Abstract
The mental health of nurses including burnout is an important issue. The purpose of this systematic review was to evaluate whether mind-body modalities improve burnout and other mental health aspects of nurses. A comprehensive search was conducted using six electronic databases. Randomized controlled trials using mind-body modalities on the mental health of nurses, up to January 2021, were included. The methodological quality of the included studies was assessed using the Cochrane Risk of Bias tool. Seventeen studies were included in the review. Data on mindfulness-based interventions (MBIs) and yoga were available for burnout, and there was no evidence that multimodal resilience programs including MBIs statistically significantly improved burnout levels compared to no intervention or active control groups. However, one study reported that yoga could significantly improve emotional exhaustion and depersonalization, which are subscales of burnout, compared to usual care. In addition, the effects of MBIs, relaxation, yoga, and music on various mental health outcomes and stress-related symptoms have been reported. In conclusion, there was some evidence that yoga was helpful for improvement in burnout of nurses. However, due to the heterogeneity of interventions and outcomes of the studies included, further high-quality clinical trials are needed on this topic in the future.
1. Introduction
The mental health problems of nurses are common, and nurses are exposed to a variety of mental health risk factors, including work demands, psychological demands, violence, aggression, poor relationships with administrators, accidents involving the risk of exposure to human immunodeficiency virus, stress, and errors in the execution of labor activities [1]. Among various mental health problems, burnout is a major cause of emotional exhaustion, high depersonalization, and low personal accomplishment, and its prevalence in primary care nurses is common at 28%, 15%, and 31%, respectively [2]. Importantly, the burnout of nurses can affect, beyond the individual level, the organization to which they belong, or patient outcomes on account of their decreased job performance, more sick leave, and more absences [3].
Mind-body modalities have been used to cope with stress-related problems for a long time, and as evaluated currently, they are moving to the mainstream based on the empirical clinical evidence accumulated in the aspect of evidence-based medicine (EBM) [4]. Mind-body modalities including tai chi, qigong, yoga, and meditation have been used in several populations to manage stress and improve physical and mental health, including in patients with cardiac disease [5], multiple sclerosis [6], fibromyalgia [7], and chronic pain [8]. Moreover, according to the 2007 National Health Interview Survey, adults with common neurological conditions, such as headache, stroke, and cognitive impairment, used mind-body modalities significantly more often than adults who did not, at a rate of 24.5% [9]. Studies examining the biological mechanisms of mind-body modalities have confirmed that these treatments have immunomodulatory and anti-inflammatory properties [10,11] that may be related to enhanced neurogenesis and neuroplasticity [12]. In addition, studies have reported that mind-body modalities may have a positive role in stress responsiveness by affecting biomarkers such as cortisol, dehydroepiandrosterone sulfate, and testosterone accordingly [13].
Likewise, mind-body modalities have the potential to improve nurses’ overall health and level of well-being and prevent and/or reduce burnout levels by alleviating the accompanying physical symptoms as well as improving the psychological stress of nurses. For example, a tertiary care hospital in the United States reported that mindfulness-based stress reduction (MBSR), a typical type of mindfulness-based interventions (MBIs), was introduced to staff nurses in the hospital, and it was reported that the program effectively reduced job burnout and improved mindfulness, self-compassion, and serenity in the participants [14]. Mindfulness practice is also being considered as an effective self-management method or a stress reduction technique for healthcare workers including nurse exposed to the COVID-19 pandemic and threatened with their mental health and well-being [15,16]. Therefore, examining the impact of mind-body modalities on the mental health of nurses will potentially help establish strategies to improve the mental health of healthcare workers in this unprecedented pandemic, and further potentially increase humanity’s capacity to respond to this pandemic. However, no study has systematically analyzed the effectiveness of mind-body modalities on the mental health problems of nurses. The purpose of this systematic review was hence to evaluate whether mind-body modalities improve burnout and other mental health aspects of nurses in hospital setting.
2. Methods
This systematic review complied with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement for reporting systematic reviews and meta-analyses [17] (Supplementary Table S1). The protocol of this systematic review was registered in OSF registries (doi:10.17605/OSF.IO/U8P3T), and this review followed the protocol.
2.1. Study Search
Comprehensive searches were conducted in a total of six international electronic databases, including MEDLINE (via PubMed), EMBASE (via Elsevier), the Cochrane Library Central Register of Controlled Trials, the Cumulative Index of Nursing and Allied Health Literature, the Allied and Complementary Medicine Database, and PsycARTICLES. In addition, a manual search on Google Scholar was conducted to search for gray and potentially missing literature, and a list of references from related papers including the studies included in this review was reviewed accordingly. The search date was 28 January 2021, and all related studies published up to the search date were reviewed. The study search was performed by a single researcher (Lee B). Search strategies for each database and search results are presented in Supplementary Table S2.
2.2. Study Selection and Inclusion Criteria
Two independent researchers (Jung SE and Ha DJ) selected the studies according to the following inclusion criteria: Title/abstract and full-text review. In case of disagreement between them, a third-party researcher (Kwon CY) intervened accordingly. (1) Population: Nurses in hospital settings, regardless of sex, age, and ethnicity (2) Intervention: Mind-body modalities including meditation, mindfulness intervention, autogenic training, yoga, tai chi, qigong, breathing exercise, music therapy, guided imagery, and biofeedback. (3) Comparator: No treatment, wait-list, sham control, attention control, or active comparators. (4) Outcomes: The primary outcome included the level of burnout assessed using validated assessment tools such as the Maslach Burnout Inventory [18], and secondary outcomes included all other mental health aspects or stress-related symptoms. (5) Study design: Only randomized controlled trials (RCTs) were allowed, and no restrictions on language were imposed in the study. That is, there are no restrictions on language sources in the selection for review.
2.3. Risk of Bias Assessment
The methodological quality of the included studies was assessed by two independent reviewers (Jung SE and Ha DJ) using the Cochrane risk of bias (RoB) tool. This tool judges the RoB of RCTs as high, low, or unclear in the domains of selection, performance, detection, attrition, reporting, and other biases. RoB evaluation followed the method described in the Cochrane Handbook for Systematic Reviews of Interventions version 5.1.0 [19]. In case of disagreement between the two independent reviewers, a third-party researcher (Kwon CY) intervened accordingly. The evaluated RoB results are presented as figures using RevMan 5.4.
2.4. Data Extraction
The following data from the eligible studies were extracted and entered into a Microsoft Excel file: Publication year, name of 1st author, information for RoB assessment, country where the study was performed, sample size, mean age, ward in which the participants worked, pathological condition of participants, treatment intervention, control intervention, intervention period, time of assessment, outcomes, and results.
2.5. Data Analysis
All included studies were analyzed qualitatively. Quantitative synthesis was not performed considering the heterogeneity of the interventions used in the included studies. Instead, the reported results were classified into occupational and environmental outcomes, individual resistance to stress, global health and wellness, psychological symptoms, physical symptoms, and biological data according to their characteristics. In addition, interventions were classified into MBIs, relaxation, yoga, music, and aromatherapy according to their characteristics. Upon comparison of the two groups, a case with p-value less than 0.05 was considered to be statistically significant.
2.6. Publication Bias
Due to the heterogeneity of the interventions and outcomes of the included studies, quantitative synthesis was not performed in this study. Therefore, publication bias using a funnel plot could not be evaluated.
3. Results
3.1. Study Search
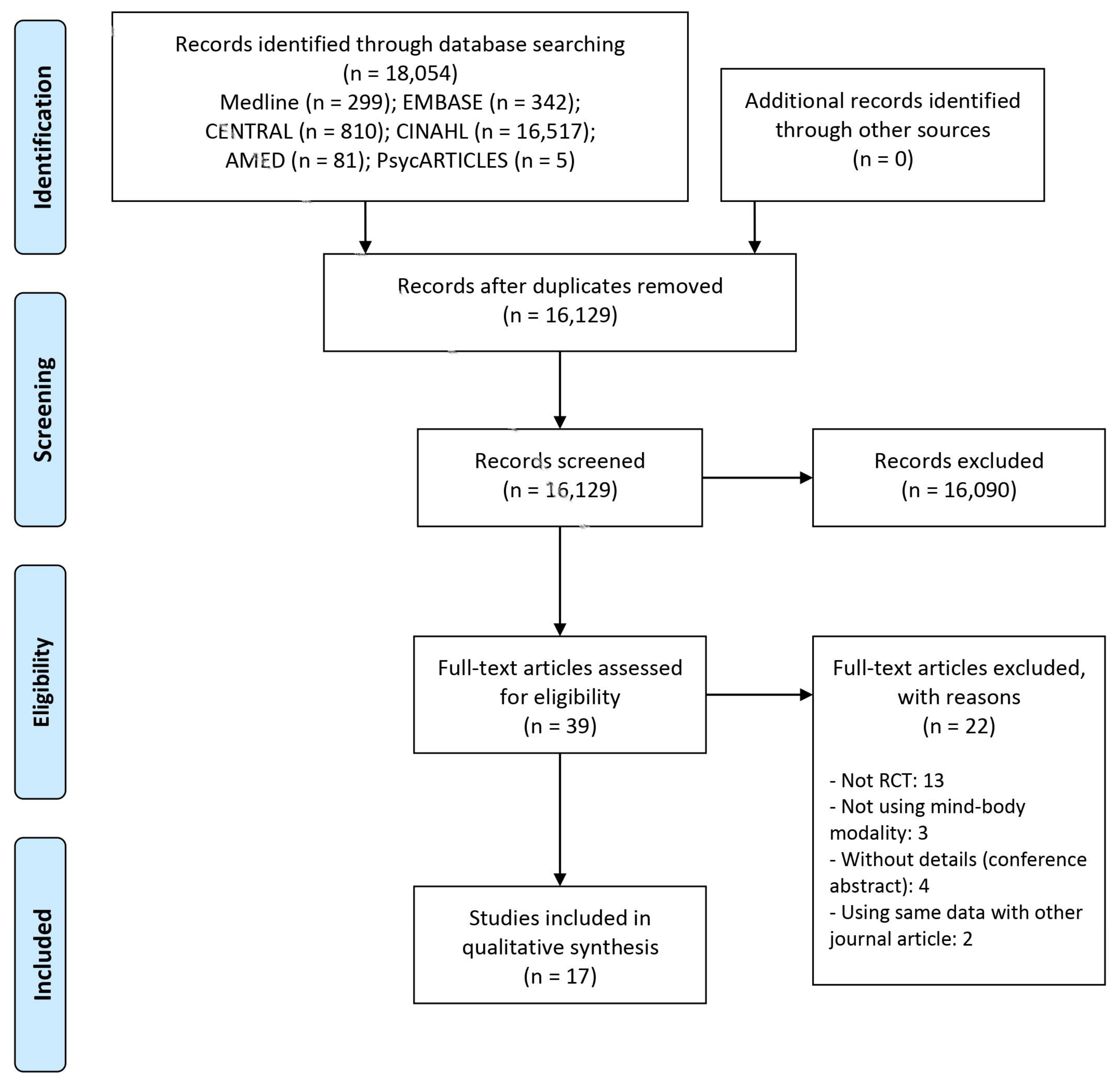
As a result of the literature search, 16,129 documents were identified after excluding duplicates. Among them, 39 potentially relevant articles were selected using the first title/abstract screening process. As a result of secondary screening for the full texts, 13 that were not RCTs [20,21,22,23,24,25,26,27,28,29,30,31,32], three that did not use mind-body modalities [33,34,35], four which were without details (conference abstract) [36,37,38,39], and two using the same data as other journal articles (thesis or conference abstract) [40,41], were excluded from the study. Finally, a total of 17 RCTs were included in this review [42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58] (Figure 1).
Figure 1.
A PRISMA flow diagram of the literature screening and selection processes. AMED, Allied and Complementary Medicine Database; CENTRAL, Cochrane Central Register of Controlled Trials; CINAHL, Cumulative Index to Nursing and Allied Health Literature.
3.2. Characteristics of Included Studies
Among the included studies, 15 were parallel RCTs [42,43,45,46,47,48,49,50,51,53,54,55,56,57,58] while the other two were cross-over RCTs [44,52]. All these studies were published between 1993 and 2020. Three studies each were conducted in the US [45,46,57] and China [47,50,51], two each in Taiwan [42,44] and Japan [52,55], and one each in Hong Kong [43], Korea [48], Greece [49], Turkey [53], France [54], Malaysia [56], and Iran [58]. The analyzed sample sizes of the included studies varied from 27 to 224. Four studies used yoga [46,47,52,54] as their intervention, three used music [44,49,58], and one used music combined with aromatherapy as well as music in its four-arm RCT [58]. Seven studies used MBIs, including MBSR in three [45,50,51], meditation [48], and mindfulness-based programs in three [55,56,57]. Three studies used relaxation [42,43,53]. Two studies used multimodal interventions, such as multimodal resilience training programs, including MBSR [45] and community resiliency models, including mindful eating [57] (Table 1).

Table 1.
Characteristics of included studies.
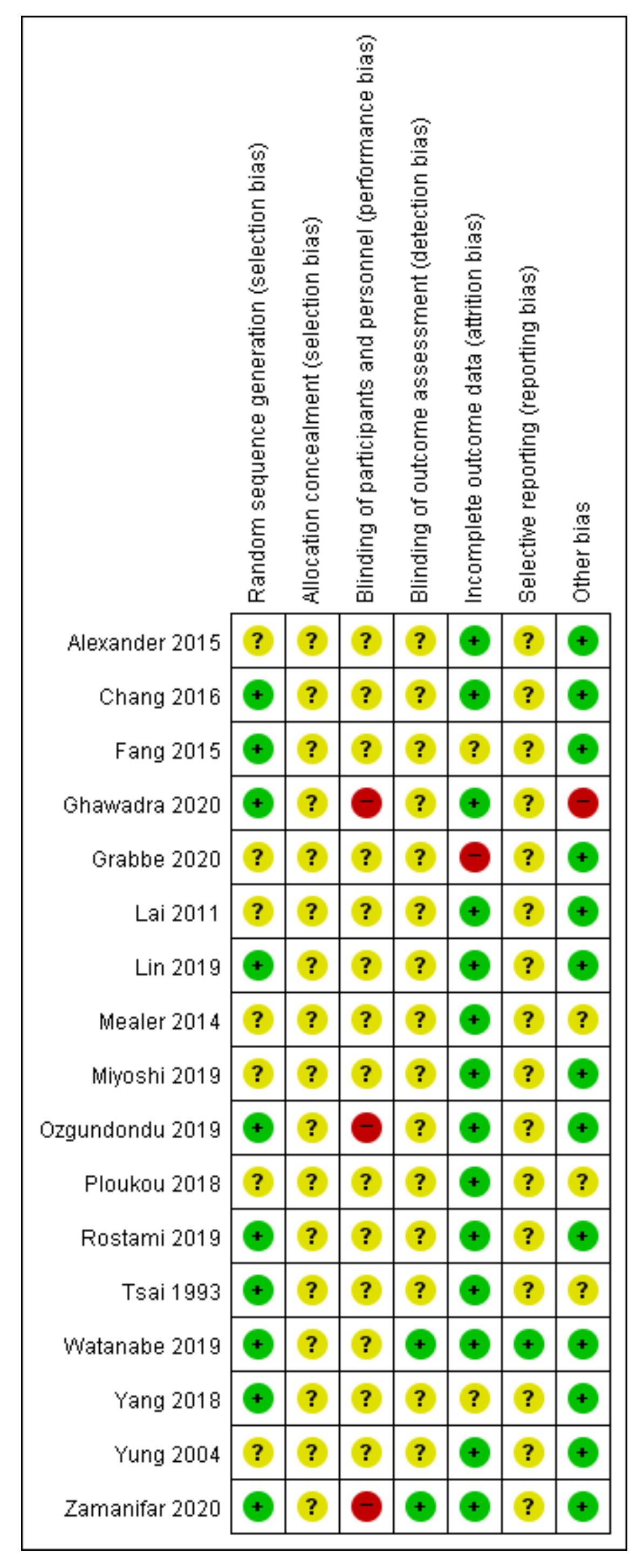
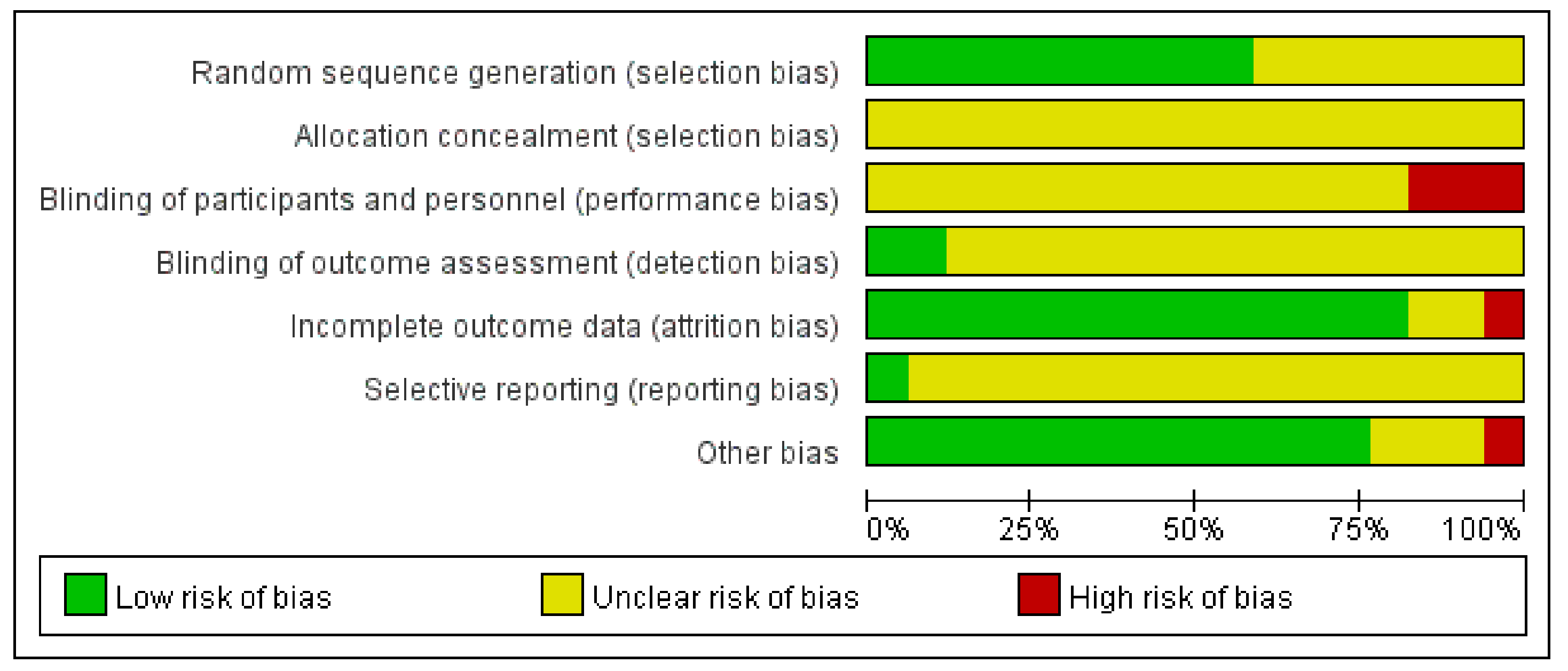
3.3. Methodological Qualities of Included Studies
In the random sequence generation domain, 10 studies [42,47,48,50,51,53,54,55,56,58] that used proper random sequence generation methods such as random number tables or simple randomization were rated as having low RoB, while the other seven [43,44,45,46,49,52,57] without a description of randomization method were rated to have unclear RoB. None of the included studies described allocation concealment and blinding of participants and personnel. In the blinding of participants and personnel domain, three [53,56,58] were rated as having a high RoB due to the nature of the intervention, while the others [42,43,44,45,46,47,48,49,50,51,52,54,55,57] were rated as having an unclear RoB. Only two studies [55,58] described that they performed the blinding of outcome assessment, while the rest of the studies [42,43,44,45,46,47,48,49,50,51,52,53,54,56,57] did not. In eight studies, there were no drop-out cases [43,44,45,46,49,52,54,58]. Some drop-out cases existed in the remaining studies; however, the numbers of the cases probably did not affect the study results [42], they were similar between groups with appropriate reasons for drop-out [48,51,53], and/or appropriate statistical analysis (i.e., intent-to-treat analysis) was applied accordingly [55,56]. Since no previously published protocols were identified except for one study [55], the other studies [42,43,44,45,46,47,48,49,50,51,52,53,54,56,57,58] were evaluated as having unclear RoB in the selective reporting domain. Regarding other biases, 13 studies [43,44,46,47,48,50,51,52,53,54,55,57,58] describing statistically homogeneous demographic and clinical characteristics between the groups at baseline were evaluated as having low RoB. One study [56] describing the significant difference between the groups at baseline was evaluated as having a high RoB. The other three did not describe statistical homogeneity between the groups at baseline [42,45,49] (Figure 2 and Figure 3).
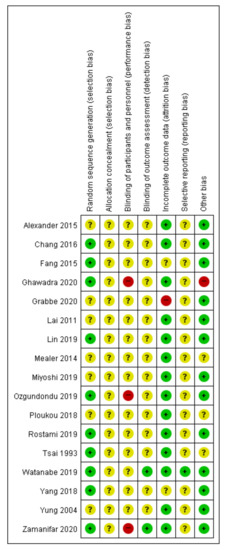
Figure 2.
Risk of bias summary for all included studies. Low, unclear, and high risk, respectively, are represented with the following symbols: “+”, “?”, and “–”.
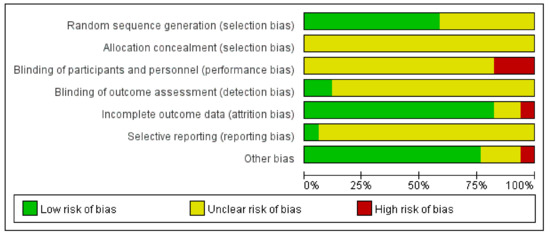
Figure 3.
Risk of bias graph for all included studies.
3.4. Main Results
3.4.1. Primary Outcome (Burnout)
(1) MBIs: Two studies using a multimodal resilience program including mindfulness training were compared with no intervention or nutrition/healthy eating group. In the former [45], no statistical comparison was performed between groups using the Maslach Burnout Inventory, and in the latter [57], no statistically significant difference was found between the two groups in the Copenhagen Burnout Inventory (p = 0.777). Watanabe (2019) found that there was no significant difference between the brief mindfulness-based stress management program group and the psychoeducation group in any subscale of the Maslach Burnout Inventory (p = 0.266 to 0.664) [55] (Table 2).

Table 2.
Main results of included studies.
(2) Yoga: Alexander (2015) reported that yoga had a statistically superior improvement in emotional exhaustion (p = 0.041) and depersonalization (p = 0.035), but not in the lack of personal accomplishment (p = 0.554), among the Maslach Burnout Inventory compared to usual care [46] (Table 2).
3.4.2. Secondary Outcomes
Except for the case of not performing a statistical comparison between the two groups, it is as follows:
(1) MBIs: Regarding the outcomes of occupation and environment, compared to no intervention, Ghawadra (2020) [56] found that MBIs significantly improved job satisfaction as assessed by the Job Satisfaction Scale (p = 0.040) compared to no intervention, while Lin (2019) [51] found that MBSR did not significantly improve job satisfaction as assessed by the McCloskey/Mueller Satisfaction Scale (p > 0.05). Additionally, according to Watanabe (2019) [55], there was no significant difference in absolute presenteeism (p = 0.258) and relative presenteeism (p = 0.065) in the World Health Organization Health and Work Performance Questionnaire between MBIs and psychoeducation groups. Regarding the outcomes of the individual’s resistance to stress, Lin (2019) [51] found that MBIs did not significantly improve resilience assessed by the Connor–Davidson Resilience Scale (CDRS) (p > 0.05) compared to no intervention, and Grabbe (2020) [57] reported that there was no significant difference in CDRS (p = 0.910), between multimodal intervention including mindful eating group and nutrition/healthy eating group. Chang (2016) [48] found that, compared to no intervention, meditation significantly improved the sense of power assessed by Power as Knowing Participation in Change Tool (p = 0.001 to 0.049 according to the subscale). According to Ghawadra (2020) [56], there was no significant difference in absolute mindfulness assessed by the Mindful Attention Awareness Scale (p = 0.967) between the MBI and no intervention groups. Regarding the outcomes of the individual’s global health and wellness, Chang (2016) [48] found that, compared to no intervention, meditation significantly improved global score and most subscales of quality of life assessed using the abbreviated World Health Organization Quality of Life (WHOQOL-BREF) questionnaire (p = 0.006 to 0.039 for global score, physical domain, psychological domain, and social domain; p = 0.057 for environmental domain), while Watanabe (2019) [55] found no significant difference in quality of life assessed by the EuroQol five-dimension scale utility score between the MBIs group and the psychoeducation group (p = 0.131). Grabbe (2020) [57] found that there was no significant difference in well-being assessed by the five-item World Health Organization Well-Being Index (p = 0.168), between the multimodal intervention including mindful eating group and nutrition/healthy eating group. Regarding the outcomes of psychological symptoms, Yang (2018) [50] found that MBSR significantly improved psychological pathology assessed by the Symptom Checklist-90-Revised (p < 0.001), stress level assessed by the Nursing Stress Scale (p < 0.001), anxiety level assessed by Self-Rating Anxiety Scale (p < 0.001), and depression level assessed using the Self-Rating Depression Scale (p < 0.001), compared to routine psychological support and activities. Lin (2019) [51] also found that MBSR significantly improved stress levels assessed by the Perceived Stress Scale (PSS) (p < 0.01) and positive and negative emotions assessed by the Positive and Negative Affect Schedule (p < 0.01 to 0.05, according to the subscale). However, in Grabbe’s study (2020) [57], there was no significant difference in posttraumatic stress assessed by the secondary traumatic stress scale (p = 0.846) between the multimodal intervention including mindful eating and in the nutrition/healthy eating groups. Moreover, Watanabe (2019) [55] found that there was no significant difference in depression (p = 0.192) and anxiety (p = 0.190) assessed by the Hospital Anxiety and Depression Scale (HADS), anxiety assessed by the Generalized Anxiety Disorder seven-Item Scale (p = 0.057), depression assessed by the Patient Health Questionnaire-9 (p = 0.315), and insomnia assessed using the Insomnia Severity Index (ISI) (p = 0.435), between the MBIs and psychoeducation groups. In the case of Ghawadra (2020) [56], the MBI group showed significantly improved scores for anxiety (p = 0.008), but not for stress (p = 0.159) and depression (p = 0.709) in the Depression, Anxiety, and Stress Scales-21, compared to the no-intervention group. Regarding the outcomes of somatic symptoms, Grabbe (2020) [57] reported that there was no significant difference in somatic symptoms assessed using the Somatic Symptoms Scale-8 (p = 0.563), between the multimodal intervention including mindful eating group and nutrition/healthy eating group (Table 2).
(2) Relaxation: Regarding outcomes on the individual’s resistance to stress, according to Ozgundondu (2019) [53], progressive muscle relaxation (PMR) group showed significantly improved score of acceptance (p = 0.038), but not of use of instrumental support (p = 0.980), humor (p = 0.425), active coping (p = 0.237), substance use (p = 0.631), venting (p = 0.235), religion (p = 0.108), denial (p = 0.302), behavioral disengagement (p = 0.413), self-distraction (p = 0.224), self-blame (p = 0.758), positive reframing (p = 0.295), use of emotional support (p = 0.101), and planning (p = 0.160), in the abbreviated version of the Coping Orientation to Problems Experienced Inventory, compared to the education group. Regarding the outcomes of an individual’s global health and wellness, Tsai (1993) [42] reported that relaxation significantly improved general health as assessed by the General Health Questionnaire (GHQ) (p < 0.05), compared to traditional in-service education. However, in Yung’s study (2004) [43], there was no significant difference in GHQ between the stretch-release relaxation group, the cognitive relaxation group, and the no-intervention group (p = 0.320). Regarding the outcomes of psychological symptoms, Tsai (1993) [42] reported that relaxation significantly improved stress levels assessed by the Nurse Stress Checklist (p < 0.05), compared to a traditional in-service education. In addition, Ozgundondu (2019) [53] reported that the PMR group showed significantly better results on PSS (p = 0.030) than the education group. However, in Yung’s study (2004) [43], there was no significant difference in anxiety state (p = 0.097) and anxiety trait (p = 0.679) in the Stat-Trait Anxiety Inventory, between the stretch-release relaxation group, the cognitive relaxation group, and the no-intervention group.
Regarding the outcomes of somatic symptoms, Ozgundondu (2019) [53] found that PMR significantly improved fatigue levels assessed by the Fatigue Severity Scale (p < 0.001), compared to education (Table 2).
(3) Yoga: Regarding the outcomes of the individual’s resistance to stress, Alexander (2015) [46] found that the yoga group showed significantly better results on healthy lifestyle assessed by Health Promoting Lifestyle Profile II (p = 0.006), but not on the mindfulness level assessed by the Freiburg Mindfulness Inventory (p = 0.067), compared to usual care. Regarding the outcomes of individual’s global health and wellness, Rostami (2019) [54] found that all subscales in the WHOQOL-BREF, including global score and physical, psychological, social, and environmental domains (all, p < 0.001) were significantly better in the yoga group than in the no-intervention group. Regarding the outcomes of psychological symptoms, Miyoshi (2019) [52] found that the yoga group showed significantly better results on stress level assessed by the Brief Job Stress Questionnaire (p = 0.01), compared to the stress relief method group. Fang (2015) [47] found that the yoga group showed a significantly lower number of scores more than 32 (which means high stress level) (p = 0.001) on the Questionnaire on Medical Workers’ Stress, compared to the no-intervention group (Table 2).
(4) Music: Regarding the outcomes of psychological symptoms, Lai (2011) [44] found that music significantly improved stress levels assessed by self-perceived stress (p < 0.001), compared to chair rest. However, in Ploukou’s study (2018) [49], there was no significant difference in depression scores in the HADS (p > 0.05) between the percussion music group and the no-intervention group. In Zamanifar’s study (2020) [58], the music therapy group (p = 0.0001), the aromatherapy group (p = 0.0001), and the music therapy combined with aromatherapy group (p = 0.0001) showed significantly lower Beck Anxiety Inventory scores than the no-intervention group. Regarding the outcomes of somatic symptoms, Ploukou (2018) [49] did not find significant differences in psychosomatic symptoms assessed by the Pennebaker Inventory of Limbic Languidness (p > 0.05), between the percussion music group and the no-intervention group. Regarding the outcomes on biological data, Lai (2011) [44] found that the music group showed significantly less mean arterial blood pressure (BP) (p < 0.001), serum cortisol (p < 0.025), and heart rate (HR) (p < 0.001), and significantly higher finger temperature (p < 0.001), compared to the chair rest group (Table 2).
3.4.3. Safety Data
Only three studies reported safety data [52,53,55], and no adverse events occurred in these studies.
4. Discussion
4.1. Main Findings
This review aimed to comprehensively analyze the effectiveness and safety of mind-body modalities on burnout and other mental health aspects of nurses in hospital settings. A total of 17 RCTs were included, and the mind-body modalities used were classified into MBIs, relaxation, yoga, and music according to their characteristics.
Data on MBIs and yoga were available for burnout, and there was no evidence that multimodal resilience programs including MBSR or mindful eating and MBIs statistically significantly improved burnout levels compared to the no-intervention group or active control groups. However, one study [46] reported that yoga could significantly improve emotional exhaustion and depersonalization, which are subscales of burnout, compared to usual care.
The effects of MBIs, relaxation, yoga, and music on several secondary outcomes, including the primary outcome, can be summarized as follow. In the case of MBIs, studies have reported that MBIs showed significant benefits on the sense of power, psychological pathology, positive and negative emotions, but showed non-significant effects on presenteeism, resilience, mindfulness, well-being, posttraumatic stress, insomnia, and somatic symptoms, compared to control groups. Mixed results have been reported for job satisfaction, quality of life, stress, anxiety, and depression. In the case of relaxation, studies have reported that relaxation has significant benefits on coping style, stress, and fatigue, but a non-significant effect on anxiety, compared to control groups. Mixed results have been reported for general health. In the case of yoga, studies have reported that it showed significant benefits on healthy lifestyle, quality of life, and stress, but a non-significant effect on mindfulness, compared to control groups. In the case of music, studies have reported that it showed significant benefits on stress, anxiety, and some biological data, including mean arterial BP, serum cortisol, HR, and finger temperature, but non-significant effects on depression and somatic symptoms, compared to control groups, although it was the immediate result of one session in the study. Overall, stress could be positively affected by most mind-body modalities. However, the methodological quality of the included studies was not optimal. This means that the certainty of the findings of this review is not high, suggesting that our findings may change depending on the results of future high-quality and large-scale studies.
4.2. Clinical Implications
The mental health of nurses is both individually and socially an important issue [3]. Mind-body modalities are promising for managing a variety of physical and psychiatric symptoms, including anxiety, depression, perceived stress, coronary artery disease, headaches, insomnia, incontinence, chronic lower back pain, and even cancer symptoms [4]. In this review, we examined the potential applications of several mind-body modalities in terms of improving the mental health of nurses. In particular, in this review, the authors conducted a comprehensive study search and data analysis to establish clinical evidence for reliable data of mind-body modalities from the perspective of EBM. However, the findings were limited by the consequent lack of the number of included studies and the lack of methodological quality of the included studies. Although mind-body modalities may have beneficial impacts on improving mental health, mental health outcomes in this population vary widely, and the mind-body modalities used in the studies included in this review also varied. Meanwhile, studies evaluating the effectiveness of the potentially most effective mind-body modalities as well as the most treatment-sensitive outcomes may have clinical significance. In that sense, this review provides comprehensive evidence on this topic by performing a comprehensive analysis of the available studies. However, this review also points out that there are still many areas that have not been studied, such as the heterogeneity of different interventions or outcomes.
4.3. Limitations and Suggestions for Further Studies
This review presents results of the most comprehensive systematic review available on mind-body modalities for burnout as well as other mental health aspects of nurses. The use of various mind-body modalities as well as various mental-health-related outcomes has been identified for this issue, and its heterogeneity is also highlighted in this review. The following limitations should be considered when interpreting this study.
First, the number of studies included in this review was small, and the interventions and outcomes used were also varied. As a result, the results for each outcome depended on the results from one to three studies in general, and the evidence supported by the small number of studies with small sample sizes cannot be evaluated as having sufficient reliability. Therefore, further research on this topic is required. Second, the overall methodological quality of the included studies was poor. In particular, there was ambiguity regarding the blinding procedure in most included studies, potentially suggesting that the results reported in these studies may have been overestimated or influenced by the placebo effect. Therefore, it is necessary to conduct a high-quality clinical trial with proper blinding procedures in relation to this topic in the future. Third, in this review, we categorized mind-body modalities into four categories, but the details may vary for each mind-body modality. For example, one three-arm study [43] used both stretch-release relaxation and cognitive relaxation, which were both considered as relaxations by us. In addition, even with the same MBSR, in a standardized mindfulness program, there are some modifications depending on the characteristics of the participants or the environment. That is, the classification of this review does not sufficiently guarantee the homogeneity of the individual interventions analyzed. In future studies, based on the findings of this review, it may be possible to specify population, intervention, comparator, and outcomes by focusing on mental health-related outcomes where specific mind-body modalities can have positive effects. Fourth, the reported outcomes in the included studies were too diverse to be meta-analyzed. Unlike the clear primary outcome for patients with certain mental disorders, nurses are a non-clinical population, and it is thought that this is so because there is no gold standard primary outcome for nursing mental health. However, some outcomes such as job-related stress, job satisfaction, burnout, and the occurrence of medical errors may be unique and relevant in this population. Fifth, data on biology among the outcomes reported in the included studies were lacking, although one study [44] reported the effects of music on biomarkers including BP, serum cortisol, HR, and finger temperature. Reporting effects on these biomarkers, as well as participant self-reports, are necessary to objectively evaluate the effectiveness of the interventions studied. Currently, considerable research is being conducted on biomarkers related to mental health, including genetics, transcriptomics, proteomics, metabolomics, and epigenetics [59]. Therefore, evaluation of these mental-health-related biomarkers should be introduced in the future. Finally, because quantitative synthesis was not performed due to the heterogeneity between the studies included in this review, an evaluation of publication bias through funnel plot generation was not possible [60], but this does not prove the absence of publication bias. That is, the possibility of publication bias suggests that unpublished studies in this field may have exaggerated the net benefit of the intervention [61]. Therefore, the findings of this review should be interpreted with caution.
5. Conclusions
This review is the most comprehensive one available on the impact of mind-body modalities on burnout as well as other mental health aspects of nurses in hospital settings. For burnout, which was the primary outcome, there was some evidence that yoga was helpful for improvement. In addition, the outcome that reported improved results in all mind-body modalities, including MBIs, relaxation, yoga, and music, was perceived stress. However, due to the heterogeneity of interventions and outcomes, and the methodological limitations of the studies included, further high-quality clinical trials are needed on this topic in the future.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/ijerph18168855/s1, Table S1: Supplementary Digital Content 1. PRISMA 2020 checklists, Table S2: Supplementary Digital Content 2. Search strategies used in each database.
Author Contributions
Conceptualization, C.-Y.K.; methodology, S.-E.J., D.-J.H., J.-H.P., B.L. and C.-Y.K.; software, S.-E.J., D.-J.H., J.-H.P., B.L. and C.-Y.K.; validation, B.L. and C.-Y.K.; formal analysis, C.-Y.K.; writing—original draft preparation, S.-E.J., D.-J.H. and C.-Y.K.; writing—review and editing, B.L., M.-S.K., K.-L.S., Y.-H.C. and C.-Y.K.; supervision, C.-Y.K.; project administration, C.-Y.K.; funding acquisition, C.-Y.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by the MSIT (Ministry of Science and ICT), Korea, under the Grand Information Technology Research Center support program (IITP-2020-0-01791) supervised by the IITP (Institute for Information & communications Technology Planning & Evaluation).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
These data used to support the findings of this study are included within the article.
Conflicts of Interest
The authors have no conflict of interest to declare.
References
- Vasconcelos, S.C.; De Souza, S.L.; Sougey, E.B.; Ribeiro, E.C.D.O.; Nascimento, J.J.C.D.; Formiga, M.B.; Ventura, L.B.D.S.; Lima, M.D.D.C.; Silva, A.O. Nursing Staff Members Mental’s Health and Factors Associated with the Work Process: An Integrative Review. Clin. Pract. Epidemiology Ment. Health 2016, 12, 167–176. [Google Scholar] [CrossRef] [Green Version]
- Monsalve-Reyes, C.S.; Luis-Costas, C.S.; Gómez-Urquiza, J.L.; Albendín-García, L.; Aguayo, R.; La Fuente, G.A.C.-D. Burnout syndrome and its prevalence in primary care nursing: A systematic review and meta-analysis. BMC Fam. Pract. 2018, 19, 59. [Google Scholar] [CrossRef] [Green Version]
- Parker, P.A.; Kulik, J.A. Burnout, self- and supervisor-rated job performance, and absenteeism among nurses. J. Behav. Med. 1995, 18, 581–599. [Google Scholar] [CrossRef]
- Brower, V. Mind-body research moves towards the mainstream. EMBO Rep. 2006, 7, 358–361. [Google Scholar] [CrossRef]
- Younge, O.J.; Gotink, R.; Baena, C.P.; Roos-Hesselink, J.W.; Hunink, M.G.M. Mind-body practices for patients with cardiac disease: A systematic review and meta-analysis. Eur. J. Prev. Cardiol. 2015, 22, 1385–1398. [Google Scholar] [CrossRef]
- Senders, A.; Wahbeh, H.; Spain, R.; Shinto, L. Mind-Body Medicine for Multiple Sclerosis: A Systematic Review. Autoimmune Dis. 2012, 2012, 567324. [Google Scholar] [CrossRef] [Green Version]
- Theadom, A.; Cropley, M.; Smith, E.H.; Feigin, V.L.; Mc Pherson, K. Mind and body therapy for fibromyalgia. Cochrane Database Syst. Rev. 2015, 4, CD001980. [Google Scholar] [CrossRef]
- Lee, M.C.; Crawford, P.; Hickey, A. Active Self-Care Therapies for Pain (PACT) Working Group Mind-body Therapies for the Self-Management of Chronic Pain Symptoms. Pain Med. 2014, 15, S21–S39. [Google Scholar] [CrossRef] [Green Version]
- Wells, R.E.; Phillips, R.S.; McCarthy, E.P. Patterns of Mind-Body Therapies in Adults with Common Neurological Conditions. Neuroepidemiology 2011, 36, 46–51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bower, J.E.; Irwin, M.R. Mind-body therapies and control of inflammatory biology: A descriptive review. Brain Behav. Immun. 2016, 51, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sanada, K.; Montero-Marin, J.; Barceló-Soler, A.; Ikuse, D.; Ota, M.; Hirata, A.; Yoshizawa, A.; Hatanaka, R.; Valero, M.S.; DeMarzo, M.; et al. Effects of Mindfulness-Based Interventions on Biomarkers and Low-Grade Inflammation in Patients with Psychiatric Disorders: A Meta-Analytic Review. Int. J. Mol. Sci. 2020, 21, 2484. [Google Scholar] [CrossRef] [Green Version]
- Cahn, B.R.; Goodman, M.S.; Peterson, C.T.; Maturi, R.; Mills, P.J. Yoga, Meditation and Mind-Body Health: Increased BDNF, Cortisol Awakening Response, and Altered Inflammatory Marker Expression after a 3-Month Yoga and Meditation Retreat. Front. Hum. Neurosci. 2017, 11, 315. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- MacLaughlin, B.W.; Wang, D.; Noone, A.-M.; Liu, N.; Harazduk, N.; Lumpkin, M.; Haramati, A.; Saunders, P.; Dutton, M.; Amri, H. Stress Biomarkers in Medical Students Participating in a Mind Body Medicine Skills Program. Evid. Based Complement. Altern. Med. 2011, 2011, 950461. [Google Scholar] [CrossRef] [Green Version]
- Penque, S. Mindfulness to promote nurses’ well-being. Nurs. Manag. (Springhouse) 2019, 50, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Søvold, L.E.; Naslund, J.A.; Kousoulis, A.A.; Saxena, S.; Qoronfleh, M.W.; Grobler, C.; Münter, L. Prioritizing the Mental Health and Well-Being of Healthcare Workers: An Urgent Global Public Health Priority. Front. Public Health 2021, 9, 679397. [Google Scholar] [CrossRef]
- Callus, E.; Bassola, B.; Fiolo, V.; Bertoldo, E.G.; Pagliuca, S.; Lusignani, M. Stress Reduction Techniques for Health Care Providers Dealing With Severe Coronavirus Infections (SARS, MERS, and COVID-19): A Rapid Review. Front. Psychol. 2020, 11, 589698. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, A.E.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef]
- Maslach, C.; Jackson, S.E.; Leiter, M.P.; Schaufeli, W.B.; Schwab, R.L. Maslach Burnout Inventory; Consulting psychologists press Palo Alto: Palo Alto, CA, USA, 1986; Volume 21. [Google Scholar]
- Higgins, J.; Altman, D.; Sterne, C. Chapter 8; Assessing the risk of bias in included studies. From the Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 [updated 2011]. The Cochrane Collaboration. 2011. Available online: https://handbook-5-1.cochrane.org/ (accessed on 18 March 2021).
- Foureur, M.; Besley, K.; Burton, G.; Yu, N.; Crisp, J. Enhancing the resilience of nurses and midwives: Pilot of a mindfulnessbased program for increased health, sense of coherence and decreased depression, anxiety and stress. Contemp. Nurse 2013, 45, 114–125. [Google Scholar] [CrossRef]
- Gauthier, T.; Meyer, R.; Grefe, D.; Gold, J. An On-the-Job Mindfulness-Based Intervention for Pediatric ICU Nurses: A Pilot Study. J. Altern. Complement. Med. 2014, 20, A87. [Google Scholar] [CrossRef]
- Watanabe, N.; Furukawa, A.T.; Horikoshi, M.; Katsuki, F.; Narisawa, T.; Kumachi, M.; Oe, Y.; Shinmei, I.; Noguchi, H.; Hamazaki, K.; et al. A mindfulness-based stress management program and treatment with omega-3 fatty acids to maintain a healthy mental state in hospital nurses (Happy Nurse Project): Study protocol for a randomized controlled trial. Trials 2015, 16, 36. [Google Scholar] [CrossRef] [Green Version]
- Kim, Y.A.; Park, J.S. Development and Application of an Overcoming Compassion Fatigue Program for Emergency Nurses. J. Korean Acad. Nurs. 2016, 46, 260–270. [Google Scholar] [CrossRef] [Green Version]
- Calisi, C.C. The Effects of the Relaxation Response on Nurses’ Level of Anxiety, Depression, Well-Being, Work-Related Stress, and Confidence to Teach Patients. J. Holist. Nurs. 2017, 35, 318–327. [Google Scholar] [CrossRef]
- Halm, M. The Role of Mindfulness in Enhancing Self-Care for Nurses. Am. J. Crit. Care 2017, 26, 344–348. [Google Scholar] [CrossRef]
- Daigle, S.; Talbot, F.; French, D.J. Mindfulness-based stress reduction training yields improvements in well-being and rates of perceived nursing errors among hospital nurses. J. Adv. Nurs. 2018, 74, 2427–2430. [Google Scholar] [CrossRef]
- Pan, C.; Wang, H.; Chen, M.; Cai, Y.; Xiao, C.; Tang, Q.; Koniak-Griffin, D. Mindfulness-Based Intervention For Nurses In AIDS Care In China: A Pilot Study. Neuropsychiatr. Dis. Treat. 2019, 15, 3131–3141. [Google Scholar] [CrossRef] [Green Version]
- Torres, L.-A.P.-D.; Atalaya, J.C.V.-M.; García-Campayo, J.; Roldán-Villalobos, A.; Magallón-Botaya, R.; Bartolomé-Moreno, C.; Moreno-Martos, H.; Melús-Palazón, E.; Liétor-Villajos, N.; Valverde-Bolívar, F.J.; et al. Controlled clinical trial comparing the effectiveness of a mindfulness and self-compassion 4-session programme versus an 8-session programme to reduce work stress and burnout in family and community medicine physicians and nurses: MINDUUDD study protocol. BMC Fam. Pract. 2019, 20, 24. [Google Scholar] [CrossRef]
- Yong, J.; Park, J.; Park, Y.; Lee, H.; Lee, G.; Rim, S. Effects of Holy Name Meditation on the Quality of Life of Hospital Middle Manager Nurses in Korea: A 6-Month Follow-Up. J. Contin. Educ. Nurs. 2020, 51, 215–224. [Google Scholar] [CrossRef] [PubMed]
- Maguire, P. The Effect of Coloring Mandalas on the Anxiety of Medical-Surgical Nurses and Nursing Support Staff. MEDSURG Nurs. 2020, 29, 192–199. [Google Scholar]
- Owens, R.A.; Alfes, C.; Evans, S.; Wyka, K.; Fitzpatrick, J.J. An Exploratory Study of a 3-Minute Mindfulness Intervention on Compassion Fatigue in Nurses. Holist. Nurs. Pract. 2020, 34, 274–281. [Google Scholar] [CrossRef] [PubMed]
- Xie, C.; Zeng, Y.; Lv, Y.; Li, X.; Xiao, J.; Hu, X. Educational intervention versus mindfulness-based intervention for ICU nurses with occupational burnout: A parallel, controlled trial. Complement. Ther. Med. 2020, 52, 102485. [Google Scholar] [CrossRef] [PubMed]
- McElligott, D.; Holz, M.B.; Carollo, L.; Somerville, S.; Baggett, M.; Kuzniewski, S.; Shi, Q. A pilot feasibility study of the effects of touch therapy on nurses. J. N. Y. State Nurses’ Assoc. 2003, 34, 16–24. [Google Scholar]
- Bost, N.; Wallis, M. The effectiveness of a 15 minute weekly massage in reducing physical and psychological stress in nurses. Aust. J. Adv. Nurs. Q. Publ. R. Aust. Nurs. Fed. 2006, 23, 28–33. [Google Scholar]
- El Khamali, R.; Mouaci, A.; Valera, S.; Cano-Chervel, M.; Pinglis, C.; Sanz, C.; Allal, A.; Attard, V.; Malardier, J.; Delfino, M.; et al. Effects of a Multimodal Program Including Simulation on Job Strain Among Nurses Working in Intensive Care Units. JAMA 2018, 320, 1988–1997. [Google Scholar] [CrossRef]
- Wlazelek, B.G. The Effects of Stress Inoculation for Anger Control and Relaxation Training on Anger and Related Measures with Nurses. Ph.D. Thesis, Lehigh University, Bethlehem, PA, USA, 1990. [Google Scholar]
- Rad, Z.Z.; Shafiabadi, A.; ZareBahramAbadi, M.; Moghaddam, L.F. The Use of Mindfulness-based Cognitive Therapy for Improving Flow Experience of Nurses in the Psychiatric Hospitals. Eur. Psychiatry 2015, 30, 1037. [Google Scholar] [CrossRef]
- Smith, O.; Faulkner, K.; Skiffington, A.; McShane, J.; Wan, C.; Krock, M. A randomized controlled trial of an intervention to enhance resilience in acute care nurses (ARISE). Crit. Care Med. 2019, 47, 35. [Google Scholar] [CrossRef]
- Watanabe, N. Brief mindfulness-based stress management program for a better mental state in working populations-happy nurse project: A randomized controlled trials. Psychosomat. Med. 2019, 81, A136. [Google Scholar] [CrossRef] [PubMed]
- Tsai, S. The Effects of Relaxation Training, Combining Meditation and Guided Imagery, on Self-Perceived Stress among Chinese Nurses in Large Teaching Hospitals in Taiwan, China. Ph.D. Thesis, University of Texas at Austin, Austin, TX, USA, 1992. [Google Scholar]
- Mealer, M.; Conrad, D.; Evans, J.; Jooste, K.; Rothbaum, B.; Moss, M. A 12-week multimodal resilience training program for intensive care unit nurses: Results of a pilot study. Am. J. Respir. Crit. Care Med. 2014, 189, A5217–A5247. [Google Scholar]
- Tsai, S.-L.; Crockett, M.S. Effects of Relaxation Training, Combining Imagery, and Meditation the Stress Level of Chinese Nurses Working in Modern Hospitals in Taiwan. Issues Ment. Health Nurs. 1993, 14, 51–66. [Google Scholar] [CrossRef]
- Yung, P.M.B.; Fung, M.Y.; Chan, T.M.F.; Lau, B.W.K. Relaxation training methods for nurse managers in Hong Kong: A controlled study. Int. J. Ment. Health Nurs. 2004, 13, 255–261. [Google Scholar] [CrossRef]
- Lai, H.-L.; Li, Y.-M. The effect of music on biochemical markers and self-perceived stress among first-line nurses: A randomized controlled crossover trial. J. Adv. Nurs. 2011, 67, 2414–2424. [Google Scholar] [CrossRef]
- Mealer, M.; Conrad, D.; Evans, J.; Jooste, K.; Solyntjes, J.; Rothbaum, B.; Moss, M. Feasibility and Acceptability of a Resilience Training Program for Intensive Care Unit Nurses. Am. J. Crit. Care 2014, 23, e97–e105. [Google Scholar] [CrossRef]
- Alexander, G.K.; Rollins, K.; Walker, D.; Wong, L.; Pennings, J. Yoga for Self-Care and Burnout Prevention Among Nurses. Work. Health Saf. 2015, 63, 462–470. [Google Scholar] [CrossRef]
- Fang, R.; Li, X. A regular yoga intervention for staff nurse sleep quality and work stress: A randomised controlled trial. J. Clin. Nurs. 2015, 24, 3374–3379. [Google Scholar] [CrossRef]
- Chang, S.J.; Kwak, E.Y.; Hahm, B.-J.; Seo, S.H.; Lee, D.W.; Jang, S.J. Effects of a Meditation Program on Nurses’ Power and Quality of Life. Nurs. Sci. Q. 2016, 29, 227–234. [Google Scholar] [CrossRef]
- Ploukou, S.; Panagopoulou, E. Playing music improves well-being of oncology nurses. Appl. Nurs. Res. 2018, 39, 77–80. [Google Scholar] [CrossRef]
- Yang, J.; Tang, S.; Zhou, W. Effect of mindfulness-based stress reduction therapy on work stress and mental health of psychiatric nurses. Psychiatr. Danub. 2018, 30, 189–196. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.; He, G.; Yan, J.; Gu, C.; Xie, J. The Effects of a Modified Mindfulness-Based Stress Reduction Program for Nurses: A Randomized Controlled Trial. Work. Health Saf. 2018, 67, 111–122. [Google Scholar] [CrossRef] [PubMed]
- Miyoshi, Y. Restorative yoga for occupational stress among Japanese female nurses working night shift: Randomized crossover trial. J. Occup. Health 2019, 61, 508–516. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ozgundondu, B.; Metin, Z.G. Effects of progressive muscle relaxation combined with music on stress, fatigue, and coping styles among intensive care nurses. Intensiv. Crit. Care Nurs. 2019, 54, 54–63. [Google Scholar] [CrossRef]
- Rostami, K.; Ghodsbin, F. Effect of Yoga on the Quality of Life of Nurses Working in Intensive Care Units. Randomized Controlled Clinical Trial. Investig. Educ. Enferm. 2019, 37. [Google Scholar] [CrossRef] [Green Version]
- Watanabe, N.; Horikoshi, M.; Shinmei, I.; Oe, Y.; Narisawa, T.; Kumachi, M.; Matsuoka, Y.; Hamazaki, K.; Furukawa, T.A. Brief mindfulness-based stress management program for a better mental state in working populations—Happy Nurse Project: A randomized controlled trial✰✰. J. Affect. Disord. 2019, 251, 186–194. [Google Scholar] [CrossRef]
- Ghawadra, S.F.; Abdullah, K.L.; Choo, W.Y.; Danaee, M.; Phang, C.K. The effect of mindfulness-based training on stress, anxiety, depression and job satisfaction among ward nurses: A randomized control trial. J. Nurs. Manag. 2020, 28, 1088–1097. [Google Scholar] [CrossRef]
- Grabbe, L.; Higgins, M.K.; Baird, M.; Craven, P.A.; Fratello, S.S. The Community Resiliency Model® to promote nurse well-being. Nurs. Outlook 2020, 68, 324–336. [Google Scholar] [CrossRef] [PubMed]
- Zamanifar, S.; Bagheri-Saveh, M.I.; Nezakati, A.; Mohammadi, R.; Seidi, J. The Effect of Music Therapy and Aromatherapy with Chamomile-Lavender Essential Oil on the Anxiety of Clinical Nurses: A Randomized and Double-Blind Clinical Trial. J. Med. Life 2020, 13, 87–93. [Google Scholar] [PubMed]
- García-Gutiérrez, M.S.; Navarrete, F.; Sala, F.; Gasparyan, A.; Austrich-Olivares, A.; Manzanares, J. Biomarkers in Psychiatry: Concept, Definition, Types and Relevance to the Clinical Reality. Front. Psychiatry 2020, 11, 432. [Google Scholar] [CrossRef]
- Parekh-Bhurke, S.; Kwok, C.S.; Pang, C.L.; Hooper, L.; Loke, Y.K.; Ryder, J.J.; Sutton, A.J.; Hing, C.; Harvey, I.; Song, F. Uptake of methods to deal with publication bias in systematic reviews has increased over time, but there is still much scope for improvement. J. Clin. Epidemiol. 2011, 64, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Murad, M.H.; Chu, H.; Lin, L.; Wang, Z. The effect of publication bias magnitude and direction on the certainty in evidence. BMJ Evid. Based Med. 2018, 23, 84–86. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).