The Role of DNA Repair (XPC, XPD, XPF, and XPG) Gene Polymorphisms in the Development of Myeloproliferative Neoplasms
Abstract
1. Introduction
2. Materials and Methods
2.1. Research Ethics Considerations
2.2. Patients and Controls
2.3. SNP Selection
2.4. Sample Collection and Processing
2.5. Statistical Methods
3. Results
3.1. Demographic Characteristics
3.2. Distribution of Investigated XPC, XPD, XPF, and XPG SNPs in MPN Patients and Controls
3.3. Possible Predictors for Patients Outcome
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ALL | Acute lymphoblastic leukemia |
| AML | Acute myeloid leukemia |
| CALR | Calreticulin |
| CML | Chronic myeloid leukemia |
| ET | Essential thrombocythemia |
| HL | Hodgkin’s Lymphoma |
| HU | Hydroxyurea |
| JAK2 | Janus kinase 2 |
| MAF | Minor Allele Frequency |
| MPL | Myeloproliferative leukemia virus oncogene |
| MPN | Myeloproliferative neoplasms |
| NHL | Non-Hodgkin’s Lymphoma |
| NER | Nucleotide excision repair |
| PMF | Primary myelofibrosis |
| PV | Polycythemia vera |
| PCR-RFLP | Polymerase chain reaction–restriction fragment length polymorphism |
| SNP | Single nucleotide polymorphism |
| WHO | World Health Organization |
| XP | Xeroderma pigmentosum |
| XPC | Xeroderma pigmentosum complementation |
| UV | Ultraviolet |
References
- Trifa, A.P.; Lighezan, D.L.; Jucan, C.; Tripon, F.; Arbore, D.R.; Bojan, A.; Gligor-Popa, Ș.; Pop, R.M.; Dima, D.; Bănescu, C. SH2B3 (LNK) Rs3184504 Polymorphism Is Correlated with JAK2 V617F-Positive Myeloproliferative Neoplasms. Rev. Romana Med. Lab. 2020, 28, 267–277. [Google Scholar] [CrossRef]
- Boddu, P.; Chihara, D.; Masarova, L.; Pemmaraju, N.; Patel, K.P.; Verstovsek, S. The Co-Occurrence of Driver Mutations in Chronic Myeloproliferative Neoplasms. Ann. Hematol. 2018, 97, 2071–2080. [Google Scholar] [CrossRef]
- Bellanné-Chantelot, C.; Rabadan Moraes, G.; Schmaltz-Panneau, B.; Marty, C.; Vainchenker, W.; Plo, I. Germline Genetic Factors in the Pathogenesis of Myeloproliferative Neoplasms. Blood Rev. 2020, 42, 100710. [Google Scholar] [CrossRef]
- Rumi, E.; Cazzola, M. Diagnosis, Risk Stratification, and Response Evaluation in Classical Myeloproliferative Neoplasms. Blood 2017, 129, 680–692. [Google Scholar] [CrossRef] [PubMed]
- Barbui, T.; Thiele, J.; Gisslinger, H.; Kvasnicka, H.M.; Vannucchi, A.M.; Guglielmelli, P.; Orazi, A.; Tefferi, A. The 2016 WHO Classification and Diagnostic Criteria for Myeloproliferative Neoplasms: Document Summary and in-Depth Discussion. Blood Cancer J. 2018, 8, 15. [Google Scholar] [CrossRef]
- Lighezan, D.L.; Bojan, A.S.; Iancu, M.; Pop, R.M.; Gligor-Popa, Ș.; Tripon, F.; Cosma, A.S.; Tomuleasa, C.; Dima, D.; Zdrenghea, M.; et al. TET2 Rs1548483 SNP Associating with Susceptibility to Molecularly Annotated Polycythemia Vera and Primary Myelofibrosis. J. Pers. Med. 2020, 10, 259. [Google Scholar] [CrossRef]
- Frawley, T.; O’Brien, C.P.; Conneally, E.; Vandenberghe, E.; Percy, M.; Langabeer, S.E.; Haslam, K. Development of a Targeted Next-Generation Sequencing Assay to Detect Diagnostically Relevant Mutations of JAK2, CALR, and MPL in Myeloproliferative Neoplasms. Genet. Test. Mol. Biomark. 2018, 22, 98–103. [Google Scholar] [CrossRef]
- Tefferi, A. Myeloproliferative Neoplasms: A Decade of Discoveries and Treatment Advances: Myeloproliferative Neoplasms. Am. J. Hematol. 2016, 91, 50–58. [Google Scholar] [CrossRef]
- Trifa, A.P.; Bănescu, C.; Bojan, A.S.; Voina, C.M.; Popa, Ș.; Vișan, S.; Ciubean, A.D.; Tripon, F.; Dima, D.; Popov, V.M.; et al. MECOM, HBS1L-MYB, THRB-RARB, JAK2, and TERT Polymorphisms Defining the Genetic Predisposition to Myeloproliferative Neoplasms: A Study on 939 Patients. Am. J. Hematol. 2018, 93, 100–106. [Google Scholar] [CrossRef]
- Benavente, C.; Zocchi, L. DNA repair and epigenetic regulation in cancer. In Molecular Medicines for Cancer: Concepts and Applications of Nanotechnology, 1st ed.; Chitkara, D., Mittal, A., Mahato, R.I., Eds.; CRC Press Taylor & Francis Publishers: Boca Raton, FL, USA, 2018; Volume 1, pp. 529–561. Available online: https://escholarship.org/uc/item/9j37f638 (accessed on 10 December 2023).
- Wu, Y.; Lu, Z.P.; Zhang, J.J.; Liu, D.F.; Shi, G.D.; Zhang, C.; Qin, Z.Q.; Zhang, J.Z.; He, Y.; Wu, P.F.; et al. Association between ERCC2 Lys751Gln Polymorphism and the Risk of Pancreatic Cancer, especially among Asians: Evidence from a Meta-Analysis. Oncotarget 2017, 8, 50124–50132. [Google Scholar] [CrossRef]
- Carbone, M.; Arron, S.T.; Beutler, B.; Bononi, A.; Cavenee, W.; Cleaver, J.E.; Croce, C.M.; D’Andrea, A.; Foulkes, W.D.; Gaudino, G.; et al. Tumour Predisposition and Cancer Syndromes as Models to Study Gene-Environment Interactions. Nat. Rev. Cancer 2020, 20, 533–549. [Google Scholar] [CrossRef] [PubMed]
- ElMahgoub, I.R.; Gouda, H.M.; Samra, M.A.; Shaheen, I.A.; ElMaraashly, A.H. Polymorphisms of Xeroderma Pigmentosum Genes (XPC, XPD, and XPG) and Susceptibility to Acute Leukemia among a Sample of Egyptian Patients. J. Hematop. 2017, 10, 3–7. [Google Scholar] [CrossRef]
- Rahimian, E.; Amini, A.; Alikarami, F.; Pezeshki, S.M.S.; Saki, N.; Safa, M. DNA Repair Pathways as Guardians of the Genome: Therapeutic Potential and Possible Prognostic Role in Hematologic Neoplasms. DNA Repair 2020, 96, 102951. [Google Scholar] [CrossRef] [PubMed]
- Santiago, S.P.; Junior, H.L.R.; de Sousa, J.C.; de Paula Borges, D.; de Oliveira, R.T.G.; Farias, I.R.; Costa, M.B.; Maia, A.R.S.; da Nóbrega Ito, M.; Magalhães, S.M.M.; et al. New Polymorphisms of Xeroderma Pigmentosum DNA Repair Genes in Myelodysplastic Syndrome. Leuk. Res. 2017, 58, 73–82. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.Q.; Lu, M.Y.; Liu, B. Polymorphisms in XPC Gene and Risk of Uterine Leiomyoma in Reproductive Women. Pathol. Oncol. Res. 2020, 26, 1459–1464. [Google Scholar] [CrossRef]
- Xie, C.; Zhao, J.; Hua, W.; Tan, P.; Chen, Y.; Rui, J.; Sun, X.; Fan, J.; Wei, X.; Xu, X.; et al. Effect of XPC Polymorphisms on the Response to Platinum-Based Chemotherapy: A Meta-Analysis. OncoTargets Ther. 2019, 12, 3839–3848. [Google Scholar] [CrossRef]
- Jiang, X.; Zhou, L.T.; Zhang, S.C.; Chen, K. XPC Polymorphism Increases Risk of Digestive System Cancers: Current Evidence from A Meta-Analysis. Chin. J. Cancer Res. 2012, 24, 181–189. [Google Scholar] [CrossRef][Green Version]
- He, B.S.; Xu, T.; Pan, Y.Q.; Wang, H.J.; Cho, W.C.; Lin, K.; Sun, H.L.; Gao, T.Y.; Wang, S.K. Nucleotide Excision Repair Pathway Gene Polymorphisms Are Linked to Breast Cancer Risk in a Chinese Population. Oncotarget 2016, 7, 84872–84882. [Google Scholar] [CrossRef]
- He, J.; Shi, T.Y.; Zhu, M.L.; Wang, M.Y.; Li, Q.X.; Wei, Q.Y. Associations of Lys939Gln and Ala499Val Polymorphisms of the XPC Gene with Cancer Susceptibility: A Meta-Analysis: XPC Lys939Gln and Ala499Val with Cancer Susceptibility. Int. J. Cancer 2013, 133, 1765–1775. [Google Scholar] [CrossRef]
- de Verdier, P.J.; Sanyal, S.; Bermejo, J.L.; Steineck, G.; Hemminki, K.; Kumar, R. Genotypes, Haplotypes and Diplotypes of Three XPC Polymorphisms in Urinary-Bladder Cancer Patients. Mutat. Res. 2010, 694, 39–44. [Google Scholar] [CrossRef]
- Wang, Y.; Li, Z.; Liu, N.; Zhang, G. Association between CCND1 and XPC Polymorphisms and Bladder Cancer Risk: A Meta-Analysis Based on 15 Case-Control Studies. Tumour Biol. 2014, 35, 3155–3165. [Google Scholar] [CrossRef] [PubMed]
- Sankhwar, M.; Sankhwar, S.N.; Bansal, S.K.; Gupta, G.; Rajender, S. Polymorphisms in the XPC Gene Affect Urinary Bladder Cancer Risk: A Case-Control Study, Meta-Analyses and Trial Sequential Analyses. Sci. Rep. 2016, 6, 27018. [Google Scholar] [CrossRef]
- D’Amelio, A.M., Jr.; Monroy, C.; El-Zein, R.; Etzel, C.J. Using Haplotype Analysis to Elucidate Significant Associations between Genes and Hodgkin Lymphoma. Leuk. Res. 2012, 36, 1359–1364. [Google Scholar] [CrossRef]
- Monroy, C.M.; Cortes, A.C.; Lopez, M.; Rourke, E.; Etzel, C.J.; Younes, A.; Strom, S.S.; El-Zein, R. Hodgkin Lymphoma Risk: Role of Genetic Polymorphisms and Gene-Gene Interactions in DNA Repair Pathways. Mol. Carcinog. 2011, 50, 825–834. [Google Scholar] [CrossRef]
- Hernández-Boluda, J.C.; Pereira, A.; Cervantes, F.; Alvarez-Larrán, A.; Collado, M.; Such, E.; Arilla, M.J.; Boqué, C.; Xicoy, B.; Maffioli, M.; et al. A Polymorphism in the XPD Gene Predisposes to Leukemic Transformation and New Nonmyeloid Malignancies in Essential Thrombocythemia and Polycythemia Vera. Blood 2012, 119, 5221–5228. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Douzi, K.; Ouerhani, S.; Menif, S.; Safra, I.; Abbes, S. Polymorphisms in XPC, XPD and XPG DNA Repair Genes and Leukemia Risk in a Tunisian Population. Leuk. Lymphoma 2015, 56, 1856–1862. [Google Scholar] [CrossRef]
- Zhao, Z.; Zhang, A.; Zhao, Y.; Xiang, J.; Yu, D.; Liang, Z.; Xu, C.; Zhang, Q.; Li, J.; Duan, P. The Association of Polymorphisms in Nucleotide Excision Repair Genes with Ovarian Cancer Susceptibility. Biosci. Rep. 2018, 38, BSR20180114. [Google Scholar] [CrossRef] [PubMed]
- Bănescu, C.; Iancu, M.; Trifa, A.P.; Dobreanu, M.; Moldovan, V.G.; Duicu, C.; Tripon, F.; Crauciuc, A.; Skypnyk, C.; Bogliș, A.; et al. Influence of XPC, XPD, XPF, and XPG Gene Polymorphisms on the Risk and the Outcome of Acute Myeloid Leukemia in a Romanian Population. Tumour Biol. 2016, 37, 9357–9366. [Google Scholar] [CrossRef]
- Chen, S.; Zhu, J.H.; Wang, F.; Huang, S.Y.; Xue, W.Q.; Cui, Z.; He, J.; Jia, W.H. Association of the Asp312Asn and Lys751Gln Polymorphisms in the XPD Gene with the Risk of Non-Hodgkin’s Lymphoma: Evidence from a Meta-Analysis. Chin. J. Cancer 2015, 34, 108–114. [Google Scholar] [CrossRef] [PubMed]
- Strom, S.S.; Estey, E.; Outschoorn, U.M.; Garcia-Manero, G. Acute Myeloid Leukemia Outcome: Role of Nucleotide Excision Repair Polymorphisms in Intermediate Risk Patients. Leuk. Lymphoma 2010, 51, 598–605. [Google Scholar] [CrossRef]
- Dhangar, S.; Shanbhag, V.; Shanmukhaiah, C.; Vundinti, B.R. Lack of Association between Functional Polymorphism of DNA Repair Genes (XRCC1, XPD) and Clinical Response in Indian Chronic Myeloid Leukemia Patients. Mol. Biol. Rep. 2019, 46, 4997–5003. [Google Scholar] [CrossRef]
- Bănescu, C.; Trifa, A.P.; Demian, S.; Benedek Lazar, E.; Dima, D.; Duicu, C.; Dobreanu, M. Polymorphism of XRCC1, XRCC3, and XPD Genes and Risk of Chronic Myeloid Leukemia. Biomed Res. Int. 2014, 2014, 213790. [Google Scholar] [CrossRef] [PubMed]
- Poletto, V.; Villani, L.; Catarsi, P.; Campanelli, R.; Massa, M.; Vannucchi, A.M.; Rosti, V.; Barosi, G. No Association between the XPD Lys751Gln (Rs13181) Polymorphism and Disease Phenotype or Leukemic Transformation in Primary Myelofibrosis. Haematologica 2013, 98, e83-4. [Google Scholar] [CrossRef] [PubMed]
- Batar, B.; Güven, M.; Bariş, S.; Celkan, T.; Yildiz, I. DNA Repair Gene XPD and XRCC1 Polymorphisms and the Risk of Childhood Acute Lymphoblastic Leukemia. Leuk. Res. 2009, 33, 759–763. [Google Scholar] [CrossRef]
- Sorour, A.; Ayad, M.W.; Kassem, H. The Genotype Distribution of the XRCC1, XRCC3, and XPD DNA Repair Genes and Their Role for the Development of Acute Myeloblastic Leukemia. Genet. Test. Mol. Biomark. 2013, 17, 195–201. [Google Scholar] [CrossRef]
- Liu, Y.; Cao, L.; Chang, J.; Lin, J.; He, B.; Rao, J.; Zhang, Z.; Zhang, X. XPF-673C>T Polymorphism Effect on the Susceptibility to Esophageal Cancer in Chinese Population. PLoS ONE 2014, 9, e94136. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Chen, S.; Zhou, H.; Zhang, T.; Liu, Y.; He, J.; Zhu, J.; Ruan, J. XPG Rs17655 G>C Polymorphism Associated with Cancer Risk: Evidence from 60 Studies. Aging 2018, 10, 1073–1088. [Google Scholar] [CrossRef]
- Senghore, T.; Chien, H.T.; Wang, W.C.; Chen, Y.X.; Young, C.K.; Huang, S.F.; Yeh, C.C. Polymorphisms in ERCC5 Rs17655 and ERCC1 Rs735482 Genes Associated with the Survival of Male Patients with Postoperative Oral Squamous Cell Carcinoma Treated with Adjuvant Concurrent Chemoradiotherapy. J. Clin. Med. 2019, 8, 33. [Google Scholar] [CrossRef]
- Feng, Y.B.; Fan, D.Q.; Yu, J.; Bie, Y.K. Association between XPG Gene Polymorphisms and Development of Gastric Cancer Risk in a Chinese Population. Genet. Mol. Res. 2016, 15, 2. [Google Scholar] [CrossRef]
- Du, H.; Zhang, X.; Du, M.; Guo, N.; Chen, Z.; Shu, Y.; Zhang, Z.; Wang, M.; Zhu, L. Association Study between XPG Asp1104His Polymorphism and Colorectal Cancer Risk in a Chinese Population. Sci. Rep. 2014, 4, 6700. [Google Scholar] [CrossRef]
- Ming-Shiean, H.; Yu, J.C.; Wang, H.W.; Chen, S.T.; Hsiung, C.N.; Ding, S.L.; Wu, P.E.; Shen, C.Y.; Cheng, C.W. Synergistic Effects of Polymorphisms in DNA Repair Genes and Endogenous Estrogen Exposure on Female Breast Cancer Risk. Ann. Surg. Oncol. 2010, 17, 760–771. [Google Scholar] [CrossRef]
- Arber, D.A.; Orazi, A.; Hasserjian, R.; Thiele, J.; Borowitz, M.J.; Le Beau, M.M.; Bloomfield, C.D.; Cazzola, M.; Vardiman, J.W. The 2016 Revision to the World Health Organization Classification of Myeloid Neoplasms and Acute Leukemia. Blood 2016, 127, 2391–2405. [Google Scholar] [CrossRef] [PubMed]
- Recensământul Populației și Caselor, Om cu Om, Casă cu Casă (The Census of Population and Houses, Person by Person, House by House). Available online: https://www.recensamantromania.ro/rezultate-rpl-2021/rezultate-definitive-caracteristici-demografice/ (accessed on 4 March 2024).
- Ensembl Genome Browser 111. Available online: https://www.ensembl.org/index.html (accessed on 3 March 2024).
- Berhane, N.; Sobti, R.C.; Mahdi, S.A. DNA Repair Genes Polymorphism (XPG and XRCC1) and Association of Prostate Cancer in a North Indian Population. Mol. Biol. Rep. 2012, 39, 2471–2479. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Wang, H.; Lin, T.; Wei, Q.; Zhi, Y.; Yuan, F.; Song, B.; Yang, J.; Chen, Z. Interactions between Cigarette Smoking and XPC-PAT Genetic Polymorphism Enhance Bladder Cancer Risk. Oncol. Rep. 2012, 28, 337–345. [Google Scholar] [CrossRef] [PubMed]
- Seedhouse, C.; Bainton, R.; Lewis, M.; Harding, A.; Russell, N.; Das-Gupta, E. The Genotype Distribution of the XRCC1 Gene Indicates a Role for Base Excision Repair in the Development of Therapy-Related Acute Myeloblastic Leukemia. Blood 2002, 100, 3761–3766. [Google Scholar] [CrossRef]
- Jones, A.V.; Kreil, S.; Zoi, K.; Waghorn, K.; Curtis, C.; Zhang, L.; Score, J.; Seear, R.; Chase, A.J.; Grand, F.H.; et al. Widespread Occurrence of the JAK2 V617F Mutation in Chronic Myeloproliferative Disorders. Blood 2005, 106, 2162–2168. [Google Scholar] [CrossRef]
- Trifa, A.P.; Cucuianu, A.; Popp, R.A. Familial Essential Thrombocythemia Associated with MPL W515L Mutation in Father and JAK2 V617F Mutation in Daughter. Case Rep. Hematol. 2014, 2014, 841787. [Google Scholar] [CrossRef]
- Masselli, E.; Pozzi, G.; Gobbi, G.; Merighi, S.; Gessi, S.; Vitale, M.; Carubbi, C. Cytokine Profiling in Myeloproliferative Neoplasms: Overview on Phenotype Correlation, Outcome Prediction, and Role of Genetic Variants. Cells 2020, 9, 2136. [Google Scholar] [CrossRef]
- Hasselbalch, H.C.; Elvers, M.; Schafer, A.I. The pathobiology of thrombosis, microvascular disease, and hemorrhage in the myeloproliferative neoplasms. Blood 2021, 137, 2152–2160. [Google Scholar] [CrossRef] [PubMed]
- Farina, M.; Russo, D.; Hoffman, R. The possible role of mutated endothelial cells in myeloproliferative neoplasms. Haematologica 2021, 106, 2813–2823. [Google Scholar] [CrossRef]
- Thakkar, D.N.; Kodidela, S.; Sandhiya, S.; Dubashi, B.; Dkhar, S.A. A Polymorphism Located near PMAIP1/Noxa Gene Influences Susceptibility to Hodgkin Lymphoma Development in South India. Asian Pac. J. Cancer Prev. 2017, 18, 2477–2483. [Google Scholar] [CrossRef]
- Kim, H.N.; Kim, N.Y.; Yu, L.; Kim, Y.-K.; Lee, I.K.; Yang, D.H.; Lee, J.J.; Shin, M.H.; Park, K.S.; Choi, J.S.; et al. Polymorphisms in DNA Repair Genes and MDR1 and the Risk for Non-Hodgkin Lymphoma. Int. J. Mol. Sci. 2014, 15, 6703–6716. [Google Scholar] [CrossRef]
- Bahceci, A.; Paydas, S.; Tanriverdi, K.; Ergin, M.; Seydaoglu, G.; Ucar, G. DNA Repair Gene Polymorphisms in B Cell Non-Hodgkin’s Lymphoma. Tumour Biol. 2015, 36, 2155–2161. [Google Scholar] [CrossRef]
- El-Zein, R.; Monroy, C.M.; Etzel, C.J.; Cortes, A.C.; Xing, Y.; Collier, A.L.; Strom, S.S. Genetic Polymorphisms in DNA Repair Genes as Modulators of Hodgkin Disease Risk. Cancer 2009, 115, 1651–1659. [Google Scholar] [CrossRef]
- Guillem, V.M.; Cervantes, F.; Martínez, J.; Alvarez-Larrán, A.; Collado, M.; Camós, M.; Sureda, A.; Maffioli, M.; Marugán, I.; Hernández-Boluda, J.-C. XPC Genetic Polymorphisms Correlate with the Response to Imatinib Treatment in Patients with Chronic Phase Chronic Myeloid Leukemia. Am. J. Hematol. 2010, 85, 482–486. [Google Scholar] [CrossRef]
- Liu, D.; Wu, D.; Li, H.; Dong, M. The Effect of XPD/ERCC2 Lys751Gln Polymorphism on Acute Leukemia Risk: A Systematic Review and Meta-Analysis. Gene 2014, 538, 209–216. [Google Scholar] [CrossRef]
- Björkholm, M.; Hultcrantz, M.; Derolf, Å.R. Leukemic Transformation in Myeloproliferative Neoplasms: Therapy-Related or Unrelated? Best Pract. Res. Clin. Haematol. 2014, 27, 141–153. [Google Scholar] [CrossRef]
- Chen, Y.; Zheng, T.; Lan, Q.; Kim, C.; Qin, Q.; Foss, F.; Chen, X.; Holford, T.; Leaderer, B.; Boyle, P.; et al. Polymorphisms in DNA Repair Pathway Genes, Body Mass Index, and Risk of Non-Hodgkin Lymphoma. Am. J. Hematol. 2013, 88, 606–611. [Google Scholar] [CrossRef]
- Wang, S.S.; Maurer, M.J.; Morton, L.M.; Habermann, T.M.; Davis, S.; Cozen, W.; Lynch, C.F.; Severson, R.K.; Rothman, N.; Chanock, S.J.; et al. Polymorphisms in DNA Repair and One-Carbon Metabolism Genes and Overall Survival in Diffuse Large B-Cell Lymphoma and Follicular Lymphoma. Leukemia 2009, 23, 596–602. [Google Scholar] [CrossRef][Green Version]
- Özcan, A.; Pehlivan, M.; Tomatir, A.G.; Karaca, E.; Özkinay, C.; Özdemir, F.; Pehlivan, S. Polymorphisms of the DNA Repair Gene XPD (751) and XRCC1 (399) Correlates with Risk of Hematological Malignancies in Turkish Population. Afr. J. Biotechnol. 2011, 10, 8860–8870. [Google Scholar] [CrossRef]
- Shao, M.; Ma, H.; Wang, Y.; Xu, L.; Yuan, J.; Wang, Y.; Hu, Z.; Yang, L.; Wang, F.; Liu, H.; et al. Polymorphisms in excision repair cross-complementing group 4 (ERCC4) and susceptibility to primary lung cancer in a Chinese Han population. Lung Cancer 2008, 60, 332–339. [Google Scholar] [CrossRef] [PubMed]
- Yu, D.K.; Wu, C.; Tan, W.; Lin, D. Functional XPF polymorphisms associated with lung cancer susceptibility in a Chinese population. Front. Med. China. 2010, 4, 82–89. [Google Scholar] [CrossRef]
- Ruiz-Cosano, J.; Torres-Moreno, D.; Conesa-Zamora, P. Influence of Polymorphisms in ERCC5, XPA and MTR DNA Repair and Synthesis Genes in B-Cell Lymphoma Risk. A Case-Control Study in Spanish Population. J. BUON 2013, 18, 486–490. [Google Scholar]
- Al Sayed Ahmed, H.; Raslan, W.F.; Deifalla, A.H.S.; Fathallah, M.D. Overall Survival of Classical Hodgkins Lymphoma in Saudi Patients Is Affected by XPG Repair Gene Polymorphism. Biomed. Rep. 2019, 10, 10–16. [Google Scholar] [CrossRef]
- Broséus, J.; Park, J.H.; Carillo, S.; Hermouet, S.; Girodon, F. Presence of calreticulin mutations in JAK2-negative polycythemia vera. Blood 2014, 124, 3964–3966. [Google Scholar] [CrossRef]
- Gavande, N.S.; VanderVere-Carozza, P.S.; Hinshaw, H.D.; Jalal, S.I.; Sears, C.R.; Pawelczak, K.S.; Turchi, J.J. DNA repair targeted therapy: The past or future of cancer treatment? Pharmacol. Ther. 2016, 160, 65–83. [Google Scholar] [CrossRef] [PubMed]
- Prosz, A.; Duan, H.; Tisza, V.; Sahgal, P.; Topka, S.; Klus, G.T.; Börcsök, J.; Sztupinszki, Z.; Hanlon, T.; Diossy, M.; et al. Nucleotide excision repair deficiency is a targetable therapeutic vulnerability in clear cell renal cell carcinoma. Sci. Rep. 2023, 13, 20567. [Google Scholar] [CrossRef]
- Szalat, R.; Samur, M.K.; Fulciniti, M.; Lopez, M.; Nanjappa, P.; Cleynen, A.; Wen, K.; Kumar, S.; Perini, T.; Calkins, A.S.; et al. Nucleotide excision repair is a potential therapeutic target in multiple myeloma. Leukemia 2018, 32, 111–119. [Google Scholar] [CrossRef] [PubMed]
| Variable | MPN Patients (n = 393) | Controls (n = 323) | p-Value |
|---|---|---|---|
| Gender | |||
| Male gender [n (%)] | 188 (47.8) | 155 (48) | 0.96 |
| Female gender [n (%)] | 205 (52.2) | 168 (52) | |
| Age | |||
| Age at diagnosis, years; median | 60 (17–85) | 56.15 (25–94) | |
| ≥60 [n (%)] | 199 (50.6) | 194 (49.4) | 0.11 |
| <60 [n (%)] | 194 (49.4) | 179 (55.4) |
| Gene Polymorphism | rs ID | MAF | Risk Allele Frequency ALL | Risk Allele Frequency in Europe | Most Severe Consequence | Clinical Significance | ||
|---|---|---|---|---|---|---|---|---|
| WT-Allele | Variant | WT-Allele | Variant | |||||
| XPC 1496C>T | rs2228000 | 0.48 | G—0.77 | A—0.23 | G—0.74 | A—0.26 | Missense variant | Benign |
| XPC 2920A>C | rs2228001 | 0.49 | G—0.32 | T—0.66 | G—0.40 | T—0.60 | Missense variant | Benign, likely benign |
| XPD 2251A>C | rs13181 | 0.45 | T—0.76 | G—0.24 | T—0.64 | G—0.36 | Stop gained | Benign, likely benign |
| XPF-673C>T | rs3136038 | 0.49 | C—0.66 | T—0.34 | C—0.66 | T—0.34 | TF binding site | - |
| XPF 11985A>G | rs254942 | 0.25 | G—0.05 | A—0.95 | G—0.02 | A—0.98 | Splice region variant | Benign |
| XPG 3507G>C | rs17655 | 0.5 | G—0.64 | C—0.36 | G—0.75 | C—0.25 | Missense variant | Benign |
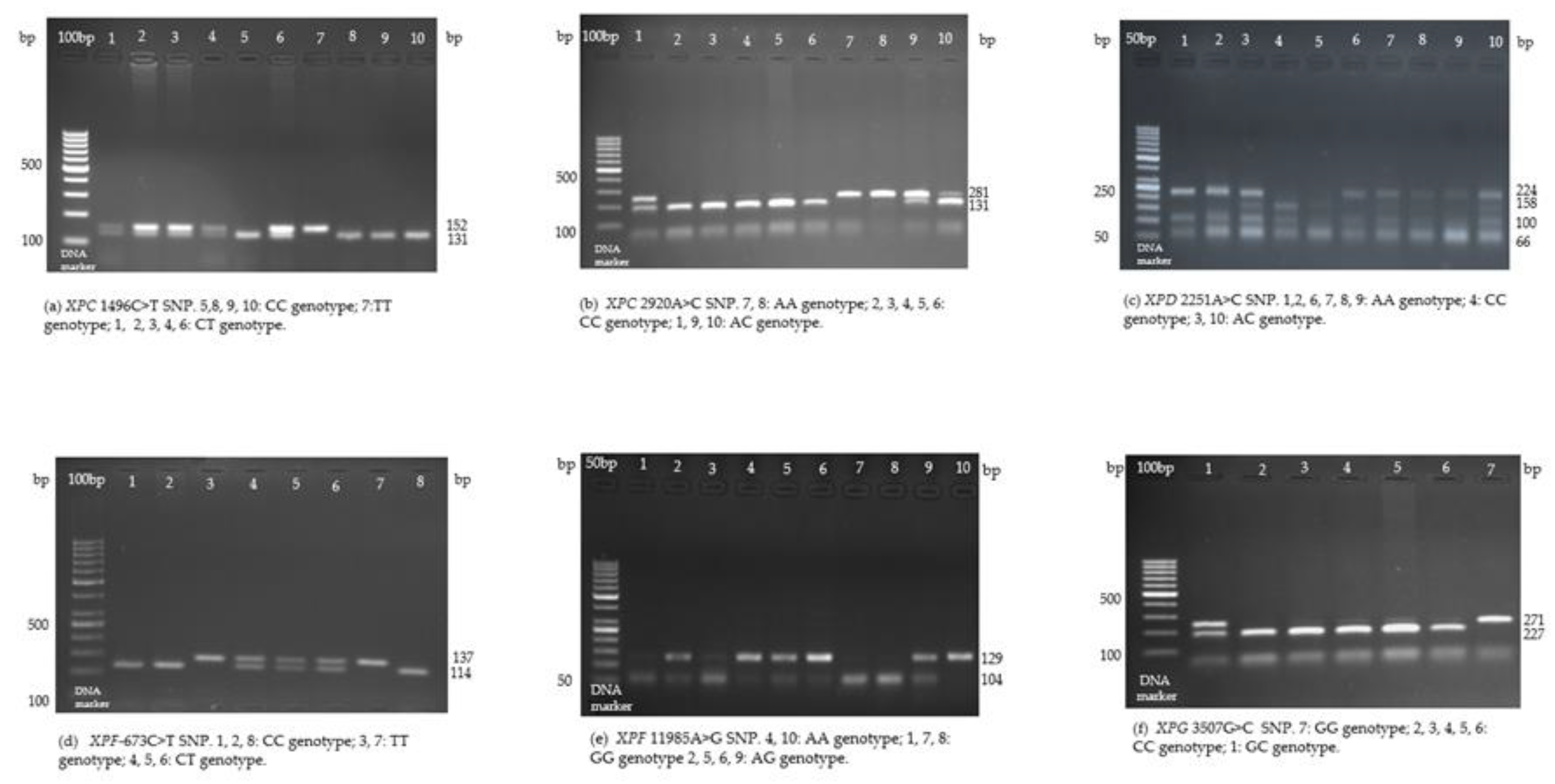
| Gene Polymorphism | Restriction Enzyme Used | Base Pair Change | Genotype | Length (bp) | Primers Sequences |
|---|---|---|---|---|---|
| XPC 1496C>T (XPC Ala499Val, rs2228000) | Cfr42I (SacII) | C→T | CC | 131, 21 | Fw: TAA GGA CCC AAG CTT GCC CG Rev: CCC ACT TTT CCT CCT GCT CAC AG |
| CT | 152, 131, 21 | ||||
| TT | 152 | ||||
| XPC 2920A>C (XPC Lys939Gln, rs2228001) | Pvu II | A→C | AA | 281 | Fw: GAT GCA GGA GGT GGA CTC TCT Rev: GTA GTG GGG CAG CAG CAA CT |
| AC | 281, 150, 131 | ||||
| CC | 150, 131 | ||||
| XPD 2251A>C (XPD Lys751Gln, rs13181) | Pst I | A→C | AA | 224, 100 | Fw: TC CTG TCC CTA CTG GCC ATT C Rev: GT GGA CGT GAC AGT GAG AAA T |
| AC | 224, 158, 100, 66 | ||||
| CC | 158, 100, 66 | ||||
| XPF-673C>T (rs3136038) | EcoRI | C→T | CC | 114, 23 | Fw: GGG AGG CAA ACA GAG GTC TGA ATT Rev: TGC GAT TAC TCC CCA TCC TTC TT |
| CT | 137, 114, 23 | ||||
| TT | 137 | ||||
| XPF 11985A>G (rs254942) | RsaI | A→G | AA | 129 | Fw: GGA GTC AAG AAA CAG CCA ACC TAG TA Rev: AGG AAG ACA GGA TGA CAG CCA G |
| AG | 129, 104, 25 | ||||
| GG | 104, 25 | ||||
| XPG 3597G>C (XPG Asp1104His, rs17655) | NlaIII (Hin1 II) | G→C | GG | 271 | Fw: GAC CTG CCT CTC AGA ATC ATC Rev: CCT CGC ACG TCT TAG TTT CC |
| GC | 271, 227, 44 | ||||
| CC | 227, 44 |
| Characteristics | Patients with PV (n = 153) | Patients with ET (n = 201) | Patients with PMF (n = 39) | All Patients (n = 393) |
|---|---|---|---|---|
| Age at diagnosis, years, median (range) | 59 (17–80) | 60 (18–85) | 59 (34–76) | 60 (17–85) |
| < 30 [n (%)] | 10 (6.54) | 7 (3.49) | - | 17 (4.32) |
| 30–49 [n (%)] | 29 (18.95) | 48 (23.89) | 7 (17.95) | 84 (21.38) |
| 50–69 [n (%)] | 85 (55.55) | 94 (46.77) | 27 (69.23) | 206 (52.42) |
| ≥ 70 [n (%)] | 29 (18.96) | 52 (25.87) | 5 (12.82) | 86 (21.88) |
| Gender | ||||
| Male [n (%)] | 94 (61.43) | 75 (37.31) | 19 (48.71) | 188 (47.83) |
| Female [n (%)] | 59 (38.57) | 126 (62.69) | 20 (51.29) | 205 (52.17) |
| Blood counts | ||||
| Hemoglobin (g/dL), median (range) | 17.2 (7.7–22.7) | 13.2 (4.8–20) | 10 (5.9–14.5) | 14.4 (4.8–22.7) |
| Hemoglobin < 10 g/dL [n (%)] | 3 (1.96) | 35 (17.41) | 19 (48.72) | 57 (14.50) |
| Hemoglobin 10–16.5 g/dL [n (%)] | 54 (35.30) | 160 (79.61) | 20 (51.28) | 234 (59.53) |
| Hemoglobin > 16.5 g/dL [n (%)] | 96 (62.74) | 6 (2.98) | - | 106 (26.97) |
| Hematocrit value, median (range) | 50.91 (24.3–73.4) | 39.5 (6.29–55.6) | 31.7 (18.9–46.3) | 43.4 (6.29–73.4) |
| Hematocrit > 49 [n (%)] | 89 (58.17) | 13 (6.47) | 0 | 102 (25.95) |
| Hematocrit ≤ 49 [n (%)] | 64 (41.83) | 188 (93.53) | 39 (100) | 291 (74.05) |
| Red blood cells median (range) | 5.74 (2.7–9.3) | 4.37 (1.86–9) | 3.41 (2.22–5.63) | 4.71 (1.86–9.3) |
| Platelets (×109/L), median (range) | 282 (77–1619) | 720 (34–3160) | 260 (4–1167) | 543 (4–3160) |
| Platelets < 100 × 109/L [n (%)] | 3 (1.97) | 1 (0.49) | 8 (20.51) | 13 (3.3) |
| Platelets 100–450 × 109/L [n (%)] | 113 (73.85) | 16 (7.96) | 25 (64.11) | 154 (39.19) |
| Platelets > 450 × 109/L [n (%)] | 37 (24.18) | 184 (91.55) | 6 (15.38) | 226 (57.51) |
| Leukocytes (×109/L), median (range) | 9.88 (3.44–182.3) | 9.51 (3.59–113.83) | 9.5 (0.6–82.30) | 9.67 (0.6–182.3) |
| Leukocytes < 11 × 109/L [n (%)] | 88 (57.51) | 125 (62.19) | 22 (56.41) | 235 (59.8) |
| Leukocytes ≥ 11 × 109/L [n (%)] | 65 (42.48) | 76 (37.81) | 17 (43.58) | 158 (40.20) |
| Leukocytes 11–15 × 109/L [n (%)] | 30 (19.6) | 44 (21.89) | 6 (15.38) | 80 (22.36) |
| Leukocytes ≥ 15 × 109/L [n (%)] | 35 (22.87) | 32 (15.92) | 11 (28.20) | 78 (19.84) |
| Leukocytes 15–25 × 109/L [n (%)] | 24 (15.7) | 19 (9.45) | 5 (12.82) | 48 (12.21) |
| Leukocytes ≥ 25 × 109/L [n (%)] | 11 (7.19) | 13 (6.47) | 6 (15.39) | 30 (7.63) |
| LDH median U/L (range) | 284 (102–2015) | 308 (113–2197) | 379 (130–3098) | 307 (102–3098) |
| Driver mutational status | ||||
| JAK2 mutation [n (%)] | 69 (45.09) | 88 (43.78) | 17 (43.59) | 174 (44.27) |
| CALR mutation [n (%)] | 1 (0.65) | 37 (18.4) | 8 (20.51) | 46 (11.7) |
| 2x-negative [n (%)] | 68 (44.44) | 72 (35.8) | 13 (33.33) | 153 (38.93) |
| Constitutional symptoms [n (%)] | 73 (47.71) | 99 (49.25) | 25 (64.1) | 197 (50.12) |
| Palpable splenomegaly [n (%)] | 66 (43.13) | 66 (32.83) | 29 (74.35) | 161 (40.96) |
| History of any thrombosis [n (%)] | 47 (30.71) | 61 (30.34) | 10 (25.64) | 118 (30.02) |
| History of venous thrombosis [n (%)] | 22 (14.37) | 22 (10.94) | 8 (20.51) | 52 (13.23) |
| History of arterial thrombosis [n (%)] | 32 (20.91) | 43 (21.39) | 5 (12.82) | 80 (20.35) |
| History of bleeding [n (%)] | 6 (3.92) | 14 (6.96) | 5 (12.82) | 25 (6.35) |
| Leukemic transformations [n (%)] | 8 (5.22) | 15 (7.46) | 9 (23.07) | 32 (8.11) |
| MPN Patients n-393 (%) | Controls n-323 (%) | Crude OR (95% CI) | p-Value | |
|---|---|---|---|---|
| XPC 1496C>T (rs2228000, Ala499Val) | ||||
| CC | 180 (45.8) | 148 (45.8) | Ref. | Ref. |
| CT | 134 (34.1) | 108 (33.4) | 1.02 (0.731–1.425) | 0.907 |
| TT | 79 (20.1) | 67 (20.7) | 0.969 (0.655–1.434) | 0.877 |
| CT + TT | 213 (54.2) | 175 (54.1) | 1.001 (0.745–1.345) | 0.996 |
| C allele | 494 (62.84) | 404 (62.53) | Ref. | Ref. |
| T allele | 292 (37.15) | 242 (37.46) | 0.986 (0.795–1.224) | 0.903 |
| XPC 2920A>C (rs2228000, XPC Lys939Gln) | ||||
| AA | 104 (26.5) | 79 (24.5) | Ref. | Ref. |
| AC | 204 (51.9) | 179 (55.4) | 0.866 (0.607–1.234) | 0.425 |
| CC | 85 (21.6) | 65 (20.1) | 0.993 (0.642–1.536) | 0.976 |
| AC + CC | 289 (73.5) | 244 (75.5) | 0.9 (0.641–1.262) | 0.541 |
| A allele | 412 (52.41) | 337 (52.17) | Ref. | Ref. |
| C allele | 374 (47.58) | 309 (47.83) | 0.99 (0.804–1.219) | 0.925 |
| XPD 2251A>C (rs13181, XPD Lys751Gln) | ||||
| AA | 147 (37.4) | 155 (48) | Ref. | Ref. |
| AC | 185 (47.1) | 104 (32.2) | 1.876 (1.349–2.608) | <0.001 |
| CC | 61 (15.5) | 64 (19.8) | 1.005 (0.662–1.525) | 0.981 |
| AC + CC | 246 (62.6) | 168 (52) | 1.544 (1.145–2.082) | 0.004 |
| A allele | 479 (60.94) | 414 (64.08) | Ref. | Ref. |
| C allele | 307 (39.05) | 232 (35.91) | 1.144 (0.922–1.418) | 0.222 |
| XPF-673C>T (rs3136038) | ||||
| CC | 212 (53.9) | 128 (39.6) | Ref. | Ref. |
| CT | 106 (27) | 129 (39.9) | 0.496 (0.354–0.696) | <0.001 |
| TT | 75 (19.1) | 66 (20.4) | 0.686 (0.461–1.020) | 0.062 |
| CT + TT | 181 (46.1) | 195 (60.3) | 0.56 (0.416–0.755) | <0.001 |
| C allele | 530 (67.43) | 385 (59.59) | Ref. | Ref. |
| T allele | 256 (32.56) | 261 (40.4) | 0.712 (0.573–0.884) | 0.002 |
| XPF 11985A>G (rs254942) | ||||
| AA | 313 (79.6) | 164 (50.8) | Ref. | Ref. |
| AG | 62 (15.8) | 109 (33.7) | 0.298 (0.207–0.429) | <0.001 |
| GG | 18 (4.6) | 50 (15.5) | 0.189 (0.107–0.334) | <0.001 |
| AG + GG | 80 (20.4) | 159 (49.2) | 0.264 (0.190–0.366) | <0.001 |
| A allele | 688 (87.53) | 437 (67.64) | Ref. | Ref. |
| G allele | 98 (12.46) | 209 (32.35) | 0.297 (0.227–0.389) | <0.001 |
| XPG 3507G>C (rs17655, XPG Asp1104His) | ||||
| GG | 236 (60.1) | 191 (59.1) | Ref. | Ref. |
| GC | 144 (36.6) | 118 (36.5) | 0.988 (0.725–1.346) | 0.937 |
| CC | 13 (3.3) | 14 (4.3) | 0.752 (0.345–1.637) | 0.471 |
| GC + CC | 157 (39.9) | 132 (40.8) | 0.963 (0.713–1.299) | 0.803 |
| G allele | 616 (78.37) | 500 (77.4) | Ref. | Ref. |
| C allele | 170 (21.62) | 146 (22.6) | 0.9452 (0.7356–1.215) | 0.658 |
| Characteristics | All Patients [n (%)] | XPC 1496C>T | XPC 2920A>C | XPD 2251A>C | XPF-673C>T | XPF 11985A>G | XPG 3507G>C | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CC | Variant TT + CT | p-Value | AA | Variant CC + AC | p-Value | AA | Variant TT + AC | p-Value | CC | Variant TT + CT | p-Value | AA | Variant GG + AG | p-Value | GG | Variant CC + GC | p-Value | ||
| Mutations | |||||||||||||||||||
| JAK2+ | 174 (44.27) | 86 | 88 | 0.2 | 42 | 132 | 0.35 | 60 | 114 | 0.29 | 96 | 78 | 0.66 | 140 | 34 | 0.72 | 105 | 69 | 0.92 |
| JAK2− | 219 (55.72) | 94 | 125 | 62 | 157 | 87 | 132 | 116 | 103 | 173 | 46 | 131 | 88 | ||||||
| CALR+ | 46 (11.7) | 21 | 25 | 0.98 | 12 | 34 | 0.95 | 18 | 28 | 0.8 | 28 | 18 | 0.32 | 40 | 6 | 0.19 | 30 | 16 | 0.45 |
| CALR− | 347 (88.29) | 159 | 188 | 92 | 255 | 129 | 218 | 184 | 163 | 273 | 74 | 206 | 141 | ||||||
| Subtype | |||||||||||||||||||
| PV | 153 (38.93) | 73 | 80 | 0.71 | 38 | 115 | 0.84 | 58 | 95 | 0.85 | 86 | 67 | 0.76 | 121 | 32 | 0.47 | 96 | 57 | 0.62 |
| ET | 201 (51.14) | 88 | 113 | 55 | 146 | 73 | 128 | 106 | 95 | 158 | 43 | 116 | 85 | ||||||
| MPF | 39 (9.92) | 19 | 20 | 11 | 28 | 16 | 23 | 20 | 19 | 34 | 5 | 24 | 15 | ||||||
| Gender | |||||||||||||||||||
| Male | 188 (47.8) | 83 | 105 | 0.53 | 49 | 139 | 0.86 | 69 | 119 | 0.78 | 104 | 84 | 0.6 | 144 | 44 | 0.15 | 119 | 69 | 0.21 |
| Female | 205 (52.2) | 97 | 108 | 55 | 150 | 78 | 127 | 108 | 97 | 169 | 36 | 117 | 88 | ||||||
| Constitutional symptoms | |||||||||||||||||||
| Present | 197 (50.12) | 93 | 104 | 0.58 | 58 | 139 | 0.18 | 74 | 123 | 0.95 | 111 | 86 | 0.34 | 157 | 40 | 0.98 | 114 | 83 | 0.38 |
| Absent | 196 (49.87) | 87 | 109 | 46 | 150 | 73 | 123 | 101 | 95 | 156 | 40 | 122 | 74 | ||||||
| Palpable splenomegaly | |||||||||||||||||||
| Present | 161 (40.96) | 73 | 88 | 0.88 | 41 | 120 | 0.71 | 54 | 107 | 0.19 | 117 | 115 | 0.09 | 134 | 27 | 0.14 | 104 | 57 | 0.13 |
| Absent | 232 (59.03) | 107 | 125 | 63 | 169 | 93 | 139 | 95 | 66 | 179 | 53 | 132 | 100 | ||||||
| Exposure to cytoreductive agents | |||||||||||||||||||
| Agents alone or in combination | 160 (40.71) | 80 | 80 | 0.17 | 46 | 114 | 0.4 | 56 | 104 | 0.41 | 91 | 69 | 0.33 | 139 | 21 | 0.003 | 100 | 60 | 0.41 |
| No exposure | 233 (59.28) | 100 | 133 | 58 | 175 | 91 | 142 | 121 | 112 | 174 | 59 | 136 | 97 | ||||||
| Blood emissions | |||||||||||||||||||
| Yes | 24 | 20 | 0.22 | 11 | 33 | 0.82 | 10 | 34 | 0.03 | 25 | 19 | 0.69 | 37 | 7 | 0.44 | 31 | 13 | 0.14 | |
| No | 349 (88.8) | 156 | 193 | 93 | 256 | 137 | 212 | 187 | 162 | 276 | 73 | 205 | 144 | ||||||
| Aspirine | |||||||||||||||||||
| Yes | 150 (38.16) | 67 | 83 | 0.72 | 50 | 100 | 0.02 | 43 | 107 | 0.005 | 77 | 73 | 0.42 | 117 | 33 | 0.53 | 90 | 60 | 0.99 |
| No | 243 (61.83) | 113 | 130 | 54 | 189 | 104 | 139 | 135 | 108 | 196 | 47 | 146 | 97 | ||||||
| Interferon Alfa | |||||||||||||||||||
| Yes | 5 (1.27) | 3 | 2 | 0.52 | 3 | 2 | 0.09 | 3 | 2 | 0.29 | 3 | 2 | 0.79 | 5 | 0 | 0.26 | 2 | 3 | 0.36 |
| No | 388 (98.78) | 177 | 211 | 101 | 287 | 144 | 244 | 209 | 179 | 308 | 80 | 234 | 154 | ||||||
| Hemoglobin in Males | |||||||||||||||||||
| Hemoglobin > 16.5 g/dL | 75 (19.08) | 29 | 46 | 0.22 | 24 | 51 | 0.13 | 31 | 44 | 0.28 | 39 | 36 | 0.46 | 58 | 86 | 0.85 | 46 | 29 | 0.65 |
| Hemoglobin ≤ 16.5 g/dL | 113 (28.75) | 54 | 59 | 25 | 88 | 38 | 75 | 65 | 48 | 17 | 27 | 73 | 40 | ||||||
| Hemoglobin in Females | |||||||||||||||||||
| Hemoglobin > 16 g/dL | 35 (8.91) | 19 | 16 | 0.37 | 3 | 32 | 0.007 | 16 | 19 | 0.31 | 23 | 12 | 0.09 | 29 | 6 | 0.94 | 19 | 16 | 0.71 |
| Hemoglobin ≤ 16 g/dL | 170 (43.26) | 78 | 92 | 52 | 118 | 62 | 108 | 85 | 85 | 140 | 30 | 98 | 72 | ||||||
| Hematocrit in Males | |||||||||||||||||||
| Hematocrit > 49% | 118 (30.03) | 26 | 41 | 0.26 | 23 | 44 | 0.05 | 28 | 39 | 0.34 | 34 | 33 | 0.31 | 51 | 90 | 0.98 | 38 | 29 | 0.13 |
| Hematocrit ≤ 49% | 67 (17.05) | 56 | 62 | 25 | 93 | 41 | 77 | 69 | 49 | 16 | 28 | 80 | 38 | ||||||
| Hematocrit in Females | |||||||||||||||||||
| Hematocrit > 48% | 39 (9.92) | 24 | 15 | 0.048 | 4 | 35 | 0.009 | 17 | 22 | 0.43 | 23 | 16 | 0.38 | 33 | 6 | 0.69 | 20 | 19 | 0.42 |
| Hematocrit ≤ 48% | 166 (42.24) | 73 | 93 | 51 | 115 | 61 | 105 | 85 | 81 | 136 | 30 | 97 | 69 | ||||||
| Platelets (×109/L) | |||||||||||||||||||
| Platelets > 450 × 109/L | 227 (57.76) | 104 | 122 | 0.92 | 56 | 170 | 0.38 | 86 | 140 | 0.76 | 120 | 106 | 0.7 | 181 | 45 | 0.8 | 128 | 98 | 0.11 |
| Platelets ≤ 450 × 109/L | 166 (42.23) | 76 | 91 | 48 | 119 | 61 | 106 | 92 | 75 | 132 | 35 | 108 | 59 | ||||||
| Leukocytes (×109/L) | |||||||||||||||||||
| Leukocytes ≥ 11 × 109/L | 80 (20.35) | 39 | 41 | 0.81 | 18 | 62 | 0.85 | 30 | 50 | 0.73 | 42 | 38 | 0.99 | 61 | 19 | 0.41 | 54 | 26 | 0.008 |
| Leukocytes ≥ 25 × 109/L | 48 (12.21) | 21 | 27 | 9 | 39 | 21 | 27 | 25 | 23 | 41 | 7 | 22 | 26 | ||||||
| Leukocytes ≥ 15 × 109/L | 30 (7.63) | 13 | 17 | 7 | 23 | 11 | 19 | 16 | 14 | 25 | 5 | 13 | 17 | ||||||
| Leukemic transformations | |||||||||||||||||||
| Yes | 32 (8.14) | 12 | 20 | 0.33 | 10 | 22 | 0.52 | 15 | 17 | 0.23 | 16 | 16 | 0.64 | 21 | 11 | 0.04 | 21 | 11 | 0.5 |
| No | 361 (91.85) | 168 | 193 | 94 | 267 | 132 | 229 | 196 | 165 | 292 | 69 | 215 | 146 | ||||||
| Nonmyeloid malignancies | |||||||||||||||||||
| Yes | 28 (7.12) | 12 | 16 | 0.75 | 13 | 15 | 0.01 | 8 | 20 | 0.32 | 16 | 12 | 0.73 | 19 | 9 | 0.19 | 18 | 10 | 0.64 |
| No | 365 (92.87) | 168 | 197 | 91 | 274 | 139 | 226 | 196 | 169 | 294 | 71 | 218 | 147 | ||||||
| Smoking habits | |||||||||||||||||||
| Yes | 118 (30.02) | 58 | 60 | 0.38 | 31 | 87 | 0.955 | 44 | 74 | 0.98 | 72 | 46 | 0.07 | 101 | 17 | 0.06 | 70 | 48 | 0.85 |
| No | 275 (69.97) | 122 | 153 | 73 | 202 | 103 | 172 | 140 | 135 | 212 | 63 | 166 | 109 | ||||||
| Alcohol habits | |||||||||||||||||||
| Regular | 8 (2.03) | 2 | 6 | 0.06 | 2 | 6 | 0.31 | 3 | 5 | 0.99 | 4 | 4 | 0.88 | 5 | 3 | 0.41 | 3 | 5 | 0.35 |
| Social | 33 (17.3) | 39 | 29 | 13 | 55 | 25 | 43 | 35 | 33 | 56 | 12 | 39 | 29 | ||||||
| Never | 144 (80.66) | 139 | 178 | 89 | 228 | 119 | 198 | 173 | 144 | 252 | 65 | 194 | 123 | ||||||
| Exposure to noxes | |||||||||||||||||||
| Yes | 44 (11.19) | 19 | 25 | 0.71 | 10 | 255 | 0.55 | 18 | 26 | 0.61 | 26 | 18 | 0.47 | 37 | 7 | 0.44 | 22 | 22 | 0.15 |
| No | 349 (88.8) | 161 | 188 | 94 | 34 | 129 | 220 | 186 | 163 | 276 | 73 | 214 | 135 | ||||||
| History of bleeding | |||||||||||||||||||
| Yes | 25 (6.36) | 12 | 13 | 0.82 | 7 | 18 | 0.86 | 7 | 18 | 0.32 | 9 | 16 | 0.06 | 22 | 3 | 0.28 | 8 | 17 | 0.003 |
| No | 368 (93.63) | 168 | 200 | 97 | 271 | 140 | 228 | 203 | 165 | 291 | 77 | 228 | 140 | ||||||
| History of any thrombosis | |||||||||||||||||||
| Yes | 118 (30.02) | 54 | 64 | 0.99 | 31 | 87 | 0.96 | 53 | 65 | 0.04 | 61 | 57 | 0.56 | 94 | 24 | 1 | 66 | 52 | 0.28 |
| No | 275 (69.97) | 126 | 149 | 73 | 202 | 94 | 181 | 151 | 124 | 219 | 56 | 170 | 105 | ||||||
| History of venous thrombosis | |||||||||||||||||||
| Yes | 52 (13.23) | 21 | 31 | 0.4 | 13 | 39 | 0.8 | 24 | 28 | 0.16 | 24 | 28 | 0.23 | 38 | 14 | 0.21 | 30 | 22 | 0.71 |
| No | 86 (86.76) | 159 | 182 | 91 | 250 | 123 | 218 | 188 | 153 | 275 | 66 | 206 | 135 | ||||||
| History of arterial thrombosis | |||||||||||||||||||
| Yes | 80 (20.35) | 41 | 39 | 0.27 | 20 | 60 | 0.74 | 34 | 46 | 0.29 | 41 | 39 | 0.59 | 67 | 13 | 0.31 | 46 | 34 | 0.6 |
| No | 313 (79.64) | 139 | 174 | 84 | 229 | 113 | 200 | 171 | 142 | 246 | 67 | 190 | 123 | ||||||
| Possible Predictors | MPN | ||
|---|---|---|---|
| n (%) | p-value | Crude OR (95% CI) | |
| Age ≥ 60 years | 199 (50.6) | 0.11 | 1.28 (0.95–1.71) |
| Gender (male) | 188 (47.8) | 0.97 | 1.006 (0.75–1.35) |
| XPC Ala499Val (variant) | 213 (54.2) | 0.97 | 0.99 (0.74–1.34) |
| XPC Lys939Gln (variant) | 289 (73.5) | 0.54 | 1.11 (0.79–1.56) |
| XPD Lys751Gln (variant) | 246 (62.6) | 0.004 | 0.65 (0.48–0.87) |
| XPF-673C>T (variant) | 181 (46.1) | <0.001 | 1.78 (1.32–2.41) |
| XPF 11985A>G (variant) | 80 (20.4) | <0.001 | 3.79 (1.32–2.41) |
| XPG Asp1104His (variant) | 157 (39.9) | 0.8 | 1.039 (0.77–1.40) |
| Possible Predictors | PV Patients with PV (%) | PV | Patients with ET (%) | ET | Patients with PMF (%) | PMF | |||
|---|---|---|---|---|---|---|---|---|---|
| p-Value | Crude OR (95% CI) | p-Value | Crude OR (95% CI) | p-Value | Crude OR (95% CI) | ||||
| Age ≥60 years | 72 (47.05) | 0.22 | 1.29 (0.86–1.94) | 109 (54.22) | 0.15 | 0.75 (0.5–1.11) | 19 (52.77) | 0.8 | 1.09 (0.56–2.11) |
| Gender (male) | 94 (61.43) | <0.001 | 4.42 (1.6–3.67) | 75 (37.31) | <0.001 | 0.42 (0.28–0.62) | 19 (48.71) | 0.91 | 1.04 (0.54–2.02) |
| JAK2 (positive) | 69 (45.09) | 0.88 | 0.97 (0.65–1.46) | 88 (43.78) | 0.84 | 1.04 (0.7–1.55) | 174 (43.59) | 0.93 | 1.03 (0.53–2) |
| CALR (positive) | 1 (0.65) | <0.001 | 34.67 (4.75–254.37) | 37 (18.4) | <0.001 | 0.22 (0.102–0.47) | 8 (20.51) | 0.08 | 0.47 (0.2–1.08) |
| Smoking habits | 56 (36.6) | 0.035 | 0.63 (0.40–0.98) | 50 (24.87) | 0.023 | 1.66 (1.07–2.56) | 12 (30.76) | 0.92 | 0.96 (0.47–1.97) |
| Alcohol habits | 28 (18.3) | 0.72 | 1.10 (0.66–1.85) | 41 (20.40) | l0.87 | 0.87 (0.53–1.44) | 7 (17.95) | 0.82 | 1.11 (0.47–2.61) |
| Hemoglobin > 16.5 g/dL | 96 (62.74) | <0.001 | 0.018 (0.008–0.041) | 6 (2.98) | <0.001 | 32.5 (13.75–76.82) | - | - | - |
| Platelets > 450 × 109/L | 37 (24.18) | 0.41 | 1.77 (0.46–6.85) | 184 (91.54) | <0.001 | 0.021 (0.003–1.67) | 6 (15.38) | <0.001 | 73.67 (17.32–31.58) |
| Leukocytes ≥ 11 × 109/L | 65 (42.48) | 0.41 | 1.77 (0.46–6.85) | 76 (37.81) | 0.275 | 1.25 (0.84–1.88) | 17 (43.58) | 0.63 | 0.85 (0.43–1.65) |
| Exposure to cytoreductive agents | 63 (41.17) | 0.98 | 0.99 (0.66–1.5) | 81 (40.29) | 0.86 | 1.03 (0.69–1.55) | 16 (41.02) | 0.97 | 0.99 (0.5–1.93 |
| Exposure to noxious substances | 14 (9.15) | 0.27 | 0.7 (0.37–1.32) | 26 (12.93) | 0.27 | 0.7 (0.37–1.32) | 4 (10.25) | 0.85 | 1.12 (0.38–3.3) |
| Palpable splenomegaly | 66 (43.13) | 0.57 | 0.89 (0.59–1.34) | 66 (32.83) | 0.001 | 2 (1.33–3.01) | 29 (74.35) | 0.53 | 1.27 (0.6–2.71) |
| History of thrombosis | 47 (30.71) | 0.76 | 0.93 (0.6–1.451) | 61 (30.34) | 0.89 | 0.97 (0.63–1.5) | 10 (25.64) | 0.89 | 0.97 (0.63–1.5) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Crișan, A.-S.; Tripon, F.; Bogliș, A.; Crauciuc, G.-A.; Trifa, A.P.; Lázár, E.; Macarie, I.; Gabor, M.R.; Bănescu, C. The Role of DNA Repair (XPC, XPD, XPF, and XPG) Gene Polymorphisms in the Development of Myeloproliferative Neoplasms. Medicina 2024, 60, 506. https://doi.org/10.3390/medicina60030506
Crișan A-S, Tripon F, Bogliș A, Crauciuc G-A, Trifa AP, Lázár E, Macarie I, Gabor MR, Bănescu C. The Role of DNA Repair (XPC, XPD, XPF, and XPG) Gene Polymorphisms in the Development of Myeloproliferative Neoplasms. Medicina. 2024; 60(3):506. https://doi.org/10.3390/medicina60030506
Chicago/Turabian StyleCrișan, Adriana-Stela, Florin Tripon, Alina Bogliș, George-Andrei Crauciuc, Adrian P. Trifa, Erzsébet Lázár, Ioan Macarie, Manuela Rozalia Gabor, and Claudia Bănescu. 2024. "The Role of DNA Repair (XPC, XPD, XPF, and XPG) Gene Polymorphisms in the Development of Myeloproliferative Neoplasms" Medicina 60, no. 3: 506. https://doi.org/10.3390/medicina60030506
APA StyleCrișan, A.-S., Tripon, F., Bogliș, A., Crauciuc, G.-A., Trifa, A. P., Lázár, E., Macarie, I., Gabor, M. R., & Bănescu, C. (2024). The Role of DNA Repair (XPC, XPD, XPF, and XPG) Gene Polymorphisms in the Development of Myeloproliferative Neoplasms. Medicina, 60(3), 506. https://doi.org/10.3390/medicina60030506








