Emerging Trends of Infectious Diseases in Canada
A special issue of Tropical Medicine and Infectious Disease (ISSN 2414-6366).
Deadline for manuscript submissions: closed (6 July 2025) | Viewed by 20301
Special Issue Editor
Interests: climate change; travel health; migrant health; surveillance; OneHealth; vaccine-preventable diseases; tuberculosis; vector-borne diseases; neglected tropical diseases
Special Issue Information
Dear Colleagues,
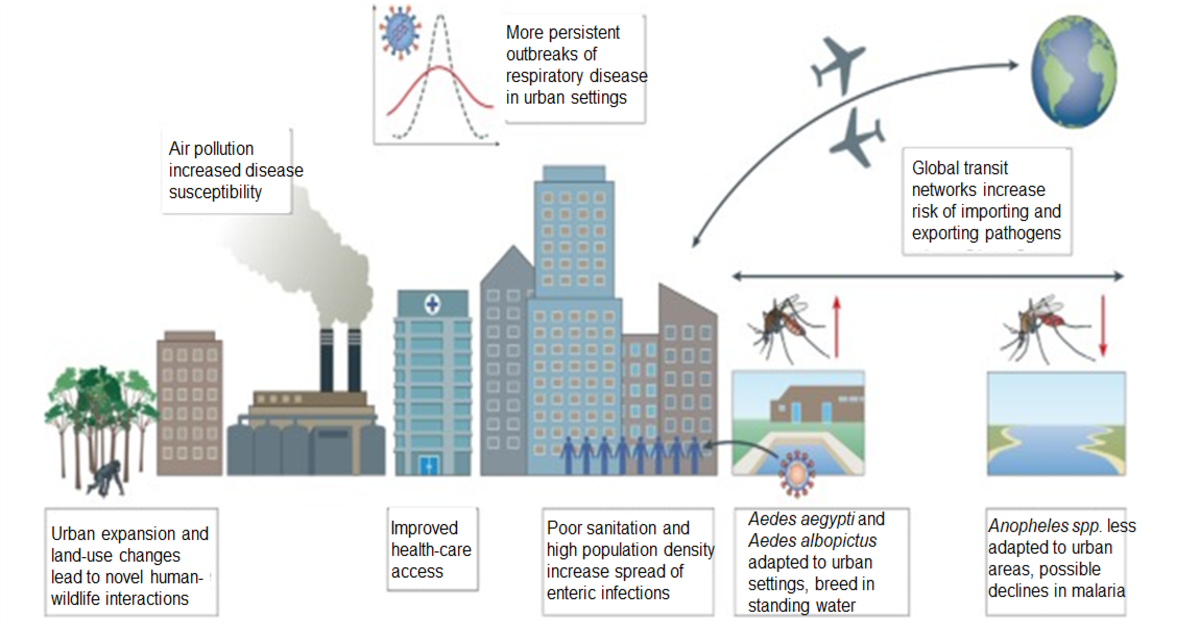
Emerging trends in infectious diseases in Canada reveal a dynamic landscape influenced by climate change, global travel, close interactions with livestock or wild animals, and increased antimicrobial resistance. Rising global temperatures and altered ecosystems have expanded the geographic range for key vector-borne diseases such as Lyme disease, tick-borne illnesses like anaplasmosis and babesiosis, and West Nile virus. Furthermore, urbanization and travel have complicated the overlapping interactions between humans, intermediate hosts (e.g., livestock and rodents), and insect/arthropod vectors.
The resurgence of vaccine-preventable diseases post pandemic, including measles and pertussis, underscores the critical role of immunization programs to manage downstream impacts of vaccine hesitancy. The COVID-19 pandemic highlighted the need for robust public health infrastructure and preparedness to manage novel pathogens. Genomic surveillance and advanced diagnostics are enhancing the ability to detect and respond to outbreaks more swiftly.
Additionally, the ongoing opioid crisis and disruptions to comprehensive healthcare have exacerbated the spread of bloodborne infections like HIV, hepatitis C, and tuberculosis among vulnerable populations. Moreover, Canada's multicultural population requires tailored public health strategies to address its diverse healthcare needs and disparities. Ongoing research, active surveillance, and interdisciplinary collaboration for clinical guidelines are essential to mitigate the impact of these emerging infectious diseases.
Dr. Yazdan Mirzanejad
Guest Editor
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the special issue website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 250 words) can be sent to the Editorial Office for assessment.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Tropical Medicine and Infectious Disease is an international peer-reviewed open access monthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2700 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- zoonoses
- climate change
- travel health
- migrant health
- surveillance
- CATMAT
- OneHealth
- vaccine-preventable diseases
- tuberculosis
- Lyme disease
- tick-borne diseases
- mosquito-borne diseases
- vector-borne diseases
- neglected tropical diseases
Benefits of Publishing in a Special Issue
- Ease of navigation: Grouping papers by topic helps scholars navigate broad scope journals more efficiently.
- Greater discoverability: Special Issues support the reach and impact of scientific research. Articles in Special Issues are more discoverable and cited more frequently.
- Expansion of research network: Special Issues facilitate connections among authors, fostering scientific collaborations.
- External promotion: Articles in Special Issues are often promoted through the journal's social media, increasing their visibility.
- Reprint: MDPI Books provides the opportunity to republish successful Special Issues in book format, both online and in print.
Further information on MDPI's Special Issue policies can be found here.






