Abstract
Polyorchidism is a rare male urogenital tract anomaly characterized by at least one supernumerary testis in the scrotum or ectopically. According to data based on our systematic review, 76% of the supernumerary testes (SNTs) were located in the scrotum, and 24% were extra-scrotal (p < 0.001). Among testes located outside the scrotum, 87% were found in the inguinal canal and 13% in the abdominal cavity. In 80% of cases, the diagnosis of SNT was made based on imaging tests, and the remaining 20% of cases were detected incidentally during surgery. The imaging tests performed (US or MRI) resulted in a significantly higher rate of patients who qualified for observation vs. surgical treatment (45% vs. 35%, p < 0.001). The most common conditions associated with SNT were ipsilateral inguinal hernia (15% of cases) and cryptorchidism (15% of cases). Surgery (orchidopexy/orchidectomy) was performed on 54% of patients with SNT, and the decision to observe the SNT was made in a total of 46% of patients (p = 0.001). The therapeutic approach depends on the location of the SNT and the presence of factors that raise suspicion of neoplastic proliferation.
1. Introduction
Polyorchidism is a rare male urogenital tract anomaly characterized by at least one supernumerary testis (SNT) situated in the scrotum or ectopically. Despite the awareness of this defect for more than 120 years [], there is still a lack of consensus between clinicians regarding the management of this condition. So far, robust data that could help create an algorithm for clinical decision support while detecting polyorchidism is still lacking. The cases described to date confirm the problematic nature of the anomaly both in terms of diagnosis (various locations of SNT and difficult differential diagnosis, e.g., problems with distinguishing it from tumor masses) and therapy (surgical intervention versus observation).
Embryologically, polyorchidism can result from an accidental division of the germinal ridge before eight weeks of gestation. Different levels at which the transverse genital ridge division may occur reflect the diverse types of the supernumerary testes, taking into account that the different variants are characterized by the presence or absence of extra vas deferens and epididymis [].
In the present analysis, the polyorchidism classification proposed by Bergholz et al. [] was applied, and bilobed testis cases (incomplete polyorchidism) were treated as a separate type of SNT. Based on the classification of Bergholz et al. [], a testis drained by a deferent duct is known as type A, while all other cases are referred to as type B. Type A testes can be further divided into subgroups according to the attached structures as follows: A1, the drained SNT has its own epididymis and vas deferens; A2, the drained SNT can have its own epididymis, but shares a common deferent duct with its neighbor (i.e., the properly developed ipsilateral testis); and A3, the drained SNT can share a common epididymis (and duct) with its neighbor. Type B testes can also be divided into subgroups according to the attached epididymis as follows: B1, the undrained SNT has its own epididymis; B2, the undrained SNT does not have its own epididymis and consists only of testicular tissue.
This review aims to analyze and evaluate the applied diagnostic and therapeutic interventions for cases of polyorchidism described in the last two decades. The available literature needs an up-to-date systematic analysis of polyorchidism cases to propose an algorithm for managing this rare defect.
2. Materials and Methods
2.1. Search Strategy
A systematic literature search was conducted by two authors independently, using major electronic medical databases (Science Direct, Web of Science, and PubMed) up to August 2021, for articles that could potentially be used in this systematic review. The search strategy used in this study included the following terms: “polyorchidism” and “supernumerary testis”.
The number of records found in the PubMed database for polyorchidism/SNT for the years 1931–2021 was 231. After initially examining the publications, it was decided to narrow the time frame of the literature search to the last two decades. Therefore, the publication period included the past 22 years (2000–2021). The primary reason for this is the lack of data in early publications was due to the inability to perform high-quality ultrasound (US) scanning and magnetic resonance imaging (MRI). Following acquisition of the full texts, a reference search was carried out to identify other potentially eligible articles that could have been missed in the electronic database search. The Preferred Reporting Items for Systematic Reviews and Meta-analyses [PRISMA] guidelines were followed while conducting this study [] (Figure 1).
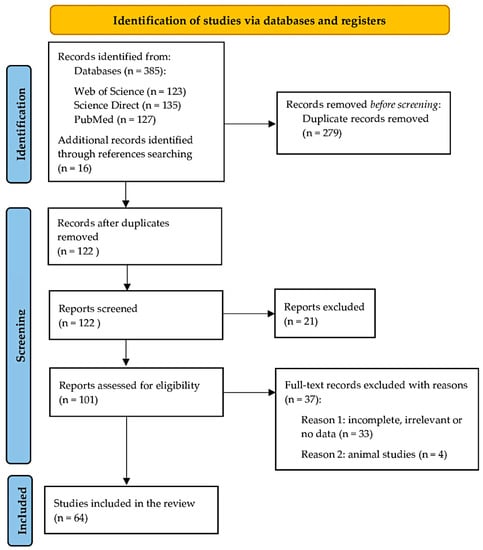
Figure 1.
The PRISMA flow diagram.
2.2. Eligibility Assessment
Study selection and data extraction were divided between two authors to allow for an independent double-check of articles and data. We applied the following exclusion criteria:
- Review articles and conference abstracts;
- Incomplete or impossible to extract data;
- Or research performed on animals.
Since there were many studies that involved patients with concomitant pathologies (i.e., inguinal hernia, cryptorchidism, hydrocele, testicular tumor, testicular torsion, male infertility), it was decided that articles reporting the presence of the SNT during such interventions will be included in this systematic review.
Help from medical professionals who were fluent in both English and the language of the publication was sought in times when the authors lacked fluency in the latter. Any inconsistencies within the included works were solved by contacting the authors of the original studies. Whenever the information could not be obtained, all reviewers participated in the assessment until a consensus was reached.
2.3. Data Extraction
Data extraction of all studies that met the inclusion criteria for this systematic review was carried out by two reviewers individually. Data on the modality of the studies, sample size, and anatomical variants of the SNT were obtained. The authors of the original studies were contacted for clarification or additional information whenever any discrepancy was found in the reported research.
2.4. Study Endpoints
The analysis paid particular attention to the type of SNT according to the Bergholz et al. classification (details of classification in the Introduction) [], the location of the SNT (scrotal or ectopic), and the presence of more than one SNT. The secondary endpoint addressed the relationship between the presence of SNT and comorbidities (cryptorchidism, hernia, testicular torsion, hydrocele, testicular tumors) and the use of imaging studies in differential diagnosis. The tertiary endpoint was the evaluation of the treatment used for the diagnosis of SNT (surgery versus observation) and the type of surgery (orchidopexy versus orchiectomy).
2.5. Quality Assessment
The AQUA tool was used to estimate the quality and reliability of the included studies. Five domains were evaluated in the analysis: Objective(s) and Subject Characteristics, Study Design, Methodology Characterization, Descriptive Anatomy, and Reporting of Results. Each domain was evaluated as having a “Low”, “High”, or “Unclear” risk of bias [].
2.6. Statistical Analysis
The Chi2 test and regression analysis (linear and quadratic) were used to analyze the synthesized data in this study. The data for the model were selected based on the experience of the researchers. The R Studio program was used to calculate the results (RStudio Team (2020), Integrated Development for R. RStudio, PBC, Boston, MA URL http://www.rstudio.com/, 1 August 2022). Statistical significance was set with a p-value < 0.05. Since the obtained data came from case reports or case series, meta-analytical evaluation was not performed.
3. Results
3.1. Study Identification
The study identification process is summarized in Figure 1. In the preliminary search, 385 articles were found in the preliminary search that could meet the inclusion criteria. Further, 16 studies were identified during the reference search. A total of 279 studies were duplicates which were excluded. After the initial screening of abstracts and titles, 21 records were considered ineligible: the majority were reviews or reported irrelevant data. One hundred and one articles were subject to full-text analysis, and finally, 64 studies were included in this systematic review.
3.2. Characteristics of the Included Studies
The characteristics of the included studies are summarized in Table 1. Sixty-four patients were evaluated in this systematic review. The research included in this study had a published date range of 2000–2021. After initially examining the publications, the decision was made to narrow the time frame of the literature search to the last two decades. The primary reason for this is the lack of data in early publications due to the inability to perform high-quality ultrasound (US) scanning and magnetic resonance imaging (MRI). The scope of searched literature was worldwide. Since not all patients had both US and MRI imaging studies performed, individual cases were selectively chosen for analysis.

Table 1.
Characteristics of the included studies. SNT—supernumerary testis; US—ultrasound; MRI—magnetic resonance imaging; S—scrotum; E—ectopic; R—right; L—left; Y—yes; N—no.
3.3. Quality Assessment
The AQUA tool evaluation is summarized in Table 2. Overall, the vast majority of studies were evaluated as having a “High” risk of bias in Objective(s) and Subject Characteristics and Methodology Characterization due to the lack of complete information on the baseline characteristics and demographics of the patients, as well as the specialty and experience of the scientists in charge of a particular part of the study. Domains: Study Design and Reporting of Results were evaluated as having a “Low” risk of bias for all included studies.

Table 2.
The risk of bias analysis based on the AQUA tool evaluation.
3.4. Prevalence of Polyorchidism and Localization of the SNT
About 76% of the SNTs were located in the scrotum, and 24% were extra-scrotal; (p < 0.001). Among testes located outside the scrotum, 87% were found in the inguinal canal and 13% in the abdominal cavity. In 65% of the cases, SNT occurred on the left side (p < 0.001).
3.5. Types of Polyorchidism
According to the classification by Bergholz et al., the most common subtype of SNT was type A2 (38%), followed by type A1 (26%) and type A3 (16%). Type B accounted for 10% of SNTs (B1-6%, B2-4%), and bilobed testes accounted for 10% of all SNTs.
3.6. Radiological Examinations of the SNT
In 80% of cases, the diagnosis of SNT was made based on radiological examinations, and the remaining 20% of cases were detected incidentally during surgery. The radiological examinations such as US and/or MRI resulted in a significantly higher rate of patients qualifying for observation vs. surgical treatment (45% vs. 35%, p < 0.001). The US examinations helped qualify STN patients for observation vs. surgical treatment (in 45% vs. 33%, p < 0.001; Table 3). MRIs also allowed SNT patients to qualify for observation vs. surgical treatment (in 33% vs. 13%, p < 0.001; Table 4).

Table 3.
Management of supernumerary testis in a group of patients with ultrasound performed in the course of diagnosis.

Table 4.
Management of supernumerary testis in a group of patients with magnetic resonance imaging of the scrotum/abdomen performed in the course of diagnosis.
3.7. Conditions and Symptoms Associated with Polyorchidism
The most common conditions associated with SNT were ipsilateral inguinal hernia (15% of cases) and cryptorchidism (15% of cases). Testis hydrocele was found in 7% of the cases, and testicular torsion in 7%. In 4% of the cases, cancer was diagnosed in the SNT (seminoma and intratubular germ cell neoplasia (IGCN). 31% of patients with SNT reported scrotal pain. 35% of patients were diagnosed with SNT incidentally during examinations for unrelated conditions (inguinal hernia, hydrocele, testicular torsion). Among the 65 SNT cases analyzed, only nine patients underwent semen analysis (in this group, five patients had semen analysis abnormalities-low sperm concentration, abnormal sperm morphology, and decreased sperm motility).
3.8. Size of the SNT
The mean size in the long axis of the SNT was 19.9 mm (SD ± 7.47 mm). The analysis included 42 surveyed observations; the remaining reports selected for analysis did not have data on the dimensions of the SNT. Quadratic regression analysis showed a significant prediction (F [2, 39] = 4.07; p < 0.05). Analysis of the R-squared coefficient values showed that the regression model of the included independent variables (age, age-squared) explained about 17% (13% after correction) of the variation in SNT length (Table 5). The correlation coefficients were R2 = 0.17 and adj. R2 = 0.13, respectively. These coefficients indicate that the quadratic model provides a better explanation of the variation in SNT length in the long axis (Figure 2). The number of significant predictors in the model was 2. The analysis showed that the mean level of the SNT length variable was 8.11 mm.

Table 5.
Linear and quadratic influence of age on the level of variable results—the supernumerary testis length. B = non-standardized regression coefficient; s.e. = standard error for B; p = statistical significance.
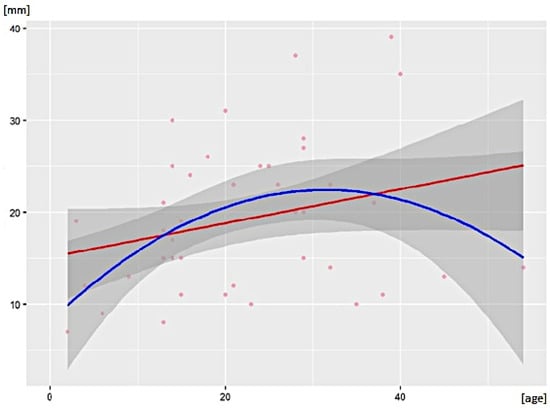
Figure 2.
Linear (red curve) and quadratic (blue curve) effects of age on the score level of the variable “supernumerary testis length [mm]”.
3.9. Type of Treatment
Surgery (orchidopexy/orchidectomy) was performed on 54% of patients with SNT, and the decision to observe the SNT was made in 46% of patients (p = 0.001). For the group of patients with SNT in the scrotum, 59% were referred to observation, while 41% underwent surgical intervention (p = 0.001). In the group of patients with ectopic SNT, 92% underwent surgery, and 8% were qualified for observation (p = 0.001).
Among the patients who underwent surgery, 45% underwent orchidopexy, while 55% underwent orchidectomy. In cases with SNT located in the scrotum, orchidopexy was performed in 59% of patients, while orchidectomy was performed in 41% of patients (p = 0.071; Table 6). In the ectopic SNT group, 75% had orchidectomy, and 25% underwent orchidopexy (p = 0.071; Table 6).

Table 6.
Surgical interventions for supernumerary testis depending on the location.
3.10. Tetraorchidism and Pentaorchidism
There were nine cases of tetraorchidism (2 SNTs) and two cases of pentaorchidism (3 SNTs) in the study group. In eight patients, the SNTs were located in the scrotum (89%). The most common types of tetraorchidism were A2, A3, and B2 based on the Bergholz et al. classification (25% of each type), and seven patients had bilateral SNTs. Tetraorchidism was histologically confirmed in 44% of patients, while all patients underwent the US, and 56% of them underwent MRI. Among the tetra/pentaorchidism cases, no neoplasms were found; 22% of patients were diagnosed with cryptorchidism, 11% with hydrocele, and 33% with testicular torsion. One-third of those cases were detected incidentally, and 44% of patients reported scrotal pain. 56% of patients with tetraorchidism qualified for observation, 22% underwent orchidopexy, and 22% underwent orchidectomy.
4. Discussion
Polyorchidism is a very rare developmental anomaly of the male reproductive system. The knowledge of embryology, clinical manifestations, and diagnostic and therapeutic pathways for SNT is based on single case reports and one meta-analysis published in 2009 []. The current analysis aimed to update the knowledge on polyorchidism—considering contemporary medical imaging methods—and attempts to create a diagnostic and therapeutic consensus in detecting an isoechoic/isodense tissue mass located in the scrotum or ectopically. 80% of all SNT cases were testes that had developed a deferent duct (separate or shared with the ipsilateral testis, depending on the type), and 76% were located in the scrotum. Considering a supernumerary testis’s 50–65% reproductive potential [,], this makes a compelling case for testicular preservation.
The etiology of SNT still needs to be fully understood. Articles published to date point to a transverse division of the genital ridge before the eighth week of gestation as the most likely theory for the formation of SNTs [,,,]. The different levels at which the transverse genital ridge division may occur reflect the diverse types of SNTs, bearing in mind that the presence or absence of an extra ductus deferens and epididymis can characterize individual variants. A distinct and extremely rare form of polyorchidism is the bilobed testis, which most likely results from an incomplete division of the germinal ridge [,,]. This variant accounted for 10% of all SNT cases in the present analysis.
Polyorchidism cases are typically detected incidentally in men presenting with comorbid conditions or in patients concerned with discovering an extra mass in the scrotum. The most common comorbidities included ipsilateral inguinal hernia and cryptorchidism. Despite a lack of clinical manifestation in many cases, one-third of SNT patients reported scrotal pain. In young SNT patients with associated pain, testicular torsion should always be considered in the differential diagnosis. The risk of testicular torsion in the general population is 0.025% [], while for cryptorchidism, it is 0.25% []. In the current analysis, 7% of patients with SNT were diagnosed with torsion (a 280-fold higher absolute risk compared to the general population). Bergholz et al. [] reported that up to 15% of SNT patients are diagnosed with torsion of one of the testes on the ipsilateral side.
Polyorchidism is associated with an increased risk of testicular cancer. Given that the estimated risk of testicular cancer in the general population is 0.006% [], the existence of SNT increases this risk. In our study, the prevalence of testicular malignancy was 4%, while Bergholz et al. [] reported a rate of 5.7%. An additional factor that increases this risk is an ectopic SNT (cryptorchidism increases the risk of testicular cancer by 2.2 to 4.7 compared to the general population [,]). Due to the relatively low incidence of cancers associated with SNT, it is not easy to assess which histological types are the most common. For the cases included in our analysis, histopathological examinations revealed seminoma and intratubular germ cell neoplasia (IGCN) [,]. Bergholz et al. [] also reported choriocarcinoma, teratoma, and embryonal carcinoma cases.
Modern imaging radiological techniques for identifying paratesticular masses include high-resolution US and MRI. Today, owing to their widespread availability, high sensitivity, and specificity, these methods should be the examinations of the first choice for the differential diagnosis of paratesticular masses. In our analysis, in patients diagnosed between 2000 and 2021, up to 80% had a US, and 50% had an MRI (in a previous analysis, only 27% of patients had a US or an MRI [], which, for obvious reasons, was due to the limited availability of the equipment and the poorer quality of equipment at the time). An alternative to MRI for diagnosing a scrotal mass may be a contrast-enhanced ultrasound (CEUS), performed after intravenous administration of ultrasound contrast agents consisting of microbubbles. CEUS is a safe method well tolerated by patients. This technique has been used to evaluate scrotal lesions and produces a better visualization of vascularity than the color Doppler technique (it can detect microvessels as small as 2–7 µm) [].
The primary purpose of radiological diagnostic techniques imaging when suspecting an SNT is to rule out neoplastic lesions and reduce surgical intervention rates when the SNT is structurally normal. To the best of our knowledge, the current study is the first to have statistically evaluated the effects of radiological techniques during the diagnostic procedures for the SNT. Radiological techniques such as US and/or MRI resulted in significantly more patients being qualified for observation versus surgical intervention (45% vs. 35%). When considering only the group of patients with an SNT diagnosed using MRI, up to 72% were qualified for observation. According to the European Society of Urogenital Radiology (ESRU), MRI imaging of normal adult testes shows T2 hyper- and T1 hypo-to-isointense, homogenous oval structures with diffusion restriction, surrounded by T2/T1 hypointense tunica albuginea. The signal intensity of an SNT is almost identical to that of an anatomically normal testis [].
Moreover, the imaging examinations allowed for an analysis of the size of SNTs. The current study used a mathematical model that demonstrated that the size of the SNT depends on the patient’s age and is subject to the same variability observed for anatomically normal testes [,]. The length of the SNT, measured in the long axis, increases with the development of the body until about 25 years of age and, subsequently, undergoes a gradual involution, which is observed in older males (Figure 2).
The management of polyorchidism has evolved over time and is still under debate. As polyorchidism is an extremely rare congenital abnormality, there are a few cases to facilitate evidence-based recommendations. Traditional management involves surgical removal of the SNT due to the increased risk of malignancy. Histological examination of surgically explored cases revealed functional parenchyma in 50–65% of SNTs []. Thus, patients with a scrotal SNT without radiological indications of malignancy may be recommended for conservative management and monitoring, with regular self-examination, clinical examinations by health professionals, and non-invasive imaging (US or MRI). In our study, 59% of patients with an SNT in the scrotum were qualified for observation, whereas, in the surgical intervention group, 59% had orchidopexy. These results indicate a testicular preservation trend in urology reflected by significantly more frequent qualification for observation or orchidopexy when an SNT is detected in the scrotum. A separate issue in the case of intent to preserve the SNT is the assessment of the presence of pathways releasing sperm count of the SNT. The differentiation of SNTs based on Bergholz et al.’s classification [] into type A or type B is possible with MRI or intraoperative observation. In polyorchidism with an extra-scrotal testis, especially in a young patient of reproductive age, orchidopexy is recommended if feasible, followed by observation. If an SNT is associated with any signs of malignancy, radical orchidectomy is recommended.
Here, we propose a therapeutic algorithm based on the current knowledge that can be used in everyday clinical practice (Figure 3). The resulting algorithm is particularly applicable to the diagnosis of triorchidism. Detecting two or more SNTs requires a personalized therapeutic approach for each case, depending on the location and the progression of the SNTs (tetraorchidism and pentaorchidism accounted for 13% and 3% of patients, respectively, in our study).
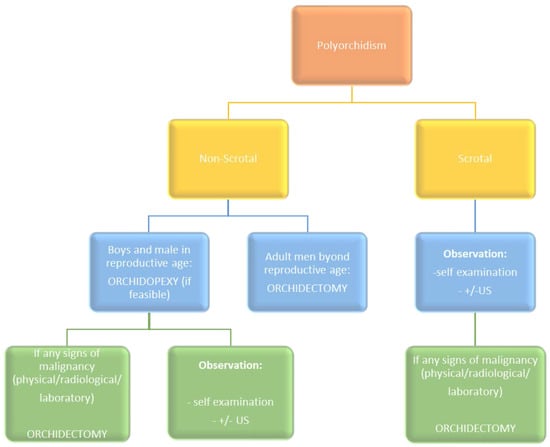
Figure 3.
Proposed therapeutic algorithm for polyorchidism. Adopted from Balawender et al. [] under Creative Commons Attribution-Non Commercial (unported, v3.0) License.
Limitations
Due to the casuistic nature of the issue, our systematic review is based on an analysis of case reports or case series; the lack of broader studies in previous publications did not allow us to conduct a meta-analysis. After analyzing the collected publications, the authors decided to apply the time criterion to the selection of the literature (publications from the period 2000–2021 were analyzed). The primary reason for this is the lack of data in early publications due to the inability to perform high-quality ultrasound (US) scanning and magnetic resonance imaging (MRI).
5. Conclusions
Polyorchidism is a rare anomaly of the male reproductive system; however, the differential diagnosis of paratesticular masses should always consider the possible presence of an SNT. Current results show a trend toward testicular preservation after SNT diagnoses. Contemporary diagnostic imaging should include a mandatory US and an MRI of the abdomen and scrotum. The therapeutic approach depends on the location of the SNT and the presence of factors that raise suspicion of neoplastic proliferation.
Author Contributions
Conceptualization, K.B.; methodology, K.B., M.Z., G.W. and A.W.; validation, K.B., G.W., M.Z., M.B., J.K. and M.G.; formal analysis, J.W., J.K., G.W., M.P. and A.S.; investigation, K.B., M.Z., G.W., J.W., A.Ż., M.B., A.D. and A.M.; data curation, K.B. and M.G.; writing—original draft preparation, K.B., M.Z., G.W., E.C., J.K. and M.G.; writing—review and editing, K.B., M.Z., J.W., A.W., J.K., M.B., M.G., A.S., A.M., A.D., E.C. and A.S.; supervision, G.W., J.W., M.P., J.K. and A.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All the data is available within the study. This process can be initiated upon request to the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Uğuz, S.; Gürağaç, A.; Demirer, Z.; Yilmaz, S.; Aydur, E. Bilateral polyorchidism with ipsilateral two undescended testes: A rare congenital anomaly. Andrologia 2017, 49, e12643. [Google Scholar] [CrossRef] [PubMed]
- Lawrentschuk, N.; MacGregor, R.J. Polyorchidism: A case report and review of the literature. ANZ J. Surg. 2004, 74, 1130–1132. [Google Scholar] [CrossRef] [PubMed]
- Bergholz, R.; Wenke, K. Polyorchidism: A Meta-Analysis. J. Urol. 2009, 182, 2422–2427. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; Moher, D.; McKenzie, J.E. Introduction to preferred reporting items for systematic reviews and meta-analyses 2020 and implications for research synthesis methodologists. Res. Synth. Methods 2022, 13, 156–163. [Google Scholar] [CrossRef]
- Bergholz, R.; Koch, B.; Spieker, T.; Lohse, K. Polyorchidism: A case report and classification. J. Pediatr. Surg. 2007, 42, 1933–1935. [Google Scholar] [CrossRef]
- Henry, B.M.; Tomaszewski, K.A.; Walocha, J.A. Methods of Evidence-Based Anatomy: A guide to conducting systematic reviews and meta-analysis of anatomical studies. Ann. Anat. 2016, 205, 16–21. [Google Scholar] [CrossRef] [PubMed]
- Mandalia, U.; Pakdemirli, E. A case of triorchidism. Radiol. Case Rep. 2020, 15, 1643–1645. [Google Scholar] [CrossRef] [PubMed]
- Chowdhary, S. Case report of a rare variant of polyorchidism. J. Pediatr. Surg. Case Rep. 2016, 5, 30–31. [Google Scholar] [CrossRef]
- Alamsahebpour, A.; Hidas, G.; Kaplan, A.; McAleer, I.M. Bilateral Polyorchidism with Diffuse Microlithiasis: A Case Report of an Adolescent with 4 Testes. Urology 2013, 82, 1421–1423. [Google Scholar] [CrossRef]
- Ibrahim, H.; Roberts, M.J.; Hussey, D. Quadruple Orchidopexy for Torsion Testis in an Adolescent with Polyorchidism: A Case Report. Urology 2016, 87, 196–199. [Google Scholar] [CrossRef]
- Ojili, V.; Shanbhogue, K.P.; Doherty, G.P. An unusual case of polyorchidism with three homolateral testes and contralateral anorchia. Eur. J. Radiol. Extra 2009, 72, e129–e131. [Google Scholar] [CrossRef]
- Leodoro, B.; Beasley, S.; Stringer, M. Polyorchidism with presumed contralateral intrauterine testicular torsion. Int. J. Surg. Case Rep. 2014, 5, 865–867. [Google Scholar] [CrossRef]
- Haley, M.J.; Arkovitz, M.S. Polyorchidism in a child with imperforate anus. J. Pediatr. Surg. 2008, 43, 1548–1550. [Google Scholar] [CrossRef]
- Repetto, P.; Ceccarelli, P.; Bianchini, A.; Durante, V.; Biondini, D.; Cacciari, A. Three small testes in left hemiscrotum: A rarer caseof polyorchidism. J. Pediatr. Surg. 2010, 45, e21–e23. [Google Scholar] [CrossRef] [PubMed]
- Arslanoglu, A.; Tuncel, S.A.; Hamarat, M. Polyorchidism: Color Doppler ultrasonography and magnetic resonance imaging findings. Clin. Imaging 2013, 37, 189–191. [Google Scholar] [CrossRef]
- Méndez-Gallart, R.; Estevez-Martínez, E.; Rodríguez-Barca, P.; García-Palacios, M.; Bautista-Casasnovas, A. Incomplete unilateral polyorchidism (bilobed testicle) mimicking testicular tumour. J. Pediatr. Surg. 2012, 47, 2140–2142. [Google Scholar] [CrossRef] [PubMed]
- Sarma, S.K.; Ranjit, P. Polyorchidism: A rare congenital anomaly. Eur. J. Radiol. Extra 2008, 66, e29–e31. [Google Scholar] [CrossRef]
- Ozturk, E.; Mutlu, H.; Erdem, I.; Sildiroglu, H.O. Polyorchidism: Report of a case and review of the literature. Eur. J. Radiol. Extra 2006, 58, 93–95. [Google Scholar] [CrossRef]
- Ferro, F.; Iacobelli, B. Polyorchidism and torsion. A lesson from 2 cases. J. Pediatr. Surg. 2005, 40, 1662–1664. [Google Scholar] [CrossRef]
- Spranger, R.; Gunst, M.; Kühn, M. Polyorchidism: A strange anomaly with unsuspected properties. J. Urol. 2002, 168, 198. [Google Scholar] [CrossRef]
- Tigabie, W.; Belachew, D. Triorchidism: Unilateral double atrophic undescended testis in Tertiary Specialized Hospital, Ethiopia. J. Pediatr. Surg. Case Rep. 2020, 61, 101633. [Google Scholar] [CrossRef]
- Bayissa, B.B.; Tesfaye, D. Triorchidism; an incidental finding at inguinal hernia repair: A case report. Int. J. Surg. Case Rep. 2020, 77, 813–815. [Google Scholar] [CrossRef] [PubMed]
- Cohen, T.; Agard, H.; Parekh, N.; Clark, C. Management of Bilateral Undescended Bilobed Testes and Review of the Literature. Urology 2017, 110, 213–215. [Google Scholar] [CrossRef] [PubMed]
- Boussaffa, H.; Naouar, S.; Ati, N.; Amri, M.; Ben Khelifa, B.; Salem, B.; El Kamel, R. Neoplasm of a supernumerary undescended testis: A case report and review of the literature. Int. J. Surg. Case Rep. 2018, 53, 345–347. [Google Scholar] [CrossRef]
- Myers, A.; Morganstern, B.; Fine, R. A Unique Case of Pentaorchidism. Urology 2017, 104, 196–197. [Google Scholar] [CrossRef]
- Kumar, B.; Sharma, C.; Sinha, D. Supernumerary testis: A case report and review of literature. J. Pediatr. Surg. 2008, 43, E9–E10. [Google Scholar] [CrossRef] [PubMed]
- Abduljabbar, A.H. A Case Report: Triorchidism; is a Rare Mistaken Cause for Extra Testicular Neoplasm. Urol. Case Rep. 2015, 3, 89–91. [Google Scholar] [CrossRef]
- Aldughiman, A.W.; El-Tholoth, H.S.; Alsunbul, A.; Badawy, E.; Alelaiwai, A. Management of polyorchidism in a prepubertal boy: A case report and literature review. Urol. Ann. 2020, 12, 385–387. [Google Scholar] [CrossRef]
- Ojaghzadeh, D.; Mahmoudpour, M.; Ezzati, N.; Milani, A.A. Polyorchidism in ultrasound examination: A case report. Andrologia 2021, 53, e13832. [Google Scholar] [CrossRef]
- Zahirian, M.T.; Mohseni, R.H.; Zandian, H.; Hosseinkhani, A. Five testicles in the genital area of a thirteen-month-old baby: A case report. BMC Urol. 2020, 20, 128. [Google Scholar] [CrossRef]
- Fonseca-Sosa, F.K. Polyorchidism and inguinoscrotal hernia. Case presentation. Poliorquidismo y hernia inguinoescrotal. presentación de un caso. Arch Esp Urol. 2019, 72, 616–618. [Google Scholar]
- Nepal, S.P.; Nakasato, T.; Naoe, M.; Shimoyama, H.; Ogawa, Y.; Fuji, K.; Maeda, Y.; Morita, J.; Oshinomi, K.; Matsui, Y.; et al. Management of right-sided polyorchidism with torsion: A case report with literature review. Urol. Sci. 2019, 30, 191. [Google Scholar] [CrossRef]
- Özman, O.; Yener, S.; Selçuk, B.; Önal, B. Polyorchidism: A Case Report and Review of the Literature. J. Urol. Surg. 2018, 5, 211–213. [Google Scholar] [CrossRef]
- Kealey, J.; Yao, H.H.; Grummet, J. Acute scrotum-Torsion of the third testicle! Urol. Case Rep. 2018, 20, 92–93. [Google Scholar] [CrossRef] [PubMed]
- Lustig, D.B.; Martin, K.; Nasr, A. Management of supernumerary testis: A rare case of polyorchidism in a 2-year-old boy. Ann. Pediatr. Surg. 2017, 13, 225–227. [Google Scholar] [CrossRef]
- Gune, A.R.; Gune, R.P. Triorchidism: A rare case report. Afr. J. Urol. 2021, 27, 15. [Google Scholar] [CrossRef]
- Di Cosmo, G.; Silvestri, T.; Bucci, S.; Bertolotto, M.; Trombetta, C. A singular case of polyorchidism. Arch. Ital. di Urol. e Androl. 2016, 88, 333–334. [Google Scholar] [CrossRef]
- Bhandarwar, A.H.; Gandhi, S.S.; Patel, C.B.; Wagh, A.N.; Gawli, V.; Jain, N.A. Triorchidism: Presenting as Undescended Testis in a Case of Indirect Inguinal Hernia. Clin. Pr. 2016, 6, 786. [Google Scholar] [CrossRef]
- Rafailidis, V.; Arvaniti, M.; Rafailidis, D.; Sfoungaris, D. Multiparametric ultrasound findings in a patient with polyorchidism. Ultrasound 2017, 25, 177–181. [Google Scholar] [CrossRef]
- Balasar, M.; Sönmez, M.G.; Oltulu, P.; Kandemir, A.; Kılıç, M.; Göger, Y.E.; Pişkin, M.M. Polyorchidism; unilateral, one atrophic undescended double testicles. Urol. Ann. 2017, 9, 208–210. [Google Scholar] [CrossRef]
- Celik, O.; Budak, S.; Cakmak, O.; Tarhan, H.; Yalbuzdag, O.N.; Peker, A.; Ilbey, Y.O. Triorchidism: A rare genital abnormality. Asian J. Androl. 2014, 16, 923–924. [Google Scholar] [CrossRef] [PubMed]
- Nayak, S.P.; Sreejayan, M.P. Management of supernumerary testis in an adult: Case report and review. Andrologia 2011, 43, 149–152. [Google Scholar] [CrossRef]
- Arlen, A.M.; Holzman, S.A.; Weiss, A.D.; Garola, R.E.; Cerwinka, W.H. Functional supernumerary testis in a child with testicular torsion and review of polyorchidism. Pediatr. Surg. Int. 2014, 30, 565–568. [Google Scholar] [CrossRef] [PubMed]
- Jakhere, S.G.; Saifi, S.A.; Ranwaka, A.A. Supernumerary testis: Imaging appearance of a rare entity. Indian J. Urol. 2014, 30, 233–234. [Google Scholar] [CrossRef] [PubMed]
- Belba, A.; Riversi, V.; Mari, F.; Cellesi, E.; Ponchietti, R. Triorchidism: Genetic and imaging evaluation in an adult male. Arch. Ital. Urol. Androl. 2014, 86, 156–157. [Google Scholar] [CrossRef] [PubMed]
- Sağlam, H.S.; Önol, F.F.; Avcı, E.; Erguven, A. Report of a boy with polyorchidism and a review of current knowledge regarding this unusual anomaly. Turk. J. Urol. 2013, 39, 119–121. [Google Scholar] [CrossRef] [PubMed]
- Chintamani, J.; Nyapathy, V.; Chauhan, A.; Krishnamurthy, U. Supernumerary Testis. J. Radiol. Case Rep. 2009, 3, 29–32. [Google Scholar] [CrossRef]
- Hassan, A.; El-Mogy, S.; Mostafa, T. Triorchidism: A case report and review of similar conditions. Andrologia 2008, 40, 265–269. [Google Scholar] [CrossRef]
- Khedis, M.; Nohra, J.; Dierickx, L.; Walschaerts, M.; Soulié, M.; Thonneau, P.F.; Plante, P.; Huyghe, E. Polyorchidism: Presentation of 2 Cases, Review of the Literature and a New Management Strategy. Urol. Int. 2008, 80, 98–101. [Google Scholar] [CrossRef]
- Rajbabu, K.; Morel, J.; Thompson, P.; Sidhu, P.S. Multi-cystic (rete testis) supernumerary testis in polyorchidism with underlying microlithiasis: Ultrasound features. Australas. Radiol. 2007, 51, B56–B58. [Google Scholar] [CrossRef] [PubMed]
- Bhogal, R.H.; Palit, A.; Prasad, K.K. Conservative management of polyorchidism in a young man: A case report and review of literature. Pediatr. Surg. Int. 2007, 23, 689–691. [Google Scholar] [CrossRef] [PubMed]
- Nane, I.; Özkan, L.; Ander, H. Inguinal orchiectomy for the extra testis with suspected tumor in a polyorchidic patient: A case report. Int. Urol. Nephrol. 2007, 39, 557–559. [Google Scholar] [CrossRef] [PubMed]
- Deveci, S.; Aygün, C.; Agildere, A.M.; Ozkardes, H. Bilateral double by testis: Evaluation magnetic resonance imaging. Int. J. Urol. 2004, 11, 813–815. [Google Scholar] [CrossRef] [PubMed]
- Danrad, R.; Ashker, L.; Smith, W. Polyorchidism: Imaging may denote reproductive potential of accessory testicle. Pediatr. Radiol. 2004, 34, 492–494. [Google Scholar] [CrossRef]
- de Buys Roessingh, A.S.; El Ghoneimi, A.; Enezian, G.; Aigrain, Y. Triorchidism and testicular torsion in a child. J. Pediatr. Surg. 2003, 38, E13–E14. [Google Scholar] [CrossRef]
- Chung, T.-J.; Yao, W.-J. Sonographic features of polyorchidism. J. Clin. Ultrasound 2002, 30, 106–108. [Google Scholar] [CrossRef] [PubMed]
- Schafer, E.S. The Sonographic Appearance of Polyorchidism: A Multiple Case Report. J. Diagn. Med Sonogr. 2019, 35, 499–503. [Google Scholar] [CrossRef]
- Duymuş, M.; Menzilcioğlu, M.S.; Çetinçakmak, M.; Avcu, S. A Rare Case of Polyorchidism: Four Testes. Pol. J. Radiol. 2016, 81, 39–41. [Google Scholar] [CrossRef]
- Ghose, A.; Rodrigues, G.; Izawa, J. Two primary seminomas in a patient with polyorchidism. Can. Urol. Assoc. J. 2007, 1, 285–287. [Google Scholar] [CrossRef]
- Topsakal, K.; Ak, H.; Yumurtas, N. Polyorchidism with varicocele: A case report and review of literature. Andrologia 2012, 44, 829–832. [Google Scholar] [CrossRef]
- Balawender, K.; Wiatr, T.; Wawrzyniak, A.; Orkisz, S. Management of Incidental Finding of Triorchidism Diagnosed during Routine Hernia Repair. Res. Rep. Urol. 2021, ume 13, 127–131. [Google Scholar] [CrossRef]
- Nikolic, O.; Stankov, M.; Popov, M.; Dajko, S.T.; Golusin, Z. Supernumerary testicle presented as an extra scrotal lump. J. Ultrasound 2022, 25, 403–407. [Google Scholar] [CrossRef] [PubMed]
- Beiko, D.; MacNeily, A.E. Torsion of bilobed testis and biopsy-proven ipsilateral supernumerary testis in an adolescent. Can. Urol. Assoc. J. 2010, 4, E67–E70. [Google Scholar] [CrossRef] [PubMed]
- De Carli, C.; Guerra, L.; Leonard, M. Bilobed testicle in children: Diagnosis and management. Can. Urol. Assoc. J. 2009, 3, E87–E88. [Google Scholar] [CrossRef] [PubMed]
- Haffar, A.; Crigger, C.; Goldinger, M.; Jaffe, T. Two halves of a whole: Bilobed testis case report and implications in management of a rare condition. Urol. Case Rep. 2021, 38, 101737. [Google Scholar] [CrossRef]
- Halliday, L.J. Management of a bilobed testicle in a 12-year-old boy. J. Surg. Case Rep. 2013, 2013, rjt112. [Google Scholar] [CrossRef] [PubMed]
- Kajbafzadeh, A.-M.; Ghahestani, S.M.; Zamani, M.M.; Kajbafzadeh, M.; Kia, M.M. A Novel Approach in Eight Polyorchidism Cases: Vasoepidydimal or Epididymo-epididymal Approximation in Single Vas Deferens Duplicated Testis. Urology 2012, 79, 1346–1349. [Google Scholar] [CrossRef]
- Jackson, D.F.; Bronson, M.A.; Neff, W.G. Polyorchidism. J. Diagn. Med. Sonogr. 2005, 21, 413–419. [Google Scholar] [CrossRef]
- Lip, S.Z.L.; Murchison, L.E.D.; Cullis, P.; Govan, L.; Carachi, R. A meta-analysis of the risk of boys with isolated cryptorchidism developing testicular cancer in later life. Arch. Dis. Child. 2013, 98, 20–26. [Google Scholar] [CrossRef]
- Giwercman, A.; Grindsted, J.; Hansen, B.; Jensen, O.M.; Skakkebaek, N.E. Testicular Cancer Risk in Boys with Maldescended Testis: A Cohort Study. J. Urol. 1987, 138, 1214–1216. [Google Scholar] [CrossRef]
- Paniagua, R.; Martín, A.; Nistal, M.; Amat, P. Testicular involution in elderly men: Comparison of histologic quantitative studies with hormone patterns. Fertil. Steril. 1987, 47, 671–679. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).