Abstract
Background and Objectives: Table tennis represents one of the fastest ball games in the world and, as such, is characterized by unique physiological demands. Despite its popularity, there is a dearth of data related to table-tennis-related risk factors and injuries. Therefore, the present review was conducted to fill in this gap of knowledge. Material and Methods: The present review was designed as a scoping review. Eleven online databases were searched with no language/date limitations. Results: Forty-two investigations were retained in the present review. These studies indicated that tenosynovitis, benign muscle injuries, strains, and sprains were the most common injury types. In order, the most commonly affected anatomical regions were the lower limb, shoulder, spine, knee, upper limb, and trunk. When comparing the injury occurrence between training and competition, the results were contradictory. National/international athletes had higher indices of injury than regional players, even though other investigations failed to replicate such findings. According to some scholars, there was a difference between female and male athletes: in females, more injuries involved the upper limbs when compared to men who had more injuries to the lower limbs, while other studies did not find differences in terms of gender. Conclusions: Table tennis is generally considered at lower risk for injuries than other sports. However, the present scoping review showed that injuries can occur and affect a variety of anatomic regions. Sports scientists/physicians could utilize the information contained in the current review for devising ad hoc programs to adopt an effective/appropriate prevention strategy and to monitor table tennis players’ training load and to achieve maximal fitness, as these will reduce the risk of injuries. However, most of the studies included in our scoping review are methodologically weak or of low-to-moderate evidence, being anecdotal or clinical case reports/case series, warranting caution when interpreting our findings and, above all, further high-quality research in the field is urgently needed.
1. Introduction
Table tennis (TT) represents one of the fastest ball games in the world and, as such, is characterized by unique physiological demands [1,2,3,4], even though, according to Mitchell’s sports classification, it is a group 1B sport, with low static and moderate dynamic components [5].
Previous reviews have reported that TT requires moderate-to-high levels of aerobic/anaerobic power [2]. Poor anaerobic or aerobic capacity is of concern for the unconditioned, inexperienced competitor and, therefore, less technical skill and a lower physiological profile may be related to an increased risk of injury. Thus, prolonged periods of TT training each week and/or overtraining might increase such a risk.
Further, TT is characterized by highly skilled and coordinated movements of the hand/forearm acquired through repetitive exercises [6]. TT is a complex, challenging discipline that requires explosive speed, power, accuracy, reflexes, instantaneous decisions, and good management of the effects and the technique [7,8,9,10]. As such, players have to maintain high levels of prolonged focused attention and can be exposed to competitive anxiety [11,12] since competitions can last days [1].
For these reasons, the high psycho-physical demands of TT may increase the risk of injury. Several factors can predispose TT players to injuries and sports-related lesions. TT implies the adoption of a particular posture, namely flexed/semi-flexed knee and asymmetrically rotated trunk [13,14,15]. Barczyk-Pawelec et al. [13] evaluated the body posture in 40 TT players and 43 controls not practicing any sport. They found that TT players exhibited a kyphotic body posture, and they observed a statistically significant correlation between training experience in years and the amount of asymmetry of the inclination angle of the shoulder line. This finding has been confirmed and replicated by other investigations [14,15].
However, despite the popularity of this sport, to our knowledge, there are no reviews focusing on TT-related injuries. Identifying TT-related injuries may assist in preventing these injuries. Usually, TT is perceived as a safe sport, and injuries are generally managed with the RICER regime (R = rest the injured part; I = apply ice for 20 min every 2–3 h for the first 48 h; C = perform compression by applying a bandage; E = elevate/raise the affected part above the level of the heart; and, R = refer to a trained professional) [16].
The purpose of this scoping review was to systematically investigate and critically appraise the extant studies about TT-related risk factors and injuries. The synthesis contained in this review may inform sports scientists as well as coaches and provide useful information for future research and studies as well as for ad hoc training strategies and programs.
2. Materials and Methods
Given the breadth of our research questions, a scoping review was conducted to summarize data concerning TT-related risk factors and injuries. This emerging knowledge synthesis technique was preferred over other types of reviews (narrative or systematic ones) since the question was not narrow and focused on a specific topic but was, instead, quite open and inclusive, and we were more interested in width rather than depth. Relevant studies, major concepts, theories/theoretical frameworks, sources, and gaps in knowledge were identified, combined, and analyzed to map currently available evidence and to provide an overview of the extant scholarly research on the topics of the epidemiology of TT-related injuries and the related determinants/risk factors using a systematic and reproducible approach. Conclusions were based on available studies with suggestions for practical applications for strength and conditioning professionals as well as future investigations.
The present scoping review was carried out according to the “Preferred Reporting Items for Systematic Reviews and Meta-Analyses” (PRISMA) checklist [17] and its extension for scoping reviews (PRISMA-ScR) statement/guidelines [18]. The study was registered on the “Open Science Framework” (OSF) platform. Registration number: DOI 10.17605/OSF.IO/FQG7C.
Eleven databases were extensively searched from inception, looking for the following string of keywords with proper Boolean connectors: TT, sports-related injuries, sports-related lesion, and trauma. Truncated words with the wild card option and Medical Subject Headings (MeSH) terms were used when appropriate. The platform “Primo Central Ex Libris UNO per tutti” was used. No time restriction or language filter was applied. An update was carried out during the revision process of the article to include potentially relevant articles that were accepted and published in the interim period. The search strategy is detailed in Table 1.

Table 1.
Search strategy items and details.
Target journals—and in particular, the “International Journal of TT Science”, the official scientific journal of the organization International TT Federation, ITTF—were hand-searched.
In order to catch all relevant manuscripts, gray literature was also searched by means of Google Scholar. Theses and dissertations were also included. TT was searched also in different languages (for example: Tischtennis, tenis de mesa, tennis da tavolo, ping pong, among others). The studies were independently screened by two authors by reading study titles and abstracts during the first step and full texts during the second step for potential eligibility. The agreement rate was assessed using κ statistics and was solved by discussion; a third reviewer was involved when necessary.
Studies meeting the following “Population/Exposure/Comparison/Outcome(s)/Study design” (PECOS) criteria were considered for inclusion:
- ▸
- P (population): male and female TT players at any age category and competitive level; in case the study also included other sports and disciplines, only data concerning TT players were extracted and retained in the present scoping review. If this was not possible (i.e., data were presented aggregated and were hard to disaggregate), the article was excluded;
- ▸
- E (exposure): reporting sports-related injuries;
- ▸
- C (comparison/comparator): between male and female TT players, various age categories, competitive levels, etc.;
- ▸
- O: the type of injury, its epidemiology (incidence/prevalence rate), and determinants of injuries;
- ▸
- S (study design): original peer-reviewed articles of any type (clinical case report, case series, observational study—incidence, prevalence or case-control investigation, randomized controlled trial, etc.) except for expert commentaries, editorials, and review articles, which were excluded but were scanned for potential articles to be included in the present scoping review;
- ▸
- Languages: all languages available.
The risk of bias for all included studies was evaluated independently by two reviewers using the Joanna Briggs Institute (JBI)’s critical appraisal tools, which basically assess three major domains: (i) the trustworthiness, (ii) the relevance, and (iii) the results of included studies. Based on the specific investigation, the most appropriate JBI tool was selected, depending on whether the study was devised as a prevalence, incidence, case–control study, etc. The score was interpreted according to the JBI’s handbook: a percentage of “yes” in the range 100–70% was considered a low risk of bias, in the range 70–50% a moderate risk of bias, and in the range 50–0% a high risk of bias.
3. Results
From the search of the electronic databases, a total of 87 articles were found from PubMed/MEDLINE (n = 26), ProQuest Research Library (n = 14), ProQuest Health & Medical Complete (n = 14), ProQuest Science Journals (n = 6), Taylor & Francis Online—Journals (n = 5), BMJ Journals (BMJ Publishing Group) (n = 5), Informa—Taylor & Francis (CrossRef) (n = 5), Directory of Open Access Journals (DOAJ), (n = 4), ProQuest Health Management (n = 3), ProQuest Nursing & Allied Health Source (n = 3), and Wiley Online Library (n = 2).
After removing duplicates, 53 unique items were screened for potential inclusion. Forty-nine articles were added from the gray literature search. Reading titles and/or abstracts resulted in the elimination of 31 articles. Twenty-five studies were excluded for the following reasons: 10 investigations were focused on disabled TT players, for 7 articles it was not possible to distinguish TT players from other athletes (data is aggregated and not broken down for single-sport discipline), 3 studies did not meet the PECOS criteria (being focused on illnesses and not on sports-related injuries), 2 were not pertinent to the review question, 1 study was an expert opinion article, a further study contained little information, and finally, 1 investigation was a clinical commentary. A total of 41 studies [1,6,7,14,15,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54] were included in the present review (Table 2 and Table 3).

Table 2.
Main features of the included studies (clinical case reports and case series are excluded and reported in a separate table).

Table 3.
List of case reports and case series included in the present scoping review.
For further details about the identification and retention of the studies, the reader is referred to Figure 1.
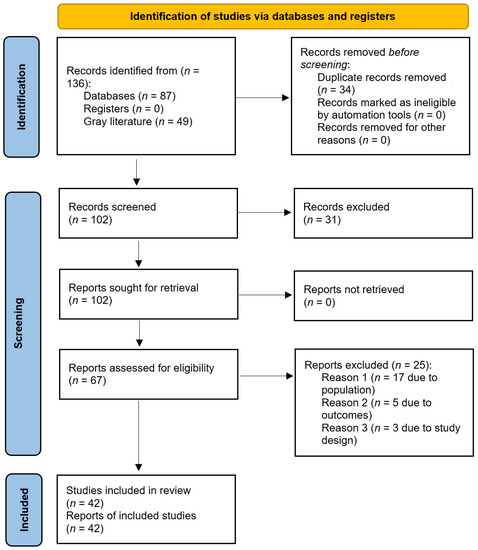
Figure 1.
PRISMA flow-chart.
Concerning the study design, 28 studies (66.7%) were devised as observational studies—in particular, 18 (64.3%) were incidence studies, 9 (32.1%) were prevalence studies, and 1 (3.6%) was a case–control study. Fourteen studies (33.3%) were designed as clinical case reports or case series. Finally, three (7.1%) were university theses/dissertations.
The sampling technique was mainly conducted by including consecutive participants, all athletes, or utilizing a convenience sample. Only in one case [20], athletes were randomly selected, and in one other article [7], a priori sample size estimation and power analysis were carried out.
Most studies focused on orthopedic injuries, while only a few considered eye injuries, cardiological risk factors, dental and facial injuries, dermatological lesions, neurological injuries, TT-related tumoral lesions, catastrophic injuries, and deaths. Finally, only one focused on risk injury perception and risk management strategies.
3.1. Risk of Bias Assessment
Concerning the risk of bias assessment, based on the JBI’s critical appraisal tools, only a few studies were deemed of high quality, the majority of the other studies included were methodologically poor/weak (low–moderate risk of bias) (Table 4).

Table 4.
Risk of bias assessment of the observational studies included in the present scoping review (excluded clinical cases reports/case series).
More specifically, considering the observational studies, 39.3% and 53.6% of them presented moderate and high risk of bias, respectively, whilst 7.1% exhibited a low risk of bias.
3.2. Injury Rate
Two studies (4.8%) computed the overall injury rate among TT players [1,7]. As reported in the extant scholarly literature retained in the present scoping review, this rate is highly variable [1]. De la Torre Combarros et al. [1] (low risk of bias) observed that injury incidence in TT players rate was 2.8% (1.0% among males, 4.5% among females), and 66.6% of injuries occurred during the first day of the championship and 60% of lesions in the first hour of the afternoon. Correa-Mesa [7] (moderate risk of bias) found an injury rate of 44% among TT players. Males exhibited a 25% lower risk of developing TT-related injuries compared to females.
3.3. Orthopedic Injuries by Competitive Level, Gender, and Type of Contest (Training vs. Competition), and Location of Injuries
Twenty-two articles (52.4%) were focused on orthopedic injuries among TT players.
Due to rotational torques applied at the level of the knee joint, TT players may be predisposed to osteoarthritis of the knee. Rajabi et al. [15] (low risk of bias) found that 78.3% of the ex-elite TT players exhibited different radiographic signs of osteoarthritis versus 36.3% of controls. The Kellgren and Lawrence scale, which ranges from 0 to 4 and is used to quantitatively assess the radiographic severity of osteoarthritis, statistically differed between the two groups. Further, 68.2% of the ex-elite TT players reported symptoms of knee pain with the Western Ontario and McMaster University Osteoarthritis Index questionnaire versus 27.3% of controls. However, the stiffness and physical function categories of the questionnaire did not reveal any significant difference. On the other hand, 73.7% of the ex-elite athletes and 32% of the control group showed altered lower limb alignment (genu varum). The lower limb angulation also statistically differed between the two groups. In conclusion, radiographic evidence of osteoarthritis did not result in physical disability or knee stiffness. Shimazaki et al. [20] (moderate risk of bias) found that international and national athletes presented higher indices of injury (52.9%) than regional players (48.8%); the upper limbs (93.6%) and the trunk (87.5%) were the most affected sites. Finally, injuries were more likely to occur during training.
Correa-Mesa and Correa-Morales [21] (high risk of bias) found that the shoulder (17%), knee (16%), back (9.3%), and elbow (9.3%) were the most affected sites. The most prevalent type of injury was tendinopathy (38.2%) followed by benign muscle injuries (17.1%) and sprain lesions (10.9%). The most common diagnosis was rotator cuff syndrome (10.6%). Fong et al. [22] (moderate risk of bias) computed 240 sports-related lesions: 3 (1.3%) were ankle injuries and 3 (1.5%) were ligamentous sprains, while no fractures were detected. De la Torre Combarros et al. [1] (low risk of bias) found the injury incidence rate was 2.8% (1.0% among males, 4.5% among females), and 66.6% of injuries occurred during the first day of the championship and 60% of lesions during the first hour of the afternoon. The most serious lesion was a traumatic meniscus injury; other lesions affected the left knee joint, the internal malleolus of the right ankle, the rectus femoris, the supraspinatus of the dominant arm, and the thoracolumbar and the paravertebral muscles. Almost all injuries were acute, apart from a chronic one, namely the tendinosis of the supraspinatus. In conclusion, the most affected anatomic sites were, in order, lower limb, upper limb, and trunk. Di Carlo et al. [23] (high risk of bias) in Venezuela, recruited 26 players (18 males, 8 females) aged 10–50 years. Shoulder injury occurred in 84.6% of the sample, whereas lumbago was found in 100% of the individuals. Furthermore, supraspinatus and biceps tendinitis affected 63.6% and 36.4% of athletes, respectively.
Concerning risk factors, age was found to be the main determinant, with 54.6% of injured subjects being aged in the range of 10–20 years. Fernández Córdova and Barrios González [24] (high risk of bias) reported the following injuries: bursitis and synovitis (88%), lumbago (75%), tendinitis (25.21%), sacro-iliac joint pain (10.08%), tenosynovitis (8.40%), chondromalacia and insertion impairment (7.56%), and other injuries such as fasciitis, ganglionitis, capsulitis, subluxations, Osgood–Schlatter disease, herniated disc, and residual meniscus (7.56%). Risk factors were found to be international competitions and strenuous practice.
Furthermore, in a 10-year study, Majewski et al. [25] (high risk of bias) described 37 cases of knee joint traumas in 123,653 TT players (with a coefficient rate of 0.03).
Lo et al. [26] (high risk of bias) interviewed 373 physiotherapy students in the Hong Kong Polytechnic (242 males, 130 females) and reported 5 cases of shoulder impingement; in 3 athletes (60%), there was a frank clinical presentation of pain.
When comparing injury rates between male and female athletes and training and competition, Kondric et al. [27] (high risk of bias) recruited a sample of 83 top Slovenian athletes (29 players of TT, 39 of tennis, and 15 of badminton) and found that the most affected anatomic sites were the shoulder girdle (17.3%), spine (16.6%), ankle (15.8%), foot (10.1%), and wrist (12.2%). Most injuries involved muscle tissues and, to a lesser extent, joints and tendons/ligaments. According to the authors, injuries in TT are the consequences of “short, abrupt and extremely rapid movements, particularly in forehand strokes with no swing phase”. With the introduction of a bigger ball, the injury rate seems to have increased. Further, most injuries occurred both during a training session or a competition event at similar rates. Males and females were equally affected. The authors concluded that TT-related injuries are uncommon and occur at lower rates when compared to other sports disciplines in a statistically significant fashion.
Junge et al. [28] (moderate risk of bias) reviewed the injuries that occurred during the 2008 Summer Olympic Games and found that 9 athletes (5.2%) were injured with an estimated 2.6% of athletes reporting time-loss injuries. Five athletes (83.3%) reported injuries during training, only one (16.7%) during competition. Among the different sports disciplines, TT is the discipline with the highest injury rate occurring during training: one injury was a fracture and one a dislocation/rupture of tendon or ligament. The most hazardous sports disciplines were soccer, taekwondo, hockey, handball, weightlifting, and boxing, whereas TT was as safe as sailing, canoeing/kayaking, rowing, synchronized swimming, and diving, fencing, and swimming.
In contrast, Engebretsen et al. [29] (moderate risk of bias) found that out of 174 TT players (88 females, 86 males), 11 (6.3%) reported injuries. Seven (4.0%) and two (1.1%) injuries led to time loss ≥1 day and >7 days, respectively. Seven (70.0%) occurred during competition and three (30.0%) during training.
Linderoth [30] (high risk of bias) found differences between female and male athletes: in females, more injuries involved the upper limbs when compared to men who had more injuries to the lower limbs, possibly because women are generally weaker in the upper body and have hypermobile joints. Further risk factors for injuries can be warm-up and stretching performed poorly, as well as returning to sports practice immediately after the injury without a proper resting period.
Folorunso et al. [14] (high risk of bias) observed that 25% of TT-playing Nigerians complained of upper limb chronic pain. Further, Pieper et al. [31] reported three clinical cases (two males, one female) of impingement of the rotator cuff. Among the racket games, the sports that were more related to instability of the shoulder joint were handball (15 cases) and tennis (11 cases). TT was responsible for 4.5% of observed and treated shoulder injuries.
Nicolini et al. [32] described a clinical case of patellar tendinopathy in a female TT player treated at the Specialized Outpatient Clinics in São Paulo, Brazil, out of a series of 440 patients taking part in 33 different types of sports disciplines. Li [33] reported 19 clinical cases of De Quervain’s tenosynovitis. Other orthopedic injuries have been anecdotally reported, indicating they may be very rare among TT players. Pintore and Maffulli [34] reported the case of an osteochondritis dissecans of the elbow affecting the right lateral humeral condyle and clinically presenting as intra-articular loose bodies of the elbow. This lesion may be ascribed to repetitive valgus compressive stresses at the radio-capitellar joint. Ron et al. [35] described a case of simultaneous dislocation of both interphalangeal joints in one finger. Dufek et al. [36] reported a case of a stress fracture of the ulna in a 26-year-old professional TT player, probably related to the change of the intensity of training and of the TT racket.
Petschnig et al. [37] described a case of a stress fracture of the diaphyseal ulna in a 19-year-old female TT player, who also reported a history of secondary amenorrhea. The stress fracture was related to the vigorous movements carried out during the sport and repeated forearm flexor muscle activity due to overtraining. Conversely, no injuries were reported by Laoruengthana et al. [38] (high risk of bias), who concluded that TT is safe compared to sports disciplines such as handball, basketball, rugby, and football, which together accounted for 32% of all injuries, whereas no injuries were reported for other disciplines including shooting, dancing, and golf.
3.4. Dental and Facial Injuries
Three articles (7.1%) dealt with dental and facial injuries among TT players. Generally, TT is commonly perceived as a sports discipline characterized by a low rate of dental and facial injuries. Hill et al. [39] (moderate risk of bias) performed a cross-sectional study recruiting 130 patients from 21 different sports played in the Bradford area in the United Kingdom over five years. They found that miniature motorcycling and horseback riding were the most dangerous individual sports, while, as far as team sports are concerned, rugby, soccer, and cricket players reported the highest facial and dental injury rates.
Furthermore, de la Torre Combarros et al. [1] (low risk of bias) reported that facial injuries were the least common lesions among 10 types of injuries that occurred during the 2005 Spanish National Championships. Andrade et al. [40] (high risk of bias) reported no dental injuries among the five TT players who took part in the Pan American Games. The authors concluded that TT is at low risk for dental injuries; therefore, mouthguards are not necessary. Wrestling, boxing, karate, taekwondo, and field hockey should be considered at high risk, and basketball, team handball, soccer, water polo, baseball, judo, diving, and synchronized swimming at middle risk.
3.5. Dermatological Lesions
Patches and skin lesions have rarely been reported [41]. De la Torre Combarros et al. [1] (low risk of bias) reported 10 dermatological lesions overall, of which 2 (blisters affecting the fingers of the dominant hand in a female player) were due to TT.
3.6. Ocular Lesions
Blunt eye trauma is associated with many ball games, and TT players also seem to be predisposed to eye injuries. A systematic review performed by Barrell et al. [42] (moderate risk of bias) of the records of 118 patients treated at Southampton Eye Hospital during 1978–1979 for sports-related injuries revealed that even rare ocular lesions may require the use of eye protection. More in detail, 58 lesions (49.2%) were due to squash, 23 (19.5%) to badminton, 22 (18.6%) to football, 9 (7.6%) to tennis, 5 (4.2%) to cricket, and only 1 (0.8%) to TT.
Chandran [43] (moderate risk of bias) reported two cases of eye injuries among TT players in a period of 5 years in a series of 63 ocular lesions treated at the Eye Clinic of the University Hospital, Kuala Lumpur, Malaysia, involving a variety of sports (hockey, tennis, cricket, soccer, rugby, golf, squash, and other disciplines). Jeffers [44] (high risk of bias) reported two cases of eye injuries in two male TT players in the period 1984–1986 in a series of 203 ocular lesions. Kelly and Nolan [45] (moderate risk of bias) reported one case of a TT player with an eye injury out of 45 consecutive players who required admission to the hospital between 1 January 1979 and 31 December 1982.
3.7. Neurological Lesions and TT-Related Tumors
Information regarding neurological lesions and TT-related tumors is contained in anecdotal clinical case reports. For instance, Le Floch et al. [6] described four cases of focal task-specific dystonia, two involving professional international competitors. Copcu [51] described a case of one TT player who developed a very quickly grown lipoma on his right scapular area, probably a reaction to chronically minor traumas, especially to the scapular area.
As for cardiological risk factors, catastrophic injuries, and deaths, Fujiwara et al. [52] investigated 30 patients with sports-related acute myocardial infarction. They found that playing ball games was associated with this adverse event: 3 out of 30 played tennis or TT. Sudden death during TT play is anecdotal [53,54]. TT is safe with respect to other sports disciplines, such as horseback riding (98 deaths), air sports (92 deaths), motorsports (86 deaths), and mountaineering (74 deaths), which represent the most hazardous activities for adults, whereas the most hazardous activity for children is horseback riding (19 deaths), according to a comprehensive survey of sporting and leisure activities in England and Wales, carried out in the period 1982–1988.
3.8. Injury Risk Perception and Risk Management Strategies
Only one study assessed the knowledge and perception of injury risk among TT players. Chen-Liang and Wen-Guu [55] recruited 352 members of TT clubs in Taichung, Changhua, Chiayi, and Tainan via convenience sampling. Of these, 326 accepted to answer the questionnaire (92.6% participation rate, 7.4% dropout rate). They found that marital status influenced the perception of risk of injury in terms of “internal psychological factors”, but not in terms of “external environmental factors”. Further, “internal psychological factors”, “external environmental factors”, “self-cognitive factors”, “facility and equipment factors”, and “coach management factors” did not significantly correlate with one another.
Assessing injury risk perception as well as understanding risk factors and biomechanics of pain and injuries among TT athletes is of paramount importance to devise effective preventative training strategies. Evidence-based rehabilitation programs carried out in synergy with ad hoc training could allow pain- and injury-free sports activity, optimizing and enhancing the overall health benefits for TT athletes [56,57,58,59].
4. Discussion
TT is generally considered at lower risk for injuries than other sports [1,2,3,4,5]. However, injuries can occur and affect a variety of anatomic regions including the wrist, the elbow, the shoulders, the neck, upper back, and lower back, the hip, the ankle as well as muscles, ligaments, and tendons of these anatomical regions. Specifically, tenosynovitis, benign muscle injuries, strains, and sprains are the most commonly reported TT-related injury types [15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35].
In order, the most commonly affected anatomical regions are the lower limbs, the shoulders, the spine, the knees, the upper limbs, and the trunk [15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35]. TT-related injuries can be due to several parameters, such as poor warm-up and stretching, as well as poor training programs and overtraining. In the present scoping review, we have comprehensively scanned the extant scholarly literature. We have found an increasing interest in reporting and describing TT-related injuries over time, even though the range of injury rates is highly variable (depending on the study design, study population, country, and year). While there seems to be a general consensus that TT-related injuries occur at lower rates than with other sports disciplines, we found contrasting findings concerning their determinants.
For instance, when comparing the injury occurrence between training and competition, the results were contradictory. At the 2012 Olympic Games, higher injury occurrence during competition than during training was reported both in male and female TT players, whereas an opposite trend had been noticed during the 2008 Olympic Games [28,29]. Furthermore, national/international athletes presented higher indices of injury than regional players, even though other investigations failed to replicate this finding.
According to some scholars, there was a difference between female and male athletes: in females, more injuries involved the upper limbs when compared to men who had more injuries to the lower limbs, while other studies did not find differences in terms of gender. As such, the study of injury determinants in TT requires further high-quality research, also considering the overall low-to-moderate quality of the articles retained in the present scoping review.
Strengths and Limitations of the Present Study
The strength of our scoping review consists of a rigorous, highly reproducible, and systematic literature search strategy, based on a solid rationale, clearly defined study inclusion/exclusion criteria and clearly defined primary and secondary endpoints/outcomes for evidence synthesis. Specifically, the search was without language/date limitations, and the risk of bias was assessed. In terms of the number of studies, we included 42 studies, and most of them focused on orthopedic injuries, which can help us extract data about the most commonly affected anatomical regions, injury types, and injury occurrence according to the type of contest, competitive level, and gender.
However, a number of limitations should be mentioned. We could not find in all the studies included injury rates during competitions reported stratified by gender and age, warranting that more data are urgently needed. Moreover, most of the studies included in our scoping review are methodologically weak or of low-to-moderate evidence, with some studies being anecdotal or clinical case reports/case series. Thus, few studies provided details of eye injuries, cardiological risk factors, dental and facial injuries, dermatological lesions, neurological injuries, TT-related tumoral lesions, and death. Only one study performed randomization of the sample and one computed a priori the power of the sampling technique. Therefore, these few published studies markedly understate the worldwide situation.
On the other hand, the present overview can serve to plan future higher-quality studies and epidemiological surveys to advance a field, which is generally overlooked, and to identify the best evidence-based training strategy aimed at preventing injuries among TT athletes.
5. Conclusions
The most frequently reported and studied TT-related injuries are orthopedic. Even if not precisely known, the rate of injuries seems to be low, especially when compared to other more dangerous sports. Generally speaking, TT is a relatively safe discipline [60,61], even though evidence collected and identified through the methodology of this study is of low-to-moderate quality based on the study designs and other intrinsic methodological deficiencies that we have underlined with our risk of bias assessment. Since most injuries occur during training, coaches should monitor the intensity of the training program. Overall, however, there is scant evidence about TT-related injuries. There is an urgent need for high-quality randomized studies, as also advocated by Steffen and Engebretsen [62]. A key approach for practitioners and sports physicians is to monitor TT players’ training load and to achieve maximal fitness, as these will reduce the risk of injuries.
Author Contributions
Conceptualization, C.B. and N.L.B.; methodology, L.P., M.S. and N.L.B.; validation, C.B. and P.S.; formal analysis, N.L.B.; investigation, M.S., P.S., W.D. and L.P.; data curation, C.B., M.S., N.L.B., P.S. and W.D.; writing—original draft preparation, C.B., N.L.B., L.P. and P.S.; writing—review and editing, C.B., L.P. and N.L.B.; visualization, C.B. and P.R.; supervision, N.L.B. and P.R.; project administration, L.P., M.S. and N.L.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All data are available in the main text.
Conflicts of Interest
The authors declare no conflict of interest.
References
- de la Torre Combarros, A.; Carrasco Páez, L.; Pradas de la Fuente, F. Injury Incidence among Young Table Tennis Players during 2005 Spanish National Championship. In Proceedings of the 10th International Table Tennis Sports Science Congress, Zagreb, Croatia, 18–20 May 2007; Available online: http://www.ittf.com/ittf_science/SSCenter/10ITTSSC_Zagreb_07/docs/08-de%20la%20torre_injury%20incidence.pdf (accessed on 31 December 2021).
- Kondrič, M.; Zagatto, A.M.; Sekulić, D. The physiological demands of table tennis: A review. J. Sport. Sci. Med. 2013, 12, 362–370. [Google Scholar]
- Zagatto, A.M.; De Mello Leite, J.V.; Papoti, M.; Beneke, R. Energetics of table tennis and table tennis–specific exercise testing. Int. J. Sport. Physiol. Perform. 2016, 11, 1012–1017. [Google Scholar] [CrossRef] [PubMed]
- Zagatto, A.M.; Morel, E.A.; Gobatto, C.A. Physiological responses and characteristics of table tennis matches determined in official tournaments. J. Strength Cond. Res. 2010, 24, 942–949. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, J.H.; Haskell, W.L.; Raven, P.B. Classification of sports. J. Am. Coll. Cardiol. 1994, 24, 864–866. [Google Scholar] [CrossRef]
- Le Floch, A.; Vidailhet, M.; St, C.F.-R.; Grabli, D.; Mayer, J.-M.; Gonce, M.; Broussolle, E.; Roze, E. Table tennis dystonia. Mov. Disord. 2010, 25, 394–397. [Google Scholar] [CrossRef]
- Correa Mesa, J.F. Prevalencia de Lesiones Osteomusculares en Tenimesistas de alto Rendimiento de la Federación Colombiana de Tenis de Mesa. 2014. Available online: https://repositorio.unal.edu.co/bitstream/handle/unal/56085/1037576078.pdf?sequence=1&isAllowed=y (accessed on 31 December 2021).
- Padulo, J.; Di Giminiani, R.; Iacono, A.D.; Zagatto, A.M.; Migliaccio, G.M.; Grgantov, Z.; Ardigò, L.P. Lower arm muscle activation during indirect-localized vibration: The influence of skill levels when applying different acceleration loads. Front. Physiol. 2016, 7, 242. [Google Scholar] [CrossRef]
- Zagatto, A.M.; Gobatto, C.A. Relationship between anaerobic parameters provided from MAOD and critical power model in specific table tennis test. Int. J. Sport. Med. 2012, 33, 613–620. [Google Scholar] [CrossRef]
- Zagatto, A.M.; Papoti, M.; Gobatto, C.A. Anaerobic capacity may not be determined by critical power model in elite table tennis players. J. Sport. Sci. Med. 2008, 7, 54–59. [Google Scholar]
- Martinent, G.; Ferrand, C. A Naturalistic study of the directional interpretation process of discrete emotions during high-stakes table tennis matches. J. Sport Exerc. Psychol. 2009, 31, 318–336. [Google Scholar] [CrossRef]
- Martinent, G.; Ferrand, C. A field study of discrete emotions: Athletes’ cognitive appraisals during competition. Res. Q. Exerc. Sport 2015, 86, 51–62. [Google Scholar] [CrossRef]
- Barczyk-Pawelec, K.; Bankosz, Z.; Derlich, M. Body postures and asymmetries in frontal and transverse planes in the trunk area in table tennis players. Biol. Sport 2012, 29, 127–132. [Google Scholar] [CrossRef]
- Folorunso, O.M.; Ademola, O.A. The playing posture, activities and health of the table tennis player. Int. J. Table Tennis Sci. 2010, 6, 99–104. [Google Scholar]
- Rajabi, R.; Johnson, G.M.; Alizadeh, M.H.; Meghdadi, N. Radiographic knee osteoarthritis in ex-elite table tennis players. BMC Musculoskelet. Disord. 2012, 13, 12. [Google Scholar] [CrossRef]
- McAfee, R.E. Table Tennis: Steps to Success; Human Kinetics: Champaign, IL, USA, 2009. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 105906. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Nillius, S.A.; Nilsson, B.E.; Westlin, N.E.; Niixius, S.A. The incidence of Achilles tendon rupture. Acta Orthop. Scand. 1976, 47, 118–121. [Google Scholar] [CrossRef]
- Shimazaki, T.; Almeida, E.d.; Vanderlei, F.M.; Cintra Filho, D.d.A.; Vanderlei, L.C.M.; Pastre, C.M.; Bastos, F.N. Exploração de fatores de risco para lesões desportivas em atletas de tênis de mesa. Fisioter. Pesqui. 2012, 19, 158–164. [Google Scholar] [CrossRef]
- Correa-Mesa, J.F.; Correa-Morales, J.C. Prevalencia de lesiones musculoesqueléticas en jugadores de tenis de mesa. Rev. Cienc. Bioméd. 2020, 5, 48–54. [Google Scholar] [CrossRef]
- Fong, D.T.-P.; Man, C.-Y.; Yung, P.S.-H.; Cheung, S.-Y.; Chan, K.-M. Sport-related ankle injuries attending an accident and emergency department. Injury 2008, 39, 1222–1227. [Google Scholar] [CrossRef]
- Di Carlo, M.; Formigoni, M.; Peña, S.; Fernández Palazzi, F. Biomecánica y lesiones del hombro aplicadas al tenis de mesa. Cent. Méd. 1997, 42, 18–21. [Google Scholar]
- Fernández Córdova, L.S.; Barrios González, J. Lesiones más frecuentes en atletas del equipo nacional cubano de tenis de mesa en el período 2005–2008. Rev. Digital B. Aires 2010, 151. [Google Scholar]
- Majewski, M.; Susanne, H.; Klaus, S. Epidemiology of athletic knee injuries: A 10-year study. Knee 2006, 13, 184–188. [Google Scholar] [CrossRef] [PubMed]
- Lo, Y.P.; Hsu, Y.C.; Chan, K.M. Epidemiology of shoulder impingement in upper arm sports events. Br. J. Sport. Med. 1990, 24, 173–177. [Google Scholar] [CrossRef]
- Kondric, M.; Matković, B.R.; Furjan-Mandić, G.; Hadzić, V.; Dervisević, E. Injuries in racket sports among Slovenian players. Coll. Antropol. 2011, 35, 413–417. [Google Scholar] [PubMed]
- Junge, A.; Engebretsen, L.; Mountjoy, M.L.; Alonso, J.M.; Renström, P.A.F.H.; Aubry, M.J.; Dvorak, J. Sports injuries during the summer Olympic games 2008. Am. J. Sport. Med. 2009, 37, 2165–2172. [Google Scholar] [CrossRef] [PubMed]
- Engebretsen, L.; Soligard, T.; Steffen, K.; Alonso, J.M.; Aubry, M.; Budgett, R.; Dvorak, J.; Jegathesan, M.; Meeuwisse, W.H.; Mountjoy, M.; et al. Sports injuries and illnesses during the London Summer Olympic Games 2012. Br. J. Sport. Med. 2013, 47, 407–414. [Google Scholar] [CrossRef] [PubMed]
- Linderoth, M. Kan man bli Skadad i Pingis?: En Studie om Förekomsten av Skador i Svensk Elitbordtennis. Institutionen för Idrotts-och Hälsovetenskap. 2006. Available online: http://www.diva-portal.org/smash/get/diva2:852/FULLTEXT01.pdf (accessed on 31 December 2021).
- Pieper, H.-G.; Quack, G.; Krahl, H. Impingement of the rotator cuff in athletes caused by instability of the shoulder joint. Knee Surg. Sport. Traumatol. Arthrosc. 1993, 1, 97–99. [Google Scholar] [CrossRef]
- Nicolini, A.P.; De Carvalho, R.T.; Matsuda, M.M.; Filho, J.S.; Cohen, M. Common injuries in athletes’ knee: Experience of a specialized center. Acta Ortop. Bras. 2014, 22, 127–131. [Google Scholar] [CrossRef]
- Li, Y. Tenosynovitis of table tennis players and its treatment. Sport. Sci./Tiyu Kexue 1996, 16, 67–70. [Google Scholar]
- Pintore, E.; Maffulli, N. Osteochondritis dissecans of the lateral humeral condyle in a table tennis player. Med. Sci. Sport. Exerc. 1991, 23, 889–891. [Google Scholar] [CrossRef]
- Ron, D.; Alkalay, D.; Torok, G. Simultaneous closed dislocation of both interphalangeal joints in one finger. J. Trauma Inj. Infect. Crit. Care 1983, 23, 66–67. [Google Scholar] [CrossRef] [PubMed]
- Dufek, P.; Ostendorf, U.; Thormählen, F. Stress fracture of the ulna in a table tennis player. Sportverletz. Sportschaden Organ Der Ges. Fur Orthop.-Traumatol. Sportmed. 1999, 13, 62–64. [Google Scholar] [CrossRef] [PubMed]
- Petschnig, R.; Wurnig, C.; Rosen, A.; Baron, R. Stress fracture of the ulna in a female table tennis tournament player. J. Sport. Med. Phys. Fit. 1997, 37, 225–227. [Google Scholar]
- Laoruengthana, A.; Poosamsai, P.; Fangsanau, T.; Supanpaiboon, P.; Tungkasamesamran, K. The epidemiology of sports injury during the 37th Thailand National Games 2008 in Phitsanulok. J. Med. Assoc. Thail. 2009, 92, S204–S210. [Google Scholar]
- Hill, C.M.; Crosher, R.F.; Mason, D.A. Dental and facial injuries following sports accidents: A study of 130 patients. Br. J. Oral Maxillofac. Surg. 1985, 23, 268–274. [Google Scholar] [CrossRef]
- Andrade, R.A.; Evans, P.L.S.; Almeida, A.L.S.; Silva, J.D.J.R.D.; Guedes, A.M.L.; Guedes, F.R.; Ranalli, D.N.; Modesto, A.; Tinoco, E.M.B. Prevalence of dental trauma in Pan American Games athletes. Dent. Traumatol. 2010, 26, 248–253. [Google Scholar] [CrossRef] [PubMed]
- Scott, M.J., Jr.; Scott, M.J., 3rd. Ping pong patches. Cutis 1989, 43, 363–364. [Google Scholar]
- Barrell, G.V.; Cooper, P.J.; Elkington, A.R.; Macfadyen, J.M.; Powell, R.G.; Tormey, P. Squash ball to eye ball: The likelihood of squash players incurring an eye injury. Br. Med. J. (Clin. Res. Ed.) 1981, 283, 893–895. [Google Scholar] [CrossRef]
- Chandran, S. Ocular hazards of playing badminton. Br. J. Ophthalmol. 1974, 58, 757–760. [Google Scholar] [CrossRef]
- Jeffers, J.B. The role of organized ophthalmology in preventing ocular injuries. Int. Ophthalmol. Clin. 1988, 28, 255–258. [Google Scholar] [CrossRef]
- Kelly, S.; Nolan, J. Eye injuries in organised sport in a rural area. Br. J. Ophthalmol. 1983, 67, 837–839. [Google Scholar] [CrossRef] [PubMed]
- Lovell, G. The diagnosis of chronic groin pain in athletes: A review of 189 cases. Aust. J. Sci. Med. Sport 1995, 27, 76–79. [Google Scholar] [PubMed]
- Shida, Y.; Shida, S.; Suzuki, S.; Murakami, H.; Yuza, N. Injuries and systemic disorders of table tennis players: Results of a survey. Int. J. Table Tennis Sci. 1992, 1, 11–16. [Google Scholar]
- Shida, Y.; Shida, S.; Suzuki, S.; Murakami, H.; Youza, N. Injuries and systematic disorders of table tennis players. Int. J. Table Tennis Sci. 1994, 2, 121–122. [Google Scholar]
- Soligard, T.; Steffen, K.; Palmer, D.; Alonso, J.M.; Bahr, R.; Lopes, A.; Dvorak, J.; Grant, M.-E.; Meeuwisse, W.; Mountjoy, M.; et al. Sports injury and illness incidence in the Rio de Janeiro 2016 Olympic Summer Games: A prospective study of 11274 athletes from 207 countries. Br. J. Sport. Med. 2017, 51, 1265–1271. [Google Scholar] [CrossRef] [PubMed]
- Tin Oo, M.M.; Razali, R. Sport-related oral injuries and mouthguard use among athletes in Kelantan, Malaysia. Arch. Orofac. Sci. 2012, 7, 21–27. [Google Scholar]
- Copcu, E. Sport-induced lipoma. Int. J. Sport. Med. 2004, 25, 182–185. [Google Scholar]
- Fujiwara, M.; Asakuma, S.; Nakamura, K.; Nakamura, T.; Yasutomi, N.; Iwasaki, T. Acute myocardial infarction during sport. J. Cardiol. 1995, 26. [Google Scholar]
- Avery, J.G.; Harper, P.; Ackroyd, S. Do we pay too dearly for our sport and leisure activities? An investigation into fatalities as a result of sporting and leisure activities in England and Wales, 1982–1988. Public Health 1990, 104, 417–423. [Google Scholar] [CrossRef]
- Turk, E.E.; Riedel, A.; Pueschel, K. Natural and traumatic sports-related fatalities: A 10-year retrospective study. Br. J. Sport. Med. 2008, 42, 604–608. [Google Scholar] [CrossRef]
- Chen-Liang, C.; Wen-Guu, L. Sport Injuries and Risk Management regarding Table Tennis Club Members. 2010. Available online: https://people.dyu.edu.tw/paper/9901192_c.pdf (accessed on 31 December 2021). (In Chinese).
- Farì, G.; Fischetti, F.; Zonno, A.; Marra, F.; Maglie, A.; Bianchi, F.; Messina, G.; Ranieri, M.; Megna, M. Musculoskeletal pain in gymnasts: A retrospective analysis on a cohort of professional athletes. Int. J. Environ. Res. Public Health 2021, 18, 5460. [Google Scholar] [CrossRef] [PubMed]
- Farì, G.; Santagati, D.; Macchiarola, D.; Ricci, V.; Di Paolo, S.; Caforio, L.; Invernizzi, M.; Notarnicola, A.; Megna, M.; Ranieri, M. Musculoskeletal pain related to surfing practice: Which role for sports rehabilitation strategies? A cross-sectional study. J. Back Musculoskelet. Rehabil. 2022; preprint. [Google Scholar] [CrossRef]
- Farì, G.; Notarnicola, A.; Di Paolo, S.; Covelli, I.; Moretti, B. Epidemiology of injuries in water board sports: Trauma versus overuse injury. J. Sport. Med. Phys. Fit. 2021, 61, 707–711. [Google Scholar] [CrossRef] [PubMed]
- de Sire, A.; Marotta, N.; Lippi, L.; Scaturro, D.; Farì, G.; Liccardi, A.; Moggio, L.; Mauro, G.L.; Ammendolia, A.; Invernizzi, M. Pharmacological treatment for acute traumatic musculoskeletal pain in athletes. Medicina 2021, 57, 1208. [Google Scholar] [CrossRef] [PubMed]
- Hassan, I.H.I.; Elgammal, M.A. Common injuries in racket sports: A mini review. Ortho. Surg. Ortho. Care Int. J. 2018, 1, 1–3. [Google Scholar] [CrossRef]
- Wang, Y.P.; Chen, G. Table Tennis, 2nd ed.; XanEdu Publishing Company: Ann Arbor, MI, USA, 2006. [Google Scholar]
- Steffen, K.; Engebretsen, L. More data needed on injury risk among young elite athletes. Br. J. Sport. Med. 2010, 44, 485–489. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).