Abstract
A record outbreak of community-spread COVID-19 started on 10 May 2021, in Taiwan. In response to the COVID-19 pandemic, care facilities have adopted various protocols using instant communication technology (ICT) to provide remote yet timely healthcare while ensuring staff safety. The challenges of patient evaluation in the emergency department (ED) using ICT are seldom discussed in the literature. The objective of this study was to investigate the factors influencing the utility of ICT for patient assessment in emergency settings during the pandemic. The patient flow protocol and the ED layout were modified and regionalized into different areas according to the patient’s risk of COVID-19 infection. Nine iPads were stationed in different zones to aid in virtual patient assessment and communication between medical personnel. A focus group study was performed to assess and analyze the utility of the ICT module in the ED. Eight emergency physicians participated in the study. Of them, four (50%) had been directly involved in the development of the ICT module in the study hospital. Three main themes that influenced the application of the ICT module were identified: setting, hardware, and software. The setting theme included six factors: patient evaluation, subspecialty consultation, patient privacy and comfortableness, sanitation, cost, and patient acceptability. The hardware theme included six factors: internet connection, power, quality of image and voice, public or personal mode, portable or fixed mode, and maintenance. The software theme included six factors: platform choices, security, ICT accounts, interview modes, video/voice recording, and time limitation. Future studies should focus on quantifying module feasibility, user satisfaction, and protocol adjustment for different settings.
1. Introduction
Instant communication technology (ICT) has been applied to improve healthcare in various innovative modalities [1]. The model of patient care, especially in the emergency department (ED), is changing dramatically in response to the ongoing COVID-19 pandemic [2,3,4]. Achieving adequate patient evaluation while minimizing direct contact with patients to reduce the risk of infection is an important concern.
Several models of delivering healthcare through computer devices have been designed for different settings [5,6,7,8]. The Infectious Diseases Society of America has previously used telemedicine to provide subspecialty care, manage patients with chronic disease, and prevent and control infection transmission [9]. The use of telehealth communication in intensive care unit settings, specifically between physicians and families, is an effective means of communication to avoid direct in-person contact [10]. Telemedicine has been effectively used to reduce physician exposure risks and conserve personal protection equipment (PPE) [3,11]. During the COVID-19 pandemic, telemedicine has been applied in different subspecialties, including neurology [12], orthopedics [13], neurosurgery [14], dermatology [15], and even in ophthalmology [4], for remote consultations and assessment. Family meetings and conversations between patients and families can be carried out by using telecommunication [16].
Different devices can be used for instant telecommunication, including two-way radio transceivers, phones, smartphones, computers, and tablets. Two-way radio transceivers have the advantage of being relatively inexpensive, simple to operate while wearing PPE, and easy to decontaminate after use [17]. However, two-way radio transceivers do not have a secure channel, and there is often miscommunication between personnel sharing the same channel. Radio frequencies are often blocked by lead-lined walls [17]. Both audio and video communications are available on telephone devices, and video consultations are preferred by physicians managing acute conditions [18,19]. When consulting by video, however, technical problems are frequently noted, and the information gained from communication is often inferior to that gained from face-to-face interaction. Therefore, video consultation is more suitable for less complicated clinical problems that do not require physical examination [20].
Of the devices available for video communications, handheld video devices are useful for emergency imaging teleconsultation [21]. Evaluation, diagnosis, and clinical advice can be provided in a distant yet timely fashion by using smartphones [22]. Mobile devices with larger screens are preferred by physicians [23]. In comparison with desktop computers, tablets can minimize the time a physician spends at a computer workstation and can aid in computing at the bedside [24]. The use of tablets for video consultation can improve clinical performance, analysis of clinical information, and communication between physicians and patients [25,26].
Taiwan has seen a record outbreak of community-spread COVID-19 in 2021. The EDs throughout Taiwan were confronted with a surge of patients with risk of infection in May 2021. Prior to this community outbreak, suspected COVID-19 cases managed in the ED were very few in numbers. The ED managed patients with a high risk of COVID-19 infection in negative-pressure isolation rooms, donning and doffing PPE during each encounter. This patient care model was immediately challenged by the increase in suspected cases of COVID-19 infections during the beginning of the outbreak. In response to the pandemic, the model of patient care has changed dramatically, and applications of ICT have been used in several medical environments. During this pandemic, ED workers have faced several challenges. Strategies to reduce exposure risks and to decrease disease transmissions must be made. Patients must be diverted into different areas according to their clinical status and risk of infection to reduce risks of disease transmission. Evaluating and reallocating patients while ensuring staff safety prompted the use of telemedicine in the ED environment.
To overcome the obstacles in patient evaluation in the ED during the COVID-19 pandemic, the ED has utilized an ICT module based on tablets. Application of ICT modules in the ED may be costly and time consuming. There are several aspects to be handled and the infrastructure of the module involves several departments, including information technology teams and medical teams of physicians and nurses. Hospitals and healthcare facilities play a critical role in response to epidemics and must react immediately to the disaster. To act promptly to a communicable disease epidemic, an ICT module can be added to a strategic preparedness and response plan. However, the challenges of patient evaluation in the ED using ICT are seldom discussed in the literature [3,6,27,28]. Introducing a novel module in the ED, especially during a pandemic, can be an arduous experience. For those interested in utilizing ICT modules, avoidance of “reinventing the wheel” is recommended. Identification of the challenges may facilitate the process of ICT setup, reduce the cost of implementation, and improve the satisfaction of stakeholders. Therefore, we conducted this study to explore the factors influencing the development and use of ICT to assess patients in the ED.
2. Materials and Methods
2.1. Study Setting
This study was conducted in the ED of a tertiary teaching hospital in Tainan City. Tainan has a population of 1.87 million in an area of 2192 square kilometers in southern Taiwan. The average number of daily ED visits was approximately 200 patients, of which approximately 20% were triaged as critical. The ED was staffed with 54 emergency physicians and 157 registered nurses.
An outbreak of community-spread COVID-19 started on 10 May 2021, in Taiwan. One-third of patients presented to the ED with symptoms such as fever, rhinorrhea, cough, ageusia, or anosmia, which poses a certain risk of COVID-19 infection. The rapid screening test to detect COVID-19 infection was not widely available at the time. We adjusted our workflow and operation system in response to the surge in suspected COVID-19 cases. Triage, redistribution, reallocation, and evaluation of patients while ensuring the safety of the staff were of utmost importance. Strategies to minimize exposure risks included redesigning the ED into different zones, patient diversion, and the use of ICT.
2.2. Regionalization within the ED
To segregate non-COVID-19 cases from suspected cases, all patients who visited the ED were diverted to separate areas according to their risks of potential COVID-19. We therefore regionalized our ED as high-risk, moderate-risk, and low-risk areas. Figure 1 shows the modified floor plan of the ED during the pandemic.
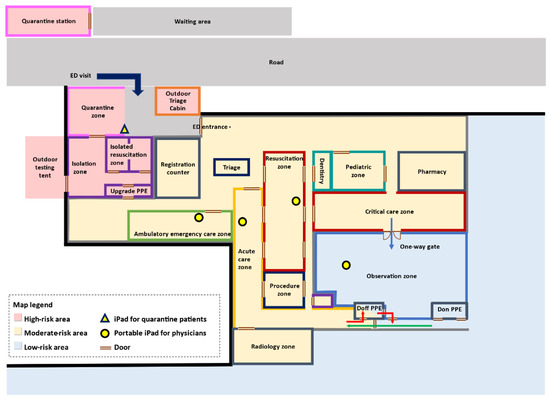
Figure 1.
Modified floor plan during the COVID-19 pandemic. The ED was sectioned into three main areas: high-risk (pink), moderate-risk (yellow), and low-risk (blue) areas. High-risk areas included an outdoor triage, a quarantine zone, a quarantine station, and an isolation area that was composed of an isolation zone, two isolated resuscitation rooms, and a room to don and doff PPE. The moderate-risk area included an indoor triage, a resuscitation zone and a critical-care zone for critically ill patients, an ambulatory emergency care zone, and an acute care zone. The low-risk area (blue) consisted of an observation zone, where patients with negative COVID-19 PCR tests awaited admission or further management, and rooms to don and doff PPE. The blue arrow shows a one-way path to reallocate patients from moderate-risk areas to low-risk areas. The green arrow shows the direction of the staff flow to don PPE. The red arrow shows the direction to doff PPE and leave the ED. The iPad in the quarantine zone was placed on an immobile tablet security stand (triangle), and two iPads were given to physicians in the resuscitation zone, ambulatory emergency care (AEC) zone, acute care zone, and observation zone (circles).
In the high-risk area, we demarcated four spaces: an outdoor triage, a quarantine zone, a quarantine station, and an isolation sector that consisted of an isolation zone and an isolation resuscitation zone. Ambulatory patients with high-risk and stable vitals were diverted to the quarantine sectors. Across the quarantine zone, a quarantine station was set up. The quarantine station, designed to relieve the surging ED workload, was a structured building with 18 isolated compartments and was operated by a separate team. The isolation sector consisted of an isolation zone and two negative-pressure isolated resuscitation rooms. The isolation zone was designed to allocate high-risk, non-ambulatory patients with stable vitals. Those at high risk and in need of emergency critical care were placed in negative-pressure resuscitation rooms.
The moderate-risk area included an ambulatory emergency care zone, an acute care zone, a resuscitation zone, and a critical-care zone. The acute care zone, with a capacity of 12 beds, was used to manage non-ambulatory patients. The resuscitation zone and critical-care zone had space for 36 beds.
All patients were tested with rapid COVID-19 polymerase chain reaction (PCR) tests. The low-risk area, composed of an observation zone and dressing rooms to don and doff PPE, was used to allocate patients with negative COVID-19 PCR tests who were awaiting admission or further management. This zone had a capacity of 30 beds.
Different levels of PPE were required for staff according to the risk level. The PPE had to be changed when the medical staff moved from one zone to another.
2.3. Patient Flow and the Diversion Protocol
All patients who visited the ED were diverted to the designated areas according to their risk of COVID-19 infection. To accomplish this diversion policy and to streamline the process, the patient flow was modified into a triple triage protocol: (1) the first triage in the outdoor triage area to screen each patient’s history of travel, occupation, clusters of contacts, and symptoms; (2) the second triage to assess the patient’s vitals; and (3) the third triage to evaluate the patient’s ambulatory status. The protocol of patient flow is shown in Figure 2.
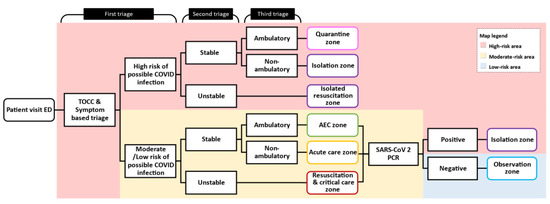
Figure 2.
Patient flow and protocol. We modified a triple triage protocol to stratify patients’ risks of COVID-19 infection and diverted them into different areas accordingly. Abbreviations: Acute emergency care zone (AEC).
The first triage was set up outside the ED entrance. All ED patients first underwent TOCC (travel, occupation, contact, and cluster) and symptom-based triage. Patients who had positive TOCC, fever up to 37.5 °C within the last three days, or any two of five symptoms (cough, rhinorrhea, diarrhea, lethargy, or anosmia) were triaged as high-risk. The purpose of the outdoor triage with TOCC and symptom-based triage was to segregate high-risk patients from others to prevent disease spread and to remind staff to take appropriate precautions. After the first triage, the patient was diverted to either the high-risk or the moderate-risk area and proceeded to step two, the second triage.
The second triage took place in the outdoor triage if the patient was of high-risk and indoors if the patient was of moderate/low-risk. The purpose of the second triage was to evaluate whether the patient was stable. Patients who had either an ambient oxygen saturation below 92% or a shock index (defined as the heart rate (beats/minute) divided by systolic blood pressure (mmHg) greater than 1 were defined as unstable. High-risk patients who were unstable were placed in the isolated resuscitation room for urgent medical management. Moderate/low-risk patients who were unstable were placed in the resuscitation bay or critical-care zone. Those who were stable proceeded to step three, the third triage.
The third triage was to evaluate the stable patients’ ambulatory status. During pandemics, the number of stable patients who still need ED care can be exceedingly high, so the third triage was essential to divert the ED patient flow. In the high-risk area, stable and ambulatory patients were placed in the quarantine zone; non-ambulatory patients were placed in the isolation zone. In the moderate-risk area, stable and ambulatory patients were allocated to the ambulatory emergency care zone; non-ambulatory patients were placed in the acute care zone.
Patients with moderate/low-risk were treated and managed in the ED. All patients were tested with rapid COVID-19 PCR tests. Those who had negative rapid COVID-19 PCR test results were defined as low-risk and subsequently reallocated to the observation zone in the low-risk area.
2.4. The ICT Module
Our information technology team deployed nine iPads (iPad 8th generation with iPad OS 14 system and Wi-Fi, Apple Inc., Cupertino, CA, USA) in the ED, one in the quarantine zone and two in each other zone (Figure 1). Each iPad was equipped with FaceTime (Apple Inc., Cupertino, CA, USA), which provided the ability to make free audio or video calls. We composed and provided an instruction manual to our staff. The iPads in the different zones were mobile and handled by physicians in each zone, while the iPad in the quarantine zone was placed on a stand.
The patient-side iPad was in the quarantine zone. The iPad was placed on a tablet security stand (Figure 3), covered with a transparent wrap, and anchored in the quarantined area. The iPad in the quarantine zone was disinfected with 70% alcohol sanitizer after each encounter, and the transparent cover was changed regularly.

Figure 3.
iPad in the quarantine zone. (A). The iPad in the quarantine zone was placed on an immobile security stand and covered with a transparent plastic wrap, which was regularly changed, and the tablet was sanitized after each encounter. (B). This picture shows the patient’s view of the tablet in the quarantine zone when a physician initiated virtual communication via FaceTime. (C). Virtual communication between physicians in different zones could be achieved with iPads and FaceTime. The photo consent was obtained.
The physician-side iPads were in the resuscitation zone, acute care zone, ambulatory emergency care zone, and observation zone. Patient handover between different zones or work shifts could also utilize ICT communication to reduce contact between medical personnel. With the iPad equipped in each area, physicians could initiate either audio or video communication, thereby obtaining the patient’s history and presenting illness without direct contact. Explaining examination results and discussing treatment plans among physicians, patients, and their families could be achieved through this ICT module.
2.5. Focus Group Study
As we discussed previously, the purpose of conducting this research was to explore the factors influencing the development of the ICT to assess patients in the ED. Consequently, we employed a qualitative approach to design this study. A qualitative approach is preferable for investigating the quality of a social phenomenon as it provides rich discussions and descriptions considering the research question we proposed [29,30,31].
More specifically, we conducted focus group interviews to gain insights and understanding from those physicians who utilized the ICT (see Appendix A for the interview guide). The value of a focus group is its ability to enable the research team to further understand those key factors influencing the effectiveness of applying the ICT during the COVID-19 pandemic. Moreover, it provides a more comprehensive approach to further explore those common themes and concepts mentioned by our interviewees. In this research, a single-disciplined focus group study was conducted two weeks after the implementation of patient evaluation using ICT. A homogeneous focus group facilitates information sharing and the process of reaching conclusions [32]. Participants were recruited from a population of 54 emergency physicians.
Following the principles of conducting a qualitative study, the research team utilized the standard case sampling method, which reflects the “average-like sample” in the selected hospital [31]. Consequently, the research team determined the number of participants, including the moderator, which was set to be between six and ten. Of those participants, it was determined that half would come from being directly involved in the development of ICT modules in the study hospital and the other half would come from having had experience using the ICT module. Participation was voluntary, and no financial reimbursement was provided. Participants were free to drop out at any time.
The focus-group discussion had three sessions and was conducted in June 2021. Each session lasted approximately 1–1.5 h. The sessions were conducted every other day and were led by an experienced moderator. The discussions were internet-based, using the video-conference application Google Meet (Google Inc., Mountain View, CA, USA). To facilitate the data collection and analysis, a member of the research team took notes during every discussion. These notes were then shared with all participants after those interviews to ensure they reflected the discussions and insights of the group interviews.
As a result, the research team analyzed the notes and grouped those common themes and concepts manually together. Since there were a relatively small number of interview notes, and there was little previous research relevant to this subject, the researchers selected the grounded theory approach to analyze the data [33]. The researchers utilized the open coding process to identify concepts and themes within the interview notes and later connected them to develop a complete analysis. More specifically, researchers first performed an inductive thematic analysis of the data, including coding and categorizing the data. During this process, data were thematically analyzed using the theoretical framework of acceptability of healthcare interventions to assess the acceptability they experienced from the perspective of implementation delivery [34].
To enhance the validity of this research, the research team met every week to discuss the definitions of each code and compare the results from the data collection. By cross-coding the same qualitative data, the research team was able to merge certain codes and develop new codes. This method, peer debriefing, ensures the coding processes would reflect the insights and consensus from all researchers, and not merely from individual perspectives [35]. Those themes and factors generated from the data analysis were then reviewed by the research team, and similar ideas and concepts were merged to reach a final consensus.
3. Results
Eight emergency physicians, with the highest education level of Doctor of Medicine, participated in the study. None of the participants dropped out. Of them, four (50%) had been directly involved in the development of the ICT module in the study hospital. Two (25%) of the participants were female. The age and working experience of the participants ranged from 28 to 48 years and 3 to 20 years, respectively.
Three main themes were identified in their considerations on using ICT for patient assessment in the ED: setting, hardware, and software.
The first theme, “setting”, has six major factors: patient evaluation, consultation with subspecialty, patient privacy and comfortableness, sanitation, cost, and patient acceptability. Important considerations regarding the setting are summarized in Table 1.

Table 1.
Important considerations regarding the setting when using instant communication technology for patient assessment in an emergency department.
The second theme, “hardware”, has six major factors: Wi-Fi/internet connection, power, image and voice quality, public/personal modes, portable/fixed modes, and maintenance (Table 2).

Table 2.
Important considerations regarding the hardware when using instant communication technology for patient assessment in an emergency department.
The third theme, “software”, has six major factors: platform choices, security, ICT accounts, interview modes, video/voice recording, and time limitation (Table 3).

Table 3.
Important considerations regarding the software when using instant communication technology for patient assessment in an emergency department.
4. Discussion
Our study identified several important factors in deploying an ICT module to assess patients in an ED. We found that ICT may be an option for evaluating patients presenting with mild symptoms and could be an important way to reduce infection risk during the pandemic.
The pandemic has significantly transformed the concept of telemedicine. Before the COVID-19 pandemic, telemedicine was commonly applied to chronic and stable patients in remote areas or less accessible settings. For instance, telemedicine was applied in home palliative hospice care to reduce emergency department visits [36]. Telemedicine was efficiently used in monitoring chronic conditions such as management of heart failure or blood sugar control consultations in diabetic patients [37]. Telemedicine was also widely utilized in prehospital settings, such as patient interviews and consultations, patient triage, and telemonitoring. In prehospital settings, synchronous video communication aided in providing the call dispatcher with more information on the scene when handling emergency calls [38]. In contrast to traditional remote telemedicine in outpatient settings, the purpose of applying ICT in the ED during the COVID-19 pandemic was to reduce direct contact between healthcare providers and patients and thus minimize disease transmission risk.
During the pandemic, we modified and regionalized our ED into different areas and zones according to the patient’s risk of COVID-19 infection. Different levels of PPE were suggested for different areas and had to be changed if personnel were to move from one area to another. Communication between medical staff in different areas who were wearing full PPE was a challenge. However, this was largely resolved by the implementation of the ICT module.
We found the use of ICT for patient assessment was more suitable for ambulatory patients that presented with mild symptoms. Although ICT was useful for history taking, general appearance assessment, and collecting information from patients’ families that were not present in the ED, most emergency physicians were less comfortable performing physical examinations using ICT due to previous practice habits.
The internet signal and bandwidth connectivity influenced the quality of images and video, which thereby impacted the effectiveness of ICT. Our hospital provided a stable, low-cost, and high-quality internet connection. However, different hospital settings may pose challenges in this area. A stable, wide-bandwidth, high-quality internet or Wi-Fi connection was essential to make the ICT module workable. Hospitals located in rural areas or those that have lower levels of specialty care may face challenges in providing stable and sufficient internet connection and maintenance. Choice of communication applications and platform was based on the tablet’s operating system and user familiarity. The device and platform used in our ICT module were iPad and FaceTime since their dominant market share might diminish utility barriers, especially among patients. Sanitation was achieved by regularly changing the covering wraps on the tablet and disinfecting the device with 70% alcohol sanitizer after each encounter [39].
We faced several challenges when setting up the ICT module in our ED. Some challenges we found in the setting themes were application of ICT in the evaluation of disabled patients or those with language barriers, protecting patient privacy, and the familiarity of ICT use in elder patients. Elder patients and those with a lower socioeconomic status may be less familiar with the use of tablets and can negatively affect the efficiency of virtual patient evaluation. Those who were elderly, disabled, and lacked digital literacy were less able to access computer devices.
Telemedicine platforms seldom aid in communication for patients with hearing, visual, or cognitive disabilities. ICT accessibilities for disabled patients should be taken into consideration and enforced [40]. To overcome this obstacle, when designing protocols in the future, hearing impairments and other disabilities should be taken into consideration. Communications between physicians and patients with hearing disabilities or language barriers could be performed via ICT that has add-on functions of lip reading, sign language, or real-time audio interpretation.
Another challenge we faced concerning software aspects was patients’ cybersecurity. Security checks and upgrades were performed regularly by our information technology team to prevent personal information breaches. However, not all hospitals or EDs have an information technology team. Maintenance service and efforts must be taken into consideration when planning an ICT module.
Our module required both the patient and physicians to learn how to use the iPad and FaceTime, so we provided an instruction manual. An ICT module should be set up on a regular basis. Medical staff should use this module more frequently to evaluate patients and practice communicating with each other to such an extent that all staff members are familiar with the module. Hence, when there is an outbreak of an infectious disease, the module can be useful to all staff members and shorten the accustoming time.
Our study had several limitations. First, this study was conducted during the initial phase of community outbreak and the resource of rapid diagnostic tools for COVID-19 was extremely scanty. The ED workflow and regionalization could have been extensively modified with a different model should the rapid screening tests have been readily available. Second, we did not evaluate the patients’ perspectives. The comfortableness of medical and nursing staff using tablets for communication was not addressed in our study as well. Questionnaires on satisfaction of using ICT will be provided in the future. Third, prehospital settings were not included in our investigation. However, with appropriate devices and software applications, our protocol can be applied to connect physicians and nonphysicians, such as medical staff in nursing homes or emergency medical technicians. Finally, we used grounded theory in this study because as an exploratory method, grounded theory is suitable for investigating issues that have attracted limited prior research attention. As a method that has advanced over time, grounded theory is a broadly applied research method that has incorporated several different variants [41]. Our study was a pilot study focusing on the challenges of using ICT in the EDs during pandemics. Although digital expertise and ICT have rapidly advanced, there is a disparity in the attitudes and competence levels towards technology among different populations. During the pandemic, the pace of ED workflow changes and adjustments have been expeditious, adding to the difficulties of this study. Although our study interviewed a limited number of practitioners, we believe the results of our study will facilitate the application of communication technology in medical scenarios and could be valuable for future researchers.
5. Conclusions
We identified several important considerations that should be addressed in the future development of ICT modules for ED patient assessment, categorized under the setting, hardware, and software. Studies that quantify the utility and feasibility of this module, along with patient and staff satisfaction, should be investigated. With adjustments to the protocol, the ICT module could be applied in prehospital or critical-care settings to provide more thorough, contact-free healthcare.
Author Contributions
Conceptualization, Y.-S.K., C.-H.L. (Chien-Hsin Lu) and C.-H.L. (Chih-Hao Lin); data curation, Y.-S.K., C.-H.L. (Chien-Hsin Lu), P.-W.C., H.-C.C., P.-Y.W., C.-J.C., I.-C.L. and C.-H.L. (Chih-Hao Lin); formal analysis, Y.-S.K., C.-H.L. (Chien-Hsin Lu), P.-W.C. and C.-H.L. (Chih-Hao Lin); funding acquisition, C.-H.L. (Chien-Hsin Lu) and C.-H.L. (Chih-Hao Lin); investigation, Y.-S.K., C.-H.L. (Chien-Hsin Lu), P.-W.C., H.-C.C., P.-Y.W., C.-J.C., I.-C.L. and C.-H.L. (Chih-Hao Lin); methodology, R.H.C., J.-S.T. and C.-H.L. (Chih-Hao Lin); project administration, C.-H.L. (Chien-Hsin Lu), R.H.C., Y.-H.C. and C.-H.L. (Chih-Hao Lin); resources, Y.-H.C. and C.-H.L. (Chih-Hao Lin); software, C.-H.L. (Chien-Hsin Lu) and R.H.C.; supervision, C.-H.L. (Chih-Hao Lin); validation, C.-H.L. (Chien-Hsin Lu), P.-W.C., H.-C.C., P.-Y.W., C.-J.C. and C.-H.L. (Chih-Hao Lin); Visualization, Y.-S.K., C.-H.L. (Chien-Hsin Lu) and C.-H.L. (Chih-Hao Lin); writing—original draft, Y.-S.K., C.-H.L. (Chien-Hsin Lu) and C.-H.L. (Chih-Hao Lin); writing—review and editing, Y.-S.K., C.-H.L. (Chien-Hsin Lu), P.-W.C., R.H.C., J.-S.T., H.-C.C., P.-Y.W., C.-J.C., I.-C.L., S.-P.H., Y.-Y.L., Y.-H.C. and C.-H.L. (Chih-Hao Lin). Y.-S.K. and C.-H.L. (Chien-Hsin Lu) contributed equally as first authors. R.H.C. and C.-H.L. (Chih-Hao Lin) contributed equally as corresponding authors and take responsibility for the paper as a whole. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by the National Cheng Kung University Hospital (NCKUH-11003031) and the Taiwan Ministry of Science and Technology (MOST 109-2327-B-006-008 and MOST 109-2327-B-006-005).
Institutional Review Board Statement
The study was in accordance with ethical standards and was approved by the Institutional Review Board in National Cheng Kung University Hospital (B-ER-110-438-T).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare that they have no known competing financial interest or personal relationship that could have appeared to influence the work reported in this paper.
Abbreviations
| ED | Emergency department |
| ICT | Instant communication technology |
| PCR | polymerase chain reaction |
| PPE | personal protection equipment |
| TOCC | travel, occupation, contact, and cluster |
Appendix A. The Interview Guide
- Do you have experience on using the ICT to communicate with other people?
- If yes, what are the obstacles on using the ICT?
- What are the major factors influencing the usage of the ICT?
- What are the software and hardware you will use with the ICT to facilitate communications?
- What are the factors that would influence your selection of these software and/or hardware?
- Do you have any experience on using the ICT to communicate with your patience in hospitals?
- If yes, what are the major factors contribute to the usage of the ICT in the field of Emergency Medicine (EM).
- If yes, what are the obstacles on using the ICT in the field of EM.
- If yes, what are the pros and cons of using the ICT in the field of EM during the COVID-19 pandemic?
- Anything you think should be improved to better using the ICT in the field of EM during this pandemic?
- From your perspectives, how does the ICT contribute to the communication between physicians and patients?
References
- Lin, C.-H.; Hsieh, C.-C.; Chi, C.-H. Hospital Emergency Management of Emerging Infectious Disease using Instant Communication Technology. Prehospital Disaster Med. 2020, 35, 465–466. [Google Scholar] [CrossRef]
- Friedman, J.; Lame, M.; Clark, S.; Gogia, K.; Platt, S.L.; Kim, J.W. Telemedicine Medical Screening Evaluation Expedites the Initiation of Emergency Care for Children. Pediatr. Emerg. Care 2021, 37, e417–e420. [Google Scholar] [CrossRef]
- Fang, J.; Liu, Y.T.; Lee, E.Y.; Yadav, K. Telehealth Solutions for In-hospital Communication with Patients Under Isolation during COVID-19. West. J. Emerg. Med. 2020, 21, 801–806. [Google Scholar] [CrossRef]
- Li, J.-P.O.; Thomas, A.A.; Kilduff, C.L.; Logeswaran, A.; Ramessur, R.; Jaselsky, A.; Sim, D.A.; Hay, G.R.; Thomas, P.B. Safety of video-based telemedicine compared to in-person triage in emergency ophthalmology during COVID-19. EClinicalMedicine 2021, 34, 100818. [Google Scholar] [CrossRef] [PubMed]
- Wittbold, K.A.; Baugh, J.J.; Yun, B.J.; Raja, A.S.; White, B.A. iPad deployment for virtual evaluation in the emergency department during the COVID-19 pandemic. Am. J. Emerg. Med. 2020, 38, 2733–2734. [Google Scholar] [CrossRef]
- Lowe, J.; Shen, S. Off the Shelf: Rapid Deployment of an Emergency Department Telemedicine Platform Using Readily Available Consumer Products. J. Emerg. Med. 2020, 59, 726–729. [Google Scholar] [CrossRef]
- Sabırlı, R.; Karsli, E.; Canacik, O.; Ercin, D.; Çiftçi, H.; Sahin, L.; Dolanbay, T.; Tutuncu, E.E. Use of WhatsApp for Polyclinic Consultation of Suspected Patients With COVID-19: Retrospective Case Control Study. JMIR mHealth uHealth 2020, 8, e22874. [Google Scholar] [CrossRef] [PubMed]
- AlShaya, M.; Assery, M.K.; Pani, S.C. Reliability of mobile phone teledentistry in dental diagnosis and treatment planning in mixed dentition. J. Telemed. Telecare 2020, 26, 45–52. [Google Scholar] [CrossRef]
- Siddiqui, J.; Herchline, T.; Kahlon, S.; Moyer, K.J.; Scott, J.D.; Wood, B.R.; Young, J. Infectious Diseases Society of America Position Statement on Telehealth and Telemedicine as Applied to the Practice of Infectious Diseases. Clin. Infect. Dis. 2017, 64, 237–242. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, N.R.; Steinberg, A.; Arnold, R.M.; Doshi, A.A.; White, D.B.; DeLair, W.; Nigra, K.; Elmer, J. Perspectives on Telephone and Video Communication in the Intensive Care Unit during COVID-19. Ann. Am. Thorac. Soc. 2021, 18, 838–847. [Google Scholar] [CrossRef]
- Candel, B.G.J.; Vaes, S.M.M.; van Bree, E.M.; Groenen, S.M.A.; Derkx, F.; Mignot, L.A.A.; de Groot, B. Telemedicine in the emergency department to decrease personal protective equipment use: A before-and-after study. Emerg. Med. J. 2021, 38, 224–228. [Google Scholar] [CrossRef]
- Domingues, R.B.; Mantese, C.E.; Aquino, E.D.S.; Fantini, F.G.M.M.; Prado, G.F.D.; Nitrini, R. Telemedicine in neurology: Current evidence. Arq. Neuro-Psiquiatr. 2020, 78, 818–826. [Google Scholar] [CrossRef]
- Makhni, M.C.; Riew, G.J.; Sumathipala, M.G. Telemedicine in Orthopaedic Surgery. J. Bone Jt. Surg. Am. Vol. 2020, 102, 1109–1115. [Google Scholar] [CrossRef]
- Chau, M.J.; Quintero, J.E.; Guiliani, A.; Hines, T.; Samaan, C.; Seybold, K.; Stowe, M.; Hanlon, D.; Gerhardth, G.A.; van Horne, C.G. Telehealth Sustainability in a Neurosurgery Department During the COVID-19 Pandemic. World Neurosurg. 2021, 152, e617–e624. [Google Scholar] [CrossRef] [PubMed]
- Villa, L.; Matz, O.; Dague, K.O.; Kluwig, D.; Rossaint, R.; Brokmann, J.C. The assessment of dermatological emergencies in the emergency department via telemedicine is safe: A prospective pilot study. Intern. Emerg. Med. 2020, 15, 1275–1279. [Google Scholar] [CrossRef] [PubMed]
- Flint, L.; Kotwal, A. The New Normal: Key Considerations for Effective Serious Illness Communication Over Video or Telephone During the Coronavirus Disease 2019 (COVID-19) Pandemic. Ann. Intern. Med. 2020, 173, 486–488. [Google Scholar] [CrossRef]
- Fenn, D.; Coppel, J.; Kearney, J.; Everson, L.; Braithwaite, S.; Chodhari, R. Walkie talkies to aid health care workers’ compliance with personal protective equipment in the fight against COVID-19. Crit. Care 2020, 24, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Alhajri, N.; Simsekler, M.C.E.; Alfalasi, B.; Alhashmi, M.; AlGhatrif, M.; Balalaa, N.; Al Ali, M.; Almaashari, R.; Al Memari, S.; Al Hosani, F.; et al. Physicians’ Attitudes Toward Telemedicine Consultations During the COVID-19 Pandemic: Cross-sectional Study. JMIR Med. Inform. 2021, 9, e29251. [Google Scholar] [CrossRef] [PubMed]
- Wilhite, J.A.; Altshuler, L.; Fisher, H.; Gillespie, C.; Hanley, K.; Goldberg, E.; Wallach, A.; Zabar, S. The Telemedicine Takeover: Lessons Learned During an Emerging Pandemic. Telemed. e-Health 2021. [Google Scholar] [CrossRef]
- Hammersley, V.; Donaghy, E.; Parker, R.; McNeilly, H.; Atherton, H.; Bikker, A.; Campbell, J.; McKinstry, B. Comparing the content and quality of video, telephone, and face-to-face consultations: A non-randomised, quasi-experimental, exploratory study in UK primary care. Br. J. Gen. Pr. 2019, 69, e595–e604. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boissin, C.; Blom, L.; Wallis, L.; Laflamme, L. Image-based teleconsultation using smartphones or tablets: Qualitative assessment of medical experts. Emerg. Med. J. 2017, 34, 95–99. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Iyengar, K.; Upadhyaya, G.K.; Vaishya, R.; Jain, V. COVID-19 and applications of smartphone technology in the current pandemic. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 733–737. [Google Scholar] [CrossRef] [PubMed]
- Saleem, J.J.; Savoy, A.; Etherton, G.; Herout, J. Investigating the need for clinicians to use tablet computers with a newly envisioned electronic health record. Int. J. Med. Inform. 2018, 110, 25–30. [Google Scholar] [CrossRef] [Green Version]
- Horng, S.; Goss, F.R.; Chen, R.S.; Nathanson, L.A. Prospective pilot study of a tablet computer in an Emergency Department. Int. J. Med. Inform. 2012, 81, 314–319. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mickan, S.; Atherton, H.; Roberts, N.W.; Heneghan, C.; Tilson, J.K. Use of handheld computers in clinical practice: A systematic review. BMC Med. Inform. Decis. Mak. 2014, 14, 56. [Google Scholar] [CrossRef] [Green Version]
- Kaczmarek, B.F.; Trinh, Q.-D.; Menon, M.; Rogers, C.G. Tablet Telerounding. Urology 2012, 80, 1383–1388. [Google Scholar] [CrossRef]
- Hamm, J.M.; Greene, C.; Sweeney, M.; Mohammadie, S.; Thompson, L.B.; Wallace, E.; Schrading, W. Telemedicine in the emergency department in the era of COVID-19: Front-line experiences from 2 institutions. J. Am. Coll. Emerg. Physicians Open 2020, 1, 1630–1636. [Google Scholar] [CrossRef]
- Legler, S.; Diehl, M.; Hilliard, B.; Olson, A.; Markowitz, R.; Tignanelli, C.; Melton, G.B.; Broccard, A.; Kirsch, J.; Usher, M. Evaluation of an Intrahospital Telemedicine Program for Patients Admitted With COVID-19: Mixed Methods Study. J. Med. Internet Res. 2021, 23, e25987. [Google Scholar] [CrossRef]
- Berg, B.; Lune, H. Qualitative Research Methods for the Social Scientists; Pearson Education, Inc.: Hoboken, NJ, USA, 2012. [Google Scholar]
- Creswell, J.W.; Poth, C.N. Qualitative Inquiry and Research Design: Choosing Among Five Approaches; Sage Publications: Thousand Oaks, CA, USA, 2018. [Google Scholar]
- Patton, M.Q. Qualitative Research and Evaluation Methods, 3rd ed.; Sage Publications: Thousand Oaks, CA, USA, 2002. [Google Scholar]
- Mansell, I.; Bennett, G.; Northway, R.; Mead, D.; Moseley, L. The learning curve: The advantages and disadvantages in the use of focus groups as a method of data collection. Nurse Res. 2004, 11, 79–88. [Google Scholar] [CrossRef]
- Grbich, C. Qualitative Data Analysis: An. Introduction, 2nd ed.; Sage Publication Ltd.: London, UK, 2013. [Google Scholar]
- Sekhon, M.; Cartwright, M.; Francis, J.J. Acceptability of healthcare interventions: An overview of reviews and development of a theoretical framework. BMC Health Serv. Res. 2017, 17, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Cynthia, S. Franklin PACMB. Reliability and validity in qualitative research. In The Handbook of Social Work Research Methods, 2nd ed.; Thyer, B.A., Ed.; Sage Publication Inc.: London, UK, 2010; pp. 355–374. [Google Scholar]
- Teter, C.M.; Whitted, K.; Vardaman, S.A. Reducing Hospital Visit Rates in Hospice Patients Using Telemedicine. CIN Comput. Inform. Nurs. 2021, 39, 682–688. [Google Scholar] [CrossRef]
- Flodgren, G.; Rachas, A.; Farmer, A.J.; Inzitari, M.; Shepperd, S. Interactive telemedicine: Effects on professional practice and health care outcomes. Cochrane Database Syst. Rev. 2015, 2015, CD002098. [Google Scholar] [CrossRef] [PubMed]
- Avest, E.T.; Lambert, E.; De Coverly, R.; Tucker, H.; Griggs, J.; Wilson, M.H.; Ghorbangholi, A.; Williams, J.; Lyon, R.M. Live video footage from scene to aid helicopter emergency medical service dispatch: A feasibility study. Scand. J. Trauma Resusc. Emerg. Med. 2019, 27, 55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Apple.com. How to Clean Your Apple Products. Available online: https://support.apple.com/en-us/HT204172 (accessed on 16 June 2021).
- Annaswamy, T.M.; Verduzco-Gutierrez, M.; Frieden, L. Telemedicine barriers and challenges for persons with disabilities: COVID-19 and beyond. Disabil. Health J. 2020, 13, 100973. [Google Scholar] [CrossRef]
- Foley, G.; Timonen, V. Using Grounded Theory Method to Capture and Analyze Health Care Experiences. Health Serv. Res. 2014, 50, 1195–1210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).