Management and Medical Therapy of Mild Hypercortisolism
Abstract
1. Introduction
2. Diagnosis of Mild Hypercortisolism
3. Management of Mild Hypercortisolism
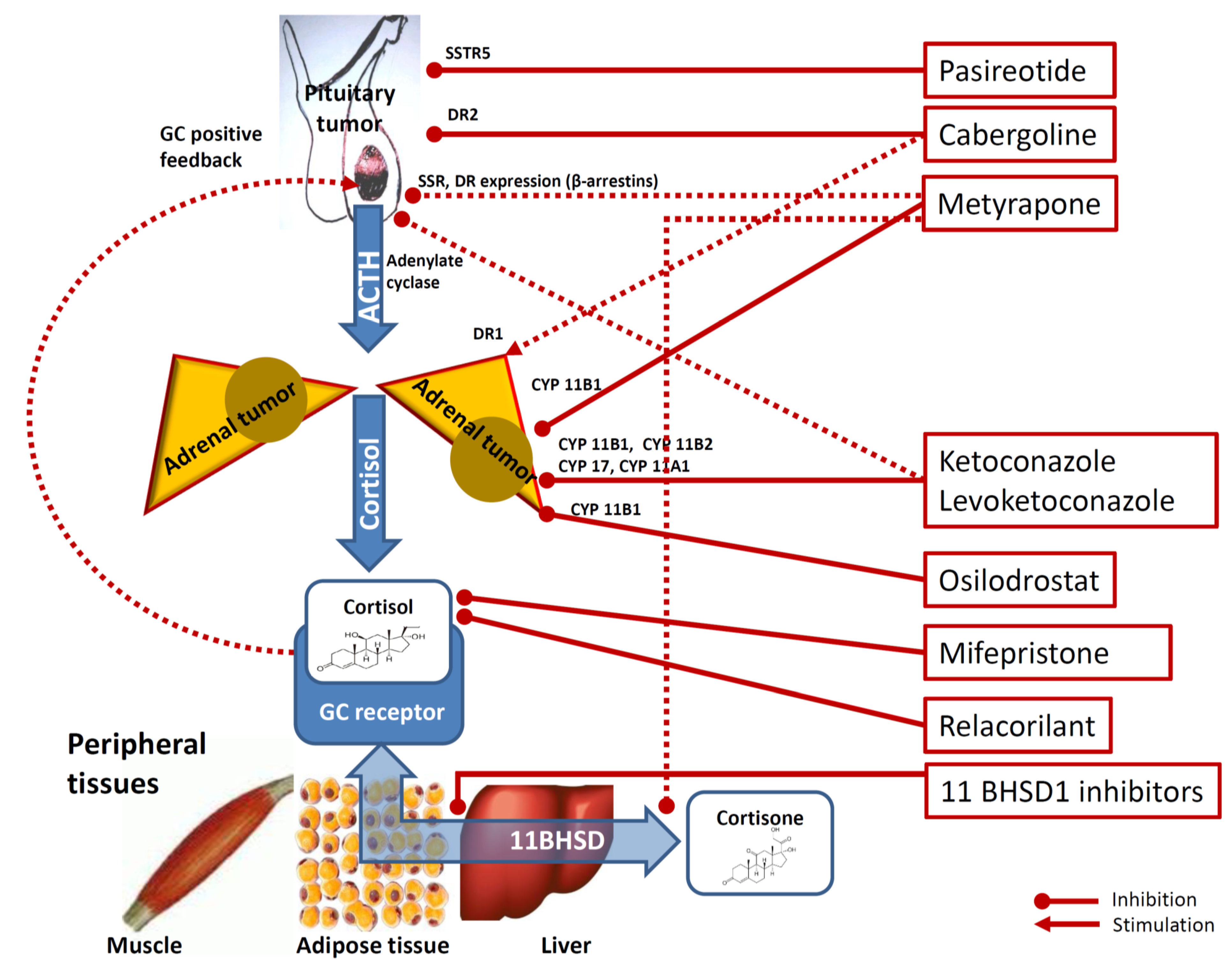
4. Medical Therapy of Mild Hypercortisolism
4.1. Pituitary-Directed Drugs
4.1.1. Pasireotide
4.1.2. Cabergoline
4.2. Adrenal Steroidogenesis Inhibiting Agents
4.2.1. Metyrapone
4.2.2. Ketoconazole
4.2.3. Levoketoconazole
4.2.4. Osilodrostat
4.3. Glucocorticoid Receptor-Directed Drugs
4.3.1. Mifepristone
4.3.2. Relacorilant
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nieman, L.K. Cushing’s syndrome: Update on signs, symptoms and biochemical screening. Eur. J. Endocrinol. 2015, 173, M33–M38. [Google Scholar] [CrossRef] [PubMed]
- Chiodini, I. Diagnosis and Treatment of Subclinical Hypercortisolism. J. Clin. Endocrinol. Metab. 2011, 96, 1223–1236. [Google Scholar] [CrossRef]
- Morelli, V.; Ghielmetti, A.; Caldiroli, A.; Grassi, S.; Siri, F.M.; Caletti, E.; Mucci, F.; Aresta, C.; Passeri, E.; Pugliese, F.; et al. Mental Health in Patients with Adrenal Incidentalomas: Is There a Relation with Different Degrees of Cortisol Secretion? J. Clin. Endocrinol. Metab. 2021, 106, e130–e139. [Google Scholar] [CrossRef]
- Aresta, C.; Favero, V.; Morelli, V.; Giovanelli, L.; Parazzoli, C.; Falchetti, A.; Pugliese, F.; Gennari, L.; Vescini, F.; Salcuni, A.; et al. Cardiovascular complications of mild autonomous cortisol secretion. Best Pract. Res. Clin. Endocrinol. Metab. 2021, 35, 101494. [Google Scholar] [CrossRef]
- Zavatta, G.; Di Dalmazi, G. Recent Advances on Subclinical Hypercortisolism. Endocrinol. Metab. Clin. N. Am. 2018, 47, 375–383. [Google Scholar] [CrossRef] [PubMed]
- Di Dalmazi, G.; Vicennati, V.; Garelli, S.; Casadio, E.; Rinaldi, E.; Giampalma, E.; Mosconi, C.; Golfieri, R.; Paccapelo, A.; Pagotto, U.; et al. Cardiovascular events and mortality in patients with adrenal incidentalomas that are either non-secreting or associated with intermediate phenotype or subclinical Cushing’s syndrome: A 15-year retrospective study. Lancet Diabetes Endocrinol. 2014, 2, 396–405. [Google Scholar] [CrossRef]
- Chiodini, I.; Eller-Vainicher, C.; Morelli, V.; Palmieri, S.; Cairoli, E.; Salcuni, A.S.; Copetti, M.; Scillitani, A. Mechanisms in endocrinology: Endogenous subclinical hypercortisolism and bone: A clinical review. Eur. J. Endocrinol. 2016, 175, R265–R282. [Google Scholar] [CrossRef]
- Debono, M.; Bradburn, M.; Bull, M.; Harrison, B.; Ross, R.J.; Newell-Price, J. Cortisol as a Marker for Increased Mortality in Patients with Incidental Adrenocortical Adenomas. J. Clin. Endocrinol. Metab. 2014, 99, 4462–4470. [Google Scholar] [CrossRef] [PubMed]
- Kjellbom, A.; Lindgren, O.; Puvaneswaralingam, S.; Löndahl, M.; Olsen, H. Association between Mortality and Levels of Autonomous Cortisol Secretion by Adrenal Incidentalomas. Ann. Intern. Med. 2021, 174, 1041–1049. [Google Scholar] [CrossRef]
- Patrova, J.; Kjellman, M.; Wahrenberg, H.; Falhammar, H. Increased mortality in patients with adrenal incidentalomas and autonomous cortisol secretion: A 13-year retrospective study from one center. Endocrine 2017, 58, 267–275. [Google Scholar] [CrossRef] [PubMed]
- Elhassan, Y.; Alahdab, F.; Prete, A.; Delivanis, D.A.; Khanna, A.; Prokop, L.; Murad, M.H.; O’Reilly, M.W.; Arlt, W.; Bancos, I. Natural History of Adrenal Incidentalomas with and without Mild Autonomous Cortisol Excess. Ann. Intern. Med. 2019, 171, 107–116. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Kaur, R.J.; Zhang, C.D.; Ebbehoj, A.; Singh, S.; Atkinson, E.J.; Achenbach, S.J.; Rocca, W.; Khosla, S.; Bancos, I. Risk of bone fractures after the diagnosis of adrenal adenomas: A population-based cohort study. Eur. J. Endocrinol. 2021, 184, 597–606. [Google Scholar] [CrossRef] [PubMed]
- Giovanelli, L.; Aresta, C.; Favero, V.; Bonomi, M.; Cangiano, B.; Eller-Vainicher, C.; Grassi, G.; Morelli, V.; Pugliese, F.; Falchetti, A.; et al. Hidden hypercortisolism: A too frequently neglected clinical condition. J. Endocrinol. Investig. 2021, 44, 1581–1596. [Google Scholar] [CrossRef]
- Fassnacht, M.; Arlt, W.; Bancos, I.; Dralle, H.; Newell-Price, J.; Sahdev, A.; Tabarin, A.; Terzolo, M.; Tsagarakis, S.; Dekkers, O. Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. Eur. J. Endocrinol. 2016, 175, G1–G34. [Google Scholar] [CrossRef]
- Terzolo, M.; Stigliano, A.; Chiodini, I.; Loli, P.; Furlani, L.; Arnaldi, G.; Reimondo, G.M.; Pia, A.; Toscano, V.; Zini, M.; et al. AME Position Statement on adrenal incidentaloma. Eur. J. Endocrinol. 2011, 164, 851–870. [Google Scholar] [CrossRef] [PubMed]
- Pasternak, J.D.; Seib, C.D.; Seiser, N.; Tyrell, J.B.; Liu, C.; Cisco, R.M.; Gosnell, J.E.; Shen, W.T.; Suh, I.; Duh, Q.-Y. Differences Between Bilateral Adrenal Incidentalomas and Unilateral Lesions. JAMA Surg. 2015, 150, 974–978. [Google Scholar] [CrossRef] [PubMed]
- Morelli, V.; Palmieri, S.; Salcuni, A.S.; Eller-Vainicher, C.; Cairoli, E.; Zhukouskaya, V.; Scillitani, A.; Beck-Peccoz, P.; Chiodini, I. Bilateral and unilateral adrenal incidentalomas: Biochemical and clinical characteristics. Eur. J. Endocrinol. 2013, 168, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Chiodini, I.; Ramos-Rivera, A.; Marcus, A.O.; Yau, H. Adrenal Hypercortisolism: A Closer Look at Screening, Diagnosis, and Important Considerations of Different Testing Modalities. J. Endocr. Soc. 2019, 3, 1097–1109. [Google Scholar] [CrossRef]
- Nieman, L.K.; Biller, B.M.K.; Findling, J.W.; Newell-Price, J.; Savage, M.O.; Stewart, P.M.; Montori, V. The Diagnosis of Cushing’s Syndrome: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2008, 93, 1526–1540. [Google Scholar] [CrossRef] [PubMed]
- Toini, A.; Dolci, A.; Ferrante, E.; Verrua, E.; Malchiodi, E.; Sala, E.; Lania, A.G.; Chiodini, I.; Beck-Peccoz, P.; Arosio, M.; et al. Screening for ACTH-dependent hypercortisolism in patients affected with pituitary incidentaloma. Eur. J. Endocrinol. 2015, 172, 363–369. [Google Scholar] [CrossRef] [PubMed]
- Aresta, C.; Soranna, D.; Giovanelli, L.; Favero, V.; Parazzoli, C.; Gennari, L.; Persani, L.; Scillitani, A.; Blevins, L.S.; Brown, D.; et al. Endocrine Practice When to suspect hidden hypercortisolism in type 2 diabetes: A meta-analysis. Endocr. Pract. 2021. [Google Scholar] [CrossRef] [PubMed]
- Bancos, I.; Alahdab, F.; Crowley, R.K.; Chortis, V.; Delivanis, D.A.; Erickson, D.; Natt, N.; Terzolo, M.; Arlt, W.; Young, W.F.; et al. Improvement of cardiovascular risk factors after adrenalectomy in patients with adrenal tumors and subclinical Cushing’s syndrome: A systematic review and meta-Analysis. Eur. J. Endocrinol. 2016, 175, R283–R295. [Google Scholar] [CrossRef] [PubMed]
- Salcuni, A.S.; Morelli, V.; Vainicher, C.E.; Palmieri, S.; Cairoli, E.; Spada, A.; Scillitani, A.; Chiodini, I. Adrenalectomy reduces the risk of vertebral fractures in patients with monolateral adrenal incidentalomas and subclinical hypercortisolism. Eur. J. Endocrinol. 2016, 174, 261–269. [Google Scholar] [CrossRef]
- Vassiliadi, D.A.; Partsalaki, E.; Tsagarakis, S. Approach to patients with bilateral adrenal incidentalomas. Curr. Opin. Endocrinol. Diabetes Obes. 2020, 27, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Albiger, N.; Ceccato, F.; Zilio, M.; Barbot, M.; Occhi, G.; Rizzati, S.; Fassina, A.; Mantero, F.; Boscaro, M.; Iacobone, M.; et al. An analysis of different therapeutic options in patients with Cushing’s syndrome due to bilateral macronodular adrenal hyperplasia: A single-centre experience. Clin. Endocrinol. 2015, 82, 808–815. [Google Scholar] [CrossRef] [PubMed]
- Delivanis, D.A.; Athimulam, S.; Bancos, I. Modern Management of Mild Autonomous Cortisol Secretion. Clin. Pharmacol. Ther. 2019, 106, 1209–1221. [Google Scholar] [CrossRef] [PubMed]
- Chiodini, I.; Albani, A.; Ambrogio, A.G.; Campo, M.; de Martino, M.C.; Marcelli, G.; Morelli, V.; Zampetti, B.; Colao, A.; Pivonello, R. Six controversial issues on subclinical Cushing’s syndrome. Endocrine 2017, 56, 262–266. [Google Scholar] [CrossRef] [PubMed]
- Fassnacht, M.; Dekkers, O.M.; Else, T.; Baudin, E.; Berruti, A.; de Krijger, R.R.; Haak, H.R.; Mihai, R.; Assie, G.; Terzolo, M. European society of endocrinology clinical practice guidelines on the management of adrenocortical carcinoma in adults, in collaboration with the European Network for the study of adrenal tumors. Eur. J. Endocrinol. 2018, 179, G1–G46. [Google Scholar] [CrossRef]
- Cesareo, R.; Attanasio, R.; Caputo, M.; Castello, R.; Chiodini, I.; Falchetti, A.; Guglielmi, R.; Papini, E.; Santonati, A.; Scillitani, A.; et al. Italian Association of Clinical Endocrinologists (AME) and Italian Chapter of the American Association of Clinical Endocrinologists (AACE) Position Statement: Clinical Management of Vitamin D Deficiency in Adults. Nutrients 2018, 10, 546. [Google Scholar] [CrossRef] [PubMed]
- Sherlock, M.; Scarsbrook, A.; Abbas, A.; Fraser, S.; Limumpornpetch, P.; Dineen, R.; Stewart, P.M. Adrenal incidentaloma. Endocr. Rev. 2020, 41, 775–820. [Google Scholar] [CrossRef]
- Bancos, I.; Taylor, A.E.; Chortis, V.; Sitch, A.; Jenkinson, C.; Davidge-Pitts, C.J.; Lang, K.; Tsagarakis, S.; Macech, M.; Riester, A.; et al. Urine steroid metabolomics for the differential diagnosis of adrenal incidentalomas in the EURINE-ACT study: A prospective test validation study. Lancet Diabetes Endocrinol. 2020, 8, 773–781. [Google Scholar] [CrossRef]
- Morelli, V.; Masserini, B.; Salcuni, A.S.; Eller-Vainicher, C.; Savoca, C.; Viti, R.; Coletti, F.; Guglielmi, G.; Battista, C.; Iorio, L.; et al. Subclinical Hypercortisolism: Correlation between biochemical diagnostic criteria and clinical aspects. Clin. Endocrinol. 2010, 73, 161–166. [Google Scholar] [CrossRef] [PubMed]
- Palmieri, S.; Morelli, V.; Polledri, E.; Fustinoni, S.; Mercadante, R.; Olgiati, L.; Vainicher, C.E.; Cairoli, E.; Zhukouskaya, V.V.; Beck-Peccoz, P.; et al. The role of salivary cortisol measured by liquid chromatography–tandem mass spectrometry in the diagnosis of subclinical hypercortisolism. Eur. J. Endocrinol. 2013, 168, 289–296. [Google Scholar] [CrossRef]
- Braun, L.T.; Riester, A.; Oßwald-Kopp, A.; Fazel, J.; Rubinstein, G.; Bidlingmaier, M.; Beuschlein, F.; Reincke, M. Toward a Diagnostic Score in Cushing’s Syndrome. Front. Endocrinol. 2019, 10, 766. [Google Scholar] [CrossRef] [PubMed]
- Chiodini, I.; Gennari, L. Grand Challenge in Adrenal Endocrinology: Is the Legacy of the Past a Challenge for the Future of Precision Medicine? Front. Endocrinol. 2021, 12, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Nieman, L.K.; Biller, B.M.K.; Findling, J.W.; Murad, M.H.; Newell-Price, J.; Savage, M.O.; Tabarin, A. Treatment of Cushing’s Syndrome: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2015, 100, 2807–2831. [Google Scholar] [CrossRef]
- Miller, B.S.; Auchus, R.J. Evaluation and Treatment of Patients with Hypercortisolism. JAMA Surg. 2020, 155, 1152. [Google Scholar] [CrossRef] [PubMed]
- Perogamvros, I.; Vassiliadi, D.A.; Karapanou, O.; Botoula, E.; Tzanela, M.; Tsagarakis, S. Biochemical and clinical benefits of unilateral adrenalectomy in patients with subclinical hypercortisolism and bilateral adrenal incidentalomas. Eur. J. Endocrinol. 2015, 173, 719–725. [Google Scholar] [CrossRef]
- Morelli, V.; Palmieri, S.; Lania, A.; Tresoldi, A.; Corbetta, S.; Cairoli, E.; Eller-Vainicher, C.; Arosio, M.; Copetti, M.; Grossi, E.; et al. Cardiovascular events in patients with mild autonomous cortisol secretion: Analysis with artificial neural networks. Eur. J. Endocrinol. 2017, 177, 73–83. [Google Scholar] [CrossRef] [PubMed]
- Eller-Vainicher, C.; Morelli, V.; Salcuni, A.S.; Battista, C.; Torlontano, M.; Coletti, F.; Iorio, L.; Cairoli, E.; Beck-Peccoz, P.; Arosio, M.; et al. Accuracy of several parameters of hypothalamic–pituitary–adrenal axis activity in predicting before surgery the metabolic effects of the removal of an adrenal incidentaloma. Eur. J. Endocrinol. 2010, 163, 925–935. [Google Scholar] [CrossRef]
- Oda, S.; Ashida, K.; Uchiyama, M.; Sakamoto, S.; Hasuzawa, N.; Nagayama, A.; Wang, L.; Nagata, H.; Sakamoto, R.; Kishimoto, J.; et al. An Open-label Phase I/IIa Clinical Trial of 11β-HSD1 Inhibitor for Cushing’s Syndrome and Autonomous Cortisol Secretion. J. Clin. Endocrinol. Metab. 2021, 106, e3865–e3880. [Google Scholar] [CrossRef]
- Pivonello, R.; Ferrigno, R.; de Martino, M.C.; Simeoli, C.; Di Paola, N.; Pivonello, C.; Barba, L.; Negri, M.; de Angelis, C.; Colao, A. Medical Treatment of Cushing’s Disease: An Overview of the Current and Recent Clinical Trials. Front. Endocrinol. 2020, 11, 648. [Google Scholar] [CrossRef]
- Ferriere, A.; Tabarin, A. Cushing’s syndrome: Treatment and new therapeutic approaches. Best Pract. Res. Clin. Endocrinol. Metab. 2020, 34, 101381. [Google Scholar] [CrossRef]
- Tritos, N.A.; Biller, B.M. Advances in the Medical Treatment of Cushing Disease. Endocrinol. Metab. Clin. N. Am. 2020, 49, 401–412. [Google Scholar] [CrossRef] [PubMed]
- Patel, Y. Somatostatin and its family of receptors. Front. Neuroendocrinol. 1999, 20, 157–198. [Google Scholar] [CrossRef] [PubMed]
- Gatto, F.; Arvigo, M.; Amarù, J.; Campana, C.; Cocchiara, F.; Graziani, G.; Bruzzone, E.; Giusti, M.; Boschetti, M.; Ferone, D. Cell specific interaction of pasireotide: Review of preclinical studies in somatotroph and corticotroph pituitary cells. Pituitary 2018, 22, 89–99. [Google Scholar] [CrossRef] [PubMed]
- Hofland, L.J.; van der Hoek, J.; Feelders, R.; van Aken, M.O.; van Koetsveld, P.M.; Waaijers, M.; Sprij-Mooij, D.; Bruns, C.; Weckbecker, G.; de Herder, W.W.; et al. The multi-ligand somatostatin analogue SOM230 inhibits ACTH secretion by cultured human corticotroph adenomas via somatostatin receptor type 5. Eur. J. Endocrinol. 2005, 152, 645–654. [Google Scholar] [CrossRef] [PubMed]
- Silva, A.P.; Schoeffter, P.; Weckbecker, G.; Bruns, C.; Schmid, H.A. Regulation of CRH-induced secretion of ACTH and corticosterone by SOM230 in rats. Eur. J. Endocrinol. 2005, 153, R7–R10. [Google Scholar] [CrossRef] [PubMed]
- Bruns, C.; Lewis, I.; Briner, U.; Meno-Tetang, G.; Weckbecker, G. SOM230: A novel somatostatin peptidomimetic with broad somatotropin release inhibiting factor (SRIF) receptor binding and a unique antisecretory profile. Eur. J. Endocrinol. 2002, 146, 707–716. [Google Scholar] [CrossRef] [PubMed]
- Colao, A.; Petersenn, S.; Newell-Price, J.; Findling, J.W.; Boguszewski, C.; Maldonado, M.; Schoenherr, U.; Biol, D.; Mills, D.; Salgado, L.R.; et al. A 12-Month Phase 3 Study of Pasireotide in Cushing’s Disease. N. Engl. J. Med. 2012, 366, 914–924. [Google Scholar] [CrossRef]
- Pivonello, R.; Ferone, D.; de Herder, W.W.; Kros, J.M.; Caro, M.D.B.D.; Arvigo, M.; Annunziato, L.; Lombardi, G.; Colao, A.; Hofland, L.J.; et al. Dopamine Receptor Expression and Function in Corticotroph Pituitary Tumors. J. Clin. Endocrinol. Metab. 2004, 89, 2452–2462. [Google Scholar] [CrossRef] [PubMed]
- Pivonello, R.; Arnaldi, G.; Scaroni, C.; Giordano, C.; Cannavò, S.; Iacuaniello, D.; Trementino, L.; Zilio, M.; Guarnotta, V.; Albani, A.; et al. The medical treatment with pasireotide in Cushing’s disease: An Italian multicentre experience based on “real-world evidence”. Endocrine 2019, 64, 657–672. [Google Scholar] [CrossRef] [PubMed]
- Lacroix, A.; Gu, F.; Gallardo, W.; Pivonello, R.; Yu, Y.; Witek, P.; Boscaro, M.; Salvatori, R.; Yamada, M.; Tauchmanova, L.; et al. Efficacy and safety of once-monthly pasireotide in Cushing’s disease: A 12 month clinical trial. Lancet Diabetes Endocrinol. 2018, 6, 17–26. [Google Scholar] [CrossRef]
- Henry, R.R.; Ciaraldi, T.P.; Armstrong, D.; Burke, P.; Ligueros-Saylan, M.; Mudaliar, S. Hyperglycemia Associated with Pasireotide: Results from a Mechanistic Study in Healthy Volunteers. J. Clin. Endocrinol. Metab. 2013, 98, 3446–3453. [Google Scholar] [CrossRef] [PubMed]
- Farah, J.M.; Malcolm, D.S.; Mueller, G.P. Dopaminergic inhibition of pituitary β-endorphin-like immunoreactivity secretion in the rat. Endocrinology 1982, 110, 657–659. [Google Scholar] [CrossRef] [PubMed]
- Yin, D.; Kondo, S.; Takeuchi, J.; Morimura, T. Induction of apoptosis in murine ACTH-secreting pituitary adenoma cells by bromocriptine. FEBS Lett. 1994, 339, 73–75. [Google Scholar] [CrossRef]
- De Bruin, C.; Hanson, J.; Meij, B.P.; Kooistra, H.S.; Waaijers, A.; Uitterlinden, P.; Lamberts, S.; Hofland, L. Expression and Functional Analysis of Dopamine Receptor Subtype 2 and Somatostatin Receptor Subtypes in Canine Cushing’s Disease. Endocrinol. 2008, 149, 4357–4366. [Google Scholar] [CrossRef] [PubMed]
- Stefaneanu, L.; Kovacs, K.; Horvath, E.; Buchfelder, M.; Fahlbusch, R.; Lancranjan, I. Dopamine D2 Receptor Gene Expression in Human Adenohypophysial Adenomas. Endocrine 2001, 14, 329–336. [Google Scholar] [CrossRef]
- Tateno, T.; Kato, M.; Tani, Y.; Oyama, K.; Yamada, S.; Hirata, Y. Differential Expression of Somatostatin and Dopamine Receptor Subtype Genes in Adrenocorticotropin (ACTH)-secreting Pituitary Tumors and Silent Corticotroph Adenomas. Endocr. J. 2009, 56, 579–584. [Google Scholar] [CrossRef]
- Cooper, O.; Greenman, Y. Dopamine Agonists for Pituitary Adenomas. Front. Endocrinol. 2018, 9, 469. [Google Scholar] [CrossRef]
- Palui, R.; Sahoo, J.; Kamalanathan, S.; Kar, S.S.; Selvarajan, S.; Durgia, H. Effect of cabergoline monotherapy in Cushing’s disease: An individual participant data meta-analysis. J. Endocrinol. Investig. 2018, 41, 1445–1455. [Google Scholar] [CrossRef]
- Matsuo, K.; Sone, M.; Honda-Kohmo, K.; Toyohara, T.; Sonoyama, T.; Taura, D.; Kojima, K.; Fukuda, Y.; Ohno, Y.; Inoue, M.; et al. Significance of dopamine D1 receptor signalling for steroidogenic differentiation of human induced pluripotent stem cells. Sci. Rep. 2017, 7, 15120. [Google Scholar] [CrossRef] [PubMed]
- Ferriere, A.; Cortet, C.; Chanson, P.; Delemer, B.; Caron, P.; Chabre, O.; Reznik, Y.; Bertherat, J.; Rohmer, V.; Briet, C.; et al. Cabergoline for Cushing’s disease: A large retrospective multicenter study. Eur. J. Endocrinol. 2017, 176, 305–314. [Google Scholar] [CrossRef] [PubMed]
- Daniel, E.; Newell-Price, J.D.C. Therapy of endocrine disease: Steroidogenesis enzyme inhibitors in Cushing’s syndrome. Eur. J. Endocrinol. 2015, 172, R263–R280. [Google Scholar] [CrossRef] [PubMed]
- Sampath-Kumar, R.; Yu, M.; Khalil, M.; Yang, K. Metyrapone is a competitive inhibitor of 11β-hydroxysteroid dehydrogenase type 1 reductase. J. Steroid Biochem. Mol. Biol. 1997, 62, 195–199. [Google Scholar] [CrossRef]
- Daniel, E.; Aylwin, S.; Mustafa, O.; Ball, S.; Munir, A.; Boelaert, K.; Chortis, V.; Cuthbertson, D.; Daousi, C.; Rajeev, S.P.; et al. Effectiveness of Metyrapone in Treating Cushing’s Syndrome: A Retrospective Multicenter Study in 195 Patients. J. Clin. Endocrinol. Metab. 2015, 100, 4146–4154. [Google Scholar] [CrossRef]
- Broersen, L.H.A.; Jha, M.; Biermasz, N.R.; Pereira, A.M.; Dekkers, O.M. Effectiveness of medical treatment for Cushing’s syndrome: A systematic review and meta-analysis. Pituitary 2018, 21, 631–641. [Google Scholar] [CrossRef] [PubMed]
- Feelders, R.A.; Newell-Price, J.; Pivonello, R.; Nieman, L.K.; Hofland, L.J.; Lacroix, A. Advances in the medical treatment of Cushing’s syndrome. Lancet Diabetes Endocrinol. 2019, 7, 300–312. [Google Scholar] [CrossRef]
- Verhelst, J.A.; Trainer, P.J.; Howlett, T.A.; Perry, L.; Rees, L.H.; Grossman, A.B.; Wass, J.A.H.; Sesser, G.M. Short and long-term responses to metyrapone in the medical management of 91 patients with Cushing’s syndrome. Clin. Endocrinol. 1991, 35, 169–178. [Google Scholar] [CrossRef]
- Ceccato, F.; Zilio, M.; Barbot, M.; Albiger, N.; Antonelli, G.; Plebani, M.; Watutantrige-Fernando, S.; Sabbadin, C.; Boscaro, M.; Scaroni, C. Metyrapone treatment in Cushing’s syndrome: A real-life study. Endocrine 2018, 62, 701–711. [Google Scholar] [CrossRef] [PubMed]
- Debono, M.; Harrison, R.F.; Chadarevian, R.; Gueroult, C.; Abitbol, J.-L.; Newell-Price, J. Resetting the Abnormal Circadian Cortisol Rhythm in Adrenal Incidentaloma Patients with Mild Autonomous Cortisol Secretion. J. Clin. Endocrinol. Metab. 2017, 102, 3461–3469. [Google Scholar] [CrossRef] [PubMed]
- Puglisi, S.; Perotti, P.; Barbot, M.; Cosio, P.; Scaroni, C.; Stigliano, A.; Lardo, P.; Morelli, V.; Polledri, E.; Chiodini, I.; et al. Preoperative treatment with metyrapone in patients with Cushing’s syndrome due to adrenal adenoma: A pilot prospective study. Endocr. Connect. 2018, 7, 1227–1235. [Google Scholar] [CrossRef] [PubMed]
- Tsujimoto, Y.; Shichi, H.; Fukuoka, H.; Yamamoto, M.; Sato, I.; Imanishi, T.; Nakamura, T.; Inoshita, N.; Ishida, A.; Yamada, S.; et al. Tumor Shrinkage by Metyrapone in Cushing Disease Exhibiting Glucocorticoid-Induced Positive Feedback. J. Endocr. Soc. 2021, 5, bvab055. [Google Scholar] [CrossRef] [PubMed]
- Ayroldi, E.; Cannarile, L.; Delfino, D.V.; Riccardi, C. A dual role for glucocorticoid-induced leucine zipper in glucocorticoid function: Tumor growth promotion or suppression? Cell Death Dis. 2018, 9, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Gatto, F.; Feelders, R.A.; van der Pas, R.; van Koetsveld, P.; Bruzzone, E.; Arvigo, M.; Dogan, F.; Lamberts, S.W.; Ferone, D.; Hofland, L. β-arrestin expression in corticotroph tumor cells is modulated by glucocorticoids. J. Endocrinol. 2020, 245, 101–113. [Google Scholar] [CrossRef]
- Iwayama, H.; Hirase, S.; Nomura, Y.; Ito, T.; Morita, H.; Otake, K.; Okumura, A.; Takagi, J. Spontaneous adrenocorticotropic hormone (ACTH) normalisation due to tumour regression induced by metyrapone in a patient with ectopic ACTH syndrome: Case report and literature review. BMC Endocr. Disord. 2018, 18, 19. [Google Scholar] [CrossRef]
- De Martin, M.; Toja, P.M.; Goulene, K.; Radaelli, P.; Cavagnini, F.; Stramba-Badiale, M.; Giraldi, F.P. No Untoward Effect of Long-Term Ketoconazole Administration on Electrocardiographic QT Interval in Patients with Cushing’s Disease. Basic Clin. Pharmacol. Toxicol. 2015, 118, 279–283. [Google Scholar] [CrossRef] [PubMed]
- Oates, J.A.; Wood, A.J.; Sonino, N. The Use of Ketoconazole as an Inhibitor of Steroid Production. N. Engl. J. Med. 1987, 317, 812–818. [Google Scholar] [CrossRef]
- Fleseriu, M.; Castinetti, F. Updates on the role of adrenal steroidogenesis inhibitors in Cushing’s syndrome: A focus on novel therapies. Pituitary 2016, 19, 643–653. [Google Scholar] [CrossRef] [PubMed]
- Stalla, G.K.; Stalla, J.; Huber, M.; Loeffler, J.-P.; Höllt, V.; Von Werder, K.; Müller, O.A. Ketoconazole Inhibits Corticotropic Cell Function in Vitro. Endocrinology 1988, 122, 618–623. [Google Scholar] [CrossRef]
- Yan, J.Y.; Nie, X.L.; Tao, Q.M.; Zhan, S.Y.; de Zhang, Y. Ketoconazole associated hepatotoxicity: A systematic review and meta- analysis. Biomed. Environ. Sci. 2013, 26, 605–610. [Google Scholar] [CrossRef] [PubMed]
- Tritos, N.A. Adrenally Directed Medical Therapies for Cushing Syndrome. J. Clin. Endocrinol. Metab. 2021, 106, 16–25. [Google Scholar] [CrossRef]
- Castinetti, F.; Morange, I.; Jaquet, P.; Conte-Devolx, B.; Brue, T. Ketoconazole revisited: A preoperative or postoperative treatment in Cushing’s disease. Eur. J. Endocrinol. 2008, 158, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Castinetti, F.; Guignat, L.; Giraud, P.; Muller, M.; Kamenicky, P.; Drui, D.; Caron, P.; Luca, F.; Donadille, B.; Vantyghem, M.C.; et al. Ketoconazole in Cushing’s Disease: Is It Worth a Try? J. Clin. Endocrinol. Metab. 2014, 99, 1623–1630. [Google Scholar] [CrossRef] [PubMed]
- Comte-Perret, S.; Zanchi, A.; Gomez, F. Long-term low-dose ketoconazole treatment in bilateral macronodular adrenal hyperplasia. Endocrinol. Diabetes Metab. Case Rep. 2014, 2014, 140083. [Google Scholar] [CrossRef]
- Novotna, A.; Krasulová, K.; Bartoňková, I.; Korhonova, M.; Bachleda, P.; Anzenbacher, P.; Dvorak, Z. Dual Effects of Ketoconazole cis-Enantiomers on CYP3A4 in Human Hepatocytes and HepG2 Cells. PLoS ONE 2014, 9, e111286. [Google Scholar] [CrossRef]
- Blass, B.E.; Iyer, P.; Abou-Gharbia, M.; Childers, W.E.; Gordon, J.C.; Ramanjulu, M.; Morton, G.; Arumugam, P.; Boruwa, J.; Ellingboe, J.; et al. Design, synthesis, and evaluation of (2 S,4 R)-Ketoconazole sulfonamide analogs as potential treatments for Metabolic Syndrome. Bioorg. Med. Chem. Lett. 2016, 26, 5825–5829. [Google Scholar] [CrossRef] [PubMed]
- Arakaki, R.; Welles, B. Ketoconazole enantiomer for the treatment of diabetes mellitus. Expert Opin. Investig. Drugs 2010, 19, 185–194. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, S.L.; Rendell, M.; Ahmann, A.J.; Thomas, A.; Arauz-Pacheco, C.J.; Welles, B.R. Safety Profile and Metabolic Effects of 14 Days of Treatment with DIO-902: Results of a Phase IIa Multicenter, Randomized, Double-Blind, Placebo-Controlled, Parallel-Group Trial in Patients with Type 2 Diabetes Mellitus. Clin. Ther. 2008, 30, 1081–1088. [Google Scholar] [CrossRef]
- Eller-Vainicher, C.; Scillitani, A.; Chiodini, I. Is the hypothalamic–pituitary–adrenal axis disrupted in type 2 diabetes mellitus and is this relevant for bone health? Endocrine 2017, 58, 201–202. [Google Scholar] [CrossRef] [PubMed]
- Chiodini, I.; Adda, G.; Scillitani, A.; Coletti, F.; Morelli, V.; Di Lembo, S.; Epaminonda, P.; Masserini, B.; Beck-Peccoz, P.; Orsi, E.; et al. Cortisol Secretion in Patients with Type 2 Diabetes: Relationship with chronic complications. Diabetes Care 2006, 30, 83–88. [Google Scholar] [CrossRef] [PubMed]
- Morelli, V.; Aresta, C.; Gaudio, A.; Eller-Vainicher, C.; Zhukouskaya, V.V.; Merlotti, D.; Orsi, E.; Barbieri, A.M.; Fustinoni, S.; Polledri, E.; et al. Prediction of hypertension, diabetes and fractures in eucortisolemic women by measuring parameters of cortisol milieu. Endocrine 2020, 68, 411–419. [Google Scholar] [CrossRef]
- Chiodini, I.; Gaudio, A.; Eller-Vainicher, C.; Morelli, V.; Aresta, C.; Zhukouskaya, V.V.; Merlotti, D.; Orsi, E.; Barbieri, A.M.; Fustinoni, S.; et al. Cortisol Secretion, Sensitivity, and Activity are Associated with Hypertension in Postmenopausal Eucortisolemic Women. J. Clin. Endocrinol. Metab. 2019, 104, 4441–4448. [Google Scholar] [CrossRef]
- Pivonello, R.; Elenkova, A.; Fleseriu, M.; Feelders, R.A.; Witek, P.; Greenman, Y.; Geer, E.B.; Perotti, P.; Saiegh, L.; Cohen, F.; et al. Levoketoconazole in the Treatment of Patients with Cushing’s Syndrome and Diabetes Mellitus: Results from the SONICS Phase 3 Study. Front. Endocrinol. 2021, 12, 595894. [Google Scholar] [CrossRef]
- Geer, E.B.; Salvatori, R.; Elenkova, A.; Fleseriu, M.; Pivonello, R.; Witek, P.; Feelders, R.A.; Bex, M.; Borresen, S.W.; Puglisi, S.; et al. Levoketoconazole improves clinical signs and symptoms and patient-reported outcomes in patients with Cushing’s syndrome. Pituitary 2021, 24, 104–115. [Google Scholar] [CrossRef]
- Creemers, S.G.; Feelders, R.A.; de Jong, F.H.; Franssen, G.J.H.; de Rijke, Y.B.; van Koetsveld, P.M.; Hofland, L.J. Levoketoconazole, the 2S,4R Enantiomer of Ketoconazole, a New Steroidogenesis Inhibitor for Cushing’s Syndrome Treatment. J. Clin. Endocrinol. Metab. 2021, 106, e1618–e1630. [Google Scholar] [CrossRef] [PubMed]
- Dougherty, J.A.; Desai, D.S.; Herrera, J.B. Osilodrostat: A Novel Steroidogenesis Inhibitor to Treat Cushing’s Disease. Ann. Pharmacother. 2021, 55, 1050–1060. [Google Scholar] [CrossRef]
- Rasool, S.; Skinner, B.W. Osilodrostat for the treatment of Cushing’s disease. Expert Opin. Pharmacother. 2021, 22, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Pivonello, R.; Fleseriu, M.; Newell-Price, J.; Bertagna, X.; Findling, J.; Shimatsu, A.; Gu, F.; Auchus, R.; Leelawattana, R.; Lee, E.J.; et al. Efficacy and safety of osilodrostat in patients with Cushing’s disease (LINC 3): A multicentre phase III study with a double-blind, randomised withdrawal phase. Lancet Diabetes Endocrinol. 2020, 8, 748–761. [Google Scholar] [CrossRef]
- Castinetti, F.; Amodru, V.; Brue, T. Osilodrostat in Cushing’s disease: The risk of delayed adrenal insufficiency should be carefully monitored. Clin. Endocrinol. 2021. [Google Scholar] [CrossRef] [PubMed]
- Castinetti, F.; Fassnacht, M.; Johanssen, S.; Terzolo, M.; Bouchard, P.; Chanson, P.; Cao, C.D.; Morange, I.; Pico, A.; Ouzounian, S.; et al. Merits and pitfalls of mifepristone in Cushing’s syndrome. Eur. J. Endocrinol. 2009, 160, 1003–1010. [Google Scholar] [CrossRef] [PubMed]
- Bertagna, X.; Bertagna, C.; Luton, J.-P.; Husson, J.-M.; Girard, F. The New Steroid Analog RU 486 Inhibits Glucocorticoid Action in Man. J. Clin. Endocrinol. Metab. 1984, 59, 25–28. [Google Scholar] [CrossRef]
- Pivonello, R.; de Leo, M.; Cozzolino, A.; Colao, A. The Treatment of Cushing’s Disease. Endocr. Rev. 2015, 36, 385–486. [Google Scholar] [CrossRef] [PubMed]
- Fleseriu, M.; Biller, B.M.K.; Findling, J.W.; Molitch, M.E.; Schteingart, D.E.; Gross, C.; Auchus, R.; Bailey, T.; Carroll, T.; Colleran, K.; et al. Mifepristone, a Glucocorticoid Receptor Antagonist, Produces Clinical and Metabolic Benefits in Patients with Cushing’s Syndrome. J. Clin. Endocrinol. Metab. 2012, 97, 2039–2049. [Google Scholar] [CrossRef] [PubMed]
- Fein, H.G.; Vaughan, T.B.; Kushner, H.; Cram, D.; Nguyen, D. Sustained weight loss in patients treated with mifepristone for Cushing’s syndrome: A follow-up analysis of the SEISMIC study and long-term extension. BMC Endocr. Disord. 2015, 15, 63. [Google Scholar] [CrossRef] [PubMed]
- Debono, M.; Chadarevian, R.; Eastell, R.; Ross, R.J.; Newell-Price, J. Mifepristone Reduces Insulin Resistance in Patient Volunteers with Adrenal Incidentalomas That Secrete Low Levels of Cortisol: A Pilot Study. PLoS ONE 2013, 8, e60984. [Google Scholar] [CrossRef]
- Belokovskaya, R.; Ravikumar, A.; Arumugam, D.; Izadmehr, S.; Goddard, G.M.; Geer, E.B.; Levine, A.C. Mifepristone Treatment for Mild Autonomous Cortisol Secretion Due to Adrenal Adenomas: A Pilot Study. Endocr. Pract. 2019, 25, 846–853. [Google Scholar] [CrossRef]
- Cohan, P.; East, H.E.; Galati, S.-J.; Mercado, J.U.; Lim, P.J.; Lamerson, M.; Smith, J.J.; Peters, A.L.; Yuen, K.C.J. Mifepristone Treatment in Four Cases of Primary Bilateral Macronodular Adrenal Hyperplasia (BMAH). J. Clin. Endocrinol. Metab. 2019, 104, 6279–6290. [Google Scholar] [CrossRef] [PubMed]
- Pivonello, R.; Bancos, I.; Feelders, R.A.; Kargi, A.Y.; Kerr, J.M.; Gordon, M.B.; Mariash, C.N.; Terzolo, M.; Ellison, N.; Moraitis, A.G. Relacorilant, a Selective Glucocorticoid Receptor Modulator, Induces Clinical Improvements in Patients with Cushing Syndrome: Results from A Prospective, Open-Label Phase 2 Study. Front. Endocrinol. 2021, 12, 1. [Google Scholar] [CrossRef] [PubMed]
- Diederich, S.; Grossmann, C.; Hanke, B.; Quinkler, M.; Herrmann, M.; Bähr, V.; Oelkers, W. In the search for specific inhibitors of human 11b-hydroxysteroid-dehydrogenases (11b-HSDs): Chenodeoxycholic acid selectively inhibits 11b-HSD-I. Eur. J. Endocrinol. 2020, 142, 200–207. [Google Scholar]
- Rosenstock, J.; Banarer, S.; Fonseca, V.A.; Inzucchi, S.E.; Sun, W.; Yao, W.; Hollis, G.; Flores, R.; Levy, R.; Williams, W.V.; et al. The 11- -Hydroxysteroid Dehydrogenase Type 1 Inhibitor INCB13739 Improves Hyperglycemia in Patients with Type 2 Diabetes Inadequately Controlled by Metformin Monotherapy. Diabetes Care 2010, 33, 1516–1522. [Google Scholar] [CrossRef] [PubMed]
| Drug Name | Mechanism of Action | Usual Dose Range in CS and Indication | Possible Schedule in mHC | Main Adverse Events in CS Patients (%) | Data on Possible Use in mHC |
|---|---|---|---|---|---|
| Pasireotide | SS receptor agonist - corticotrophs inhibition |
| Never tested |
| No data available in mHC Hypothetical use in pituitary mHC in the absence of diabetes |
| Pasireotide LAR | SS receptor agonist - corticotrophs inhibition |
| Never tested |
| No data available in mHC Hypothetical use in pituitary mHC in the absence of diabetes |
| Cabergoline | DA receptors
|
| Never tested |
| No data available in mHC The effect more likely in patients with less severe hypercortisolism |
| Metyrapone | Steroidogenesis inhibitor
|
| 250–500 mg bid (late afternoon and evening) |
| Correction of the abnormal circadian rhythm of cortisol if given in the late afternoon and evening Presurgery short-term |
| Ketoconazole | Steroidogenesis inhibitor
|
| 200–400 mg/day |
| Case report showing cortisol secretion normalization and blood pressure amelioration with low dose (200–400 mg/day) |
| Levoketoconazole | Steroidogenesis inhibitor
|
| Never tested |
| No data available in mHC In patients with type 2 diabetes mellitus without hypercortisolism amelioration of glycometabolic control, lipid levels, body weight and blood pressure |
| Osilodrostat | Steroidogenesis inhibitor
|
| Never tested |
| No data available in mHC |
| Mifepristone | Non selective GC receptor antagonist |
| 200–400 mg |
| Three studies with amelioration of insulin resistance, hypertension, QoL and cardiometabolic parameters, with good tolerability |
| Relacorilant | Selective GC receptor antagonist |
| Never tested |
| A phase III, randomized, double-blind, placebo-controlled study (NCT04308590) ongoing |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Favero, V.; Cremaschi, A.; Falchetti, A.; Gaudio, A.; Gennari, L.; Scillitani, A.; Vescini, F.; Morelli, V.; Aresta, C.; Chiodini, I. Management and Medical Therapy of Mild Hypercortisolism. Int. J. Mol. Sci. 2021, 22, 11521. https://doi.org/10.3390/ijms222111521
Favero V, Cremaschi A, Falchetti A, Gaudio A, Gennari L, Scillitani A, Vescini F, Morelli V, Aresta C, Chiodini I. Management and Medical Therapy of Mild Hypercortisolism. International Journal of Molecular Sciences. 2021; 22(21):11521. https://doi.org/10.3390/ijms222111521
Chicago/Turabian StyleFavero, Vittoria, Arianna Cremaschi, Alberto Falchetti, Agostino Gaudio, Luigi Gennari, Alfredo Scillitani, Fabio Vescini, Valentina Morelli, Carmen Aresta, and Iacopo Chiodini. 2021. "Management and Medical Therapy of Mild Hypercortisolism" International Journal of Molecular Sciences 22, no. 21: 11521. https://doi.org/10.3390/ijms222111521
APA StyleFavero, V., Cremaschi, A., Falchetti, A., Gaudio, A., Gennari, L., Scillitani, A., Vescini, F., Morelli, V., Aresta, C., & Chiodini, I. (2021). Management and Medical Therapy of Mild Hypercortisolism. International Journal of Molecular Sciences, 22(21), 11521. https://doi.org/10.3390/ijms222111521











