Abstract
(1) Background: A traumatic birth can lead to the development of childbirth-related posttraumatic stress symptoms or disorder (CB-PTS/D). Literature has identified the risk factors for developing CB-PTS/D within the first six months postpartum thoroughly. However, the impact of mode of birth on CB-PTS/D beyond 6 months postpartum is scarcely studied. (2) Methods: A systematic search of the literature was conducted in the databases PubMed, Embase and CINAHL and PRISMA guidelines were followed. Studies were included if they reported the impact of mode of birth on CB-PTS/D beyond 6 months postpartum. (3) Results: In total, 26 quantitative and 2 qualitative studies were included. In the quantitative studies the percentage of women with CB-PTS/D ranged from 0.7% to 42% (between six months and five years postpartum). Compared with vaginal birth, operative vaginal birth, and emergency caesarean section were associated with CB-PTS/D beyond 6 months postpartum. Qualitative studies revealed that some women were suffering from CB-PTS/D as long as 18 years after birth. (4) Conclusions: Long- term screening of women for PTSD in the postnatal period could be beneficial. More research is needed on models of care that help prevent CB-PTS/D, identifying women at risk and factors that maintain CB-PTS/D beyond 6 months postpartum.
1. Introduction
Childbirth is one of the most profound experiences in a woman’s life and can be positive and empowering, but also stressful or even traumatic [1]. Although post-traumatic stress disorder (PTSD) was originally studied in military veterans, during the last two decades, childbirth has too been recognized as a potentially traumatic event that can lead to PTSD symptoms or even PTSD diagnosis. Experiencing fear and powerlessness during childbirth or, most profoundly, fearing for one’s own life or one’s own child dying can trigger a post-traumatic stress (PTS) response which presents with symptoms such as persistent involuntary and intrusive memories, nightmares, avoidance of certain stimuli, difficulties concentrating and hypervigilance [2,3]. According to the criteria of the Diagnostic and Statistical Manual (DSM-V), PTSD is diagnosed when those symptoms persist for at least one month and interfere with daily functioning. Studies reported that 2% to 9% of new mothers suffer from childbirth-related post-traumatic stress disorder (CB-PTS/D) assessed within a range of 4 weeks to 9 months after childbirth [4,5,6,7].
Childbirth related post traumatic stress symptoms and disorder (CB-PTS/D) do not only affect maternal wellbeing but may also have negative impact on the child and other family members [8]. Severe fear of reliving the traumatic event can result in fear of future childbirth, postponing another pregnancy, or ultimately not having any more children, despite a wish to have them [9].
Furthermore, traumatic childbirth experience can lead to a woman’s avoidance of intimacy, which could eventually be detrimental to the relationship with her partner [9]. Being around the newborn can trigger reliving traumatic birth memories repeatedly, which may have an impact on maternal bonding and result in the mother being emotionally unavailable and unresponsive to her child’s needs [10]. This can all contribute to poor infant sleep, disrupted eating patterns and suboptimal cognitive and emotional development [11,12].
Previous studies have linked CB-PTS/D with unexpected health complications and life threatening situations during childbirth [13,14,15]. Emergency caesarean section (emergency CS) and operative vaginal birth have particularly been found to be associated with CB-PTS/D [14,15], although research in this area is still emerging and the results of the studies are conflicting [16,17]. Nevertheless, not being able to give birth vaginally and having an unplanned CS can be experienced as traumatic, leading to CB-PTS/D [3,18]. As the CS rate almost doubled (rose from 12% to 21% worldwide) between 2000 and 2015 [19], examining the association between mode of birth and CB-PTS/D is warranted.
It must however be pointed out that CB-PTS/D may also develop as a response to physiological, uncomplicated vaginal birth if the subjective experience of childbirth is traumatic, for example due to lack of respect and involvement in decision-making, unsupportive attitude of caregivers and lack of emotional support provided to the laboring woman [4,20,21,22]. Existing studies report a higher risk of CB-PTS/D in primiparous compared to multiparous women [23,24]; other factors that increase the risk for CB-PTS/D include a history of mental health problems, such as depression and anxiety [13,25,26,27], previous PTSD [28] and trauma, such as sexual abuse or domestic violence [26,29].
Previous literature reviews on CB-PTS/D focused on prevention [30], prevalence and risk factors [31,32,33], impact on the couple’s relationship [34], and effects on child development [11,12]. Although several reviews included mode of birth as a potential predictor of CB-PTS/D, to date there is no published review assessing the association between CB-PTS/D and the different mode of birth specifically. A systematic review examining the association between mode of birth and PSTD in the first six months postpartum is underway, [35] but literature summarizing the knowledge regarding the impact of mode of birth on CB-PTS/D beyond this period is lacking. As several studies show a significant number of women suffering from CB-PTS/D [36,37,38] beyond the first six postpartum months, investigating the impact of birth mode on CB-PTS/D in the long term is warranted.
It was therefore the aim of this integrative review to examine the impact of different modes of birth (e.g., vaginal birth, CS) on CB-PTS/D beyond six months postpartum.
2. Materials and Methods
2.1. Type of Review and Search Strategy
To answer our research question, we conducted an integrative review according to the PRISMA guidelines [39]. We searched the following databases to identify articles potentially eligible for this review: PubMed, Embase, and CINAHL. The search included the following keywords: mode of birth (e.g., caesarean section, operative vaginal birth), postpartum period (e.g., postpartum), and PTSD (e.g., post-traumatic stress disorder/symptoms).
The detailed search strategy is presented in the Appendix A. Apart from the studies identified through the systematic search of the databases, we also screened the references listed in the selected studies and added articles identified by a manual search. The search period for publications was limited to the last 30 years (from 1 January 1990 until 17 May 2022). This integrative review was registered in PROSPERO (CRD42020212745).
2.2. Inclusion and Exclusion Criteria
Both quantitative and qualitative studies were eligible for this review. We included English written published articles and did not include results of unpublished data or materials. Studies that recruited women during pregnancy or after childbirth were eligible. We excluded studies reporting results exclusively for women younger than 18 and/or for those with less favorable perinatal outcomes (such as postpartum hemorrhage and premature or low-birth weight newborns), as those conditions are associated with CB-PTS/D [40,41].
Quantitative studies were included if they reported CB-PTS/D measurement scores differentiated by mode of birth and correlations and/or (crude/adjusted) associations between CB-PTS/D and mode of birth. Studies reporting data on the following modes of birth were included: vaginal birth, operative vaginal birth, caesarean section (CS), emergency CS or elective CS.
We included studies assessing CB-PTS/D on the basis of interviews or questionnaires designed in accordance with DSM-IV or DSM-V criteria [42,43], that were either measures of PTSD related to childbirth specifically or measures of PTSD generally related to any traumatic event, with additional questions identifying childbirth as the traumatic event.
Only studies reporting on CB-PTS/D at 6 months postpartum or later, or with a mean time point of 6 months postpartum or more, were included.
2.3. PTSD Symptomatology Criteria
According to the DSM-IV, the PTSD diagnosis is based on the following six criteria (A-F), out of which three are the symptom clusters (B-D). Criterion A identifies the traumatic event. Criterion B describes the re-experiencing/intrusion symptom cluster (e.g., nightmares or intrusive thoughts of the event), where at least one out of five symptoms need to be present to meet the criteria for PTSD diagnosis. Criterion C consists of seven avoidance symptoms (e.g., avoidance of thoughts, places or people associated with the trauma, or inability to recall aspects of the trauma) of which three need to be present. Criterion D describes five hyperarousal symptoms (e.g., difficulties concentrating and hypervigilance) of which two need to be present. Criterion E is fulfilled when the symptoms listed under B, C and D are present for at least one month, and the symptoms need to lead to clinically significant distress or impairment in functioning to fulfill criterion F [42]. Criteria A–F must be present to meet the diagnostic criteria for PTSD diagnosis.
The criteria for PTSD diagnosis have been modified in the DSM-V published in 2013 [44].
In DSM-IV, criterion A, which identifies the traumatic event, consists of two parts: experiencing an event that involved an actual or threatened death or serious injury and the personal response to the event with fear, helplessness or horror. The personal response to the event was removed in DSM-V [43,45]. Additionally, a symptom cluster referring to negative alterations in cognition and mood (e.g., feelings of detachment, inability to experience positive emotions) was added in DSM-V [42,43]. A further description of the DSM-IV and DSM-V criteria and their differences is provided by Pai et al., and in the APA factsheet [43,45].
There are several validated questionnaires and structured interviews that can be used to assess PTSD in accordance with DSM-IV or DSM-V criteria. Although most of the existing questionnaires designed to measure PTSD are related to any type of trauma, there are few questionnaires developed specifically to measure CB-PTS/D [44].
2.4. Selection of Studies
References from the studies identified as potentially eligible for this review were exported to the bibliographic management software Endnote, where a removal of the duplicates was carried out. Subsequently, they were exported to Rayyan, a reference management app for data collection and initial screening of titles and abstracts [46]. Rayyan was used for overall management and storage of the studies including repeated deduplication and removal of non-English articles. A two-step selection process was adopted: in the first step, two researchers (NG, MB) independently screened the titles and abstracts of the articles for their eligibility. The second step consisted of evaluation of full texts of the studies regarding the inclusion and exclusion criteria. Any discrepancy between the researchers were solved by consensus or, if necessary, a third researcher (LT) was consulted to resolve uncertainties about eligibility.
2.5. Quality Assessment
The quality of the studies was assessed by two researchers (NG, MB) independently using the Critical Appraisal Skills Programme (CASP) for quantitative and qualitative studies [47].
The CASP-scoring system developed by Barnett et al. (2012) was used to assess the quality of cohort and cross-sectional studies [48]. The CASP checklist assesses internal validity by appraising potential measurement biases and confounding, and external validity by appraising a potential selection bias and is therefore suitable for both cohort and cross-sectional studies [48,49] (Supplementary Table S1).
The CASP-checklist comprised 12 items which were used to assess the overall quality and assessing the following criteria (1) selection bias; (2) exposure measurement bias (mode of birth); (3) outcome measurement bias (CB-PTS/D); and (4) confounding variables [48] (Supplementary Table S1). A score of either 0 or 1 was given to each criterion. Reason for limitations were defined for each criterion, if studies met one of the limitations they received a score of 0 for the criterion. The sum of given scores ranged from 0 to 4, with score 0–1 representing a low quality, score 2 a modest quality and score 3–4 a high quality [48].
The CASP checklist for qualitative studies is the most commonly used checklist for quality assessment in health-related research [50,51]. It comprises 10 items which were used to assess the overall quality of qualitative studies [52]. The results of the quality assessment were tabulated which is also seen in another review by Burke et al. (2022) [52] (Supplementary Table S2).
2.6. Data Extraction and Management
The following information was extracted from the included articles and reported using the Population, Exposure, Comparator and Outcomes (PECO) framework [53]: author, year of publication, country, population (i.e., number of participants, ethnicity, age and parity), exposure/comparator (mode of birth), outcomes (the measure used for assessing CB-PTS/D including the interval from birth to CB-PTS/D measurement (i.e., ≥6 months), and the main findings. The main findings report crude and adjusted associations expressed as odds ratio with 95% confidence intervals (OR (95% CI) calculated with univariable and multivariable logistic regression analyses. Additionally, we reported correlations (calculated with Spearman Rank- or Pearson correlation coefficient) and comparison of CB-PTS/D measurement scores (calculated with Student’s t-test or ANOVA).
3. Results
3.1. Search
The initial database searches identified 1319 articles of which 310 were identified through PubMed, 775 through Embase and 243 through CINAHL. Out of those articles, the total of 783 remained after removing the duplicates and articles written in languages other than English. After screening the titles and abstracts of the articles against our inclusion/exclusion criteria, a total of 136 articles were deemed eligible. After evaluating the full-texts of those articles, 28 articles were included in this integrative review. The detailed screening and selection process is outlined in a PRISMA flowchart (Figure 1).
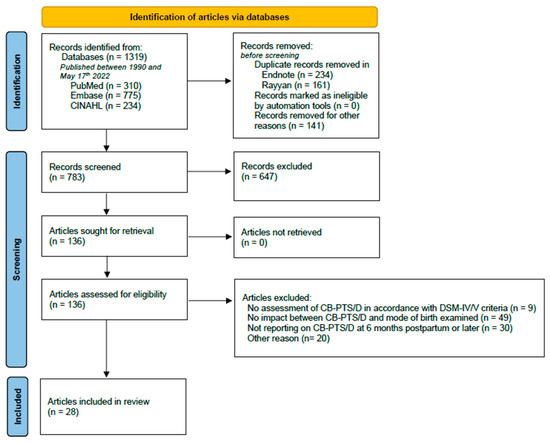
Figure 1.
PRISMA flowchart illustrating the systematic database search and extraction of articles that met the inclusion criteria (MOB: mode of birth).
3.2. Study Characteristics
A total of 28 studies were included in this review. Out of the included studies, 13 were longitudinal prospective cohort studies, 12 cross-sectional studies, one was a retrospective cohort study and two were qualitative studies. The included studies were published between 2004 and 2022, of which 15 studies were published after 2018 (Figure 2). They originated from 11 countries including the United Kingdom, Croatia, France, Netherlands, Turkey, Germany, Spain, United States of America, Australia, Sri Lanka, and New Zealand.
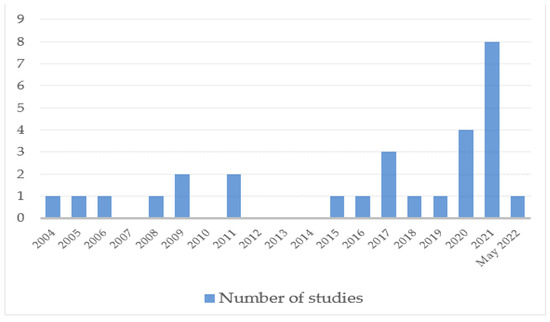
Figure 2.
Number of studies per year.
The sample size ranged from six to 4509. In total, 26 studies reported the prevalence of CB-PTS/D, which ranged from 0.7% to 42%.
Regarding the reported mode of birth in the included studies, four studies examined one mode of birth, i.e., vaginal birth [36,54,55] or emergency caesarean section (emergency CS) [56], whereas two studies examined two modes of birth, i.e., vaginal birth and caesarean section (CS) [22,57]. Six studies differentiated between vaginal birth, operative vaginal birth and CS [37,38,58,59,60,61], whereas three studies differentiated between vaginal birth, elective caesarean section (elective CS) and emergency CS [62,63,64]. Eleven studies distinguished between vaginal birth, operative vaginal birth, elective CS and emergency CS [18,65,66,67,68,69,70,71,72,73]. The two qualitative studies described women’s experiences after vaginal birth and CS [1,9].
In the selected studies, several questionnaires were used to screen for CB-PTS/D. Some were based on the DSM-IV criteria, including the Posttraumatic Diagnostic Scale (PDS) [9,22,38,57,59], PTSD Symptom Scale—self report (PSS-SR) [4,18,68], Traumatic Event Scale (TES) [36,60,61,66], Impact of Event Scale (IES) [36,58,67], Posttraumatic Stress Disorder Checklist (PCL) [65], Post-traumatic checklist scale (PCLS) [56], and Primary Care PTSD Screen (PC-PTSD-IV) [70]. The City Birth Trauma Scale (CityBits) [62,64,67,69,74], PTSD-short scale [54] and Perinatal PTSD Questionnaire (PPQ) [37,55,73,75] were based on the DSM-V criteria.
Five studies administered the questionnaires during an interview with assistance from a healthcare professional [4,9,54,58,62], while 20 studies administered self-report questionnaires sent by postal mail, e-mail or online survey [18,22,36,37,38,55,56,58,59,60,61,64,65,66,67,68,69,70,73,75].
The data collection time ranged from 6 months to 5 years postpartum in the quantitative studies, while it ranged from 6 months until 18 years after childbirth in the qualitative studies. For the detailed information about the included studies see Table 1. In total twelve studies examined (crude or adjusted) associations between mode of birth and CB-PTS/D [22,36,37,38,58,59,61,66,70,72,73,75] (Figure 3).

Table 1.
Overview of included studies in the integrative review.
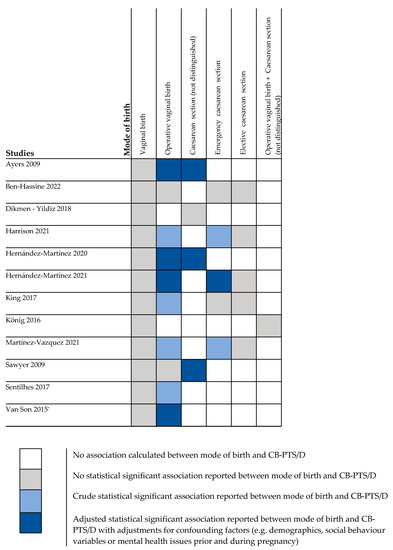
Figure 3.
Associations between mode of birth and CB-PTS/D (≥6 months postpartum). * Significant association reported at 6 months postpartum not at 12 months postpartum.
3.3. Quality of the Studies
The majority of the included quantitative studies were of modest to high quality (Table 2). All qualitative studies met most of the criteria of high methodological quality, except for the criterion related to the description of the role of researcher [1,9]. Detailed quality assessment of the qualitative studies can be found in the Supplementary Table S2.

Table 2.
Quality assessment of the included studies using the Critical Appraisal Skills Programme (CASP) methodology.
3.4. Findings Quantitative Studies
3.4.1. Vaginal Birth
Compared with uncomplicated spontaneous vaginal births, vaginal births with intrapartum interventions and complications were associated with CB-PTS/D. One study found several intrapartum interventions such as administration of an enema, Kristeller maneuver, requirement to give birth in a supine position, artificial rupture of membranes without consent and repeated vaginal examination by different people during vaginal birth to be associated with CB-PTS/D [55]. However, no association was found if the labouring women were informed about those practices in advance and gave informed consent [55].
Moreover, the importance of the place of birth has been emphasized: compared with home births, women who gave birth in the hospital experienced CB-PTS/D more frequently [18,58]. One study focusing on vaginal birth, found that at 3 months post partum PTSD symptoms occurred particularly in women who reported lower physical labour comfort (individual satisfaction). However, lower physical labour comfort had no impact on PTSD symptoms at 6 months postpartum. [54]. One study reported that, although women with spontaneous vaginal birth versus those with other modes of birth, did not experience higher levels of PTSD symptoms, there were still individual women with spontaneous vaginal births who experienced severe PTSD symptoms 6 months postpartum [38].
3.4.2. Operative Vaginal Birth
Eight studies indicated that operative vaginal birth was associated with CB-PTS/D, compared with spontaneous vaginal birth [36,37,38,58,66,70,72,75]. Four of those studies found an association between operative vaginal birth and CB-PTS/D in the univariate analyses, but this association was no longer significant after controlling for confounders such as social behavioral variables [36,66,70,75]. Nevertheless, in other studies the association between operative vaginal birth and CB-PTS/D remained significant even after controlling for confounders [37,38,58,72]. No association was found in one study [73]. One study reported a weak correlation between operative vaginal birth and CB-PTS/D in comparison with spontaneous vaginal birth [58]. Two studies reported statistically significantly higher symptom levels in women after operative vaginal birth compared to elective CS and vaginal birth [67,74] and three studies did not observe a significant effect on symptom scores [4,59,68].
3.4.3. Caesarean Section (CS) (Not Differentiated into Elective and Emergency CS)
Three studies observed associations between CS (not differentiated into elective or emergency) and CB-PTS/D [37,38,59], as compared with vaginal birth Accompanying medical procedures for CS, e.g., general anesthesia, predicted specifically CB-PTS/D [61]. Two studies reported a very weak correlation between CS and CB-PTS/D symptom scores [38,57]. However, two studies did not observe an association [22] or correlation [57] between CS and CB-PTS/D. One study showed that women undergoing CS experienced less pain and had a less negative experience than women with vaginal birth; however, those women experienced more feelings of loneliness, losing control and hopelessness and feelings that correlated with CB-PTS/D at 1 year postpartum [60].
3.4.4. Emergency Caesarean Section and Elective Caesarean Section
Eleven studies differentiated between emergency and elective CS in reporting their results. Three of them found an association between emergency CS and CB-PTS/D [70,72,75] compared with vaginal births. Two studies reported crude associations [70,75] whereas one study reported an adjusted association [72]. Seven studies reported higher CB-PTS/D symptom levels after emergency CS in comparison to other modes of birth [62,64,65,67,69,72,74], whereas two other studies did not find statistically significant elevated symptoms of PTSD in women after emergency CS compared to other modes of birth [58,68].
In two studies, emergency CS was not identified as a predictor of CB-PTS/D [66,73]. In addition, one study including only women with emergency CS, observed that women who experienced low satisfaction with emergency CS versus those experiencing high satisfaction with emergency CS were at higher risk of CB-PTS/D [56].
One study found that women with elective CS had higher levels of PTSD symptoms compared with other modes of birth [4]. Another study reported statistically significant higher symptom scores in women with elective CS compared to those with vaginal birth [69]. However, five studies found no association between elective CS and CB-PTS/D [66,70,72,73,75].
3.5. Findings Qualitative Studies
Two of the included studies were qualitative studies describing women’s experiences of CB-PTS/D. One study gathered information about CB-PTS/D by conducting a semi-structured interview with women (n = 6) [9]. The other study obtained data by sending out e-mails or postal mails, asking women (n = 38) to describe their experience of CB-PTS/D [1]. The qualitative studies suggest that CB-PTS/D can have severe and lasting effects on women’s lives such as struggling to survive each day while suffering from nightmares and flashbacks (i.e., at the moment of sexual penetration) which can lead to the avoidance of intimate relationships and suffering from anxiety, depression, anger and the feeling of isolation from other mothers [1,9].
4. Discussion
This is the first integrative review of the studies examining the impact of mode of birth (i.e., vaginal birth, operative vaginal birth, CS, elective CS and emergency CS) on CB-PTS/D beyond ≥6 months postpartum. The included studies were published from 2004 and 2022, the majority of them were published after 2018 which shows that this topic has attracted considerable clinical attention recently. Overall, the existing studies provide evidence that mode of birth represents a risk factor for CB-PTS/D in the long-term. More specifically, CB-PTS/D has been found to be associated with emergency CS and operative vaginal birth, but under certain circumstances also with elective CS and vaginal birth. Qualitative studies revealed that women were suffering from CB-PTS/D even 18 years after birth [9]. Several studies showed that the percentage of women suffering CB-PTS/D several months and years after childbirth (up to 5 years) remains high. The quantitative studies included in this review reported CB-PTS/D prevalence ranging from 0.7% to 42% in a time-frame of 6 months to 5 years postpartum. On a population level, CB-PTS/D prevalence of 2–9% has been reported in Western countries [4,5,6,7]. In comparison, postpartum depression, the most known psychiatric disorder in the postpartum period, has a prevalence of 17% worldwide [76].
The discrepancy between the CB-PTS/D prevalence found in the studies included in this systematic review and that reported in the literature [4,5,6,7] can be explained by the fact that one study included in this review reported a very high number of women with CB-PTS/D [54]. This study had however a relatively small sample size (n = 102) and used a recently developed measure to screen for PTSD that was not yet used in other studies [54]. Except for this study, the prevalence rate for CB-PTS/D reported in the studies included in this review is consistent with the range reported in the literature. It is not clear yet whether changes in the DSM criteria introduced in DSM-V result in changes in prevalence of CB-PTS/D [44]. Removal of the personal experience from the criterion A, which describes the traumatic event, might increase the number of births considered as traumatic [3,44], which could mean that more women might be diagnosed with CB-PTS/D.
Our integrative review contained a wide range of studies that varied in design, sample size and confounders controlled for. On comparison, it was found that cohort and longitudinal studies had more studies that examined associations between mode of birth and CB-PTS/D, than cross-sectional studies. Also, studies with lower sample size reported fewer associations than studies with a greater sample size. Additionally, some studies adjusted the associations between mode of birth and CB-PTS/D with mental health issues prior and during pregnancy (e.g., depression), the reported adjusted associations showed inconclusive results [22,58,61,70,73].
4.1. Mode of Birth
Compared with uncomplicated spontaneous vaginal births, vaginal births with intrapartum interventions and complications were more likely to be associated with CB-PTS/D [36,37,55,72]. As no association was found when women are informed and give consent before interventions [55], the lack of consent appears to be the precipitating factor and not the birth interventions as such [77].
Conditions under which operative vaginal birth is indicated are often extremely stressful due to the health condition of the mother or the fetus (such as maternal exhaustion or fetal distress) [78], but sometimes also due to lack of communication from healthcare professionals which may lead to a feeling of ‘non-care’, violation and powerlessness [4].
The studies included in this review and other published studies and systematic reviews that assessed short-term impact [15,79,80,81] show that operative vaginal birth is a risk factor for future CB-PTS/D. However, when operative vaginal birth was included in the models using multiple regression or hierarchical regression analyses along with other potential risk factors, it often did not remain a significant predictor of CB-PTS/D [36,66,70,75]. This could be explained by the lack of power due to a small study sample size in some studies [36], pre-existing conditions such as perinatal mental health issues [26], or social factors such as perceived safety during birth and partner support [66] which might be stronger risk factors for CB-PTS/D than mode of birth. Moreover, compassionate, and supportive care provided by the health care professionals may modify the impact of operative vaginal birth on CB-PTS/D [66].
Most of the studies indicated that, compared with vaginal birth, (elective and emergency) CS was associated with CB-PTS/D. Fetal distress and slow progress labour are the two main indications for emergency CS. While CS is a life-saving intervention the stress of the situation it occurs in can eventually increase the risk of CB-PTS/D [16,79,82]. Women who undergo elective CS may still develop PTS/D. Possible explanations for this may include fear of the procedure itself, a high-risk pregnancy, previous birth trauma or lack of support from the health care professionals during the procedure [83]. Also, some women tend to perceive CS as a personal failure [4,84,85]. In contrast, in countries with low medical resources and low CS rates, women who had to undergo medical interventions such as CS may consider themselves privileged to have been able to receive this (possibly) life-saving surgery [60]. In countries with high CS rates, CS is a more acceptable form of delivery [22,86] and this perception can minimize negative psychological consequences. This was potentially the case in the one study where operative vaginal birth and CS were not associated with CB-PTS/D [51]. Also, studies indicated that negative childbirth experiences of family members increase the risk of perceiving one’s own childbirth as traumatic [25,54]. It is important to acknowledge that it is not only support from, and optimal communication with health care professionals, but also the complex intersectional background of each woman that may play a role in the nature of her birth experience, i.e., in the extent to what she experiences operative birth as traumatic. Therefore, it is always important to consider the personal meaning of childbirth, family experiences, and cultural beliefs, in order to understand unique experience of childbirth and prevent trauma wherever possible.
Moreover, the subjective experience of childbirth which is influenced by social support from healthcare professionals plays an important role [21,87]. Personal perception of the extent to which the birthing mother is involved in the decision-making process (including respecting a birth plan) plays an important role in the quality of childbirth experience [37,75,88,89]. Lack of respect for the birth plan from health care professionals was associated with CB-PTS/D in two studies [37,55] as women’s wishes and expectations expressed in their birth plan were not in concordance with the experience they ultimately ended up having [37,55]. Obstetric violence such as verbal abuse from health providers during childbirth was reported to increase the risk of CB-PTS/D [55,68], as well as not being respected [55].
4.2. CB-PTS/D in the Long-Term
The majority of the cohort and longitudinal studies reported a slight decrease of CB-PTS/D over a period of time from baseline to 6 or 10 months [18,54,57,68,73]. These results were published between 2015 and 2022 suggesting that, given awareness regarding CB-PTS/D in both healthcare professionals and public in the last years, women were more likely to receive professional support and help. On the other hand, one longitudinal study and a meta-analysis reported, an increase in prevalence of CB-PTS/D over time from childbirth to 6 months, or from 6 months to 12 months postpartum [58,90]. It was explained that the increase was probably due to postnatal factors, such as sleep deprivation which might postpone CB-PTS/D symptoms onset and/or prevent remission [90]. One qualitative study reported that some women still suffered from CB-PTS/D 18 years postpartum [9]. They had flashbacks and avoided getting pregnant out of fear of reliving the traumatic birth [9]. An increase of the prevalence in CB-PTS/D diagnoses over time was observed in one prospective longitudinal cohort study [58]. This may be due to the development of more serious symptoms in women with partial CB-PTS/D (not full symptom spectrum measured by DSM-IV or V) or by additional traumatic events occurring after birth [83,91] which has also been observed in the studies assessing CB-PTS/D repeatedly up to 6 months [27,91]. However, it has been noted that if the symptoms last more than 6 months, spontaneous recovery is less likely, and the CB-PTS/D may require treatment [92]. One study suggested an association between chronic CB-PTS/D and poor social support after childbirth [26]. Another study stressed that the risk of developing chronic CB-PTS/D is linked with experiencing additional trauma since childbirth [22]. Importantly, when interpreting the course of CB-PTS/D in longitudinal studies, attrition rates should always be taken into consideration as the dropout of (vulnerable) participants can distort the results related to the longitudinal course and prevalence of CB-PTS/D.
4.3. Strengths and Limitations
The key strengths of this integrative review include the focus on the long-term outcomes of mode of birth on CB-PTS/D. Careful identification of the studies that assessed CB-PTS/D using questionnaires or interviews based on DSM-IV and DSM-V criteria is also a strength.
However, several limitations must be noted. First, methodological differences among the included studies, such as non-uniform categorizing of mode of birth (for instance: elective CS and emergency CS vs. CS not differentiated into subtypes), and different research aims and therefore varying emphasis on mode of birth in the individual studies made the comparison between studies challenging. Second, aside from selection bias and response bias in self-reporting questionnaires leading to over- or under-reporting of symptoms, assessing CB-PTS/D with different questionnaires in different studies resulted in varying prevalence rates of CB-PTS/D. Also, studies using clinical interviews versus questionnaires may report higher prevalence of CB-PTS/D [90]. Third, although all CB-PTS/D measures used in the included studies considered childbirth as the trigger for PTSD, some women already fulfilled the criteria for PTSD diagnosis during pregnancy. It is therefore unclear whether childbirth was indeed the trigger of their CB-PTS/D or whether it rather aggravated pre-existing or undiagnosed PTSD or new-onset of PTSD as a response to an event unrelated to childbirth which could coexist with a perceived traumatic childbirth [70].
4.4. Implications for Future Research and Recommendations
More longitudinal studies examining the impact of events occurring in pre-pregnancy, prenatal period on CB-PTS/D are needed. For example, invasive birth interventions such as vaginal examinations could increase the risk of developing CB-PTS/D in women with a history of sexual abuse [49]. According to the estimates by the WHO, 1 in 3 women globally are subjected to sexual violence [93], which means that many women are vulnerable to retraumatisation. Future longitudinal studies should be designed by incorporating the PECO framework: a population of pregnant women (without complications, women with obstetric risk factors or mental health disorders), exposure (birth interventions such as operative vaginal birth, caesarean section, induction or episiotomy), comparator (spontaneous vaginal birth), outcomes (measures of CB-PTS/D) assessed multiple times throughout a period of at least 1 year. Past traumatic life events (e.g., domestic violence), a history of mental health problems (e.g., anxiety or depression) and other risk factors for developing of aggravating CB-PTS/D should be controlled for along with protective factors promoting recovery from CB-PTS/D [22].
5. Conclusions
This integrative review summarizes the existing evidence about the long-term effects of mode of birth on CB-PTS/D. CB-PTS/D appears to be associated with emergency CS and operative vaginal birth. It is however of note that even vaginal birth may elicit severe CB-PTS/D. Therefore, screening for CB-PTS/D in the postnatal period could be of benefit although appropriate tools for and timing of such assessment is yet to be determined. Given its long-term adverse effects, CB-PTS/D should receive similar attention as postpartum depression among health care professionals and general population. Making new mothers familiar with CB-PTS/D might facilitate recognizing the symptoms and seeking professional support and help.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph19148830/s1, Table S1: Tool used for the quality assessment of the cohort and cross-sectional studies, based on Critical Appraisal Skills Programme (CASP) checklist for cohort studies and cross-sectional studies by Barnett et al., 2012; Table S2: Quality assessment of the included qualitative studies based on Critical Appraisal Skills Programme (CASP) Methodology.
Author Contributions
N.G., L.T., M.J.M.B. and L.L.P. were involved in the conceptualization of the integrative systematic review. N.G., M.J.M.B. and L.L.P. developed the search strategy in consultation with all authors. N.G. and M.J.M.B. screened the articles and conducted quality appraisal and data extraction, afterwards discrepancies were discussed with L.T., L.L.P. and N.G. wrote the manuscript under supervision of L.T. and L.L.P. and all other involved authors (M.J.M.B., C.J.M.V. and H.G.D.) made substantial contributions in several review processes. All authors have read and agreed to the published version of the manuscript.
Funding
L.T. was supported by the European Regional Development Fund—Project “Creativity and Adaptability as Conditions of the Success of Europe in an Interrelated World” (No. CZ.02.1.01/0.0/0.0/16_019/0000734).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
We thank Anne-Marie Fanshawe, Department of General Practice & Elderly Medicine, UMCG, for proofreading the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A. Search Strategy
Pubmed
- (“Postpartum Period”[Mesh] OR postpartum[tiab] OR post-partum[tiab] OR puerperium[tiab] OR after childbirth[tiab] OR after birth[tiab] OR after delivery[tiab] OR after labor[tiab] OR after labour[tiab] OR perinatal*[tiab] OR postnatal*[tiab] OR after birth[tiab] OR following childbirth[tiab] OR following birth[tiab] OR following delivery[tiab] OR following labour[tiab] OR following labor[tiab] OR subsequent pregnancy[tiab] OR multiparous[tiab])
AND
- (“Delivery, Obstetric/adverse effects”[Mesh] OR “Delivery, Obstetric/methods”[Mesh] OR “Parturition/adverse effects”[Mesh] OR “Delivery, Obstetric/psychology”[Mesh] OR “Parturition/psychology”[Mesh] OR “Labor Pain”[Mesh] OR “Labor Presentation”[Mesh] OR ((mode[tiab] OR modes[tiab] OR route*[tiab] OR type*[tiab] OR vaginal[tiab] OR morbid*[tiab]) AND (labor[tiab] OR labour[tiab] OR delivery[tiab] OR birth[tiab] OR childbirth[tiab])) OR method of birth[tiab] OR method of delivery[tiab] OR instrumental delivery[tiab] OR episiotom*[tiab] OR caesarean[tiab] OR c-section[tiab])
AND
- (“Stress Disorders, Post-Traumatic”[Mesh] OR posttraumatic[tiab] OR post-traumatic[tiab] OR ptss[tiab] OR PTSD[tiab])
CINAHL
- (MH “Postnatal Period+”) OR postpartum OR post-partum OR puerperium OR after childbirth OR after birth OR after delivery OR after labor OR after labour OR perinatal OR postnatal OR after birth OR following childbirth OR following birth OR following delivery OR following labour OR following labor OR subsequent pregnancy OR multiparous
AND
- (MH “Delivery, Obstetric+”) OR (MH “Labor+”) OR (MH “Labor Pain”) OR (MH “Labor Presentation+”) OR ((mode OR modes OR route* OR type* OR vaginal OR morbid*) AND (labor OR labour OR delivery OR birth OR childbirth)) OR method of birth OR method of delivery OR instrumental delivery OR episiotom OR caesarean OR c-section)
AND
- (MH “Stress Disorders, Post-Traumatic+”) OR posttraumatic OR post-traumatic OR ptss OR PTSD)
Embase:
- (‘puerperium’/exp OR ((‘Postpartum’ OR ‘post-partum’ OR ‘puerperium’ OR ‘after birth’ OR ‘after delivery’ OR ‘after labor’ OR ‘after labour’ OR ‘perinatal*’ OR ‘postnatal*’ OR ‘after birth’ OR ‘after childbirth’ OR ‘following childbirth’ OR ‘following birth’ OR ‘following delivery’ OR ‘following labour’ OR ‘following labor’ OR ‘subsequent pregnancy’):ab,ti))
AND
- (‘obstetric delivery’/exp OR ‘birth’/exp OR ‘labor pain’/exp OR (((‘mode’ OR ‘modes’ OR ‘route’ OR ‘type’ OR ‘vaginal’ OR ‘morbid’) AND (‘labor’ OR ‘labour’ OR ‘delivery’ OR ‘birth’ OR ‘childbirth’)) OR ‘method of birth’ OR ‘method of delivery’ OR ‘instrumental delivery’ OR ‘episiotom*’ OR ‘caesarean’ OR ‘c-section’):ab,ti)
AND
- (‘posttraumatic stress disorder’/exp OR ((‘Posttraumatic’ OR ‘post-traumatic’ OR ‘ptss’ OR ‘PTSD’):ab,ti))
AND
- (‘cohort analysis’/exp OR ‘case control study’/exp OR ‘cross-sectional study’/exp OR ‘risk’/exp OR ‘questionnaire’/exp OR (‘prospectiv*’ OR ‘follow-up’ OR ‘longitudinal*’ OR ‘risk’ OR ‘associat*’ OR ‘relat*’ OR ‘influenc*’ OR ‘predict*’ OR ‘questionnair*’ OR ‘cohort’ OR ‘case-control’ OR ‘crosssectional*’ OR ‘cross-sectional*’ OR ‘longterm’ OR ‘long-term’):ab,ti)
References
- Beck, C.T. Post-traumatic stress disorder due to childbirth: The aftermath. Nurs. Res. 2004, 53, 216–224. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lancaster, C.; Teeters, J.; Gros, D.; Back, S. Posttraumatic Stress Disorder: Overview of Evidence-Based Assessment and Treatment. J. Clin. Med. 2016, 5, 105. [Google Scholar] [CrossRef] [PubMed]
- Boorman, R.J.; Devilly, G.J.; Gamble, J.; Creedy, D.K.; Fenwick, J. Childbirth and criteria for traumatic events. Midwifery 2014, 30, 255–261. [Google Scholar] [CrossRef]
- Beck, C.T.; Gable, R.K.; Sakala, C.; Declercq, E.R. Posttraumatic Stress Disorder in New Mothers: Results from a Two-Stage U.S. National Survey. Birth 2011, 38, 216–227. [Google Scholar] [CrossRef] [PubMed]
- Grekin, R.; O’Hara, M.W. Prevalence and risk factors of postpartum posttraumatic stress disorder: A meta-analysis. Clin. Psychol. Rev. 2014, 34, 389–401. [Google Scholar] [CrossRef]
- Denis, A.; Parant, O.; Callahan, S. Post-traumatic stress disorder related to birth: A prospective longitudinal study in a French population. J. Reprod. Infant Psychol. 2011, 29, 125–135. [Google Scholar] [CrossRef]
- Ford, E.; Ayers, S. Support during birth interacts with prior trauma and birth intervention to predict postnatal post-traumatic stress symptoms. Psychol. Health 2011, 26, 1553–1570. [Google Scholar] [CrossRef] [Green Version]
- Ayers, S.; Bond, R.; Bertullies, S.; Wijma, K. The aetiology of post-traumatic stress following childbirth: A meta-analysis and theoretical framework. In Psychological Medicine; Cambridge University Press: Cambrigde, MA, USA, 2016; Volume 46, pp. 1121–1134. [Google Scholar]
- Ayers, S.; Eagle, A.; Waring, H. The effects of childbirth-related post-traumatic stress disorder on women and their relationships: A qualitative study. Psychol. Health Med. 2006, 11, 389–398. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davies, J.; Slade, P.; Wright, I.; Stewart, P. Posttraumatic stress symptoms following childbirth and mothers’ perceptions of their infants. Infant Ment. Health J. 2008, 29, 537–554. [Google Scholar] [CrossRef] [PubMed]
- Pierrehumbert, B.; Nicole, A.; Muller-Nix, C.; Forcada-Guex, M.; Ansermet, F. Parental post-traumatic reactions after premature birth: Implications for sleeping and eating problems in the infant. Arch. Dis. Child. Fetal Neonatal Ed. 2003, 88, F400–F404. [Google Scholar] [CrossRef]
- McKenzie-McHarg, K.; Ayers, S.; Ford, E.; Horsch, A.; Jomeen, J.; Sawyer, A.; Stramrood, C.; Thomson, G.; Slade, P. Post-traumatic stress disorder following childbirth: An update of current issues and recommendations for future research. J. Reprod. Infant Psychol. 2015, 33, 219–237. [Google Scholar] [CrossRef] [Green Version]
- Shaban, Z.; Dolatian, M.; Shams, J.; Majd, H.A.; Mahmoodi, Z. Post-traumatic stress disorder (PTSD) after childbirth: Prevalence and contributing factors. Iran. Red Crescent Med. J. 2013, 15, 177. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Modarres, M.; Afrasiabi, S.; Rahnama, P.; Montazeri, A. Prevalence and risk factors of childbirth-related post-traumatic stress symptoms. BMC Pregnancy Childbirth 2012, 12, 88. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Söderquist, J.; Wijma, K.; Wijma, B. Traumatic stress after childbirth: The role of obstetric variables. J. Psychosom. Obstet. Gynecol. 2002, 23, 31–39. [Google Scholar] [CrossRef]
- Cohen, M.M.; Ansara, D.; Schei, B.; Stuckless, N.; Stewart, D.E. Posttraumatic stress disorder after pregnancy labor, and delivery. J. Women’s Health 2004, 13, 315–324. [Google Scholar] [CrossRef]
- Srkalović Imširagić, A.; Begić, D.; Šimičević, L.; Bajić, Ž. Prediction of posttraumatic stress disorder symptomatology after childbirth—A Croatian longitudinal study. Women Birth 2017, 30, e17–e23. [Google Scholar] [CrossRef]
- Haagen, J.F.G.; Moerbeek, M.; Olde, E.; van der Hart, O.; Kleber, R.J. PTSD after childbirth: A predictive ethological model for symptom development. J. Affect. Disord. 2015, 185, 135–143. [Google Scholar] [CrossRef]
- Boerma, T.; Ronsmans, C.; Melesse, D.Y.; Barros, A.J.D.; Barros, F.C.; Juan, L.; Moller, A.B.; Say, L.; Hosseinpoor, A.R.; Yi, M.; et al. Global epidemiology of use of and disparities in caesarean sections. Lancet 2018, 392, 1341–1348. [Google Scholar] [CrossRef]
- Kitzinger, S.; Green, J.M.; Chalmers, B.; Keirse, M.J.N.C.; Lindstrom, K.; Hemminki, E. Why Do Women Go Along with This Stuff? Birth 2006, 33, 154–158. [Google Scholar] [CrossRef]
- Thomson, G.M.; Downe, S. Changing the future to change the past: Women’s experiences of a positive birth following a traumatic birth experience. J. Reprod. Infant Psychol. 2010, 28, 102–112. [Google Scholar] [CrossRef]
- Dikmen-Yildiz, P.; Ayers, S.; Phillips, L. Longitudinal trajectories of post-traumatic stress disorder (PTSD) after birth and associated risk factors. J. Affect. Disord. 2018, 229, 377–385. [Google Scholar] [CrossRef] [PubMed]
- Angelini, C.R.; Pacagnella, R.C.; Parpinelli, M.A.; Silveira, C.; Andreucci, C.B.; Ferreira, E.C.; Santos, J.P.; Zanardi, D.M.; Souza, R.T.; Cecatti, J.G. Post-traumatic stress disorder and severe maternal morbidity: Is there an association? Clinics 2018, 73, e309. [Google Scholar] [CrossRef] [PubMed]
- Stramrood, C.A.I.; Paarlberg, K.M.; Huis In’T Veld, E.M.J.; Berger, L.W.A.R.; Vingerhoets, A.J.J.M.; Weijmar Schultz, W.C.M.; Pampus, M.G. Posttraumatic stress following childbirth in homelike-and hospital settings. J. Psychosom. Obstet. Gynecol. 2011, 32, 88–97. [Google Scholar] [CrossRef] [PubMed]
- Zambaldi, C.F.; Cantilino, A.; Sougey, E.B. Bio-socio-demographic factors associated with post-traumatic stress disorder in a sample of postpartum Brazilian women. Arch. Women’s Ment. Health 2011, 14, 435–439. [Google Scholar] [CrossRef] [PubMed]
- Verreault, N.; da Costa, D.; Marchand, A.; Ireland, K.; Banack, H.; Dritsa, M.; Khalifé, S. PTSD following childbirth: A prospective study of incidence and risk factors in Canadian women. J. Psychosom. Res. 2012, 73, 257–263. [Google Scholar] [CrossRef] [PubMed]
- Zaers, S.; Waschke, M.; Ehlert, U. Depressive symptoms and symptoms of post-traumatic stress disorder in women after childbirth. J. Psychosom. Obstet. Gynecol. 2008, 29, 61–71. [Google Scholar] [CrossRef]
- Seng, J.S.; Sperlich, M.; Low, L.K.; Ronis, D.L.; Muzik, M.; Liberzon, I. Childhood Abuse History, Posttraumatic Stress Disorder, Postpartum Mental Health, and Bonding: A Prospective Cohort Study. J. Midwifery Women’s Health 2013, 58, 57–68. [Google Scholar] [CrossRef]
- Sexton, M.B.; Hamilton, L.; McGinnis, E.W.; Rosenblum, K.L.; Muzik, M. The roles of resilience and childhood trauma history: Main and moderating effects on postpartum maternal mental health and functioning. J. Affect. Disord. 2015, 174, 562–568. [Google Scholar] [CrossRef] [Green Version]
- De Graaff, L.F.; Honig, A.; van Pampus, M.G.; Stramrood, C.A.I. Preventing post-traumatic stress disorder following childbirth and traumatic birth experiences: A systematic review. In Acta Obstetricia et Gynecologica Scandinavica; Wiley-Blackwell: Hoboken, NJ, USA, 2018; Volume 97, pp. 648–656. [Google Scholar]
- Olde, E.; van der Hart, O.; Kleber, R.; van Son, M. Posttraumatic stress following childbirth: A review. Clin. Psychol. Rev. 2006, 26, 1–16. [Google Scholar] [CrossRef]
- Andersen, L.B.; Melvaer, L.B.; Videbech, P.; Lamont, R.F.; Joergensen, J.S. Risk factors for developing post-traumatic stress disorder following childbirth: A systematic review. Acta Obstet. Gynecol. Scand. 2012, 91, 1261–1272. [Google Scholar] [CrossRef]
- Dekel, S.; Stuebe, C.; Dishy, G. Childbirth induced posttraumatic stress syndrome: A systematic review of prevalence and risk factors. Front. Psychol. Front. Res. Found. 2017, 8, 560. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Delicate, A.; Ayers, S.; Easter, A.; McMullen, S. The impact of childbirth-related post-traumatic stress on a couple’s relationship: A systematic review and meta-synthesis. J. Reprod. Infant Psychol. 2018, 36, 102–115. [Google Scholar] [CrossRef] [PubMed]
- Carter, J.; Bick, D.; Chang, Y.S.; Gallacher, D. Mode of Birth and Development of Maternal Postnatal Post-Traumatic Stress Disorder: A Mixed Methods Systematic Review and Meta-Analysis. Available online: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=89132 (accessed on 23 August 2020).
- Sentilhes, L.; Maillard, F.; Brun, S.; Madar, H.; Merlot, B.; Goffinet, F.; Deneux-Tharaux, C. Risk factors for chronic post-traumatic stress disorder development one year after vaginal delivery: A prospective, observational study. Sci. Rep. 2017, 7, 8724. [Google Scholar] [CrossRef]
- Hernández-Martínez, A.; Rodríguez-Almagro, J.; Molina-Alarcón, M.; Infante-Torres, N.; Rubio-Álvarez, A.; Martínez-Galiano, J.M. Perinatal factors related to post-traumatic stress disorder symptoms 1–5 years following birth. Women Birth 2020, 33, e129–e135. [Google Scholar] [CrossRef]
- Ayers, S.; Harris, R.; Sawyer, A.; Parfitt, Y.; Ford, E. Posttraumatic stress disorder after childbirth: Analysis of symptom presentation and sampling. J. Affect. Disord. 2009, 119, 200–204. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Shaw, R.J.; Bernard, R.S.; de Blois, T.; Ikuta, L.M.; Ginzburg, K.; Koopman, C. The relationship between acute stress disorder and posttraumatic stress disorder in the neonatal intensive care unit. Psychosomatics 2009, 50, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Lefkowitz, D.S.; Baxt, C.; Evans, J.R. Prevalence and correlates of posttraumatic stress and postpartum depression in parents of infants in the neonatal intensive care unit (NICU). J. Clin. Psychol. Med. Settings 2010, 17, 230–237. [Google Scholar] [CrossRef]
- Treatment C for SA. Appendix E: DSM-IV-TR Criteria for Posttraumatic Stress Disorder. 2009. Available online: https://www.ncbi.nlm.nih.gov/books/NBK83241/ (accessed on 23 August 2020).
- Pai, A.; Suris, A.M.; North, C.S. Posttraumatic stress disorder in the dsm-5: Controversy, change, and conceptual considerations. Behav. Sci. 2017, 7, 7. [Google Scholar] [CrossRef]
- Ayers, S.; Wright, D.B.; Thornton, A. Development of a measure of postpartum PTSD: The city birth trauma scale. Front. Psychiatry 2018, 9, 409. [Google Scholar] [CrossRef] [Green Version]
- Posttraumatic Stress Disorder. 2013. Available online: www.psychiatry.org (accessed on 2 July 2022).
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan-a web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- CASP. Critical Appraisal Skills Programme; CASP: Oxford, UK, 2018. [Google Scholar]
- Barnett, I.; van Sluijs, E.M.F.; Ogilvie, D. Physical Activity and Transitioning to Retirement: A Systematic Review. American J. Prev. Med. 2012, 43, 329–336. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Critical Appraisal Skills Programme. CASP (Cohort Study) Checklist. 2018. Available online: https://casp-uk.net/wp-content/uploads/2018/01/CASP-Cohort-Study-Checklist_2018.pdf (accessed on 1 January 2022).
- Long, H.A.; French, D.P.; Brooks, J.M. Optimising the value of the critical appraisal skills programme (CASP) tool for quality appraisal in qualitative evidence synthesis. Res. Methods Med. Health Sci. 2020, 1, 31–42. [Google Scholar] [CrossRef]
- Critical Appraisal Skills Programme. CASP (Qualitative) Checklist. 2018. Available online: https://casp-uk.net/wp-content/uploads/2018/03/CASP-Qualitative-Checklist-2018_fillable_form.pdf (accessed on 23 August 2020).
- Burke, C.; Conway, Y. Factors that influence hospital nurses’ escalation of patient care in response to their early warning score: A qualitative evidence synthesis. J. Clin. Nurs. 2022, 1–50. [Google Scholar] [CrossRef] [PubMed]
- Morgan, R.L.; Whaley, P.; Thayer, K.A.; Schünemann, H.J. Identifying the PECO: A framework for formulating good questions to explore the association of environmental and other exposures with health outcomes. Environ. Int. 2018, 121, 1027. [Google Scholar] [CrossRef]
- Türkmen, H.; Yalniz Dilcen, H.; Akin, B. The Effect of Labor Comfort on Traumatic Childbirth Perception, Post-Traumatic Stress Disorder, and Breastfeeding. Breastfeed. Med. 2020, 15, 779–788. [Google Scholar] [CrossRef]
- Martinez-Vázquez, S.; Rodríguez-Almagro, J.; Hernández-Martínez, A.; Delgado-Rodríguez, M.; Martínez-Galiano, J.M. Obstetric factors associated with postpartum post-traumatic stress disorder after spontaneous vaginal birth. Birth 2021, 48, 406–415. [Google Scholar] [CrossRef]
- Deninotti, J.; Denis, A.; Berdoulat, É. Emergency C-section, maternal satisfaction and emotion regulation strategies: Effects on PTSD and postpartum depression symptoms. J. Reprod. Infant Psychol. 2020, 38, 1–15. [Google Scholar] [CrossRef]
- Dikmen-Yildiz, P.; Ayers, S.; Phillips, L. Factors associated with post-traumatic stress symptoms (PTSS) 4–6 weeks and 6 months after birth: A longitudinal population-based study. J. Affect. Disord. 2017, 221, 238–245. [Google Scholar] [CrossRef]
- Van Son, M.; Verkerk, G.; van der Hart, O.; Komproe, I.; Pop, V. Prenatal depression, mode of delivery and perinatal dissociation as predictors of postpartum posttraumatic stress: An empirical study. Clin. Psychol. Psychother. 2005, 12, 297–312. [Google Scholar] [CrossRef]
- Sawyer, A.; Ayers, S. Post-traumatic growth in women after childbirth. Psychol. Health 2009, 24, 457–471. [Google Scholar] [CrossRef] [Green Version]
- König, J. The German W-DEQ version B—Factor structure and prediction of posttraumatic stress symptoms six weeks and one year after childbirth. Health Care Women Int. 2019, 40, 581–596. [Google Scholar] [CrossRef]
- König, J.; Schmid, S.; Löser, E.; Neumann, O.; Buchholz, S.; Kästner, R. Interplay of demographic variables, birth experience, and initial reactions in the prediction of symptoms of posttraumatic stress one year after giving birth. Eur. J. Psychotraumatology 2016, 7, 32377. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bayri Bingol, F.; Demirgoz Bal, M. The risk factors for postpartum posttraumatic stress disorder and depression. Perspect. Psychiatr. Care 2020, 56, 851–857. [Google Scholar] [CrossRef] [PubMed]
- MacKinnon, A.L.; Yang, L.; Feeley, N.; Gold, I.; Hayton, B.; Zelkowitz, P. Birth setting, labour experience, and postpartum psychological distress. Midwifery 2017, 50, 110–116. [Google Scholar] [CrossRef]
- Bayrı Bingöl, F.; Bal, M.D.; Dişsiz, M.; Sormageç, M.T.; Yildiz, P.D. Validity and reliability of the Turkish version of the City Birth Trauma Scale (CityBiTS). J. Obstet. Gynaecol. 2021, 41, 1023–1031. [Google Scholar] [CrossRef]
- Leeds, L.; Hargreaves, I. The psychological consequences of childbirth. J. Reprod. Infant Psychol. 2008, 26, 108–122. [Google Scholar] [CrossRef] [Green Version]
- King, L.; McKenzie-McHarg, K.; Horsch, A. Testing a cognitive model to predict posttraumatic stress disorder following childbirth. BMC Pregnancy Childbirth 2017, 17, 32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nakić Radoš, S.; Matijaš, M.; Kuhar, L.; Anđelinović, M.; Ayers, S. Measuring and conceptualizing PTSD following childbirth: Validation of the City Birth Trauma Scale. Psychol. Trauma 2020, 12, 147–155. [Google Scholar] [CrossRef]
- Gankanda, W.I.; Gunathilake, I.A.G.M.P.; Kahawala, N.L.; Ranaweera, A.K.P. Prevalence and associated factors of post-traumatic stress disorder (PTSD) among a cohort of Srilankan post-partum mothers: A cross-sectional study. BMC Pregnancy Childbirth 2021, 21, 626. [Google Scholar] [CrossRef]
- Weigl, T.; Beck-Hiestermann, F.M.L.; Stenzel, N.M.; Benson, S.; Schedlowski, M.; Garthus-Niegel, S. Assessment of Childbirth-Related PTSD: Psychometric Properties of the German Version of the City Birth Trauma Scale. Front. Psychiatry 2021, 12, 731537. [Google Scholar] [CrossRef] [PubMed]
- Harrison, S.E.; Ayers, S.; Quigley, M.A.; Stein, A.; Alderdice, F. Prevalence and factors associated with postpartum posttraumatic stress in a population-based maternity survey in England. J. Affect. Disord. 2021, 279, 749–756. [Google Scholar] [CrossRef]
- Martínez-Galiano, J.M.; Martinez-Vazquez, S.; Rodríguez-Almagro, J.; Hernández-Martinez, A. The magnitude of the problem of obstetric violence and its associated factors: A cross-sectional study. Women Birth 2021, 34, e526–e536. [Google Scholar] [CrossRef]
- Hernández-Martínez, A.; Martínez-Vazquez, S.; Rodríguez-Almagro, J.; Delgado-Rodríguez, M.; Martínez-Galiano, J.M. Elaboration and Validation of Two Predictive Models of Postpartum Traumatic Stress Disorder Risk Formed by Variables Related to the Birth Process: A Retrospective Cohort Study. Int. J. Environ. Res. Public Health 2020, 18, 92. [Google Scholar] [CrossRef]
- Ben-Hassine, S.; Chabbert, M.; Rozenberg, P.; Wendland, J. Prevalence, Evolution, and Predictive Factors of Symptoms of Postpartum Posttraumatic Stress Disorder in a French-Speaking Cohort. J. Midwifery Women’s Health 2022. Available online: https://onlinelibrary.wiley.com/doi/full/10.1111/jmwh.13350 (accessed on 20 March 2022). [CrossRef]
- Dobson, H.; Malpas, C.; Kulkarni, J. Measuring posttraumatic stress disorder following childbirth. Australas. Psychiatry 2022, 103985622210779. Available online: http://journals.sagepub.com/doi/10.1177/10398562221077900 (accessed on 27 March 2022). [CrossRef]
- Martínez-Vazquez, S.; Rodríguez-Almagro, J.; Hernández-Martínez, A.; Delgado-Rodríguez, M.; Martínez-Galiano, J.M. Long-Term High Risk of Postpartum Post-Traumatic Stress Disorder (PTSD) and Associated Factors. J. Clin. Med. 2021, 10, 488. [Google Scholar] [CrossRef]
- Wang, Z.; Liu, J.; Shuai, H.; Cai, Z.; Fu, X.; Liu, Y.; Xiao, X.; Zhang, W.; Krabbendam, E.; Liu, S.; et al. Systematic Review Mapping global prevalence of depression among postpartum women. Transl. Psychiatry 2021, 11, 543. [Google Scholar] [CrossRef]
- Çalik, K.Y.; Karabulutlu, Ö.; Yavuz, C. First do no harm interventions during labor and maternal satisfaction: A descriptive cross-sectional study. BMC Pregnancy Childbirth 2018, 18, 415. [Google Scholar] [CrossRef] [Green Version]
- Patel, R.R.; Murphy, D.J. Forceps delivery in modern obstetric practice. Br. Med. J. 2004, 328, 1302–1305. [Google Scholar] [CrossRef] [Green Version]
- Simpson, M.; Schmied, V.; Dickson, C.; Dahlen, H.G. Postnatal post-traumatic stress: An integrative review. Women Birth 2018, 31, 367–379. [Google Scholar] [CrossRef]
- Milosavljevic, M.; Tosevski, D.L.; Soldatovic, I.; Vukovic, O.; Miljevic, C.; Peljto, A.; Kostic, M.; Olff, M. Posttraumatic Stress Disorder after Vaginal Delivery at Primiparous Women. Sci. Rep. 2016, 6, 27554. [Google Scholar] [CrossRef] [Green Version]
- Adewuya, A.; Ologun, Y.; Ibigbami, O. Post-traumatic stress disorder after childbirth in Nigerian women: Prevalence and risk factors. BJOG Int. J. Obstet. Gynaecol. 2006, 113, 284–288. [Google Scholar] [CrossRef]
- Guan, P.; Tang, F.; Sun, G.; Ren, W. Prediction of emergency cesarean section by measurable maternal and fetal characteristics. J. Investig. Med. 2020, 68, 799–806. [Google Scholar] [CrossRef]
- Keogh, E.; Ayers, S.; Francis, H. Does anxiety sensitivity predict post-traumatic stress symptoms following childbirth? A preliminary report. Cogn. Behav. Ther. 2002, 31, 145–155. [Google Scholar] [CrossRef]
- Beck, C.T.; Watson, S. Impact of birth trauma on breast-feeding: A tale of two pathways. Nurs. Res. 2008, 57, 228–236. [Google Scholar] [CrossRef]
- Eriksson, C.; Westman, G.; Hamberg, K. Experiential factors associated with childbirth-related fear in Swedish women and men: A population based study. J. Psychosom. Obstet. Gynecol. 2005, 26, 63–72. [Google Scholar] [CrossRef]
- Santas, G.; Santas, F. Trends of caesarean section rates in Turkey. J. Obstet. Gynaecol. 2018, 38, 658–662. [Google Scholar] [CrossRef]
- Elmir, R.; Schmied, V.; Wilkes, L.; Jackson, D. Women’s perceptions and experiences of a traumatic birth: A meta-ethnography. J. Adv. Nurs. 2010, 66, 2142–2153. [Google Scholar] [CrossRef]
- Kjerulff, K.H.; Attanasio, L.B.; Sznajder, K.K.; Brubaker, L.H. A prospective cohort study of post-traumatic stress disorder and maternal-infant bonding after first childbirth. J. Psychosom. Res. 2021, 144, 110424. [Google Scholar] [CrossRef]
- Mei, J.Y.; Afshar, Y.; Gregory, K.D.; Kilpatrick, S.J.; Esakoff, T.F. Birth Plans: What Matters for Birth Experience Satisfaction. Birth 2016, 43, 144–150. [Google Scholar] [CrossRef] [PubMed]
- Dikmen Yildiz, P.; Ayers, S.; Phillips, L. The Prevalence of Posttraumatic Stress Disorder in Pregnancy and after Birth: A Systematic Review and Meta-Analysis. 2016. Available online: www.elsevier.com/locate/jad (accessed on 6 July 2022).
- Alcorn, K.L.; O’Donovan, A.; Patrick, J.C.; Creedy, D.; Devilly, G.J. A prospective longitudinal study of the prevalence of post-traumatic stress disorder resulting from childbirth events. Psychol. Med. 2010, 40, 1849–1859. [Google Scholar] [CrossRef] [Green Version]
- Ayers, S.; Pickering, A.D. Do women get posttraumatic stress disorder as a result of childbirth? A prospective study of incidence. Birth 2001, 28, 111–118. [Google Scholar] [CrossRef] [Green Version]
- Violence against Women. Available online: https://www.who.int/news-room/fact-sheets/detail/violence-against-women (accessed on 3 March 2022).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).