Abstract
Background: The new characteristics of today’s population, together with the presence of chronic diseases in the elderly, require a new approach to care, promoting coordination between different levels of care. In this sense, we find the figure of the nurse case manager (NCM) in primary health care mainly responsible for ensuring continuity of care in complex patients with chronic diseases. Objective: to describe the role of the NCM in care management, determining its effectiveness in addressing chronic disease (health outcomes and quality of life) and its efficiency in the health system. Methods: Bibliographic review of scientific evidence on case management applied to nursing. Between March and April 2020 a bibliographic search was carried out in the Dialnet, Scielo, Scopus and Pubmed databases. Inclusion criteria: articles written in the last 5 years, which analyze how this nursing rol influences the care and health of patients. Results: A total of 16 articles were selected. The NCM reduced the use of the emergency department, hospital admissions, readmissions, and the duration of these in the patients studied. Conclusion: The NCM is effective and efficient for both patients and health institutions, and a common practice model is needed that includes standardized protocols and evidence-based practices.
1. Introduction
In all health services, placing the patient at the center of the care system is linked to the quality of the health system. Thus, the user ceases to be a passive subject who receives information and becomes an active user, who has more information about his or her health and rights and has a more proactive attitude [1]. In this health care, nurses are key professionals, because scientific evidence indicates that the lack of nurses generates a situation of significant risk for the health of patients [2].
The health status of the population has generally improved in recent years; however, “long-term disability and chronic diseases are increasing due to a rapidly aging population” [3]. In this line, attention to chronicity is a challenge for any health system, also for Spain, due to the consequences of the aging population, the need to respond to the increase of users with chronic diseases and the high existing comorbidity [4]. The attention to all these health problems entails a high cost in services and benefits, which must be faced. This situation requires the implementation of new professional nursing profiles, with expanded and advanced skills that are developed in response to new demands in different contexts and areas of care. The figure of the Nurse Case Manager (NCM) is a good example of an emerging professional figure worldwide [4].
Case management was born in the United States (USA) in the years 1950/1960, applied for the first time in mental health cases; later it was used for the care of people with high-risk health problems and high costs, “with the aim of improving efficiency and decreasing variability” [5]. Case management is “the collaborative process by which the options and services needed to meet an individual’s health needs are assessed, planned, implemented, coordinated, monitored, and evaluated, articulating communication and available resources to promote quality and cost-effective outcomes” [5]. The NCM has become a common figure also in Spain, to offer care in a changing society, and to people with complex situations derived from chronicity, pluripathology, frailty and aging [4]. In Spain, the NCM plans and coordinates the care of patients with chronic diseases, mainly in the area of Primary Health Care (PHC), especially those more complex cases that require better coordination of the health system [4].
Despite the fact that case management has not been carried out exclusively and always by nursing professionals, nurses have usually been the figure chosen in different healthcare settings, although doctors or social workers have also carried out this work [6]. The fact that nurses usually lead case management is because they have a comprehensive vision of covering human needs, promoting self-care, as well as assessing and planning care. The NCM uses the nursing process as a dynamic method with a theoretical basis that allows for humanistic care, focused on optimally achieving objectives. This nurse has an in-depth knowledge of the bio-psycho-social context of the user (and his or her community, networks, environments etc.), which facilitates joint decision-making with other professionals when planning care [7], assuming responsibility for case management.
Background
The case management model followed was the Chronic Care Model (CCM), developed by E. Wagner, in 1998 (USA) [8]. The CCM considers the following elements as a requirement for managing chronic diseases: the health system, clinical information systems, patient decision support, patient self-management, delivery system design, and the community (including patient organizations and resources) which interact with clinical practice [8]. The main objective of this model is for patients to be active and informed at all times during the clinical relationship, through proactive professionals with the skills to perform quality care and excellent health outcomes (along with a high degree of patient satisfaction) [8,9]. The ultimate idea of this model is that patients are the ones who will finally take care of their disease, thanks to the elements seen above.
Furthermore, the Kaiser Permanente risk stratification model, which classifies patients according to the level of care they need, has also been considered as a complementary model [7,10]. Thus, at the top of the pyramid there are the highly complex chronic patients, which require specific care directed by professionals with advanced levels of competence, such as the NCM, capable of having an exhaustive knowledge of the patient and his or her environment, and can provide multidisciplinary work and continuity of care [4,6,7,8].
The case management model is a way to improve the Integrated, Coordinated and Continuous Care, allowing to establish a link between the Hospital Care (HC) and the PHC. With this, the articulation of these care areas is improved, avoiding loss of care that affects the integrity and continuity of the health system [6]. With the work of the NCM these problems of the patient who needs health care in multiple environments are solved, which generates more complexity and fully justifies the need for case management.
In more current terms, it is pointed out that case management is a model of advanced nursing practice [11], which is holistic, patient-centered (in its environment), promotes personal autonomy and social participation, and facilitates access to resources. In addition, some of the tasks of the NCM are the recruitment of dependent patients who need a comprehensive multiprofessional approach; to identify people with higher pathological burden and high risk of hospital admission; to try to perform the least invasive care; to establish alliances between PHC and HC professionals; to ensure coordination and continuity of care in patients who require complex care and treatment at different levels of care; to make a personalized plan of care (including the PHC giver in this plan); and to promote individual and family self-care [4,6].
Since the type of patients with whom the NCM works are users with chronic diseases and multimorbidity, especially complex patients, it is interesting to analyze the results of an advanced practice figure such as the NCM. This is important because currently long-term disability and chronic diseases have increased, with a severe socio-demographic transformation as a result of the aging population that underpins the redesign of health services and the skills of their professionals [3].
The research question that emerges from the literature review is: How do the activities performed by nurse case managers affect the management of patient care? The patient is the person receiving care, the intervention is the activities performed by these advanced practice nurses, and the outcomes are those derived from care management and efficiency. Therefore, we intend with this study to describe the role of the NCM in care management, determining its effectiveness in addressing chronic disease (health outcomes) and its efficiency in the health system.
2. Methods
2.1. Study Design
Bibliographic review was carried out between January and April 2020.
2.2. Search Strategy
Two independent researchers consulted the following electronic databases: PUBMED, SCIELO, SCOPUS and DIALNET. Terms from the “Medical Subject Heading“ [12] (nurse, case management, crhonic disease) and the DeCS [13] (enfermera, enfermedad crónica, gestor de casos) were used. Additionally, the free term “care management” was used too. Subsequently, a manual review of the bibliographic references of the selected articles was carried out in order to include other studies potentially valid for the review through the reverse or secondary search method (Table 1). The last search was conducted on 30 April 2020.

Table 1.
Search strategy.
2.3. Selection Criteria
Inclusion criteria: articles describing the activity of NCM or case management applied to nursing; articles related the NCM to chronic diseases; studies describing the efficiency of the interventions carried out by NCM (cost reduction, reduction of complications etc.).
Exclusion criteria: gray literature (web pages, conference abstracts, unpublished theses etc.); clinical practice guidelines; published articles before 2015 (in Scopus the filter of years 2016–2020 was used, due to the limitations of the database); articles describing the role of NCM without studying the results of their interventions.
2.4. Research Variables
The information obtained was grouped on two variables: effectiveness (hospital admissions, days of hospitalization, improvement in health status, satisfaction) and efficiency (use of resources and cost of care).
2.5. Methodological Quality and Level Of Evidence
To evaluate the quality of the studies obtained, we used the Critical Reading Methodology of the Spanish Critical Appraisal Skills Programme (CASPe, Oxford, UK) [14] and the quality criteria of the STROBE statement (Strengthening The Reporting of Observational Studies in Epidemiology) [15]. Besides, the degree of evidence and the level of recommendation through the Scottish Intercollegiate Guidelines Network (SIGN) scale were also assessed [16].
2.6. The Selection Process of the Studies
The selection process of the studies was carried out through the reading of the title and abstract of each article. After the elimination of duplicates and the application of the inclusion and exclusion criteria, the articles were read in full, with an evaluation of the quality of each article with critical reading guidelines. Finally, the references of the selected articles were reviewed in order to apply the reverse search method.
The result of the literature search process is shown in Figure 1.
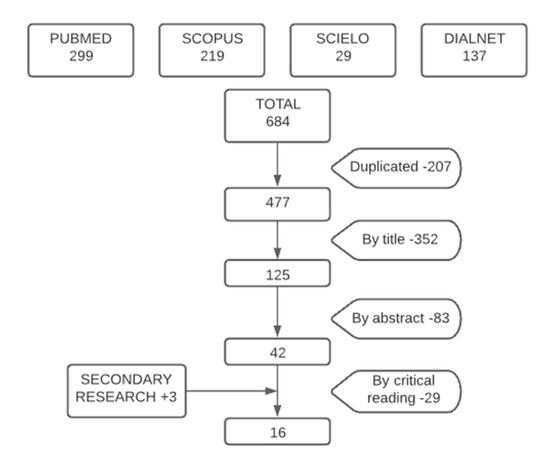
Figure 1.
Flow chart of research.
3. Results
Sixteen articles were selected after the search procedure: 13 were obtained from the bibliographic search and 3 were included by reverse search. Among them were two descriptive studies [10,17] both published in Spain. López and Puente [17] describe the degree of institutionalization of the NCM, while Valverde et al. [10] analyzed the functions and target population of NCM. We also found six literature reviews. Of these, two bibliographic reviews [18,19], carried out in Spain and the USA, respectively) and four systematic reviews [20,21,22,23], the latter is a meta-analysis. Of these studies, one was carried out in the United States [22], two in the United Kingdom [20,23] and one in South Korea [21] (Figure 2). With regard to the longitudinal observational studies, two were obtained from follow-up cohorts served by case management services [24,25]). In addition, we found two experimental studies; a clinical trial [26] and a randomized clinical trial with a control group [27]. In both, it was observed how the activities of the NCM influence the care of patients. One pure qualitative study [28] was retrieved in which 23 nurse case managers in South Korea were interviewed in focus groups and individually. Finally, three studies of mixed methods design were obtained [29,30,31] (Figure 2).
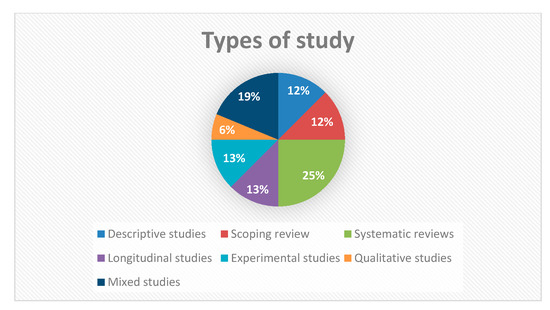
Figure 2.
Types of study designs.
3.1. Health Effects: Efficacy Results on Patients with Chronic Diseases
The interventions carried out by the NCM were more effective and efficient in addressing people with chronic diseases than those carried out according to the traditional model [28]. This nurse can provide the same quality of care as physicians in a wide variety of services (such as routine monitoring of chronic patients and first contact with patients with minor health problems). Improvement in disease self-management, knowledge of the disease and quality of life was observed in the patients studied [25,27].
Case management has proven effective in the treatment of many chronic diseases, such as diabetes, hypertension, obstructive pulmonary disease, and cancer care [18,26,27]. This was due to the interventions made by the nurse, which included the regular presence of the NCM with the patient and family in the consultations, home visits, telephone contacts (a higher level of care), aids in daily decisions for disease control (individual patient planning) and the structuring of a follow-up protocol for complications.
The interventions described above agreed with those analyzed by Joo and Huber [22] and Davisson and Swason [31], in which the objective of the NCM was to provide continuous care for the patient with optimal follow-up to improve his or her health condition. Caregivers were also supported through active listening and emotional and instrumental support so that they could continue to perform their tasks, providing the best possible care to patients.
The aspects most valued by participants concerning to the case management program were its accessibility, both by telephone and in person; always being cared for by the same professionals and the interpersonal relationship established between the nurse and the patient [31]. This professional-patient relationship made it possible for the nurse to advise the patient so that he or she would not immediately resort to self-medication (this new form of care helped patients to understand their pathologies and to detect signs of alarm, thus regaining the effectiveness of the self-management described above [25,27]).
The improvement of psychological outcomes was analyzed in studies that had several similarities, such as a gradual transition of care from hospitals to communities, continuously through follow-up by home visits or telephone calls (coordinated and continuous care from the hospital environment to the communities). These interventions provided comprehensive care, referral services, patient support, and the establishment of common and agreed-upon goals [10,21,22,30].
Considering the unfavorable results for case management models, a meta-analysis found that there are no significant differences in patient mortality [22]. However, very small significant effects were observed that favored case management for self-reported health status in the short term, for patient satisfaction (short and long term), and for functional health, as we had seen previously [10,18,19,21,24,29,30,31].
3.2. Profitability Results: Efficiency
The NCM reduced the use of the emergency department, hospital admissions, readmissions, and the duration of these in the patients studied [10,17,21,22,25,29]. In this way, there was a reduction in direct and indirect costs for the health system since, with less frequent use of the hospital emergency department, patients underwent fewer diagnostic tests and with the accessibility of the case management program, they required fewer hospitalizations [17,20,21].
Furthermore, there was greater activation of social resources when patients with chronic diseases are treated by the NCM [24,25,29,30]. Furthermore, it was described that patients with low income and lower educational levels achieved the same benefits as those observed in patients with higher income and higher levels of schooling (in terms of diabetes treatment), thus generating an efficient and effective cost to improve the complications of diabetes [26], reducing social inequalities.
The only study that did not show favorable results on the effectiveness and efficiency of case management was a meta-analysis [23], in which no significant differences were seen in the total cost or the use of primary or hospital care.
Table 2 summarizes the content of the documents selected in the literature search.

Table 2.
Information summary table.
4. Discussion
With our study, we aimed to know the most effective interventions of the NCM to improve the health of the population, and the resulting benefits for the health system. Most of the studies consulted previously agreed that the interventions related to a case management program, generally developed by nurses, had a positive impact on people’s health and generated savings in health institutions [10,17,18,19,21,22,24,25,26,27,29,30,31].
The fact of being able to analyze articles from different countries allows us to understand that health data of people with chronic pathologies and comorbidities are quite common all over the world, predominantly elderly chronic patients who generate a high cost in health care [10,17,19,20,23,24,28]. For this reason, strategies have been implemented to generate savings by optimizing the skills of professionals, mainly nurses. The interventions carried out by the NCM have shown a comprehensive nature, assessing the needs and context of the person to provide care that responds to their health problems [10,17,18,19,21,26,27]. These activities are aimed at reducing the defragmentation of health services in order to provide coordinated and continuous care [10,19,23,31].
4.1. Health Results: Effectiveness
The interventions carried out by the NCM were comprehensive, assessing in depth the needs and context of the person to provide care that responds to their health problems [10,19,21,26,27]. These activities are aimed at reducing the defragmentation of health services to provide coordinated and continuous care [10,19,23,31]. Besides, we found a high rate of patient satisfaction with the services offered by the NCM, because this nurse spends more time with patients, giving them more information and advice, especially in chronic follow-up processes [18,19,26,31]. With the exception of the last referenced article [31], it is important to note that patient satisfaction with the role of NCM is supported by an adequate level of evidence.
In the literature consulted, it was observed that nurse case managers improved certain health outcomes: reduction of high blood pressure by facilitating adherence to medication [19,24,27]; reduction of glycated hemoglobin in patients with type II diabetes mellitus due to this nurse’s contact with the patients [19,26]; and decrease the consumption of addictive substances by offering users the services available from the health system by following up with patients who have more frequent contact with them [19,22]. The high level of evidence from these studies gives us confidence that improving clinical outcomes in patients is a fact that reinforces the need for NCM. All these studies also highlighted the empowerment achieved by both the patients themselves and their caregivers, thanks to the training that the NCM offered, improving coping with chronic diseases (high blood pressure, diabetes, chronic obstructive pulmonary disease or use of addictive substances) [18,26,27,31]. Some of the activities carried out by the NCM were the regular presence of this professional with the patient and his or her family in the consultations, help in the daily decisions, structuring a follow-up protocol for complications, support for caregivers or telephone follow-up [22,25,26,27,31].
Several studies affirmed that the NCM is capable of producing better results in patients with mental illnesses [20,22,30], thanks to motivational interviews or the greater contact of this Advanced Practice Nurse, with advanced competencies, with the patients. Although there is also literature that does not favor case management, the same authors show improvements in terms of patient satisfaction or functional health [23].
4.2. Profitability Results: Efficiency
As a result of the case management program, the above-mentioned studies indicate that there is a decrease in the use of health services related to complications of patients’ pathologies, as well as a lower risk of complications such as between hospitalizations, emergencies or readmissions. Due to this, there were evident savings in health costs, which shows us how profitable the services offered by the NCM are [19,21,22]. Although the details of the case management programs varied among the studies analyzed, all mention a continuum of follow-up care through home visits or phone calls made by the NCM. The authors described that regular contact with the case manager may have influenced the results of hospital utilization [10,17,18,19,21,22,24,25,26,27,29,30,31]. Although the efficiency of NCM appears to be demonstrated, it is true that the evidence may be controversial as a result of the type of studies implemented.
Some aspects well-valued by patients were the accessibility (both telephone and face-to-face), the continuity of care (same nurse) and the interpersonal relationship established between nurse and patient, in addition to the perception of greater support by health professionals. These benefits have been concluded by various studies [21,25,26,27,31], which affirm that the NCM makes it easier for clients to know more about their illness and to avoid having to go to the emergency services in case of doubts or complications. The evidence found seems to indicate that, indeed, the accessibility and type of patient relationship with NCM is a strength for the health system.
The only study that does not support the case management model is the one conducted by Stokes et al. [23], who argued that this type of care is not effective for those patients called “at risk” (co-morbid) in PHC. This study only describes some improvements in patient satisfaction. These conclusions may be debatable, since Davisson and Swanson [31] defend that the patients themselves recognized the nurse as the most important element of the program, being the professional most linked to the care and attention of the patients. Even so, the fact that most of the literature consulted expresses the improvement of the health of the patients studied after the implementation of a case management program highlights the importance of NCM as a key figure for health systems.
Most studies [18,20,21,22,23,28], all of them with strong or acceptable evidence, show that nurses did not engage in evidence-based practice due to the lack of a model integrating NCM interventions. As a result of this problem, in some reviews [20,21,24] a great variety in the interventions carried out has been observed, which leads to the fact that, although effective and efficient results are generated, they cannot be generalized and analyzed in greater depth because there is no common theoretical model that uniformly encompasses all the practices of these nurses.
4.3. Limitations
Some of the limitations of this literature review are that the NCM activities in various countries have been contemplated, so that, despite the fact that the activities carried out are similar, the socio-cultural context and the level of academic development and competence of nurses in each country may influence them. Furthermore, by considering different chronic diseases, it has not been possible to make a more comprehensive comparison between case management intervention programs applied to a single disease.
On the other hand, some studies did not expressly talk about the NCM, but stated a model of case management in general (while it is true that most of these models were made up of nurses, some also included other professionals, such as social workers). It would therefore be necessary to carry out new research focused on the model developed by nurses, to describe the effects obtained without generating possible biases.
The new research should measure the time from which the NCM begins to generate positive effects for the health of patients, an aspect that has not been studied. In addition, they should incorporate standardized protocols/common clinical practice guidelines and a proprietary model of care, to avoid the variability of interventions found during the literature review.
5. Conclusions
The interventions carried out by the NCM have an integral character, considering the objectives and needs of each person, and providing coordinated and continuous care. The activities carried out by the NCM improve the health of people with chronic diseases and comorbidity, allowing better results in health indicators. Case management is effective and efficient in most of the literature consulted, reducing health care costs and improving the quality of care.
Author Contributions
Conceptualization, V.D.-B., R.G.R., I.d.M.-M. and V.G.-C.; methodology, V.D.-B., R.G.R., I.d.M.-M., M.I.M.-L., V.G.-C. and J.R.M.; software, R.J.-V., M.V.V.-G. and V.D.-B.; validation, V.G.-C., J.R.M.-R., R.J.-V., Á.S.-R., M.I.M.-L. and J.R.M.-R.; formal analysis, V.D.-B., R.G.R., R.J.-V., Á.S.-R. and I.d.M.-M.; investigation, V.G.-C., V.D.-B., and R.G.R.; resources, J.R.M.-R., R.G.R. and V.G.-C.; data curation R.J.-V. and R.G.R.; writing—original draft preparation, V.D.-B., Á.S.-R., R.G., I.d.M.-M., and M.V.V.-G.; writing—review and editing, J.R.M.-R., R.J.-V., R.G.R. and V.G.-C; visualization, V.G.-C., V.D.-B., Á.S.-R., R.G.R., M.I.M.-L., M.V.V.-G., I.d.M.-M. and J.R.M; supervision, J.R.M.-R., R.G.R., I.d.M.-M., V.G.-C. and R.J.-V.; project administration, R.G.R., I.d.M.-M. and V.G.-C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Consejo Económico y Social. Desarrollo Autonómico, Competitividad y Cohesión Social en el Sistema Sanitario. Madrid, 2010, 01. Available online: http://www.ces.es/documents/10180/18510/Inf0110/a13da181-b58e-4256-a90c-bb8693f215b8 (accessed on 15 August 2020).
- Consejo General de Enfermeria. Madrid: Consejo General de Colegios Oficiales de Enfermería de España. 2015. Available online: https://www.consejogeneralenfermeria.org/sala-de-prensa/noticias/item/16720-la-oms-ratifica-que-en-espana-faltan-enfermeras (accessed on 15 August 2020).
- Bernal-Delgado, E.; García-Arnesto, S.; Oliva, J.; Sánchez Martínez, F.; Repullo, J.R.; Peña-Longobardo, L.M.; Ridao-López, M.; Hernández-Quevedo, C. España: Informe del Sistema Sanitario. Sistemas Sanitarios en Transición 2018, 20, 1–179. Available online: https://www.mscbs.gob.es/biblioPublic/publicaciones/recursos_propios/resp/pdf/REVISION_SISTEMA_SANITARIO_ESPANOL_2018.pdf (accessed on 18 August 2020).
- Sánchez-Martín, C.I. Cronicidad y complejidad: Nuevos roles en Enfermería. Enfermeras de Práctica Avanzada y paciente crónico. Enferm. Clínic 2013, 24, 79–89. [Google Scholar] [CrossRef] [PubMed]
- Gómez Sánchez, M.C. Intervención de la enfermera gestora de casos durante el ingreso hospitalario de pacientes con infección VIH. Rev. Esp. Salud. Pública 2011, 3, 237–244. Available online: http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S1135-57272011000300002 (accessed on 20 August 2020). [CrossRef] [PubMed]
- Morales-Asencio, J.M. Gestión de casos y cronicidad compleja: Conceptos, modelos, evidencias e incertidumbres. Enferm. Clínic 2013, 24, 23–34. [Google Scholar] [CrossRef] [PubMed]
- Valverde Jiménez, M.R.; Hernández Corominas, M.A. Modelo de gestión de casos e investigación. Enferm. Glob. 2012, 11, 246–250. [Google Scholar] [CrossRef][Green Version]
- Yeoh, E.K.; Wong, M.C.S.; Wong, E.L.Y.; Yam, C.; Poon, C.M.; Chung, R.Y.; Chong, M.; Fang, Y.; Wang, H.H.X.; Liang, M.; et al. Benefits and limitations of implementing Chronic Care Model (CCM) in PHC programs: A systematic review. Int. J. Cardiol. 2018, 1, 279–288. [Google Scholar] [CrossRef] [PubMed]
- Uittenbroek, R.J.; van der Mei, S.F.; Reijneveld, S.A. Experiences of case manageners in providing person-centered and integrated care base on the Chronic care model: A qualitative study on embrace. PLoS ONE 2018, 13, e0207109. [Google Scholar] [CrossRef]
- Valverde Jiménez, M.R.; López Benavente, Y.; Hernández Corominas, M.A.; Gómez Ruiz, M.; Blázquez Pedrero, M.; Echevarría Pérez, P. Enfermera Gestora de Casos del Servicio Murciano de Salud: Un año de puesta en marcha del programa. Enferm. Glob. 2014, 13, 57–69. Available online: http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S1695-61412014000400004 (accessed on 25 August 2020). [CrossRef][Green Version]
- García-Fernández, F.P.; Arrabal Orpez, M.J.; Rodríguez Torres, M.C.; Gila Selas, C.; Carrascosa García, I.; Laguna Parras, J.M. Influencia de las enfermeras gestoras de casos en la calidad de vida de las cuidadoras de pacientes pluripatológicos. Gerokomos 2014, 25, 68–71. [Google Scholar] [CrossRef]
- U.S. National Library of Medicine (NIH). Medical Subject Headings (MeSH). 2019. Available online: https://meshb.nlm.nih.gov/search (accessed on 20 August 2020).
- Centro Latinoamericano y del Caribe de Información en Ciencias de la Salud (BIREME). Descriptores en Ciencias de la Salud (DeCS). 2018. Available online: http://decs.bvs.br/E/homepagee.htm (accessed on 10 September 2020).
- Critical Appraisal Skills Programme Español (CASPe). 2018. Available online: http://www.redcaspe.org/ (accessed on 11 September 2020).
- Altman, D.G.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. Declaración de la iniciativa STROBE (Strengthening the Reporting of Observational studies in Epidemiology): Directrices para la comunicación de estudios observacionales. Revisit. Esp. Salud Pública 2008, 22, 144–150. Available online: http://www.ee.lafe.san.gva.es/aulavirtual/file.php/95/CURSO_2017-2018/STROBE_short_Spanish.pdf (accessed on 20 August 2020).
- Scottish Intercollegiate Guidelines Network. Forming guideline recommendations. In SIGN 50: A Guideline Developer’s Handbook; SIGN: Edinburgh, Scotland, 2008; Available online: https://www.sign.ac.uk/assets/sign50_2011.pdf (accessed on 22 August 2020).
- López Vallejo, M.; Puente Alcaraz, J. El proceso de institucionalización de la enfermera gestora de casos en España. Análisis comparativo entre los sistemas autonómicos de salud. Enferm. Clinic 2019, 29, 107–118. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Gómez, M.B.; Ramos-Santana, S.; Gómez-Salgado, J.; Sánchez-Nicolás, F.; Moreno-Garriga, C.; Duarte-Clíments, G. Benefits of advanced practice nursing for its expansion in the Spanish context. Int. J. Environ. Res. Public Health 2019, 16, 680. [Google Scholar] [CrossRef] [PubMed]
- Joo, J.Y.; Huber, D.L. Scoping Review of Nursing Case Management in the United States. Clin. Nurs. Res. 2017, 27, 1002–1016. [Google Scholar] [CrossRef] [PubMed]
- Reilly, S.; Miranda-Castillo, C.; Malouf, R.; Hoe, J.; Toot, S.; Challis, D.; Orrell, M. Case management approaches to home support for people with dementia. Cochrane Database Syst. Rev. 2015. [Google Scholar] [CrossRef]
- Joo, J.Y.; Liu, M.F. Case management effectiveness in reducing hospital use: A systematic review. Int. Nurs. 2016, 64, 296–308. [Google Scholar] [CrossRef]
- Joo, J.Y.; Huber, D.L. Community-based case management effectiveness in populations that abuse substances. Int. Nurs. Rev. 2015, 62, 536–545. [Google Scholar] [CrossRef]
- Stokes, J.; Panagioti, M.; Alam, R.; Checkland, K.; Cheraghi-Sohi, S.; Bower, P. Effectiveness of case management for “At Risk” patients in PHC: A systematic review and meta-analysis. PLoS ONE 2015, 10, e0132340. [Google Scholar] [CrossRef]
- Morales-Asencio, J.M.; Cuevas-Fernández-Gallego, M.; Morilla-Herrera, J.C.; Martín-Santos, F.J.; Silvano Arranz, A.; Batres Sicilia, J.P.; Delgado-Romero, A.; Palacios-Gómez, L.; Cejudo López, Á.; Kaknani-Uttumchandani, S. Características de la provisión del servicio de gestión de casos en el entorno comunitario en Andalucía a partir del registro RANGECOM. Enferm. Clin. 2019, 29, 67–73. [Google Scholar] [CrossRef]
- Tortajada, S.; Giménez-Campos, M.S.; Villar-López, J.; Faubel-Cava, R.; Donat-Castelló, L.; Valdivieso-Martínez, B.; Soriano-Melchor, E.; Bahamontes-Mulió, A.; García-Gómez, J.M. Case Management for Patients with Complex Multimorbidity: Development and Validation of a Coordinated Intervention Between Primary and Hospital Care. Int. J. Integr. Care 2017, 17, 4. [Google Scholar] [CrossRef]
- Castanho, R.; Mantovani, M.D.; Soriano, J. Nursing Case Management and Glycemic Control Among Brazilians with Type 2 Diabetes: Pragmatic Clinical Trial. Nurs. Res. 2015, 64, 272–281. [Google Scholar] [CrossRef]
- Ozpancar, N.; Pakyuz, S.C.; Topcu, B. Hypertension management: What is the role of case management? Rev. Esc. Enferm. USP 2017, 51, e03291. [Google Scholar] [CrossRef] [PubMed]
- Oh, J.; Oh, S. Nurse Case Managers’ Experiences on Case Management for Long-term Hospitalization in Korea. Asian Nurs. Res. 2017, 11, 283–289. [Google Scholar] [CrossRef] [PubMed]
- Scherlowski Leal David, H.M.; Martínez-Riera, J.R.; Herraiz Mallebrera, A.; de Lima da Costa, M.F. A enfermeira gestora de casos na Espanha: Enfrentando o desafio da cronicidade por meio de uma prática integral. Ciênc. Saúde Coletiva 2020, 25, 315–324. [Google Scholar] [CrossRef] [PubMed]
- Burgel, B.J.; Devito, B.; Collins-Bride, G.; Sullivan, B.; Retzlaff, A.; Hyde, S. Nursing Case Management Strategies for Adults with Serious Mental Illness Seeking Dental Services. Issues Ment. Health Nurs. 2018, 39, 311–319. [Google Scholar] [CrossRef]
- Davisson, E.A.; Swanson, E.A. Patient and Nurse Experiences in a Rural Chronic Disease Management Program: A qualitative evaluation. Prof. Case Manag. 2018, 23, 10–18. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).