Abstract
The physical environment is of critical importance to child development. Understanding how exposure to physical environmental domains such as greenspace, urbanicity, air pollution or noise affects aggressive behaviours in typical and neurodiverse children is of particular importance given the significant long-term impact of those problems. In this narrative review, we investigated the evidence for domains of the physical environment that may ameliorate or contribute to the display of aggressive behaviours. We have considered a broad range of study designs that include typically developing and neurodiverse children and young people aged 0–18 years. We used the GRADE system to appraise the evidence. Searches were performed in eight databases in July 2020 and updated in June 2022. Additional articles were further identified by hand-searching reference lists of included papers. The protocol for the review was preregistered with PROSPERO. Results: We retrieved 7174 studies of which 67 are included in this review. The studies reported on green space, environmental noise and music, air pollution, meteorological effects, spatial density, urban or rural setting, and interior home elements (e.g., damp/sensory aspects/colour). They all used well validated parent and child reported measures of aggressive behaviour. Most of the studies were rated as having low or unclear risk of bias. As expected, noise, air pollution, urbanicity, spatial density, colour and humidity appeared to increase the display of aggressive behaviours. There was a dearth of studies on the role of the physical environment in neurodiverse children. The studies were heterogeneous and measured a range of aggressive behaviours from symptoms to full syndromes. Greenspace exposure was the most common domain studied but certainty of evidence for the association between environmental exposures and aggression problems in the child or young person was low across all domains. We found a large knowledge gap in the literature concerning neurodiverse children, which suggests that future studies should focus on these children, who are also more likely to experience adverse early life experiences including living in more deprived environments as well as being highly vulnerable to the onset of mental ill health. Such research should also aim to dis-aggregate the underlying aetiological mechanisms for environmental influences on aggression, the results of which may point to pathways for public health interventions and policy development to address inequities that can be relevant to ill health in neurodiverse young people.
1. Introduction
The physical environment encompasses all aspects of a child’s physical world and may be defined as objective characteristics of the physical context in which children spend their time (e.g., home, neighbourhood, school). The influence of children’s physical exposures has been summarised differentially by various models, theorems, and theorists over the previous century. Notably, these include the physical environmental elements of children’s exposome (a term introduced by Wild [1,2] regarding the non-genetic influences on outcomes across the lifespan) and Bronfenbrenner’s bioecological model [3,4,5], proposing that children develop within an environmental milieu of five interconnected systems, spanning aspects from urban design (e.g., presence and structure of sidewalks), traffic density, and design of venues for physical activity (e.g., playgrounds, parks, and school yards), to biologically active chemicals, radiation, the internal chemical environment, and psychosocial aspects [6]. The difficulty with these conceptualisations of child development is that they include both physical environmental and (psycho)social influences. As exemplified in a review of the influence of interior hospital environmental interior conditions, Harris [7] segmented the environment into distinct physical exposure categories: ambient, architectural, and interior design.
In this work, an operationalised definition of “physical environment” was incorporated to identify eligible environmental exposures. This classification was derived from a coalescence of Harris’s [7], Bronfenbrenner’s [3,4,5] and Wild’s [1,2] theorems. This resulted in the inclusion of a diverse array of domains, from ambient exposures (sunlight, sound, meteorology), interior design elements (colour, lighting), architectural features (space/spatial crowding), and biological active agents (i.e., air particulate pollutants), to physical aspects of children’s microsystem (i.e., home, school, and neighbourhood characteristics).
A variety of theories have attempted to explain the mechanisms via which environmental domains influence physical and mental health. Although none of these mechanistic models have been fully proven, there are suggestions that positive effects may be the end product of pathways that link several elements, such as mitigation (reduction in air pollution or traffic noise), restoration (stress reduction and attention restoration in alignment with what the Attention Restoration Theory posits) and instoration, whereby attributes of the physical environment, such as greenness in particular, may promote physical activity and social capital and cohesion [8,9,10].
Previous theories have primarily focused on the stress-reducing effects of greenspace, either via a protective influence from harmful environmental stimuli (noise and air pollution) [11,12,13], or via the restoration of attentional resources [14,15]. Recently, it has been posited that greenspaces may provide more direct physiological benefits via increased exposure to phytoncides (plant-derived antimicrobial volatile organic compounds) [16]. Whilst preliminary research into the effects of phytoncide exposure is positive, it is currently inconclusive and additional studies are required [17]. Neuroimaging studies are also shedding insight into potential mechanisms for greenspace exposures potential mechanisms, with one study [18] showing that it can beneficially deactivate the prefrontal cortex in regions linked to depression and rumination.
The literature also indicates that aspects such as ambient air particulate matter exposure may negatively impact development via neuroinflammatory pathways [19,20,21,22,23,24]. Noise pollution may also have detrimental effects via contributions to subjective annoyance and irritation; whilst not necessarily directly causing aggression, noise exposure in those with low threshold for expressing anger may increase its severity [25,26] via draining of attentional and cognitive resources and subsequently leading to increased self-regulatory difficulties [27]. Social-behavioural mechanisms may explain the relationship between behaviour and fluctuations in meteorological effects (such as temperature), e.g., the routine activity theory that proposes that warmer temperatures facilitate more frequent social interaction, increasing opportunity for aggression [28] or that heat increases hostility and physiological arousal and consequently to aggressive behaviour [29]. Theories have posited that high spatial density triggers perceptions of crowding and a subsequent physiological stress arousal response [30,31,32]. Why proximity elicits these responses is still unclear and has been linked to competition for resources and invasion of personal space [33]. Baird et al. [34] reported a beneficial association between household crowding and reduced conduct problems in children with intellectual disabilities. The authors propose several theories about these potentially counterintuitive findings, suggesting that increased availability of and proximity to family members, in intergenerational households, and parental habituation to problematic conduct behaviours are all potential mechanisms underpinning this finding. Using a sensory room unaccompanied may be associated with a sense of autonomy in children and young people which in turn reduces distress [35]. Other pathways may contribute to the impact that music listening has on a broad range of psychological and physiological benefits [36,37,38,39,40,41].
As discussed, social-behavioural mechanisms may explain the relationship between aggression and climate effects, for example the routine activity theory proposes that warmer temperatures facilitate more frequent social interaction, increasing opportunity for aggression [28]. Alternatively, the general aggression model (GAM) is more grounded in a physiological aetiology of aggression, suggesting that heat increases hostility and physiological arousal and consequently aggressive behaviours [29].
From the evidence presented so far, it appears that both physical and social environments, in addition to genetic and epigenetic influences, shape the developmental trajectories of children [42,43,44,45,46]. However, in the main, published research is focused on typically developing rather than neurodiverse children [47]. Previous work has evidenced disproportionate influence of children’s early environmental milieu in shaping a range of socio-emotional and cognitive developmental outcomes. Specifically, learning disabled children are more likely to be affected by social adversity, poor housing, and poverty [48]. These children are also exponentially more likely to be exposed to negative environmental exposures such as air pollution [49]. To address failings in supporting these children and their families, an important element is to reduce socioeconomic inequality and improve residential conditions [50]. Furthermore, children with complex neurodisabilities have increased barriers to accessing potentially therapeutic aspects of both the physical and social early environments [51]. Disabled child access to urban greenspaces, for example, is not only infrequent in comparison to their typically developing peers [52], but when significant resources are employed to facilitate access for neurodisabled children, the high-risk nature of visiting these spaces requires rigid structure, impacting on the quality of nature experiences when they do occur [53]. This is one example of the health inequities and disparities experienced by neurodiverse children in comparison to their peers, exemplifying the need for additional research in these domains.
Externalising disorders are characterised by display of a range of behaviours which are associated with poor impulse-control, and include rule breaking, impulsivity, and inattention; in addition, a core component of these conditions is the presence of heightened aggression.
Specific child and adolescent externalising disorders include conduct disorder (CD), oppositional defiant disorder (ODD), and attention- deficit-hyperactivity disorder (ADHD). Of particular concern is this repeated presence of aggressive behaviour in these disorders as it is often associated with referral to services and application of a range of restrictive practices, most commonly antipsychotic medications but also inpatient admissions.
Aggressive behaviours and general behavioural problems such as destructive behaviours have an overall negative influence on carers due to stress and negative interactions between carers and the person they care for, likely resulting in a deterioration of the quality of care [54]. Moreover, behavioural problems are associated with increased service costs because of the impact of behaviours on staff and need for high support levels [55]. Aggressive episodes also provoke concerns about threat to personal safety as well as cause panic and upset [56,57].
These behaviours in both typically developing and neurodiverse children compound societal and educational limitations [58,59,60,61]. They reduce life satisfaction via degradation of social and familial relationships [62], increase economic costs [63], require higher use of physical restraints [64] and restrictive environmental placements [65,66], limit access to support services [67], impair caregiver functioning [68,69], reduce educational opportunities due to teacher burnout [70] and encourage use of restrictive practices including psychotropic medication use [71,72].
Neurodevelopmental disorders (NDDs) are a category of “etiologically diverse conditions” with onset during the developmental period and are characterised by below average intellectual functioning and adaptive behaviour [73]. This classification includes disorders such as intellectual disability (also called learning disability in the UK), autism spectrum disorders (ASD), and other developmental delays (DD). Whilst we appreciate the nuances of the definitions for brevity and clarity, we will refer to those children with NDDs as neurodiversity in this context.
About one in one hundred individuals has a neurodevelopmental disorder and there are about 351,000 children with intellectual disability in the UK, often coexisting with other neurodevelopmental disorders [74]. Prevalence of aggressive behaviours in NDDs appears to fluctuate depending on sampling methods and assessment strategies, ranging from 8.3% in community samples [75] to 64% in inpatient care [76,77]. Children with intellectual disability were six times more likely to have conduct disorder measured by the Strengths and Difficulties Questionnaire compared to their typically developing peers [78]. Aggressive behaviours are persistent over time [79], with displays of aggression being consistently linked with neurodiversity [57,80,81,82,83,84,85] though prevalence rates reported can be inconsistent.
Whilst previous research has examined predictors of broadly defined challenging behaviour in children with intellectual disability [86,87,88], none of the studies has included examination of the influence of the physical environment specifically on such behaviours to date. Here, we build on previous work examining the influence of single domains of the physical environment on aggressive behaviour of typically developing and neurodiverse children by including (1) children across the spectrum of ability and (2) all available objective domains of the physical environment.
Therefore, in this narrative review, we examine the certainty of evidence of the impact of the physical environment on typically developing and neurodiverse children’s aggressive behaviours. The outcome of interest was either psychological or biological proxies of aggressive behaviour, annoyance and irritability measured by validated psychometric questionnaires (measures or outcomes which have been empirically evaluated for reliability) or biological markers such as blood pressure, heart rate and skin conductance. The findings are presented by environmental domain (Greenspace, noise pollution, air pollution, meteorology, spatial density, rurality of residence, interior design, and music) and separately for typically developing and neurodiverse children.
2. Materials and Methods
2.1. Search Strategy
We adhered to the Preferred Reporting Items of Systematic reviews and Meta-analyses (PRISMA) statement checklist [89] in conducting the review, as well as guidance from the Synthesis Without Meta-analysis [90], and the Meta-analysis of Observational Studies in Epidemiology [91] to improve the precision of our reporting. The study protocol was preregistered on PROSPERO (CRD42020160251). Because of the heterogeneity in outcome used and the variation in exposure measures, we were unable to perform a meta-analysis. Instead, we reported the degree of certainty of the evidence available in terms of protective/detrimental, inconclusivity, or no association for each outcome and exposure metric across each domain of the physical environment.
The electronic search strategy comprised 8 bibliographic databases (MEDLINE, PsychINFO, Web of Science, CHINAHLplus, Embase, Cochrane library, EThOS and ProQeust dissertations and theses) and two grey literature sources (NICE evidence search and Google scholar). The inclusion of the latter sources facilitated the retrieval of additional studies from a more diverse range of sources (including policy and public health), whilst mitigating publication bias and increasing the comprehensiveness of the review [92,93]. The search was carried out in July 2020, and replicated in the update to June 2022 with no year of publication limit. Bibliographies of retrieved articles were searched to maximise retrieval of relevant articles. The search strategy was overseen by a specialist librarian (see Supplementary Materials).
2.2. Selection Criteria
Studies were included if they (a) reported primary research, (b) were written in English, French, German, Mandarin Chinese and Spanish which were languages spoken by fellow researchers and therefore could be translated, (c) included human participants aged between 0–18 years, (d) contained a psychometrically valid parent or child reported outcome measure of aggressive behaviours or physiological measures of arousal (identified as a proxy measure of aggressive behaviour) and (e) examined exposure to domains of the physical environment.
2.3. Screening and Appraisal Process
All retrieved articles were screened by the first author (A.B.). A sub-sample of titles and abstracts (10%) were co-screened by a senior researcher (A.H.) and a post-doctoral researcher (R.R.). Inter-rater reliability for this initial screening was 87% (0.868). Full text data extraction was conducted by the main author (A.B.) using a modified flexible data extraction template used for non-Cochrane reviews [94] with co-screening conducted for a proportion of studies (59%) by independent researchers (see acknowledgments). Substantial agreement between the primary author and co-screeners was reported (83%, κ = 0.6126) with disagreements resolved by the senior researcher (A.H.) who also crosschecked the extraction table for any inconsistencies.
Risk of bias assessment (RoB) and GRADE protocol were adapted from a systematic review by Clark, Crumpler, and Notley [95] on the evidence relating to effects of environmental noise pollution on mental and physical health outcomes. Four items from this review were used to assess the bias for each paper:
- Evaluation of the quality and validity of the exposure: whether the paper used established or validated environment metrics.
- Bias due to confounding: whether studies included adjustment for potential confounding variables.
- Bias due to sampling methodology and reporting of attrition rate.
- Outcome assessment leading to information bias: whether studies were using validated aggressive behavioural outcome measure(s).
One measure of RoB that was not included in this review was “due to blinding to exposure outcome” as it was not considered appropriate for the methodology of the majority of the retrieved studies which infrequently blind outcome assessors. Overall RoB ratings for each study were aggregates of high, low or unclear across the four domains. We adopted a conservative rating strategy where studies that had equal reports of low and high risk of bias were classified as high.
The GRADE system [96] is a widely used tool recommended by The Cochrane collaboration [97] which provides a ranking of quality for evidence on interventions and relevant outcomes. The modified GRADE approach assigns a priori the highest quality of evidence to longitudinal or intervention studies, and the lowest to cross-sectional studies, subsequently up- or down-grading evidence dependent upon various methodological factors such as RoB, studies not comparing the same variables, inconsistency of findings between studies, imprecision (effect estimate confidence interval containing 25% harm or benefit), publication bias of funnel plot reported, and other considerations (large effect RR > 2, adjustment for all plausible confounding, dose response gradient). As we did not carry out a meta-analysis assessment of GRADE criteria such as precision or publication bias was not possible.
2.4. Measures of Environmental Exposure
- Greenspace was measured by land use data percentage of natural space in the neighbourhood (e.g., for the UK, a census output area such as LSOA) or measured within a set distance of the child’s residence. Other indices included satellite derived neighbourhood greenspace (e.g., normalised difference vegetation index (NDVI)) and percentage of neighbourhood greenspace.
- Blue space was measured by parents reporting on number of days taking their children to a beach.
- Environmental noise pollution included road traffic, construction noise, and aircraft noise.
- Air pollution was measured by particulate matter, tobacco smoke (nitrogen dioxide: NO2), and elemental carbon attributed to traffic (ECAT).
- Meteorological variables included seasons, hot or cold weather, humidity and sunlight.
- Spatial density and interior home/facility design included space per child in square metres (high/low density), wall paint, sensory room, presence of damp.
- Urbanicity and rurality were described by the location of the child’s residence or school.
2.5. Measures of Aggressive Behaviours
The studies utilised a number of psychometrically valid parent and child reported measures of aggressive behaviour, as well as observer ratings. These comprised the full instrument or conduct, aggression, and externalising behaviour domains as follows:
- Strengths and Difficulties Questionnaire (SDQ) [98]
- Age-appropriate Behaviour Assessment System for Children, Second Edition (BASC-2) [99]
- Child Behaviour Checklist (CBCL) [100]
- Health Related Quality of Life in Children (KINDL-R) [101,102]
- WHO Global School-based Student Health Survey [103]
- National Institute of Mental Health Diagnostic Interview Schedule for Children 4th version (NIMH DISC-IV) [104]
- State-Trait Anger Expression Inventory-2 (STAXI-2) [105]
- Other outcomes used were observer rated frequency of aggressive behaviour
3. Results
The two searches retrieved 7434 records. After deduplication, 7174 were screened of which 257 underwent full-text assessment, resulting in the inclusion of 67 papers (details are shown in the PRISMA flow diagram, Figure 1). Six of which reported on the physical environment and aggressive behaviours in neurodiverse participants.
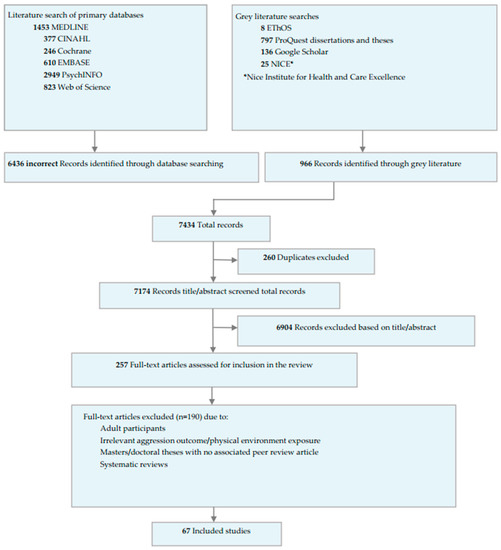
Figure 1.
PRISMA flow diagram of the included studies.
We report RoB separately for studies carried out with typically developing (Table 1) and neurodiverse populations (Table 2). We follow the same format for the GRADE evidence summaries for the environmental exposures on outcomes of aggressive behaviours for typically developing and neurodiverse children (Table 3 and Table 4).

Table 1.
Risk of Bias (RoB) summary for studies reporting on the association between environmental domains and aggressive behaviours in typically developing children.

Table 2.
Risk of bias (RoB) summary for studies reporting on environmental domains and aggressive behaviours in neurodiverse children.

Table 3.
GRADE summary of quality of evidence for typically developing children.

Table 4.
GRADE summary of quality of evidence for neurodiverse populations.
3.1. Typically Developing Children
3.1.1. Greenspace
Eleven longitudinal and seven cross-sectional studies (~46,684 participants) examined associations between greenspace exposure and childhood aggression [34,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122]. Five studies were carried out in the UK, four in the USA, two in Belgium, with the remaining in Australia, Korea, Lithuania, Germany, Spain and China. All greenspace studies were classified as low RoB.
Inconsistent evidence for harms or benefits was reported across eight studies [106,107,108,109,112,113,117,121] that examined associations between satellite derived neighbourhood greenspace (NDVI) and parental-reported child aggression related outcomes. Two studies [101,109] examining the association between parental-reported child aggression and conduct problems and percentage of land designated as natural land, reported high-quality evidence. Proximity of the child’s residence to greenspace was inconsistently associated with parent reported conduct problems across three studies [106,108,114]. Very low-quality evidence [111,116,120] reported no relationship between percentage of neighbourhood greenspace and both child and parent-reported conduct problems. Moderate-quality evidence from three studies [34,111,120] reported inconsistent beneficial effects of access to private garden space on parent-reported conduct problems.
3.1.2. Environmental Sound and Noise
Three longitudinal and eight cross-sectional studies (n = 23,665) assessed the association between environmental noise pollution including road traffic, construction noise, aircraft noise and aggression outcomes [123,124,125,126,127,128,129,130,131,132,133]. These studies were primarily conducted in the UK, Spain, Germany, and the Netherlands, and one study in China. Three of these studies [124,131,132] used data from the multi-national RANCH study examining the influence of high and low road and aircraft noise on the behaviour of pupils who attended schools that were close to main roads or under flypaths. Two studies were judged to be of unclear RoB [126,130], with the majority being rated as low RoB. A very low-quality evidence for harmful association [130] between residential aircraft noise exposure and increased child annoyance was reported. Similarly, low- and very low-quality evidence was found for associations between increased residential noise [126], predicted air and road traffic noise [131], and heightened self-reported child annoyance. Schools located in areas of high aircraft noise were associated with increased child-reported annoyance [127,128,129], but inconsistently correlated with parent-reported child conduct problems ([127,129], both very low quality). Two studies [124,132] examining the role of residential aircraft noise on the parent-administered conduct problems subscale of the SDQ reported no association (low quality). Five studies [123,124,125,133,185] reported very low quality inconsistent evidence for estimated noise exposure effects on parent-reported child aggression.
Two studies (longitudinal and within-group repeated measures) from the USA (n = 658) assessed the association of music on childhood aggression [183,184]. Both studies were rated as high RoB. Aggressive or sexual music content was associated with increased self-reported aggressive behaviour in adolescents ([183], very low quality). Low-quality evidence reported no association between alternating periods of instrumental music and observer rated aggressive behaviours [184]).
3.1.3. Air Pollution
Eight longitudinal and six cross-sectional studies from Lithuania, China, Korea, Iran, Canada, USE, and the UK (n = 45,607) explored the influence of air particulate matter on aggressive behavioural outcomes in typically developing children and young people [34,107,116,123,135,136,138,141,142,144,145,146,147,148,149]. One study was rated as high RoB [146], one as unclear RoB [136], and the remaining as low RoB.
Five studies [135,136,146,147] provided either low- or very low-quality evidence supporting the harmful influences of tobacco smoke exposure across various aggressive behavioural questionnaires. Very Low-quality evidence for a harmful association [132] between active or passive tobacco exposure and child self-reported anger and aggressive behaviour was found.
Three studies [116,141,149] examined the relationship between Nitrogen Dioxide (NO2) exposure and child self-reported conduct problems symptoms and reported inconsistent evidence for a harmful association (Very Low quality). No effect of Elemental Carbon Attributed to Traffic (ECAT) on parent-reported externalising behaviours (BASC-2) was found ([145], Moderate quality).
In addition, there was inconsistent evidence for an association between exposure to particulate matter less than 2.5 microns (PM2.5), and child self-reported conduct problems [141,149]. No effect was found in a study that examined the influence of PM2.5 on parent reported conduct problem scores [107]. Another study by Loftus et al., 2020 [144] explored the influence of exposure to particulate matter less than 10 microns (PM10) on parent reported child aggressive behaviours but it did not show a significant association (Very Low quality). Ambient air lead exposure (PbA)) was associated with high parent-reported aggressive behaviour ([148], Very Low quality).
3.1.4. Meteorological Exposure
Five longitudinal and two cross-sectional studies (approximately = 6314) from Chile, Canada, the Netherlands, USA, and Italy, assessed associations between meteorological variables and child aggression outcomes [151,152,153,154,155,156,157,158,159]. One study was rated as high RoB [158] with the remaining studies rated as low RoB.
The study by Muñoz-Reyes et al. [158] contrasted the frequency of observed aggressive behaviours during the warm season (summer/spring) with the frequency of such behaviours during the cold season (autumn/winter), reporting Very Low-quality evidence for harmful effect of warm seasonality. Low-quality evidence associated increased humidity with harmful increases in teacher-reported child aggressive behaviours [151,156]. Studies examining the effects of sunlight exposure on teacher reported [151,156] and child self-assessment [152] behavioural outcomes reported inconsistent or no evidence, respectively (very low quality). Low- and Moderate-quality evidence for the harmful influence of increased temperature on teacher and parent-reported child aggression symptoms was reported in three studies [151,156,159]. However, we found one Very Low-quality study that provided evidence for beneficial effect of temperature on children’s self-reported anger [152]. Aggression during summer recess was lower compared with aggression during the school year ([154]; Low quality). No association between hours of precipitation per day and children’s self-reported anger was found ([152], Very Low-quality evidence). Finally, a study carried out by Lochman et al. [153] examined longitudinal associations between tornado exposure and externalising symptoms, and reported a harmful associations of Moderate quality.
3.1.5. Spatial Density and Interior Design
Four observational and two longitudinal studies [34,160,161,162,163,165] (n = 8568) from the USA and the UK examined spatial density and architectural design in relation to childhood aggression. RoB was judged as high in all studies except one rated as unclear [163] and one rated as low [34]. A study [165] reported a beneficial effect of increased playroom openness, but no effect of space per child or room group size on observed aggressive behaviours. Low-quality evidence assessing the association between high density (in comparison to low density) child playrooms and frequency of aggressive behaviours reported inconsistent results [160,161,162]. Moderate-quality evidence examining the effect of overcrowding in the home [34,163] reported inconsistent associations with parent-reported conduct problems but was associated with reduced teacher-reported externalising behaviours.
Three studies, two quasi-experimental and one longitudinal (n = 8257) conducted in Iran, the UK, and the USA examined the associations between interior design features and childhood aggression [34,179,181]. Low-quality evidence of association ([181] unclear RoB) between red painted classroom walls and increased self-reported aggression was found. In-patient psychiatric ward sensory room modifications were correlated with beneficial reductions in observer rated aggressive behaviour ([179] unclear RoB Moderate quality). Additionally, presence of damp in the house was associated with elevated trajectories of conduct problems in children ([34], Moderate quality).
3.1.6. Urbanicity and Rurality
Three longitudinal and three cross-sectional studies (n = 17,630) from the USA, the Netherlands, and Thailand explored the influence of urbanicity and rurality of residence on children’s aggressive behavioural outcomes [34,164,168,170,172,176]. One study was rated as high RoB [168] with the remaining assessed as low or moderate RoB. One study [176] reported inconsistent associations between the location of the participants and scores across three self-reported aggression outcomes (Very Low quality). Moderate-quality inconsistent evidence [34,172] was reported for the effect of urban residence on child conduct problems and aggressive behaviour in parent-reported questionnaires, whilst evidence for a lack of association was found for teacher-completed aggression outcomes [172]. Another study [170] examined the effects of urban or rural settings on aggressive behaviours in schoolchildren attending schools from either setting. It reported no association of setting with parent-reported behaviours, but a harmful effect of urban school location on teacher-assessed behaviours (both Very Low quality). Very Low-quality evidence reported no association between children recruited from rural or urban Head Start centres and teacher-reported anger ratings ([168]: AML Behaviour Rating Scale). Neighbourhood urbanicity (mean number of addresses within a 1 km radius of participant’s residence) was associated with increased teacher-reported child problem behaviours ([166] Low quality).
3.2. Neurodiverse Children
Six studies (n = 79,249) from the USA, Pakistan, the UK, and Australia included neurodiverse participants exclusively [34,188,190,191,192,193]. The studies are heterogenous utilising a variety of designs including longitudinal, cross-sectional, quasi-experimental, interventional, including two case studies. Two studies were judged to be of high RoB [190,192], one unclear [193] and the remaining three of low RoB.
Baird et al. [34] explored interaction effects between a sub-sample of children with intellectual disability (assessed via cognitive measures) from the Millennium Cohort Study (MCS) and various physical environmental exposures (neighbourhood greenspace: NDVI, access to a private garden, air pollution: NO2, urban or rural residence, household density, presence of damp. The authors reported no mediating influence of intellectual disability on the association between environmental exposures and children’s conduct problem trajectories, except for household density (beneficial effect, moderate quality). Another study [188] reported no correlation between urban tree canopy coverage and frequency of aggressive behaviours in children with ASD but found an association between residing in lower urban tree canopy areas with increased parent-reported conduct problem severity. However, the evidence was deemed to be of low quality in both studies. The case study by Durand and Mapstone [190] examined the impact of fast and slow beat music on a child with intellectual disability, reporting reductions in observed frequency of aggressive behaviour during the fast beat condition and increases during the slow beat condition in comparison to a no-music baseline (Low quality). Additionally, a clinical trial of new age and classical music [191] provided Moderate-quality evidence for the beneficial effects of music on self-reported aggression in children with intellectual disabilities. A case study [192] assessing the impact of spatial proximity between an adolescent girl with intellectual disability and the therapist, provided a Very Low-quality evidence for a correlation between closer proximity and increased duration of observed aggressive behaviours. Finally, a study [193] examined the efficacy of modified sensory rooms in reducing distress in adolescent psychiatric inpatients, reporting additional benefits for individuals who had a history of aggression (Moderate quality).
4. Discussion
This is the first narrative review that updates previous literature across several environmental domains as well as including neurodiverse children, a previously under reported population in other reviews.
4.1. Physical Environmental Domains
4.1.1. Greenspace
We found evidence that supports the therapeutic benefits of increased natural land and greenness surrounding child residences. Previous reviews have also shown associations between greenspace exposure and reductions in violent behaviours [194,195].
The greenspace evidence synthesised primarily supports the therapeutic influence of neighbourhood nature exposure on child aggressive behavioural outcomes. These effects, at least partially, were also present in NDDs populations. Whilst more epidemiological and experimental research paradigms are required to solidify the evidence for this therapeutic relationship and understand its underlying mechanistic pathways, we provide initial evidence for the role of nature in reducing aggression in neurotypical and diverse children. Initial attempts at establishing guidelines for integration and therapeutic adoption are beginning to be developed [196]. Studies examining socio-cultural barriers to children accessing urban greenspaces [197] are of crucial importance, but these findings need to be communicated to institutions and policy decision makers. We also recommend future experimental studies that aim to elucidate the underlying (neuro)mechanistic pathways via which nature exposure conveys these potential benefits. Advances in this regard would drastically redefine architectural and urban design for physical and mental health.
4.1.2. Noise Pollution
Children appear to consistently self-report higher aggressive and annoyance related behaviours related to environmental noise, whereas parent reported outcomes either show a lack of association or inconsistent associations both for harm and benefit. This may suggest that noise exposure operates on pathways involving subjective annoyance and irritation which may not translate into objective longer-term increases in aggression problems. Additionally, although noise annoyance may not play a direct role in the aetiology of those problems, noise exposure of individuals who experience frustration or irritable mood has been shown to increase its severity [25,26]. Noise pollution, therefore, may not operate as a causal mechanism of aggression, but exacerbate pre-existing manifestation, potentially via draining of attentional and cognitive resources, leading to increased self-regulatory difficulties [27].
4.1.3. Air Pollution
We found absent and inconsistent associations between ECAT, particulate matter less than PM2.5, particulate matter less than PM10 and NO2 exposure and childhood aggression problems. Tobacco smoke exposure showed a harmful association with aggressive behavioural outcomes irrespective of who was the outcome assessor. We also found this harmful association for childhood exposure to ambient air lead exposure (PbA). The lack of association of PM2.5 and PM10 with these behaviours is potentially anomalous when considering research that has linked air pollution with increased risk of mental health disorders [198]. The harmful effects of tobacco smoke and ambient lead exposure may increase the risk of neuropsychiatric disorders and violent crime, possibly via neuroinflammation [19,20,21,22,23,24].
Whilst none of the retrieved articles examined the effects of air pollution on neurodiverse children, it was shown that families of these children disproportionately reside in areas of higher particulate concentration than those of typically developing children [49], as well as exhibiting elevated rates of aggressive behaviour [199,200].
4.1.4. Meteorological Effects
Summer seasonality, humidity, temperature, and previous tornado exposure were consistently correlated with increased childhood aggressive behaviours. We found little evidence for either harmful or beneficial effects of ambient temperature and seasonality. Previous studies suggest that humidity compounds the negative effects of heat on mental health [201], as well as being associated with increased emergency department visits for mental health problems [202]. Elevated temperature has also been associated with increased violent crime [203]; however, those associations warrant further examination.
4.1.5. Spatial Density
The negative impact of high spatial density on aggression in young people [204] and inpatients in psychiatric wards has been highlighted previously [205,206,207]. Notwithstanding the beneficial effects of increased playroom openness, inconsistent influences for other spatial characteristics prevent a firm explanation of findings. Theories have posited that high spatial density triggers perceptions of crowding and a subsequent physiological stress arousal response [30,31,32]. Further studies on possible mechanistic pathways between high spatial density and aggression in children could lead to therapeutic adaptations in clinical and residential spaces [208].
4.1.6. Urbanicity and Rurality of Residence
Due to the quality of retrieved evidence, we were unable to extricate any definitive conclusions for associations between urban or rural residence and childhood aggressive behaviours. This is potentially anomalous considering that children residing in rural areas are exposed to more greenspace which generally appears to have calming effects [209,210,211,212,213,214]. Rurality, however, is only one factor in a great number of confounders on childhood aggression. Furthermore, studies do not often use operationalised definitions of “rural” or “rurality” [215], potentially leading to heterogeneity in the underlying conceptual constructs being examined, limiting the replicability and specificity of results.
4.1.7. Interior Design and Housing Quality
Previous work has associated damp problems with increased toxic mould, contributing to poor air quality [216] and/or potential neuroinflammatory and/or neurotoxic responses [20,22]. Damp in a house may also be associated with other adversities such as low socio-economic status and household disruption [217] exemplified by previous research linking poor household conditions to psychological distress [218].
Whilst preliminary evidence from this review supported the positive impact of modified sensory rooms to de-escalate aggression, it is very limited in scope. One study [35] suggested that the increased reduction in distress related to sensory deficits may be attributable to a sense of autonomy children and young people may gain by using the room unaccompanied.
4.1.8. Music
We found preliminary evidence for the therapeutic potential of music in neurodiverse children which is similar with findings reported in adults [219]. Music listening has been associated with a broad range of psychological and physiological benefits [38,39,40]. Some [36,37] have stated that the therapeutic influences of music may operate mechanistically via enhancing emotional regulation, but such evidence is not yet available [41]. Music is a complex physical phenomenon, which requires additional targeted research to examine its effects on aggressive behaviours in typically developing and neurodiverse young people.
4.2. Strengths and Limitations
This review is comprehensive and has examined the evidence of a wide range of environmental exposures in relation to the display of aggressive behaviours in typical and neurodiverse children. To the best of our knowledge, this is the first review that comparatively examines available research on environmental determinants of aggression in these two groups. The review shows clearly the disproportionately sparse literature relating those children and the physical environment despite the fact that they are more likely to be affected by social adversity, poor housing, air pollutants, and poverty [48,49,50,220,221].
The incorporation of GRADE to assess the quality of evidence in this review may well be simultaneously both a strength and a limitation. Whilst it facilitated the examination of the certainty of included evidence, the adaptation of GRADE for use in a non-meta-analytic review including epidemiological studies, may, as highlighted previously [95], inadvertently result in downgrading of evidence irrespective of study quality. We also adopted a modified risk of bias protocol which may have impacted the RoB assessments of included studies. There may also have been potential conflicts of interest based on the source of funding which we did not consider in this review.
A final limitation of this evidence synthesis is the inclusion of studies that adopt a diverse range of heterogenous physical environmental exposures and metrics. As has been highlighted previously by experts in physical environmental epidemiological analysis on child socio-cognitive outcomes [116], further research is needed on improving environmental measures of aspects such as air pollution exposure, and access to and quality of children’s greenspaces. Developing more holistic, accurate, and reliable measures of environmental exposures will facilitate novel research paradigms (computational, simulatory and experimental) that can elucidate the influences of these aspects, reciprocally informing direction for future research into (neurobiological)mechanistic pathways.
5. Conclusions
Physical environmental exposures sit at the intersection of social, biochemical, and (epi)genetic aetiological influences on the development and progression of a spectrum of physical and mental health outcomes. Further research can support stakeholders, ranging from city planners and environmental legislators to politicians and clinicians, in considering the role of the physical environment in the context of adverse impact on child (neuro)development. Whilst there is obvious need to further examine environmental and climate influences on mental health of all children, particular attention must be paid to neurodiverse children and their families. A recent report recommended that in order to pursue and achieve health parity for those children, we must “reduce poverty and improve living environments” [50]. Research focusing on that population will help to bridge the equity gap that has significant therapeutic and health implications for all citizens.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph20032549/s1, Table S1: search strategy.
Author Contributions
Conceptualization: E.F., A.H., N.T. and A.B.; methodology, A.H., A.B. and B.C.; writing—original draft preparation, A.B.; writing—review and editing, N.T., B.C. and A.H. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
We thank Nancy Kouroupa, Steven Naughton, Laura Paulauskaite, Peiyao Tang and Rachel Royston for assisting in co-screening studies; Bori Vegh for support with preparation of the manuscript; Louise Marston, for guidance on study heterogeneity and narrative synthesis reporting; Deborah Marletta for assistance with the electronic database protocol development.
Conflicts of Interest
Multiple studies included in this review involved the authorship of Eirini Flouri. Flouri had no influence/involvement in the selection or appraisal of these studies. No other authors report any potential conflict of interest.
References
- Wild, C.P. Complementing the Genome with an “Exposome”: The Outstanding Challenge of Environmental Exposure Measurement in Molecular Epidemiology. Cancer Epidemiol. Biomark. Prev. 2005, 14, 1847–1850. [Google Scholar] [CrossRef] [PubMed]
- Wild, C.P. The exposome: From concept to utility. Int. J. Epidemiol. 2012, 41, 24–32. [Google Scholar] [CrossRef] [PubMed]
- Bronfenbrenner, U. Toward an experimental ecology of human development. Am. Psychol. 1977, 32, 513–531. [Google Scholar] [CrossRef]
- Bronfenbrenner, U. The Ecology of Human Development: Experiments by Nature and Design; Harvard University Press: Cambridge, MA, USA, 1949. [Google Scholar]
- Bronfenbrenner, U.; Ceci, S.J. Nature-nuture reconceptualized in developmental perspective: A bioecological model. Psychol. Rev. 1994, 101, 568–586. [Google Scholar] [CrossRef] [PubMed]
- Vineis, P.; Robinson, O.; Chadeau-Hyam, M.; Dehghan, A.; Mudway, I.; Dagnino, S. What is new in the exposome? Environ. Int. 2020, 143, 105887. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.B.; McBride, G.; Ross, C.; Curtis, L. A Place to Heal: Environmental Sources of Satisfaction Among Hospital Patients1. J. Appl. Soc. Psychol. 2002, 32, 1276–1299. [Google Scholar] [CrossRef]
- Davison, K.K.; Lawson, C.T. Do attributes in the physical environment influence children’s physical activity? A review of the literature. Int. J. Behav. Nutr. Phys. Act. 2006, 3, 19. [Google Scholar] [CrossRef]
- Markevych, I.; Schoierer, J.; Hartig, T.; Chudnovsky, A.; Hystad, P.; Dzhambov, A.M.; de Vries, S.; Triguero-Mas, M.; Brauer, M.; Nieuwenhuijsen, M.J.; et al. Exploring pathways linking greenspace to health: Theoretical and methodological guidance. Environ. Res. 2017, 158, 301–317. [Google Scholar] [CrossRef]
- Luque-García, L.; Corrales, A.; Lertxundi, A.; Díaz, S.; Ibarluzea, J. Does exposure to greenness improve children’s neuropsychological development and mental health? A Navigation Guide systematic review of observational evidence for associations. Environ. Res. 2022, 206, 112599. [Google Scholar] [CrossRef]
- Berto, R. The Role of Nature in Coping with Psycho-Physiological Stress: A Literature Review on Restorativeness. Behav. Sci. 2014, 4, 394–409. [Google Scholar] [CrossRef]
- Ulrich, R.S. Natural Versus Urban Scenes: Some Psychophysiological Effects. Environ. Behav. 1981, 13, 523–556. [Google Scholar] [CrossRef]
- Ulrich, R.S.; Simons, R.F.; Losito, B.D.; Fiorito, E.; Miles, M.A.; Zelson, M. Stress recovery during exposure to natural and urban environments. J. Environ. Psychol. 1991, 11, 201–230. [Google Scholar] [CrossRef]
- Kaplan, R.; Kaplan, S. The Experience of Nature: A Psychological Perspective; Cambridge University Press: Cambridge, UK, 1989; ISBN 978-0-521-34139-4. [Google Scholar]
- Ohly, H.; White, M.P.; Wheeler, B.W.; Bethel, A.; Ukoumunne, O.C.; Nikolaou, V.; Garside, R. Attention Restoration Theory: A systematic review of the attention restoration potential of exposure to natural environments. J. Toxicol. Environ. Health Part B 2016, 19, 305–343. [Google Scholar] [CrossRef] [PubMed]
- Sumitomo, K.; Akutsu, H.; Fukuyama, S.; Minoshima, A.; Kukita, S.; Yamamura, Y.; Sato, Y.; Hayasaka, T.; Osanai, S.; Funakoshi, H.; et al. Conifer-Derived Monoterpenes and Forest Walking. Mass Spectrom. 2015, 4, A0042. [Google Scholar] [CrossRef]
- Pagès, A.B.; Peñuelas, J.; Clarà, J.; Llusià, J.; Campillo i López, F.; Maneja, R. How Should Forests Be Characterized in Regard to Human Health? Evidence from Existing Literature. Int. J. Environ. Res. Public Health 2020, 17, 1027. [Google Scholar] [CrossRef]
- Bratman, G.N.; Hamilton, J.P.; Hahn, K.S.; Daily, G.C.; Gross, J.J. Nature experience reduces rumination and subgenual prefrontal cortex activation. Proc. Natl. Acad. Sci. USA 2015, 112, 8567–8572. [Google Scholar] [CrossRef]
- Bondy, M.; Roth, S.; Sager, L. Crime Is in the Air: The Contemporaneous Relationship between Air Pollution and Crime. J. Assoc. Environ. Resour. Econ. 2020, 7, 555–585. [Google Scholar] [CrossRef]
- Brockmeyer, S.; D’Angiulli, A. How air pollution alters brain development: The role of neuroinflammation. Transl. Neurosci. 2016, 7, 24–30. [Google Scholar] [CrossRef]
- Burkhardt, J.; Bayham, J.; Wilson, A.; Berman, J.D.; O’Dell, K.; Ford, B.; Fischer, E.V.; Pierce, J.R. The relationship between monthly air pollution and violent crime across the United States. J. Environ. Econ. Policy 2019, 9, 188–205. [Google Scholar] [CrossRef]
- Calderón-Garcidueñas, L.; Leray, E.; Heydarpour, P.; Torres-Jardón, R.; Reis, J. Air pollution, a rising environmental risk factor for cognition, neuroinflammation and neurodegeneration: The clinical impact on children and beyond. Rev. Neurol. 2016, 172, 69–80. [Google Scholar] [CrossRef]
- Herrnstadt, E.; Heyes, A.; Muehlegger, E.; Saberian, S. Air Pollution as a Cause of Violent Crime: Evidence from Los Angeles and Chicago. Manuscript in preparation, 2016. Available online: http://www.erichmuehlegger.com/Working%20Papers/crime_and_Pollution_fv.pdf (accessed on 25 March 2021).
- Lu, J.G. Air pollution: A systematic review of its psychological, economic, and social effects. Curr. Opin. Psychol. 2019, 32, 52–65. [Google Scholar] [CrossRef] [PubMed]
- Donnerstein, E.; Wilson, D.W. Effects of noise and perceived control on ongoing and subsequent aggressive behavior. J. Pers. Soc. Psychol. 1976, 34, 774–781. [Google Scholar] [CrossRef] [PubMed]
- Konecni, V.J. The mediation of aggressive behavior: Arousal level versus anger and cognitive labeling. J. Pers. Soc. Psychol. 1975, 32, 706–712. [Google Scholar] [CrossRef] [PubMed]
- Mueller, M.A.; Flouri, E. Neighbourhood greenspace and children’s trajectories of self-regulation: Findings from the UK Millennium Cohort Study. J. Environ. Psychol. 2020, 71, 101472. [Google Scholar] [CrossRef]
- Cohen, L.E.; Felson, M. Social Change and Crime Rate Trends: A Routine Activity Approach. Am. Sociol. Rev. 1979, 44, 588–608. [Google Scholar] [CrossRef]
- Anderson, C.A.; Deuser, W.E.; DeNeve, K.M. Hot temperatures, hostile affect, hostile cognition, and arousal: Tests of a general model of affective externalising behaviours. Pers. Soc. Psychol. Bull. 1995, 21, 434–448. [Google Scholar] [CrossRef]
- Cox, T.; Houdmont, J.; Griffiths, A. Rail passenger crowding, stress, health and safety in Britain. Transp. Res. Part A Policy Pract. 2006, 40, 244–258. [Google Scholar] [CrossRef]
- Aiello, J.R.; Nicosia, G.; Thompson, D.E. Physiological, Social, and Behavioral Consequences of Crowding on Children and Adolescents. Child Dev. 1979, 50, 195–202. [Google Scholar] [CrossRef]
- Walden, T.A.; Forsyth, D.R. Close encounters of the stressful kind: Affective, physiological, and behavioral reactions to the experience of crowding. J. Nonverbal Behav. 1981, 6, 46–64. [Google Scholar] [CrossRef]
- Lawrence, D.L.; Low, S.M. The Built Environment and Spatial Form. Annu. Rev. Anthropol. 1990, 19, 453–505. [Google Scholar] [CrossRef]
- Baird, A.; Papachristou, E.; Hassiotis, A.; Flouri, E. The role of physical environmental characteristics and intellectual disability in conduct problem trajectories across childhood: A population-based Cohort study. Environ. Res. 2022, 209, 112837. [Google Scholar] [CrossRef] [PubMed]
- Lindberg, H.M.; Samuelsson, M.; Perseius, K.-I.; Björkdahl, A. The experiences of patients in using sensory rooms in psychiatric inpatient care. Int. J. Ment. Health Nurs. 2019, 28, 930–939. [Google Scholar] [CrossRef] [PubMed]
- Juslin, P.N.; Sloboda, J. Handbook of Music and Emotion: Theory, Research, Applications; Oxford University Press: Oxford, UK, 2011. [Google Scholar]
- Saarikallio, S.; Erkkilä, J. The role of music in adolescents’ mood regulation. Psychol. Music. 2007, 35, 88–109. [Google Scholar] [CrossRef]
- McKinney, C.H.; Antoni, M.H.; Kumar, M.; Tims, F.C.; McCabe, P.M. Effects of guided imagery and music (GIM) therapy on mood and cortisol in healthy adults. Health Psychol. 1997, 16, 390–400. [Google Scholar] [CrossRef]
- Lai, H.-L.; Good, M. Music improves sleep quality in older adults. J. Adv. Nurs. 2006, 53, 134–144. [Google Scholar] [CrossRef]
- Teng, X.F.; Wong, M.Y.M.; Zhang, Y.T. The Effect of Music on Hypertensive Patients. In Proceedings of the 2007 29th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Lyon, France, 22–26 August 2007; pp. 4649–4651. [Google Scholar] [CrossRef]
- Thoma, M.; Scholz, U.; Ehlert, U.; Nater, U. Listening to music and physiological and psychological functioning: The mediating role of emotion regulation and stress reactivity. Psychol. Health 2012, 27, 227–241. [Google Scholar] [CrossRef] [PubMed]
- Evans, G.W. Child Development and the Physical Environment. Annu. Rev. Psychol. 2006, 57, 423–451. [Google Scholar] [CrossRef] [PubMed]
- Clark, C.; Myron, R.; Stansfeld, S.; Candy, B. A systematic review of the evidence on the effect of the built and physical environment on mental health. J. Public Ment. Health 2007, 6, 14–27. [Google Scholar] [CrossRef]
- Simons, R.L.; Lei, M.K.; Beach, S.R.H.; Brody, G.H.; Philibert, R.; Gibbons, F.X. Social Environment, Genes, and Aggression: Evidence Supporting the Differential Susceptibility Perspective. Am. Sociol. Rev. 2011, 76, 883–912. [Google Scholar] [CrossRef]
- Ferguson, K.T.; Cassells, R.C.; MacAllister, J.W.; Evans, G.W. The physical environment and child development: An international review. Int. J. Psychol. 2013, 48, 437–468. [Google Scholar] [CrossRef]
- Waltes, R.; Chiocchetti, A.G.; Freitag, C.M. The neurobiological basis of human aggression: A review on genetic and epigenetic mechanisms. Am. J. Med. Genet. Part B Neuropsychiatr. Genet. 2015, 171, 650–675. [Google Scholar] [CrossRef]
- Gao, Y.; Zhang, L.; Kc, A.; Wang, Y.; Zou, S.; Chen, C.; Huang, Y.; Mi, X.; Zhou, H. Housing environment and early childhood development in sub-Saharan Africa: A cross-sectional analysis. PLoS Med. 2021, 18, e1003578. [Google Scholar] [CrossRef]
- Blackburn, C.M.; Spencer, N.J.; Read, J.M. Prevalence of childhood disability and the characteristics and circum-stances of disabled children in the UK: Secondary analysis of the Family Resources Survey. BMC Pediatr. 2010, 10, 21. [Google Scholar] [CrossRef] [PubMed]
- Emerson, E.; Robertson, J.; Hatton, C.; Baines, S. Risk of exposure to air pollution among British children with and without intellectual disabilities. J. Intellect. Disabil. Res. 2019, 63, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Rickard, W.; Donkin, A. A Fair, Supportive Society: Summary Report; Institute of Health Equity: 2022. Available online: https://www.instituteofhealthequity.org/resources-reports/a-fair-supportive-society-summary-report/a-fair-supportive-society-summary-report.pdf (accessed on 10 January 2023).
- Anaby, D.; Hand, C.; Bradley, L.; DiRezze, B.; Forhan, M.; Digiacomo, A.; Law, M. The effect of the environment on participation of children and youth with disabilities: A scoping review. Disabil. Rehabil. 2013, 35, 1589–1598. [Google Scholar] [CrossRef]
- Law, M.; Petrenchik, T.; King, G.; Hurley, P. Perceived environmental barriers to recreational, community, and school participation for children and youth with physical disabilities. Arch. Phys. Med. Rehabil. 2007, 88, 1636–1642. [Google Scholar] [CrossRef] [PubMed]
- von Benzon, N. Discussing Nature, ‘Doing’ Nature: For an emancipatory approach to conceptualizing young people’s access to outdoor green space. Geoforum 2018, 93, 79–86. [Google Scholar] [CrossRef]
- Visser, E.M.; Berger, H.J.C.; Prins, J.B.; Van Schrojenstein Lantman-De Valk, H.M.J.; Teunisse, J.P. Shifting impairment and aggression in intellectual disability and Autism Spectrum Disorder. Res. Dev. Disabil. 2014, 35, 2137–2147. [Google Scholar] [CrossRef]
- Hassiotis, A.; Parkes, C.; Jones, L.; Fitzgerald, B.; Romeo, R. Individual Characteristics and Service Expenditure on Challenging Behaviour for Adults with Intellectual Disabilities. J. Appl. Res. Intellect. Disabil. 2008, 21, 438–445. [Google Scholar] [CrossRef]
- Kiely, J.; Pankhurst, H. Violence faced by staff in a learning disability service. Disabil. Rehabil. 1998, 20, 81–89. [Google Scholar] [CrossRef]
- Brosnan, J.; Healy, O. A review of behavioral interventions for the treatment of aggression in individuals with developmental disabilities. Res. Dev. Disabil. 2011, 32, 437–446. [Google Scholar] [CrossRef]
- Maughan, B.; Rutter, M. Antisocial children grown up. In Conduct Disorders in Childhood and Adolescence; Hill, J., Maughan, B., Eds.; Cambridge University Press: Cambridge, UK, 2001; pp. 507–552. ISBN 0521786398(pb). [Google Scholar]
- Romeo, R.; Knapp, M.; Scott, S. Economic cost of severe antisocial behaviour in children—And who pays it. Br. J. Psychiatry 2006, 188, 547–553. [Google Scholar] [CrossRef] [PubMed]
- Broidy, L.; Willits, D.; Denman, K.; Schools and neighborhood crime. Prepared for Justice Research Statistics Association 2009. Available online: http://isr.unm.edu/reports/2009/schools-and-crime.pdf (accessed on 14 October 2022).
- Reef, J.; Diamantopoulou, S.; Van Meurs, I.; Verhulst, F.; Van Der Ende, J. Child to adult continuities of psychopathology: A 24-year follow-up. Acta Psychiatr. Scand. 2009, 120, 230–238. [Google Scholar] [CrossRef] [PubMed]
- White, S.W.; Roberson-Nay, R. Anxiety, Social Deficits, and Loneliness in Youth with Autism Spectrum Disorders. J. Autism Dev. Disord. 2009, 39, 1006–1013. [Google Scholar] [CrossRef] [PubMed]
- Foster, E.M.; Jones, D.E. The Conduct Problems Prevention Research Group The High Costs of Aggression: Public Expenditures Resulting from Conduct Disorder. Am. J. Public Health 2005, 95, 1767–1772. [Google Scholar] [CrossRef] [PubMed]
- Dagnan, D.; Weston, C. Physical Intervention with People with Intellectual Disabilities: The Influence of Cognitive and Emotional Variables. J. Appl. Res. Intellect. Disabil. 2006, 19, 219–222. [Google Scholar] [CrossRef]
- Shoham-Vardi, I.; Davidson, P.W.; Cain, N.N.; Sloane-Reeves, J.E.; Giesow, V.E.; Quijano, L.E.; Houser, K.D. Factors predicting re-referral following crisis intervention for community-based persons with developmental disabilities and behavioral and psychiatric disorders. Am. J. Ment. Retard. 1996, 101, 109–117. [Google Scholar]
- Dryden-Edwards, R.C.; Combrinck-Graham, L. Developmental Disabilities from Childhood to Adulthood: What Works for Psychiatrists in Community and Institutional Settings; John Hopkins University Press: Baltimore, MA, USA, 2010; ISBN 10: 0801894182. [Google Scholar]
- Hodgetts, S.; Nicholas, D.B.; Zwaigenbaum, L. Home Sweet Home? Families’ Experiences with Aggression in Children with Autism Spectrum Disorders. Focus Autism Other Dev. Disabil. 2013, 28, 166–174. [Google Scholar] [CrossRef]
- Raaijmakers, M.A.; Posthumus, J.A.; Van Hout, B.A.; Van Engeland, H.; Matthys, W. Cross-Sectional Study into the Costs and Impact on Family Functioning of 4-Year-Old Children with Aggressive Behavior. Prev. Sci. 2011, 12, 192–200. [Google Scholar] [CrossRef]
- Neece, C.L.; Green, S.A.; Baker, B.L. Parenting Stress and Child Behavior Problems: A Transactional Relationship Across Time. Am. J. Intellect. Dev. Disabil. 2012, 117, 48–66. [Google Scholar] [CrossRef]
- Otero-López, J.M.; Bolaño, C.C.; Mariño, M.J.S.; Pol, E.V. Exploring stress, burnout, and job dissatisfaction in secondary school teachers. Int. J. Psychol. Psychol. Ther. 2010, 10, 107–123. [Google Scholar]
- McLaren, J.L.; Lichtenstein, J.D. The pursuit of the magic pill: The overuse of psychotropic medications in children with intellectual and developmental disabilities in the USA. Epidemiol. Psychiatr. Sci. 2018, 28, 365–368. [Google Scholar] [CrossRef] [PubMed]
- Bassarath, L. Medication Strategies in Childhood Aggression: A Review. Can. J. Psychiatry 2003, 48, 367–373. [Google Scholar] [CrossRef] [PubMed]
- Girimaji, S.C.; Pradeep, A.J.V. Intellectual disability in international classification of Diseases-11: A developmental perspective. Indian J. Soc. Psychiatry 2018, 34, 68–74. [Google Scholar] [CrossRef]
- Maulik, P.K.; Mascarenhas, M.N.; Mathers, C.D.; Dua, T.; Saxena, S. Prevalence of intellectual disability: A meta-analysis of population-based studies. Res. Dev. Disabil. 2011, 32, 419–436. [Google Scholar] [CrossRef]
- Bowring, D.L.; Totsika, V.; Hastings, R.P.; Toogood, S.; Griffith, G.M. Challenging behaviours in adults with an intellectual disability: A total population study and exploration of risk indices. Br. J. Clin. Psychol. 2017, 56, 16–32. [Google Scholar] [CrossRef]
- Crocker, A.G.; Mercier, C.; Lachapelle, Y.; Brunet, A.; Morin, D.; Roy, M.-E. Prevalence and types of aggressive behaviour among adults with intellectual disabilities. J. Intellect. Disabil. Res. 2006, 50, 652–661. [Google Scholar] [CrossRef] [PubMed]
- Lowe, K.; Allen, D.; Jones, E.; Brophy, S.; Moore, K.; James, W. Challenging behaviours: Prevalence and topographies. J. Intellect. Disabil. Res. 2007, 51, 625–636. [Google Scholar] [CrossRef]
- Emerson, E.; Hatton, C. Mental health of children and adolescents with intellectual disabilities in Britain. Br. J. Psychiatry 2007, 191, 493–499. [Google Scholar] [CrossRef]
- Davies, L.; Oliver, C. The age related prevalence of aggression and self-injury in persons with an intellectual disability: A review. Res. Dev. Disabil. 2013, 34, 764–775. [Google Scholar] [CrossRef]
- Matson, J.L.; Mayville, S.B.; Kuhn, D.E.; Sturmey, P.; Laud, R.; Cooper, C. The behavioral function of feeding problems as assessed by the questions about behavioral function (QABF). Res. Dev. Disabil. 2005, 26, 399–408. [Google Scholar] [CrossRef] [PubMed]
- Dominick, K.C.; Davis, N.O.; Lainhart, J.; Tager-Flusberg, H.; Folstein, S. Atypical behaviors in children with autism and children with a history of language impairment. Res. Dev. Disabil. 2007, 28, 145–162. [Google Scholar] [CrossRef] [PubMed]
- Lesch, K.-P.; Waider, J. Serotonin in the Modulation of Neural Plasticity and Networks: Implications for Neurodevelopmental Disorders. Neuron 2012, 76, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Mazurek, M.O.; Kanne, S.M.; Wodka, E.L. Physical aggression in children and adolescents with autism spectrum disorders. Res. Autism Spectr. Disord. 2013, 7, 455–465. [Google Scholar] [CrossRef]
- Fitzpatrick, S.E.; Srivorakiat, L.; Wink, L.K.; Pedapati, E.V.; Erickson, C.A. Aggression in autism spectrum disorder: Presentation and treatment options. Neuropsychiatr. Dis. Treat. 2016, ume 12, 1525–1538. [Google Scholar] [CrossRef]
- Retz, W.; Rösler, M. The relation of ADHD and violent aggression: What can we learn from epidemiological and genetic studies? Int. J. Law Psychiatry 2009, 32, 235–243. [Google Scholar] [CrossRef] [PubMed]
- McClintock, K.; Hall, S.; Oliver, C. Risk markers associated with challenging behaviours in people with intellectual disabilities: A meta-analytic study. J. Intellect. Disabil. Res. 2003, 47, 405–416. [Google Scholar] [CrossRef]
- Kiernan, C.; Kiernan, D. Challenging behaviour in schools for pupils with severe learning difficulties. Ment. Handicap. Res. 1994, 7, 177–201. [Google Scholar] [CrossRef]
- Oliver, C.; Murphy, G.H.; Corbett, J.A. Self-injurious behaviour in people with learning disabilities: Determinants and interventions. Int. Rev. Psychiatry 1987, 2, 101–116. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 89. [Google Scholar] [CrossRef]
- Campbell, M.; McKenzie, J.E.; Sowden, A.; Katikireddi, S.V.; Brennan, S.E.; Ellis, S.; Hartmann-Boyce, J.; Ryan, R.; Shepperd, S.; Thomas, J.; et al. Synthesis without meta-analysis (SWiM) in systematic reviews: Reporting guideline. BMJ 2020, 368, l6890. [Google Scholar] [CrossRef] [PubMed]
- Stroup, D.F.; Berlin, J.A.; Morton, S.C.; Olkin, I.; Williamson, G.D.; Rennie, D.; Moher, D.; Becker, B.J.; Sipe, T.A.; Thacker, S.B. Meta-analysis of observational studies in epidemiology: A proposal for reporting. JAMA 2000, 283, 2008–2012. [Google Scholar] [CrossRef] [PubMed]
- Mahood, Q.; Van Eerd, D.; Irvin, E. Searching for grey literature for systematic reviews: Challenges and benefits. Res. Synth. Methods 2013, 5, 221–234. [Google Scholar] [CrossRef] [PubMed]
- Paez, A. Gray literature: An important resource in systematic reviews. J. Evid.-Based Med. 2017, 10, 233–240. [Google Scholar] [CrossRef]
- Cochrane Effective Practice and Organisation of Care (EPOC). Data Collection Form. EPOC Resources for Review Authors. 2013 Oslo: Norwegian Knowledge Centre for the Health Services. Available online: http://epoc.cochrane.org/epoc-specific-resources-review-authors (accessed on 17 October 2022).
- Clark, C.; Crumpler, C.; Notley, H. Evidence for Environmental Noise Effects on Health for the United Kingdom Policy Context: A Systematic Review of the Effects of Environmental Noise on Mental Health, Wellbeing, Quality of Life, Cancer, Dementia, Birth, Reproductive Outcomes, and Cognition. Int. J. Environ. Res. Public Health 2020, 17, 393. [Google Scholar] [CrossRef]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.E.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schünemann, H.J. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008, 336, 924–926. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (Updated February 2022). Cochrane, 2022. Available online: www.training.cochrane.org/handbook (accessed on 17 October 2022).
- Goodman, R. The Strengths and Difficulties Questionnaire: A Research Note. J. Child Psychol. Psychiatry 1997, 38, 581–586. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, C.R.; Kamphaus, R.W. Behavior Assessment System for Children, 2nd ed.; Pearson Assessments: Bloomington, MN, USA, 2004; Available online: https://pig.bio.ed.ac.uk/pig/sites/sbsweb2.bio.ed.ac.uk.pig/files/pdf/BASC2_Manual.pdf (accessed on 14 October 2022).
- Achenbach, T.M. The Child Behavior Checklist and related instruments. In The Use of Psychological Testing for Treatment Planning and Outcomes Assessment; Maruish, M.E., Ed.; Lawrence Erlbaum Associates Publishers: New York, NY, USA, 1999; pp. 429–466. Available online: https://www.apa.org/depression-guideline/child-behavior-checklist.pdf (accessed on 17 October 2022).
- Ravens-Sieberer, U.; Bullinger, M. Assessing health-related quality of life in chronically ill children with the German KINDL: First psychometric and content analytical results. Qual. Life Res. 1998, 7, 399–407. [Google Scholar] [CrossRef]
- Ravens-Sieberer, U.; Bullinger, M. News from the KINDL-Questionnaire—A new version for adolescents. Qual. Life Res. 1998, 7, 653. [Google Scholar]
- World Health Organization. Global School-Based Student Health Survey (GSHS). 2018. Available online: https://www.who.int/teams/noncommunicable-diseases/surveillance/systems-tools/global-school-based-student-health-survey (accessed on 18 October 2022).
- Shaffer, D.; Fisher, P.; Lucas, C.P.; Dulcan, M.K.; Schwab-Stone, M.E. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, Differences from Previous Versions, and Reliability of Some Common Diagnoses. J. Am. Acad. Child Adolesc. Psychiatry 2000, 39, 28–38. [Google Scholar] [CrossRef]
- Spielberger, D.C. STAXI-2 State Trait Anger Expression Inventory-2, Professional Manual; Psychological Assessment Resources: Magdalene, FL, USA, 1999; Available online: https://www.parinc.com/Products/Pkey/429 (accessed on 18 October 2022).
- Amoly, E.; Dadvand, P.; Forns, J.; López-Vicente, M.; Basagaña, X.; Julvez, J.; Alvarez-Pedrerol, M.; Nieuwenhuijsen, M.J.; Sunyer, J. Green and Blue Spaces and Behavioral Development in Barcelona Schoolchildren: The BREATHE Project. Environ. Health Perspect. 2014, 122, 1351–1358. [Google Scholar] [CrossRef] [PubMed]
- Andrusaityte, S.; Grazuleviciene, R.; Dedele, A.; Balseviciene, B. The effect of residential greenness and city park visiting habits on preschool Children’s mental and general health in Lithuania: A cross-sectional study. Int. J. Hyg. Environ. Health 2020, 223, 142–150. [Google Scholar] [CrossRef] [PubMed]
- Balseviciene, B.; Sinkariova, L.; Grazuleviciene, R.; Andrusaityte, S.; Uzdanaviciute, I.; Dedele, A.; Nieuwenhuijsen, M.J. Impact of Residential Greenness on Preschool Children’s Emotional and Behavioral Problems. Int. J. Environ. Res. Public Health 2014, 11, 6757–6770. [Google Scholar] [CrossRef] [PubMed]
- Bijnens, E.M.; Derom, C.; Thiery, E.; Weyers, S.; Nawrot, T.S. Residential green space and child intelligence and behavior across urban, suburban, and rural areas in Belgium: A longitudinal birth cohort study of twins. PLoS Med. 2020, 17, e1003213. [Google Scholar] [CrossRef] [PubMed]
- Feng, X.; Astell-Burt, T. Residential Green Space Quantity and Quality and Child Well-being: A Longitudinal Study. Am. J. Prev. Med. 2017, 53, 616–624. [Google Scholar] [CrossRef]
- Flouri, E.; Midouhas, E.; Joshi, H. The role of urban neighbourhood green space in children’s emotional and behavioural resilience. J. Environ. Psychol. 2014, 40, 179–186. [Google Scholar] [CrossRef]
- Jimenez, M.P.; Aris, I.M.; Rifas-Shiman, S.; Young, J.; Tiemeier, H.; Hivert, M.-F.; Oken, E.; James, P. Early life exposure to greenness and executive function and behavior: An application of inverse probability weighting of marginal structural models. Environ. Pollut. 2021, 291, 118208. [Google Scholar] [CrossRef] [PubMed]
- Madzia, J.; Ryan, P.; Yolton, K.; Percy, Z.; Newman, N.; LeMasters, G.; Brokamp, C. Residential Greenspace Association with Childhood Behavioral Outcomes. J. Pediatr. 2019, 207, 233–240. [Google Scholar] [CrossRef]
- Markevych, I.; Tiesler, C.M.; Fuertes, E.; Romanos, M.; Dadvand, P.; Nieuwenhuijsen, M.J.; Berdel, D.; Koletzko, S.; Heinrich, J. Access to urban green spaces and behavioural problems in children: Results from the GINIplus and LISAplus studies. Environ. Int. 2014, 71, 29–35. [Google Scholar] [CrossRef]
- McEachan, R.R.C.; Yang, T.C.; Roberts, H.; Pickett, K.E.; Arseneau-Powell, D.; Gidlow, C.J.; Wright, J.; Nieuwenhuijsen, M. Availability, use of, and satisfaction with green space, and children’s mental wellbeing at age 4 years in a multicultural, deprived, urban area: Results from the Born in Bradford cohort study. Lancet Planet. Health 2018, 2, e244–e254. [Google Scholar] [CrossRef]
- Mueller, M.A.; Flouri, E.; Kokosi, T. The role of the physical environment in adolescent mental health. Health Place 2019, 58, 102153. [Google Scholar] [CrossRef] [PubMed]
- Liao, J.; Yang, S.; Xia, W.; Peng, A.; Zhao, J.; Li, Y.; Zhang, Y.; Qian, Z.; Vaughn, M.G.; Schootman, M.; et al. Associations of exposure to green space with problem behaviours in preschool-aged children. Int. J. Epidemiol. 2020, 49, 944–953. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.; Kim, S.; Ha, M. Community greenness and neurobehavioral health in children and adolescents. Sci. Total. Environ. 2019, 672, 381–388. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Movassaghi, K.S. The role of greenness of school grounds in student violence in the Chicago public schools. Child. Youth Environ. 2021, 31, 54–82. [Google Scholar] [CrossRef]
- Richardson, E.A.; Pearce, J.; Shortt, N.K.; Mitchell, R. The role of public and private natural space in children’s social, emotional and behavioural development in Scotland: A longitudinal study. Environ. Res. 2017, 158, 729–736. [Google Scholar] [CrossRef] [PubMed]
- Van Aart, C.J.; Michels, N.; Sioen, I.; De Decker, A.; Bijnens, E.M.; Janssen, B.G.; De Henauw, S.; Nawrot, T. Residential landscape as a predictor of psychosocial stress in the life course from childhood to adolescence. Environ. Int. 2018, 120, 456–463. [Google Scholar] [CrossRef]
- Younan, D.; Tuvblad, C.; Li, L.; Wu, J.; Lurmann, F.; Franklin, M.; Berhane, K.; McConnell, R.; Wu, A.H.; Baker, L.A.; et al. Environmental Determinants of Aggression in Adolescents: Role of Urban Neighborhood Greenspace. J. Am. Acad. Child Adolesc. Psychiatry 2016, 55, 591–601. [Google Scholar] [CrossRef]
- Bao, W.-W.; Xue, W.-X.; Jiang, N.; Huang, S.; Zhang, S.-X.; Zhao, Y.; Chen, Y.-C.; Dong, G.-H.; Cai, M.; Chen, Y.-J. Exposure to road traffic noise and behavioral problems in Chinese schoolchildren: A cross-sectional study. Sci. Total. Environ. 2022, 837, 155806. [Google Scholar] [CrossRef]
- Crombie, R.; Clark, C.; Stansfeld, S.A. Environmental noise exposure, early biological risk and mental health in nine to ten year old children: A cross-sectional field study. Environ. Health 2011, 10, 39. [Google Scholar] [CrossRef]
- Essers, E.; Pérez-Crespo, L.; Foraster, M.; Ambrós, A.; Tiemeier, H.; Guxens, M. Environmental noise exposure and emotional, aggressive, and attention-deficit/hyperactivity disorder-related symptoms in children from two European birth cohorts. Environ. Int. 2021, 158, 106946. [Google Scholar] [CrossRef]
- Grelat, N.; Houot, H.; Pujol, S.; Levain, J.-P.; Defrance, J.; Mariet, A.-S.; Mauny, F. Noise Annoyance in Urban Children: A Cross-Sectional Population-Based Study. Int. J. Environ. Res. Public Health 2016, 13, 1056. [Google Scholar] [CrossRef] [PubMed]
- Haines, M.M.; Stansfeld, S.A.; Brentnall, S.; Head, J.; Berry, B.; Jiggins, M.; Hygge, S. The West London Schools Study: The effects of chronic aircraft noise exposure on child health. Psychol. Med. 2001, 31, 1385–1396. [Google Scholar] [CrossRef] [PubMed]
- Haines, M.M.; Stansfeld, S.A.; Job, R.F.S.; Berglund, B.; Head, J. Chronic aircraft noise exposure, stress responses, mental health and cognitive performance in school children. Psychol. Med. 2001, 31, 265–277. [Google Scholar] [CrossRef] [PubMed]
- Haines, M.M.; Stansfeld, S.A.; Job, R.S.; Berglund, B.; Head, J. A follow-up study of effects of chronic aircraft noise exposure on child stress responses and cognition. Leuk. Res. 2001, 30, 839–845. [Google Scholar] [CrossRef]
- Spilski, J.; Rumberg, M.; Berchtold, M.; Bergström, K.; Möhler, U.; Lachmann, T.; Klatte, M. Effects of aircraft noise and living environment on children´s wellbeing and health. In Proceedings of the 23rd International Congress on Acoustics: Integrating 4th EAA Euroregio 2019, Aachen, Germany, 9–13 September 2019; pp. 7080–7087. [Google Scholar] [CrossRef]
- Stansfeld, S.; Berglund, B.; Clark, C.; Lopez-Barrio, I.; Fischer, P.; Öhrström, E.; Haines, M.; Head, J.; Hygge, S.; van Kamp, I.; et al. Aircraft and road traffic noise and children’s cognition and health: A cross-national study. Lancet 2005, 365, 1942–1949. [Google Scholar] [CrossRef]
- Stansfeld, S.; Clark, C.; Cameron, R.; Alfred, T.; Head, J.; Haines, M.; van Kamp, I.; van Kempen, E.; Lopez-Barrio, I. Aircraft and road traffic noise exposure and children’s mental health. J. Environ. Psychol. 2009, 29, 203–207. [Google Scholar] [CrossRef]
- Tiesler, C.M.; Birk, M.; Thiering, E.; Kohlböck, G.; Koletzko, S.; Bauer, C.-P.; Berdel, D.; von Berg, A.; Babisch, W.; Heinrich, J. Exposure to road traffic noise and children’s behavioural problems and sleep disturbance: Results from the GINIplus and LISAplus studies. Environ. Res. 2013, 123, 1–8. [Google Scholar] [CrossRef]
- Gintilienė, G.; Černiauskaitė, D.; Povilaitis, R.; Girdzijauskienė, S.; Lesinskienė, S.; Pūras, D. Lietuviskasis SDQ—Standartizuotas mokyklinio amziaus vaikų “Galiu ir sunkumu klausimynas”. Psichologija 2004, 2, 89–105. [Google Scholar]
- Bandiera, F.C.; Richardson, A.K.; Lee, D.J.; He, J.-P.; Merikangas, K.R. Secondhand Smoke Exposure and Mental Health Among Children and Adolescents. Arch. Pediatr. Adolesc. Med. 2011, 165, 332–338. [Google Scholar] [CrossRef]
- Bauer, N.S.; Anand, V.; Carroll, A.E.; Downs, S.M. Secondhand Smoke Exposure, Parental Depressive Symptoms and Preschool Behavioral Outcomes. J. Pediatr. Nurs. 2014, 30, 227–235. [Google Scholar] [CrossRef]
- World Health Organization. International Classification of Diseases: [9th] Ninth Revision, Basic Tabulation List with Alphabetic Index; World Health Organization: Geneva, Switzerland, 1978; Available online: https://apps.who.int/iris/handle/10665/39473 (accessed on 24 October 2022).
- Gatzke-Kopp, L.; Willoughby, M.T.; Warkentien, S.; Petrie, D.; Mills-Koonce, R.; Blair, C. Association between environmental tobacco smoke exposure across the first four years of life and manifestation of externalizing behavior problems in school-aged children. J. Child Psychol. Psychiatry 2020, 61, 1243–1252. [Google Scholar] [CrossRef] [PubMed]
- Friedman-Weieneth, J.L.; Doctoroff, G.L.; Harvey, E.A.; Goldstein, L.H. The Disruptive Behavior Rating Scale—Parent Version (DBRS-PV): Factor Analytic Structure and Validity among Young Preschool Children. J. Atten. Disord. 2009, 13, 42–55. [Google Scholar] [CrossRef] [PubMed]
- Koth, C.W.; Bradshaw, C.P.; Leaf, P.J. Teacher Observation of Classroom Adaptation—Checklist: Development and Factor Structure. Meas. Evaluation Couns. Dev. 2009, 42, 15–30. [Google Scholar] [CrossRef]
- Karamanos, A.; Mudway, I.; Kelly, F.; Beevers, S.D.; Dajnak, D.; Elia, C.; Cruickshank, J.K.; Lu, Y.; Tandon, S.; Enayat, E.; et al. Air pollution and trajectories of adolescent conduct problems: The roles of ethnicity and racism; evidence from the DASH longitudinal study. Soc. Psychiatry Psychiatr. Epidemiol. 2021, 56, 2029–2039. [Google Scholar] [CrossRef] [PubMed]
- Kelishadi, R.; Babaki, A.E.S.; Qorbani, M.; Ahadi, Z.; Heshmat, R.; Motlagh, M.E.; Ardalan, G.; Ataie-Jafari, A.; Asayesh, H.; Mohammadi, R. Joint Association of Active and Passive Smoking with Psychiatric Distress and Violence Behaviors in a Representative Sample of Iranian Children and Adolescents: The CASPIAN-IV Study. Int. J. Behav. Med. 2015, 22, 652–661. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization, Regional Office for South-East Asia. Global School-Based Student Health Survey GSHS: A Tool for Integrated Youth Behavioral Surveillance; World Health Organization, Regional Office for South-East Asia: New Delhi, India, 2018; Available online: https://apps.who.int/iris/handle/10665/275390 (accessed on 23 October 2022).
- Loftus, C.T.; Ni, Y.; Szpiro, A.A.; Hazlehurst, M.F.; Tylavsky, F.A.; Bush, N.R.; Sathyanarayana, S.; Carroll, K.N.; Young, M.; Karr, C.J.; et al. Exposure to ambient air pollution and early childhood behavior: A longitudinal cohort study. Environ. Res. 2020, 183, 109075. [Google Scholar] [CrossRef]
- Newman, N.C.; Ryan, P.; LeMasters, G.; Levin, L.; Bernstein, D.; Hershey, G.K.K.; Lockey, J.E.; Villareal, M.; Reponen, T.; Grinshpun, S.; et al. Traffic-Related Air Pollution Exposure in the First Year of Life and Behavioral Scores at 7 Years of Age. Environ. Health Perspect. 2013, 121, 731–736. [Google Scholar] [CrossRef]
- Pagani, L.S.; Lévesque-Seck, F.; Archambault, I.; Janosz, M. Prospective longitudinal associations between household smoke exposure in early childhood and antisocial behavior at age 12. Indoor Air 2017, 27, 622–630. [Google Scholar] [CrossRef]
- Park, B.; Park, B.; Kim, E.-J.; Kim, Y.J.; Lee, H.; Ha, E.-H.; Park, H. Longitudinal association between environmental tobacco smoke exposure and behavioral problems in children from ages 5 to 9. Sci. Total. Environ. 2020, 746, 141327. [Google Scholar] [CrossRef]
- Rasnick, E.; Ryan, P.H.; Bailer, A.J.; Fisher, T.; Parsons, P.J.; Yolton, K.; Newman, N.C.; Lanphear, B.P.; Brokamp, C. Identifying sensitive windows of airborne lead exposure associated with behavioral outcomes at age 12. Environ. Epidemiol. 2021, 5, e144. [Google Scholar] [CrossRef]
- Roberts, S.; Arseneault, L.; Barratt, B.; Beevers, S.; Danese, A.; Odgers, C.L.; Moffitt, T.E.; Reuben, A.; Kelly, F.J.; Fisher, H.L. Exploration of NO2 and PM2.5 air pollution and mental health problems using high-resolution data in London-based children from a UK longitudinal cohort study. Psychiatry Res. 2019, 272, 8–17. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM 4, 4th ed.; American Psychiatric Association: Washington, DC, USA, 1994. [Google Scholar]
- Ciucci, E.; Calussi, P.; Menesini, E.; Mattei, A.; Petralli, M.; Orlandini, S. Seasonal variation, weather and behavior in day-care children: A multilevel approach. Int. J. Biometeorol. 2013, 57, 845–856. [Google Scholar] [CrossRef] [PubMed]
- Klimstra, T.A.; Frijns, T.; Keijsers, L.; Denissen, J.J.A.; Raaijmakers, Q.A.W.; van Aken, M.A.G.; Koot, H.M.; van Lier, P.A.C.; Meeus, W.H.J. Come rain or come shine: Individual differences in how weather affects mood. Emotion 2011, 11, 1495–1499. [Google Scholar] [CrossRef]
- Lochman, J.E.; Vernberg, E.; Glenn, A.; Jarrett, M.; McDonald, K.; Powell, N.P.; Abel, M.; Boxmeyer, C.L.; Kassing, F.; Qu, L.; et al. Effects of Autonomic Nervous System Functioning and Tornado Exposure on Long-Term Outcomes of Aggressive Children. Res. Child Adolesc. Psychopathol. 2021, 49, 471–489. [Google Scholar] [CrossRef]
- Jones, S.M.; Molano, A. Seasonal and Compositional Effects of Classroom Aggression: A Test of Developmental-Contextual Models. J. Cogn. Educ. Psychol. 2016, 15, 225–247. [Google Scholar] [CrossRef]
- Dodge, K.A.; Coie, J.D. Social-information-processing factors in reactive and proactive aggression in children’s peer groups. J. Pers. Soc. Psychol. 1987, 53, 1146–1158. [Google Scholar] [CrossRef] [PubMed]
- Lagacé-Séguin, D.G.; D’Entremont, M.L. Weathering the preschool environment: Affect moderates the relations between meteorology and preschool behaviors. Early Child Dev. Care 2005, 175, 379–394. [Google Scholar] [CrossRef]
- Behar, L.B. The Preschool Behavior Questionnaire. J. Abnorm. Child Psychol. 1977, 5, 265–275. [Google Scholar] [CrossRef]
- Muñoz-Reyes, J.A.; Flores-Prado, L.; Beltrami, M. Seasonal differences of aggressive behavior in Chilean adolescents. J. Aggress. Confl. Peace Res. 2014, 6, 129–138. [Google Scholar] [CrossRef]
- Younan, D.; Li, L.; Tuvblad, C.; Wu, J.; Lurmann, F.; Franklin, M.; Berhane, K.; McConnell, R.; Wu, A.H.; Baker, L.A.; et al. Long-Term Ambient Temperature and Externalizing Behaviors in Adolescents. Am. J. Epidemiol. 2018, 187, 1931–1941. [Google Scholar] [CrossRef]
- Ginsburg, H.J.; Pollman, V.A.; Wauson, M.S.; Hope, M.L. Variation of aggressive interaction among male elementary school children as a function of changes in spatial density. J. Nonverbal Behav. 1977, 2, 67–75. [Google Scholar] [CrossRef]
- Loo, C.; Kennelly, D. Social density: Its effects on behaviors and perceptions of preschoolers. J. Nonverbal Behav. 1979, 3, 131–146. [Google Scholar] [CrossRef]
- Loo, C.; Smetana, J. The effects of crowding on the behavior and perception of 10-year-old boys. J. Nonverbal Behav. 1978, 2, 226–249. [Google Scholar] [CrossRef]
- Supplee, L.H.; Unikel, E.B.; Shaw, D.S. Physical environmental adversity and the protective role of maternal monitoring in relation to early child conduct problems. J. Appl. Dev. Psychol. 2007, 28, 166–183. [Google Scholar] [CrossRef]
- Achenbach, T.M.; Rescorla, L.A. Manual for the ASEBA School-Age Forms and Profiles; University of Vermont Research Center for Children, Youth, & Families: Burlington, VT, USA, 2001. [Google Scholar]
- Neill, S.R.S.J. Preschool design and child behaviour. J. Child Psychol. Psychiatry 1982, 23, 309–318. [Google Scholar] [CrossRef] [PubMed]
- Evans, B.E.; Buil, J.M.; Burk, W.J.; Cillessen, A.H.N.; van Lier, P.A.C. Urbanicity is Associated with Behavioral and Emotional Problems in Elementary School-Aged Children. J. Child Fam. Stud. 2018, 27, 2193–2205. [Google Scholar] [CrossRef]
- Erasmus, M.C. Problem Behavior at School Interview; Department of Child and Adolescent Psychiatry: Rotterdam, The Netherlands, 2000. [Google Scholar]
- Handal, P.J.; Hopper, S. Relationship of Sex, Social Class and Rural/Urban Locale to Preschoolers’ AML Scores. Psychol. Rep. 1985, 57, 707–713. [Google Scholar] [CrossRef]
- Durlak, J.A.; Stein, M.A.; Mannarino, A.P. Behavioral validity of a brief teacher rating scale (the AML) in identifying high-risk acting-out schoolchildren. Am. J. Community Psychol. 1980, 8, 101–115. [Google Scholar] [CrossRef]
- Hope, T.L.; Bierman, K.L. Patterns of Home and School Behavior Problems in Rural and Urban Settings. J. Sch. Psychol. 1998, 36, 45–58. [Google Scholar] [CrossRef] [PubMed]
- Achenbach, T.M. Integrative Guide to the 1991 CBCL/4-18, YSR, and TRF Profiles; University of Vermont, Department of Psychology: Burlington, VT, USA, 1991. [Google Scholar]
- Sheridan, S.M.; Koziol, N.A.; Clarke, B.L.; Rispoli, K.M.; Coutts, M.J. The Influence of Rurality and Parental Affect on Kindergarten Children’s Social and Behavioral Functioning. Early Educ. Dev. 2014, 25, 1057–1082. [Google Scholar] [CrossRef]
- Merrell, K.W. Preschool and Kindergarten Behavior Scales, 2nd ed.; Pro-Ed: Austin, TX, USA, 2003. [Google Scholar]
- Gresham, F.M.; Elliott, S.N. The Social Skills Rating System; American Guidance Service: Circle Pines, MN, USA, 1990. [Google Scholar]
- U.S. Department of Health and Human Services. Head Start Family and Child Experiences Survey (FACES); Administration for Children and Families: Washington, DC, USA, 1997–2013. [Google Scholar]
- Wongtongkam, N.; Ward, P.R.; Day, A.; Winefield, A.H. The Relationship Between Exposure to Violence and Anger in Thai Adolescents. J. Interpers. Violence 2015, 31, 2291–2301. [Google Scholar] [CrossRef]
- Loeber, R.; Farrington, D.P.; Stouthamer-Loeber, M.; Moffitt, T.E.; Caspi, A.; White, H.R.; Wei, E.H.; Beyers, J.M. The Development of Male Offending: Key Findings from Fourteen Years of the Pittsburgh Youth Study. In Taking Stock of Delinquency: An Overview of Findings from Contemporary Longitudinal Studies; Thornberry, T.P., Krohn, M.D., Eds.; Kluwer Academic/Plenum Publishers: New York, NY, USA, 2003; pp. 93–136. [Google Scholar]
- Kelder, S.H.; Orpinas, P.; McAlister, A.; Frankowski, R.; Friday, J. The students for peace project: A comprehensive violence-prevention program for middle school students. Am. J. Prev. Med. 1996, 12, 22–30. [Google Scholar] [CrossRef] [PubMed]
- Glod, C.A.; Teicher, M.H.; Butler, M.; Savino, M.; Harper, D.; Magnus, E.; Pahlavan, K. Modifying Quiet Room Design Enhances Calming of Children and Adolescents. J. Am. Acad. Child Adolesc. Psychiatry 1994, 33, 558–566. [Google Scholar] [CrossRef]
- Yudofsky, S.C.; Silver, J.M.; Jackson, W.; Endicott, J.; Williams, D. The Overt Aggression Scale for the objective rating of verbal and physical aggression. Am. J. Psychiatry 1986, 143, 35–39. [Google Scholar] [CrossRef] [PubMed]
- Vakili, H.; Niakan, M.H.; Najafi, N. The Effect of Classroom Red Walls on the Students’ Aggression. Int. J. Sch. Health 2019, in press. [Google Scholar] [CrossRef]
- Buss, A.H.; Perry, M. The Aggression Questionnaire. J. Pers. Soc. Psychol. 1992, 63, 452–459. [Google Scholar] [CrossRef]
- Coyne, S.M.; Padilla-Walker, L.M. Sex, violence, & rock n’ roll: Longitudinal effects of music on aggression, sex, and prosocial behavior during adolescence. J. Adolesc. 2015, 41, 96–104. [Google Scholar] [CrossRef]
- Hinds, P.S. Music: A Milieu Factor with Implications for the Nurse-Therapist. J. Psychosoc. Nurs. Ment. Health Serv. 1980, 18, 28–33. [Google Scholar] [CrossRef]
- Woerner, W.; Fleitlich-Bilyk, B.; Martinussen, R.; Fletcher, J.; Cucchiaro, G.; Dalgalarrondo, P.; Lui, M.; Tannock, R. The Strengths and Difficulties Questionnaire overseas: Evaluations and applications of the SDQ beyond Europe. Eur. Child Adolesc. Psychiatry 2004, 13, II47–II54. [Google Scholar] [CrossRef]
- Hoeksma, J.B.; Sep, S.M.; Vester, F.C.; Groot, P.F.C.; Sijmons, R.; De Vries, J. The electronic mood device: Design, construction, and application. Behav. Res. Methods Instrum. Comput. 2000, 32, 322–326. [Google Scholar] [CrossRef]
- Vernberg, E.M. (University of Kansas, Lawrence, KS, USA); Jacobs, A.K. (University of Kansas, Lawrence, KS, USA). Tornado related traumatic exposure scale. 2005, unpublished manuscript. [Google Scholar]
- Barger, B.; Larson, L.R.; Ogletree, S.; Torquati, J.; Rosenberg, S.; Gaither, C.J.; Bartz, J.M.; Gardner, A.W.; Moody, E. Tree Canopy Coverage Predicts Lower Conduct Problem Severity in Children with ASD. J. Ment. Health Res. Intellect. Disabil. 2020, 13, 43–61. [Google Scholar] [CrossRef]
- Bramlett, M.D.; Blumberg, S.J.; Zablotsky, B.; George, J.M.; Ormson, A.E.; Frasier, A.M.; Santos, K.B. Design and operation of the National Survey of Children’s Health, 2011–2012. Vital Health stat 2017, 59, 1–256. [Google Scholar]
- Durand, V.M.; Mapstone, E. Influence of “Mood-Inducing” Music on Challenging Behavior. Am. J. Ment. Retard. 1997, 102, 367–378. [Google Scholar] [CrossRef]
- Gul, N.; Jameel, H.T.; Mohsin, M.N. Effectiveness of background music on aggressive behavior of intellectually disabled children. Int. J. Incl. Educ. 2019, 3, 49–61. [Google Scholar]
- Oliver, C.; Oxener, G.; Hearn, M.; Hall, S. Effects of social proximity on multiple aggressive behaviors. J. Appl. Behav. Anal. 2001, 34, 85–88. [Google Scholar] [CrossRef]
- West, M.; Melvin, G.; McNamara, F.; Gordon, M. An evaluation of the use and efficacy of a sensory room within an adolescent psychiatric inpatient unit. Aust. Occup. Ther. J. 2017, 64, 253–263. [Google Scholar] [CrossRef]
- Bogar, S.; Beyer, K.M. Green Space, Violence, and Crime: A Systematic Review. Trauma Violence Abus. 2015, 17, 160–171. [Google Scholar] [CrossRef]
- Shepley, M.; Sachs, N.; Sadatsafavi, H.; Fournier, C.; Peditto, K. The Impact of Green Space on Violent Crime in Urban Environments: An Evidence Synthesis. Int. J. Environ. Res. Public Health 2019, 16, 5119. [Google Scholar] [CrossRef]
- Barakat, H.A.-E.; Bakr, A.; El-Sayad, Z. Nature as a healer for autistic children. Alex. Eng. J. 2019, 58, 353–366. [Google Scholar] [CrossRef]
- Li, D.; Larsen, L.; Yang, Y.; Wang, L.; Zhai, Y.; Sullivan, W.C. Exposure to nature for children with autism spectrum disorder: Benefits, caveats, and barriers. Health Place 2019, 55, 71–79. [Google Scholar] [CrossRef]
- Hao, G.; Zuo, L.; Xiong, P.; Chen, L.; Liang, X.; Jing, C. Associations of PM2.5 and road traffic noise with mental health: Evidence from UK Biobank. Environ. Res. 2022, 207, 112221. [Google Scholar] [CrossRef] [PubMed]
- Politte, L.C.; Fitzpatrick, S.E.; Erickson, C. Externalising behaviours in autism spectrum disorder and other neurodevelopmental disorders. In Externalising behaviours: Clinical Features and Treatment Across the Diagnostic Spectrum; American Psychiatric Association Publishing: Washington, DC, USA, 2018; pp. 53–80. [Google Scholar]
- Kanne, S.M.; Mazurek, M. Aggression in Children and Adolescents with ASD: Prevalence and Risk Factors. J. Autism Dev. Disord. 2011, 41, 926–937. [Google Scholar] [CrossRef] [PubMed]
- Ding, N.; Berry, H.L.; Bennett, C.M. The Importance of Humidity in the Relationship between Heat and Population Mental Health: Evidence from Australia. PLoS ONE 2016, 11, e0164190. [Google Scholar] [CrossRef] [PubMed]
- Vida, S.; Durocher, M.; Ouarda, T.B.M.J.; Gosselin, P. Relationship Between Ambient Temperature and Humidity and Visits to Mental Health Emergency Departments in Québec. Psychiatr. Serv. 2012, 63, 1150–1153. [Google Scholar] [CrossRef]
- Tiihonen, J.; Halonen, P.; Tiihonen, L.; Kautiainen, H.; Storvik, M.; Callaway, J. The Association of Ambient Temperature and Violent Crime. Sci. Rep. 2017, 7, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Makinde, O.; Björkqvist, K.; Österman, K. Overcrowding as a risk factor for domestic violence and antisocial behaviour among adolescents in Ejigbo, Lagos, Nigeria. Glob. Ment. Health 2016, 3, e16. [Google Scholar] [CrossRef]
- Aquilina, C. Violence by Psychiatric In-Patients. Med. Sci. Law 1991, 31, 306–312. [Google Scholar] [CrossRef]
- Davis, S. Violence by Psychiatric Inpatients: A Review. Psychiatr. Serv. 1991, 42, 585–590. [Google Scholar] [CrossRef]
- Palmstierna, T.; Huitfeldt, B.; Wistedt, B. The Relationship of Crowding and Aggressive Behavior on a Psychiatric Intensive Care Unit. Psychiatr. Serv. 1991, 42, 1237–1240. [Google Scholar] [CrossRef]
- Nijman, H.L.I.; Rector, G. Crowding and Aggression on Inpatient Psychiatric Wards. Psychiatr. Serv. 1999, 50, 830–831. [Google Scholar] [CrossRef]
- Dzhambov, A.; Dimitrova, D. Urban green spaces′ effectiveness as a psychological buffer for the negative health impact of noise pollution: A systematic review. Noise Health 2014, 16, 157–165. [Google Scholar] [CrossRef] [PubMed]
- Zupancic, T.; Westmacott, C.; Bulthuis, M. The Impact of Green Space on Heat and Air Pollution in Urban Communities: A Meta-Narrative Systematic Review; David Suzuki Foundation: Vancouver, BC, Canada, 2015; Available online: https://davidsuzuki.org/wp-content/uploads/2017/09/impact-green-space-heat-air-pollution-urban-communities.pdf (accessed on 25 March 2021).
- Cohen-Cline, H.; Turkheimer, E.; Duncan, G.E. Access to green space, physical activity and mental health: A twin study. J. Epidemiol. Community Health 2015, 69, 523–529. [Google Scholar] [CrossRef] [PubMed]
- Dadvand, P.; Rivas, I.; Basagaña, X.; Alvarez-Pedrerol, M.; Su, J.; De Castro Pascual, M.; Amato, F.; Jerret, M.; Querol, X.; Sunyer, J.; et al. The association between greenness and traffic-related air pollution at schools. Sci. Total Environ. 2015, 523, 59–63. [Google Scholar] [CrossRef] [PubMed]
- McCracken, D.S.; Allen, D.A.; Gow, A.J. Associations between urban greenspace and health-related quality of life in children. Prev. Med. Rep. 2016, 3, 211–221. [Google Scholar] [CrossRef]
- Li, M.; Van Renterghem, T.; Kang, J.; Verheyen, K.; Botteldooren, D. Sound absorption by tree bark. Appl. Acoust. 2020, 165, 107328. [Google Scholar] [CrossRef]
- Gallent, N.; Gkartzios, M. Defining rurality and the scope of rural planning. In The Routledge Companion to Rural Planning; Scott, M., Gallent, N., Gkartzios, M., Eds.; Routledge: New York, NY, USA, 2019. [Google Scholar]
- Singh, J. Toxic Moulds and Indoor Air Quality. Indoor Built Environ. 2005, 14, 229–234. [Google Scholar] [CrossRef]
- Singh, A.; Daniel, L.; Baker, E.; Bentley, R. Housing Disadvantage and Poor Mental Health: A Systematic Review. Am. J. Prev. Med. 2019, 57, 262–272. [Google Scholar] [CrossRef]
- Evans, G.W. The Built Environment and Mental Health. J. Urban Health 2003, 80, 536–555. [Google Scholar] [CrossRef]
- Bosch, K.A.V.D.; Andringa, T.C.; Peterson, W.; Ruijssenaars, W.A.J.J.M.; Vlaskamp, C. A comparison of natural and non-natural soundscapes on people with severe or profound intellectual and multiple disabilities. J. Intellect. Dev. Disabil. 2017, 42, 301–307. [Google Scholar] [CrossRef]
- Beresford, B.; Oldman, C. Housing Matters: National Evidence Relating to Disabled Children and Their Housing; Policy Press: Bristol, UK, 2002. [Google Scholar]
- Emerson, E. Deprivation, ethnicity and the prevalence of intellectual and developmental disabilities. J. Epidemiol. Community Health 2010, 66, 218–224. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).