Dynamic Balance and Chest Mobility of Older Adults after Speleotherapy Combined with Pulmonary Rehabilitation, Endurance and Strength Training—A Prospective Study in Chronic Respiratory Diseases
Abstract
1. Introduction
2. Aim
3. Material and Methods
- Age—65 years and above
- Obtaining a min. 10 points in the SPPB (Short Physical Performance Battery) test assessing the risk of disability in the elderly [23].
- Indication for pulmonary rehabilitation with the use of subterraneotherapy methods (chronic respiratory disease) confirmed during qualification by a doctor.
- Having no contraindication for speleotherapy (i.e., cancer, immunosuppressive treatment, severe circulatory failure, clinically active infectious diseases, rheumatic and degenerative diseases of the osteoarticular system, ischemic heart disease with unstable angina or arrhythmia, depression and claustrophobia syndromes, uncontrolled hypertension and unstable diabetes [24]) confirmed during qualification by a doctor.
- Written, informed consent to participate in the project.
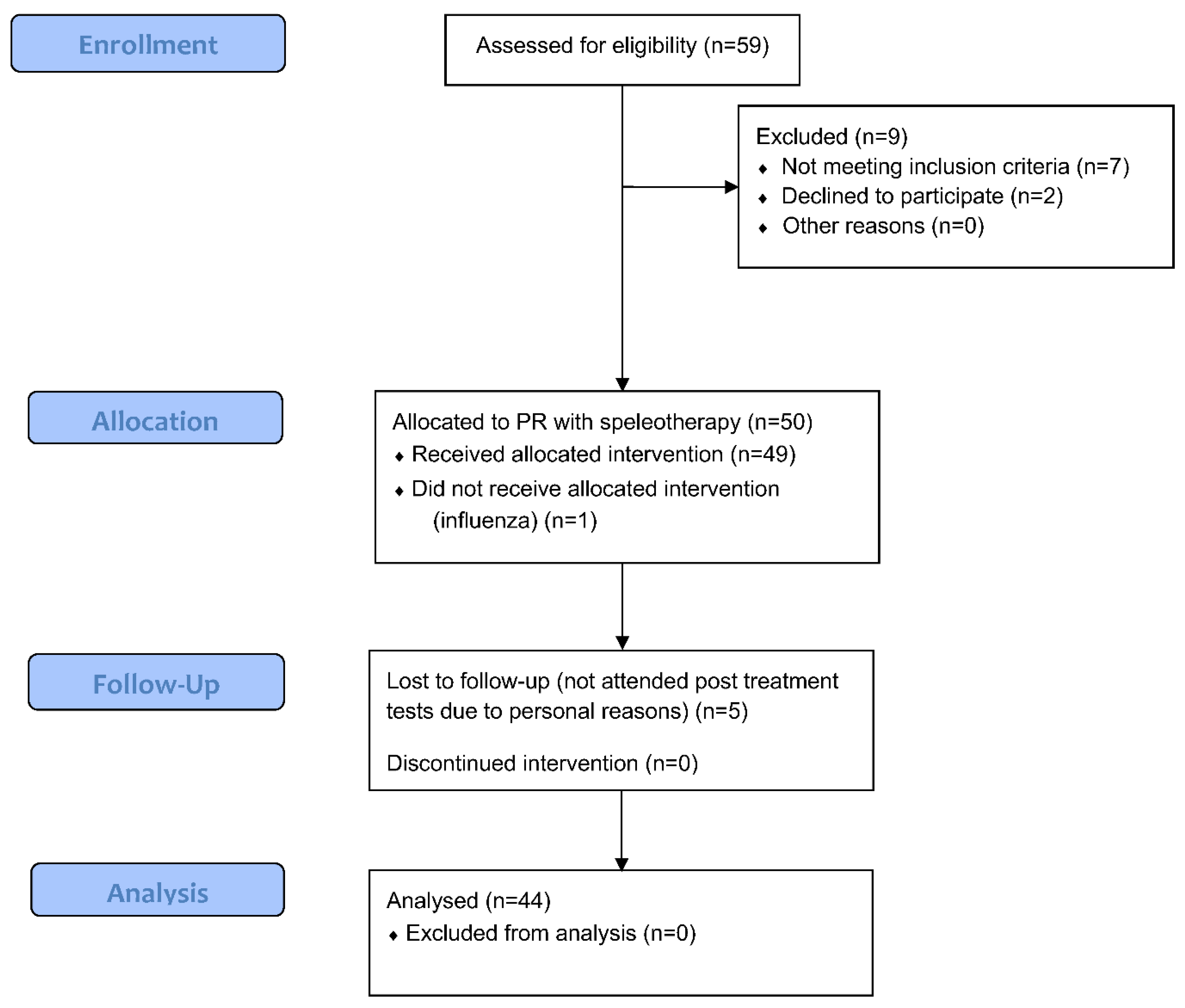
3.1. Study Design
3.2. Four Square Step Test
3.3. Chest Mobility Test
3.4. Speleotherapy
3.5. Pulmonary Rehabilitation Combined with Endurance and Strength Training in Underground Salt Chambers
3.6. Statistical Analysis
4. Results
5. Discussion
6. Limitations
- (1)
- Lack of randomization.
- (2)
- Lack of control group that would implement the same programme overground.
- (3)
- Lack of a representative sample size based on the calculation and research blinding in the initial and final evaluation protocols.
- (4)
- Lack of other performance or health-related measurements, such as body mass, following the 3-week training programme.
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Dominguez, L. Postural control and perturbation response in aging populations: Fall risk implications. J. Neurophysiol. 2020, 124, 1309–1311. [Google Scholar] [CrossRef] [PubMed]
- WHO Global Report on Falls Prevention in Older Age. Available online: https://extranet.who.int/agefriendlyworld/wp-content/uploads/2014/06/WHo-Global-report-on-falls-prevention-in-older-age.pdf (accessed on 25 May 2022).
- Spruit, M.A.; Singh, S.J.; Garvey, C.; ZuWallack, R.; Nici, L.; Rochester, C.; Hill, K.; Holland, A.E.; Lareau, S.C.; Man, W.D.C.; et al. An official American Thoracic Society/European Respiratory Society statement: Key concepts and advances in pulmonary rehabilitation. Am. J. Respir. Crit. Care 2013, 188, 13–64, Erratum in Am. J. Respir. Crit. Care Med. 2014, 189, 1570. [Google Scholar] [CrossRef] [PubMed]
- Canales-Díaz, M.B.; Olivares-Valenzuela, C.; Ramírez-Arriagada, A.; Cruz-Montecinos, C.; Vilaró, J.; Torres-Castro, R.; Núñez-Cortés, R. Clinical Effects of Rehabilitation on Balance in People With Chronic Obstructive Pulmonary Disease: A Systematic Review and Meta-Analysis. Front. Med. 2022, 9, 868316. [Google Scholar] [CrossRef] [PubMed]
- Chuatrakoon, B.; Ngai, S.P.C.; Sungkarat, S.; Uthaikhup, S. Balance Impairment and Effectiveness of Exercise Intervention in Chronic Obstructive Pulmonary Disease-A Systematic Review. Arch. Phys. Med. Rehabil. 2020, 101, 1590–1602. [Google Scholar] [CrossRef]
- Loughran, K.J.; Atkinson, G.; Beauchamp, M.K.; Dixon, J.; Martin, D.; Rahim, S.; Harrison, S.L. Balance impairment in individuals with COPD: A systematic review with meta-analysis. Thorax 2020, 75, 539–546. [Google Scholar] [CrossRef]
- Boontha, N.; Chen, S.; Lin, J.J. Impairment of scapular control in individuals with chronic obstructive pulmonary disease (COPD): Systematic review and meta-analysis. Physiother. Theory Pract. 2022, 1–16. [Google Scholar] [CrossRef]
- Roman, M.A.; Rossiter, H.B.; Casaburi, R. Exercise, ageing and the lung. Eur. Respir. J. 2016, 48, 1471–1486. [Google Scholar] [CrossRef]
- Vaz Fragoso, C.A.; Gill, T.M. Respiratory impairment and the aging lung: A novel paradigm for assessing pulmonary function. J. Gerontol. A Biol. Sci. Med. Sci. 2012, 67, 264–275. [Google Scholar] [CrossRef]
- Dipietro, L.; Campbell, W.W.; Buchner, D.M.; Erickson, K.I.; Powell, K.E.; Bloodgood, B.; Hughes, T.; Day, K.R.; Piercy, K.L.; Vaux-Bjerke, A.; et al. Physical Activity, Injurious Falls, and Physical Function in Aging: An Umbrella Review. Med. Sci. Sports Exerc. 2019, 51, 1303–1313. [Google Scholar] [CrossRef]
- McCarthy, B.; Casey, D.; Devane, D.; Murphy, K.; Murphy, E.; Lacasse, Y. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2015, 23, 2. [Google Scholar] [CrossRef]
- Ries, A.L.; Bauldoff, G.S.; Carlin, B.W.; Casaburi, R.; Emery, C.F.; Mahler, D.A.; Make, B.; Rochester, C.L.; Zuwallack, R.; Herrerias, C. Pulmonary Rehabilitation: Joint ACCP/AACVPR Evidence-Based Clinical Practice Guidelines. Chest 2007, 131 (Suppl. S5), 4S–42S. [Google Scholar] [CrossRef] [PubMed]
- Delbressine, J.M.; Vaes, A.W.; Goërtz, Y.M.; Sillen, M.J.; Kawagoshi, A.; Meijer, K.; Janssen, D.J.A.; Spruit, M.A. Effects of Exercise-Based Interventions on Fall Risk and Balance in Patients With Chronic Obstructive Pulmonary Disease: A SYSTEMATIC REVIEW. J. Cardiopulm Rehabil. Prev. 2020, 40, 152–163. [Google Scholar] [CrossRef] [PubMed]
- Horak, F.B. Postural orientation and equilibrium: What do we need to know about neural control of balance to prevent falls? Age Ageing 2006, 35 (Suppl. S2), ii7–ii11. [Google Scholar] [CrossRef]
- Moore, M.; Barker, K. The validity and reliability of the four square step test in different adult populations: A systematic review. Syst Rev. 2017, 6, 187. [Google Scholar] [CrossRef] [PubMed]
- Woźniak, A.; Nowak, K.; Pełkowska, A.; Rys, K.; Gawlik, J.; Składzień, J. The impact of treatment under subterraneotherapy conditions at the “Wieliczka” Salt Mine Health Resort on the symptoms of diseases of the nose and paranasal sinuses. Pol. Otorhinol. Rev. 2021, 10, 22–27. [Google Scholar]
- Kostrzon, M.; Śliwka, A.; Włoch, T.; Szpunar, M.; Ankowska, D.; Nowobilski, R. Subterranean Pulmonary Rehabilitation in Chronic Obstructive Pulmonary Disease. Adv. Exp. Med. Biol. 2019, 1176, 35–46. [Google Scholar] [CrossRef]
- Kostrzon, M.; Czarnobilski, K.; Czarnobilska, E. The influence of pulmonary rehabilita-tion in the Wieliczka Salt Mine on asthma control—preliminary results. Prz. Lek. 2015, 72, 716–720. [Google Scholar]
- Mętel, S.; Kostrzon, M.; Adamiak, J.; Gattner, H.; Kościelecka, D.; Sosulska, A.; Szczygieł, E.; Golec, J. The influence of speleotherapy combined with pulmonary rehabilitation on functional fitness in older adults—preliminary report. Ther. Adv. Respir. Dis. 2020, 14, 1753466620926952. [Google Scholar] [CrossRef]
- Obtułowicz, K. Mechanisms of theraputic effects of subteranoetherapy in the salt chambers of the Salt Mine in Wieliczka, Poland. Alergol. Immunol. 2013, 10, 26–29. [Google Scholar]
- Kostrzon, M.; Czarnobilski, K.; Badyda, A. Climate characteristics of salt chambers used for therapeutic purposes in the ‘Wieliczka’ Salt Mine. Acta Balneol. 2015, 57, 52–58. [Google Scholar]
- Rogula-Kozłowska, W.; Kostrzon, M.; Rogula-Kopiec, P.; Badyda, A.J. Particulate matter in the air of the underground chamber complex of the “Wieliczka” Salt Mine Health Resort. In Pathology of Pulmonary Disorders; Pokorski, M., Ed.; Series 955, Advances in Experimental Medicine and Biology; Springer International Publishing: Berlin/Heidelberg, Germany, 2016; pp. 9–18. [Google Scholar]
- de Fátima Ribeiro Silva, C.; Ohara, D.G.; Matos, A.P.; Pinto, A.C.P.N.; Pegorari, M.S. Short Physical Performance Battery as a Measure of Physical Performance and Mortality Predictor in Older Adults: A Comprehensive Literature Review. Int. J. Environ. Res. Public Health 2021, 18, 10612. [Google Scholar] [CrossRef] [PubMed]
- Ponikowska, I.; Ferson, D. Nowoczesna Medycyna Uzdrowiskowa; Medi Press: Warsaw, Poland, 2018; pp. 45–46, 191–196. [Google Scholar]
- Schönbach, C. Respiratory Tract, Upper and Lower. In Encyclopedia of Systems Biology; Dubitzky, W., Wolkenhauer, O., Cho, K.H., Yokota, H., Eds.; Springer: New York, NY, USA, 2013. [Google Scholar] [CrossRef]
- Mutchie, H.L.; Orwig, D.L.; Beamer, B.; Conroy, V.; Guralnik, J.; Magaziner, J.; Gruber-Baldini, A.L. Four Square Step Test Performance in Hip Fracture Patients. J. Geriatr. Phys. Ther. 2022, 45, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Dite, W.; Temple, V.A. A clinical test of stepping and change of direction to identify multiple falling older adults. Arch. Phys. Med. Rehabil. 2002, 83, 1566–1571. [Google Scholar] [CrossRef]
- Yazici, O.; Ceylan, E.; Demir Yazici, S.; Tas Gulen, S. Evaluation of balance in patients with chronic obstructive pulmonary disease with practical tests. Int. J. Clin. Pract. 2021, 75, e13901. [Google Scholar] [CrossRef] [PubMed]
- Olsén, M.F.; Lindstrand, H.; Broberg, J.L.; Westerdahl, E. Measuring chest expansion; A study comparing two different instructions. Adv. Ther. 2011, 13, 128–132. [Google Scholar] [CrossRef]
- Ekstrum, J.A.; Black, L.L.; Paschal, K.A. Effects of a Thoracic Mobility and Respiratory Exercise Program on Pulmonary Function and Functional Capacity in Older Adults. Phys. Occup. Ther. 2009, 27, 310–327. [Google Scholar] [CrossRef]
- Malaguti, C.; Rondelli, R.R.; de Souza, L.M.; Domingues, M.; Dal Corso, S. Reliability of Chest Wall Mobility and Its Correlation With Pulmonary Function in Patients With Chronic Obstructive Pulmonary Disease. Respir. Care 2009, 54, 1703–1711. [Google Scholar]
- Moll, J.M.; Wright, V. An objective clinical study of chest expansion. Ann. Rheum Dis. 1972, 31, 1–8. [Google Scholar] [CrossRef]
- Sharma, J.; Senjyu, H.; Williams, L.; White, C. Intra-tester and inter-tester reliability of chest expansion measurement in clients with ankylosing spondylitis and healthy individuals. J. Jpn. Phys. Ther. Assoc. 2004, 7, 23–32. [Google Scholar] [CrossRef]
- Reddy, R.S.; Alahmari, K.A.; Silvian, P.S.; Ahmad, I.A.; Kakarparthi, V.N.; Rengaramanujam, K. Reliability of Chest Wall Mobility and Its Correlation with Lung Functions in Healthy Nonsmokers, Healthy Smokers, and Patients with COPD. Can. Respir. J. 2019, 2019, 5175949. [Google Scholar] [CrossRef]
- Friedl, J.; Huber, D.; Braunschmid, H.; Romodow, C.; Pichler, C.; Weisböck-Erdheim, R.; Mayr, M.; Hartl, A. Winter Exercise and Speleotherapy for Allergy and Asthma: A randomized Controlled Clinical Trial. J. Clin. Med. 2020, 9, 3311. [Google Scholar] [CrossRef] [PubMed]
- Bralewska, K.; Rogula-Kozłowska, W.; Mucha, D.; Badyda, A.J.; Kostrzon, M.; Bralewski, A.; Biedugnis, S. Properties of Particulate Matter in the Air of the Wieliczka Salt Mine and Related Health Benefits for Tourists. Int. J. Environ. Res. Public Health 2022, 19, 826. [Google Scholar] [CrossRef] [PubMed]
- WHO. Every Move Counts towards Better Health—Says WHO. Available online: https://www.who.int/news/item/25-11-2020-every-move-counts-towards-better-health-says-who (accessed on 25 May 2022).
- WHO. Health Topics. Air Pollutions. Available online: https://www.who.int/health-topics/air-pollution#tab=tab_3 (accessed on 25 May 2022).
- Wasik, A.A.; Tuuminen, T. Salt Therapy as a Complementary Method for the Treatment of Respiratory Tract Diseases, with a Focus on Mold-Related Illness. Altern. Ther. Health Med. 2021, 27, 223–239. [Google Scholar] [PubMed]
- La Pier, T.K. Chest Wall Expansion Values in Supine and Standing Across the Adult Lifespan. Phys. Occup. Ther. 2002, 21, 65–81. [Google Scholar] [CrossRef]
- Collins, C.K.; Johnson, V.S.; Godwin, E.M.; Pappas, E. The reliability and validity of the Saliba Postural Classification System. J. Man. Manip. Ther. 2016, 24, 174–181. [Google Scholar] [CrossRef][Green Version]
- Bordoni, B.; Zanier, E. Anatomic connections of the diaphragm: Influence of respiration on the body system. J. Multidiscip. Healthc. 2013, 6, 281–291. [Google Scholar] [CrossRef]
- Kocjan, J.; Gzik-Zroska, B.; Nowakowska, K.; Burkacki, M.; Suchoń, S.; Michnik, R.; Czyżewski, D.; Adamek, M. Impact of diaphragm function parameters on balance maintenance. PLoS ONE 2018, 13, e0208697. [Google Scholar] [CrossRef]
- Cano Porras, D.; Jacobs, J.V.; Inzelberg, R.; Bahat, Y.; Zeilig, G.; Plotnik, M. Patterns of whole-body muscle activations following vertical perturbations during standing and walking. J. Neuroeng. Rehabil. 2021, 18, 75. [Google Scholar] [CrossRef]
- Smith, M.D.; Harvey, E.H.; van den Hoorn, W.; Shay, B.L.; Pereira, G.M.; Hodges, W.P. Out-Patient Pulmonary Rehabilitation Improves Medial-Lateral Balance in Subjects with Chronic Respiratory Disease: Proof-of-Concept Study. Respir. Care 2016, 61, 510–520. [Google Scholar] [CrossRef]


| Time | Timetable |
|---|---|
| 15–20 min | Descent to the mine using a shaft, 700 m group walk to the treatment chambers on uneven surface of miners’ route |
| 30–60 min | Break |
| 30 min | Endurance training: aerobic exercise with or without tools such as sensory balls, elastic bands etc. |
| 60–90 min | Break |
| 30 min | Breathing exercises including breath control strategies, respiratory muscles training, resistive training, chest elasticity exercises with or without tools such feathers, pipes etc. |
| 60–90 min | Break |
| 35 min | Strength training with or without tools/Specialized training using N.A.P. therapy, relaxation methods and others. |
| 30–60 min | Break or educational panel run by medical staff |
| 15–20 min | 700 m group walk to the shaft and ascent to the surface on uneven surface of miners’ route |
| Before Treatment [s] | After Treatment [s] | Difference [s] | t | p | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||||
| Total | 10.2 | 1.9 | 9.1 | 1.7 | 1.1 | 3.9445 | 0.0003 |
| Lower respiratory tract diseases | 10.3 | 1.8 | 9.5 | 2.1 | 0.8 | 2.1495 | 0.0415 |
| Upper respiratory tract diseases | 10.0 | 2.0 | 8.5 | 1.0 | 1.5 | 3.7516 | 0.0016 |
| Before Treatment [cm] | After Treatment [cm] | Difference [cm] | t | p | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||||
| Total | 4.5 | 2.5 | 5.4 | 2.8 | −0.9 | −3.3441 | 0.0017 |
| Lower respiratory tract diseases | 4.6 | 2.7 | 5.5 | 3.0 | −0.9 | −2.4808 | 0.0202 |
| Upper respiratory tract diseases | 4.3 | 2.3 | 5.2 | 2.4 | −0.9 | −2.1902 | 0.0427 |
| Reference to Norms | Before Treatment | After Treatment | χ2 | df | p | |||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | |||||
| Total N = 44 | Below the norms | 22 | 50 | 15 | 34 | 2.2851 | 1 | p > 0.05 |
| Within the norms | 22 | 50 | 29 | 66 | ||||
| Lower respiratory tract disorders N = 26 | Below the norms | 12 | 46 | 9 | 35 | 0.7189 | 1 | p > 0.05 |
| Within the norms | 14 | 54 | 17 | 65 | ||||
| Upper respiratory tract disorders N = 18 | Below the norms | 10 | 56 | 6 | 33 | 1.8000 | 1 | p > 0.05 |
| Within the norms | 8 | 44 | 12 | 67 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mętel, S.; Kostrzon, M.; Adamiak, J. Dynamic Balance and Chest Mobility of Older Adults after Speleotherapy Combined with Pulmonary Rehabilitation, Endurance and Strength Training—A Prospective Study in Chronic Respiratory Diseases. Int. J. Environ. Res. Public Health 2022, 19, 11760. https://doi.org/10.3390/ijerph191811760
Mętel S, Kostrzon M, Adamiak J. Dynamic Balance and Chest Mobility of Older Adults after Speleotherapy Combined with Pulmonary Rehabilitation, Endurance and Strength Training—A Prospective Study in Chronic Respiratory Diseases. International Journal of Environmental Research and Public Health. 2022; 19(18):11760. https://doi.org/10.3390/ijerph191811760
Chicago/Turabian StyleMętel, Sylwia, Magdalena Kostrzon, and Justyna Adamiak. 2022. "Dynamic Balance and Chest Mobility of Older Adults after Speleotherapy Combined with Pulmonary Rehabilitation, Endurance and Strength Training—A Prospective Study in Chronic Respiratory Diseases" International Journal of Environmental Research and Public Health 19, no. 18: 11760. https://doi.org/10.3390/ijerph191811760
APA StyleMętel, S., Kostrzon, M., & Adamiak, J. (2022). Dynamic Balance and Chest Mobility of Older Adults after Speleotherapy Combined with Pulmonary Rehabilitation, Endurance and Strength Training—A Prospective Study in Chronic Respiratory Diseases. International Journal of Environmental Research and Public Health, 19(18), 11760. https://doi.org/10.3390/ijerph191811760







