How Do Pharmacists Practice in Aged Care? A Narrative Review of Models from Australia, England, and the United States of America
Abstract
:1. Introduction
2. Materials and Methods
- The Australian pharmacist practice model in residential aged care, incorporating Residential Medication Management Review (RMMRs) and quality use of medicines (QUM) services (Australia);
- The Medicine Optimisation in Care Homes (MOCH) program (England);
- The Centers for Medicare and Medicaid (CMS) pharmacy services in long-term care (USA);
- Medication Therapy Management (MTM) (USA).
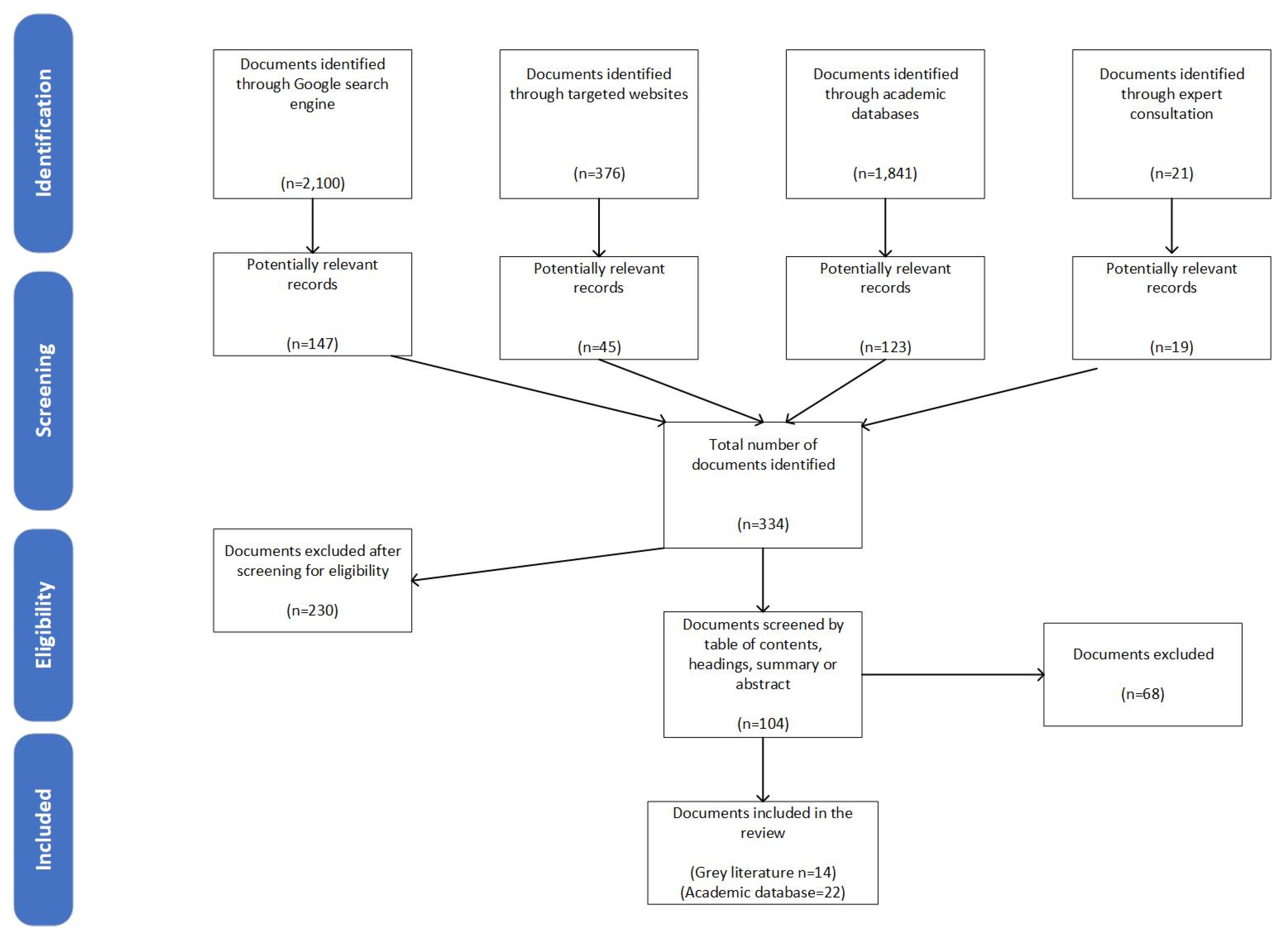
2.1. Search Strategy: Peer-Reviewed and Grey Literature
2.2. Inclusion Criteria
2.3. Data Collection Process and Synthesis of Results
3. Results
3.1. Characteristics and Activities of Models of Practice
3.2. Australian Pharmacist Model in Residential Aged Care—Residential Medication Management Review (RMMR) and Quality Use of Medicine (QUM) Programs
3.3. The Medicine Optimisation in Care Homes (MOCH) Program (England)
3.4. Centers for Medicare and Medicaid (CMS) Pharmacy Services in Long-Term Care (USA)
3.5. Medication Therapy Management in Long-Term Care (USA)
4. Discussion
4.1. Medication Review Activities
4.2. Facility-Level Activities
4.3. Current Evidence for the Practice Models
4.4. Level of Collaboration
4.5. Future Directions
4.6. Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| RACF | Residential aged care facility |
| LTC | long-term care facility |
| PIM | Potentially inappropriate medication |
| RMMR | Residential medication management review |
| GP | General practitioner |
| QUM | Quality use of medicines |
| NHS | National health services |
| MOCH | Medicine optimisation in care homes model |
| CMS | Centers for Medicare and Medicaid pharmacy services |
| MTM | Medication therapy management |
| TMR | Targeted medication review |
| CMR | Comprehensive medication review |
Appendix A
| Number | Government Organisation | URL Link |
|---|---|---|
| 1 | The National Health Service (NHS) England | https://www.england.nhs.uk/ (accessed on 8 February 2021) |
| 2 | Royal Pharmaceutical Society of Great Britain | https://www.rpharms.com/ (accessed on 15 October 2020) |
| 3 | Centers for Medicare & Medicaid Services | https://www.cms.gov/ (accessed on 23 February 2021) |
| 4 | American Pharmacists Association | https://www.pharmacist.com/ (accessed on 17 March 2021) |
| 5 | American Society of Consultant Pharmacists (ASCP) | https://www.ascp.com/ accessed on 23 February 2021) |
| 6 | Pharmaceutical Society of Australia (PSA) | https://www.psa.org.au/ (accessed on 20 February 2021) |
| 7 | Australian Government Department of Health | https://www.health.gov.au/ (accessed on 17 March 2021) |
| 8 | Pharmacy Programs Administrator (PPA) | https://www.ppaonline.com.au/ (accessed on 25 February 2021) |
Appendix B
| Search # | Concept | Other Terms |
|---|---|---|
| #1 | Pharmacist | pharmacist, pharmacists, pharmaceutical service, pharmaceutical services, pharmacy”, “pharmacists |
| #2 | Keywords of selected models | Centers for Medicare and Medicaid pharmacy services, drug regimen reviews, DRRs, Australian model, Residential Medication Management Review, RMMRs, QUMs, MACs, medication therapy management, MTM, medicines optimisation in care homes, vanguards, NHS, MOCH |
| #3 | Residential aged care settings | aged care, aged patient care, aged patient services, assisted living, care home, elder care, elder patient care, long term care, long-term care, nursing home, older person care, older patient care, patient aged care, residential care, residential aged care, skilled nursing facility |
| #4 | Selected countries | England, English, USA, The United States, United States of America, American, Australia, Australian. |
References
- Gheewala, P.A.; Peterson, G.M.; Curtain, C.M.; Nishtala, P.S.; Hannan, P.J.; Castelino, R.L. Impact of the pharmacist medication review services on drug-related problems and potentially inappropriate prescribing of renally cleared medications in residents of aged care facilities. Drugs Aging 2014, 31, 825–835. [Google Scholar] [CrossRef]
- Nishtala, P.S.; McLachlan, A.J.; Bell, J.S.; Chen, T.F. A retrospective study of drug-related problems in Australian aged care homes: Medication reviews involving pharmacists and general practitioners. J. Eval. Clin. Pract. 2011, 17, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.W.H.; Mak, V.S.L.; Tang, Y.W. Pharmacist services in nursing homes: A systematic review and meta-analysis. Br. J. Clin. Pharmacol. 2019, 85, 2668–2688. [Google Scholar] [CrossRef]
- Chen, E.Y.H.; Wang, K.N.; Sluggett, J.K.; Ilomäki, J.; Hilmer, S.N.; Corlis, M.; Bell, J.S. Process, impact and outcomes of medication review in Australian residential aged care facilities: A systematic review. Australas. J. Ageing 2019, 38, 9–25. [Google Scholar] [CrossRef] [PubMed]
- Wright, D.J.; Maskrey, V.; Blyth, A.; Norris, N.; Alldred, D.P.; Bond, C.M.; Desborough, J.; Hughes, C.M.; Holland, R.C. Systematic review and narrative synthesis of pharmacist provided medicines optimisation services in care homes for older people to inform the development of a generic training or accreditation process. Int. J. Pharm. Pract. 2020, 28, 207–219. [Google Scholar] [CrossRef] [Green Version]
- Fredrickson, B.-A.; Burkett, E. Interventions to improve the continuity of medication management upon discharge of patients from hospital to residential aged care facilities. J. Pharm. Pract. Res. 2019, 49, 162–170. [Google Scholar] [CrossRef] [Green Version]
- Gudi, S.K.; Kashyap, A.; Chhabra, M.; Rashid, M.; Tiwari, K.K. Impact of pharmacist-led home medicines review services on drug-related problems among the elderly population: A systematic review. Epidemiol. Health 2019, 41, e2019020. [Google Scholar] [CrossRef]
- CMS. CY 2020 Medication Therapy Management Program Guidance and Submission Instructions. Available online: https://www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovContra/Downloads/Memo-Contract-Year-2020-Medication-Therapy-Management-MTM-Program-Submission-v-041019-.pdf (accessed on 1 September 2020).
- CMS. State Operations Manual Appendix PP—Guidance to Surveyors for Long Term Care Facilities. Available online: https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/GuidanceforLawsAndRegulations/Downloads/Appendix-PP-State-Operations-Manual.pdf (accessed on 1 August 2020).
- NHS. England—Medicines Optimisation in Care Homes (MOCH). Available online: https://www.england.nhs.uk/wp-content/uploads/2018/03/medicines-optimisation-in-care-homes-programme-overview.pdf (accessed on 1 January 2021).
- Cooper, H.M. Organizing knowledge syntheses: A taxonomy of literature reviews. Knowl. Soc. 1988, 1, 104–126. [Google Scholar] [CrossRef]
- Baumeister, R.F.; Leary, M.R. Writing narrative literature reviews. Rev. Gen. Psychol. 1997, 1, 311–320. [Google Scholar] [CrossRef]
- Godin, K.; Stapleton, J.; Kirkpatrick, S.I.; Hanning, R.M.; Leatherdale, S.T. Applying systematic review search methods to the grey literature: A case study examining guidelines for school-based breakfast programs in Canada. Syst. Rev. 2015, 4, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1–9. [Google Scholar] [CrossRef] [Green Version]
- CPPE. Medicines Optimisation in Care Homes Training Pathway for Pharmacy Professionals. Available online: https://www.cppe.ac.uk/career/moch/training-pathway (accessed on 15 November 2020).
- PSA. Guidelines for Quality Use of Medicines (QUM) Services. Available online: https://www.ppaonline.com.au/wp-content/uploads/2020/04/PSA-Guidelines-for-Quality-Use-of-Medicines-QUM-services.pdf (accessed on 15 October 2020).
- PSA. Guidelines for Pharmacists Providing Residential Medication Management Review (RMMR) and Quality Use of Medicines (QUM) Services. Available online: https://www.ppaonline.com.au/wp-content/uploads/2019/01/PSA-RMMR-and-QUM-Guidelines.pdf (accessed on 21 December 2020).
- Residential Medication Management Review. Available online: https://www.ppaonline.com.au/wp-content/uploads/2020/04/RMMR-Program-Rules-COVID-19.pdf (accessed on 21 December 2020).
- PSA. Guidelines for Comprehensive Medication Management Reviews. Available online: https://www.ppaonline.com.au/wp-content/uploads/2020/04/PSA-Guidelines-for-Comprehensive-Medication-Management-Reviews.pdf (accessed on 17 October 2020).
- CMS. Lsit of Revised F-Tags—Updated. Available online: https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/GuidanceforLawsAndRegulations/Downloads/List-of-Revised-FTags.pdf (accessed on 21 November 2020).
- Quality Use of Medicines 2020. Available online: https://www.ppaonline.com.au/wp-content/uploads/2020/04/QUM-Program-Rules-COVID-19.pdf (accessed on 19 October 2020).
- Kaur, S.; Roberts, J.A.; Roberts, M.S. Evaluation of medication-related problems in medication reviews: A comparative perspective. Ann. Pharmacother. 2012, 46, 972–982. [Google Scholar] [CrossRef]
- Nishtala, P.S.; McLachlan, A.J.; Bell, J.S.; Chen, T.F. Psychotropic Prescribing in Long-Term Care Facilities: Impact of Medication Reviews and Educational Interventions. Am. J. Geriatr. Psychiatry 2008, 16, 621–632. [Google Scholar] [CrossRef]
- McLarin, P.E.; Peterson, G.M.; Curtain, C.M.; Nishtala, P.S.; Hannan, P.J.; Castelino, R.L. Impact of residential medication management reviews on anticholinergic burden in aged care residents. Curr. Med. Res. Opin. 2016, 32, 123–131. [Google Scholar] [CrossRef] [PubMed]
- Pouranayatihosseinabad, M.; Zaidi, T.S.; Peterson, G.; Nishtala, P.S.; Hannan, P.; Castelino, R. The impact of residential medication management reviews (RMMRs) on medication regimen complexity. Postgrad. Med. 2018, 130, 575–579. [Google Scholar] [CrossRef]
- Nishtala, P.S.; Castelino, R.L.; Peterson, G.M.; Hannan, P.J.; Salahudeen, M.S. Residential medication management reviews of antithrombotic therapy in aged care residents with atrial fibrillation: Assessment of stroke and bleeding risk. J. Clin. Pharm. Ther. 2016, 41, 279–284. [Google Scholar] [CrossRef]
- Christensen, L.; Turner, J.R.; Peterson, G.M.; Naunton, M.; Thomas, J.; Yee, K.C.; Kosari, S. Identification of Risk of QT Prolongation by Pharmacists When Conducting Medication Reviews in Residential Aged Care Settings: A Missed Opportunity? J. Clin. Med. 2019, 8, 1866. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sluggett, J.K.; Bell, J.S.; Lang, C.; Corlis, M.; Whitehead, C.; Wesselingh, S.L.; Inacio, M.C. Variation in Provision of Collaborative Medication Reviews on Entry to Long-Term Care Facilities. J. Am. Med. Dir. Assoc. 2021, 22, 148–155. [Google Scholar] [CrossRef] [PubMed]
- Five Year Forward View. Available online: https://www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf (accessed on 21 November 2020).
- New Care Models: Vanguards—Developing a Blueprint for the Future of NHS and Care Services. Available online: https://www.england.nhs.uk/wp-content/uploads/2015/11/new_care_models.pdf (accessed on 3 November 2020).
- Baqir, W.; Barrett, S.; Desai, N.; Copeland, R.; Hughes, J. A clinico-ethical framework for multidisciplinary review of medication in nursing homes. BMJ Qual. Improv. Rep. 2014, 3, u203261.w2538. [Google Scholar] [CrossRef] [Green Version]
- The Health foundation. Briefing: The Impact of Providing Enhanced Support for Care Home Residents in Wakefield. Available online: https://www.health.org.uk/publications/reports/impact-of-enhanced-support-for-Wakefield-care-home-residents (accessed on 3 November 2021).
- The Health foundation. Briefing: The Impact of Providing an Enhanced Package of Care for Care Home Residents in Nottingham City. Available online: https://www.health.org.uk/publications/reports/impact-of-enhanced-support-for-nottingham-care-home-residents (accessed on 5 November 2021).
- The Health Foundation. Briefing: The Impact of Providing Enhanced Support for Sutton Homes of Care Residents. Available online: https://www.health.org.uk/publications/the-impact-of-providing-enhanced-support-for-sutton-homes-of-care-residents (accessed on 3 November 2021).
- Brown, C.H. The Consultant Pharmacist’s Role in Long-Term Care Facilities. J. Pharm. Pract. 1988, 1, 166–172. [Google Scholar] [CrossRef]
- Wesson, K.W.; Donohoe, K.L.; Patterson, J.A. CMS Mega-Rule Update and the Status of Pharmacy-Related Deficiencies in Nursing Homes. J. Appl. Gerontol. 2020, 40, 1617–1627. [Google Scholar] [CrossRef] [PubMed]
- Simonson, W. Significant changes in CMS pharmacy services F-Tags for long-term care facilities. Geriatr. Nurs. 2018, 39, 112–114. [Google Scholar] [CrossRef] [PubMed]
- Hughes, C.M.; Lapane, K.L.; Mor, V.; Ikegami, N.; Jónsson, P.V.; Ljunggren, G.; Sgadari, A. The impact of legislation on psychotropic drug use in nursing homes: A cross-national perspective. J. Am. Geriatr. Soc. 2000, 48, 931–937. [Google Scholar] [CrossRef]
- Hughes, C.M.; Lapane, K.L. Administrative initiatives for reducing inappropriate prescribing of psychotropic drugs in nursing homes: How successful have they been? Drugs Aging 2005, 22, 339–351. [Google Scholar] [CrossRef]
- Lapane, K.L.; Hughes, C.M.; Christian, J.B.; Daiello, L.A.; Cameron, K.A.; Feinberg, J. Evaluation of the fleetwood model of long-term care pharmacy. J. Am. Med. Dir. Assoc. 2011, 12, 355–363. [Google Scholar] [CrossRef]
- Horning, K.K.; Hoehns, J.D.; Doucette, W.R. Adherence to clinical practice guidelines for 7 chronic conditions in long-term-care patients who received pharmacist disease management services versus traditional drug regimen review. J. Manag. Care Pharm. 2007, 13, 28–36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- CMS. Medicare Part D Medication Therapy Management (MTM) Programs—Fact Sheet. Available online: https://www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovContra/Downloads/CY2019-MTM-Fact-Sheet.pdf (accessed on 3 November 2020).
- Viswanathan, M.; Kahwati, L.C.; Golin, C.E.; Blalock, S.J.; Coker-Schwimmer, E.; Posey, R.; Lohr, K.N. Medication therapy management interventions in outpatient settings: A systematic review and meta-analysis. JAMA Intern. Med. 2015, 175, 76–87. [Google Scholar] [CrossRef] [PubMed]
- Caffiero, N.; Delate, T.; Ehizuelen, M.D.; Vogel, K. Effectiveness of a Clinical Pharmacist Medication Therapy Management Program in Discontinuation of Drugs to Avoid in the Elderly. J. Manag. Care Spec. Pharm. 2017, 23, 525–531. [Google Scholar] [CrossRef]
- Ramalho de Oliveira, D.; Brummel, A.R.; Miller, D.B. Medication therapy management: 10 years of experience in a large integrated health care system. J. Manag. Care Pharm. 2010, 16, 185–195. [Google Scholar] [CrossRef] [Green Version]
- Johnson, C.F.; Williams, B.; MacGillivray, S.A.; Dougall, N.J.; Maxwell, M. ‘Doing the right thing’: Factors influencing GP prescribing of antidepressants and prescribed doses. BMC Fam. Pract. 2017, 18, 72. [Google Scholar] [CrossRef] [Green Version]
- Hughes, G.A.; Rowett, D.; Corlis, M.; Sluggett, J.K. Reducing harm from potentially inappropriate medicines use in long-term care facilities: We must take a proactive approach. Res. Soc. Adm. Pharm. 2021, 17, 829–831. [Google Scholar] [CrossRef] [PubMed]
- Sluggett, J.K.; Ilomäki, J.; Seaman, K.L.; Corlis, M.; Bell, J.S. Medication management policy, practice and research in Australian residential aged care: Current and future directions. Pharmacol. Res. 2017, 116, 20–28. [Google Scholar] [CrossRef]
- Jokanovic, N.; Wang, K.N.; Dooley, M.J.; Lalic, S.; Tan, E.C.K.; Kirkpatrick, C.M.; Bell, J.S. Prioritizing interventions to manage polypharmacy in Australian aged care facilities. Res. Soc. Adm. Pharm. 2017, 13, 564–574. [Google Scholar] [CrossRef] [PubMed]
- Koria, L.G.; Zaidi, T.S.; Peterson, G.; Nishtala, P.; Hannah, P.J.; Castelino, R. Impact of medication reviews on inappropriate prescribing in aged care. Curr. Med. Res. Opin. 2018, 34, 833–838. [Google Scholar] [CrossRef]
- Nguyen, T.A.; Gilmartin-Thomas, J.; Tan, E.C.K.; Kalisch-Ellett, L.; Eshetie, T.; Gillam, M.; Reeve, E.J. The impact of pharmacist interventions on quality use of medicines, quality of life, and health outcomes in people with dementia and/or cognitive impairment: A systematic review. J. Alzheimer’s Dis. 2019, 71, 83–96. [Google Scholar] [CrossRef]
- McDerby, N.; Naunton, M.; Shield, A.; Bail, K.; Kosari, S. Feasibility of Integrating Residential Care Pharmacists into Aged Care Homes to Improve Quality Use of Medicines: Study Protocol for a Non-Randomised Controlled Pilot Trial. Int. J. Environ. Res. Public Health 2018, 15, 499. [Google Scholar] [CrossRef] [Green Version]
- McDerby, N.; Bail, K.; Kosari, S.; Shield, A.; Peterson, G.; Dawda, P.; Naunton, M. Canaries in the coalmine: Stakeholder perspectives of medication management reviews for residents with dementia. Res. Soc. Adm. Pharm. 2020, 16, 1220–1227. [Google Scholar] [CrossRef]
- Baqir, W.; Hughes, J.; Jones, T.; Barrett, S.; Desai, N.; Copeland, R.; Campbell, D.; Laverty, A. Impact of medication review, within a shared decision-making framework, on deprescribing in people living in care homes. Eur. J. Hosp. Pharm. 2017, 24, 30–33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bond, C.M.; Holland, R.; Alldred, D.P.; Arthur, A.; Barton, G.; Blyth, A.; Desborough, J.; Ford, J.; Handford, C.; Hill, H.; et al. Protocol for a cluster randomised controlled trial to determine the effectiveness and cost-effectiveness of independent pharmacist prescribing in care homes: The CHIPPS study. Trials 2020, 21, 103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kosari, S.; Koerner, J.; Naunton, M.; Peterson, G.M.; Haider, I.; Lancsar, E.; Wright, D.; Niyonsenga, T.; Davey, R. Integrating pharmacists into aged care facilities to improve the quality use of medicine (PiRACF Study): Protocol for a cluster randomised controlled trial. Trials 2021, 22, 390. [Google Scholar] [CrossRef] [PubMed]
- Tsingos, C.; Bosnic-Anticevich, S.; Smith, L. Reflective Practice and Its Implications for Pharmacy Education. Am. J. Pharm. Educ. 2014, 78, 18. [Google Scholar] [CrossRef]
| Focus | Research outcomes | Research articles and documents on pharmacist practice models offering clinical services in aged care facilities within selected countries. |
| Goal | Identification of central issues, integration/generalisation | (i) Identify and describe international pharmacist models of practice in aged care in selected countries (England, Australia and the USA), (ii) synthesise documents to characterise each practice model based on resident-level and facility-level activities, employment type and pharmacist qualifications, and (iii) provide an overview of the available evidence for benefits. |
| Perspective | Neutral representation | Research findings are presented in an unbiased manner, as in the original documents. |
| Coverage | Representative | Pharmacist practice models will be selected based on selection criteria, and studies and documents are selected to represent the specified models and their evidence. The coverage will not be exhaustive of all relevant models and studies. |
| Organisation | Conceptual | Articles and documents relating to each country’s practice model(s) are represented together. |
| Audience | Health researchers, practitioners, policy makers | Informing stakeholders such as policy makers and researchers on developing international models of pharmacist practice in aged care, the current activities within those models, and their evidence for benefits. |
| MOCH—England [10,15] | RMMR and QUM Services—Australia [16,17,18,19] | CMS in Long-Term Facilities—USA [9,20] | MTM—USA [8] | |
|---|---|---|---|---|
| Stated aims of the model/service | To train and deploy clinical pharmacists and pharmacy technicians into care home settings to improve quality of care through better medicines use, savings and waste reduction. | To improve the patient’s quality of life and health outcomes using a best practice approach, detect and address medicine-related problems, and provide education to residents, carers and other healthcare providers. | To obtain services of a licensed pharmacist by facilities to ensure the safe and effective use of medications and other pharmaceutical services. | To improve medication use, reduce the risk of adverse events, and improve medication adherence. |
| Main funding arrangement | Funded fully by NHS England’s Pharmacy Integration Fund in year 1, and subsequently 50% of costs is covered by local commissioning group (Clinical Commissioning Groups, in England). | Funded by the Australian Government Department of Health & Ageing under the 7th Community Pharmacy Agreement. | Facilities funded by the Centers for Medicare and Medicaid (CMS) must meet their requirements, which include obtaining the services from consultant pharmacists to oversee pharmacy services for the long-term care (LTC) facility. | Medicare Part D plan sponsors are funded federally by the Centers for Medicare and Medicaid Services through the Medicare Part D program. |
| Type of Employment | Pharmacy professionals are employed by a range of employers (including NHS hospitals, GP practices, community hospitals, community pharmacy, commissioning organisations)—all employers were commissioned by clinical commission groups (CCG) to work on a part-time basis depending on model. | Consultant pharmacists work as independent contractors and are compensated per service from the Community Pharmacy Agreement funds. | Consultant pharmacists can be self-employed, employed by the facility, or employed by a pharmacy provider. | Medicare Part D plan sponsors * set contracts and the fee structure to remunerate pharmacists to provide MTM services. |
| Type of qualification/accreditation required | Licensed pharmacist. Pharmacists participate in an 18-month training pathway, including the UK’s independent pharmacist prescribing pathway. | Licensed pharmacist and additional accreditation with an approved professional body such as the Association of Consultant Pharmacists (AACP) or the Society of Hospital Pharmacists of Australia (SHPA). The accreditation is renewed every 3 years by examination. | Licensed Pharmacist in state/jurisdiction. | Licensed pharmacist in state/jurisdiction. |
| MOCH—England [10,15] | RMMR and QUM Services—Australia [16,17,18,19] | CMS in Long-Term Facilities—USA [9,20] | MTM—USA [8] | |
|---|---|---|---|---|
| Description of Activity | The model incorporates direct patient-facing activities within a shared decision-making framework depending on local needs (e.g., structured medication reviews, end of life support, frailty reviews). | Involves a systematic review of resident’s medication regimen. | Drug Regimen Review (DRR) is a review of the medical chart of each resident to report and act on irregularities and must ensure residents are free from unnecessary medications. | Involves a comprehensive review of medications. |
| Eligibility criteria to receive activity | Activity must contain a risk stratification strategy to prioritise residents in need of medication review. | Residents must meet eligibility criteria (e.g., the patient is at risk of, or currently experiencing, medication misadventure). | All residents must be reviewed. | Eligible Medicare Part D * recipients who meet the eligibility requirements can be targeted by Part D plan sponsors, such as those residents with multiple chronic conditions, multiple Part D covered medications, especially those incurring high annual medication costs. |
| Frequency of service | As required, no restriction. | Permanent residents in accredited RACFs are eligible to receive an RMMR every 24 months or if deemed clinically necessary by the prescriber, with 2 follow-ups if required | A monthly review by consultant pharmacist | Involves an annual comprehensive medication review (CMRs) and targeted medication reviews (TMRs) at least quarterly with follow-up interventions when necessary. |
| Communication | Pharmacists must be able to access care home resident/GP records and appropriate data with adequate information technology support. Pharmacists must engage directly with GP Practices responsible for the primary health care of patients. | Where appropriate, the accredited pharmacist and the referring medical practitioner should discuss the findings, recommendations and suggested medicines management strategies, either by phone or face to face. | The pharmacist must document any identified irregularities in a separate written report. The report may be in paper or electronic form. The pharmacist’s findings are considered part of each resident’s medical record. The pharmacist is also responsible for reporting any identified irregularities to the attending physician, the facility’s medical director, and director of nursing. | Plan sponsors are encouraged to adopt standardised health information technology (HIT) for documentation of MTM services. The MTM provider should coordinate the recommendations for drug therapy changes as a result of an MTM encounter with the beneficiary’s treating physician and healthcare team at the facility. |
| Other attributes | Support arrangements for those with cognitive disabilities and palliative care. A focus on resident and family’s involvement in the decisions-making | An RMMR is initiated by GP referral, pharmacist sends recommendations to resident’s GP, then a medication management plan is developed. | A focus on reviewing psychotropic medications (i.e., PRN orders for psychotropics are limited to 14 days). Facility must ensure medication error rate is less than 5 percent. | Resident’s CMR may be conducted person-to-person, or via a telehealth consultation. Involves a summary with a personalised medication action plan and medication list for the residents. Promote coordinated care, intervention recommendations must target both residents and prescribers. |
| MOCH—England [10,15] | RMMR and QUM Services—Australia [16,17,18,19] | CMS in Long-Term Facilities—USA [9,20] | MTM—USA [8] |
|---|---|---|---|
| - Support antimicrobial stewardship; - Commitment to supporting frailty through working with a multidisciplinary team; - Integration as part of the multidisciplinary health care team; - Engage and collaborate with GP practices and community pharmacists; - Support care homes and their staff with medicines management tasks (e.g., ordering and safe storage of medicines); - Support nursing staff with medicines administration. | QUM services can include any of the following activities: - Medication advisory activities; - Education activities; - Continuous quality improvement activities. | A licenced pharmacist must be consulted on provision of pharmacy services in the facility, including: - Establishing a system of records of receipt and disposition of all controlled drugs; - Ensure adequate labelling and storage of drugs and biologicals in accordance with State and Federal laws. | Provides resident specific services only and does not provide any facility-level activities. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Haider, I.; Naunton, M.; Davey, R.; Peterson, G.M.; Baqir, W.; Kosari, S. How Do Pharmacists Practice in Aged Care? A Narrative Review of Models from Australia, England, and the United States of America. Int. J. Environ. Res. Public Health 2021, 18, 12773. https://doi.org/10.3390/ijerph182312773
Haider I, Naunton M, Davey R, Peterson GM, Baqir W, Kosari S. How Do Pharmacists Practice in Aged Care? A Narrative Review of Models from Australia, England, and the United States of America. International Journal of Environmental Research and Public Health. 2021; 18(23):12773. https://doi.org/10.3390/ijerph182312773
Chicago/Turabian StyleHaider, Ibrahim, Mark Naunton, Rachel Davey, Gregory M. Peterson, Wasim Baqir, and Sam Kosari. 2021. "How Do Pharmacists Practice in Aged Care? A Narrative Review of Models from Australia, England, and the United States of America" International Journal of Environmental Research and Public Health 18, no. 23: 12773. https://doi.org/10.3390/ijerph182312773
APA StyleHaider, I., Naunton, M., Davey, R., Peterson, G. M., Baqir, W., & Kosari, S. (2021). How Do Pharmacists Practice in Aged Care? A Narrative Review of Models from Australia, England, and the United States of America. International Journal of Environmental Research and Public Health, 18(23), 12773. https://doi.org/10.3390/ijerph182312773









