, Shiga, Gifu, Osaka, Tokushima, Saga, Nagasaki, and Miyazaki) with a total population of 14.84 million residents. We identified study subjects aged ≥40 years of age with newly test-confirmed COVID-19 between 3 January 2022 (the first date of the first week in 2022) and 28 August 2022 (the last date of the 9th week in 2022). Since the case fatality rate among COVID-19 cases with the Omicron variant aged 39 years and younger was considered to be very low [6], we only included cases for those aged 40 years and over in this trend investigation. Japan experienced a sixth endemic wave that was mainly caused by the BA.1 Omicron sublineage and a seventh endemic wave due to the BA.5 sublineage (Figure 1 and Figure A1).
According to their clinical status, all the SARS-CoV-2-positive symptomatic cases were required to isolate at home, stay in a residence made available by the local government, or in hospital for at least 10 days from the onset and for 72 h after symptom resolution. All test-positive asymptomatic cases were also required to isolate at home for 7 to 10 days. If such asymptomatic cases acquired any symptoms during their isolation period, they were also required to isolate for 72 h after symptom disappearance. Public health nurses in the Japanese public health system monitored the health status of the isolated COVID-19 cases in their jurisdiction mainly using ICT. Death certificates were required to be made out by the physician according to the Infectious Diseases Control Law during the isolation period, regardless of the actual cause of death. This report was sent to the public health center of the jurisdiction in which the deceased had lived. Study subjects were passively followed up until the end of their isolation, date of death, or 28 days after the COVID-19 diagnosis (whichever occurred first) by infectious control departments within the participating public health centers.
The Ibaraki Prefecture Epidemiological Research Joint Ethics Review Committee approved this study.
2.2. Calculation of Case Fatality Rate
The case fatality rate (CFR) was calculated using deceased patients as the numerator. We stratified study subjects into 9 subgroups according to the time of COVID-19 diagnosis, beginning from the first 4 weeks (3 to 31 January) through to the 8th 4-week period (18 July to 14 August) and the final 2 weeks (15 to 28 August) in 2022. To characterize the temporal change in the CFR among Japanese COVID-19 patients with the Omicron variant, we calculated age-standardized CFR and its 95% confidence interval [19] using the Japanese population aged ≥40 years in 2022.
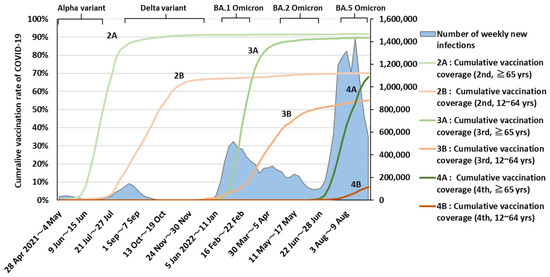
Figure 1.
Trends in cumulative vaccination coverage and number of weekly new instances of COVID-19 in Japan. Data on the number of weekly new infections were obtained from the Ministry of Health, Labour and Welfare. Cumulative vaccination rate data were obtained from the Prime Minister’s Office of Japan [20]. Graph indicates dominant period (≧85%).
To compare age-specific CFR between COVID-19 cases with BA.1, BA.2, or BA.5 sublineage infections, we compared study subjects diagnosed between 3 January and 20 March (a period during which BA.1 was dominant) with those diagnosed 25 April to 19 June (BA.2 dominant) and those diagnosed 18 July to 28 August (BA.5 dominant), representing the subvariant distribution of ≥95% in COVID-19 patients in Japan at those times [3].
2.3. Causes of Death
We distinguished COVID-19-related or non-related death or causes unknown. Death related to COVID-19 was defined as having occurred in patients with dyspnea, pneumonia, and hypoxia (<93% oxygen saturation) or a physician’s diagnosis of death from COVID-19. On the other hand, COVID-19 non-related death was determined from the physician’s diagnosis of death from non-COVID-19 disease or sudden death without any pulmonary symptoms. We calculated the proportion of deaths associated with COVID-19 among all the deaths with known causes within in each of the 9 diagnostic time periods.
3. Results
We extracted data on 552,581 COVID-19 cases diagnosed between 3 January and 28 August 2022 (Table A1). The highest age-standardized CFR (0.85%, 95% confidence interval (CI): 0.78–0.92) was estimated for cases diagnosed in the second 4-week period (31 January to 27 February). The CFR then declined significantly in the 6th 4-week period (0.23%, 95% CI: 0.13–0.33, 23 May to 19 June) (Figure 2). The rate then increased again but remained lower than it was earlier, at 0.39% in the 8th 4-week period (18 July to 28 August). Figure 3 presents trends in the proportion of deaths associated with COVID-19 among all deceased cases with known causes of death. The highest proportion is seen in cases diagnosed in the 3rd 4-week period (83.3%, 95% CI:77.0%–89.7%). This began to decline for cases diagnosed in the 5th period (53.8%, 95% CI:26.7%–80.9%), although this did not reach statistical significance.
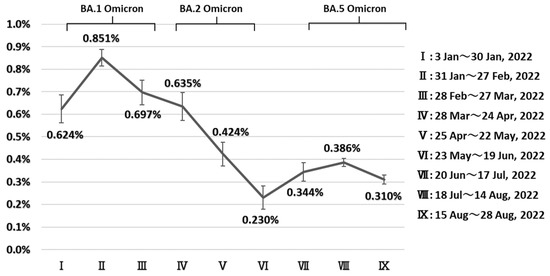
Figure 2.
Trends in age-standardized fatality rate in patients aged 40 years infected with the Omicron variant diagnosed between 3 January and 28 August 2022, in Japan. Age-standardization was performed using the whole Japanese population aged 40 years in 2022. Graph indicates dominant period (≧85%).
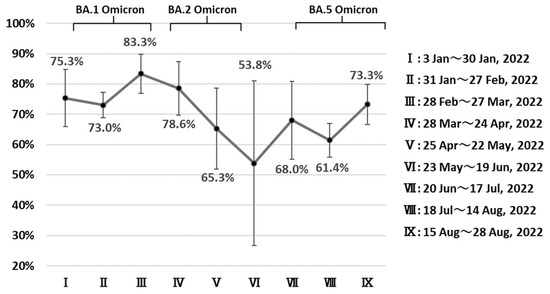
Figure 3.
Trend in the proportion of deaths with COVID-19 among deceased individuals aged ≥40 years who were diagnosed with COVID-19 between 3 January and 28 August 2022, in Japan. Graph Indicates dominant period (≧85%).
The age-specific CFRs for cases with the BA.1 sublineage at ten-year intervals from 40, 50, 60, 70 and ≥80 years were 0.007%, 0.06%, 0.19%, 0.91% and 3.78%, respectively (Figure 4). The CFRs for cases with BA.2 sublineage infections at age 60–70, 70–80 and >80 years (0.02%, 0.33% and 1.96%, respectively) were significantly lower than for BA.1 sublineage infections. Finally, the CFRs in cases infected with BA.5 grouped at ten-year intervals from 50 to ≥80 years of age (0.026%, 0.053%, 0.39% and 1.81%, respectively) were significantly lower than in those with BA.1 sublineage infections in the corresponding age group (Figure 4).
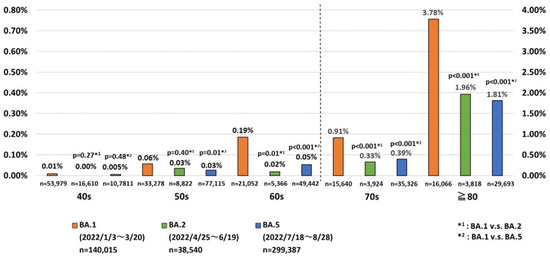
Figure 4.
Comparison of fatality rates among Japanese COVID-19 cases infected with one of three sublineages of the Omicron variant in 2022.
4. Discussion
At the introduction of the vaccine, the government decided to give priority to the elderly (≧65 years) (Figure 1) and health care workers. The government of Japan has implemented policies regarding vaccination and antivirals to reduce the fatality rate of COVID-19. BNT162b2 (Pfizer–BioNTech) was approved by the government on 14 February 2021 and was deployed on 17 February 2021 [21,22]. On 21 May 2021, ChAdOx1 nCoV-19 (AstraZeneca) and mRNA-1273 (Moderna) were approved [23]. On 19 April 2022, NVX-CoV2373 (Novavax) was approved [24]. Molnupiravir was approved by the government on 3 December 2021, and the combination of Nirmatrelvir and Ritonavir was approved on 14 January 2022 [25,26]. Our study revealed that the risk of death among COVID-19 cases with the Omicron variant in Japan changed markedly between January and August, 2022. The highest CFR as observed in cases diagnosed from 31 January to 27 February. Japan faced the endemic peak of BA.1 Omicron from 2 to 8 February [27]. Hospital admission rates for COVID-19 patients declined from 14.2% on January 12 to 3.2% on February 9 because of the shortage of in-patient capacity, which possibly affected full accessibility to medical care in COVID-19 patients who actually needed admission [28].
The risk of death started to decrease in March and was reduced to less than one-third in late May to mid-June, relative to earlier in the year. What accounted for this trend? One explanation is likely the timing of increasing SARS-CoV-2 vaccination rates among Japanese aged 65 and over [20] (Figure 1). All Japanese local governments conducted booster COVID-19 vaccination campaigns starting in mid-January, 2022; the cumulative vaccination rate reached 80% by mid-March [20]. Previous COVID-19 vaccine studies showed that protection against infection declines 1 to 2 months after vaccination, whereas protection against severe disease is maintained for much longer [6,13,29]. Therefore, it is plausible that the efficacy of the third COVID-19 vaccination in older Japanese adults in terms of avoiding very severe disease would manifest itself 2 to 3 months after vaccination (i.e., the time when susceptibility to infection is increasing again). The trend for declining proportions of COVID-19-related deaths among all cases seen in essentially the same period may support this notion.
We compared the age-specific risk of death in our cases with BA.1 Omicron cases in a study in England [6] which investigated death within 28 days after confirmed infection between 29 November 2021 and 9 January 2022. This revealed a similar situation in the two studies, at least regarding cases for patients in the 40-to-70 age range [6]. However, the risk of death in people aged 80 and over was significantly lower in Japan than in England (3.78% vs. 5.12%). The lower risk observed in the Japanese may possibly be at least in part attributed to the longer life expectancy before the COVID-19 pandemic in 80-year-old Japanese (10.35 vs. 9.03 year in 2015) [30].
The risk of death for cases with BA.5 sublineage infections was significantly lower than for cases with BA.1 at age ≥50 years. This was possibly associated with the increasing COVID-19 vaccination rate (Figure 1), seasonal variation in mortality driven by temperature [31,32], and increasing availability of Molnupiravir and the combination of Nirmatrelvir and Ritonavir this year [25,26] in Japan. Although our descriptive epidemiological approach cannot estimate the impact of the pathogenicity of Omicron sublineage mutants, the low risk of death in patients with BA.5 infections observed in this study may change our view of COVID-19. Countries formulate policies on infection control by considering the impact of COVID-19 on public health and social economic activities. We need to think about the impact on public health in terms of lower current fatality rates.
This study does have some limitations. First, asymptomatic individuals would have been less likely to have been diagnosed than symptomatic patients during the peak endemic period because they would have had less opportunity to be tested under the then-prevailing conditions of insufficient accessibility to testing. This might have induced selection bias that would have increased the apparent risk of death among cases diagnosed in the second and eighth 4-week periods (diagnosed at the peak incidence in the endemic waves) (Figure 1). Second, our data source did not contain individualized information on COVID-19 variants nor Omicron sublineages. Therefore, some misclassification of the sublineage infection was inevitable. However, because we defined sublineage in the study groups based on the time of the dominant penetration of one of the sublineages (≧95%) according to sampling and testing populations from the whole of Japan Figure A1 [3], we believe that the effects of any such misclassification on the risk of death would be minimal.
Third, as this study design is a descriptive epidemiology that assess the changing Japanese CFR of COVID-19 caused by Omicron, we did not elucidate factors associated with the changing of CFR. Further analytical studies are needed to explore it. Fourth, the accuracy in determining the causes of death was modest because the majority of the COVID-19 cases in this period were isolated in their home or residence provided by the local governments but not in hospital. When the case was isolated in their home or residence, the doctor was less likely to grasp his/her clinical course from the onset. Therefore, the deceased cases who had been isolated at their home or residence possibly had less opportunity to receive a detailed examination, which might have affected the accuracy in determining causes of death. However, as this situation was the same throughout the study period, the influence of this inaccuracy on the proportion of COVID-19-related deaths among the deceased cases would be modest.
5. Conclusions
Our analysis shows that the risk of death in patients infected with the Omicron variant declined significantly in Japan in 2022. A very low CFR in cases with BA.5 sublineage infection would change the recognition of this disease as a high-risk pathogen in this country.
Author Contributions
Conceptualization and methodology, H.T.; software, Y.T.; validation and formal analysis, H.T.; investigation, Y.T.; resources and data curation, Y.T., H.T., Y.K., S.T., S.O., S.I., H.M., Y.M., T.T., F.I., Y.B., F.Y., T.S. (Tomoyuki Suzuki), I.A., C.S., S.M., M.S., T.S. (Toshiyuki Shibata), H.N., M.K. and R.F.; writing—original draft preparation, Y.T. and H.T.; writing—review and draft preparation, Y.T., H.T. and T.O.; visualization, Y.T.; supervision, T.O.; administration, Y.T. and H.T.; funding acquisition, H.T. All authors have read and agreed to the published version of the manuscript.
Funding
This study was financially supported by a grant-in-aid for “Public Health Research on COVID-19 in Comprehensive Programs on Community Health” sponsored by the Ministry of Health, Labour and Welfare, Japan.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by The Ibaraki Prefecture Epidemiological Research Joint Ethics Review Committee (R3-11).
Informed Consent Statement
Informed consent was not required from the patients and contacts because the active epidemiological investigation data analyses were performed in accordance with the Infectious Diseases Control Law.
Data Availability Statement
The data presented here is not publicly available due to the privacy policy of the Cooperated Prefectural and Municipal Governments.
Acknowledgments
The authors thank the infection control staff of PHC of Cooperated Prefectural and Municipal Government for releasing the data required for our study.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A
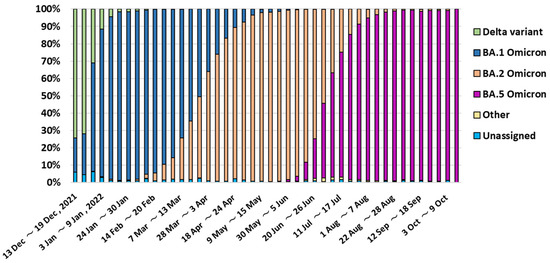
Figure A1.
Trends in the changing proportions of the lineage of SARS-CoV-2 in Japan (December 2021~October 2022). These data were obtained from the National Institute of Infectious Diseases [3].

Table A1.
Age-standardized fatality rate of COVID-19 cases aged ≥40 years caused by the Omicron variant diagnosed between January and August in Japan, 2022.
Table A1.
Age-standardized fatality rate of COVID-19 cases aged ≥40 years caused by the Omicron variant diagnosed between January and August in Japan, 2022.
| Diagnosed Period | Number of Cases | Number of Death | Age-Standardized Fatality Rate | 95%CI (Lower-Upper) |
|---|---|---|---|---|
| I (3 January~30 January 2022) | 27,674 | 108 | 0.624% | (0.563%–0.685%) |
| II (31 January~27 February 2022) | 80,101 | 557 | 0.851% | (0.814%–0.888%) |
| III (28 February~27 March 2022) | 39,303 | 169 | 0.697% | (0.642%–0.752%) |
| IV (28 March~24 April 2022) | 34,113 | 110 | 0.635% | (0.572%–0.697%) |
| V (25 April~22 May 2022) | 24,358 | 71 | 0.424% | (0.371%–0.477%) |
| VI (23 May~19 June 2022) | 14,182 | 21 | 0.230% | (0.179%–0.281%) |
| VII (20 June~17 July 2022) | 33,463 | 72 | 0.344% | (0.302%–0.385%) |
| VIII (18 July~14 August 2022) | 182,366 | 474 | 0.386% | (0.368%–0.404%) |
| IX (15 August~28 August 2022) | 117,021 | 254 | 0.310% | (0.290%–0.330%) |
Age—standardization was performed using Japanese population aged 40 and over in 2022.

Table A2.
Proportion of deaths with COVID-19 among deceased individuals aged ≥40 years who were diagnosed with COVID-19 between 3 January and 28 August 2022, in Japan.
Table A2.
Proportion of deaths with COVID-19 among deceased individuals aged ≥40 years who were diagnosed with COVID-19 between 3 January and 28 August 2022, in Japan.
| Diagnosed Period | Cases of COVID-19 Related Deaths | Cases of COVID-19 Non-Related Deaths | Cause of Death Not Known | Total |
|---|---|---|---|---|
| Ⅰ (3 January~30 January 2022) | 61 | 20 | 27 | 108 |
| Ⅱ (31 January~27 February 2022) | 314 | 116 | 127 | 557 |
| Ⅲ (28 February~27 March 2022) | 110 | 22 | 37 | 169 |
| Ⅳ (28 March~24 April 2022) | 66 | 18 | 26 | 110 |
| Ⅴ (25 April~22 May 2022) | 32 | 17 | 22 | 71 |
| Ⅵ (23 May~19 June 2022) | 7 | 6 | 8 | 21 |
| Ⅶ (20 June~17 July 2022) | 34 | 16 | 22 | 72 |
| Ⅷ (18 July~14 August 2022) | 183 | 115 | 176 | 474 |
| Ⅸ (15 August~28 August 2022) | 126 | 46 | 82 | 254 |

Table A3.
Fatality rates of COVID-19 cases caused by one of three sublineages of the Omicron variant in Japan, 2022 (40s, 50s, 60s, 70s and ≧80 years).
Table A3.
Fatality rates of COVID-19 cases caused by one of three sublineages of the Omicron variant in Japan, 2022 (40s, 50s, 60s, 70s and ≧80 years).
| BA.1(B.1.1.529.1) *1 | BA.2(B.1.1.529.2) *2 | BA.5(B.1.1.529.5) *3 | p-Value (1) *4 | p-Value (2) *4 | |
|---|---|---|---|---|---|
| 40s | 4/53979 (0.00741%) | 0/16610 (0.00%) | 5/107811 (0.00464%) | 0.27 | 0.48 |
| 50s | 19/33278 (0.0571%) | 3/8822 (0.0340%) | 20/77115 (0.0259%) | 0.40 | 0.01 |
| 60s | 39/21052 (0.185%) | 1/5366 (0.0186%) | 26/49442 (0.0526%) | 0.01 | <0.001 |
| 70s | 143/15640 (0.914%) | 13/3924 (0.331%) | 139/35326 (0.393%) | <0.001 | <0.001 |
| ≧80 | 607/16066 (3.78%) | 75/3818 (1.96%) | 538/29693 (1.81%) | <0.001 | <0.001 |
*1 3 January~20 March 2022, *2 5 April~19 June 2022, *3 18 July~28 August 2022, *4 Equality of proportions hypothesis test (1) Difference between BA.1 and BA.2 (2) Difference between BA.1 and BA.5.
References
- World Health Organization. Classification of Omicron (B.1.1.529): SARS-CoV-2 Variant of Concern. Available online: https://www.who.int/news/item/26-11-2021-classification-of-omicron-(b.1.1.529)-sars-cov-2-variant-of-concern (accessed on 11 December 2022).
- GISAID. Tracking of HCoV-19 Variants. Available online: https://www.re3data.org/repository/r3d100010126 (accessed on 11 December 2022).
- National Institute of Infectious Diseases. About SARS-CoV-2 Variants. Available online: https://www.niid.go.jp/niid/ja/2019-ncov/2551-cepr/10745-cepr-topics.html (accessed on 11 December 2022).
- Ogata, T.; Tanaka, H.; Tanaka, E.; Osaki, N.; Noguchi, E.; Osaki, Y.; Tono, A.; Wada, K. Increased Secondary Attack Rates among the Household Contacts of Patients with the Omicron Variant of the Coronavirus Disease 2019 in Japan. Int. J. Environ. Res. Public Health 2022, 19, 8068. [Google Scholar] [CrossRef] [PubMed]
- Jørgensen, S.B.; Nygård, K.; Kacelnik, O.; Telle, K. Secondary Attack Rates for Omicron and Delta Variants of SARS-CoV-2 in Norwegian Households. JAMA 2022, 327, 1610–1611. [Google Scholar] [CrossRef] [PubMed]
- Nyberg, T.; Ferguson, N.M.; Nash, S.G.; Webster, H.H.; Flaxman, S.; Andrews, N.; Hinsley, W.; Bernal, J.L.; Kall, M.; Bhatt, S.; et al. Comparative Analysis of the Risks of Hospitalisation and Death Associated with SARS-CoV-2 Omicron (B.1.1.529) and Delta (B.1.617.2) Variants in England: A Cohort Study. Lancet 2022, 399, 1303–1312. [Google Scholar] [CrossRef] [PubMed]
- Auvigne, V.; Vaux, S.; Strat, Y.L.; Schaeffer, J.; Fournier, L.; Tamandjou, C.; Montagnat, C.; Coignard, B.; Levy-Bruhl, D.; Parent du Châtelet, I. Severe Hospital Events Following Symptomatic Infection with Sars-CoV-2 Omicron and Delta Variants in France, December 2021–January 2022: A Retrospective, Population-Based, Matched Cohort Study. eClinicalMedicine 2022, 48, 101455. [Google Scholar] [CrossRef] [PubMed]
- Abdullah, F.; Myers, J.; Basu, D.; Tintinger, G.; Ueckermann, V.; Mathebula, M.; Ramlall, R.; Spoor, S.; de Villiers, T.; Van der Walt, Z.; et al. Decreased Severity of Disease during the First Global Omicron Variant Covid-19 Outbreak in a Large Hospital in Tshwane, South Africa. Int. J. Infect. Dis. 2022, 116, 38–42. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Liu, B.; Zhang, S.; Huang, N.; Zhao, T.; Lu, Q.-B.; Cui, F. Differences in Incidence and Fatality of COVID-19 by SARS-CoV-2 Omicron Variant versus Delta Variant in Relation to Vaccine Coverage: A World-Wide Review. J. Med. Virol. 2022. [Google Scholar] [CrossRef] [PubMed]
- Esper, F.P.; Adhikari, T.M.; Tu, Z.J.; Cheng, Y.-W.; El-Haddad, K.; Farkas, D.H.; Bosler, D.; Rhoads, D.; Procop, G.W.; Ko, J.S.; et al. Alpha to Omicron: Disease Severity and Clinical Outcomes of Major SARS-CoV-2 Variants. J. Infect. Dis. 2022, 227, 344–352. [Google Scholar] [CrossRef] [PubMed]
- Sheikh, A.; Kerr, S.; Woolhouse, M.; McMenamin, J.; Robertson, C.; Simpson, C.R.; Millington, T.; Shi, T.; Agrawal, U.; Shahul Hameed, S.; et al. Severity of Omicron Variant of Concern and Effectiveness of Vaccine Boosters against Symptomatic Disease in Scotland (EAVE II): A National Cohort Study with Nested Test-Negative Design. Lancet Infect. Dis. 2022, 22, 959–966. [Google Scholar] [CrossRef] [PubMed]
- Xue, L.; Jing, S.; Zhang, K.; Milne, R.; Wang, H. Infectivity versus Fatality of SARS-CoV-2 Mutations and Influenza. Int. J. Infect. Dis. 2022, 121, 195–202. [Google Scholar] [CrossRef] [PubMed]
- Gram, M.A.; Emborg, H.-D.; Schelde, A.B.; Friis, N.U.; Nielsen, K.F.; Moustsen-Helms, I.R.; Legarth, R.; Lam, J.U.H.; Chaine, M.; Malik, A.Z.; et al. Vaccine Effectiveness against SARS-CoV-2 Infection or COVID-19 Hospitalization with the Alpha, Delta, or Omicron SARS-CoV-2 Variant: A Nationwide Danish Cohort Study. PLoS Med. 2022, 19, e1003992. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, U.; Bedston, S.; McCowan, C.; Oke, J.; Patterson, L.; Robertson, C.; Akbari, A.; Azcoaga-Lorenzo, A.; Bradley, D.T.; Fagbamigbe, A.F.; et al. Severe COVID-19 Outcomes after Full Vaccination of Primary Schedule and Initial Boosters: Pooled Analysis of National Prospective Cohort Studies of 30 Million Individuals in England, Northern Ireland, Scotland, and Wales. Lancet 2022, 400, 1305–1320. [Google Scholar] [CrossRef] [PubMed]
- McConeghy, K.W. Effectiveness of a Second COVID-19 Vaccine Booster Dose Against Infection, Hospitalization, or Death Among Nursing Home Residents—19 States, March 29–July 25, 2022. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 1235–1238. [Google Scholar] [CrossRef] [PubMed]
- Smith, D.J.; Hakim, A.J.; Leung, G.M.; Xu, W.; Schluter, W.W.; Novak, R.T.; Marston, B.; Hersh, B.S. COVID-19 Mortality and Vaccine Coverage—Hong Kong Special Administrative Region, China, January 6, 2022-March 21, 2022. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 545–548. [Google Scholar] [CrossRef] [PubMed]
- Davies, M.-A.; Kassanjee, R.; Rosseau, P.; Morden, E.; Johnson, L.; Solomon, W.; Hsiao, N.-Y.; Hussey, H.; Meintjes, G.; Paleker, M.; et al. Outcomes of Laboratory-Confirmed SARS-CoV-2 Infection in the Omicron-Driven Fourth Wave Compared with Previous Waves in the Western Cape Province, South Africa. medRxiv 2022. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health, Labour and Welfare Approval Information of a Medical Product for Extracorporeal Checks of New-Style Coronavirus Infectious Disease (Check Kit). Available online: https://www.mhlw.go.jp/stf/newpage_11331.html (accessed on 29 January 2023).
- Jacques, E.; Ellen, B.; Luc, R. Statistical Methods in Cancer Research Volume IV: Descriptive Epidemiology; The International Agency for Research on Cancer: Lyon, France, 1994; ISBN 978-92-832-2128-9. [Google Scholar]
- Prime Minister’s Office of Japan. COVID-19 Vaccines. Available online: https://japan.kantei.go.jp/ongoingtopics/vaccine.html (accessed on 11 December 2022).
- Ministry of Health, Labour and Welfare. General Information about the First Time Inoculation (It’s Inoculated the 1st Time the 2nd Time.). Available online: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000121431_00218.html (accessed on 31 January 2023).
- Ministry of Health, Labour and Welfare. About Special Case Approval of a New-Style Coronavirus Vaccine Based on a Medical Product Medical Device Mood. Available online: https://www.mhlw.go.jp/stf/newpage_16734.html (accessed on 29 January 2023).
- Ministry of Health, Labour and Welfare. About Special Case Approval of a New-Style Coronavirus Vaccine Based on a Medical Product Medical Device Mood. Available online: https://www.mhlw.go.jp/stf/newpage_18787.html (accessed on 31 January 2023).
- Ministry of Health, Labour and Welfare. About Making and Selling Approval of a New-Style Coronavirus Vaccine. Available online: https://www.mhlw.go.jp/stf/newpage_25294.html (accessed on 31 January 2023).
- Ministry of Health, Labour and Welfare. About Special Case Approval of New-Style Coronavirus Medicine. Available online: https://www.mhlw.go.jp/stf/newpage_23047.html (accessed on 11 December 2022).
- Ministry of Health, Labour and Welfare. About Special Case Approval of New-Style Coronavirus Medicine. Available online: https://www.mhlw.go.jp/stf/newpage_23815.html (accessed on 11 December 2022).
- Ministry of Health, Labour and Welfare. Visualizing the Data: Information on COVID-19 Infections. Available online: https://covid19.mhlw.go.jp/en/ (accessed on 11 December 2022).
- Ministry of Health, Labour and Welfare. About an Investigation about the Recuperation Situation etc. and the Inpatient Acceptance Number of Beds, etc. Available online: https://www.mhlw.go.jp/stf/seisakunitsuite/newpage_00023.html (accessed on 11 December 2022).
- Lin, D.-Y.; Gu, Y.; Xu, Y.; Wheeler, B.; Young, H.; Sunny, S.K.; Moore, Z.; Zeng, D. Association of Primary and Booster Vaccination and Prior Infection With SARS-CoV-2 Infection and Severe COVID-19 Outcomes. JAMA 2022, 328, 1415–1426. [Google Scholar] [CrossRef] [PubMed]
- knoema®. World and National Data, Maps & Ranking. Available online: https://jp.knoema.com/atlas (accessed on 11 December 2022).
- Madaniyazi, L.; Armstrong, B.; Chung, Y.; Ng, C.F.S.; Seposo, X.; Kim, Y.; Tobias, A.; Guo, Y.; Sera, F.; Honda, Y.; et al. Seasonal Variation in Mortality and the Role of Temperature: A Multi-Country Multi-City Study. Int. J. Epidemiol. 2022, 51, 122–133. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, H.; Shinjo, M.; Tsukuma, H.; Kawazuma, Y.; Shimoji, S.; Kinoshita, N.; Morita, T. Seasonal Variation in Mortality from Ischemic Heart Disease and Cerebrovascular Disease in Okinawa and Osaka: The Possible Role of Air Temperature. J. Epidemiol. 2000, 10, 392–398. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).