Environmental Planning and Non-Communicable Diseases: A Systematic Review on the Role of the Metabolomic Profile
Abstract
1. Introduction
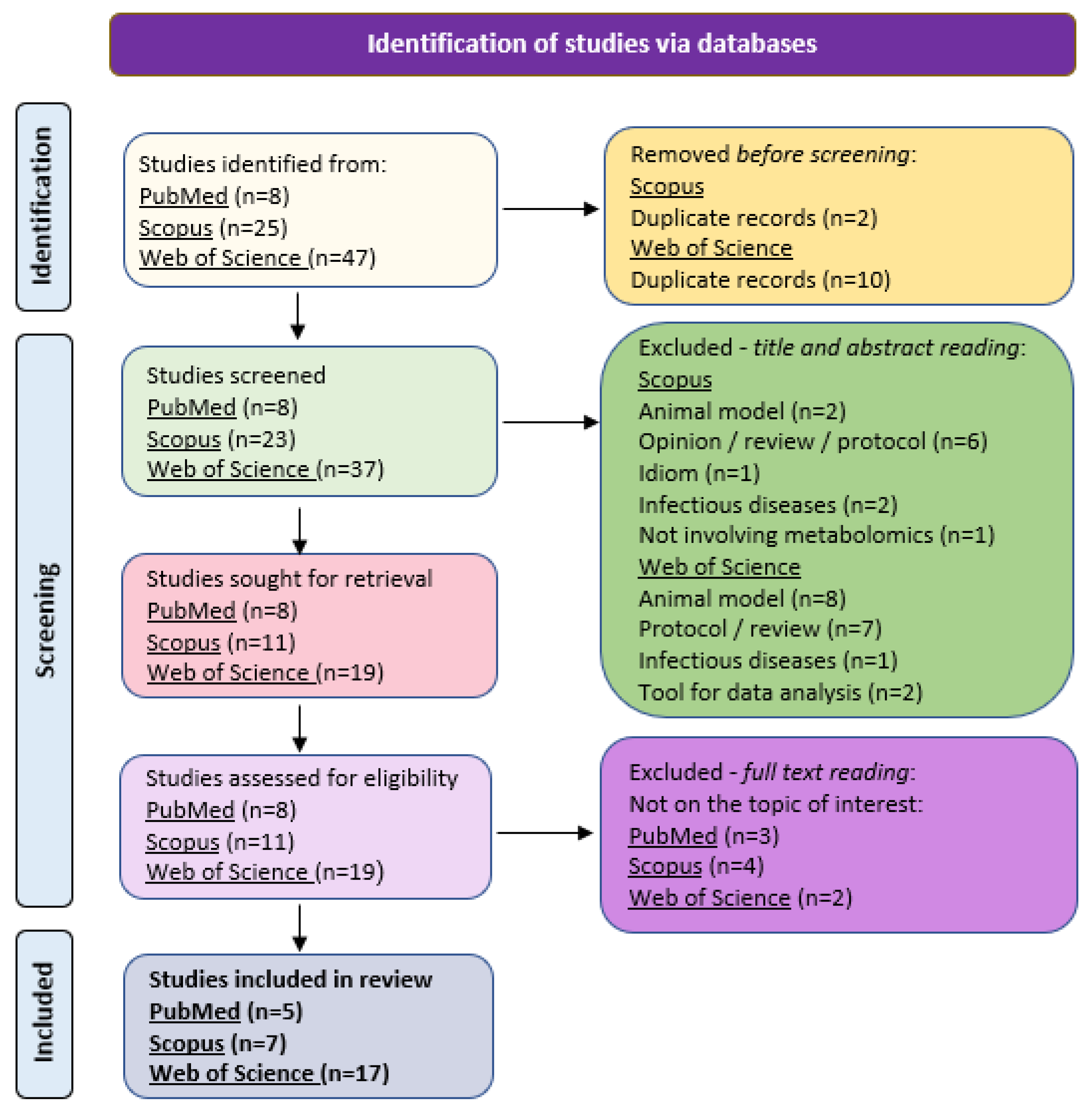
2. Materials and Methods
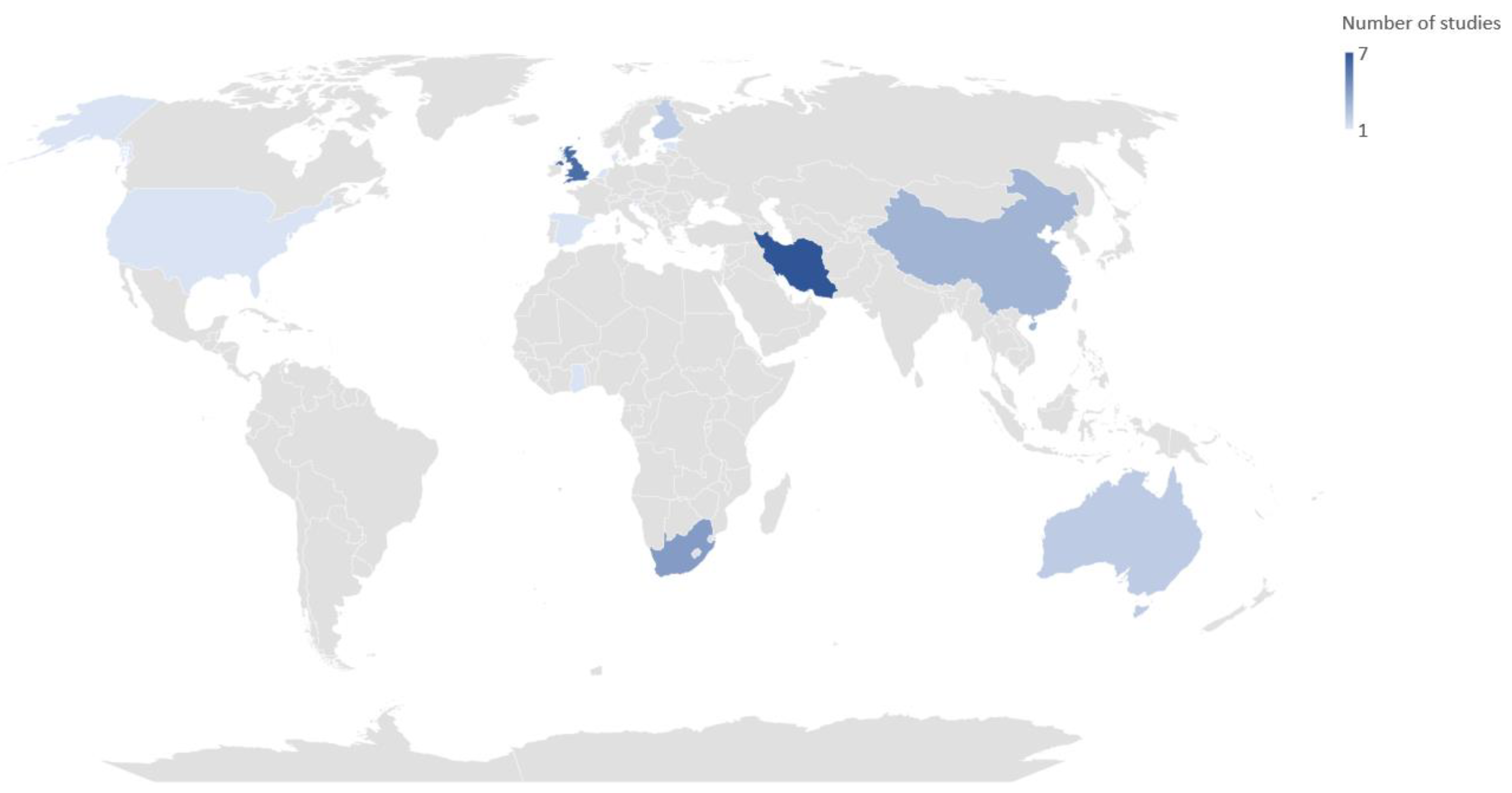
3. Results and Discussion
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhang, A.; Sun, H.; Wang, X. Urinary metabolic profiling of rat models revealed protective function of scoparone against alcohol induced hepatotoxicity. Sci. Rep. 2014, 4, 6768. [Google Scholar] [CrossRef] [PubMed]
- Bagheri, M.; Farzadfar, F.; Qi, L.; Yekaninejad, M.S.; Chamari, M.; Zeleznik, O.A.; Kalantar, Z.; Ebrahimi, Z.; Sheidaie, A.; Koletzko, B.; et al. Obesity-Related Metabolomic Profiles and Discrimination of Metabolically Unhealthy Obesity. J. Proteome Res. 2018, 17, 1452–1462. [Google Scholar] [CrossRef] [PubMed]
- Aderemi, A.V.; Ayeleso, A.O.; Oyedapo, O.O.; Mukwevho, E. Metabolomics: A Scoping Review of Its Role as a Tool for Disease Biomarker Discovery in Selected Non-Communicable Diseases. Metabolites 2021, 11, 418. [Google Scholar] [CrossRef] [PubMed]
- Mastrangelo, A.; Barbas, C. Chronic diseases and lifestyle biomarkers identification by metabolomics. Metab. Fundam. Clin. Appl. 2017, 965, 235–263. [Google Scholar] [CrossRef]
- Brouwer, E.D.; Watkins, D.; Olson, Z.; Goett, J.; Nugent, R.; Levin, C. Provider costs for prevention and treatment of cardiovascular and related conditions in low- and middle-income countries: A systematic review. BMC Public Health 2015, 15, 1183. [Google Scholar] [CrossRef]
- Prüss-Ustün, A.; Van Deventer, E.; Mudu, P.; Campbell-Lendrum, D.; Vickers, C.; Ivanov, I.; Forastiere, F.; Gumy, S.; Dora, C.; Adair-Rohani, H.; et al. Environmental risks and non-communicable diseases. BMJ 2019, 364, l265. [Google Scholar] [CrossRef]
- Forouzanfar, M.H.; Afshin, A.; Alexander, L.T.; Anderson, H.R.; Bhutta, Z.A.; Biryukov, S.; Brauer, M.; Burnett, R.; Cercy, K.; Charlson, F.J.; et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1659–1724. [Google Scholar] [CrossRef]
- Bennett, J.E.; Tamura-Wicks, H.; Parks, R.M.; Burnett, R.T.; Pope, C.A.; Bechle, M.J.; Marshall, J.D.; Danaei, G.; Ezzati, M. Particulate matter air pollution and national and county life expectancy loss in the USA: A spatiotemporal analysis. PLOS Med. 2019, 16, e1002856. [Google Scholar] [CrossRef]
- Howse, E.; Crane, M.; Hanigan, I.; Gunn, L.; Crosland, P.; Ding, D.; Hensher, M.; Rychetnik, L. Air pollution and the noncommunicable disease prevention agenda: Opportunities for public health and environmental science. Environ. Res. Lett. 2021, 16, 065002. [Google Scholar] [CrossRef]
- World Health Organization. SDG Target 3.4 Reduce by One Third Premature Mortality from Non-Communicable Diseases through Prevention and Treatment and Promote Mental Health and Well-Being. 2023. Available online: https://www.who.int/data/gho/data/themes/topics/indicator-groups/indicator-group-details/GHO/sdg-target-3.4-noncommunicable-diseases-and-mental-health (accessed on 2 June 2023).
- Skevaki, C.; Berg, J.V.D.; Jones, N.; Garssen, J.; Vuillermin, P.; Levin, M.; Landay, A.; Renz, H.; Calder, P.C.; Thornton, C.A. Immune biomarkers in the spectrum of childhood noncommunicable diseases. J. Allergy Clin. Immunol. 2016, 137, 1302–1316. [Google Scholar] [CrossRef] [PubMed]
- Franco, M.; Bilal, U.; Diez-Roux, A.V. Preventing non-communicable diseases through structural changes in urban environments. J. Epidemiol. Community Health 2014, 69, 509–511. [Google Scholar] [CrossRef] [PubMed]
- Tawfik, G.M.; Dila, K.A.S.; Mohamed, M.Y.F.; Tam, D.N.H.; Kien, N.D.; Ahmed, A.M.; Huy, N.T. A step by step guide for conducting a systematic review and meta-analysis with simulation data. Trop. Med. Health 2019, 47, 46. [Google Scholar] [CrossRef] [PubMed]
- Rauschert, S.; Mori, T.A.; Beilin, L.J.; Jacoby, P.; Uhl, O.; Koletzko, B.; Oddy, W.H.; Hellmuth, C. Early Life Factors, Obesity Risk, and the Metabolome of Young Adults. Obesity 2017, 25, 1549–1555. [Google Scholar] [CrossRef] [PubMed]
- Ellul, S.; Wake, M.; A Clifford, S.; Lange, K.; Würtz, P.; Juonala, M.; Dwyer, T.; Carlin, J.B.; Burgner, D.P.; Saffery, R. Metabolomics: Population epidemiology and concordance in Australian children aged 11–12 years and their parents. BMJ Open 2019, 9 (Suppl. S3), 106–117. [Google Scholar] [CrossRef]
- Drenos, F.; Smith, G.D.; Ala-Korpela, M.; Kettunen, J.; Würtz, P.; Soininen, P.; Kangas, A.J.; Dale, C.; Lawlor, D.A.; Gaunt, T.R.; et al. Metabolic Characterization of a Rare Genetic Variation Within APOC3 and Its Lipoprotein Lipase–Independent Effects. Circ. Cardiovasc. Genet. 2016, 9, 231–239. [Google Scholar] [CrossRef]
- Hübel, C.; Herle, M.; Ferreira, D.L.S.; Abdulkadir, M.; Bryant-Waugh, R.; Loos, R.J.F.; Bulik, C.M.; Lawlor, D.A.; Micali, N. Childhood overeating is associated with adverse cardiometabolic and inflammatory profiles in adolescence. Sci. Rep. 2021, 11, 12478. [Google Scholar] [CrossRef]
- Yu, X.; Dong, J.; Xiang, S.; Li, X.; Qin, Y.; Zhu, S.; Zheng, J.; Yan, Y.; Mi, J. Association of intestinal microbiota and its metabolite markers with excess weight in Chinese children and adolescents. Pediatr. Obes. 2023, 18, e13019. [Google Scholar] [CrossRef]
- Orrù, S.; Imperlini, E.; Vitucci, D.; Caterino, M.; Mandola, A.; Randers, M.B.; Schmidt, J.F.; Hagman, M.; Andersen, T.R.; Krustrup, P.; et al. Insight into the Molecular Signature of Skeletal Muscle Characterizing Lifelong Football Players. Int. J. Environ. Res. Public Health 2022, 19, 15835. [Google Scholar] [CrossRef]
- Deutsch, L.; Sotiridis, A.; Murovec, B.; Plavec, J.; Mekjavic, I.; Debevec, T.; Stres, B. Exercise and Interorgan Communication: Short-Term Exercise Training Blunts Differences in Consecutive Daily Urine 1H-NMR Metabolomic Signatures between Physically Active and Inactive Individuals. Metabolites 2022, 12, 473. [Google Scholar] [CrossRef]
- Harding, B.N.; Skene, D.J.; Espinosa, A.; Middleton, B.; Castaño-Vinyals, G.; Papantoniou, K.; Navarrete, J.M.; Such, P.; Torrejón, A.; Kogevinas, M.; et al. Metabolic profiling of night shift work—The HORMONIT study. Chrono- Int. 2022, 39, 1508–1516. [Google Scholar] [CrossRef]
- Garcia-Perez, I.; Posma, J.M.; Gibson, R.; Chambers, E.S.; Hansen, T.H.; Vestergaard, H.; Hansen, T.; Beckmann, M.; Pedersen, O.; Elliott, P.; et al. Objective assessment of dietary patterns by use of metabolic phenotyping: A randomised, controlled, crossover trial. Lancet Diabetes Endocrinol. 2017, 5, 184–195. [Google Scholar] [CrossRef]
- Pietzner, M.; Stewart, I.D.; Raffler, J.; Khaw, K.-T.; Michelotti, G.A.; Kastenmüller, G.; Wareham, N.J.; Langenberg, C. Plasma metabolites to profile pathways in noncommunicable disease multimorbidity. Nat. Med. 2021, 27, 471–479. [Google Scholar] [CrossRef] [PubMed]
- Würtz, P.; Cook, S.; Wang, Q.; Tiainen, M.; Tynkkynen, T.; Kangas, A.J.; Soininen, P.; Laitinen, J.; Viikari, J.; Kähönen, M.; et al. Metabolic profiling of alcohol consumption in 9778 young adults. Leuk. Res. 2016, 45, 1493–1506. [Google Scholar] [CrossRef] [PubMed]
- Grace, D. Food Safety in Low and Middle Income Countries. Int. J. Environ. Res. Public Health 2015, 12, 10490–10507. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Imamura, F.; Wedekind, R.; Stewart, I.D.; Pietzner, M.; Wheeler, E.; Forouhi, N.G.; Langenberg, C.; Scalbert, A.; Wareham, N.J. Development and validation of a metabolite score for red meat intake: An observational cohort study and randomized controlled dietary intervention. Am. J. Clin. Nutr. 2022, 116, 511–522. [Google Scholar] [CrossRef]
- Zeng, Y.; Mtintsilana, A.; Goedecke, J.H.; Micklesfield, L.K.; Olsson, T.; Chorell, E. Alterations in the metabolism of phospholipids, bile acids and branched-chain amino acids predicts development of type 2 diabetes in black South African women: A prospective cohort study. Metabolism 2019, 95, 57–64. [Google Scholar] [CrossRef]
- Hosseinkhani, S.; Arjmand, B.; Dilmaghani-Marand, A.; Fateh, S.M.; Dehghanbanadaki, H.; Najjar, N.; Alavi-Moghadam, S.; Ghodssi-Ghassemabadi, R.; Nasli-Esfahani, E.; Farzadfar, F.; et al. Targeted metabolomics analysis of amino acids and acylcarnitines as risk markers for diabetes by LC–MS/MS technique. Sci. Rep. 2022, 12, 8418. [Google Scholar] [CrossRef]
- Sarin, H.V.; Taba, N.; Fischer, K.; Esko, T.; Kanerva, N.; Moilanen, L.; Saltevo, J.; Joensuu, A.; Borodulin, K.; Männistö, S.; et al. Food neophobia associates with poorer dietary quality, metabolic risk factors, and increased disease outcome risk in population-based cohorts in a metabolomics study. Am. J. Clin. Nutr. 2019, 110, 233–245. [Google Scholar] [CrossRef] [PubMed]
- Arjmand, B.; Fana, S.E.; Ghasemi, E.; Kazemi, A.; Ghodssi-Ghassemabadi, R.; Dehghanbanadaki, H.; Najjar, N.; Kakaii, A.; Forouzanfar, K.; Nasli-Esfahani, E.; et al. Metabolic signatures of insulin resistance in non-diabetic individuals. BMC Endocr. Disord. 2022, 22, 212. [Google Scholar] [CrossRef]
- Strauss-Kruger, M.; Kruger, R.; Van Vuren, E.J.; Jacobs, A.; Louw, R.; Mels, C. Identifying a metabolomics profile associated with masked hypertension in two independent cohorts: Data from the African-PREDICT and SABPA studies. Hypertens. Res. 2022, 45, 1781–1793. [Google Scholar] [CrossRef]
- Arjmand, B.; Dehghanbanadaki, H.; Yoosefi, M.; Rezaei, N.; Fateh, S.M.; Ghodssi-Ghassemabadi, R.; Najjar, N.; Hosseinkhani, S.; Tayanloo-Beik, A.; Adibi, H.; et al. Association of plasma acylcarnitines and amino acids with hypertension: A nationwide metabolomics study. PLoS ONE 2023, 18, e0279835. [Google Scholar] [CrossRef] [PubMed]
- Taghizadeh, H.; Emamgholipour, S.; Hosseinkhani, S.; Arjmand, B.; Rezaei, N.; Dilmaghani-Marand, A.; Ghasemi, E.; Panahi, N.; Dehghanbanadaki, H.; Ghodssi-Ghassemabadi, R.; et al. The association between acylcarnitine and amino acids profile and metabolic syndrome and its components in Iranian adults: Data from STEPs 2016. Front. Endocrinol. 2023, 14, 1058952. [Google Scholar] [CrossRef] [PubMed]
- Tareen, S.H.K.; Kutmon, M.; de Kok, T.M.; Mariman, E.C.M.; van Baak, M.A.; Evelo, C.T.; Adriaens, M.E.; Arts, I.C.W. Stratifying cellular metabolism during weight loss: An interplay of metabolism, metabolic flexibility and inflammation. Sci. Rep. 2020, 10, 1651. [Google Scholar] [CrossRef] [PubMed]
- Mendham, A.E.; Goedecke, J.H.; Zeng, Y.; Larsen, S.; George, C.; Hauksson, J.; Smidt, M.C.F.-D.; Chibalin, A.V.; Olsson, T.; Chorell, E. Exercise training improves mitochondrial respiration and is associated with an altered intramuscular phospholipid signature in women with obesity. Diabetologia 2021, 64, 1642–1659. [Google Scholar] [CrossRef] [PubMed]
- Yan, T.; Shi, L.; Xu, K.; Bai, J.; Wen, R.; Liao, X.; Dai, X.; Wu, Q.; Zeng, L.; Peng, W.; et al. Habitual intakes of sugar-sweetened beverages associated with gut microbiota-related metabolites and metabolic health outcomes in young Chinese adults. Nutr. Metab. Cardiovasc. Dis. 2023, 33, 359–368. [Google Scholar] [CrossRef] [PubMed]
- Dugas, L.R.; Chorell, E.; Plange-Rhule, J.; Lambert, E.V.; Cao, G.; Cooper, R.S.; Layden, B.T.; Scholten, D.; Olsson, T.; Luke, A.; et al. Obesity-related metabolite profiles of black women spanning the epidemiologic transition. Metabolomics 2016, 12, 45. [Google Scholar] [CrossRef] [PubMed]
- Bagheri, M.; Djazayery, A.; Farzadfar, F.; Qi, L.; Yekaninejad, M.S.; Aslibekyan, S.; Chamari, M.; Hassani, H.; Koletzko, B.; Uhl, O. Plasma metabolomic profiling of amino acids and polar lipids in Iranian obese adults. Lipids Health Dis. 2019, 18, 94. [Google Scholar] [CrossRef]
- Chashmniam, S.; Ghafourpour, M.; Farimani, A.R.; Gholami, A.; Ghoochani, B.F.N.M. Metabolomic Biomarkers in the Diagnosis of Non-Alcoholic Fatty Liver Disease. Hepat. Mon. 2019, 19, e92244. [Google Scholar] [CrossRef]
- Chashmniam, S.; Mirhafez, S.R.; Dehabeh, M.; Hariri, M.; Nezhad, M.A.; Gh, B.F.N.M. A pilot study of the effect of phospholipid curcumin on serum metabolomic profile in patients with non-alcoholic fatty liver disease: A randomized, double-blind, placebo-controlled trial. Eur. J. Clin. Nutr. 2019, 73, 1224–1235. [Google Scholar] [CrossRef] [PubMed]
- Amiri-Dashatan, N.; Yekta, R.F.; Koushki, M.; Oskouie, A.A.; Esfahani, H.; Taheri, S.; Kazemian, E. Metabolomic study of serum in patients with invasive ductal breast carcinoma with LC-MS/MS approach. Int. J. Biol. Markers 2022, 37, 349–359. [Google Scholar] [CrossRef]
- Li, F.; Qin, X.; Chen, H.; Qiu, L.; Guo, Y.; Liu, H.; Chen, G.; Song, G.; Wang, X.; Li, F.; et al. Lipid profiling for early diagnosis and progression of colorectal cancer using direct-infusion electrospray ionization Fourier transform ion cyclotron resonance mass spectrometry. Rapid Commun. Mass Spectrom. 2012, 27, 24–34. [Google Scholar] [CrossRef] [PubMed]
- Kovalskys, I.; Herscovici, C.R.; Rougier, P.I.; De Gregorio, M.J.; Zonis, L.; Orellana, L. Study Protocol of MINI SALTEN: A technology-based multi-component intervention in the school environment targeting healthy habits of first grade children and their parents. BMC Public Health 2017, 17, 401. [Google Scholar] [CrossRef] [PubMed]
- Kondo, M.C.; Fluehr, J.M.; McKeon, T.; Branas, C.C. Urban Green Space and Its Impact on Human Health. Int. J. Environ. Res. Public Health 2018, 15, 445. [Google Scholar] [CrossRef] [PubMed]
- Astell-Burt, T.; Feng, X. Urban green space, tree canopy, and prevention of heart disease, hypertension, and diabetes: A longitudinal study. Lancet Planet. Health 2019, 3, S16. [Google Scholar] [CrossRef]
- Adhikari, B.; Mishra, S.R.; Dirks, K.N. Green space, health, and wellbeing: Considerations for South Asia. Lancet Planet. Health 2020, 4, e135–e136. [Google Scholar] [CrossRef] [PubMed]
- Astell-Burt, T.; Navakatikyan, M.A.; Walsan, R.; Davis, W.; Figtree, G.; Arnolda, L.; Feng, X. Green space and cardiovascular health in people with type 2 diabetes. Health Place 2021, 69, 102554. [Google Scholar] [CrossRef]
- De la Fuente, F.; Saldías, M.A.; Cubillos, C.; Mery, G.; Carvajal, D.; Bowen, M.; Bertoglia, M.P. Green Space Exposure Association with Type 2 Diabetes Mellitus, Physical Activity, and Obesity: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 97. [Google Scholar] [CrossRef]
- Yang, T.; Gu, T.; Xu, Z.; He, T.; Li, G.; Huang, J. Associations of residential green space with incident type 2 diabetes and the role of air pollution: A prospective analysis in UK Biobank. Sci. Total. Environ. 2023, 866, 161396. [Google Scholar] [CrossRef] [PubMed]
- Shuvo, F.K.; Feng, X.; Akaraci, S.; Astell-Burt, T. Urban green space and health in low and middle-income countries: A critical review. Urban For. Urban Green. 2020, 52, 126662. [Google Scholar] [CrossRef]
- West, J.J.; Smith, S.J.; Silva, R.A.; Naik, V.; Zhang, Y.; Adelman, Z.; Fry, M.M.; Anenberg, S.; Horowitz, L.W.; Lamarque, J.-F. Co-benefits of mitigating global greenhouse gas emissions for future air quality and human health. Nat. Clim. Chang. 2013, 3, 885–889. [Google Scholar] [CrossRef]
| Reference | Population | Intervention | Comparison | Observation |
|---|---|---|---|---|
| Rauschert et al., (2017) [14] | 1024 offspring followed for 20 years (Western Australian Pregnancy Cohort Study) | Retrospective study of breastfeeding duration, anthropometric measures, and metabolomic profile of plasma samples from prenatal to 20 years of age | Association between early life breastfeeding, BMI, WC, and metabolomic profile at 20 years | Metabolomic profile might be influenced by current lifestyle and environmental factors (sex, rather than breastfeeding). Physical activity, genetics, and eating habits may explain the association of maternal and paternal BMI with higher levels of waist circumference and BMI at 20 years of age |
| Ellul et al., (2019) [15] | 1180 Australian children aged 11–12 years and 1325 parents | Cross-sectional study involving analysis of 74 blood biomarkers (amino acid species, lipoprotein subclass measures, lipids, fatty acids, measures related to fatty acid saturation, and composite markers of inflammation and energy homeostasis) | Children and adults, males and females | Aduts presented higher metabolite concentrations than children, and sex differences were also larger in adults when compared to children. There was also considerable evidence of association between parent and child measurements. Identification of risk biomarkers for several non-communicable diseases early in life can provide a target for interventions and follow up with efficacy |
| Drenos et al., (2016) [16] | 13,285 participants of 2 UK population cohorts | Follow-up study with metabolic measures of children collected at ages 7, 15, and 17 years and mothers (at median age of 48 years), as well as women aged 60–79 years old from another cohort | APOC3 and LPL associations | The effects of APOC3(rs138326449) loss of function mutation in lipoprotein metabolism and its potential to affect triglyceride levels were characterized. The association with triglyceride, VLDL, and HDL levels was confirmed, and additional associations with VLDL and HDL composition, other cholesterol measures, and fatty acids were identified. Such an approach is useful for assessing drug targets, particularly in dyslipidemic individuals |
| Hübel et al., (2021) [17] | 3107 adolescents, a subsample of a longitudinal population-based study conducted in the UK | Follow up of parent-reported eating behavior trajectory during childhood | Plasma metabolomic profile at age 16 of subgroups of eating behavior during childhood | Adolescents who used to overeat in childhood presented a metabolic profile characterized by higher lipid concentrations and chronic inflammation. This profile is a risk factor for a variety of NCDs. Children reported to undereat in childhood presented higher concentrations of glutamine in adolescence (an alternative energy substrate when diet lacks energy). Children persistently fussy about eating presented lower concentrations of BCAA (obtained from diet only) |
| Yu et al., (2023) [18] | 163 children aged 6–14 years from Chinese boarding schools | Cross-sectional study on metabolic markers of intestinal microbiota in fecal samples | Normal weight and overweight/obesity | Bifidobacterium, Alistipes, and Megamonas were presented as possible biomarkers to distinguish between children who are overweight/obese and those with normal body weight. Fecal metabolites (especially fatty acids) were significantly altered in obese children. Intestinal microbiota and its related metabolites may play an important role in the development of obesity |
| Orrú et al., (2022) [19] | 9 lifelong male football players and 9 male age-matched (64–71 years old) untrained subjects (Denmark) | Cross-sectional study with muscle biopsies | Protein and metabolite profile of veteran football players and sedentary subjects | Mitochondrial biogenesis is effectively triggered lifelong in football players. Increased concentration of molecules with anti-inflammatory properties was found in veterans when compared to controls. Structured physical activity significantly influences the expression of proteins and metabolites related to successful aging and help reduce the onset of NCDs in the elderly |
| Deutsch et al., (2022) [20] | 20 healthy young male (10 trained and 10 untrained individuals) from Slovenia | 10 days of aerobic training (60 min of supervised cycling) | Exercise performance in and urine metabolomic profile of trained and untrained individuals | Significant multivariate differences were observed in physiological characteristics between trained and untrained groups, pre and post exercise protocol. Cholate, tartrate, cadaverine, lysine, and N6-acetyllisine were the most important metabolites allowing distinguishment between trained and untrained groups. A relatively little effort in terms of exercise invested by the untrained individuals was enough to modify their urine metabolome into an indistinguishable pattern from the trained group, providing a good basis for future recommendations for health maintenance and prevention of NCDs |
| Harding et al., (2022) [21] | 49 males, rotating factory shift workers (Spain) | Cross-sectional study involving metabolomic analysis of plasma samples | Night shift and day shift workers | Working the night shift produced association with changes in metabolites and perturbation of metabolic and biochemical pathways connected to a variety of health outcomes. Levels of several amino acids, glycerophospholipids, and one biogenic amine were higher during the night shift compared to day shift after at least a week of adaptation. Findings support the associations between night shift work and many common NCDs |
| Garcia-Perez et al., (2017) [22] | 19 healthy volunteers, aged 21–65 years old (UK) | Dietary intervention in four 3-day inpatient periods | Urinary metabolic phenotype of subjects after 4 types of diet, varying according to compliance with WHO guidelines | Urinary biomarkers concentrations from healthy foods were significantly higher after the consumption of a diet with better compliance with WHO guidelines to prevent NCDs, reflecting an increased intake of fruits, vegetables, salmon, and chicken. Metabolic phenotyping can provide objective measures of adherence to dietary recommendations without the need for dietary surveys |
| Pietzner et al., (2021) [23] | 11,966 men and women from the EPIC-Norfolk prospective cohort (UK) | Retrospective study of metabolomic profile of patients who died or were hospitalized by NCDs | Plasma metabolomic profile (since 1993–1997) | 420 metabolites were common to at least 2 NCDs, representing 65.5% of all 640 significant metabolite–disease associations. Low-grade inflammation, obesity, smoking, impaired glucose homeostasis, lipoprotein metabolism, and liver and kidney function were identified as common actionable antecedents of NCD multimorbidity, and all of them are potentially preventable early. |
| Würtz et al., (2016) [24] | 9778 young adults from 3 population-based cohorts in Finland | 6-year follow-up study on plasma metabolomics | Individuals with and without usual alcohol consumption | Increased alcohol intake was related to cardiometabolic risk markers in multiple metabolic pathways. The metabolic signature of alcohol consumption involved molecular perturbations linked with higher and lower cardiovascular risk. Many metabolic measures displayed an optimum level at low or moderate alcohol intake. |
| Reference | Population | Intervention | Comparison | Observation |
|---|---|---|---|---|
| Li et al., (2022) [26] | 11,432 males and females aged 40–79 years, plus a randomized crossover intervention with 12 volunteers (UK) | 3-day diet intervention (red meat or nonmeat) followed by 10-day washout period (normal diet), followed by 3-day diet intervention (red meat or nonmeat) | Metabolomic analysis of plasma samples and meat consumption assessed with a 7-day dietary diary | Eleven top-ranked metabolites were associated with red meat intake, suggesting a link between this eating habit and change in these metabolites. Red meat metabolite score was associated with T2D incidence and also potentially associated with other cardiometabolic diseases |
| Zeng et al., (2019) [27] | 476 black women with normal glucose tolerance at baseline and 144 subjects at follow up (South Africa) | Prospective cohort study, follow up for 13 years | Development of T2D, impaired glucose tolerance, or none | Women that developed T2D presented a higher baseline LPC(C18:2):LPE(C18:2) ratio, a different bile acid metabolite profile, and higher levels of leucine, along with its catabolic intermediates (i.e., ketoleucine and C5-carnitine), compared to women that remained normally glucose tolerant during the same period. These metabolite patterns can be useful for identifying and monitoring T2D risk > 10 years prior to the disease onset |
| Hosseinkhani et al., (2022) [28] | 206 diabetic individuals and 206 healthy controls (Iran) | Cross-sectional study involving metabolomic analysis of plasma samples | Diabetic individuals and healthy subjects | Some amino acids and acylcarnitines were considered potential risk markers for diabetes. They reflect disturbances in various metabolic pathways among the diabetic population and can be targeted to prevent, diagnose, and treat this disease |
| Sarin et al., (2019) [29] | Subsample of adults and elderly individuals from the Finnish Dietary, Lifestyle, and Genetic determinants of Obesity and Metabolic Syndrome cohort (n = 2982) and the Estonian Biobank cohort (n = 1109) | Cross-sectional study involving assessment of food neophobia, dietary quality, and plasma metabolomic profile | Association of food neophobia with dietary quality and health-related biomarkers | Food neophobia was significantly associated with many health-related biomarkers, most strongly with ω-3 fatty acids. It was also associated with poor overall dietary quality in Finnish individuals. A high level of food neophobia was associated with increased incidence of T2D in the Finnish cohort, whereas an increased incidence of CHD was detected in the Estonian Biobank cohort |
| Arjmand et al., (2022) [30] | 403 non-diabetic adults (aged 18–75 years) from a population-based study (Iran) | Cross-sectional study involving plasma metabolite profiling | Patients with and without IR | A specific metabolomic profile perturbation is associated with IR. There was a strong positive association between serum BCAAs (valine and leucine), AAAs (tyrosine, tryptophan, and phenylalanine), alanine, and C0 (free carnitine) and IR, while C18:1 (oleoyl L-carnitine) was negatively correlated with IR |
| Strauss-Kruger et al., (2022) [31] | 910 healthy young adults and 210 older adults from 2 independent cohorts in South Africa | Cross-sectional study involving anthropometric measures, dietary intake, and blood pressure and urine metabolomic profiling | Normotensive persons and individuals with masked hypertension | Significant differences were observed between the metabolomic profiles of normotensive and hypertensive adults. They may reflect different stages in the alteration of BCAA metabolism. These changes may be modulated by central adiposity, which indicates that metabolic dysfunction may be an underlying contributor to the etiology of masked hypertension |
| Arjmand et al., (2023) [32] | 1200 Iranian persons aged over 18 years old | Cross-sectional study involving measure of plasma concentrations of 30 acylcarnitines and 20 amino acids using a targeted approach with flow injection tandem mass spectrometry | Persons with normal blood pressure, elevated blood pressure, stage 1 hypertension, and stage 2 hypertension | After adjustment for confounders, 5 metabolites were considered good risk markers for stage 2 hypertension. High plasma levels of carnitines, various acylcarnitines, and low plasma levels of glycine may play a crucial role in the development and progression of hypertension |
| Taghizadeh et al., (2023) [33] | 1192 participants from a large-scale study conducted in Iran, 529 with MetS and 663 without MetS | Cross-sectional study on circulating levels of metabolites (amino acids and acylcarnitines) | Patients with and without MetS | Changes in amino acid and acylcarnitines profiles were observed in patients with MetS. The alteration in circulating levels of acylcarnitines and amino acids followed the increase in MetS component number. Amino acid and acylcarnitines profiles can provide valuable information on evaluating and monitoring MetS risk |
| Reference | Population | Intervention | Comparison | Observation |
|---|---|---|---|---|
| Tareen et al., (2020) [34] | 57 Caucasian participants of a weight loss study conducted in the Netherlands aged 32–67 years | Low- or very-low-calorie diets for 12 and 5 weeks, respectively, plus follow up | Weight loss period and maintenance period | Obese individuals who changed their metabolic profiles in response to caloric restriction had a significant retention of lost weight compared to individuals who did not change it. Cellular metabolism was downregulated during weight loss, with gene expression of all major cellular metabolic processes being lowered during weight loss and maintenance. In parallel, gene expression of immune-system-related processes involving interferons and interleukins increased |
| Mendham et al., (2021) [35] | 35 sedentary obese black South African women aged 20–35 years old | Secondary analysis of a randomized, controlled trial with 12 weeks of combined aerobic and resistance training or control (metabolomic, lipidomic of muscle samples) | Exercise group and sedentary controls | Exercise training altered specific intramuscular lipid intermediates which were associated with content-driven increases in mitochondrial respiration and not whole-body insulin sensitivity or GLUT-4 protein content. Exercise increases lipid utilization in the more bioenergetically active organelles and membranes, which may prevent future skeletal muscle lipotoxicity |
| Yan et al., (2023) [36] | 86 healthy Chinese young adults, 31 men and 55 women | Cross-sectional study involving anthropometry measures, food and drink frequency and lifestyle habits questionnaires, metabolomic and lipid profile analysis of plasma samples | Association between intake of sugar-sweetened beverages and obesity-related, gut-microbiota-related metabolic markers and blood lipids | SSBs were positively associated with obesity-related markers and blood lipids. In contrast, presweetened coffee was negatively associated with the obesity-related traits. A total of 79 metabolites were associated with both SSBs and metabolic markers, particularly obesity markers. Branched-chain amino acid catabolism and aminoacyl-tRNA biosynthesis were identified as links between SSB intake and metabolic health outcomes, relevant to non-communicable diseases |
| Dugas et al., (2016) [37] | Black women from USA (n = 69), South Africa (n = 97), and Ghana (n = 82) | Cross-sectional study involving BMI, physical activity, dietary intake, and metabolomic analysis of plasma samples | Normal weight and obese black women | A common amino acid metabolite profile was associated with obesity in black women from the USA and South Africa but was not detected in Ghanian women. Site-specific, obesity-related metabolites associated with obesity included intermediates in lipid and carbohydrate metabolism, reflecting the populations’ habitual diet. Local environment (and consequently lifestyle factors) seems to be a key moderator of obesity |
| Bagheri et al., (2019) [38] | 200 Iranian obese adults and 100 healthy controls | Cross-sectional study involving plasma metabolomic profiling, arterial blood pressure, anthropometric data, dietary intake, and physical activity | Obese and healthy controls | A metabolomic profile containing 9 amino acids and 10 polar lipids may serve as a potential biomarker of adult obesity. Obese patients had significantly higher blood pressure than controls. No significant associations between metabolites and energy intake or physical activity were observed |
| Bagheri et al., (2018) [2] | 285 Iranian adults aged 18–50 years old | Cross-sectional study with anthropometric data, blood pressure and biochemical measurements, dietary intake, physical activity, and plasma metabolomic analysis | MHO, MUHO, and normal-weight metabolically healthy subjects | Some metabolites discriminated MHO from MUHO and highlighted MHO- and MUHO-related metabolite patterns associated with cardiometabolic biomarkers. Two MHO-associated and three MUHO-linked factors related to more than 75% of the assessed cardiometabolic parameters. BCAAs, glutamic acid, tyrosine, and a specific pattern of lysophosphatidylcholines were associated with risk of both MHO and MUHO phenotypes. A particular pattern of amino acids and choline-containing phospholipids may aid in the identification of metabolic health among obese patients |
| Reference | Population | Intervention | Comparison | Observation |
|---|---|---|---|---|
| Chashmniam et al., (2019) [39] | 36 healthy controls and 37 patients with NAFLD (Iran) | Cross-sectional study involving clinical data, anthropometric measures, and serum metabolomic profiling | Metabolomic profile of healthy controls and patients with NAFLD | Nineteen metabolites were altered in NAFLD patients when compared to control group. Metabolomics biomarkers revealed changes in some amino acids and their derivatives, bile acids, short-chain fatty acids, and tricarboxylic acid cycle intermediates in subjects with NAFLD compared to healthy controls. Precursors of glutathione, glutamine, serine, and glycine were reduced in NAFLD patients. Supplementation of these amino acids might be useful for treatment of this condition. Decreased levels of short-chain fatty acids could be result of altered levels of gut microbiota. Supplementation with probiotics is also recommended |
| Chashmniam et al., (2019) [40] | 45 adults, NAFLD outpatients from an Iranian hospital | 8 weeks of curcumin supplementation, followed by plasma metabolomic profiling, anthropometric, and clinical measures | Curcumin supplementation (50 mg/day) and control (placebo) group | Curcumin intake for 8 weeks in patients with NAFLD had effects in some amino acids, TCA cycle metabolites, gut-microbiota-derived metabolites, and BAs. TCA cycle was the metabolic pathway found to be changed most significantly between groups. A decrease in oxidative and inflammatory mediators was observed with the use of this polyphenol |
| Amiri-Dashatan et al., (2022) [41] | 22 females with invasive ductal breast cancer aged 30–65 years old (Iran) and 10 healthy controls | Cross-sectional study involving plasma metabolomic profiling | Women with invasive ductal carcinoma and healthy controls | The 20 significantly altered metabolites in cancer patients’ samples mostly belonged to amino acids and lipids. Results indicated significant dysregulation of metabolic pathways in breast cancer patients. Their metabolite profile was related to the reprogramming of amino acids and lipid metabolism, mainly arginine and proline metabolism. Metabolomics profiling in breast cancer patients might be useful for identifying biomarkers related to diagnostic and prognosis and also for monitoring treatment |
| Li et al., (2013) [42] | 52 CRC patients and 52 healthy controls (China) | Cross-sectional study involving metabolomic profile of serum samples | CRC patients in early stage, late stage, and healthy subjects | Analyses revealed a successful differentiation of a biomarker panel between CRC patients and healthy controls and revealed signature lipid changes as CRC progresses. The determination of changes during disease progression may provide therapeutic opportunities, such as nutritional support and disease condition monitoring, as well as evaluation of the effectiveness of various treatment options |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oliveira, N.C.d.; Balikian Júnior, P.; Júnior, A.T.d.C.; Bento, E.d.S.; Tonholo, J.; Aquino, T.; Sousa, F.A.d.B.; Araujo, G.G.d.; Ferreira, M.L. Environmental Planning and Non-Communicable Diseases: A Systematic Review on the Role of the Metabolomic Profile. Int. J. Environ. Res. Public Health 2023, 20, 6433. https://doi.org/10.3390/ijerph20146433
Oliveira NCd, Balikian Júnior P, Júnior ATdC, Bento EdS, Tonholo J, Aquino T, Sousa FAdB, Araujo GGd, Ferreira ML. Environmental Planning and Non-Communicable Diseases: A Systematic Review on the Role of the Metabolomic Profile. International Journal of Environmental Research and Public Health. 2023; 20(14):6433. https://doi.org/10.3390/ijerph20146433
Chicago/Turabian StyleOliveira, Natália Cristina de, Pedro Balikian Júnior, Arnaldo Tenório da Cunha Júnior, Edson de Souza Bento, Josealdo Tonholo, Thiago Aquino, Filipe Antonio de Barros Sousa, Gustavo Gomes de Araujo, and Maurício Lamano Ferreira. 2023. "Environmental Planning and Non-Communicable Diseases: A Systematic Review on the Role of the Metabolomic Profile" International Journal of Environmental Research and Public Health 20, no. 14: 6433. https://doi.org/10.3390/ijerph20146433
APA StyleOliveira, N. C. d., Balikian Júnior, P., Júnior, A. T. d. C., Bento, E. d. S., Tonholo, J., Aquino, T., Sousa, F. A. d. B., Araujo, G. G. d., & Ferreira, M. L. (2023). Environmental Planning and Non-Communicable Diseases: A Systematic Review on the Role of the Metabolomic Profile. International Journal of Environmental Research and Public Health, 20(14), 6433. https://doi.org/10.3390/ijerph20146433








