Current Challenges in Heart Failure and Cardiac Transplantation
A topical collection in Journal of Cardiovascular Development and Disease (ISSN 2308-3425). This collection belongs to the section "Cardiac Surgery".
Viewed by 84045Editors
Interests: heart failure; heart transplantation; ventricular assist devices; pacemaker/ICD/CRT systems; arrhythmias; atrial fibrillation; cardiomyopathies
Special Issues, Collections and Topics in MDPI journals
Interests: heart failure; heart transplantation
Interests: pulmonary hypertension; heart failure; pulmonary embolism; hypertension
2. Department of Cardiology, Angiology and Pneumology, Heidelberg University Hospital, 69120 Heidelberg, Germany
Interests: heart failure; heart transplantation; ventricular assist devices; preventive cardiology; physical medicine and rehabilitation; sports cardiology
Topical Collection Information
Dear Colleagues,
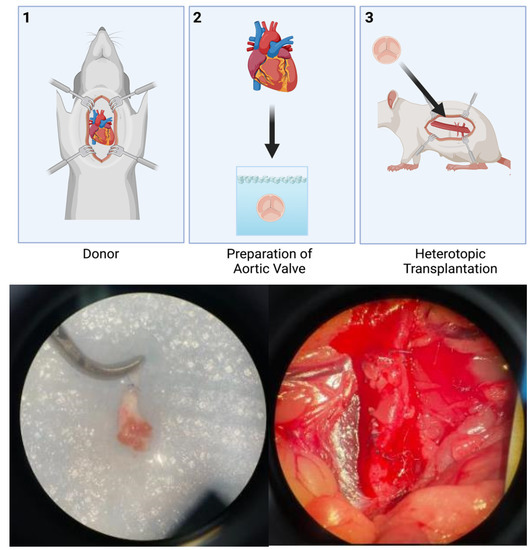
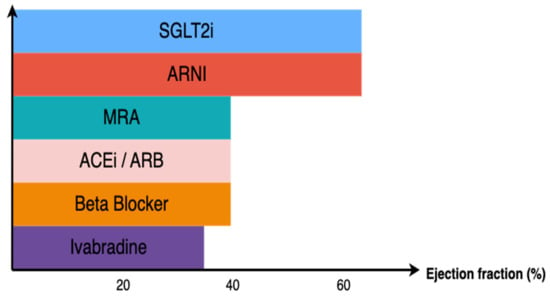
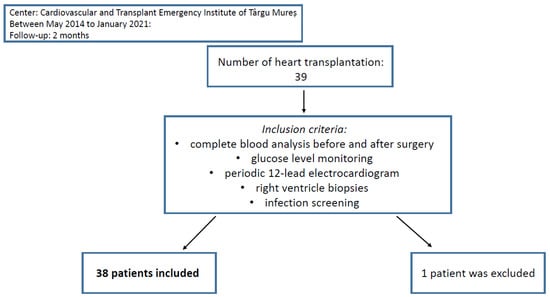
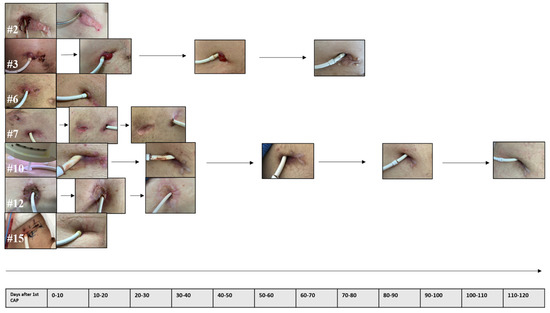
This Topical Collection will contain a selection of papers highlighting the current challenges in heart failure and cardiac transplantation. We welcome the submission of original research (basic research or clinical research), short communications, and review manuscripts focusing on the diagnosis, risk factors, treatment, and prognosis of as well as novel approaches to cardiac arrhythmias, cardiac pacemakers, cardiac resynchronization therapy, cardiomyopathies, congenital heart defects, heart failure, heart transplantation, implantable cardioverter-defibrillators, mechanical circulatory support, and ventricular assist devices.
Prof. Dr. Rasmus Rivinius
Dr. Daniel Oehler
Dr. Andreas J. Rieth
Prof. Dr. Andreas Doesch
Collection Editors
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 250 words) can be sent to the Editorial Office for assessment.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Journal of Cardiovascular Development and Disease is an international peer-reviewed open access monthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2700 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- cardiac arrhythmias
- cardiac pacemaker
- cardiac resynchronization therapy
- cardiomyopathies
- congenital heart defects
- heart failure
- heart transplantation
- implantable cardioverter-defibrillator
- mechanical circulatory support
- ventricular assist devices