Abstract
Introduction and purpose of the study: SARS-CoV-2 virus does not only affect the respiratory system. It may cause damage to many organ systems with long-term effects. The latest scientific reports inform that this virus leaves a long-term trace in the nervous, circulatory, respiratory, urinary and reproductive systems. It manifests itself in disturbances in the functioning of the organs of these systems, causing serious health problems. The aim of the study was to review the latest research into the long-term effects of COVID-19 and determine how common these symptoms are and who is most at risk. Based on a literature review using the electronic scientific databases of PubMed and Web of Science on the long-term effects of SARS-CoV-2 infection, 88 studies were included in the analysis. The information contained in the analyzed literature shows that the SARS-CoV-2 virus can cause multi-organ damage, causing a number of long-term negative health complications. Conclusions: There is evidence that the virus can cause long-term complications lasting more than six months. They mainly concern disturbances in the functioning of the nervous, circulatory and respiratory systems. However, these studies are small or short-lasting, and many are speculative.
1. Introduction
1.1. The Global Pandemic of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2)
Coronaviruses have been known to mankind for decades. At first, they were thought to cause mild infections of the upper respiratory tract. The SARS outbreak occurred for the first time in 2003 and was mastered within six months [1]. There was a large time gap before the second, closely related coronavirus—the Middle East respiratory syndrome coronavirus, which emerged in 2012 [2]. Apart from severe respiratory disease, it also often caused renal failure [3]. They led to the death of a significant number of patients, which showed a significant threat to the situation in the world from these pathogens. As of 30 November 2019, the World Health Organization (WHO) has registered 2494 cases of MERS-CoV worldwide [4]. The 21st century was marked by a pandemic caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus, the seventh coronavirus known to infect humans, causing the infectious respiratory disease COVID-19 [5]. The first cases of infection were identified and described in December 2019 in the city of Wuhan, Hubei province in central China. Already in mid-January, the virus had spread throughout China, in the second half of February, outbreaks of infections with hundreds of patients broke out in South Korea, Italy and Iran. The virus spread very quickly across all continents, causing a global pandemic officially announced by the World Health Organization (WHO) on 11 March 2020, describing this disease as a serious threat to public health of international scope [6]. The consequences of the COVID-19 pandemic include a significant number of cases and deaths, failure of health systems, mental disorders and unprecedented methods of fighting a pandemic requiring the closure of large sectors of the economy and a drastic reduction of people-to-people contact [7]. A comparison of the SARS-CoV-2 genome sequence and other possible B-coronavirus genomes shows the greatest similarity (96%) of SARS-CoV-2 with the BatCov RaTG13 bat coronavirus strain. This suggests that the SARS-CoV-2 virus naturally evolved from the RaTG13 virus strain transmitted by bats. However, confirmation of its origin requires further research and investigation [8,9].
According to the latest scientific research, the SARS-CoV-2 virus can cause pathology in various organs of the human body. Previous reports refer to selected systems, there are numerical and methodological limitations in research, the effects of infection presented in the literature are often unclear and presumed. For this reason, the authors of this article decided to synthesize the existing research on the effects of infection with this virus and its impact on various organs and organ systems in order to be able to determine which of them affects the most and combine individual reports into a coherent whole [10,11,12,13,14,15,16,17,18,19].
1.2. Symptoms of Infection
This disease primarily affects the respiratory system with symptoms such as dyspnea, dry cough and, in severe cases, causes acute respiratory failure. Other common symptoms include elevated body temperature, general weakness, skeletal pain, as well as neurological symptoms such as loss or impairment of the sense of smell and taste, and headaches [4,6,20].
1.3. Characteristics of Infections Caused by SARS-CoV-2 Virus
Respiratory failure and acute respiratory distress syndrome (ARDS) are the most common complications of a severe COVID-19 infection. Most hospitalized COVID-19 patients suffer from severe lung injuries, fatal multi-organ failure, and hemolytic anemia [6,21]. The high rates of airborne and contact dispersal, and the persistence of the SARS-CoV-2 virus on the surface explain the rapid spread and difficulty of controlling the development of COVID-19 infection [1,4,6]. According to the currently available scientific evidence, it turns out that despite the resolution of typical symptoms, infection with SARS-CoV-2 virus can leave a long-lasting mark in the form of the damage and dysfunction of many organs [22,23,24]. The SARS-CoV-2 virus, in addition to changes in the lungs, can disturb the functions of almost all organs, but mainly the heart, blood vessels, brain and neurons, as well as the kidneys, liver and reproductive organs [16,22,23,24,25,26,27,28,29]. These effects have been noticed relatively recently and may signal an increased risk of long-term health problems. Complications of viral infection, as well as the possibility of reinfection, due to the lack of immunity and the weakening of the functions of the organs after infection, are becoming a major health problem. While most SARS-CoV-2 infected patients recover very quickly, the potential long-term problems caused by the infection make it imperative to look for and investigate late complications caused by the SARS-CoV-2 virus [22].
1.4. Pathogenesis
The virus causes multi-organ damage. It is assumed that this may be due to a systemic increase in inflammatory mediators, i.e., cytokine storm caused by virus infection. The release of a large number of pro-inflammatory cytokines causes a significant increase in the permeability of blood vessels and disorders of blood coagulation, which easily cause organ damage. It is also assumed that the same mechanism causes increased permeability of brain microvessels, so that the SARS-CoV-2 virus can easily cross the blood–brain barrier and enter the nervous system, thus causing a number of disorders, not only typically neurological, but also to other organ systems [23]. An uncontrolled and poorly recognized host response to a cytokine storm is one of the leading causes of severe COVID-19 conditions. In this pandemic scenario, there is an irresistible need to investigate the mechanisms involved in the hyper-inflammatory process and the production of extracellular neutrophil traps (NET) in response to COVID-19, which can lead to a cascade of inflammatory reactions that destroy surrounding tissues including the lungs, heart and kidneys [30]. It is also worth mentioning that SARS-CoV-2 has approximately 80% of the amino acid sequences consistent with SARS-CoV-1 of severe acute respiratory syndrome, which caused over 8000 infections in 2003 [20]. Both viruses use serine transmembrane protease 2 (TMPRSS2) and angiotensin converting enzyme receptor 2 (ACE2) to infect host cells. In addition to the lungs, ACE2 is expressed in many tissues including the cardiovascular system, gastrointestinal tract and liver. Correspondingly, damage to these organs has been observed in COVID-19 patients [6,31]. Observing the effects of previous epidemics of similar viruses can provide a wealth of clues for analyzing the impact of the SARS-CoV-2 virus and predict the potential long-term effects of COVID-19 as they are just emerging in the current pandemic.
2. Objective
The aim of the study was to review the latest research on the long-term effects of COVID-19 and determine how common these symptoms are and who is most at risk of them.
3. Materials and Methods
3.1. Search Strategy and Selection Criteria
We used Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) to conduct this systematic review. An electronic search of scientific articles written in English was made in the electronic databases of PubMed and Web of Science (from 2019 to 2021). The compilation of scientific articles was based on the following search strategy and keywords: long-term effects, long-term complications, long-term manifestations, SARS-CoV-2, COVID-19, health complications after COVID-19, cardiovascular system, heart, nervous system, brain, respiratory system, reproductive system, urinary tract, kidney. Terms and keywords were entered in various configurations with an AND or OR hyphen. In this way, a total of 991 works were found. Published case reports, clinical trials and literature reviews were included. All selected studies met the following inclusion criteria: studies published in the years 2019–2021, written in English, referring to the long-term health effects of SARS-CoV-2 infection, and conducted on people over 18 years of age. The exclusion criteria included articles that did not address the effects of SARS-CoV-2 (e.g., treatment only), which covered hospitalization and symptoms and short-term effects, and studies describing deceased patients as well as the effects of SARS-CoV-2 observed on cadavers. In addition, studies on the effects of the pandemic as lockdown, lockdown and isolation on quality of life and health. Animal studies were also excluded. The inclusion and exclusion criteria are also presented in Table 1.

Table 1.
Inclusion and exclusion criteria.
3.2. Results
A total of 1008 articles were identified in the databases, although some were excluded because they analyzed explicit topics that were beyond the scope of this study. After eliminating duplicated studies, 964 studies remained. After selecting by title, abstract and full text, 935 articles were excluded. Ultimately, 88 studies met the inclusion criteria, and they were subjected to the final analysis (Figure 1).
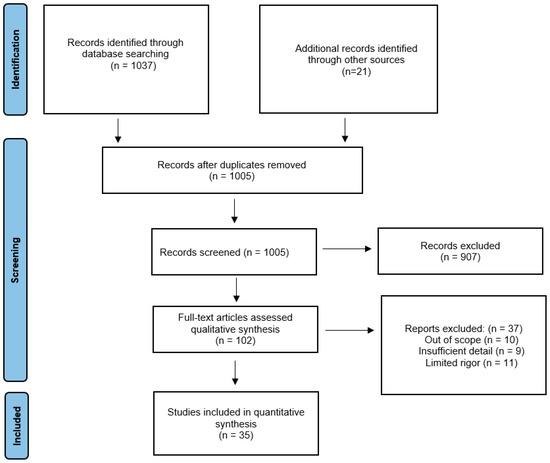
Figure 1.
PRISMA Flow diagram.
4. Circulatory System
According to the Centers for Disease Control and Prevention, elderly patients with coronary artery disease, hypertension or diabetes are more likely to be infected with SARS-CoV-2. Cardiovascular diseases are also associated with a worse prognosis and a more severe course of COVID-19. The virus can also cause heart injuries such as cardiomyopathy and malfunction of the conduction system. Research suggests direct myocardial involvement in some patients [25,32,33].
Overall, infectious myocarditis is the most common cardiac complication of COVID-19 infection. SARS-CoV-2 uses angiotensin converting enzyme 2 (ACE2) receptors to infect host cells, which may cause pneumonia and damage to the heart muscle. High expression of ACE2 receptors in the lungs and heart may increase the risk of cardiac injuries in COVID-19 patients [33]. Tachycardia is also a common cardiovascular complication in COVID-19 patients [34]. Patients with COVID-19 may experience venous and arterial thrombosis due to acute inflammation and hypoxia [26,35]. There are also a large number of late arterial and venous complications.
Cardiovascular complications that are hazardous to health after suffering from SARS-CoV-2 virus infection may develop even several months after the disease and also concern young people, not burdened with additional chronic diseases, which could worsen the course of the infection. The convalescent’s circulatory system manifests its deteriorating condition through, inter alia, arrhythmia, chest pain, and shortness of breath during minimal physical exertion [22]. Patients who have recovered from COVID-19 may experience persistent myocardial involvement as shown by CMR (cardiac magnetic resonance) examination. The main symptoms of CMR included edema, fibrosis, and impaired right ventricular systolic function. The heart condition of COVID-19 patients and survivors must be closely monitored, cardiac CMR can be a sensitive imaging tool coupled with laboratory tests to identify myocardial involvement in COVID-19 patients [10,11,36]. Electrocardiography and echocardiography can also be used to diagnose and predict prognosis in patients with COVID-19 [34] Table 2.

Table 2.
The main effects of COVID-19 on the circulatory system.
5. Nervous System
Numerous studies indicate that the virus is neurotrophic, which means that the virus can enter the nervous system and cause disturbances in its functioning, which also increases the chances of causing long-term effects. The mechanism by which the virus enters the brain is not fully understood. The considerations to date indicate that the S protein of the virus is bound by the ACE2 receptor, which is found in significant amounts in endothelial cells of brain microvasculature. It is believed that this protein may cross the blood–brain barrier. In addition, an infection-induced cytokine storm causes vasodilation in the brain, further facilitating the passage of the virus through the blood–brain barrier into the nervous system. In addition, the virus can enter the brain bypassing the bloodstream. This occurs via the olfactory nerve and travels through the trans-synaptic route to the brain [39]. Neuronal damage caused by COVID-19 may be a driving force behind chronic degenerative diseases of the nervous system. Regardless of its direct or indirect effects, damage to the CNS (central nervous system) following COVID-19 can be permanent [23]. The exact mechanisms by which the virus acts on the nervous system and the underlying causes of the neurological symptoms and effects are unknown. There is only probable speculation that there may be degenerative damage to neurons and glial cells, which are two of the essential elements needed for proper nerve conduction and for the physiological functioning of the brain [40]. In early 2020, the first reports of neuropsychiatric complications during COVID-19 appeared. They related to the occurrence of frequent headaches and dizziness during the infection. Case analysis showed the presence of these symptoms in 36.4% of COVID-19 patients. On the other hand, the group with the severe course of the disease reported disturbed consciousness and cerebrovascular disease [41]. Complications such as encephalitis and encephalopathy have been reported less frequently in the literature [27,28,42,43]. One study estimated that long-term neuropsychiatric consequences may affect approximately 20% of people. The most frequently mentioned were insomnia, depression, anxiety and psychosis. The most frequently presented long-term symptoms include chronic fatigue (53.6), anxiety, depressive symptoms (26.8) and PTSD symptoms (12.2) [28]. First of all, the more known and frequently occurring neurological symptoms caused by SARS-CoV-2 are cognitive disorders, also known as brain fog. These symptoms include general disorientation, confusion, forgetfulness, loss of short-term memory, and significant attention and concentration problems. Headaches and dizziness are also characteristic [44]. This is confirmed by the work on changes in the EEG recording in patients with COVID-19. The information contained in it shows that as a result of infection, new, previously unknown patterns in the EEG recording may appear, which may indicate completely new disorders, or there are waves with specific frequencies characteristic for given neurological diseases and disorders. For example, one of the more common changes in an electroencephalogram are patterns characteristic of encephalopathy, which may explain the appearance of cognitive impairment and a general phenomenon called brain fog [45]. These changes may be caused by a cytokine storm resulting from an excessive response of the immune system, brain hypoxia as a result of which neurons with higher oxygen demand are damaged or by cerebral microcirculation disorders related to infection. Factors such as stress related to infection, dehydration due to difficulties in drinking fluids and fever, sleep disturbances and limited physical activity are also indicated. The individual health situation of the patient is also important [46]. The term brain fog often appears in reports on the chronic effects of COVID-19, and despite the lack of a formal definition, diagnostic categories and inclusion in the international classifications ICD-10 and DSM-V, this concept has been around for a long time. It is used to describe the symptom complexes occurring, inter alia, in Lyme disease, neurosis, Leśniewski-Crohn’s disease, chronic fatigue syndrome, fibromyalgia or celiac disease [47,48,49,50]. A questionnaire study was carried out on a group of 2696 people with documented COVID-19 disease, aged between 18–55 years, a minimum of 3 months after the onset of symptoms. Of these people, 62.3% had long COVID-19 syndrome, and related brain fog occurred in 7.2% of patients, correlating with the female sex and breathing problems in the acute phase of COVID-19 [46]. A very common result of infection are neurological symptoms in the form of long-lasting disturbances of smell and taste. They appear at early stages of the disease and are more common in SARS-CoV-2 infection than in other upper respiratory tract infections. They mainly consist of the loss of these senses, but it may be that they are weakened or appear in the form of parosmia, i.e., feeling a smell completely different from what is actually present, or in the form of a phantosmia, i.e., olfactory hallucinations consisting in perceiving non-existent smells. Post-viral anosmia accounts for up to 40% of cases infected with SARS-CoV-2 [13], with previous coronavirus outbreaks reporting only 10–15% of such cases [51]. There were also reports of 33.9% of those infected with at least one of the olfactory or taste disorders, and 18.3% had both [13]. In another study, 83% of people had anosmia as the first symptom, and 2/3 of them were female. It is worth noting that olfactory disorders occurred without inflammation or symptoms of rhinitis, which leads to the conclusion that the virus directly attacks the mechanisms of odor processing [52]. These symptoms last for about two months [53]. However, there are studies showing that in some infected people, changes in taste and smell persist even 6 months after the infection [52].
It is also considered that SARS-CoV-2 may also contribute to the emergence of mental disorders. This virus activates mechanisms in the body that engage pro-inflammatory cytokine pathways and mechanisms of oxidative stress. They can lead to an imbalance in the regulation of glutamic acid, which contributes to the development of mental disorders [54] Table 3.

Table 3.
The main effects of COVID-19 on the nervous system.
6. Respiratory System
Due to the fact that the virus primarily affects the respiratory system, it seems justified that it leaves a trace of its infection in the organs of this system. First of all, among convalescents, difficulties in breathing, quick fatigue and significantly reduced endurance to physical exertion are observed. In diagnostic tests, a reduction in the diffusion capacity of carbon dioxide is often observed. In addition, a frequent sight in CT (computed tomography) scans are lung fibrosis or scarring of the respiratory tissues, but depending on the period after hospitalization, the results of diagnostic tests and the observed disorders differ. Nevertheless, these changes may hinder the functioning of the respiratory system and result in the above-mentioned symptoms for a long time after recovery [23,24,59]. Most scientific studies have examined the effects of COVID-19 six months after hospitalization. It has been proven that the vast majority of patients six months after undergoing SARS-CoV-2 show dysfunctions related to the respiratory system. These include mainly accompanying chronic fatigue or severely reduced performance capacity, persistent cough, and exercise dyspnea. In patients examined six months after hospitalization for COVID-19, changes in CT were often associated with the appearance of opacities and fibrosis in the lung tissue. In a large number of patients, a reduced diffusion capacity was also revealed in the functional test [29,60,61,62]. Studies were also carried out one year after hospitalization of COVID-19 patients. Long-term respiratory effects were also observed in them, however, they were associated with a smaller percentage of the subjects and were less intense. The most persistent symptoms are associated fatigue, increased sweating, and tightness in the chest. Patients continued to exhibit reduced performance and reduced diffusion capacity. In the conducted experiments on changes in the CT image, fibrosis was observed in most of the studied patients [63,64,65] Table 4.

Table 4.
The main effects of COVID-19 on the respiratory system.
7. Urinary System
Kidney-related conditions are also included among the long-term effects faced by convalescents. Effects such as proteinuria, oliguria or hematuria are observed [16]. Acute nephritis is frequently observed during infection. It can be the result of multi-organ damage caused by a virus or a direct infection of the virus [17]. An episode of acute nephritis during infection may result in long-term consequences in the form of permanent impairment of kidney function, which in the future may result in kidney failure and the need for dialysis. For this reason, constant monitoring of patients after SARS-CoV-2 infection is necessary [70] Table 5.

Table 5.
The main effects of COVID-19 on the urinary system.
8. Reproductive System
Current research confirms that SARS-CoV-2 may affect the male reproductive system [71]. SARS-CoV-2 virus attacks host cells through a cell receptor, angiotensin-converting enzyme 2 (ACE2), which provides a binding site for the coronavirus S (Spike) protein. This is important due to the fact that ACE2 plays a dominant role in fertility, especially in oocyte maturation, ovulation and spermatogenesis [72]. This is because the ACE2 receptor is present in the testes and male genital tract, which is where the S protein is expressed while viral infection occurs, suggesting a high probability that it attacks the male reproductive organs during infection [73]. Abnormal levels of sex hormones and deteriorating sperm quality were observed in patients during and after recovery from COVID-19, and severe inflammatory lesions were detected in the testicles. Testicular samples from 2 of the 10 postmortems showed testicular inflammation of unknown origin, but very little data was reported in the study [74]. In addition, in two separate study reports, lesions such as inflammatory damage to the seminiferous tubules with interstitial edema, embolism, inflammatory cell infiltration, and red blood cell effusion were observed in 6 and 11 of 12 patients who died from SARS-CoV-2, respectively [18,75]. In addition, eight patients had varying degrees of impairment in spermatogenesis [75]. In 23 patients hospitalized due to COVID-19, Li et al. also took semen samples. Upon examination, the number of apoptotic cells in the seminal tubules was significantly higher in COVID-19 compared to control cases. It also showed an increased concentration of CD3+ and CD68+ in the interstitial cells of testicular tissue and the presence of IgG in the seminal tubules. The semen of patients hospitalized for COVID-19 showed that 39.1% (n = 9) of them had oligozoospermia, and 60.9% (n = 14) showed a significant increase in semen leukocytes. Reduced sperm concentration and increased levels of IL-6, TNF-α and MCP-1 in semen were observed compared to the control group [18]. Most importantly, both studies did not detect the SARS-CoV-2 virus in testicular samples with testicular inflammation, suggesting that inflammatory responses rather than viral infections predominated in these lesions [18,75]. The potential impact of fever on sperm quality is indicated. Four patients with moderate infection and fever had reduced semen quality, but whether it was due to inflammation or fever remained unresolved [76]. Infection-related fever has transient adverse effects on spermatogenesis and sperm quality, but usually does not cause irreversible negative effects on male fertility. The adverse effect on sperm is characterized by reduced concentrations, changes in morphology, reduced mobility, and increased DNA fragmentation. These defects may persist for months after the fever has resolved. However, there is no conclusive evidence of the presence of the virus in testicular tissue. The SARS-CoV-2 virus was not present in the testicular tissue of a patient who died in the acute phase of COVID-19 [77]. However, another study showed that the virus can be detected in many organs including the testes [78]. Yang et al., examined testicular samples from 12 deceased COVID-19 patients. The virus was detected in only one patient who had a high viral titer. The SARS-CoV-2 virus was not present in the seminal tubules, but only in the interstitium, and it was not clear whether the virus was derived from the blood or from a testicular infection [18]. In the case of COVID-19, a very important question was whether the virus is sexually transmitted. In six small cohort studies, no viral nucleic acids were found in sperm samples from male patients with mild disease and in the healing phase [18,76,78,79,80,81]. The SARS-CoV-2 virus was not found in the prostate fluid in two independent studies [82,83]. However, one study has shown that SARS-CoV-2 can pass into semen. In this study, out of 23 recovering from COVID-19 and 15 with acute phase patients, 2 (8.7%) and 4 (26.7%) patients, respectively, had positive test for the virus in their semen. This study stands in contrast to previous studies, but it lacks a detailed methodology [84].
All of these studies have a small number of samples. Moreover, the amount of viral RNA in semen was low compared to other tissues and ejaculate collection procedures are prone to contamination. Larger and multicenter studies are needed to draw convincing results regarding the presence or absence of SARS-CoV-2 in semen, especially in patients with early disease or asymptomatic disease. However, according to the available studies, the likelihood of the virus entering the semen in patients in a mild state or in the recovery phase is very low. The injurious effect on male fertility has already been observed during infections with Zika viruses (ZIKV), mumps (MuV) and SARS-CoV-1, while in the case of SARS-CoV-2 the picture of the virus is still incomplete. Long-term surveillance and research will be required to better understand the mechanisms of infection and pathophysiology. However, previous studies of the aforementioned viruses, especially SARS-CoV-1, could provide significant clues regarding the analysis of the effects of COVID-19 on male reproductive performance [85].
Some researchers also link COVID-19 with erectile dysfunction. A study was conducted to assess the odds ratio of the occurrence of erectile dysfunction in patients with a history of COVID-19 with and without comorbidities. Out of a total population of 1,066,108 patients, 9554 were diagnosed with erectile dysfunction. The total number of COVID-19 patients was 7098 (3098 are male) and 146 were diagnosed with both erectile dysfunction and COVID-19. In all cases, the diagnosis of COVID-19 preceded the diagnosis of erectile dysfunction. This means that patients with COVID-19 were 3.68 times more likely to develop erectile dysfunction than patients without COVID-19. SARS-CoV-2 virus infection and erectile dysfunction are strongly related, even after considering known risk factors and demographics [86]. Male gonads may potentially be susceptible to SARS-CoV-2 infection, suggesting caution in observing and evaluating infected men who are planning to conceive. More research is needed to determine if this impairment is temporary or permanent, to elucidate the strategies for SARS-CoV-2 entry into the testes, and how this might affect sperm quality and quantity [87]. The probability of SARS-CoV-2 occurring in the semen of COVID-19 patients is very low, and the semen should rarely be considered a carrier of the SARS-CoV-2 genetic material. However, COVID-19 can cause spermatogenic testicular dysfunction through immune or inflammatory responses. Long-term follow-up is needed in male COVID-19 patients and fetuses conceived during the father’s infection [88]. Information on the involvement of the genitourinary system in recovered COVID-19 patients is very limited. A study was conducted involving men aged 20–50 who were diagnosed with SARS-CoV-2 infection and recovered. Urine samples, prostate secretion, and semen were collected from them in order to detect SARS-CoV-2 RNA. Semen quality and hormonal profiles were analyzed. Seventy-four men were examined. The median interval between the last positive pharyngeal swab RT-PCR test and semen collection was 80 days. The median age was 31 years. The overall sperm quality of COVID-19 patients who recovered was above the WHO lower reference limit. Compared to the healthy control, sperm concentration, total sperm count, and total mobility were all significantly reduced. Moreover, the different clinical types of COVID-19 show no significant differences in semen parameters, but the total sperm count shows a downward trend. Interestingly, people with longer recovery times showed worse data on sperm quality [89] Table 6.

Table 6.
The main effects of COVID-19 on the reproductive system.
Although research suggests that SARS-CoV-2 may also attack female fertility, no known damage to the reproductive system of a COVID-19 patient has been reported so far, and there is very little information on this topic.
9. Digestive System
More and more studies have reported liver damage in patients with COVID-19, and several have shown that patients with COVID-19 have an increased risk of liver dysfunction [90,91,92,93,94]. Most studies showed a higher risk of liver damage in severe COVID-19 than in mildly affected patients, however the exact extent of liver involvement is not clear [95,96]. In a meta-analysis of 12 studies with 1267 patients, the combined incidence of liver injury was 19%, the incidence of ALT elevation was 18%, the incidence of AST elevation was 21% and the incidence of total bilirubin elevation was 6% [97]. Additionally, the level of liver damage appears to correlate with the occurrence of gastrointestinal symptoms. Jini et al. found that the incidence of elevated AST levels was significantly higher in patients with gastrointestinal symptoms than in those without [97]. Xu et al. observed moderate microbial steatosis and mild lobular and portal activity in liver biopsy samples from a patient with COVID-19, which provided evidence of liver damage [98]. It is worth noting that elevated prothrombin time among COVID-19 patients with digestive symptoms is common, and several studies report that thromboembolism is a clinical symptom of COVID-19 [19,99,100,101]. Therefore, liver function and liver enzyme levels should be monitored at an early stage in COVID-19 patients with digestive symptoms. COVID-19 may contribute to the deterioration of liver function in patients who have previously been diagnosed with chronic liver disease and predict an increased risk of severe liver disease. Several studies have shown that the baseline severity of liver disease is strongly associated with the morbidity and mortality associated with COVID-19. Additionally, decompensated cirrhosis, liver cancer, and alcohol-related liver disease are risk factors for adverse COVID-19 outcomes [102,103,104,105,106]. In a multicenter study involving 867 patients with chronic liver disease and COVID-19, 14.0% of patients died, 60.4% were hospitalized, 23% were admitted to the ICU, and 7.7% had decompensated liver function [103]. Another study found that the mortality rate was 32% in COVID-19 patients with pre-existing cirrhosis compared to 8% in those without [107]. Mooni et al. found that 23.3% of patients with cirrhosis and COVID-19 were admitted to the ICU, 17.5% were treated with invasive ventilation, 18.6% received non-invasive ventilation, 4.9% received renal replacement therapy, and 39.8% died [108]. The currently collected data suggest that SARS-CoV-2 infection in patients with cirrhosis appears to be a particularly lethal combination. Compared with patients without baseline liver disease, patients with baseline liver disease have an unfavorable prognosis.
The mechanisms of liver damage in COVID-19 patients are complex. The higher overall mortality among patients with cirrhosis and COVID-19 may be due to the immune dysfunction associated with cirrhosis and metabolic syndrome [109,110], while this requires further studies to be confirmed and investigated Table 7.

Table 7.
The main effects of COVID-19 on the digestive system.
10. Strengths and Limitations
The studies analyzed in this article provide important information on the risks and pathologies that can be caused by SARS-CoV-2 infection in the body. There are many reliable reports and analyses carried out on large groups of patients subjected to long observations under the supervision of specialists. Many of them clearly indicate which organs are most often abnormal due to infection, and which mechanisms have been disrupted and how [28,29,46,52,55,56,58,60,63,64,65,66,67,68,69]. Nevertheless, a significant proportion of the articles analyzed in this study have some limitations. They mainly concern small groups of respondents, or the research methodology is often unclear, while the conclusions drawn are based on guesswork and are not confirmed. More research is needed because the pandemic is too short-lived to be able to predict with certainty the long-term effects of COVID-19 on the human body. Importantly, there is no distinction made between vaccinated and non-vaccinated patients [11,12,14,16,17,37,54,61,86,89,97].
11. Conclusions
There is evidence that the virus can cause long-term complications for more than six months. They mainly concern disturbances in the functioning of the nervous, circulatory and respiratory systems. However, these studies are small or too short-term, and many are speculative. The duration of the epidemic has been too short to be able to conduct reliable studies of the long-term effects of SARS-CoV-2 infection. It is necessary to conduct many years of research on large groups of people that will take into account such factors as: age, gender, demography, level of medical care, the severity of the disease and comorbidities of a person who has had COVID-19.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Hilgenfeld, R.; Peiris, M. From SARS to MERS: 10 years of research on highly pathogenic human coronaviruses. Antivir. Res. 2013, 100, 286–295. [Google Scholar] [CrossRef] [PubMed]
- Zaki, A.M.; van Boheemen, S.; Bestebroer, T.M.; Osterhaus, A.D.; Fouchier, R.A. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N. Engl. J. Med. 2012, 367, 1814–1820. [Google Scholar] [CrossRef] [PubMed]
- Eckerle, I.; Müller, M.A.; Kallies, S.; Gotthardt, D.N.; Drosten, C. In-vitro renal epithelial cell infection reveals a viral kidney tropism as a potential mechanism for acute renal failure during Middle East Respiratory Syndrome (MERS) Coronavirus infection. Virol. J. 2013, 10, 359. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Organization World Health Coronavirus Disease 2019 (COVID-19): Situation Report, 92; World Helath Organization: Geneva, Switzerland, 2020.
- Oberfeld, B.; Achanta, A.; Carpenter, K.; Chen, P.; Gilette, N.M.; Langat, P.; Said, J.T.; Schiff, A.E.; Zhou, A.S.; Barczak, A.K.; et al. SnapShot: COVID-19. Cell 2020, 181, 954.e1. [Google Scholar] [CrossRef] [PubMed]
- Hasöksüz, M.; Kiliç, S.; Saraç, F. Coronaviruses and SARS-CoV-2. Turk. J. Med. Sci. 2020, 50, 549–556. [Google Scholar] [CrossRef]
- Poduri, R.; Joshi, G.; Jagadeesh, G. Drugs targeting various stages of the SARS-CoV-2 life cycle: Exploring promising drugs for the treatment of COVID-19. Cell. Signal. 2020, 74, 109721. [Google Scholar] [CrossRef]
- Lundstrom, K.; Seyran, M.; Pizzol, D.; Adadi, P.; Abd El-Aziz, T.M.; Hassan, S.S.; Soares, A.; Kandimalla, R.; Tambuwala, M.M.; Aljabali, A.; et al. Viewpoint: Origin of SARS-CoV-2. Viruses 2020, 12, 1203. [Google Scholar] [CrossRef]
- Wrobel, A.G.; Benton, D.J.; Xu, P.; Roustan, C.; Martin, S.R.; Rosenthal, P.B.; Skehel, J.J.; Gamblin, S.J. SARS-CoV-2 and bat RaTG13 spike glycoprotein structures inform on virus evolution and furin-cleavage effects. Nat. Struct. Mol. Biol. 2020, 27, 763–767. [Google Scholar] [CrossRef]
- Huang, L.; Zhao, P.; Tang, D.; Zhu, T.; Han, R.; Zhan, C.; Liu, W.; Zeng, H.; Tao, Q.; Xia, L. Cardiac Involvement in Patients Recovered From COVID-2019 Identified Using Magnetic Resonance Imaging. JACC Cardiovasc. Imaging 2020, 13, 2330–2339. [Google Scholar] [CrossRef]
- Puntmann, V.O.; Carerj, M.L.; Wieters, I.; Fahim, M.; Arendt, C.; Hoffmann, J.; Shchendrygina, A.; Escher, F.; Vasa-Nicotera, M.; Zeiher, A.M.; et al. Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020, 5, 1265–1273. [Google Scholar] [CrossRef]
- Veyre, F.; Poulain-Veyre, C.; Esparcieux, A.; Monsarrat, N.; Aouifi, A.; Lapeze, J.; Chatelard, P. Femoral Arterial Thrombosis in a Young Adult after Nonsevere COVID-19. Ann. Vasc. Surg. 2020, 69, 85–88. [Google Scholar] [CrossRef] [PubMed]
- Giacomelli, A.; Pezzati, L.; Conti, F.; Bernacchia, D.; Siano, M.; Oreni, L.; Rusconi, S.; Gervasoni, C.; Ridolfo, A.L.; Rizzardini, G.; et al. Self-reported Olfactory and Taste Disorders in Patients With Severe Acute Respiratory Coronavirus 2 Infection: A Cross-sectional Study. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2020, 71, 889–890. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Almeria, M.; Cejudo, J.C.; Sotoca, J.; Deus, J.; Krupinski, J. Cognitive profile following COVID-19 infection: Clinical predictors leading to neuropsychological impairment. Brain Behav. Immun.-Health 2020, 9, 100163. [Google Scholar] [CrossRef] [PubMed]
- Daher, A.; Balfanz, P.; Cornelissen, C.; Müller, A.; Bergs, I.; Marx, N.; Müller-Wieland, D.; Hartmann, B.; Dreher, M.; Müller, T. Follow up of patients with severe coronavirus disease 2019 (COVID-19): Pulmonary and extrapulmonary disease sequelae. Respir. Med. 2020, 174, 106197. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.; Luo, R.; Wang, X.; Wang, K.; Zhang, N.; Zhang, M.; Wang, Z.; Dong, L.; Li, J.; Zeng, R.; et al. The Incidence, Risk Factors, and Prognosis of Acute Kidney Injury in Adult Patients with Coronavirus Disease 2019. Clin. J. Am. Soc. Nephrol. CJASN 2020, 15, 1394–1402. [Google Scholar] [CrossRef]
- Peng, S.; Wang, H.Y.; Sun, X.; Li, P.; Ye, Z.; Li, Q.; Wang, J.; Shi, X.; Liu, L.; Yao, Y.; et al. Early versus late acute kidney injury among patients with COVID-19-a multicenter study from Wuhan, China. Nephrol. Dial. Transplant. Off. Publ. Eur. Dial. Transpl. Assoc.-Eur. Ren. Assoc. 2020, 35, 2095–2102. [Google Scholar] [CrossRef]
- Li, H.; Xiao, X.; Zhang, J.; Zafar, M.I.; Wu, C.; Long, Y.; Lu, W.; Pan, F.; Meng, T.; Zhao, K.; et al. Impaired spermatogenesis in COVID-19 patients. EClinicalMedicine 2020, 28, 100604. [Google Scholar] [CrossRef]
- Chen, S.; Liu, H.; Li, T.; Huang, R.; Gui, R.; Zhang, J. Correlation analysis of coagulation dysfunction and liver damage in patients with novel coronavirus pneumonia: A single-center, retrospective, observational study. Upsala J. Med. Sci. 2020, 125, 293–296. [Google Scholar] [CrossRef]
- Gralinski, L.E.; Menachery, V.D. Return of the Coronavirus: 2019-nCoV. Viruses 2020, 12, 135. [Google Scholar] [CrossRef] [Green Version]
- Wang, X.; Fang, X.; Cai, Z.; Wu, X.; Gao, X.; Min, J.; Wang, F. Comorbid Chronic Diseases and Acute Organ Injuries Are Strongly Correlated with Disease Severity and Mortality among COVID-19 Patients: A Systemic Review and Meta-Analysis. Research 2020, 2020, 2402961. [Google Scholar] [CrossRef] [Green Version]
- SeyedAlinaghi, S.; Afsahi, A.M.; MohsseniPour, M.; Behnezhad, F.; Salehi, M.A.; Barzegary, A.; Mirzapour, P.; Mehraeen, E.; Dadras, O. Late Complications of COVID-19; a Systematic Review of Current Evidence. Arch. Acad. Emerg. Med. 2021, 9, e14. [Google Scholar] [PubMed]
- Wang, F.; Kream, R.M.; Stefano, G.B. Long-Term Respiratory and Neurological Sequelae of COVID-19. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2020, 26, e928996. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Leon, S.; Wegman-Ostrosky, T.; Perelman, C.; Sepulveda, R.; Rebolledo, P.A.; Cuapio, A.; Villapol, S. More than 50 long-term effects of COVID-19: A systematic review and meta-analysis. Sci. Rep. 2021, 11, 16144. [Google Scholar] [CrossRef] [PubMed]
- Aghagoli, G.; Gallo Marin, B.; Soliman, L.B.; Sellke, F.W. Cardiac involvement in COVID-19 patients: Risk factors, predictors, and complications: A review. J. Card. Surg. 2020, 35, 1302–1305. [Google Scholar] [CrossRef] [PubMed]
- Klok, F.A.; Kruip, M.; van der Meer, N.; Arbous, M.S.; Gommers, D.; Kant, K.M.; Kaptein, F.; van Paassen, J.; Stals, M.; Huisman, M.V.; et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb. Res. 2020, 191, 145–147. [Google Scholar] [CrossRef] [PubMed]
- Filatov, A.; Sharma, P.; Hindi, F.; Espinosa, P.S. Neurological Complications of Coronavirus Disease (COVID-19): Encephalopathy. Cureus 2020, 12, e7352. [Google Scholar] [CrossRef] [Green Version]
- Qi, R.; Chen, W.; Liu, S.; Thompson, P.M.; Zhang, L.J.; Xia, F.; Cheng, F.; Hong, A.; Surento, W.; Luo, S.; et al. Psychological morbidities and fatigue in patients with confirmed COVID-19 during disease outbreak: Prevalence and associated biopsychosocial risk factors. medRxiv, 2020; preprint. [Google Scholar] [CrossRef] [PubMed]
- Wu, Q.; Zhong, L.; Li, H.; Guo, J.; Li, Y.; Hou, X.; Yang, F.; Xie, Y.; Li, L.; Xing, Z. A Follow-Up Study of Lung Function and Chest Computed Tomography at 6 Months after Discharge in Patients with Coronavirus Disease 2019. Can. Respir. J. 2021, 2021, 6692409. [Google Scholar] [CrossRef] [PubMed]
- Borges, L.; Pithon-Curi, T.C.; Curi, R.; Hatanaka, E. COVID-19 and Neutrophils: The Relationship between Hyperinflammation and Neutrophil Extracellulachr Traps. Mediat. Inflamm. 2020, 2020, 8829674. [Google Scholar] [CrossRef]
- Xiao, F.; Tang, M.; Zheng, X.; Liu, Y.; Li, X.; Shan, H. Evidence for Gastrointestinal Infection of SARS-CoV-2. Gastroenterology 2020, 158, 1831–1833.e3. [Google Scholar] [CrossRef]
- Mehraeen, E.; Hayati, B.; Saeidi, S.; Heydari, M.; Seyedalinaghi, S. Self-Care Instructions for People Not Requiring Hospitalization for Coronavirus Disease 2019 (COVID-19). Arch. Clin. Infect. Dis. 2020, 15 (COVID-19), e102978. [Google Scholar] [CrossRef] [Green Version]
- Inciardi, R.M.; Lupi, L.; Zaccone, G.; Italia, L.; Raffo, M.; Tomasoni, D.; Cani, D.S.; Cerini, M.; Farina, D.; Gavazzi, E.; et al. Cardiac Involvement in a Patient With Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020, 5, 819–824. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bandyopadhyay, D.; Akhtar, T.; Hajra, A.; Gupta, M.; Das, A.; Chakraborty, S.; Pal, I.; Patel, N.; Amgai, B.; Ghosh, R.K.; et al. COVID-19 Pandemic: Cardiovascular Complications and Future Implications. Am. J. Cardiovasc. Drugs Drugs Devices Other Interv. 2020, 20, 311–324. [Google Scholar] [CrossRef] [PubMed]
- Landi, A.; De Servi, S. The burden of thrombotic complications in critically ill patients with COVID-19: Charting the uncharted. Intern. Emerg. Med. 2020, 15, 893–895. [Google Scholar] [CrossRef] [PubMed]
- Shchendrygina, A.; Nagel, E.; Puntmann, V.O.; Valbuena-Lopez, S. COVID-19 myocarditis and prospective heart failure burden. Expert Rev. Cardiovasc. Ther. 2021, 19, 5–14. [Google Scholar] [CrossRef]
- Shergill, S.; Davies, J.; Bloomfield, J. Florid aortitis following SARS-CoV-2 infection. Eur. Heart J. 2020, 41, 4286. [Google Scholar] [CrossRef]
- Brito, D.; Meester, S.; Yanamala, N.; Patel, H.B.; Balcik, B.J.; Casaclang-Verzosa, G.; Seetharam, K.; Riveros, D.; Beto, R.J., 2nd; Balla, S.; et al. High Prevalence of Pericardial Involvement in College Student Athletes Recovering From COVID-19. JACC Cardiovasc. Imaging 2021, 14, 541–555. [Google Scholar] [CrossRef]
- Iadecola, C.; Anrather, J.; Kamel, H. Effects of COVID-19 on the Nervous System. Cell 2020, 183, 16–27.e1. [Google Scholar] [CrossRef]
- Baig, A.M. Deleterious Outcomes in Long-Hauler COVID-19: The Effects of SARS-CoV-2 on the CNS in Chronic COVID Syndrome. ACS Chem. Neurosci. 2020, 11, 4017–4020. [Google Scholar] [CrossRef]
- Mao, X.Y.; Jin, W.L. iPSCs-Derived Platform: A Feasible Tool for Probing the Neurotropism of SARS-CoV-2. ACS Chem. Neurosci. 2020, 11, 2489–2491. [Google Scholar] [CrossRef]
- Huang, Y.H.; Jiang, D.; Huang, J.T. SARS-CoV-2 Detected in Cerebrospinal Fluid by PCR in a Case of COVID-19 Encephalitis. Brain Behav. Immun. 2020, 87, 149. [Google Scholar] [CrossRef]
- Ye, M.; Ren, Y.; Lv, T. Encephalitis as a clinical manifestation of COVID-19. Brain Behav. Immun. 2020, 88, 945–946. [Google Scholar] [CrossRef] [PubMed]
- Østergaard, L. SARS CoV-2 related microvascular damage and symptoms during and after COVID-19: Consequences of capillary transit-time changes, tissue hypoxia and inflammation. Physiol. Rep. 2021, 9, e14726. [Google Scholar] [CrossRef] [PubMed]
- Kopańska, M.; Banaś-Ząbczyk, A.; Łagowska, A.; Kuduk, B.; Szczygielski, J. Changes in EEG Recordings in COVID-19 Patients as a Basis for More Accurate QEEG Diagnostics and EEG Neurofeedback Therapy: A Systematic Review. J. Clin. Med. 2021, 10, 1300. [Google Scholar] [CrossRef] [PubMed]
- Asadi-Pooya, A.A.; Akbari, A.; Emami, A.; Lotfi, M.; Rostamihosseinkhani, M.; Nemati, H.; Barzegar, Z.; Kabiri, M.; Zeraatpisheh, Z.; Farjoud-Kouhanjani, M.; et al. Long COVID syndrome-associated brain fog. J. Med. Virol. 2021, 94, 979–984. [Google Scholar] [CrossRef]
- Yelland, G.W. Gluten-induced cognitive impairment (“brain fog”) in coeliac disease. J. Gastroenterol. Hepatol. 2017, 32 (Suppl. S1), 90–93. [Google Scholar] [CrossRef] [Green Version]
- Ibraheem, W.; Mckenzie, S.; Wilcox-Omubo, V.; Abdelaty, M.; Saji, S.E.; Siby, R.; Alalyani, W.; Mostafa, J.A. Pathophysiology and Clinical Implications of Cognitive Dysfunction in Fibromyalgia. Cureus 2021, 13, e19123. [Google Scholar] [CrossRef]
- Ocon, A.J. Caught in the thickness of brain fog: Exploring the cognitive symptoms of Chronic Fatigue Syndrome. Front. Physiol. 2013, 4, 63. [Google Scholar] [CrossRef] [Green Version]
- Bransfield, R.C.; Aidlen, D.M.; Cook, M.J.; Javia, S. A Clinical Diagnostic System for Late-Stage Neuropsychiatric Lyme Borreliosis Based upon an Analysis of 100 Patients. Healthcare 2020, 8, 13. [Google Scholar] [CrossRef] [Green Version]
- Eccles, R. Understanding the symptoms of the common cold and influenza. Lancet Infect. Dis. 2005, 5, 718–725. [Google Scholar] [CrossRef]
- Hopkins, C.; Surda, P.; Vaira, L.A.; Lechien, J.R.; Safarian, M.; Saussez, S.; Kumar, N. Six month follow-up of self-reported loss of smell during the COVID-19 pandemic. Rhinology 2021, 59, 26–31. [Google Scholar] [CrossRef]
- Nguyen, N.N.; Hoang, V.T.; Lagier, J.C.; Raoult, D.; Gautret, P. Long-term persistence of olfactory and gustatory disorders in COVID-19 patients. Clin. Microbiol. Infect. Off. Publ. Eur. Soc. Clin. Microbiol. Infect. Dis. 2021, 27, 931–932. [Google Scholar] [CrossRef]
- Janiri, D.; Kotzalidis, G.D.; Giuseppin, G.; Molinaro, M.; Modica, M.; Montanari, S.; Terenzi, B.; Carfì, A.; Landi, F.; Sani, G.; et al. Psychological Distress After covid-19 Recovery: Reciprocal Effects With Temperament and Emotional Dysregulation. An Exploratory Study of Patients Over 60 Years of Age Assessed in a Post-acute Care Service. Front. Psychiatry 2020, 11, 590135. [Google Scholar] [CrossRef] [PubMed]
- Otte, M.S.; Eckel, H.; Poluschkin, L.; Klussmann, J.P.; Luers, J.C. Olfactory dysfunction in patients after recovering from COVID-19. Acta Oto-Laryngol. 2020, 140, 1032–1035. [Google Scholar] [CrossRef] [PubMed]
- Vaira, L.A.; Hopkins, C.; Petrocelli, M.; Lechien, J.R.; Chiesa-Estomba, C.M.; Salzano, G.; Cucurullo, M.; Salzano, F.A.; Saussez, S.; Boscolo-Rizzo, P.; et al. Smell and taste recovery in coronavirus disease 2019 patients: A 60-day objective and prospective study. J. Laryngol. Otol. 2020, 134, 703–709. [Google Scholar] [CrossRef]
- McPeake, J.; Shaw, M.; MacTavish, P.; Blyth, K.G.; Devine, H.; Fleming, G.; Griffin, J.; Gemmell, L.; Grose, P.; Henderson, M.; et al. Long-term outcomes following severe COVID-19 infection: A propensity matched cohort study. BMJ Open Respir. Res. 2021, 8, e001080. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, G.K.; Khedr, E.M.; Hamad, D.A.; Meshref, T.S.; Hashem, M.M.; Aly, M.M. Long term impact of COVID-19 infection on sleep and mental health: A cross-sectional study. Psychiatry Res. 2021, 305, 114243. [Google Scholar] [CrossRef] [PubMed]
- Leo, F.; Wormanns, D.; Grohé, C. COVID-19 aus Sicht der Pneumologie—Langzeitfolgen und Implikationen für die pneumologische Nachsorge [COVID-19: A Pneumological Point of View—Long-Term Sequelae of COVID-19—Implications For Follow-up In Respiratory Medicine]. Dtsch. Med. Wochenschr. 2020, 145, 1086–1092. [Google Scholar]
- Safont, B.; Tarraso, J.; Rodriguez-Borja, E.; Fernández-Fabrellas, E.; Sancho-Chust, J.N.; Molina, V.; Lopez-Ramirez, C.; Lope-Martinez, A.; Cabanes, L.; Andreu, A.L.; et al. Lung Function, Radiological Findings and Biomarkers of Fibrogenesis in a Cohort of COVID-19 Patients Six Months After Hospital Discharge. Arch. Bronconeumol. 2021, 58, 142–149. [Google Scholar] [CrossRef]
- Ekbom, E.; Frithiof, R.; Öi, E.; Larson, I.M.; Lipcsey, M.; Rubertsson, S.; Wallin, E.; Janson, C.; Hultström, M.; Malinovschi, A. Impaired diffusing capacity for carbon monoxide is common in critically ill COVID-19 patients at four months post-discharge. Respir. Med. 2021, 182, 106394. [Google Scholar]
- Han, X.; Fan, Y.; Alwalid, O.; Li, N.; Jia, X.; Yuan, M.; Li, Y.; Cao, Y.; Gu, J.; Wu, H.; et al. Six-month Follow-up Chest CT Findings after Severe COVID-19 Pneumonia. Radiology 2021, 299, E177–E186. [Google Scholar] [CrossRef]
- Fang, X.; Ming, C.; Cen, Y.; Lin, H.; Zhan, K.; Yang, S.; Li, L.; Cao, G.; Li, Q.; Ma, X. Post-sequelae one year after hospital discharge among older COVID-19 patients: A multi-center prospective cohort study. J. Infect. 2021, 84, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.; Tao, M.; Shang, L.; Liu, Y.; Pan, G.; Jin, Y.; Wang, L.; Hu, S.; Li, J.; Zhang, M.; et al. Assessment of Sequelae of COVID-19 Nearly 1 Year After Diagnosis. Front. Med. 2021, 8, 717194. [Google Scholar] [CrossRef]
- Steinbeis, F.; Thibeault, C.; Doellinger, F.; Ring, R.M.; Mittermaier, M.; Ruwwe-Glösenkamp, C.; Alius, F.; Knape, P.; Meyer, H.J.; Lippert, L.J.; et al. Severity of respiratory failure and computed chest tomography in acute COVID-19 correlates with pulmonary function and respiratory symptoms after infection with SARS-CoV-2: An observational longitudinal study over 12 months. Respir. Med. 2021, 191, 106709. [Google Scholar] [CrossRef] [PubMed]
- Sonnweber, T.; Sahanic, S.; Pizzini, A.; Luger, A.; Schwabl, C.; Sonnweber, B.; Kurz, K.; Koppelstätter, S.; Haschka, D.; Petzer, V.; et al. Cardiopulmonary recovery after COVID-19: An observational prospective multicentre trial. Eur. Respir. J. 2021, 57, 2003481. [Google Scholar] [CrossRef] [PubMed]
- van der Sar-van der Brugge, S.; Talman, S.; Boonman-de Winter, L.; de Mol, M.; Hoefman, E.; van Etten, R.W.; De Backer, I.C. Pulmonary function and health-related quality of life after COVID-19 pneumonia. Respir. Med. 2021, 176, 106272. [Google Scholar] [CrossRef]
- Lerum, T.V.; Aaløkken, T.M.; Brønstad, E.; Aarli, B.; Ikdahl, E.; Lund, K.; Durheim, M.T.; Rodriguez, J.R.; Meltzer, C.; Tonby, K.; et al. Dyspnoea, lung function and CT findings 3 months after hospital admission for COVID-19. Eur. Respir. J. 2021, 57, 2003448. [Google Scholar] [CrossRef]
- González, J.; Benítez, I.D.; Carmona, P.; Santisteve, S.; Monge, A.; Moncusí-Moix, A.; Gort-Paniello, C.; Pinilla, L.; Carratalá, A.; Zuil, M.; et al. Pulmonary Function and Radiologic Features in Survivors of Critical COVID-19: A 3-Month Prospective Cohort. Chest 2021, 160, 187–198. [Google Scholar] [CrossRef]
- Huang, C.; Huang, L.; Wang, Y.; Li, X.; Ren, L.; Gu, X.; Kang, L.; Guo, L.; Liu, M.; Zhou, X.; et al. 6-month consequences of COVID-19 in patients discharged from hospital: A cohort study. Lancet 2021, 397, 220–232. [Google Scholar] [CrossRef]
- Sharma, I.; Kumari, P.; Sharma, A.; Saha, S.C. SARS-CoV-2 and the reproductive system: Known and the unknown..!! Middle East Fertil. Soc. J. 2021, 26, 1. [Google Scholar] [CrossRef]
- Huang, H.H.; Wang, P.H.; Yang, Y.P.; Chou, S.J.; Chu, P.W.; Wu, G.J.; Chang, C.C. A review of severe acute respiratory syndrome coronavirus 2 infection in the reproductive system. J. Chin. Med. Assoc. JCMA 2020, 83, 895–897. [Google Scholar] [CrossRef]
- Huang, C.; Ji, X.; Zhou, W.; Huang, Z.; Peng, X.; Fan, L.; Lin, G.; Zhu, W. Coronavirus: A possible cause of reduced male fertility. Andrology 2021, 9, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Duarte-Neto, A.N.; Monteiro, R.; da Silva, L.; Malheiros, D.; de Oliveira, E.P.; Theodoro-Filho, J.; Pinho, J.; Gomes-Gouvêa, M.S.; Salles, A.; de Oliveira, I.; et al. Pulmonary and systemic involvement in COVID-19 patients assessed with ultrasound-guided minimally invasive autopsy. Histopathology 2020, 77, 186–197. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Chen, S.; Huang, B.; Zhong, J.M.; Su, H.; Chen, Y.J.; Cao, Q.; Ma, L.; He, J.; Li, X.F.; et al. Pathological Findings in the Testes of COVID-19 Patients: Clinical Implications. Eur. Urol. Focus 2020, 6, 1124–1129. [Google Scholar] [CrossRef]
- Holtmann, N.; Edimiris, P.; Andree, M.; Doehmen, C.; Baston-Buest, D.; Adams, O.; Kruessel, J.S.; Bielfeld, A.P. Assessment of SARS-CoV-2 in human semen-a cohort study. Fertil. Steril. 2020, 114, 233–238. [Google Scholar] [CrossRef] [PubMed]
- Carlsen, E.; Andersson, A.M.; Petersen, J.H.; Skakkebaek, N.E. History of febrile illness and variation in semen quality. Hum. Reprod. 2003, 18, 2089–2092. [Google Scholar] [CrossRef] [PubMed]
- Song, C.; Wang, Y.; Li, W.; Hu, B.; Chen, G.; Xia, P.; Wang, W.; Li, C.; Diao, F.; Hu, Z.; et al. Absence of 2019 novel coronavirus in semen and testes of COVID-19 patients. Biol. Reprod. 2020, 103, 4–6. [Google Scholar] [CrossRef] [PubMed]
- Guo, L.; Zhao, S.; Li, W.; Wang, Y.; Li, L.; Jiang, S.; Ren, W.; Yuan, Q.; Zhang, F.; Kong, F.; et al. Absence of SARS-CoV-2 in semen of a COVID-19 patient cohort. Andrology 2021, 9, 42–47. [Google Scholar] [CrossRef]
- Ma, L.; Xie, W.; Li, D.; Shi, L.; Ye, G.; Mao, Y.; Xiong, Y.; Sun, H.; Zheng, F.; Chen, Z.; et al. Evaluation of sex-related hormones and semen characteristics in reproductive-aged male COVID-19 patients. J. Med. Virol. 2021, 93, 456–462. [Google Scholar] [CrossRef]
- Pan, F.; Xiao, X.; Guo, J.; Song, Y.; Li, H.; Patel, D.P.; Spivak, A.M.; Alukal, J.P.; Zhang, X.; Xiong, C.; et al. No evidence of severe acute respiratory syndrome-coronavirus 2 in semen of males recovering from coronavirus disease 2019. Fertil. Steril. 2020, 113, 1135–1139. [Google Scholar] [CrossRef]
- Quan, W.; Zheng, Q.; Tian, J.; Chen, J.; Liu, Z.; Chen, X.; Wu, T.; Ji, Z.; Tang, J.; Chu, H. No SARS-CoV-2 in expressed prostatic secretion of patients with coronavirus disease 2019: A descriptive multicentre study in China. medRxiv 2020. [Google Scholar] [CrossRef]
- Zhang, S.; Wang, X.; Zhang, H.; Xu, A.; Fei, G.; Jiang, X.; Tu, J.; Qu, G.; Xu, X.; Li, Y. The absence of coronavirus in expressed prostatic secretion in COVID-19 patients in Wuhan city. Reprod. Toxicol. 2020, 96, 90–94. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Jin, M.; Bao, P.; Zhao, W.; Zhang, S. Clinical Characteristics and Results of Semen Tests Among Men With Coronavirus Disease 2019. JAMA Netw. Open 2020, 3, e208292. [Google Scholar] [CrossRef] [PubMed]
- Tian, Y.; Zhou, L.Q. Evaluating the impact of COVID-19 on male reproduction. Reproduction 2021, 161, R37–R44. [Google Scholar] [CrossRef] [PubMed]
- Katz, J.; Yue, S.; Xue, W.; Gao, H. Increased odds ratio for erectile dysfunction in COVID-19 patients. J. Endocrinol. Investig. 2021, 45, 859–864. [Google Scholar] [CrossRef]
- Agolli, A.; Yukselen, Z.; Agolli, O.; Patel, M.H.; Bhatt, K.P.; Concepcion, L.; Halpern, J.; Alvi, S.; Abreu, R. SARS-CoV-2 effect on male infertility and its possible pathophysiological mechanisms. Discoveries 2021, 9, e131. [Google Scholar] [CrossRef]
- He, Y.; Wang, J.; Ren, J.; Zhao, Y.; Chen, J.; Chen, X. Effect of COVID-19 on Male Reproductive System—A Systematic Review. Front. Endocrinol. 2021, 12, 677701. [Google Scholar] [CrossRef]
- Ruan, Y.; Hu, B.; Liu, Z.; Liu, K.; Jiang, H.; Li, H.; Li, R.; Luan, Y.; Liu, X.; Yu, G.; et al. No detection of SARS-CoV-2 from urine, expressed prostatic secretions, and semen in 74 recovered COVID-19 male patients: A perspective and urogenital evaluation. Andrology 2021, 9, 99–106. [Google Scholar] [CrossRef]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- Chen, N.; Zhou, M.; Dong, X.; Qu, J.; Gong, F.; Han, Y.; Qiu, Y.; Wang, J.; Liu, Y.; Wei, Y.; et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020, 395, 507–513. [Google Scholar] [CrossRef] [Green Version]
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA 2020, 323, 1061–1069. [Google Scholar] [CrossRef]
- Gao, Y.; Li, T.; Han, M.; Li, X.; Wu, D.; Xu, Y.; Zhu, Y.; Liu, Y.; Wang, X.; Wang, L. Diagnostic utility of clinical laboratory data determinations for patients with the severe COVID-19. J. Med. Virol. 2020, 92, 791–796. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Yu, Y.; Xu, J.; Shu, H.; Xia, J.; Liu, H.; Wu, Y.; Zhang, L.; Yu, Z.; Fang, M.; et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir. Med. 2020, 8, 475–481. [Google Scholar] [CrossRef] [Green Version]
- Zhang, C.; Shi, L.; Wang, F.S. Liver injury in COVID-19: Management and challenges. Lancet Gastroenterol. Hepatol. 2020, 5, 428–430. [Google Scholar] [CrossRef]
- Mao, R.; Qiu, Y.; He, J.S.; Tan, J.Y.; Li, X.H.; Liang, J.; Shen, J.; Zhu, L.R.; Chen, Y.; Iacucci, M.; et al. Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: A systematic review and meta-analysis. Lancet Gastroenterol. Hepatol. 2020, 5, 667–678. [Google Scholar] [CrossRef]
- Jin, X.; Lian, J.S.; Hu, J.H.; Gao, J.; Zheng, L.; Zhang, Y.M.; Hao, S.R.; Jia, H.Y.; Cai, H.; Zhang, X.L.; et al. Epidemiological, clinical and virological characteristics of 74 cases of coronavirus-infected disease 2019 (COVID-19) with gastrointestinal symptoms. Gut 2020, 69, 1002–1009. [Google Scholar] [CrossRef] [Green Version]
- Xu, Z.; Shi, L.; Wang, Y.; Zhang, J.; Huang, L.; Zhang, C.; Liu, S.; Zhao, P.; Liu, H.; Zhu, L.; et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 2020, 8, 420–422. [Google Scholar] [CrossRef]
- Oxley, T.J.; Mocco, J.; Majidi, S.; Kellner, C.P.; Shoirah, H.; Singh, I.P.; De Leacy, R.A.; Shigematsu, T.; Ladner, T.R.; Yaeger, K.A.; et al. Large-Vessel Stroke as a Presenting Feature of COVID-19 in the Young. N. Engl. J. Med. 2020, 382, e60. [Google Scholar] [CrossRef]
- Zhang, L.; Feng, X.; Zhang, D.; Jiang, C.; Mei, H.; Wang, J.; Zhang, C.; Li, H.; Xia, X.; Kong, S.; et al. Deep Vein Thrombosis in Hospitalized Patients With COVID-19 in Wuhan, China: Prevalence, Risk Factors, and Outcome. Circulation 2020, 142, 114–128. [Google Scholar] [CrossRef]
- Cao, T.; Zhang, G.; Xie, H.; Pellegrini, E.; Li, J.; Chen, X.; Pan, H. Case Report: The Coronavirus Disease 2019 (COVID-19) Pneumonia With Multiple Thromboembolism. Front. Neurol. 2020, 11, 625272. [Google Scholar] [CrossRef]
- Qi, X.; Liu, Y.; Wang, J.; Fallowfield, J.A.; Li, X.; Shi, J.; Pan, H.; Zou, S.; Zhang, H.; Chen, Z.; et al. Clinical course and risk factors for mortality of COVID-19 patients with pre-existing cirrhosis: A multicentre cohort study. Gut 2021, 70, 433–436. [Google Scholar] [CrossRef]
- Kim, D.; Adeniji, N.; Latt, N.; Kumar, S.; Bloom, P.P.; Aby, E.S.; Perumalswami, P.; Roytman, M.; Li, M.; Vogel, A.S.; et al. Predictors of Outcomes of COVID-19 in Patients with Chronic Liver Disease: US Multi-center Study. Clin. Gastroenterol. Hepatol. 2020, 19, 1469–1479.e19. [Google Scholar] [CrossRef] [PubMed]
- Kuderer, N.M.; Choueiri, T.K.; Shah, D.P.; Shyr, Y.; Rubinstein, S.M.; Rivera, D.R.; Shete, S.; Hsu, C.Y.; Desai, A.; de Lima Lopes, G., Jr.; et al. Clinical impact of COVID-19 on patients with cancer (CCC19): A cohort study. Lancet 2020, 395, 1907–1918. [Google Scholar] [CrossRef]
- Singh, S.; Khan, A. Clinical Characteristics and Outcomes of Coronavirus Disease 2019 Among Patients With Preexisting Liver Disease in the United States: A Multicenter Research Network Study. Gastroenterology 2020, 159, 768–771.e3. [Google Scholar] [CrossRef] [PubMed]
- Bajaj, J.S.; Garcia-Tsao, G.; Biggins, S.W.; Kamath, P.S.; Wong, F.; McGeorge, S.; Shaw, J.; Pearson, M.; Chew, M.; Fagan, A.; et al. Comparison of mortality risk in patients with cirrhosis and COVID-19 compared with patients with cirrhosis alone and COVID-19 alone: Multicentre matched cohort. Gut 2021, 70, 531–536. [Google Scholar] [CrossRef]
- Marjot, T.; Moon, A.M.; Cook, J.A.; Abd-Elsalam, S.; Aloman, C.; Armstrong, M.J.; Pose, E.; Brenner, E.J.; Cargill, T.; Catana, M.A.; et al. Outcomes following SARS-CoV-2 infection in patients with chronic liver disease: An international registry study. J Hepatol. 2021, 74, 567–577. [Google Scholar] [CrossRef]
- Moon, A.M.; Webb, G.J.; Aloman, C.; Armstrong, M.J.; Cargill, T.; Dhanasekaran, R.; Genescà, J.; Gill, U.S.; James, T.W.; Jones, P.D.; et al. High mortality rates for SARS-CoV-2 infection in patients with pre-existing chronic liver disease and cirrhosis: Preliminary results from an international registry. J. Hepatol. 2020, 73, 705–708. [Google Scholar] [CrossRef]
- Albillos, A.; Lario, M.; Álvarez-Mon, M. Cirrhosis-associated immune dysfunction: Distinctive features and clinical relevance. J. Hepatol. 2014, 61, 1385–1396. [Google Scholar] [CrossRef] [Green Version]
- Mehta, P.; McAuley, D.F.; Brown, M.; Sanchez, E.; Tattersall, R.S.; Manson, J.J. HLH Across Speciality Collaboration. UK COVID-19: Consider cytokine storm syndromes and immunosuppression. Lancet 2020, 395, 1033–1034. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).