The Effectiveness of Educational Interventions on Breast Cancer Screening Uptake, Knowledge, and Beliefs among Women: A Systematic Review
Abstract
1. Introduction
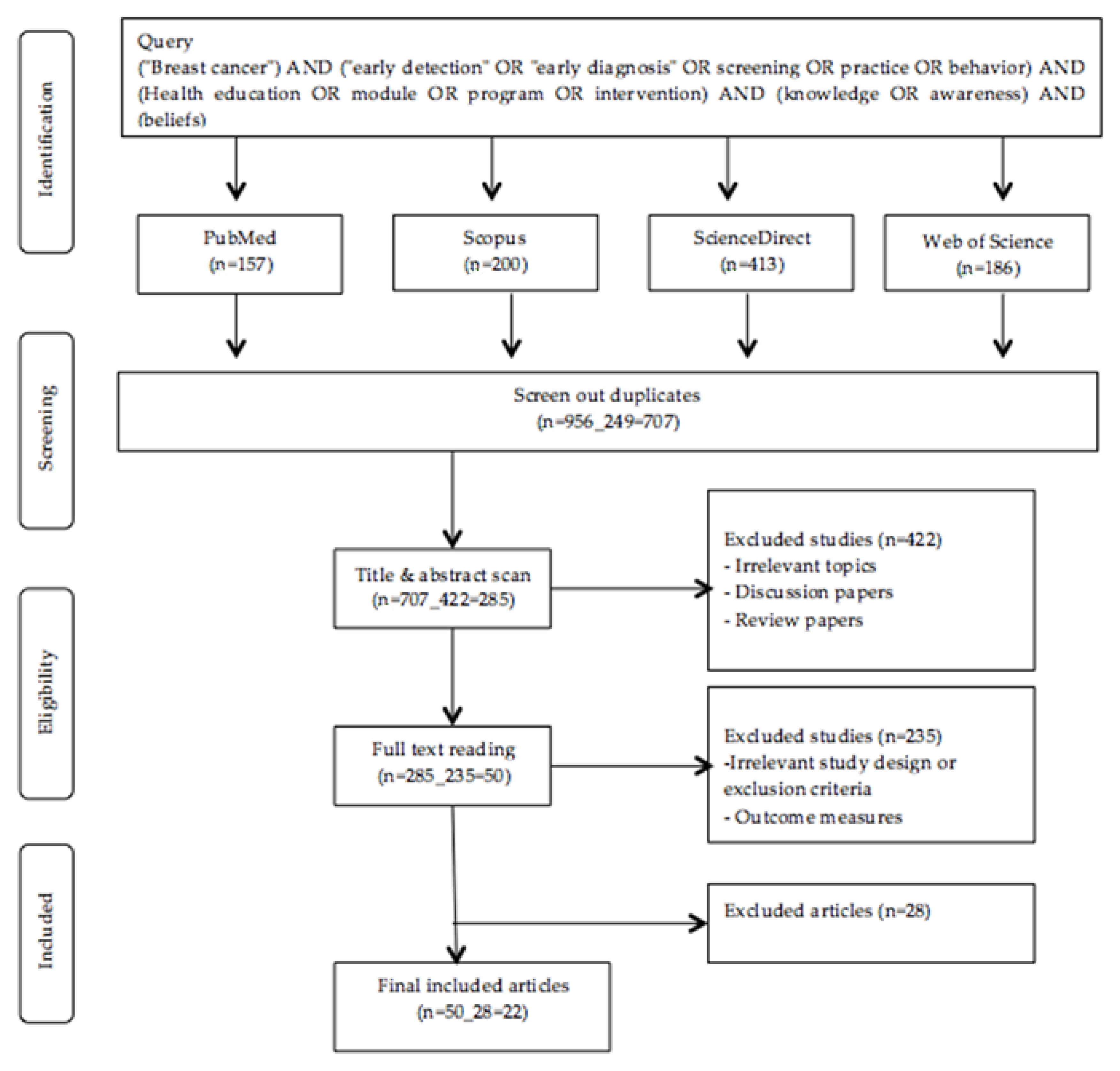
2. Materials and Methods
2.1. Literature Search
2.2. Data Synthesis
3. Results
3.1. Characteristics of Study
3.1.1. Participants and Setting
3.1.2. Conceptual Framework
3.1.3. Intervention Strategies
4. Outcome Measures and Study Results
4.1. Breast Cancer Screening Uptake
4.2. Knowledge of Breast Cancer and Breast Cancer Screening
4.3. Health beliefs of Breast Cancer and Breast Cancer Screening
5. Discussion
6. Conclusions
7. Recommendations
Supplementary Materials
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bray, F.; Ferly, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global Cancer Statistics 2018: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef]
- Torre, L.A.; Islami, F.; Siegel, R.L.; Ward, E.M.; Jemal, A. Global Cancer in Women: Burden and Trends. Cancer Epidemiol. 2017, 26, 444–457. [Google Scholar] [CrossRef]
- Youlden, D.R.; Cramb, S.M.; Yip, C.H.; Baade, P.D. Incidence and Mortality of Female Breast Cancer in the Asia-Pacific Region. Cancer Biol. Med. 2014, 11, 101–115. [Google Scholar]
- Breast Cancer Facts & Figures 2015–2016; American Cancer Society, Inc.: Atlanta, GA, USA, 2015.
- Siegel, R.; Miller, K.; Jemal, A. Cancer Statistics 2018. CA Cancer J. Clin. 2018, 68, 7–30. [Google Scholar] [CrossRef]
- World Health Organization. Breast Cancer. Available online: https://www.who.int/cancer/prevention/diagnosis-screening/breast-cancer/en/ (accessed on 29 December 2018).
- Smith, R.A.; Andrews, K.S.; Brooks, D.; Fedewa, S.A.; Manassaram-Baptiste, D.; Saslow, D. Cancer Screening in the United States, 2018: A Review of Current American Cancer Society Guidelines and Current Issues in Cancer Screening. CA Cancer J. Clin. 2018, 68, 297–316. [Google Scholar] [CrossRef] [PubMed]
- Al-Sakkaf, K.A.; Basaleem, H.O. Breast Cancer Knowledge, Perception and Breast Self- Examination Practices among Yemeni Women: An Application of the Health Belief Model. Asian Pac. J. Cancer Prev. 2016, 17, 1463–1467. [Google Scholar] [CrossRef] [PubMed]
- Freund, A.; Cohen, M.; Azaiza, F. A Culturally Tailored Intervention for Promoting Breast Cancer Screening among Women from Faith-Based Communities in Israel: A Randomized Controlled Study. Res. Soc. Work Pract. 2017, 29, 375–388. [Google Scholar] [CrossRef]
- Tuzcu, A.; Bahar, Z.; Gözüm, S. Effects of Interventions Based on Health Behavior Models on Breast Cancer Screening Behaviors of Migrant Women in Turkey. Cancer Nurs. 2016, 39, 40–50. [Google Scholar] [CrossRef]
- Yılmaz, M.; Sayın, Y.; Cengiz, H.Ö. The Effects of Training on Knowledge and Beliefs about Breast Cancer and Early Diagnosis Methods among Women. Eur. J. Breast Health 2017, 13, 175–182. [Google Scholar] [CrossRef]
- Ahmed, B.A. Awareness and Practice of Breast Cancer and Breast-Self Examination among University Students in Yemen. Asian Pac. J. Cancer Prev. 2010, 11, 101–105. [Google Scholar]
- Bawazir, A.; Bashateh, N.; Jradi, H.; Breik, A.B. Breast Cancer Screening Awareness and Practices among Women Attending Primary Health Care Centers an the Ghail Bawazir District of Yemen. Clin. Breast Cancer 2019, 19, 20–29. [Google Scholar] [CrossRef] [PubMed]
- Champion, V.; Menon, U. Predicting Mammography and Breast Self- Examination in African American Women. Cancer Nurs. 1997, 20, 315–322. [Google Scholar] [CrossRef] [PubMed]
- Temel, A.B.; Dağhan, Ş.; Kaymakçı, Ş.; Dönmez, R.Ö.; Arabacı, Z. Effect Of Structured Training Programme on the Knowledge and Behaviors of Breast and Cervical Cancer Screening among the Female Teachers in Turkey. BMC Women’s Health 2017, 17, 123. [Google Scholar]
- Akhtari-Zavare, M.; Juni, M.H.; Said, S.M.; Ismail, I.Z.; Latiff, L.A.; Eshkoor, S.A. Result of Randomized Control Trial to Increase Breast Health Awareness among Young Females in Malaysia. BMC Public Health 2016, 16, 738. [Google Scholar] [CrossRef] [PubMed]
- Alice, T.E.; Philomena, O. Breast Self-Examination among Secondary School Teachers in South-South, Nigeria: A Survey of Perception and Practice. JPHE 2014, 6, 169–173. [Google Scholar]
- Alameer, A.; Mahfouz, M.S.; Alamir, Y.; Ali, N.; Darraj, A. Effect of Health Education on Female Teachers’ Knowledge and Practices Regarding Early Breast Cancer Detection and Screening in the Jazan Area: A Quasi-Experimental Study. J. Cancer Educ. 2019, 34, 865–870. [Google Scholar] [CrossRef]
- Masoudiyekta, L.; Rezaei-Bayatiyani, H.; Dashtbozorgi, B.; Gheibizadeh, M.; Malehi, A.S.; Moradi, M. Effect of Education Based on Health Belief Model on the Behavior of Breast Cancer Screening in Women. Asia Pac. J. Oncol. Nurs. 2018, 5, 114–120. [Google Scholar]
- Ebell, M.H.; Thai, T.N.; Royalty, K.J. Cancer Screening Recommendations: An International Comparison of High Income Countries. Public Health Rev. 2018, 39, 7. [Google Scholar] [CrossRef]
- Agide, F.D.; Sadeghi, R.; Garmaroudi, G.; Tigabu, B.M. A Systematic Review of Health Promotion Interventions to Increase Breast Cancer Screening Uptake: From the Last 12 Years. Eur. J. Public Health 2018, 28, 1149–1155. [Google Scholar] [CrossRef]
- Marzo, R.R.; Salam, A. Teachers’ Knowledge, Beliefs and Practices of Breast Self-Examination in a City of Philippine: A Most Cost-Effective Tool for Early Detection of Breast Cancer. J. Appl. Pharm. Sci. 2016, 6, 16–21. [Google Scholar] [CrossRef]
- Alabi, M.A.; Abubakar, A.; Olowokere, T.; Okeyode, A.A.; Mustapha, K.; Ayoola, S.A. Knowledge, Attitude, and Practice of Breast Self- Examination among Female Teachers from Selected Secondary Schools in Ogbomosho, Oyo State. Niger. J. Exp. Clin. Biosci. 2018, 6, 8–12. [Google Scholar]
- Rosenstock, I.M. Historical Origins of the Health Belief Model. Health Educ. Monogr. 1974, 2, 328–335. [Google Scholar] [CrossRef]
- Conner, M.; Norman, P. Predicting Health Behaviour, 2nd ed.; Open University Press. Maidenhead: Berkshire, UK, 2005; pp. 28–80. ISBN 13 978 0335 21176 0. [Google Scholar]
- Lawal, O.; Murphy, F.; Hogg, P.; Nightingale, J. Health Behavioural Theories and Their Application to Women’s Participation in Mammography Screening. J. Med. Imaging Radiat. Sci. 2017, 48, 122–127. [Google Scholar] [CrossRef] [PubMed]
- Ahmadian, M.; Samah, A.A. Application of Health Behavior Theories to Breast Cancer Screening among Asian Women. Asian Pac. J. Cancer Prev. 2013, 14, 4005–4013. [Google Scholar] [CrossRef]
- Ersin, F.; Gözükara, F.; Polat, P.; Erçetin, G.; Bozkurt, M.E. Determining the Health Beliefs and Breast Cancer Fear Levels of Women Regarding Mammography. Turk. J. Med. Sci. 2015, 45, 775–781. [Google Scholar] [CrossRef] [PubMed]
- Serra, Y.A.; Colón-López, V.; Savas, L.S.; Vernon, S.W.; Fernández-Espada, N.; Vélez, C.; Ayala, A.; Fernández, M.E. Using Intervention Mapping to Develop Health Education Components to Increase Colorectal Cancer Screening in Puerto Rico. Front. Public Health 2017, 5, 324. [Google Scholar] [CrossRef]
- Huang, J.; Wang, J.; Pang, T.W.Y.; Chan, M.K.Y.; Leung, S.; Chen, X.; Leung, C.; Zheng, Z.J.; Wong, M.C.S. Does Theory of Planned Behaviour Play a Role in Predicting Uptake of Colorectal Cancer Screening? A Cross-Sectional Study in Hong Kong. BMJ Open 2020, 10, e037619. [Google Scholar] [CrossRef]
- Lau, J.; Lim, T.Z.; Wong, G.J.; Tan, K.K. The Health Belief Model and Colorectal Cancer Screening in the General Population: A Systematic Review. Prev. Med. Rep. 2020, 20, 101223. [Google Scholar] [CrossRef]
- Roncancio, A.M.; Ward, K.K.; Sanchez, I.A.; Cano, M.A.; Byrd, T.L.; Vernon, S.W.; Fernandez-Esquer, M.E.; Fernandez, M.E. Using the Theory of Planned Behavior to Understand Cervical Cancer Screening among Latinas. Health Educ. Behav. 2015, 42, 621–626. [Google Scholar] [CrossRef]
- Abamecha, F.; Tena, A.; Kiros, G. Psychographic Predictors of Intention to Use Cervical Cancer Screening Services among Women Attending Maternal and Child Health Services in Southern Ethiopia: The Theory of Planned Behavior (TPB) Perspective. BMC Public Health 2019, 19, 434. [Google Scholar] [CrossRef]
- Shida, J.; Kuwana, K.; Takahashi, K. Behavioral Intention to Prevent Cervical Cancer and Related Factors among Female High School Students in Japan. Jpn. J. Nurs. Sci. 2018, 15, 375–388. [Google Scholar] [CrossRef] [PubMed]
- Aldohaian, A.I.; Alshammari, S.A.; Arafah, D.M. Using the Health Belief Model to Assess Beliefs and Behaviors Regarding Cervical Cancer Screening among Saudi Women: A Cross-Sectional Observational Study. BMC Women’s Health 2019, 19, 6. [Google Scholar] [CrossRef] [PubMed]
- Zare, M.; Ghodsbin, F.; Jahanbin, I.; Ariafar, A.; Keshavarzi, S.; Izadi, T. The Effect of Health Belief Model-Based Education on Knowledge and Prostate Cancer Screening Behaviors: A Randomized Controlled Trial. Int. J. Community Based Nurs. Midwifery 2016, 4, 57–68. [Google Scholar] [PubMed]
- Bashirian, S.; Barati, M.; Mohammadi, Y.; Moaddabshoar, L.; Dogonchi, M. An Application of the Protection Motivation Theory to Predict Breast Self-Examination Behavior among Female Healthcare Workers. Eur. J. Public Healt. 2019, 15, 90–97. [Google Scholar] [CrossRef]
- Naz, M.S.G.; Simbar, M.; Fakari, F.R.; Ghasemi, V. Effects of Model-Based Interventions on Breast Cancer Screening Behavior of Women: A Systematic Review. Asian Pac. J. Cancer Prev. 2018, 19, 2031–2041. [Google Scholar]
- Copeland, V.C.; Kim, Y.J.; Eack, S.M. Effectiveness of Interventions for Breast Cancer Screening in African American Women: A Meta-Analysis. Health Serv. Res. 2018, 53, 3170–3188. [Google Scholar] [CrossRef]
- Secginli, S.; Nahcivan, N.O.; Gunes, G.; Fernandez, R. Interventions Promoting Breast Cancer Screening among Turkish Women with Global Implications: A Systematic Review. Worldviews Evid. Based Nurs. 2017, 14, 316–323. [Google Scholar] [CrossRef]
- Donnelly, T.T.; Hwang, J. Breast Cancer Screening Interventions for Arabic Women: A Literature Review. J. Immigr. Minor. Health 2015, 17, 925–939. [Google Scholar] [CrossRef]
- Chan, D.N.; So, W.K. A Systematic Review of Randomised Controlled Trials Examining the Effectiveness of Breast and Cervical Cancer Screening Interventions for Ethnic Minority Women. Eur. J. Oncol. Nurs. 2015, 19, 536–553. [Google Scholar] [CrossRef]
- Khan, T.M.; Leong, J.; Ming, L.C.; Khan, A.H. Association of Knowledge and Cultural Perceptions of Malaysian Women with Delay in Diagnosis and Treatment of Breast Cancer: A Systematic Review. Asian Pac. J. Cancer Prev. 2015, 16, 5349–5357. [Google Scholar] [CrossRef]
- O’Mahony, M.; Comber, H.; Fitzgerald, T.; Corrigan, M.A.; Fitzgerald, E.; Grunfeld, E.A.; Flynn, M.G.; Hegarty, J. Interventions for Raising Breast Cancer Awareness in Women. Cochrane Database Syst. Rev. 2017, 2. [Google Scholar] [CrossRef] [PubMed]
- Armijo-Olivo, S.; Stiles, C.A.; Hagen, N.D.; Biondo, P.; Cummings, G. Assessment of Study Quality for Systematic Reviews: A Comparison of the Cochrane Collaboration Risk of Bias Tool and the Effective Public Health Practice Project Quality Assessment Tool: Methodological Research. J. Eval. Clin. Pract. 2012, 18, 12–18. [Google Scholar] [CrossRef] [PubMed]
- Thomas, B.; Ciliska, D.; Dobbins, M.; Micucci, S. A Process for Systematically Reviewing the Literature: Providing the Research Evidence for Public Health Nursing Interventions. Worldviews Evid. Based Nurs. 2004, 1, 176–184. [Google Scholar] [CrossRef] [PubMed]
- Eskandari-Torbaghan, A.; Kalan-Farmanfarma, K.; Ansari-Moghaddam, A.; Zarei, Z. Improving Breast Cancer Preventive Behavior among Female Medical Staff: The Use of Educational Intervention Based on Health Belief Model. MJMS 2014, 21, 44–50. [Google Scholar]
- Fathollahi-Dehkordi, F.; Farajzadegan, Z. Health Education Models Application by Peer Group for Improving Breast Cancer Screening among Iranian Women with a Family History of Breast Cancer: A Randomized Control Trial. MJIRI 2018, 32, 51. [Google Scholar] [CrossRef]
- Heydari, E.; Noroozi, A. Comparison of Two Different Educational Methods for Teachers’ Mammography Based on the Health Belief Model. Asian Pac. J. Cancer Prev. 2015, 16, 6981–6986. [Google Scholar] [CrossRef]
- Khiyali, Z.; Aliyan, F.; Kashfi, S.H.; Mansourian, M.; Jeihooni, A.K. Educational Intervention on Breast Self-Examination Behavior in Women Referred to Health Centers: Application of Health Belief Model. Asian Pac. J. Cancer Prev. 2017, 18, 2833–2838. [Google Scholar]
- Mirmoammadi, A.; Parsa, P.; Khodakarami, B.; Roshanaei, G. Effect of Consultation on Adherence to Clinical Breast Examination and Mammography in Iranian Women: A Randomized Control Trial. Asian Pac. J. Cancer Prev. 2018, 19, 3443–3449. [Google Scholar] [CrossRef]
- Taymoori, P.; Molina, Y.; Roshani, D. Effects of a Randomized Controlled Trial to Increase Repeat Mammography Screening in Iranian Women. Cancer Nurs. 2015, 38, 288–296. [Google Scholar] [CrossRef]
- Lee-Lin, F.; Pedhiwala, N.; Nguyen, T.; Menon, U. Breast Health Intervention Effects on Knowledge and Beliefs over Time among Chinese American Immigrants—A Randomized Controlled Study. J. Cancer Educ. 2015, 30, 482–489. [Google Scholar] [CrossRef]
- Elder, J.; Haughton, J.; Perez, L.; Martínez, M.; De la Torre, C.; Slymen, D.J.; Arredondo, E.M. Promoting Cancer Screening among Churchgoing Latinas: Fe En Accion/Faith in Action. Health Educ. Res. 2017, 32, 163–173. [Google Scholar] [CrossRef] [PubMed]
- Goel, M.S.; O’Conor, R. Increasing Screening Mammography among Predominantly Spanish Speakers at a Federally Qualified Health Center Using a Brief Previsit Video. Patient Educ. Couns. 2016, 99, 408–413. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.-Y.; Lin, C. Developing and Evaluating an Individually-Tailored Intervention to Increase Mammography Adherence among Chinese American Women. Cancer Nurs. 2016, 38, 40–49. [Google Scholar] [CrossRef] [PubMed]
- Lee-Lin, F.; Nguyen, T.; Pedhiwala, N.; Dieckmann, N.; Menon, U. A Breast Health Educational Program for Chinese-American Women: 3-To 12-Month Post intervention Effect. Am. J. Health Promot. 2015, 29, 173–181. [Google Scholar] [CrossRef] [PubMed]
- Gondek, M.; Shogan, M.; Saad-Harfouche, F.G.; Rodriguez, E.M.; Erwin, D.O.; Griswold, K.; Mahoney, M.C. Engaging Immigrant and Refugee Women in Breast Health Education. J. Cancer Educ. 2015, 30, 593–598. [Google Scholar] [CrossRef]
- Kocaöz, S.; Özçelik, H.; Talas, M.S.; Akkaya, F.; Özkul, F.; Kurtuluş, A.; Ünlü, F. The Effect of Education on the Early Diagnosis of Breast and Cervix Cancer on the Women’s Attitudes and Behaviors Regarding Participating in Screening Programs. J. Cancer Educ. 2017, 33, 821–832. [Google Scholar] [CrossRef]
- Seven, M.; Akyüz, A.; Robertson, L.B. Interventional Education Methods for Increasing Women’s Participation in Breast Cancer Screening Program. J. Cancer Educ. 2014, 30, 244–252. [Google Scholar] [CrossRef]
- Rabbani, S.A.; Al Marzooqi, A.M.S.K.; Srouji, A.E.M.; Hamad, E.A.; Mahtab, A. Impact of Community-Based Educational Intervention on Breast Cancer and its Screening Awareness among Arab Women in The United Arab Emirates. Clin. Epidemiol. Glob. Health 2019, 7, 600–605. [Google Scholar] [CrossRef]
- Ouyang, Y.Q.; Hu, X. The Effect of Breast Cancer Health Education on the Knowledge, Attitudes, and Practice: A Community Health Center Catchment Area. J. Cancer Educ. 2014, 29, 375–381. [Google Scholar] [CrossRef]
- Vasishta, S.; Ramesh, S.; Babu, S.; Ramakrishnegowda, A.S. Awareness about Breast Cancer and Outcome of Teaching on Breast Self Examination in Female Degree College Students. India J. Med. Spec. 2018, 9, 56–59. [Google Scholar] [CrossRef]
- Champion, V.L. Revised Susceptibility, Benefits, and Barriers Scale for Mammography Screening. Res. Nurs. Health 1999, 22, 341–348. [Google Scholar] [CrossRef]
- Champion, V.L. Instrument Refinement for Breast Cancer Screening Behaviors. Res. Nurs. Health 1993, 42, 139–143. [Google Scholar] [CrossRef]
- Glanz, K.; Rimer, B.K.; Viswanath, K. Health Behavior and Health Education: Theory, Research, and Practice, 4nd ed.; John Wiley & Sons: Hoboken, NJ, USA, 2008. [Google Scholar]
- Prochaska, J.O.; Velicer, W.F. The Transtheoretical Model of health behavior change. Am. J. Health Promot. 1997, 12, 38–48. [Google Scholar] [CrossRef] [PubMed]
- Pender, N.J.; Murdaugh, C.; Parsons, M. The Health Promotion Model. Health Promot. Pract. 2002, 4, 59–79. [Google Scholar]
- Rimer, B.K.; Glanz, K. Theory at a Glance: A Guide for Health Promotion Practice, 2nd ed.; US Department of Health and Human Services, National Institutes of Health, National Cancer Institute: Bethesda, MD, USA, 2005. [Google Scholar]
- Kerr, J.; Rosenberg, D.E.; Nathan, A.; Millstein, R.A.; Carlson, J.A.; Crist, K.; Wasilenko, K.; Bolling, K.; Castro, C.M.; Buchner, D.M.; et al. Applying the Ecological Model of Behavior Change to a Physical Activity Trial in Retirement Communities: Description of the Study Protocol. Contemp. Clin. Trials 2012, 33, 1180–1188. [Google Scholar] [CrossRef]
| Types of Studies to Be Included | Types of Studies to Be Excluded |
|---|---|
|
|
| Participants Women aged eighteen years old and above, without history of BC. | |
| Intervention Health promotion and behavioral program on BCS targeted women. | |
| Control group Either usual care or no intervention, or minimal intervention or intervention other than the intervention groups. | |
| Outcomes Any of the following: BCS uptake (BSE (breast self-examination), CBE (clinical breast examination), MMG (mammography)), knowledge of BC and screening, health beliefs about BC and screening. | |
| Publication year From January 2014 to May 2019. | |
| Language English. | |
| Article type Original studies. |
| Study/Country | Study Design/EPHPP | Theory | Participants Characteristics/Sample size | Setting/Unit of Assignment |
|---|---|---|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Study | Intervention Characteristics | Findings |
|---|---|---|
| Akhtari Zavare et al., 2016 [16] | Content: Breast health awareness/normal breast/BC knowledge/screening methods/training on BSE performance. Method of delivery: Spoken/written materials. 2 h workshops with a group of 12–13, delivered by the study researchers (1 h lecture in the form of PPT + 1 h training on BSE and participant’s duplication on breast silicon model) + educational booklet. Control group: Received all materials after the completion of the education. |
|
| Heydari and Noroozi, 2015 [49] | Content: Breast anatomy/warning against BC/perceived susceptibility and severity/benefit and barriers of MMG/MMG performance. Method of delivery: Spoken/written materials. Delivered by the study researchers. Group education: Two training sessions lasting 45–60 min with a 1-week interval. In the form of group discussion/oral presentation/PPT slides/SMS reminder. Multimedia education group: Training through CD/educational SMS/SMS reminder. |
|
| Eskandari-Torbaghan et al., 2014 [47] | Content: BC symptoms/right time for MMG/preventive behaviors of BC including healthy diet and physical activity/perceived sensitivity and seriousness, barriers in performing BC preventive behaviors. Methods of delivery: Spoken/written materials. Three sessions, delivered by the main investigators, each about 1–1.5 h long in the form of lectures/questions and answers/PPT/videos/educational booklet. Control group: Received training after the education completing. |
|
| Goel and O’Conor, 2016 [55] | Content: Importance of MMG/experience of undergoing MMG/BC grows and spreads. Method of delivery: Spoken. Delivered by healthcare provider. A brief 30-s video meeting between the provider and the participants. Control: Usual care. |
|
| Kocaöz et al., 2017 [59] | Content: Breast anatomy/unusual changes in the breast/importance of BC/risk factors/early diagnosis/symptoms/treatment/BSE. Method of delivery: Spoken/written materials. Delivered by the study investigators, a session of 40 min in the form of visual presentation/participants’ performance of BSE/an education brochure on BC and its screening/participation in screening programs. |
|
| Elder et al., 2017 [54] | Content: Breast anatomy/importance of BC prevention/risk factors and treatment/prevention steps/myths on BC/perceived barriers. Method of delivery: Spoken/written materials. A 6-week series of classes for each 90–120 min delivered by a trained bilingual/bicultural community healthcare worker. The intervention is a multilevel model that includes: Individual-level: BC screening classes/handouts to participants. Interpersonal level: Two motivational interviewing (MI) calls/reminder calls. Organizational level: Cancer screening sessions were announced in the church brochure/churches assigned spaces for education sessions. Environmental Level: Through training, promotors give information about the services and the local clinics, and completed Affordable Care Act workshops. Control: Physical activity intervention. |
|
| Yılmaz et al., 2017 [11] | Content: Symptoms and risk factors of BC/screening approaches (BSE, CBE, MMG). Method of delivery: Spoken. A 60–90 min PPT delivered by the study researcher. |
|
| Freund et al., 2017 [9] | Content: General screening recommendations/BC facts/early detection procedures/screening barriers, cultural and religious beliefs. Method of delivery: Spoken/written materials. The education was designed to be tailored culturally and personally for each participant through interview/discussion. Control: No treatment. |
|
| Mirmoammadi et al., 2018 [51] | Content: HBM constructs/breast anatomy/physiological changes in the breast/symptoms and signs of BC/methods of BCS/treatment of BC. Method of delivery: Spoken/written materials, in 4 weekly sessions, 90 min long, of BCS individual consulting in the form of Q&A/speech/slideshow/group discussion/practical training/oral and practical test/booklet. Control: Routine care. After the study completion, the training booklet was offered to them. |
|
| Khiyali et al., 2017 [50] | Content: Risk factors/complications/screening methods including BSE/when and how to correctly perform BSE. Method of delivery: Spoken. The training program included 5 one-hour training sessions delivered by the study researcher through group discussion/video demonstration/training sessions. Control: No treatment. |
|
| Masoudiyekta et al., 2018 [19] | Content: BC facts and figures/BC epidemiology/risk factors, symptoms of BC/importance of early detection/screening methods/guidelines for MMG/health motivation/susceptibility to BC/benefits, barriers, and self-efficacy/list of public hospitals that provide MMG. Method of delivery: Spoken/written materials. Four 90–120 min teaching sessions in the form of PPT/videos/performing BSE on the models/group discussion/Q&A session/pamphlets. Control: No treatment. |
|
| Lee-Lin et al., 2015b [53] | Content for the intervention group: BC incidence/risk factors/process and benefits of MMG/cultural barriers. Content for the control group: Brochure consists of the following: do you think you are at risk of BC, what is MMG screening, who should get MMG, why and how should I get MMG, how can I pay, and where can I find information. It also stressed taking care of oneself. Method of delivery: Spoken/written materials. The TBHEP 1 h intervention included 2 parts, group teaching delivered by the study researcher followed by individual counseling by trained staff/the materials covered cultural, graphic like photos of both old and young Chinese women, Asian landscapes, and some dialogs between a Chinese grandmother, mother, and daughter/PPT/group discussions/Q&A sessions/face-to-face interactions. Control: A brochure emphasized caring for self. Reminder of follow-up survey with telephone calls in 3 months. |
|
| Lee-Lin et al., 2015a [57] | Content for the intervention group: BC incidence/risk factors/process and benefits of MMG/cultural barriers. Content for the control group: Brochure consists of the following: do you think you are at risk of BC, what is MMG screening, who should get MMG, why and how should I get MMG, how can I pay, and where can I find information. It also stressed taking care of oneself. Method of delivery: Spoken/written materials. The TBHEP 1 h intervention included 2 parts, group teaching delivered by the study researcher followed by individual counseling by trained staff/the materials covered culturally graphics like photos of both old and young Chinese women, the Asian landscapes, and some dialogs between a Chinese grandmother, mother, and daughter/PPT/group discussions/Q&A sessions/face-to-face interactions. Control: A brochure emphasized caring for self. Reminder of follow-up survey with telephone calls in 3 months. |
|
| Fathollahi-Dehkordi and Farajzadegan, 2018 [48] | Content: BC risk factors, signs and symptoms/screening tests/benefits of early diagnosis/ways to improve sensitivity, and severity of BC, methods to increase motivation, and overcoming barriers. Method of delivery: Spoken. Three sessions, 2 h long, in 4 groups with 10 to 15 women in three weeks, delivered by a peer educator in the form of oral presentation/image presentation/group discussion/women shared knowledge and beliefs on BC and BCS. The educator talked about her experiences and beliefs/women were also encouraged to connect with each other after the completion of the education and share their new practices to help one another to overcome screening barriers. Control: Invited to contribute in training session at the completion of the follow-up and education was offered to them. A telephone number for consultations were also provided to them. |
|
| Taymoori et al., 2015 [52] | The HBM intervention: Content: Perceived threat, MMG benefits and barriers, and self-efficacy. Method of delivery: Spoken/written materials. Eight sessions in the form of slides, pamphlets, films, group discussions, and role modeling with BC survivors. Delivered by research staff in groups of 5–12 women. Individual sessions tailored to women’s specific needs. Each woman received eight 45–60 min group sessions, women were divided into groups based on their reported requirements. The HBM + TPB intervention:Content: In addition to HBM intervention content, participants received sessions focused on subjective norms and perceived behavioral control. Method of delivery: Spoken/written materials. In addition to HBM methods of delivery, participants received 4 sessions on subjective norms and perceived control. Regarding subjective norms, small groups were formed to encourage peer support and to raise exposure to positive interpersonal norms, and education about the importance of developing social networks. In individual counseling sessions, participants were also asked to provide information for 5 relatives to remind them about MMG. Relatives were invited to participate in a 60 min session. Regarding perceived control, participants were trained to resolve environmental challenges. Reminder messages on scheduling MMG appointments and telephone conversations on subjective norms were also used. Control group: Received pamphlets following the completion of the follow-up survey. |
|
| Rabbani et al., 2019 [61] | Content: General information on BC/signs and symptoms of BC/BC epidemiology, risk factors, anatomy, importance of early detection/BSE/MMG/screening procedures/treatment options. Method of delivery: Spoken/written materials. A 45 min session in the form of slide show + handouts. |
|
| Gondek et al., 2015 [58] | Content: BC statistics/risk factors, signs, symptoms of BC/myths of BC/methods of BCS (BSE, CBE, MMG). Method of delivery: Spoken. A health educator and/or project director delivered educational sessions. A 60–90 min breast health education program, evidence-informed, and community-based culturally competent. Session delivered in multiple languages, in the form of presentations/interactive breast model session/local BC survivor speaks about her personal experiences/a female physician to answer participants questions/women aged 40 years or older who were not currently practicing BCS were contacted and proposed one-on-one navigation assistance in completing BCS. |
|
| Ouyang and Hu, 2014 [62] | Content: Prevalence, characteristics, risk factors, and signs of BC/early detection methods/healthy diet and exercise guidance/importance and benefit of BSE/technique of BSE. Method of delivery: Spoken/written materials. The intervention delivered by the study researcher consisted of 1 h (20 min educational session, 30 min BSE training, 10 min discussion), in the form of PPT presentation/pictures/BSE color images/BSE diagrams/videos/booklet and shower card/monthly telephone follow-up. |
|
| Seven et al., 2014 [60] | Content: Both brochures provided information on BC early signs and symptoms, risk factors/importance of BSE, CBE, MMG/current recommendations on BSE, CBE, MMG. Method of delivery: Spoken/written materials. The primary investigator delivered the intervention in the participants’ homes. Individual education: Each participant received a one-on-one education + educational brochure. Individual education and husband brochure Each woman received one-on-one training and two educational brochures; one for her and another for her husband. Group education Some 60–90-min-long educational sessions + educational brochure/women invited to participate in free BCS services. |
|
| Tuzcu et al., 2016 [10] | Content: Breast anatomy/incidence, mortality rate, risk factors of BC/changes in the breast/BSE, CBE, MMG/instructions on doing BSE/importance of screening methods/susceptibility/benefits, barriers, confidence/benefits, barriers of MMG. Method of delivery: Spoken/written materials. One hour, 10-week-long training in groups of 8–12 individuals delivered by study team members, in the form of 20 min PPT for visual images/15 min film about BSE/20 min BSE training on a breast model/10 min delivery and explanation of the reminder cards/telephone consultations/telephone calls reminders in the 3rd month/invitation card for free MMG/screening behaviors cards. Control: Usual care. After the post-test, study team offered one-to-one education on BCS and reminder cards (BSE card, BCS approaches card) to the control group. |
|
| Vasishta et al., 2018 [63] | Content: Anatomy and physiology of the breast/risk factors for BC/steps and importance of BSE. Method of delivery: Spoken, through PPT. |
|
| Wu and Lin, 2016 [56] | Content for the intervention group: Knowledge of BC/risk factors/MMG screening guidelines/perceived barrier, benefits and self-efficacy. Content for the control group: MMG brochure on breast health. Method of delivery: Spoken/written materials. Individual telephone counseling delivered by research investigators, through 1 h telephone calls interview/application (computer program). Control: Brochure. |
|
| Study and Outcome Measures | Data Collection Periods | Method of Evaluation and Content of Instrument | Psychometric Properties |
|---|---|---|---|
Akhtari Zavare et al., 2016 [16]
|
|
|
|
Heydari and Noroozi, 2015 [49]
|
|
|
|
Eskandari-Torbaghan et al., 2014 [47]
|
|
| Accepted items had content validity ratio larger than 0.62 and content validity indices larger 0.79. Cranach’s alpha = 0.76. |
Goel and O’Conor, 2016 [55]
|
|
| Psychometric properties were not reported. |
Kocaoz et al., 2017 [59]
|
|
|
|
Elder et al., 2017 [54]
|
|
| Psychometric properties were not reported. |
Yilmaz et al., 2017 [11]
|
|
|
|
Freund et al., 2017 [9]
|
| A telephone questionnaire of 22 items that included questions on socio-demographic factors, questions on adherence to MMG, CBE, and BSE screening, and questions on cultural health beliefs. |
|
Mirmoammadi et al., 2018 [51]
|
|
|
|
Khiyali et al., 2017 [50]
|
|
|
|
Masoudiyekta et al., 2018 [19]
|
|
|
|
Lee-Lin et al., 2015b [53]
|
|
|
|
Fathollahi-Dehkordi and Farajzadegan, 2018 [48]
|
|
| Cronbach’s alpha for sensitivity = 0.82, severity = 0.84, barriers = 0.73, benefits = 0.72, and health motivation = 0.77. |
Taymoori et al., 2015 [52]
|
|
|
|
Rabbani et al., 2019 [61]
|
|
| Psychometric properties were not reported. |
Gondek et al., 2015 [58]
|
|
| Psychometric properties were not reported. |
Ouyang and Hu, 2014 [62]
|
|
|
|
Seven et al., 2014 [60]
|
|
|
|
Tuzcu et al., 2016 [10]
|
|
|
|
Vasishta et al., 2018 [63]
|
|
| Tests of validity and reliability were conducted, but details of the psychometric properties were not reported in the article. |
Lee-Lin et al., 2015a [57]
|
| Self-report questionnaire. | |
Wu and Lin, 2016 [56]
|
| Self-report questionnaire. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Noman, S.; Shahar, H.K.; Abdul Rahman, H.; Ismail, S.; Abdulwahid Al-Jaberi, M.; Azzani, M. The Effectiveness of Educational Interventions on Breast Cancer Screening Uptake, Knowledge, and Beliefs among Women: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 263. https://doi.org/10.3390/ijerph18010263
Noman S, Shahar HK, Abdul Rahman H, Ismail S, Abdulwahid Al-Jaberi M, Azzani M. The Effectiveness of Educational Interventions on Breast Cancer Screening Uptake, Knowledge, and Beliefs among Women: A Systematic Review. International Journal of Environmental Research and Public Health. 2021; 18(1):263. https://doi.org/10.3390/ijerph18010263
Chicago/Turabian StyleNoman, Sarah, Hayati Kadir Shahar, Hejar Abdul Rahman, Suriani Ismail, Musheer Abdulwahid Al-Jaberi, and Meram Azzani. 2021. "The Effectiveness of Educational Interventions on Breast Cancer Screening Uptake, Knowledge, and Beliefs among Women: A Systematic Review" International Journal of Environmental Research and Public Health 18, no. 1: 263. https://doi.org/10.3390/ijerph18010263
APA StyleNoman, S., Shahar, H. K., Abdul Rahman, H., Ismail, S., Abdulwahid Al-Jaberi, M., & Azzani, M. (2021). The Effectiveness of Educational Interventions on Breast Cancer Screening Uptake, Knowledge, and Beliefs among Women: A Systematic Review. International Journal of Environmental Research and Public Health, 18(1), 263. https://doi.org/10.3390/ijerph18010263






