Abstract
Bioactive agents can stimulate osteogenesis, angiogenesis, and cell proliferation; therefore, their application in bone regeneration offers significant therapeutic potential. The aim of this systematic review was to evaluate strategies for applying chitosan-based scaffolds with growth factors in bone regeneration. A structured literature search was conducted in July 2025 across the PubMed, Scopus, and Web of Science databases. Search terms included combinations of (chitosan scaffold) AND (growth factor OR BMP-2 OR VEGF OR FGF OR TGF-beta OR periostin OR PDGF OR IGF-1 OR EGF OR ANG-1 OR ANG-2 OR GDF-5 OR SDF-1 OR osteopontin). The study selection process followed PRISMA 2020 guidelines and the PICO framework. Out of 367 records, 226 were screened, and 17 studies met the eligibility criteria for qualitative analysis. BMP-2 was the most frequently investigated growth factor, studied in both in vitro and in vivo models, with rats and rabbits as the most common animal models. Scaffold compositions varied, incorporating hydroxyapatite, heparin, polyethylene glycol diacrylate, octacalcium phosphate-mineralized graphene, silk fibroin, and aloe vera. Growth factors were introduced using diverse methods, including microspheres, chemical grafting, covalent coupling, protein carriers, and nanohydroxyapatite mesopores. Most studies reported enhanced bone regeneration, although differences in models, scaffold composition, and delivery methods preclude definitive conclusions. The addition of growth factors generally improved osteoblast proliferation, angiogenesis, bone density, and expression of osteogenic markers (RunX2, COL1, OPN, OCN). Combining two bioactive agents further amplified osteoinduction and vascularization. Sustained-release systems, particularly those using heparin or hydroxyapatite, prolonged biological activity and improved regenerative outcomes. In conclusion, functionalization of chitosan-based scaffolds with growth factors shows promising potential for bone regeneration. Controlled-release systems and combinations of different bioactive molecules may offer synergistic effects on osteogenesis and angiogenesis. Further research should focus on optimizing scaffold compositions and delivery methods to tailor bioactive agent release for specific clinical applications.
1. Introduction
Bone regeneration remains a major clinical challenge, particularly in critical-sized defects (>2 cm) resulting from severe trauma, oncological resection, osteomyelitis, or congenital anomalies, where endogenous healing alone cannot restore tissue continuity [1,2,3,4,5,6,7,8]. Conventional treatments, such as autologous, allogeneic, or xenogeneic bone grafts, face substantial limitations, including donor-site morbidity, limited availability, immunogenic reactions, and infection risk [2,3,9,10,11,12]. Although synthetic bone substitutes are standardized and commonly available, they often lack the hierarchical structure and essential bioactivity required for complete tissue regeneration [1,13,14,15,16,17,18,19,20]. Moreover, large bone defects are frequently characterized by insufficient vascularization and poor recruitment of osteoprogenitor cells, further inhibiting the repair process [2,9,11]. These challenges underscore the need for precision-engineered biomaterials that closely mimic extracellular matrix architecture, promote both angiogenesis and osteogenesis, and enable controlled delivery of bioactive agents. Multidisciplinary strategies that integrate advanced scaffold design, growth factor-based release systems, and recruitment of endogenous stem cells or progenitor cells are therefore essential to overcome current clinical barriers and achieve functional bone regeneration [2].
Chitosan is a linear polysaccharide derived from chitin. It consists of deacetylated units (β-1,4-D-glucosamine) and residual acetylated units (2-acetamido-2-deoxy-β-D-glucose). It exhibits excellent biocompatibility, biodegradability, antimicrobial properties, and strong support for cell adhesion and proliferation, making it one of the most extensively investigated scaffold materials in bone tissue engineering [3,13,21,22,23,24,25,26,27,28,29,30,31]. However, unmodified chitosan lacks osteoinductive properties, which cause the need for functionalization strategies to promote bone formation in situ [32]. Chemical modifications such as phosphorylation or sulfation enhance BMP-2 binding and stimulate osteogenic differentiation of mesenchymal stem cells [2,13,33]. Composite scaffolds that integrate chitosan with inorganic nanomaterials—including nanohydroxyapatite, bioactive glass, or graphene oxide—have been shown to improve mechanical strength, support mineralization, and increase bone volume in critical-sized defect animal models [1,34,35,36,37,38]. Moreover, chitosan-based biomaterials influence the immune microenvironment by modulating macrophage polarization toward a pro-regenerative M2 phenotype, thereby accelerating bone repair [21,39,40,41]. Collectively, while chitosan represents a comprehensive scaffold platform, its full regenerative potential is achieved through synergistic combination with osteoinductive agents, mineral reinforcements, and immunomodulatory design [13,21,22,26,42] (Figure 1).
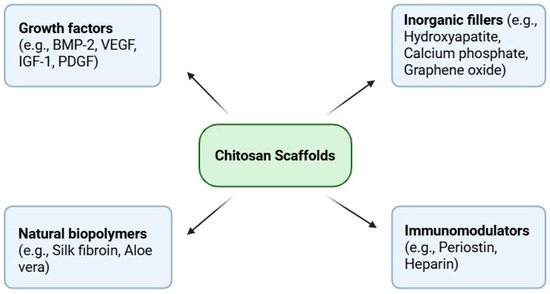
Figure 1.
Representative categories of bioactive agents incorporated into chitosan-based scaffolds for bone regeneration, including growth factors, inorganic fillers, natural biopolymers, and immunomodulators.
The functionalization of chitosan scaffolds is a rational design strategy aimed at enhancing their biological performance by incorporating growth factors into the scaffold structure. The choice of bioactive agent—such as BMP-2, BMP-6, VEGF, PDGF, IGF-1, or bFGF—depends on the intended therapeutic outcome, whether to stimulate osteogenesis, promote angiogenesis, or enhance cellular proliferation [43,44,45,46,47,48] (see Figure 2). Equally important is the method of incorporation, which directly influences release kinetics and biological activity [49,50]. Chemical grafting (e.g., P24 from BMP-2 onto CS–HA scaffolds [51]) and covalent coupling (BMP-2 linked to PEG diacrylate–CS scaffolds [52,53]) support strong cell adhesion, proliferation, and matrix deposition. Encapsulation in microspheres (e.g., BMP-2/VEGF in PLGA [54] or BMP-6 in alginate microspheres [55]) enhances osteogenesis, calcification, and cell proliferation. Surface adsorption (periostin on genipin–crosslinked CS [56]) increases osteocyte density, bone volume, and collagen fiber content, while also accelerating regeneration under unloaded conditions [57,58,59,60,61]. Immobilization on heparinized scaffolds (BMP-2 on Hep–CS [62,63]) prolongs factor release (up to 28 days) and significantly increases ALP activity, mineralization, and osteogenic gene expression [64,65,66,67,68,69,70,71,72,73]. Importantly, dual-factor systems such as BMP-2 combined with VEGF or PDGF have demonstrated synergistic effects, resulting in faster defect filling, greater bone volume, and more organized collagen deposition. The highest new bone area ratio (23.6%) was achieved with implanted scaffolds containing BMP-2 + VEGF. When the scaffold contained only BMP-2, this figure was 18.8% [74]. Thus, both the choice of bioactive agent and the method of incorporation can be adjusted to the specific requirements of the defect site and the desired regenerative timeline [75] (Table 1).
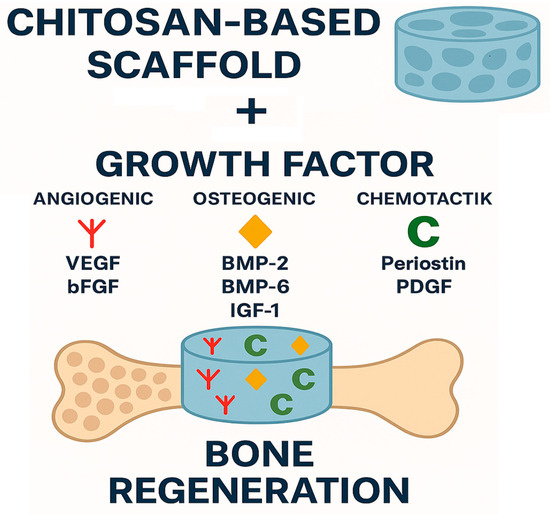
Figure 2.
Schematic representation of bone regeneration using a chitosan-based scaffold combined with growth factors. A porous chitosan scaffold serves as the carrier for three categories of growth factors: angiogenic (VEGF, bFGF), osteogenic (BMP-2, BMP-6, IGF-1), and chemotactic (periostin, PDGF). Their combined action enhances vascularization, cell recruitment, and osteogenesis, thereby promoting effective bone regeneration.

Table 1.
Bioactive factors used in chitosan-based scaffolds, their biological role, and functionalization strategies.
This systematic review aims to comprehensively evaluate strategies for application of chitosan-based scaffolds with growth factors for bone regeneration. Owing to its biocompatibility, biodegradability, and structural similarity to glycosaminoglycans, chitosan has attracted considerable interest as a comprehensive biomaterial in bone tissue engineering. Nevertheless, chitosan scaffolds often require functional enhancement through the incorporation of bioactive agents to address the complex biological and mechanical demands of bone repair [86]. Such functionalization improves osteoinductivity, osteoconductivity, and the overall regenerative performance of chitosan-based scaffolds [87]. Although numerous experimental studies describe various functionalization approaches, the literature lacks a systematic comparison of these methods, their mechanisms, and their quantitative effects on scaffold performance. A detailed assessment of factors influencing functionalization efficiency—including agent type, loading technique, release kinetics, and interactions with the chitosan matrix—is crucial for understanding their clinical potential and limitations. By consolidating and critically analyzing available evidence, this review aims to identify the most effective strategies and highlight existing knowledge gaps. This evidence-based synthesis may indicate the possibilities for design next-generation scaffolds and accelerate the translation of chitosan-based biomaterials into predictable and clinically effective solutions for bone regeneration.
2. Results
2.1. Study Selection
The initial database search across PubMed, Scopus, and Web of Science identified 367 potentially relevant records. After removal of duplicates, 226 unique articles remained for screening. Title and abstract screening led to the exclusion of 196 articles that did not investigate chitosan-based scaffolds functionalized with growth factors for bone regeneration. Of the 30 articles assessed in full text, 7 could not be retrieved, 1 was available only in Chinese, and 5 did not meet the predefined inclusion criteria. Ultimately, 17 studies fulfilled the eligibility requirements and were included in the qualitative synthesis. A meta-analysis was not feasible due to substantial heterogeneity among the included studies in terms of experimental design (animal models, defect sizes, follow-up duration), scaffold composition (crosslinking methods, composite materials), types and dosages of growth factors, as well as outcome measures (release kinetics, histological scoring systems, imaging modalities).
2.2. General Characteristics of the Included Studies
The most frequently investigated growth factor was BMP-2, reported in 10 studies [51,52,54,62,63,76,77,78,79,80], of which seven were conducted in vivo [51,54,76,77,78,79,80]. Four studies used rat models [54,76,79,80], while three employed rabbits [62,77,78]. Scaffold compositions varied considerably: hydroxyapatite was combined with chitosan in three studies [51,62,79], and heparin in two [62,63]. Other modifications included polyethylene glycol diacrylate [13], octacalcium phosphate–mineralized graphene [80], Aloe vera [82], and calcium phosphate salts (CPS) introduced via the ISISA process [78].
Incorporation methods for BMP-2 also differed. In heparin-containing scaffolds, BMP-2 was chemically immobilized [62,63]. Alternative strategies included microspheres [54], co-incorporation into chitosan gel [76], grafting of the P24 peptide derived from BMP-2 [51], covalent coupling [52], immobilization with CPS and ISISA processing [78], encapsulation in bovine serum albumin nanoparticles [80], and preloading into mesoporous hydroxyapatite nanoparticles (mHANPs) [79]. One study also investigated IGF-1 in combination with BMP-2 [77].
Two studies examined BMP-6 in vitro, delivered either via alginate microspheres [55] or PHBV submicron particles [81]. VEGF was studied in four investigations [54,82,83,84], three of which employed microsphere-based delivery [54,83,84]. Three of these were in vivo studies, two in rabbits [54,84] and one in guinea pigs (Cavia cobaya) [82]. De la Riva et al. [84] also explored PDGF by dissolving it in the aqueous phase of brushite and embedding VEGF in alginate microspheres. In vitro evaluation of bFGF in chitosan–hydroxyapatite scaffolds was reported by Tigli et al. [85], while Barakzai et al. [56] investigated periostin within genipin-crosslinked chitosan scaffolds in a rat model.
To enable comparative evaluation, many studies employed multiple outcome assessment methods. Computed tomography was reported in five studies [51,52,54,56,78], and X-rays in two [77,79]. Histological examination was the most common technique, performed in nine studies [51,54,56,76,77,78,79,80,84]. Eleven studies measured ALP activity [51,52,54,55,56,62,63,78,79,80,83], while calcium deposition was assessed in six [51,54,62,63,79,81]. ELISA testing was conducted in three studies [63,76,78]. In addition, Tigli et al. [85] uniquely analyzed fluorescence and release kinetics (Table 2).

Table 2.
General characteristics of the included studies.
2.3. Main Study Outcomes
2.3.1. Histological and Imaging Outcomes
Histological and imaging analyses consistently demonstrated improved bone regeneration in functionalized scaffolds. Sanjaya et al. [76] observed a higher proportion of woven bone and more osteoblasts in rat calvarial defects treated with BMP-2 + chitosan compared to single-component groups. Nandi et al. [77] reported denser bone tissue, accelerated healing, and earlier appearance of Haversian systems in rabbit tibiae treated with IGF-1 or BMP-2. Wang et al. [54] achieved complete filling of mandibular bone defects in rabbits within 12 weeks using BMP-2 + VEGF in microspheres with ADSCs. Guzman et al. [78] demonstrated enhanced trabecular bone formation in rabbit tibiae with BMP-2 + CPS scaffolds processed by ISISA. Barakzai et al. [56] showed greater bone volume and collagen deposition in periostin-functionalized scaffolds under non-weight-bearing conditions. Xie et al. [80] and Qiu et al. [79] confirmed that BMP-2-functionalized chitosan composites significantly enhanced bone formation in rat cranial defects.
2.3.2. Enzymatic Activity (ALP, OCN, PDGF, ELISA)
Multiple studies reported elevated enzymatic markers of osteogenesis. Sanjaya et al. [76] observed significantly higher osteocalcin (OCN) and PDGF levels in BMP-2 + chitosan scaffolds. Yun et al. [62,63] demonstrated that heparinized scaffolds prolonged BMP-2 release and significantly increased ALP activity, calcium deposition, and osteogenic gene expression. Chen et al. [51] confirmed that P24 peptide–grafted scaffolds enhanced ALP and mineralization in vitro and in vivo. Soriente et al. [52] reported higher ALP and OCN levels in BMP-2–functionalized CS-PEG scaffolds. Soran et al. [55] and Demirtaş et al. [81] also observed higher ALP activity and calcification in BMP-6–functionalized scaffolds, particularly when dual factors were used.
2.3.3. Gene Expression of Osteogenic Markers
Several studies reported upregulation of osteogenic genes in functionalized scaffolds. Demirtaş et al. [81] observed increased expression of RunX2, Col1, OPN, and OCN with dual delivery of PDGF-BB and BMP-6. Liu et al. [83] showed that VEGF-functionalized HA/SA/CS scaffolds enhanced expression of ALP, BMP2, OPN, and RunX2. Qiu et al. [79] demonstrated upregulation of RunX2, ALP, Col1, and OCN in BMP-2–loaded silk fibroin–chitosan scaffolds. Yun [63] reported higher expression of osteocalcin and osteopontin in BMP-2/heparinized scaffolds compared to controls.
2.3.4. Mineralization and Calcium Deposition
Functionalized scaffolds were consistently associated with enhanced mineralization. Soran et al. [55] observed greater calcification in BMP-6–loaded alginate microspheres compared to free BMP-6. Chen et al. [51], Soriente et al. [52], and Yun et al. [62] confirmed improved calcium deposition in BMP-2 and P24-functionalized scaffolds. Demirtaş et al. [81] reported early calcium deposits within 7 days in dual-loaded scaffolds, while Liu et al. [83] showed stronger Alizarin Red staining in VEGF-loaded scaffolds. Tigli et al. [85] indirectly linked hydroxyapatite addition to extended growth factor release and improved mineralization potential.
2.3.5. Cell Proliferation and Morphology
Functionalized scaffolds enhanced cell adhesion, proliferation, and morphology. Sanjaya et al. [76] and Nandi et al. [77] reported higher osteoblast counts in BMP-2 and IGF-1 groups. Chen et al. [51] and Soriente et al. [52] observed increased BMSC and hMSC proliferation with P24 and BMP-2–modified scaffolds. Liu et al. [83] demonstrated greater MSC adhesion and proliferation in VEGF-functionalized scaffolds. Demirtaş et al. [81] confirmed improved spreading and cell–cell interactions in dual-factor scaffolds. Xie et al. [80] reported enhanced BMSC proliferation and osteogenic differentiation with BMP-2-loaded nanoparticles, while Qiu et al. [79] found increased BMSC attachment and matrix production. Guzman et al. [78] observed higher proliferation of C2C12 myoblasts in BMP-2 + CPS scaffolds. Barakzai et al. [56] additionally confirmed greater osteocyte density and viability in periostin-coated scaffolds.
2.3.6. Angiogenesis and VEGF Expression
Angiogenesis was significantly improved in dual- and VEGF-containing systems. Wang et al. [54] showed that BMP-2 + VEGF synergistically promoted osteogenesis and angiogenesis, leading to rapid defect repair. De la Riva et al. [84] found that PDGF enhanced early bone formation, VEGF supported later-stage regeneration, and the combination yielded the largest trabecular area and multilayered osteoblasts. Sularsih et al. [82] demonstrated significantly higher VEGF expression and woven bone formation with chitosan–Aloe vera scaffolds. Nandi et al. [77] also observed intensified angiogenesis in GF-treated groups.
2.3.7. Release Kinetics and Delivery Strategies
Several studies highlighted the importance of delivery strategies in prolonging growth factor activity. Yun et al. [62] demonstrated sustained BMP-2 release up to 28 days with heparinized scaffolds. Tigli et al. [85] showed that hydroxyapatite extended bFGF release from 10 to 20 h to 7 days. Chen et al. [51] reported stable release of the P24 peptide for 90 days. Guzman et al. [78] achieved controlled release of BMP-2 from CPS-modified scaffolds, enhancing long-term osteoinduction. Xie et al. [80] encapsulated BMP-2 in BSA nanoparticles, achieving sustained release and improved bioactivity. Qiu et al. [79] confirmed slower BMP-2 release and higher retention with mHANPs. De la Riva et al. [84] demonstrated a rapid, initial release of PDGF (approximately 45% in the first 24 h) and a more controlled release of VEGF (~13% in the first 24 h, ~64% within 3 weeks), which allowed for the sequential activation of proliferation and angiogenesis. In the study by Demirtaş et al. [81], the system provided almost complete release of PDGF-BB within 14 days (~90%) and a slower, partial release of BMP-6 (~50% in 14 days), reflecting the natural sequence of bone healing processes. Nandi et al. [77], on the other hand, did not perform classical in vitro studies, but described the gradual release of IGF-1 and BMP-2 in vivo as a result of enzymatic degradation of chitosan. In the work of Wang et al. [54], a rapid burst release within 10 days (66.8% BMP-2 and 65.2% VEGF) was reported, followed by a stable release phase up to 28 days, while maintaining the bioactivity of the released proteins (see Table 3).

Table 3.
Detailed characteristics of included studies.
2.4. Quality Assessment
For all of the nine questions, 14 papers received a positive answer to nine of them [51,52,54,55,56,62,63,77,78,79,81,82,83,85] and 3 papers received a positive answer to eight of them [76,80,84] (see Table 4).

Table 4.
Quality assessment—JBI checklist for quasi-experimental studies (nonrandomized experimental studies).
2.5. Risk of Bias in Included Studies
The risk of bias for each included study was assessed using the Joanna Briggs Institute (JBI) checklist for quasi-experimental designs (non-randomized studies). Fourteen studies fulfilled all nine quality criteria, while three fulfilled eight. The most frequent limitations were the absence of long-term follow-up or incomplete reporting of blinding procedures. Despite these shortcomings, the overall methodological quality of the included studies was high, and the risk of bias was considered low to moderate. Table 4 provides a detailed summary of the assessment for each study.
2.6. Reporting Biases
We also evaluated the potential for reporting biases, particularly selective outcome reporting and publication bias. Although no clear evidence of selective reporting was identified in the included studies, the limited number of papers (n = 17) and the heterogeneity of outcome measures suggest that some degree of reporting bias may still be present. Furthermore, negative or inconclusive findings may be underrepresented in the available literature. As quantitative synthesis (meta-analysis) was not feasible, statistical tools such as funnel plots or Egger’s test could not be applied. To minimize such biases in future research, broader search strategies, inclusion of gray literature, and preregistration of study protocols are recommended.
3. Discussion
This systematic review aimed to comprehensively evaluate strategies for applying chitosan-based scaffolds with growth factors for bone regeneration. Among the 17 included studies, BMP-2 [88] was the most frequently investigated growth factor, while VEGF [54,82,83,84,89], BMP-6 [55,81,90], IGF-1 [77], PDGF [81,84], bFGF [85], periostin [56], and the BMP-2–derived P24 peptide [51] were also studied. Several works combined chitosan with additional scaffold components, including hydroxyapatite [51,54,79,91,92], heparin [62,63,93], polyethylene glycol diacrylate [52], graphene mineralized with octacalcium phosphate [80], genipin [56], Aloe vera [82,94], calcium phosphate salts [78], and silk fibroin [80]. Bone regeneration outcomes were assessed using computer tomography in five studies [51,52,54,56,78], X-ray imaging in two [77,79], and histological examination in nine [51,54,56,76,77,78,79,80,84]. Eleven studies measured ALP activity [51,52,54,55,56,62,63,78,79,80,83], and six reported calcium deposition [51,54,62,63,79,81]. ELISA testing was performed in three studies [63,76,78]. Overall, all studies confirmed that functionalization of chitosan with bioactive agents enhanced osteogenesis. The addition of BMP-2, VEGF, or IGF-1 accelerated bone formation and angiogenesis [54,76,77,82]. Increased osteocalcin levels, osteoblast counts, osteoinduction, and cell proliferation were consistently reported after incorporation of BMP-2, PDGF, VEGF, or BMP-6 [76,78,81,84,95]. Dual delivery of BMP-6 and PDGF-BB further upregulated RunX2, Col1, OPN, and OCN expression [81]. Scaffold modifications such as heparinization or hydroxyapatite addition enabled prolonged release of growth factors, sustaining their biological activity [3,8]. Importantly, the delivery strategy determined efficacy: BMP-6 encapsulated in alginate microspheres produced significantly greater osteogenesis than free BMP-6 [55].
The application of chitosan-based scaffolds combined with growth factors is considered one of the most promising strategies to enhance bone regeneration [96,97]. Numerous experimental studies have shown that such systems not only promote osteoproliferation but also significantly increase osteogenic gene expression (RunX2, Col1, OPN, OCN), ALP activity, and matrix mineralization [51,52,55,62,76,79,80,81,83,98]. The majority of findings suggest that chitosan scaffolds actively contribute to creating a biologically favorable microenvironment for bone repair [99,100]. This effect is achieved through the interaction between scaffold architecture, cellular adhesion, and the sustained release of growth factors [101,102]. The combination of these factors results in enhanced cell proliferation and more efficient osteoblast differentiation [84,103]. The ability to stimulate early-stage cell activity appears particularly important in accelerating the healing of bone defects and may ultimately reduce the time required for functional recovery in clinical practice [104]. In this context, chitosan-based composites demonstrate potential not only as osteoconductive scaffolds but also as bioactive materials capable of supporting the multiple mechanisms involved in bone repair [105,106].
In the reviewed studies, the density and quality of newly formed bone tissue were consistently enhanced when growth factors were incorporated into chitosan scaffolds. Particularly notable were dual growth factor systems, such as PDGF-BB + BMP-6 [81]. PDGF-BB strongly increased osteoblast proliferation, BMP-6 promoted differentiation, while their combination induced a synergistic effect, particularly visible in mineralization and osteocalcin expression. Similarly, Wang et al. [54] reported that after 12 weeks, the BMP-2 and BMP-2/VEGF groups achieved more than 86% new bone, but only the combination produced tissue density (CT ~1623 HU) close to normal and improved lamellar remodeling, while VEGF alone had a moderate effect (12.9% NB). De la Riva et al. [84] showed a significant increase in the new bone area in the PDGF group (0.82 mm2) and especially in the PDGF + VEGF group (1.74 mm2) compared to the control (0.12 mm2), which corresponded to an improvement of up to 14-fold. Sularsih et al. [82] further confirmed that VEGF-functionalized scaffolds promoted both neovascularization and dense bone fibrosis. Collectively, these outcomes indicate that scaffold modifications not only stimulate osteogenesis but also promote angiogenesis, thereby ensuring adequate vascularization and nutrient supply for developing bone. This dual action supports the transition from immature woven bone to compact, functionally stable structures [106,107]. The observed synergy suggests that carefully designed scaffold systems can provide superior regenerative outcomes, particularly in large or complex defects where spontaneous repair is insufficient. Moreover, the simultaneous stimulation of osteogenesis and angiogenesis may play a decisive role in reducing the risk of non-union and improving the long-term biomechanical performance of regenerated bone [108,109].
Another vital aspect of scaffold performance is the sustained and controlled release of growth factors, which has been extensively investigated in experimental studies [110,111,112]. Scaffold modifications such as the incorporation of hydroxyapatite, heparin, or immobilized calcium phosphate salts have been shown to prolong release kinetics from only a few hours to several days or even weeks [62,78,85]. Similarly, encapsulation strategies using microspheres or nanoparticles (e.g., BMP-2 or VEGF in PLGA microspheres [54,84,113], BMP-6 in alginate microspheres [55], or BMP-6 in PHBV submicron particles [81]) provided gradual and extended release profiles, maintaining factor bioactivity over time. This prolonged availability ensures that osteogenic stimulation persists not only in the early stages of healing following implantation but also during later phases of bone maturation [114,115]. A continuous supply of bioactive agents supports cell proliferation, differentiation, and extracellular matrix deposition. When combined with dual delivery systems [54,77,81,84], controlled release further enhances both osteogenesis and angiogenesis, producing superior regenerative outcomes. From a clinical perspective, scaffold systems with controlled and sustained release may offer a more effective and predictable approach to bone defect repair by ensuring long-term biological activity, enhanced tissue integration, and improved biomechanical stability of regenerated bone. Importantly, the capacity to modulate release kinetics provides opportunities to tailor scaffold design to specific clinical scenarios, ranging from small defects to critical-sized bone injuries.
This systematic review has several limitations that should be acknowledged. First, the number of eligible studies was relatively small (n = 17), and most were preclinical investigations conducted in rodents or rabbits, which restricts the direct translation of findings to humans. Considerable heterogeneity was observed in scaffold composition, methods of growth factor incorporation, dosing strategies, and outcome measurements, which precluded the possibility of conducting a meta-analysis. Moreover, many studies had short follow-up periods, limiting insights into long-term scaffold performance and potential adverse effects, such as ectopic bone formation or uncontrolled release of bioactive agents. Publication bias cannot be ruled out, as negative or inconclusive results may be underreported. Future research should focus on standardized experimental protocols that would allow for meaningful comparisons across studies, including harmonized dosing strategies, release kinetics assessment, and outcome measures. Large-animal models that better replicate the biomechanical and biological environment of human bone defects are needed before clinical translation. Clinical trials will be necessary to validate both the safety and efficacy of functionalized chitosan scaffolds, with particular emphasis on critical-sized defects and load-bearing sites. Furthermore, advanced scaffold designs combining multiple growth factors with immunomodulatory strategies or stem/progenitor cell delivery may offer synergistic effects and should be explored [116]. Ultimately, translational studies integrating bioengineering, molecular biology, and clinical expertise will be essential to optimize scaffold performance and accelerate their application in routine clinical practice.
4. Materials and Methods
4.1. Focused Question:
This systematic review was designed according to the PICO framework [117]:
Population (P): experimental models using chitosan-based scaffolds for bone regeneration,
Intervention (I): functionalization of chitosan scaffolds with growth factors,
Comparator (C): non-functionalized chitosan scaffolds (without growth factors),
Outcome (O): enhancement of bone regeneration, assessed by histological, radiological, biochemical, or molecular parameters.
The focused review question was: does the incorporation of growth factors into chitosan-based scaffolds improve bone regeneration compared with non-functionalized chitosan scaffolds?
4.2. Protocol
The selection process for articles in the systematic review was carefully outlined following the PRISMA flow diagram (Figure 3) [118]. The systematic review was registered on the Open Science Framework under the following link: https://osf.io/zhdm8 (accessed on 23 August 2025).
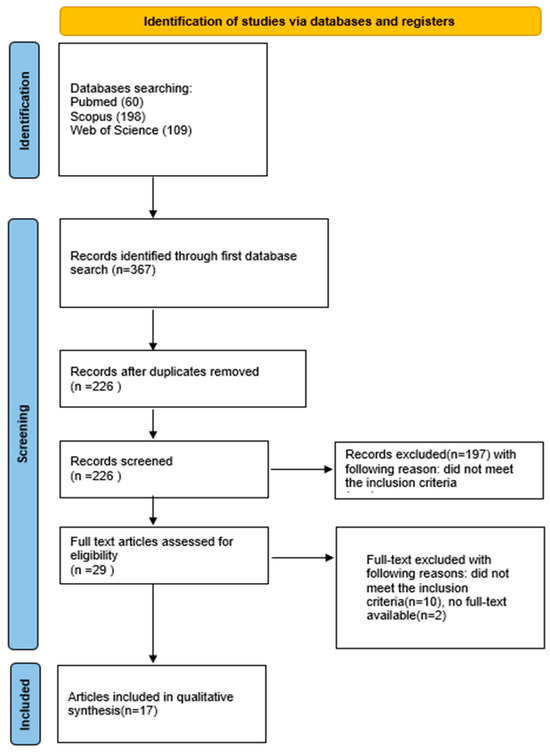
Figure 3.
PRISMA 2020 flow diagram.
4.3. Eligibility Criteria
Studies were considered acceptable for inclusion in the review if they met the following criteria [119,120,121,122,123,124,125,126,127]:
Inclusion criteria:
- Studies examining the effect of adding growth factors to chitosan scaffolds on bone regeneration.
- In vitro studies
- In vivo studies
- Studies with a control group;
- Studies in English;
- Non-randomized controlled clinical trials (NRS); and
- Randomized controlled clinical trials (RCT).
The exclusion criteria the reviewers agreed upon were as follows:
Studies not examining the effect of adding growth factors to chitosan scaffolds on bone regeneration [119,120,121,122,123,124,125,126,127].
- Non-English papers;
- Clinical reports;
- Opinions;
- Editorial papers;
- Review articles;
- No full-text accessible; or
- Duplicated publications.
No restrictions were applied with regard to the year of publication.
4.4. Information Sources, Search Strategy, and Study Selection
A comprehensive literature search was conducted in July 2025 across three electronic databases: PubMed, Scopus, and Web of Science (WoS). The search aimed to identify studies investigating the effect of growth factor incorporation into chitosan-based scaffolds for bone regeneration. Search terms combined the scaffold descriptor with individual growth factors and were applied to titles and abstracts only. The complete search strategies for each database are provided below:
PubMed: (“chitosan scaffold”[Title/Abstract]) AND (“growth factor”[Title/Abstract] OR “BMP-2”[Title/Abstract] OR “VEGF”[Title/Abstract] OR “FGF”[Title/Abstract] OR “TGF-beta”[Title/Abstract] OR “periostin”[Title/Abstract] OR “PDGF”[Title/Abstract] OR “IGF-1”[Title/Abstract] OR “EGF”[Title/Abstract] OR “ANG-1”[Title/Abstract] OR “ANG-2”[Title/Abstract] OR “GDF-5”[Title/Abstract] OR “SDF-1”[Title/Abstract] OR “osteopontin”[Title/Abstract])
Web of Science (WoS): TS = (“chitosan scaffold”) AND TS = (“growth factor” OR “BMP-2” OR “VEGF” OR “FGF” OR “TGF-beta” OR “periostin” OR “PDGF” OR “IGF-1” OR “EGF” OR “ANG-1” OR “ANG-2” OR “GDF-5” OR “SDF-1” OR “osteopontin”)
Scopus: TITLE-ABS-KEY(“chitosan scaffold”) AND TITLE-ABS-KEY(“growth factor” OR “BMP-2” OR “VEGF” OR “FGF” OR “TGF-beta” OR “periostin” OR “PDGF” OR “IGF-1” OR “EGF” OR “ANG-1” OR “ANG-2” OR “GDF-5” OR “SDF-1” OR “osteopontin”)
Following the database searches, all retrieved records were imported into a reference management system, and duplicates were removed. Two reviewers independently screened the remaining articles by title and abstract to exclude studies not meeting the inclusion criteria. Full-text articles were subsequently assessed for eligibility, with only those meeting all predefined criteria and available in full text included in the final qualitative synthesis.
4.5. Data Collection Process and, Data Items
Six reviewers (M.L., Z.N., J.K., S.K., M.M.) independently evaluated the identified publications to determine whether they fulfilled the inclusion requirements. From each eligible article, the following data were collected: name of the first author, year of publication, study design, article title, type of growth factor applied, and its reported influence on bone regeneration. All extracted information was organized and stored in a standardized Excel spreadsheet.
4.6. Risk of Bias and Quality Assessment
During the first stage of selection, titles and abstracts were independently assessed by all reviewers to reduce potential bias. Two blinded reviewers (J.M. and M.D.) independently evaluated the methodological quality of each included study using the Joanna Briggs Institute (JBI) checklist for quasi-experimental designs (non-randomized studies). This tool consists of nine targeted questions designed to assess study validity and reliability. In case of disagreement, issues were first discussed collectively, and inter-rater reliability was objectively quantified using Cohen’s kappa coefficient [128]. This ensured that the assessment process was both transparent and reproducible, and reduced the risk of subjective bias.
4.7. Quality Assessment
Two blinded reviewers (J.M. and M.D.) independently evaluated the methodological quality of each included study using the Joanna Briggs Institute (JBI) checklist for quasi-experimental designs (non-randomized studies) [129]. This assessment tool comprises nine targeted questions enables a reliable quality assessment, is methodologically recognized, enhances transparency and repeatability, and is consistent with international standards.
- Is it clear in the study what is the “cause” and what is the “effect”?
- Were the participants included in any similar comparisons?
- Were the participants included in any comparisons receiving similar treatment/care, other than the exposure or intervention of interest?
- Was there a control group?
- Were there multiple measurements of the outcome both before and after the intervention/exposure?
- Was a follow up completed, and if not, were the differences between groups in terms of their follow up adequately described and analyzed?
- Were the outcomes of the participants included in any comparisons measured in the same way?
- Were the outcomes measured in a reliable way?
- Was an appropriate statistical analysis used?
Each criterion on the checklist was rated as “yes,” “no,” “unclear,” or “not applicable.” Whenever reviewers assigned different responses, the inconsistencies were discussed until a consensus was reached. Inter-rater reliability was assessed using Cohen’s kappa, computed with MedCalc software (version 23.1.7; MedCalc Software Ltd., Brussels, Belgium). The resulting kappa value was 0.91 (p < 0.001), which corresponds to a high level of concordance and indicates almost perfect agreement among the reviewers.
5. Conclusions
This review demonstrates that the incorporation of growth factors into chitosan-based scaffolds significantly enhances bone regeneration compared with chitosan alone. Among them, BMP-2 remains the most extensively validated osteogenic mediator, consistently promoting osteoblast differentiation and mineralized matrix formation. Other factors, including BMP-6 and IGF-1, provided additional osteogenic stimulation through increased cell proliferation and metabolic activity, while VEGF primarily supported neovascularization. PDGF and bFGF contributed to extracellular matrix remodeling and fibroblast expansion, and periostin further enhanced collagen deposition and bone volume. Importantly, controlled-release strategies such as microsphere encapsulation, heparinization, and mineral-based binding prolonged the bioactivity of incorporated molecules, leading to more stable and predictable regenerative outcomes. Dual-factor systems, such as BMP-2 with VEGF or PDGF-BB with BMP-6, demonstrated synergistic effects by simultaneously stimulating osteogenesis and angiogenesis, thereby accelerating defect healing.
Altogether, the available evidence highlights functionalized chitosan–growth factor scaffolds as a promising bioactive material capable of improving both the quality and speed of bone healing. However, given the heterogeneity of study designs and the predominance of preclinical models, further standardized research and clinical trials are needed to validate their long-term safety, efficacy, and translational potential in the treatment of large and complex bone defects.
Author Contributions
Conceptualization, J.M. and M.D.; methodology, J.M. and M.M.; software, J.M., H.G. and S.S.; validation, J.M., J.K. and M.D.; formal analysis, J.M.; investigation, S.K., J.K., M.M., Z.M. and M.L.; resources, J.M.; data curation, H.G. and S.S.; writing—original draft preparation, S.K., J.K., M.M., Z.M. and M.L.; writing—review and editing, J.M.; visualization, Z.M., I.N.-H. and M.L.; supervision, M.D.; project administration, J.M.; funding acquisition, J.M. and M.D. All authors have read and agreed to the published version of the manuscript.
Funding
This work was financed by a subsidy from Wroclaw Medical University, number SUBZ.B180.25.091.
Institutional Review Board Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Guo, A.; Zheng, Y.; Zhong, Y.; Mo, S.; Fang, S. Effect of Chitosan/Inorganic Nanomaterial Scaffolds on Bone Regeneration and Related Influencing Factors in Animal Models: A Systematic Review. Front. Bioeng. Biotechnol. 2022, 10, 986212. [Google Scholar] [CrossRef]
- Zhao, Y.; Zhao, S.; Ma, Z.; Ding, C.; Chen, J.; Li, J. Chitosan-Based Scaffolds for Facilitated Endogenous Bone Re-Generation. Pharmaceuticals 2022, 15, 1023. [Google Scholar] [CrossRef]
- Piszko, P.J.; Piszko, A.; Kiryk, S.; Kiryk, J.; Horodniczy, T.; Struzik, N.; Wiśniewska, K.; Matys, J.; Dobrzyński, M. Bone Regeneration Capabilities of Scaffolds Containing Chitosan and Nanometric Hydroxyapatite—Systematic Review Based on In Vivo Examinations. Biomimetics 2024, 9, 503. [Google Scholar] [CrossRef]
- Annamalai, R.T.; Hong, X.; Schott, N.G.; Tiruchinapally, G.; Levi, B.; Stegemann, J.P. Injectable Osteogenic Microtissues Containing Mesenchymal Stromal Cells Conformally Fill and Repair Critical-Size Defects. Biomaterials 2019, 208, 32–44. [Google Scholar] [CrossRef]
- Huang, E.E.; Zhang, N.; Shen, H.; Li, X.; Maruyama, M.; Utsunomiya, T.; Gao, Q.; Guzman, R.A.; Goodman, S.B. Novel Techniques and Future Perspective for Investigating Critical-Size Bone Defects. Bioengineering 2022, 9, 171. [Google Scholar] [CrossRef] [PubMed]
- Nauth, A.; Schemitsch, E.; Norris, B.; Nollin, Z.; Watson, J.T. Critical-Size Bone Defects: Is There a Consensus for Diagnosis and Treatment? J. Orthop. Trauma 2018, 32 (Suppl. 1), S7–S11. [Google Scholar] [CrossRef] [PubMed]
- Roddy, E.; DeBaun, M.R.; Daoud-Gray, A.; Yang, Y.P.; Gardner, M.J. Treatment of Critical-Sized Bone Defects: Clinical and Tissue Engineering Perspectives. Eur. J. Orthop. Surg. Traumatol. 2018, 28, 351–362. [Google Scholar] [CrossRef] [PubMed]
- Schemitsch, E.H. Size Matters: Defining Critical in Bone Defect Size! J. Orthop. Trauma 2017, 31 (Suppl. 5), S20–S22. [Google Scholar] [CrossRef]
- Campana, V.; Milano, G.; Pagano, E.; Barba, M.; Cicione, C.; Salonna, G.; Lattanzi, W.; Logroscino, G. Bone Substitutes in Orthopaedic Surgery: From Basic Science to Clinical Practice. J. Mater. Sci. Mater. Med. 2014, 25, 2445–2461. [Google Scholar] [CrossRef]
- Shan, J.; Yu, Y.; Liu, X.; Chai, Y.; Wang, X.; Wen, G. Recent Advances of Chitosan-Based Composite Hydrogel Materials in Application of Bone Tissue Engineering. Heliyon 2024, 10, e37431. [Google Scholar] [CrossRef]
- Cheah, C.W.; Al-Namnam, N.M.; Lau, M.N.; Lim, G.S.; Raman, R.; Fairbairn, P.; Ngeow, W.C. Synthetic Material for Bone, Periodontal, and Dental Tissue Regeneration: Where Are We Now, and Where Are We Heading Next? Materials 2021, 14, 6123. [Google Scholar] [CrossRef]
- Xue, N.; Ding, X.; Huang, R.; Jiang, R.; Huang, H.; Pan, X.; Min, W.; Chen, J.; Duan, J.A.; Liu, P.; et al. Bone Tissue Engineering in the Treatment of Bone Defects. Pharmaceuticals 2022, 15, 879. [Google Scholar] [CrossRef]
- Rodríguez-Vázquez, M.; Vega-Ruiz, B.; Ramos-Zúñiga, R.; Saldaña-Koppel, D.A.; Quiñones-Olvera, L.F. Chitosan and Its Potential Use as a Scaffold for Tissue Engineering in Regenerative Medicine. Biomed. Res. Int. 2015, 2015, 821279. [Google Scholar] [CrossRef]
- Zhao, R.; Yang, R.; Cooper, P.R.; Khurshid, Z.; Shavandi, A.; Ratnayake, J. Bone Grafts and Substitutes in Dentistry: A Review of Current Trends and Developments. Molecules 2021, 26, 3007. [Google Scholar] [CrossRef]
- Tumedei, M.; Savadori, P.; Del Fabbro, M. Synthetic Blocks for Bone Regeneration: A Systematic Review and Meta-Analysis. Int. J. Mol. Sci. 2019, 20, 4221. [Google Scholar] [CrossRef] [PubMed]
- Barba, D.; Alabort, E.; Reed, R.C. Synthetic Bone: Design by Additive Manufacturing. Acta Biomater. 2019, 97, 637–656. [Google Scholar] [CrossRef]
- Zimmermann, G.; Moghaddam, A. Allograft Bone Matrix versus Synthetic Bone Graft Substitutes. Injury 2011, 42 (Suppl. S2), S16–S21. [Google Scholar] [CrossRef] [PubMed]
- Donnaloja, F.; Jacchetti, E.; Soncini, M.; Raimondi, M.T. Natural and Synthetic Polymers for Bone Scaffolds Optimization. Polymers 2020, 12, 905. [Google Scholar] [CrossRef]
- Valtanen, R.S.; Yang, Y.P.; Gurtner, G.C.; Maloney, W.J.; Lowenberg, D.W. Synthetic and Bone Tissue Engineering Graft Substitutes: What Is the Future? Injury 2021, 52 (Suppl. 2), S72–S77. [Google Scholar] [CrossRef] [PubMed]
- Ferraz, M.P. Bone Grafts in Dental Medicine: An Overview of Autografts, Allografts and Synthetic Materials. Materials 2023, 16, 4117. [Google Scholar] [CrossRef]
- Kim, Y.; Zharkinbekov, Z.; Raziyeva, K.; Tabyldiyeva, L.; Berikova, K.; Zhumagul, D.; Temirkhanova, K.; Saparov, A. Chitosan-Based Biomaterials for Tissue Regeneration. Pharmaceutics 2023, 15, 807. [Google Scholar] [CrossRef] [PubMed]
- Ressler, A. Chitosan-Based Biomaterials for Bone Tissue Engineering Applications: A Short Review. Polymers 2022, 14, 3430. [Google Scholar] [CrossRef]
- Saranya, N.; Moorthi, A.; Saravanan, S.; Devi, M.P.; Selvamurugan, N. Chitosan and Its Derivatives for Gene Delivery. Int. J. Biol. Macromol. 2011, 48, 234–238. [Google Scholar] [CrossRef]
- Sultankulov, B.; Berillo, D.; Sultankulova, K.; Tokay, T.; Saparov, A. Progress in the Development of Chitosan-Based Biomaterials for Tissue Engineering and Regenerative Medicine. Biomolecules 2019, 9, 470. [Google Scholar] [CrossRef]
- Oryan, A.; Sahvieh, S. Effectiveness of Chitosan Scaffold in Skin, Bone and Cartilage Healing. Int. J. Biol. Macromol. 2017, 104, 1003–1011. [Google Scholar] [CrossRef]
- Jangid, N.K.; Hada, D.; Rathore, K. Chitosan as an Emerging Object for Biological and Biomedical Applications. J. Polym. Eng. 2019, 39, 689–703. [Google Scholar] [CrossRef]
- Goldsztajn, K.; Godzierz, M.; Hercog, A.; Władowski, M.; Jaworska, J.; Jelonek, K.; Woźniak, A.; Kajzer, W.; Orłowska, A.; Szewczenko, J. Properties of Biodegradable Polymer Coatings with Hydroxyapatite on a Titanium Alloy Substrate. Acta Bioeng. Biomech. 2024, 26, 121–132. [Google Scholar] [CrossRef] [PubMed]
- Dobrzyński, W.; Piszko, P.J.; Kiryk, J.; Kiryk, S.; Michalak, M.; Kotela, A.; Kensy, J.; Świenc, W.; Grychowska, N.; Matys, J.; et al. Dental Resin Composites Modified with Chitosan: A Systematic Review. Mar. Drugs 2025, 23, 199. [Google Scholar] [CrossRef]
- Rucińska, K.; Osuchowska, E.; Dębek, C.; Krok-Borkowicz, M.; Pamuła, E. Antibacterial Properties of Elastomers Modified with Chitosan. Acta Bioeng. Biomech. 2024, 26, 13–23. [Google Scholar] [CrossRef]
- Saricam, E.; Altınışık, H.; Bulak, N.; Güven, B.; Yurdagül, S.Z.; Amasya, G. Effects of EDTA, Fumaric Acid, and the Chitosan Solutions Prepared with Distilled Water and Acetic Acid on Dentin Microhardness and Tubular Penetration: An in Vitro Study. Dent. Med. Probl. 2025, 62, 731–737. [Google Scholar] [CrossRef]
- Shalaby, H.A.; Soliman, N.K.; Al–Saudi, K.W. Antibacterial and Preventive Effects of Newly Developed Modified Nano-Chitosan/Glass-Ionomer Restoration on Simulated Initial Enamel Caries Lesions: An in Vitro Study. Dent. Med. Probl. 2024, 61, 353–362. [Google Scholar] [CrossRef]
- Makar, L.E.; Nady, N.; Abd El-Fattah, A.; Shawky, N.; Kandil, S.H. Unmodified Gum Arabic/Chitosan/Nanohydroxyapatite Nanocomposite Hydrogels as Potential Scaffolds for Bone Regeneration. Polymers 2022, 14, 3052. [Google Scholar] [CrossRef]
- Bombaldi de Souza, R.F.; Bombaldi de Souza, F.C.; Thorpe, A.; Mantovani, D.; Popat, K.C.; Moraes, Â.M. Phosphorylation of Chitosan to Improve Osteoinduction of Chitosan/Xanthan-Based Scaffolds for Periosteal Tissue Engineering. Int. J. Biol. Macromol. 2020, 143, 619–632. [Google Scholar] [CrossRef]
- Wiatrak, B.; Sobierajska, P.; Szandruk-Bender, M.; Jawien, P.; Janeczek, M.; Dobrzynski, M.; Pistor, P.; Szelag, A.; Wiglusz, R.J. Nanohydroxyapatite as a Biomaterial for Peripheral Nerve Regeneration after Mechanical Damage—In Vitro Study. Int. J. Mol. Sci. 2021, 22, 4454. [Google Scholar] [CrossRef] [PubMed]
- Zakrzewski, W.; Dobrzynski, M.; Nowicka, J.; Pajaczkowska, M.; Szymonowicz, M.; Targonska, S.; Sobierajska, P.; Wiglusz, K.; Dobrzynski, W.; Lubojanski, A.; et al. The Influence of Ozonated Olive Oil-Loaded and Copper-Doped Nanohydroxyapatites on Planktonic Forms of Microorganisms. Nanomaterials 2020, 10, 1997. [Google Scholar] [CrossRef] [PubMed]
- Zakrzewski, W.; Rybak, Z.; Pajączkowska, M.; Nowicka, J.; Szymonowicz, M.; Rusak, A.; Wiglusz, R.J.; Szyszka, K.; Chmielowiec, J.; Chodaczek, G.; et al. Antimicrobial Properties and Cytotoxic Effect Evaluation of Nanosized Hydroxyapatite and Fluorapatite Dedicated for Alveolar Bone Regeneration. Appl. Sci. 2024, 14, 7845. [Google Scholar] [CrossRef]
- Parfenova, L.V.; Galimshina, Z.R.; Parfenov, E.V. Organic-Inorganic Biocompatible Coatings for Temporary and Permanent Metal Implants. Int. J. Mol. Sci. 2024, 25, 11623. [Google Scholar] [CrossRef]
- Łukaszewska-Kuska, M.; Barylyak, A.; Bobitski, Y.; Piotr, K.; Buchwald, T.; Martyła, A.; Zinchenko, V.; Majchrowski, R.; Przekop, R.E.; Dorocka-Bobkowska, B. Electrodeposited Hydroxyapatite Coating on Titanium after Ultrashort-Pulsed Laser Processing for a Novel Surface of Endosseous Implants. Dent. Med. Probl. 2024, 61, 909–918. [Google Scholar] [CrossRef]
- Zhang, Y.; Chen, Z.H.; Zhao, K.; Mu, Y.D.; Li, K.L.; Yuan, Z.M.; Liu, Z.G.; Han, L.; Lü, W.D. Acellular Embryoid Body and Hydroxybutyl Chitosan Composite Hydrogels Promote M2 Macrophage Polarization and Accelerate Diabetic Cutaneous Wound Healing. Mater. Today Bio 2024, 25, 100975. [Google Scholar] [CrossRef]
- Kazimierczak, P.; Koziol, M.; Przekora, A. The Chitosan/Agarose/Nanoha Bone Scaffold-Induced M2 Macrophage Polarization and Its Effect on Osteogenic Differentiation in Vitro. Int. J. Mol. Sci. 2021, 22, 1109. [Google Scholar] [CrossRef]
- Wei, X.; Liu, C.; Li, Z.; Gu, Z.; Yang, J.; Luo, K. Chitosan-Based Hydrogel Dressings for Diabetic Wound Healing via Promoting M2 Macrophage-Polarization. Carbohydr. Polym. 2024, 331, 121873. [Google Scholar] [CrossRef]
- Zakrzewski, W.; Dobrzynski, M.; Wiglusz, R.J.; Rybak, Z.; Szymonowicz, M. Selected Nanomaterials’ Application Enhanced with the Use of Stem Cells in Acceleration of Alveolar Bone Regeneration during Augmentation Process. Nanomaterials 2020, 10, 1216. [Google Scholar] [CrossRef]
- Shi, C.; Zhu, Y.; Ran, X.; Wang, M.; Su, Y.; Cheng, T. Therapeutic Potential of Chitosan and Its Derivatives in Regenerative Medicine. J. Surg. Res. 2006, 133, 185–192. [Google Scholar] [CrossRef] [PubMed]
- Šalandová, M.; van Hengel, I.A.J.; Apachitei, I.; Zadpoor, A.A.; van der Eerden, B.C.J.; Fratila-Apachitei, L.E. Inorganic Agents for Enhanced Angiogenesis of Orthopedic Biomaterials. Adv. Healthc. Mater. 2021, 10, e2002254. [Google Scholar] [CrossRef]
- Mo, Y.; Zhao, F.; Lin, Z.; Cao, X.; Chen, D.; Chen, X. Local Delivery of Naringin in Beta-Cyclodextrin Modified Mesoporous Bioactive Glass Promotes Bone Regeneration: From Anti-Inflammatory to Synergistic Osteogenesis and Osteoclastogenesis. Biomater. Sci. 2022, 10, 1697–1712. [Google Scholar] [CrossRef] [PubMed]
- Bari, A.; Bloise, N.; Fiorilli, S.; Novajra, G.; Vallet-Regí, M.; Bruni, G.; Torres-Pardo, A.; González-Calbet, J.M.; Visai, L.; Vitale-Brovarone, C. Copper-Containing Mesoporous Bioactive Glass Nanoparticles as Multifunctional Agent for Bone Regeneration. Acta Biomater. 2017, 55, 493–504. [Google Scholar] [CrossRef] [PubMed]
- Xu, C.; Sun, Y.; Jansen, J.; Li, M.; Wei, L.; Wu, Y.; Liu, Y. Calcium Phosphate Ceramics and Synergistic Bioactive Agents for Osteogenesis in Implant Dentistry. Tissue Eng. Part C Methods 2023, 29, 197–215. [Google Scholar] [CrossRef]
- Saberi, A.; Kouhjani, M.; Mohammadi, M.; Hosta-Rigau, L. Novel Scaffold Platforms for Simultaneous Induction Osteogenesis and Angiogenesis in Bone Tissue Engineering: A Cutting-Edge Approach. J. Nanobiotechnol. 2023, 21, 351. [Google Scholar] [CrossRef]
- Deb, S.; Mandegaran, R.; Di Silvio, L. A Porous Scaffold for Bone Tissue Engineering/45S5 Bioglass® Derived Porous Scaffolds for Co-Culturing Osteoblasts and Endothelial Cells. J. Mater. Sci. Mater. Med. 2010, 21, 893–905. [Google Scholar] [CrossRef]
- Herman, K.; Wujczyk, M.; Dobrzynski, M.; Diakowska, D.; Wiglusz, K.; Wiglusz, R.J. In Vitro Assessment of Long-Term Fluoride Ion Release from Nanofluorapatite. Materials 2021, 14, 3747. [Google Scholar] [CrossRef]
- Chen, Y.; Liu, X.; Liu, R.; Gong, Y.; Wang, M.; Huang, Q.; Feng, Q.; Yu, B. Zero-Order Controlled Release of BMP2-Derived Peptide P24 from the Chitosan Scaffold by Chemical Grafting Modification Technique for Promotion of Osteogenesis in Vitro and Enhancement of Bone Repair in Vivo. Theranostics 2017, 7, 1072–1087. [Google Scholar] [CrossRef]
- Soriente, A.; Fasolino, I.; Raucci, M.G.; Demitri, C.; Madaghiele, M.; Giuri, A.; Sannino, A.; Ambrosio, L. Effect of Inorganic and Organic Bioactive Signals Decoration on the Biological Performance of Chitosan Scaffolds for Bone Tissue Engineering. J. Mater. Sci. Mater. Med. 2018, 29, 62. [Google Scholar] [CrossRef]
- Thein-Han, W.W.; Misra, R.D.K. Biomimetic Chitosan-Nanohydroxyapatite Composite Scaffolds for Bone Tissue Engineering. Acta Biomater. 2009, 5, 1182–1197. [Google Scholar] [CrossRef]
- Wang, T.; Guo, S.; Zhang, H.; Chen, Y.; Cai, Y. Injectable Hydrogel Delivering Bone Morphogenetic Protein-2, Vascular Endothelial Growth Factor, and Adipose-Derived Stem Cells for Vascularized Bone Tissue Engineering. J. Drug Deliv. Sci. Technol. 2020, 57, 101637. [Google Scholar] [CrossRef]
- Soran, Z.; Aydin, R.S.T.; Gumusderelioglu, M. Chitosan Scaffolds with BMP-6 Loaded Alginate Microspheres for Periodontal Tissue Engineering. J. Microencapsul. 2012, 29, 770–780. [Google Scholar] [CrossRef] [PubMed]
- Barakzai, S.; Salehiamin, M.; Shaban, M.O.; Azami, M.; Heidari, S.; Sobhani, A. Chitosan Scaffold Containing Periostin Can Accelerate Bone Defect Regeneration in Non-Weight-Bearing Conditions. Regen. Eng. Transl. Med. 2023, 9, 125–134. [Google Scholar] [CrossRef]
- Bonnet, N.; Brun, J.; Rousseau, J.C.; Duong, L.T.; Ferrari, S.L. Cathepsin K Controls Cortical Bone Formation by Degrading Periostin. J. Bone Miner. Res. 2017, 32, 1432–1441. [Google Scholar] [CrossRef]
- Dobrzyński, W.; Nikodem, A.; Diakowska, D.; Wiglusz, R.J.; Watras, A.; Dobrzyński, M.; Mikulewicz, M. Comparison of the Fluoride Ion Release from Nanofluorapatite-Modified Orthodontic Cement under Different PH Conditions—An in Vitro Study. Acta Bioeng. Biomech. 2023, 25, 159–176. [Google Scholar] [CrossRef]
- Janeczek, M.; Szymczyk, P.; Dobrzynski, M.; Parulska, O.; Szymonowicz, M.; Kuropka, P.; Rybak, Z.; Zywicka, B.; Ziolkowski, G.; Marycz, K.; et al. Influence of Surface Modifications of a Nanostructured Implant on Osseointegration Capacity-Preliminary: In Vivo Study. RSC Adv. 2018, 8, 15533–15546. [Google Scholar] [CrossRef]
- Dong, H.; Liu, H.; Zhou, N.; Li, Q.; Yang, G.; Chen, L.; Mou, Y. Surface Modified Techniques and Emerging Functional Coating of Dental Implants. Coatings 2020, 10, 1012. [Google Scholar] [CrossRef]
- Ururahy, M.S.L.; Barbosa, E.S.; Manente, R.; Ramos, A.P.; Crotti, A.E.M.; Corona, S.A.M. Effect of Phosphorylated Chitosan and Carbodiimide on the Surface Wettability, Surface Free Energy and Surface Morphology of the Eroded Dentin. Dent. Med. Probl. 2025, 62, 275–283. [Google Scholar] [CrossRef]
- Yun, Y.P.; Lee, S.Y.; Kim, H.J.; Song, J.J.; Kim, S.E. Improvement of Osteoblast Functions by Sustained Release of Bone Morphogenetic Protein-2 (BMP-2) from Heparin-Coated Chitosan Scaffold. Tissue Eng. Regen. Med. 2013, 10, 183–191. [Google Scholar] [CrossRef]
- Yun, Y.P.; Kim, S.E.; Kang, E.Y.; Kim, H.J.; Park, K.; Song, H.R. The Effect of Bone Morphogenic Protein-2 (BMP-2)-Immobilizing Heparinized-Chitosan Scaffolds for Enhanced Osteoblast Activity. Tissue Eng. Regen. Med. 2013, 10, 122–130. [Google Scholar] [CrossRef]
- Teixeira, S.; Yang, L.; Dijkstra, P.J.; Ferraz, M.P.; Monteiro, F.J. Heparinized Hydroxyapatite/Collagen Three-Dimensional Scaffolds for Tissue Engineering. J. Mater. Sci. Mater. Med. 2010, 21, 2385–2392. [Google Scholar] [CrossRef]
- Song, M.; Zhou, Y.; Liu, Y. VEGF Heparinized-Decellularized Adipose Tissue Scaffolds Enhance Tissue Engineering Vascularization in Vitro. RSC Adv. 2018, 8, 33614–33624. [Google Scholar] [CrossRef]
- Wu, Q.; Li, Y.; Wang, Y.; Li, L.; Jiang, X.; Tang, J.; Yang, H.; Zhang, J.; Bao, J.; Bu, H. The Effect of Heparinized Decellularized Scaffolds on Angiogenic Capability. J. Biomed. Mater. Res. A 2016, 104, 3021–3030. [Google Scholar] [CrossRef] [PubMed]
- Haghani, N.; Hassanzadeh Nemati, N.; Khorasani, M.T.; Bonakdar, S. Fabrication of Polycaprolactone/Heparinized Nano Fluorohydroxyapatite Scaffold for Bone Tissue Engineering Uses. Int. J. Polym. Mater. Polym. Biomater. 2024, 73, 544–555. [Google Scholar] [CrossRef]
- Wang, W.; Hu, J.; He, C.; Nie, W.; Feng, W.; Qiu, K.; Zhou, X.; Gao, Y.; Wang, G. Heparinized PLLA/PLCL Nanofibrous Scaffold for Potential Engineering of Small-Diameter Blood Vessel: Tunable Elasticity and Anticoagulation Property. J. Biomed. Mater. Res. A 2015, 103, 1784–1797. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Cai, Z.; Cheng, J.; Wang, C.; Fang, Z.; Xiao, Y.; Feng, Z.G.; Gu, Y. Characterization of a Heparinized Decellularized Scaffold and Its Effects on Mechanical and Structural Properties. J. Biomater. Sci. Polym. Ed. 2020, 31, 999–1023. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Lv, X.; Chen, S.; Li, Z.; Yao, J.; Peng, X.; Feng, C.; Xu, Y.; Wang, H. Use of Heparinized Bacterial Cellulose Based Scaffold for Improving Angiogenesis in Tissue Regeneration. Carbohydr. Polym. 2018, 181, 948–956. [Google Scholar] [CrossRef]
- Zamani, M.; Khafaji, M.; Naji, M.; Vossoughi, M.; Alemzadeh, I.; Haghighipour, N. A Biomimetic Heparinized Composite Silk-Based Vascular Scaffold with Sustained Antithrombogenicity. Sci. Rep. 2017, 7, 4455. [Google Scholar] [CrossRef]
- Cheng, J.; Wang, C.; Guo, L.; Gu, Y. Development of Heparinized and Hepatocyte Growth Factor-Coated Acellular Scaffolds Using Porcine Carotid Arteries. J. Biomed. Mater. Res. B Appl. Biomater. 2024, 112, e35317. [Google Scholar] [CrossRef]
- Nguyen, M.T.N.; Tran, H.L.B. In-Vitro Endothelialization Assessment of Heparinized Bovine Pericardial Scaffold for Cardiovascular Application. Polymers 2022, 14, 2156. [Google Scholar] [CrossRef]
- Liu, K.; Meng, C.X.; Lv, Z.Y.; Zhang, Y.J.; Li, J.; Li, K.Y.; Liu, F.Z.; Zhang, B.; Cui, F.Z. Enhancement of BMP-2 and VEGF carried by mineralized collagen for mandibular bone regeneration. Regen. Biomater. 2020, 7, 435–440, Erratum in Regen. Biomater. 2020, 8, rbaa054. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kim, S.; Kang, Y.; Krueger, C.A.; Sen, M.; Holcomb, J.B.; Chen, D.; Wenke, J.C.; Yang, Y. Sequential Delivery of BMP-2 and IGF-1 Using a Chitosan Gel with Gelatin Microspheres Enhances Early Osteoblastic Differentiation. Acta Biomater. 2012, 8, 1768–1777. [Google Scholar] [CrossRef] [PubMed]
- Sanjaya, I.G.P.H.; Maliawan, S.; Sudarsa, I.W.; Mahadewa, T.G.B. Administration of Recombinant Human Bone Morphogenetic Protein-2 (RhBMP-2) and Chitosan Scaffold in Calvarial Bone Defects in Wistar Rats. Bali Med. J. 2024, 13, 750–754. [Google Scholar] [CrossRef]
- Nandi, S.K.; Kundu, B.; Basu, D. Protein Growth Factors Loaded Highly Porous Chitosan Scaffold: A Comparison of Bone Healing Properties. Mater. Sci. Eng. C 2013, 33, 1267–1275. [Google Scholar] [CrossRef] [PubMed]
- Guzmań, R.; Nardecchia, S.; Gutíerrez, M.C.; Ferrer, M.L.; Ramos, V.; Del Monte, F.; Abarrategi, A.; López-Lacomba, J.L. Chitosan Scaffolds Containing Calcium Phosphate Salts and RhBMP-2: In Vitro and in Vivo Testing for Bone Tissue Regeneration. PLoS ONE 2014, 9, e87149. [Google Scholar] [CrossRef]
- Qiu, Y.; Xu, X.; Guo, W.; Zhao, Y.; Su, J.; Chen, J. Mesoporous Hydroxyapatite Nanoparticles Mediate the Release and Bioactivity of BMP-2 for Enhanced Bone Regeneration. ACS Biomater. Sci. Eng. 2020, 6, 2323–2335. [Google Scholar] [CrossRef]
- Xie, C.; Lu, X.; Han, L.; Xu, J.; Wang, Z.; Jiang, L.; Wang, K.; Zhang, H.; Ren, F.; Tang, Y. Biomimetic Mineralized Hierarchical Graphene Oxide/Chitosan Scaffolds with Adsorbability for Immobilization of Nanoparticles for Biomedical Applications. ACS Appl. Mater. Interfaces 2016, 8, 1707–1717. [Google Scholar] [CrossRef]
- Demirtaş, T.T.; Göz, E.; Karakeçili, A.; Gümüşderelioğlu, M. Combined Delivery of PDGF-BB and BMP-6 for Enhanced Osteoblastic Differentiation. J. Mater. Sci. Mater. Med. 2016, 27, 12. [Google Scholar] [CrossRef]
- Sularsih The Pore Size of Chitosan-Aloe Vera Scaffold and Its Effect on VEGF Expressions and Woven Alveolar Bone Healing of Tooth Extraction of Cavia Cobaya. Dent. J. 2020, 53, 115–121. [CrossRef]
- Liu, D.; Liu, Z.; Zou, J.; Li, L.; Sui, X.; Wang, B.; Yang, N.; Wang, B. Synthesis and Characterization of a Hydroxyapatite-Sodium Alginate-Chitosan Scaffold for Bone Regeneration. Front. Mater. 2021, 8, 648980. [Google Scholar] [CrossRef]
- De la Riva, B.; Sánchez, E.; Hernández, A.; Reyes, R.; Tamimi, F.; López-Cabarcos, E.; Delgado, A.; Évora, C. Local Controlled Release of VEGF and PDGF from a Combined Brushite-Chitosan System Enhances Bone Regeneration. J. Control. Release 2010, 143, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Tiǧli, R.S.; Akman, A.C.; Gumusderelioglu, M.; Nohutçu, R.M. In Vitro Release of Dexamethasone or BFGF from Chitosan/Hydroxyapatite Scaffolds. J. Biomater. Sci. Polym. Ed. 2009, 20, 1899–1914. [Google Scholar] [CrossRef]
- Costa-Pinto, A.R.; Reis, R.L.; Neves, N.M. Scaffolds Based Bone Tissue Engineering: The Role of Chitosan. Tissue Eng. Part B Rev. 2011, 17, 331–347. [Google Scholar] [CrossRef]
- Yilgor, P.; Tuzlakoglu, K.; Reis, R.L.; Hasirci, N.; Hasirci, V. Incorporation of a Sequential BMP-2/BMP-7 Delivery System into Chitosan-Based Scaffolds for Bone Tissue Engineering. Biomaterials 2009, 30, 3551–3559. [Google Scholar] [CrossRef]
- Chen, D.; Zhao, M.; Mundy, G.R. Bone Morphogenetic Proteins. Growth Factors 2004, 22, 233–241. [Google Scholar] [CrossRef] [PubMed]
- Ferrara, N.; Houck, K.A.; Jakeman, L.B.; Winer, J.; Leung, D.W. The Vascular Endothelial Growth Factor Family of Polypeptides. J. Cell Biochem. 1991, 47, 211–218. [Google Scholar] [CrossRef]
- Kaigler, D.; Cirelli, J.A.; Giannobile, W.V. Growth Factor Delivery for Oral and Periodontal Tissue Engineering. Expert. Opin. Drug Deliv. 2006, 3, 647–662. [Google Scholar] [CrossRef]
- Freilich, M.; Patel, C.M.; Wei, M.; Shafer, D.; Schleier, P.; Hortschansky, P.; Kompali, R.; Kuhn, L. Growth of New Bone Guided by Implants in a Murine Calvarial Model. Bone 2008, 43, 781–788. [Google Scholar] [CrossRef] [PubMed]
- Szymonowicz, M.; Korczynski, M.; Dobrzynski, M.; Zawisza, K.; Mikulewicz, M.; Karuga-Kuzniewska, E.; Zywicka, B.; Rybak, Z.; Wiglusz, R.J. Cytotoxicity Evaluation of High-Temperature Annealed Nanohydroxyapatite in Contact with Fibroblast Cells. Materials 2017, 10, 590. [Google Scholar] [CrossRef]
- Sasisekharan, R.; Ernst, S.; Venkataraman, G. On the Regulation of Fibroblast Growth Factor Activity by Heparin-like Glycosaminoglycans. Angiogenesis 1997, 1, 45–54. [Google Scholar] [CrossRef]
- Boonyagul, S.; Banlunara, W.; Sangvanich, P.; Thunyakitpisal, P. Effect of Acemannan, an Extracted Polysaccharide from Aloe Vera, on BMSCs Proliferation, Differentiation, Extracellular Matrix Synthesis, Mineralization, and Bone Formation in a Tooth Extraction Model. Odontology 2014, 102, 310–317. [Google Scholar] [CrossRef] [PubMed]
- Martino, M.M.; Briquez, P.S.; Güç, E.; Tortelli, F.; Kilarski, W.W.; Metzger, S.; Rice, J.J.; Kuhn, G.A.; Müller, R.; Swartz, M.A.; et al. Growth Factors Engineered for Super-Affinity to the Extracellular Matrix Enhance Tissue Healing. Science 2014, 343, 885–888. [Google Scholar] [CrossRef]
- Iaquinta, M.R.; Mazzoni, E.; Manfrini, M.; D’Agostino, A.; Trevisiol, L.; Nocini, R.; Trombelli, L.; Barbanti-Brodano, G.; Martini, F.; Tognon, M. Innovative Biomaterials for Bone Regrowth. Int. J. Mol. Sci. 2019, 20, 618. [Google Scholar] [CrossRef]
- Zhu, L.; Luo, D.; Liu, Y. Effect of the Nano/Microscale Structure of Biomaterial Scaffolds on Bone Regeneration. Int. J. Oral. Sci. 2020, 12, 6. [Google Scholar] [CrossRef]
- Zang, S.; Zhu, L.; Luo, K.; Mu, R.; Chen, F.; Wei, X.; Yan, X.; Han, B.; Shi, X.; Wang, Q.; et al. Chitosan Composite Scaffold Combined with Bone Marrow-Derived Mesenchymal Stem Cells for Bone Regeneration: In Vitro and in Vivo Evaluation. Oncotarget 2017, 8, 110890–110903. [Google Scholar] [CrossRef]
- De Witte, T.M.; Fratila-Apachitei, L.E.; Zadpoor, A.A.; Peppas, N.A. Bone Tissue Engineering via Growth Factor Delivery: From Scaffolds to Complex Matrices. Regen. Biomater. 2018, 5, 197–211. [Google Scholar] [CrossRef]
- Pang, E.; Paik, J.; Kim, S.; Jung, U.; Kim, C.; Cho, K.; Kim, C.; Choi, S. Effects of Chitosan on Human Periodontal Ligament Fibroblasts In Vitro and on Bone Formation in Rat Calvarial Defects. J. Periodontol. 2005, 76, 1526–1533. [Google Scholar] [CrossRef] [PubMed]
- Sukpaita, T.; Chirachanchai, S.; Pimkhaokham, A.; Ampornaramveth, R.S. Chitosan-Based Scaffold for Mineralized Tissues Regeneration. Mar. Drugs 2021, 19, 551. [Google Scholar] [CrossRef] [PubMed]
- Sivashankari, P.R.; Prabaharan, M. Prospects of Chitosan-Based Scaffolds for Growth Factor Release in Tissue Engineering. Int. J. Biol. Macromol. 2016, 93, 1382–1389. [Google Scholar] [CrossRef] [PubMed]
- Jeong Park, Y.; Moo Lee, Y.; Nae Park, S.; Yoon Sheen, S.; Pyoung Chung, C.; Lee, S.J. Platelet Derived Growth Factor Releasing Chitosan Sponge for Periodontal Bone Regeneration. Biomaterials 2000, 21, 153–159. [Google Scholar] [CrossRef]
- Ezoddini-Ardakani, F.; Navabazam, A.; Fatehi, F.; Danesh-Ardekani, M.; Khadem, S.; Rouhi, G. Histologic Evaluation of Chitosan as an Accelerator of Bone Regeneration in Microdrilled Rat Tibias. Dent. Res. J. 2012, 9, 694–699. [Google Scholar]
- Pramanik, S.; Aggarwal, A.; Kadi, A.; Alhomrani, M.; Alamri, A.S.; Alsanie, W.F.; Koul, K.; Deepak, A.; Bellucci, S. Chitosan Alchemy: Transforming Tissue Engineering and Wound Healing. RSC Adv. 2024, 14, 19219–19256. [Google Scholar] [CrossRef]
- Gerova-Vatsova, T.; Peev, S.; Yotsova, R.; Rogova, V.-V. Evaluation of the Effectiveness of Chitosan-Modified Bone Regeneration Materials: A Systematic Review. Pharmaceutics 2025, 17, 665. [Google Scholar] [CrossRef]
- Zhang, S.; Chen, J.; Yu, Y.; Dai, K.; Wang, J.; Liu, C. Accelerated Bone Regenerative Efficiency by Regulating Sequential Release of BMP-2 and VEGF and Synergism with Sulfated Chitosan. ACS Biomater. Sci. Eng. 2019, 5, 1944–1955. [Google Scholar] [CrossRef]
- Dominiak, M.; Lysiak-Drwal, K.; Gedrange, T.; Zietek, M.; Gerber, H. Efficacy of healing process of bone defects after apicectomy: Results after 6 and 12 months. J. Physiol. Pharmacol. 2009, 60 (Suppl. 8), 51–55. [Google Scholar]
- Bauer, R.; Gedrange, T.; Bauer, K.; Walter, B. Intrauterine growth restriction induces increased capillary density and accelerated type I fiber maturation in newborn pig skeletal muscles. J. Perinat. Med. 2006, 34, 235–242. [Google Scholar] [CrossRef]
- Geng, Y.; Duan, H.; Xu, L.; Witman, N.; Yan, B.; Yu, Z.; Wang, H.; Tan, Y.; Lin, L.; Li, D.; et al. BMP-2 and VEGF-A ModRNAs in Collagen Scaffold Synergistically Drive Bone Repair through Osteogenic and Angiogenic Pathways. Commun. Biol. 2021, 4, 82. [Google Scholar] [CrossRef]
- Levengood, S.K.L.; Zhang, M. Chitosan-Based Scaffolds for Bone Tissue Engineering. J. Mater. Chem. B 2014, 2, 3161–3184. [Google Scholar] [CrossRef] [PubMed]
- Vo, T.N.; Kasper, F.K.; Mikos, A.G. Strategies for Controlled Delivery of Growth Factors and Cells for Bone Regeneration. Adv. Drug Deliv. Rev. 2012, 64, 1292–1309. [Google Scholar] [CrossRef]
- Lubojanski, A.; Dobrzynski, M.; Nowak, N.; Rewak-Soroczynska, J.; Sztyler, K.; Zakrzewski, W.; Dobrzynski, W.; Szymonowicz, M.; Rybak, Z.; Wiglusz, K.; et al. Application of Selected Nanomaterials and Ozone in Modern Clinical Dentistry. Nanomaterials 2021, 11, 259. [Google Scholar] [CrossRef]
- Biju, D.; Arumugam, P.; Kannan, S.; Kumar, P.Y.; Ronsivalle, V.; Cicciù, M.; Minervini, G. Development, Characterization, and Biocompatibility and Corrosion Analyses of a Silver-Decorated Graphene Oxide and Chitosan Surface Coating for Titanium Dental Implants: A Preliminary Report. Dent. Med. Probl. 2024, 61, 627–632. [Google Scholar] [CrossRef] [PubMed]
- Dommeti, V.K.; Pramanik, S.; Roy, S. Design of Customized Coated Dental Implants Using Finite Element Analysis. Dent. Med. Probl. 2023, 60, 385–392. [Google Scholar] [CrossRef]
- Ritger, P.L.; Peppas, N.A. A Simple Equation for Description of Solute Release I. Fickian and Non-Fickian Release from Non-Swellable Devices in the Form of Slabs, Spheres, Cylinders or Discs. J. Control. Release 1987, 5, 23–36. [Google Scholar] [CrossRef]
- Huang, X.; Lin, J.; Demner-Fushman, D. Evaluation of PICO as a Knowledge Representation for Clinical Questions. AMIA Annu. Symp. Proc. 2006, 2006, 359–363. [Google Scholar] [PubMed]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. PRISMA 2020 Explanation and Elaboration: Updated Guidance and Exemplars for Reporting Systematic Reviews. BMJ 2021, 372, n160. [Google Scholar] [CrossRef]
- Małyszek, A.; Kiryk, S.; Kensy, J.; Kotela, A.; Michalak, M.; Kiryk, J.; Janeczek, M.; Matys, J.; Dobrzyński, M. Identification of Factors Influencing Fluoride Content in Tea Infusions: A Systematic Review. Appl. Sci. 2025, 15, 5974. [Google Scholar] [CrossRef]
- Tokarczuk, D.; Tokarczuk, O.; Kiryk, J.; Kensy, J.; Szablińska, M.; Dyl, T.; Dobrzyński, W.; Matys, J.; Dobrzyński, M. Fluoride Release by Restorative Materials after the Application of Surface Coating Agents: A Systematic Review. Appl. Sci. 2024, 14, 4956. [Google Scholar] [CrossRef]
- Klimas, S.; Kiryk, S.; Kiryk, J.; Kotela, A.; Kensy, J.; Michalak, M.; Rybak, Z.; Matys, J.; Dobrzyński, M. The Impact of Environmental and Material Factors on Fluoride Release from Metal-Modified Glass Ionomer Cements: A Systematic Review of In Vitro Studies. Materials 2025, 18, 3187. [Google Scholar] [CrossRef]
- Oleniacz-Trawińska, M.; Kotela, A.; Kensy, J.; Kiryk, S.; Dobrzyński, W.; Kiryk, J.; Gerber, H.; Fast, M.; Matys, J.; Dobrzyński, M. Evaluation of Factors Affecting Fluoride Release from Compomer Restorative Materials: A Systematic Review. Materials 2025, 18, 1627. [Google Scholar] [CrossRef] [PubMed]
- Rygas, J.; Matys, J.; Wawrzyńska, M.; Szymonowicz, M.; Dobrzyński, M. The Use of Graphene Oxide in Orthodontics—A Systematic Review. J. Funct. Biomater. 2023, 14, 500. [Google Scholar] [CrossRef]
- Rajewska, J.; Kowalski, J.; Matys, J.; Dobrzyński, M.; Wiglusz, R.J. The Use of Lactide Polymers in Bone Tissue Regeneration in Dentistry—A Systematic Review. J. Funct. Biomater. 2023, 14, 83. [Google Scholar] [CrossRef] [PubMed]
- Piszko, P.J.; Piszko, A.; Kiryk, J.; Lubojański, A.; Dobrzyński, W.; Wiglusz, R.J.; Matys, J.; Dobrzyński, M. The Influence of Fluoride Gels on the Physicochemical Properties of Tooth Tissues and Dental Materials—A Systematic Review. Gels 2024, 10, 98. [Google Scholar] [CrossRef]
- Struzik, N.; Wiśniewska, K.; Piszko, P.J.; Piszko, A.; Kiryk, J.; Matys, J.; Dobrzyński, M. SEM Studies Assessing the Efficacy of Laser Treatment for Primary Teeth: A Systematic Review. Appl. Sci. 2024, 14, 1107. [Google Scholar] [CrossRef]
- Kensy, J.; Dobrzyński, M.; Wiench, R.; Grzech-Leśniak, K.; Matys, J. Fibroblasts Adhesion to Laser-Modified Titanium Surfaces—A Systematic Review. Materials 2021, 14, 7305. [Google Scholar] [CrossRef]
- Watson, P.F.; Petrie, A. Method Agreement Analysis: A Review of Correct Methodology. Theriogenology 2010, 73, 1167–1179. [Google Scholar] [CrossRef]
- Tufanaru, C.; Munn, Z.; Aromataris, E.; Campbell, J.; Hopp, L. Chapter 3: Systematic Reviews of Effectiveness. In JBI Manual for Evidence Synthesis; Aromataris, E., Munn, Z., Eds.; Joanna Briggs Institute (JBI): North Adelaide, Australia, 2020. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).