Analysis of Risk Factors Associated with Proximal Junctional Kyphosis Following Long Instrumented Fusion from L1 to Sacrum: Age Itself Does Not Independently Increase the Risk
Abstract
1. Introduction
2. Materials and Methods
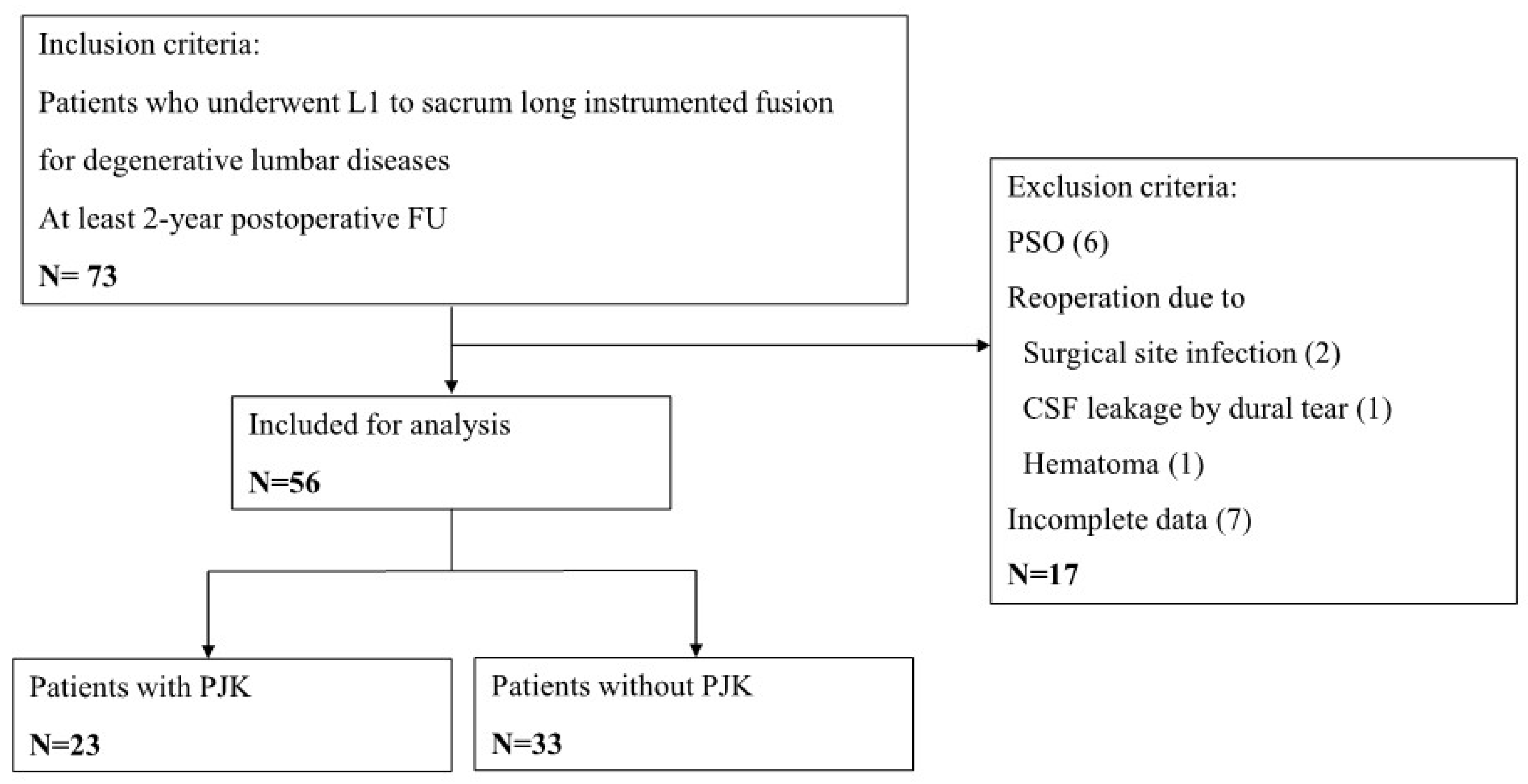
2.1. Study Design and Patient Population
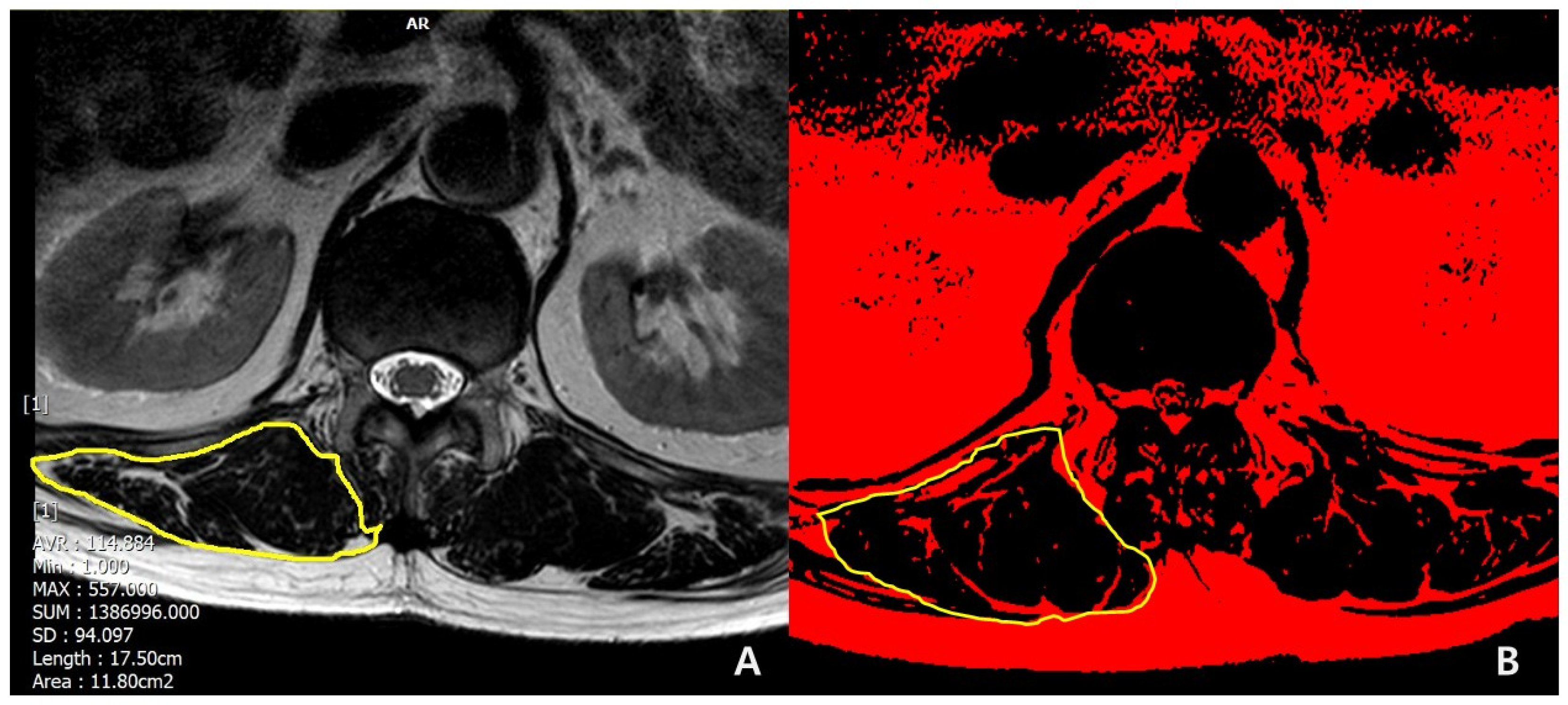
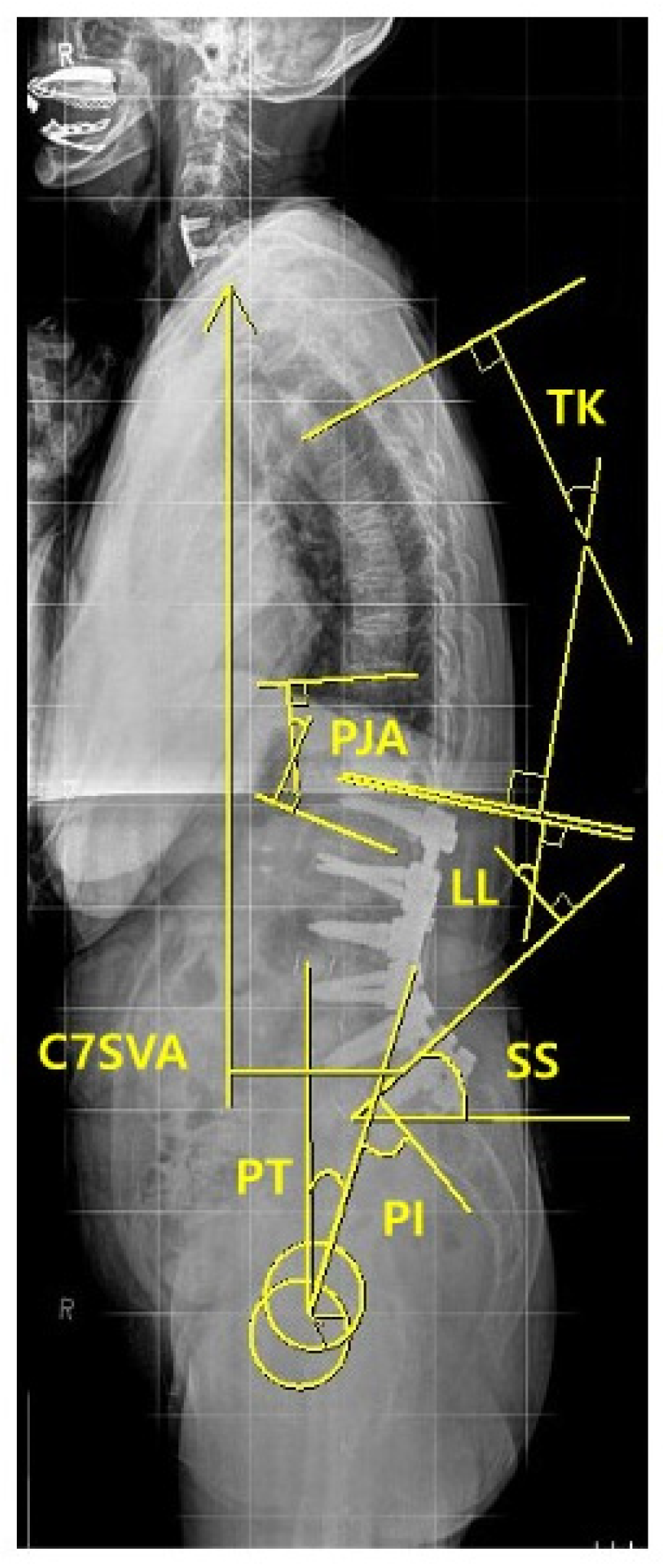
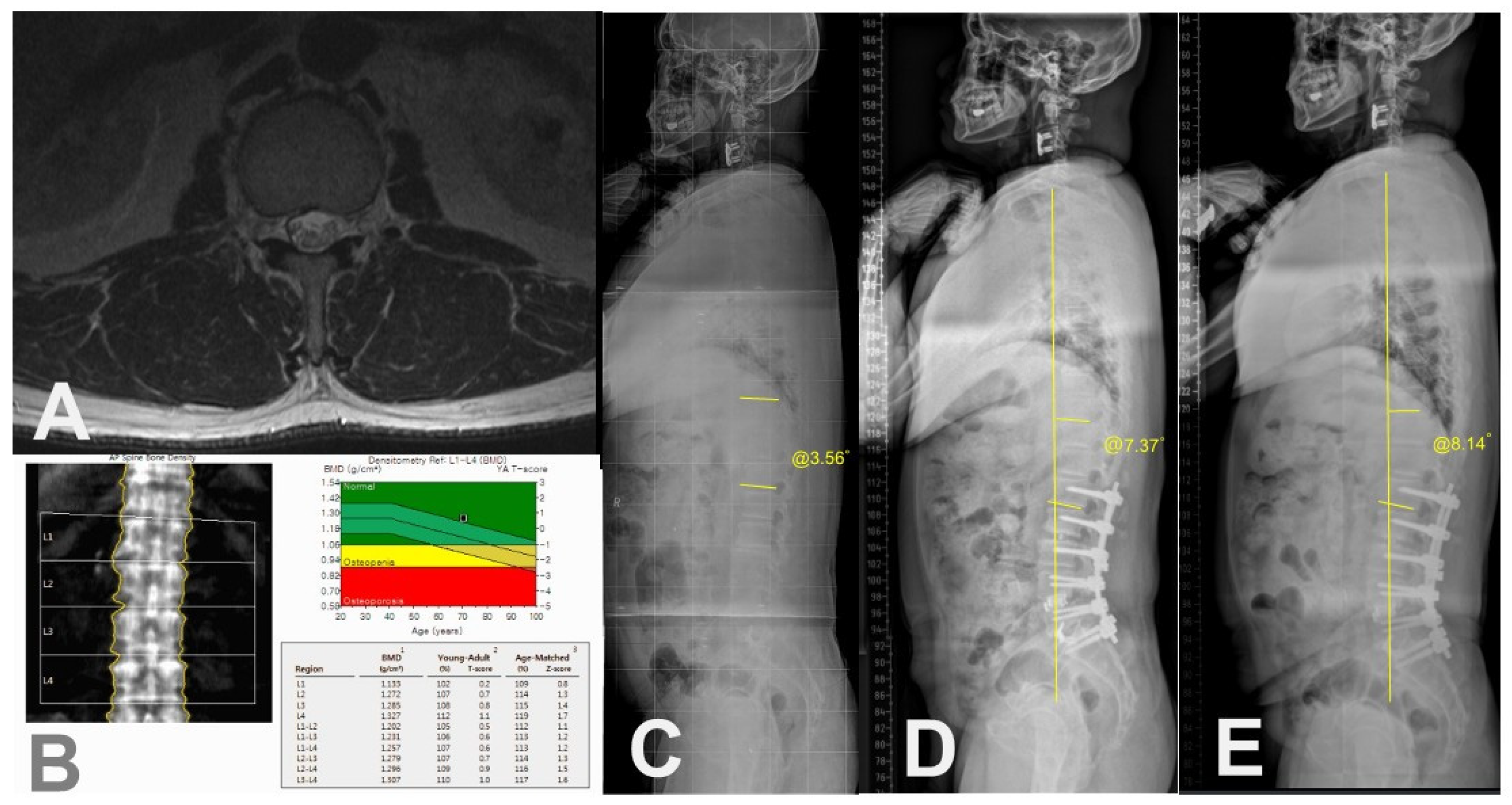
2.2. Data Collection
3. Results
3.1. Baseline Demographics and PJK Incidence of Included Patients
3.2. Univariate Analysis of Demographic or Surgical Risk Factors
3.3. Univariate Analysis of Radiographic Risk Factors after L1-Sacrum Instrumented Fusion
3.4. Logistic Regression Analysis of Potential Risk Factors Associated with PJK after L1-Sacrum Instrumented Fusion
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| PJK | Proximal junctional kyphosis |
| PJA | Proximal junctional angle |
| ASD | Adult spinal deformity |
| TK | Thoracic kyphosis |
| TLK | Thoracolumbar kyphosis |
| LL | Lumbar lordosis |
| PT | Pelvic tilt |
| SS | Sacral slope |
| PI | Pelvic incidence |
| SVA | Sagittal vertical axis |
| BMI | Body mass index |
| BMD | Bone mineral density |
| ASA | American Society of Anesthesiologists |
| CSA | Cross-sectional area |
| MR | Magnetic resonance |
| SRS | Scoliosis Research Society |
| ODI | Oswestry disability index |
References
- Watanabe, K.; Lenke, L.G.; Bridwell, K.H.; Kim, Y.J.; Koester, L.; Hensley, M. Proximal junctional vertebral fracture in adults after spinal deformity surgery using pedicle screw constructs: Analysis of morphological features. Spine 2010, 35, 138–145. [Google Scholar] [CrossRef]
- Park, W.M.; Choi, D.K.; Kim, K.; Kim, Y.J.; Kim, Y.H. Biomechanical effects of fusion levels on the risk of proximal junctional failure and kyphosis in lumbar spinal fusion surgery. Clin. Biomech. 2015, 30, 1162–1169. [Google Scholar] [CrossRef] [PubMed]
- Ono, K.; Ohmori, K.; Hori, T. Clinical and Radiological Outcomes of Corrective Surgery on Adult Spinal Deformity Patients: Comparison of Short and Long Fusion. Adv. Orthop. 2019, 2019, 9492486. [Google Scholar] [CrossRef]
- Hyun, S.J.; Kim, Y.J.; Rhim, S.C. Patients with proximal junctional kyphosis after stopping at thoracolumbar junction have lower muscularity, fatty degeneration at the thoracolumbar area. Spine J. 2016, 16, 1095–1101. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Yagi, M.; Nyugen, J.; Cunningham, M.E.; Boachie-Adjei, O. Combined anterior-posterior surgery is the most important risk factor for developing proximal junctional kyphosis in idiopathic scoliosis. Clin. Orthop. Relat. Res. 2012, 470, 1633–1639. [Google Scholar] [CrossRef] [PubMed]
- Hassanzadeh, H.; Gupta, S.; Jain, A.; El Dafrawy, M.H.; Skolasky, R.L.; Kebaish, K.M. Type of Anchor at the Proximal Fusion Level Has a Significant Effect on the Incidence of Proximal Junctional Kyphosis and Outcome in Adults After Long Posterior Spinal Fusion. Spine Deform. 2013, 1, 299–305. [Google Scholar] [CrossRef] [PubMed]
- Koike, Y.; Kotani, Y.; Terao, H.; Iwasaki, N. Risk Factor Analysis of Proximal Junctional Kyphosis after Surgical Treatment of Adult Spinal Deformity with Oblique Lateral Interbody Fusion. Asian Spine J. 2021, 15, 107–116. [Google Scholar] [CrossRef]
- Lafage, R.; Line, B.G.; Gupta, S.; Liabaud, B.; Schwab, F.; Smith, J.S.; Gum, J.L.; Ames, C.P.; Hostin, R.; Mundis, G.M.; et al. Orientation of the Upper-most Instrumented Segment Influences Proximal Junctional Disease Following Adult Spinal Deformity Surgery. Spine 2017, 42, 1570–1577. [Google Scholar] [CrossRef] [PubMed]
- Diebo, B.G.; Shah, N.V.; Stroud, S.G.; Paulino, C.B.; Schwab, F.J.; Lafage, V. Realignment surgery in adult spinal deformity: Prevalence and risk factors for proximal junctional kyphosis. Orthopade 2018, 47, 301–309. [Google Scholar] [CrossRef]
- Kim, J.H.; Kim, S.S.; Suk, S.I. Incidence of proximal adjacent failure in adult lumbar deformity correction based on proximal fusion level. Asian Spine J. 2007, 1, 19–26. [Google Scholar] [CrossRef]
- Shufflebarger, H.; Suk, S.I.; Mardjetko, S. Debate: Determining the upper instrumented vertebra in the management of adult degenerative scoliosis: Stopping at T10 versus L1. Spine 2006, 31, S185–S194. [Google Scholar] [CrossRef]
- Park, S.J.; Lee, C.S.; Park, J.S.; Lee, K.J. Should Thoracolumbar Junction Be Always Avoided as Upper Instrumented Vertebra in Long Instrumented Fusion for Adult Spinal Deformity?: Risk Factor Analysis for Proximal Junctional Failure. Spine 2020, 45, 686–693. [Google Scholar] [CrossRef] [PubMed]
- Bess, S.; Harris, J.E.; Turner, A.W.L.; LaFage, V.; Smith, J.S.; Shaffrey, C.I.; Schwab, F.J.; Haid, R.W. The effect of posterior polyester tethers on the biomechanics of proximal junctional kyphosis: A finite element analysis. J. Neurosurg. Spine 2017, 26, 125–133. [Google Scholar] [CrossRef] [PubMed]
- Ha, Y.; Maruo, K.; Racine, L.; Schairer, W.W.; Hu, S.S.; Deviren, V.; Burch, S.; Tay, B.; Chou, D.; Mummaneni, P.V.; et al. Proximal junctional kyphosis and clinical outcomes in adult spinal deformity surgery with fusion from the thoracic spine to the sacrum: A comparison of proximal and distal upper instrumented vertebrae. J. Neurosurg. Spine 2013, 19, 360–369. [Google Scholar] [CrossRef]
- Park, S.J.; Lee, C.S.; Chung, S.S.; Lee, J.Y.; Kang, S.S.; Park, S.H. Different Risk Factors of Proximal Junctional Kyphosis and Proximal Junctional Failure Following Long Instrumented Fusion to the Sacrum for Adult Spinal Deformity: Survivorship Analysis of 160 Patients. Neurosurgery 2017, 80, 279–286. [Google Scholar] [CrossRef]
- Pfirrmann, C.W.; Metzdorf, A.; Zanetti, M.; Hodler, J.; Boos, N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine 2001, 26, 1873–1878. [Google Scholar] [CrossRef]
- Lee, J.C.; Cha, J.G.; Kim, Y.; Kim, Y.I.; Shin, B.J. Quantitative analysis of back muscle degeneration in the patients with the degenerative lumbar flat back using a digital image analysis: Comparison with the normal controls. Spine 2008, 33, 318–325. [Google Scholar] [CrossRef] [PubMed]
- Janssen, M.M.; Drevelle, X.; Humbert, L.; Skalli, W.; Castelein, R.M. Differences in male and female spino-pelvic alignment in asymptomatic young adults: A three-dimensional analysis using upright low-dose digital biplanar X-rays. Spine 2009, 34, E826–E832. [Google Scholar] [CrossRef]
- Vialle, R.; Levassor, N.; Rillardon, L.; Templier, A.; Skalli, W.; Guigui, P. Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J. Bone Joint Surg. Am. 2005, 87, 260–267. [Google Scholar] [CrossRef]
- Fukushima, K.; Miyagi, M.; Inoue, G.; Shirasawa, E.; Uchiyama, K.; Takahira, N.; Takaso, M. Relationship between spinal sagittal alignment and acetabular coverage: A patient-matched control study. Arch. Orthop. Trauma Surg. 2018, 138, 1495–1499. [Google Scholar] [CrossRef]
- Zou, L.; Liu, J.; Lu, H. Characteristics and risk factors for proximal junctional kyphosis in adult spinal deformity after correction surgery: A systematic review and meta-analysis. Neurosurg. Rev. 2019, 42, 671–682. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.S.; Phan, K.; Cheung, Z.B.; Lee, N.; Vargas, L.; Arvind, V.; Merrill, R.K.; Gidumal, S.; Di Capua, J.; Overley, S.; et al. Surgical, Radiographic, and Patient-Related Risk Factors for Proximal Junctional Kyphosis: A Meta-Analysis. Glob. Spine J. 2019, 9, 32–40. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.T.; Lane, J.M. Osteoporosis: A review. Clin. Orthop. Relat. Res. 2004, 425, 126–134. [Google Scholar] [CrossRef]
- Kirkaldy-Willis, W.H.; Farfan, H.F. Instability of the lumbar spine. Clin. Orthop. Relat. Res. 1982, 165, 110–123. [Google Scholar] [CrossRef]
- Marques, E.A.; Wanderley, F.; Machado, L.; Sousa, F.; Viana, J.L.; Moreira-Gonçalves, D.; Moreira, P.; Mota, J.; Carvalho, J. Effects of resistance and aerobic exercise on physical function, bone mineral density, OPG and RANKL in older women. Exp. Gerontol. 2011, 46, 524–532. [Google Scholar] [CrossRef] [PubMed]
- Byun, C.W.; Cho, J.H.; Lee, C.S.; Lee, D.H.; Hwang, C.J. Effect of overcorrection on proximal junctional kyphosis in adult spinal deformity: Analysis by age-adjusted ideal sagittal alignment. Spine J. 2022, 22, 635–645. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Bridwell, K.H.; Lenke, L.G.; Park, M.S.; Song, K.S.; Piyaskulkaew, C.; Chuntarapas, T. Patients with proximal junctional kyphosis requiring revision surgery have higher postoperative lumbar lordosis and larger sagittal balance corrections. Spine 2014, 39, E576–E580. [Google Scholar] [CrossRef]
- Maruo, K.; Ha, Y.; Inoue, S.; Samuel, S.; Okada, E.; Hu, S.S.; Deviren, V.; Burch, S.; William, S.B.; Ames, C.P.; et al. Predictive factors for proximal junctional kyphosis in long fusions to the sacrum in adult spinal deformity. Spine 2013, 38, E1469–E1476. [Google Scholar] [CrossRef]
- Yagi, M.; King, A.B.; Boachie-Adjei, O. Incidence, risk factors, and natural course of proximal junctional kyphosis: Surgical outcomes review of adult idiopathic scoliosis. Minimum 5 years of follow-up. Spine 2012, 37, 1479–1489. [Google Scholar] [CrossRef]
- Fujimori, T.; Inoue, S.; Le, H.; Schairer, W.W.; Berven, S.H.; Tay, B.K.; Deviren, V.; Burch, S.; Iwasaki, M.; Hu, S.S. Long fusion from sacrum to thoracic spine for adult spinal deformity with sagittal imbalance: Upper versus lower thoracic spine as site of upper instrumented vertebra. Neurosurg. Focus 2014, 36, E9. [Google Scholar] [CrossRef]
- Bridwell, K.H.; Lenke, L.G.; Cho, S.K.; Pahys, J.M.; Zebala, L.P.; Dorward, I.G.; Cho, W.; Baldus, C.; Hill, B.W.; Kang, M.M. Proximal junctional kyphosis in primary adult deformity surgery: Evaluation of 20 degrees as a critical angle. Neurosurgery 2013, 72, 899–906. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.-S.; Jang, J.-Y.; Yu, Y.-D.; Heo, J.S.; Han, H.-S.; Yoon, Y.-S.; Kang, C.M.; Hwang, H.K.; Kang, S. Usefulness of artificial intelligence for predicting recurrence following surgery for pancreatic cancer: Retrospective cohort study. Int. J. Surg. 2021, 93, 106050. [Google Scholar] [CrossRef] [PubMed]

| Variables | Values |
|---|---|
| No. of included patients | 56 |
| Age at surgery (years) | 67.3 ± 7.9 (range, 45–79) |
| Sex | Female 46; Male 10 |
| BMI (kg/m2) | 26.1 ± 3.9 (range, 19.3–40.1) |
| BMD (T-score) | −1.8 ± 1.1 (range, −3.50–1.40) |
| Osteoporosis, n (%) | 18 (32.1) |
| Follow-up period (months) | 43.5 ± 31.7 (range, 24–136) |
| Smoker, n (%) | 7 (12.5) |
| ASA grade | |
| I, n (%) | 9 (16.1) |
| II, n (%) | 39 (69.6) |
| III, n (%) | 8 (14.3) |
| Iliac screw fixation, n (%) | 30 (53.6) |
| Previous spinal fusion, n (%) | 18 (32.1) |
| Incidence of PJK Until Final Follow-Up, n/Total (%) | 23/56 (41.1) |
|---|---|
| PJK within postoperative 1 year out of total PJK, n/total PJK (%) | 20/23 (87.0) |
| Compression fracture, n/total PJK (%) | 17/23 (73.9) |
| Screw loosening/pull-out, n/total PJK (%) | 4/23 (17.4) |
| Screw loosening with L1 upper endplate penetration, n/total PJK (%) | 2/23 (8.7) |
| Instability or subluxation of proximal adjacent segment, n/total PJK (%) | 3/23 (13.0) |
| PJF within PJK | 6/23 (26.1) |
| Parameters | PJK Group (n = 23) | Non-PJK Group (n = 33) | p |
|---|---|---|---|
| Age (years) | 66.4 ± 5.3 | 67.7 ± 9.2 | 0.134 |
| Female sex, n (%) | 23 (100) | 23 (72.7) | 0.011 * |
| BMD (T-score) | −2.4 ± 0.8 | −1.5 ± 1.1 | 0.006 * |
| Osteoporosis, n (%) | 14 (60.9) | 4 (12.1) | <0.001 * |
| BMI (kg/m2) | 24.4 ± 2.4 | 27.1 ± 4.3 | 0.004 * |
| Follow-up period (months) | 61.1 ± 40.6 | 23.6 ± 24.2 | <0.001 * |
| ASA grade | 0.970 | ||
| Grade I, n (%) | 6 | 8 | |
| Grade II, n (%) | 14 | 20 | |
| Grade III, n (%) | 3 | 5 | |
| Smoking, n (%) | 2 (8.7) | 5 (15.2) | 0.758 |
| Previous spinal fusion, n (%) | 7 (30.4) | 11 (33.3) | 0.995 |
| Iliac fixation, n (%) | 12 (52.2) | 18 (54.5) | 0.997 |
| Muscular quantity of T12-L1 (CSA of erector spinae), cm2 | 23.8 ± 4.2 | 32.2 ± 10.1 | <0.001 * |
| Muscular quality of T12-L1 (Fat infiltration in CSA of erector spinae) | <0.001 * | ||
| Mild to moderate (<50%), n | 4 | 21 | |
| Severe (≥50%), n | 13 | 3 | |
| Disc degeneration of T12-L1 | 0.923 | ||
| Mild to Moderate (Pfirrmann grade 1~3) | 7 | 12 | |
| Severe (Pfirrmann grade 4 and 5) | 10 | 12 |
| Risk Factors | PJK Group (n = 23) | Non-PJK Group (n = 33) | p |
|---|---|---|---|
| Preoperative Parameters | |||
| TK (°), mean ± SD | 7.6 ± 14.3 | 13.9 ± 12.7 | 0.153 |
| TLK (°), mean ± SD | 0.75 ± 0.9 | 0.67 ± 1.0 | 0.082 |
| PJA (°), mean ± SD | 2.98 ± 8.0 | 1.99 ± 12.2 | 0.583 |
| LL (°), mean ± SD | 7.2 ± 24.7 | 20.2 ± 24.5 | 0.115 |
| SS (°), mean ± SD | 23.0 ± 8.5 | 30.1 ± 12.3 | 0.057 |
| PT (°), mean ± SD | 34.0 ± 7.2 | 25.8 ± 13.0 | 0.032 * |
| PI (°), mean ± SD | 56.9 ± 7.0 | 55.5 ± 10.9 | 0.663 |
| C7 SVA (mm), mean ± SD | 92.0 ± 48.5 | 85.1 ± 43.4 | 0.720 |
| Immediate (3 months) postoperative parameters | |||
| TK (°), mean ± SD | 20.7 ± 8.4 | 19.9 ± 17.3 | 0.876 |
| TLK (°), mean ± SD | 23.5 ± 9.9 | 8.7 ± 12.2 | <0.001 * |
| PJA (°), mean ± SD | 20.9 ± 7.7 | 10.7 ± 8.1 | <0.001 * |
| LL (°), mean ± SD | 43.8 ± 13.5 | 45.9 ± 9.4 | 0.569 |
| SS (°), mean ± SD | 32.0 ± 9.4 | 35.6 ± 8.1 | 0.215 |
| PT (°), mean ± SD | 24.1 ± 11.2 | 18.7 ± 8.6 | 0.092 |
| PI (°), mean ± SD | 55.8 ± 7.4 | 53.7 ± 7.0 | 0.376 |
| C7 SVA (mm), mean ± SD | 49.9 ± 38.9 | 37.3 ± 35.6 | 0.303 |
| Changes between preoperative and immediate postoperative parameters | |||
| ΔTK (°), mean ± SD | −13.1 ± 11.5 | −5.8 ± 22.1 | 0.231 |
| ΔLL (°), mean ± SD | 36.6 ± 27.7 | 24.8 ± 27.2 | 0.180 |
| ΔSS (°), mean ± SD | 8.9 ± 10.8 | 5.2 ± 9.8 | 0.249 |
| ΔPT (°), mean ± SD | −9.9 ± 12.2 | −6.8 ± 8.3 | 0.338 |
| ΔC7 SVA (mm), mean ± SD | −42.1 ± 56.8 | −47.7 ± 45.9 | 0.724 |
| Parameters | p | OR | 95% CI |
|---|---|---|---|
| Female sex | 0.167 | ||
| Osteoporosis | 0.021 * | 20.50 | 1.59–264.99 |
| BMI (kg/m2) | 0.620 | ||
| Muscle quantity of T12-L1 (CSA of erector spinae) | 0.082 | ||
| Muscle quality of T12-L1 (Fat infiltration in CSA of erector spinae) | 0.002 * | 43.60 | 4.11–463.06 |
| Preoperative PT (°) | 0.852 | ||
| Immediate postoperatve TLK (°) | 0.161 | ||
| Immediate postoperatve PJA (°) | 0.124 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahn, J.; Kim, Y.-H.; Kim, Y.-C.; Kim, K.-T.; Kim, S.-M.; Park, J.B.; Ha, K.-Y. Analysis of Risk Factors Associated with Proximal Junctional Kyphosis Following Long Instrumented Fusion from L1 to Sacrum: Age Itself Does Not Independently Increase the Risk. Medicina 2024, 60, 1441. https://doi.org/10.3390/medicina60091441
Ahn J, Kim Y-H, Kim Y-C, Kim K-T, Kim S-M, Park JB, Ha K-Y. Analysis of Risk Factors Associated with Proximal Junctional Kyphosis Following Long Instrumented Fusion from L1 to Sacrum: Age Itself Does Not Independently Increase the Risk. Medicina. 2024; 60(9):1441. https://doi.org/10.3390/medicina60091441
Chicago/Turabian StyleAhn, Joonghyun, Young-Hoon Kim, Yong-Chan Kim, Ki-Tack Kim, Sung-Min Kim, Jun Bum Park, and Kee-Yong Ha. 2024. "Analysis of Risk Factors Associated with Proximal Junctional Kyphosis Following Long Instrumented Fusion from L1 to Sacrum: Age Itself Does Not Independently Increase the Risk" Medicina 60, no. 9: 1441. https://doi.org/10.3390/medicina60091441
APA StyleAhn, J., Kim, Y.-H., Kim, Y.-C., Kim, K.-T., Kim, S.-M., Park, J. B., & Ha, K.-Y. (2024). Analysis of Risk Factors Associated with Proximal Junctional Kyphosis Following Long Instrumented Fusion from L1 to Sacrum: Age Itself Does Not Independently Increase the Risk. Medicina, 60(9), 1441. https://doi.org/10.3390/medicina60091441






