1. Introduction
Foreign body ingestion is commonly seen in pediatric patients under five years of age [
1]. Since the early 2000s, the rising popularity and availability of neodymium magnets—rare earth magnets—have led to an increase in cases of magnet ingestion among children [
1]. If multiple high-power magnets are ingested, they can pose a significant morbidity due to their strong attractive forces [
2]. Many of these children require hospitalization, and approximately 10% have life threatening complications [
1]. These complications can include choking, bowel obstruction, tissue necrosis, perforation, fistula formation, or rarely even death [
2].
According to the latest NASPHGAN, North American Society for Pediatric Gastroenterology, Hepatology and Nutrition, the algorithm for magnet ingestion is relatively straightforward [
3]. If a magnet ingestion is symptomatic or multiple magnets are ingested, removal is recommended. If the magnet ingestion is asymptomatic, and multiple pieces are noted on x-ray, patients are typically admitted for observation with serial x-rays to confirm unobstructed passage. The following case illustrates how these guidelines inform clinical decision-making in the setting of a 2-year-old male with delayed recognition of multiple magnet ingestion from his sibling’s bracelet, requiring prompt intervention and multidisciplinary management.
2. Initial Evaluation
A 2-year-old male presented to the emergency department (ED) with persistent vomiting and abdominal discomfort following ingestion of multiple magnets from a sibling’s bracelet. His parents noted delayed recognition of the ingestion until symptoms escalated, with the admission taking place twenty-four hours post-ingestion. On examination, the patient was afebrile, with mild abdominal tenderness but no signs of peritonitis or hemodynamic instability.
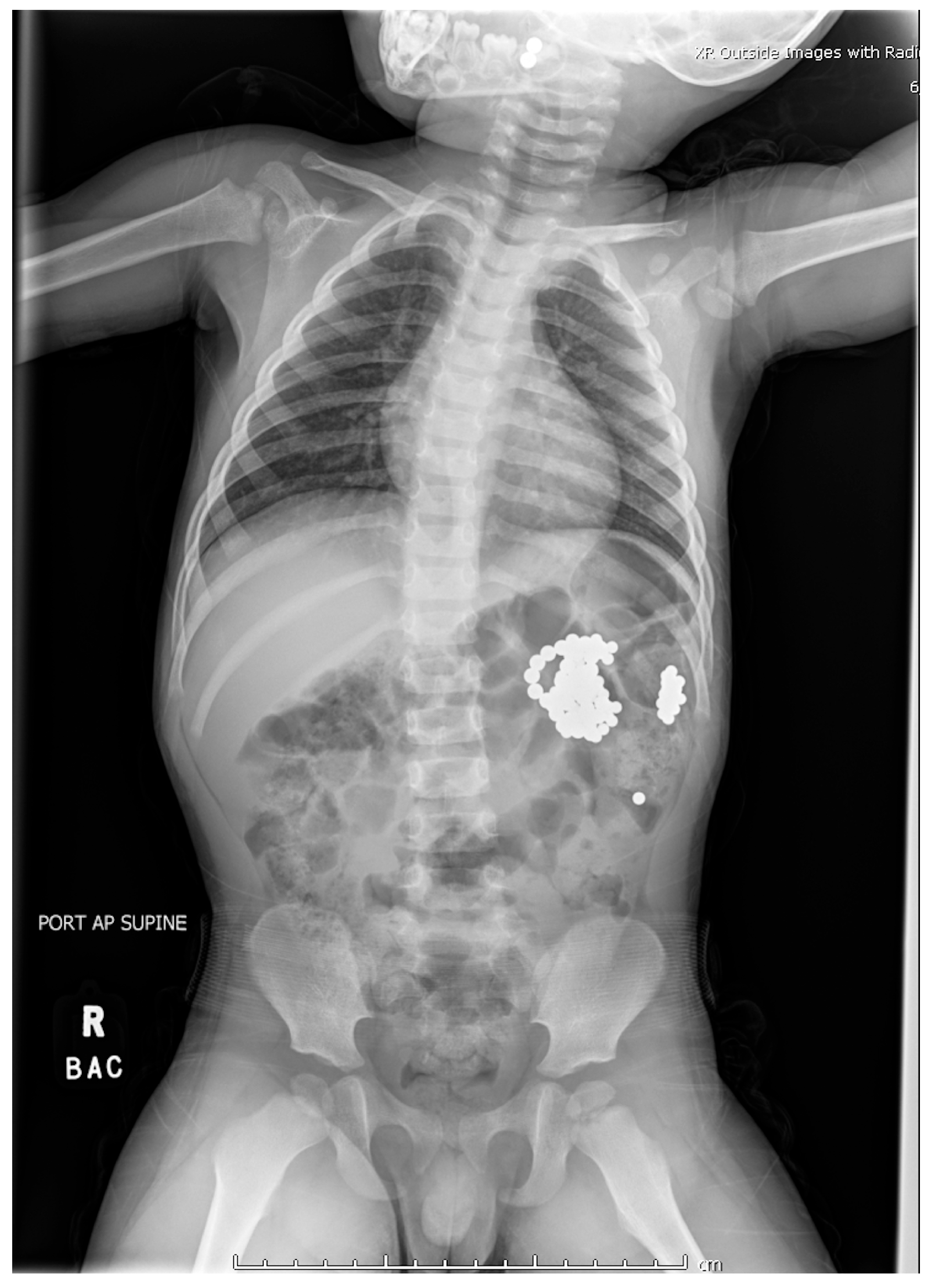
Plain radiographs demonstrated metallic densities clustered in the oropharynx, stomach, and small bowel (
Figure 1). Recognizing the risks of gastrointestinal perforation and necrosis, the ED team initiated immediate multidisciplinary consultations with otolaryngology, gastroenterology, and general surgery. Magnet ingestions have been increasingly reported in pediatric literature due to their accessibility and the unique risks they pose to gastrointestinal tissues [
4,
5,
6,
7,
8,
9,
10].
3. Intervention in the Hospital
Interventions occurred across multiple anesthetic settings. Otolaryngology performed direct laryngoscopy, successfully removing two magnets adhered to the uvula with minimal trauma, consistent with findings from previous studies [
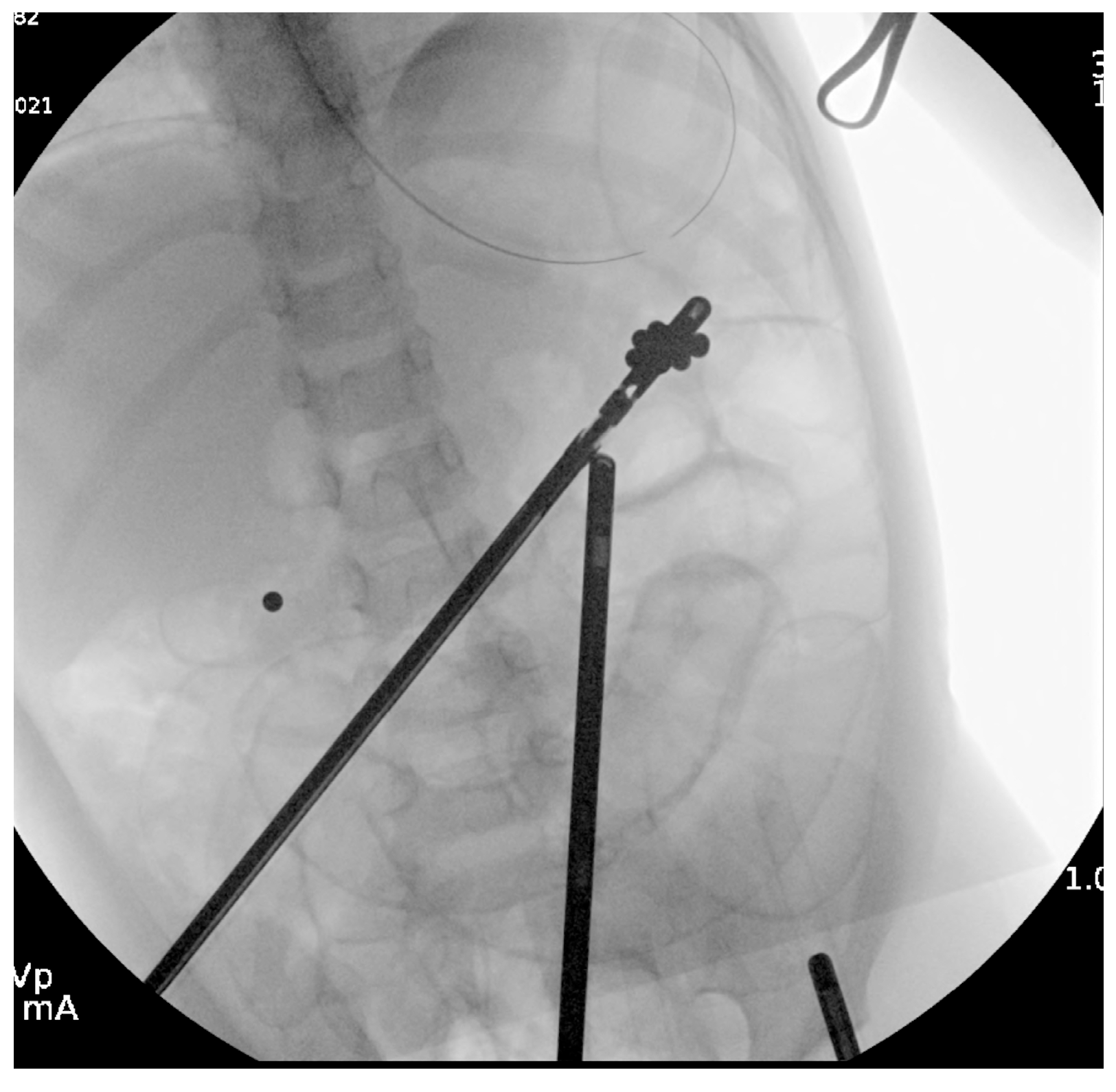
4]. Gastroenterology then conducted an upper endoscopy, revealing a tightly clustered arch of 30 bb-sized magnets compressing the gastric incisura (
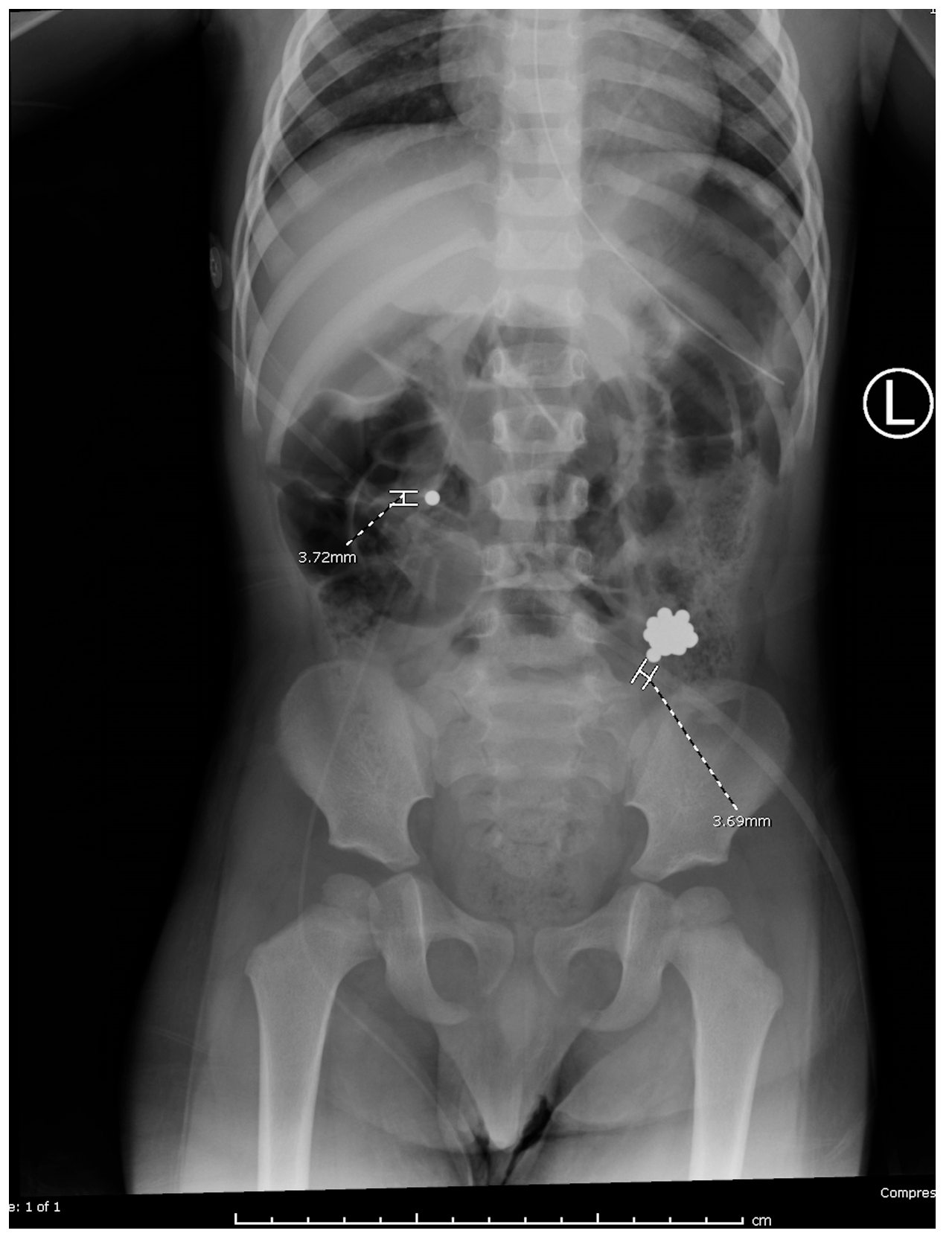
Figure 2). Using a Roth net, they removed the magnets in two passes with no complications other than minor erosions on the gastric mucosa. Post-procedural imaging revealed residual magnets in the proximal jejunum (
Figure 3).
Due to concerning gas patterns 36 h into admission and inability to locate all magnets on imaging, general surgery proceeded with diagnostic laparoscopy. The laparoscopy revealed a single magnet in the hepatic flexure of the colon and a cluster of magnets in the splenic flexure.
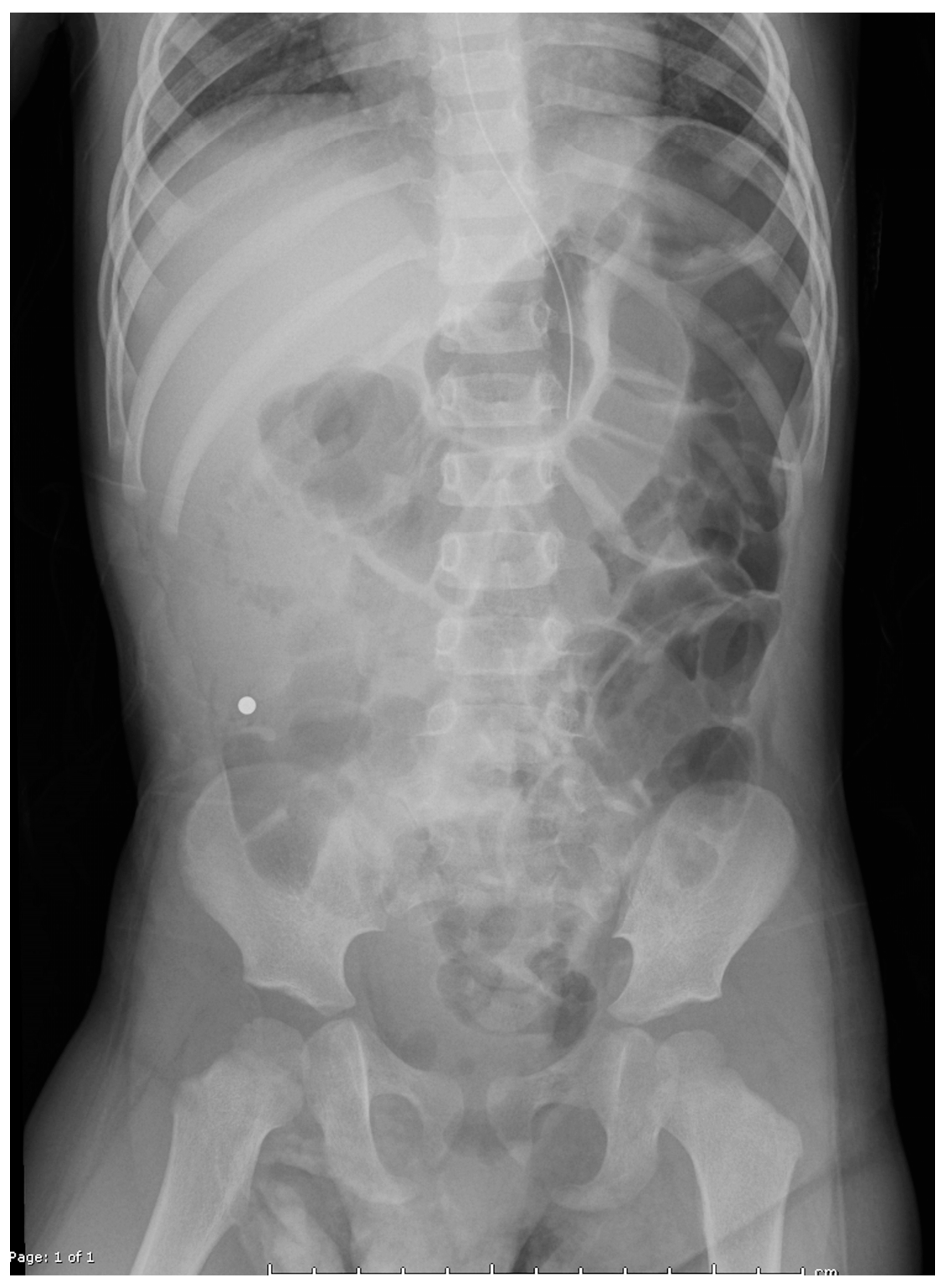
Colonoscopy was attempted by pediatric gastroenterology in an unprepped colon to avoid procedural delays. Due to formed stool, retrieval was unsuccessful. A nasogastric tube was placed for MiraLAX-based bowel prep, and serial abdominal x-rays were performed (
Figure 4a,b). This approach aligns with conservative management strategies reported in the literature [
3,
11].
Outcome
On the day of discharge, the patient had passed 12 magnets per rectum, with significant clinical improvement. He tolerated oral intake without recurrence of symptoms, and follow-up imaging confirmed complete resolution of the foreign bodies. The patient was discharged home with instructions for continued monitoring and dietary adjustments to ensure recovery (
Figure 5).
4. Discussion
High-powered magnet ingestion in children poses unique challenges due to the magnetic forces that can cause tissue compression, necrosis, and perforation. Recent cases have demonstrated the potential for severe complications, including gastrointestinal fistulas, volvulus, and perforations, necessitating surgical intervention [
7,
8,
9].
This case highlights the importance of a multidisciplinary approach, with emergency physicians playing a central role in initiating timely interventions and coordinating care across specialties. The collaboration and cooperation amongst otolaryngology, general surgery, and gastroenterology specialists was essential to the successful outcome in our case. This highlights the need for adoption of protocols, such as those published by NASPGHAN, that facilitate quick and effective interdisciplinary coordination in similar cases [
3,
11].
Regulatory actions targeting the design and sale of high-powered magnets have fluctuated over the years, correlating with the incidence of ingestion cases [
1,
12]. The U.S. Consumer Protection Safety Commission has approved a new federal standard to reduce significant risk factors such as the strength of smaller magnets sold on the market, going into effect in 2022 [
12]. Since stricter regulation has correlated with lower incidence, this recent reintroduction of stringent regulation may have a lasting impact on the incidence of ingestion in the U.S [
1]. Efforts to advocate for safer design practices must be aimed at manufacturers. However, magnets remain accessible, necessitating continued public health efforts to educate parents and caregivers about associated risks.
5. Conclusions
This case underscores the essential role of the ED in managing complex foreign body ingestions through rapid diagnosis, multidisciplinary collaboration, and conservative management strategies. It highlights the need for regulatory advocacy and public awareness to prevent pediatric magnet ingestion and associated complications.
Why Should an Emergency Physician Be Aware of This?
This case demonstrates how ED providers can play a central role in coordinating care and employing non-invasive techniques for managing complex foreign body ingestion. Recognizing the risks associated with magnet ingestion and understanding the value of rapid imaging and multidisciplinary approaches can significantly improve patient outcomes.
Author Contributions
Conceptualization, N.G. and G.F.; writing—original draft, N.G.; writing—review and editing, N.G., G.F. and D.P.Y.; supervision, G.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This case report did not require IRB approval, as it involves a single patient and is not considered human subjects research under institutional policy and federal regulations (45 CFR 46).
Informed Consent Statement
Verbal consent was obtained from the patient’s guardians to publish this paper during a follow-up telephone call, with clear understanding and agreement. A transcript of the telephone call in which informed consent was obtained was included in the manuscript submission documents.The rationale for using verbal consent is patient’s parents had already left the hospital when we decided to pursue this as a case report, we contacted them by phone and.
Data Availability Statement
No new data were generated or analyzed. All relevant information is included in the article. Additional clinical data cannot be shared due to patient privacy.
Conflicts of Interest
Authors N.G. and G.F. are employed by the company US Acute Care Solutions. The authors declare that the research was conducted in the absence of any commercial of financial relations that could be constructed as a potential conflict of interest. The company USACS had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- Middelberg, L.K.; Funk, A.R.; Hays, H.L.; McKenzie, L.B.; Rudolph, B.; Spiller, H.A. Magnet Injuries in Children: An Analysis of the National Poison Data System from 2008 to 2019. J. Pediatr. 2021, 232, 251–256.e2. [Google Scholar] [CrossRef] [PubMed]
- Guilcher, K.; Sokollik, C. Innovative Makeshift Technique for Removing Ingested Rare Earth Magnets. JPGN Rep. 2022, 3, e257. [Google Scholar] [CrossRef] [PubMed]
- Hussain, S.Z.; Bousvaros, A.; Gilger, M.; Mamula, P.; Gupta, S.; Kramer, R.; Noel, R.A. Management of ingested magnets in children. J. Pediatr. Gastroenterol. Nutr. 2012, 55, 239–242. [Google Scholar] [CrossRef] [PubMed]
- Maravilla, V.; Mentessidou, A.; Malakounides, G. Multiple Ball Magnet Ingestion With Sandwiching of the Uvula. J. Emerg. Med. 2022, 63, 306–308. [Google Scholar] [CrossRef] [PubMed]
- Stephenson, S.G.; Knight, C.T.; Rana, H.N.; Standley, T.; Figarola, S. An Unfortunate Union: A Case of Multiple Magnet Ingestion in a Pediatric Patient. Cureus 2022, 14, e21490. [Google Scholar] [CrossRef] [PubMed]
- Aishat, M.; Irshad, O.M.; Shurafa, F.M.; Mohamed, S. The Ingestion of 62 Magnetic Beads by a Two-Year-Old Child: A Case Report of a Novel Approach for Retrieval. Cureus 2024, 16, e64541. [Google Scholar] [CrossRef] [PubMed]
- Ndoye, N.A.; Welle, B.I.; Lamega, B.; Diawara, A.; Zeng, F.T.A.; Ngom, G. Ileal Perforation Peritonitis Secondary to Ingestion of Magnetic Beads in the Older Child: A Case Report. Int. J. Surg. Case Rep. 2024, 121, 109915. [Google Scholar] [CrossRef] [PubMed]
- Jain, N.; Mitra, A.; Ratan, S.K.; Panda, S.S. Necklace of magnets in the abdomen: An unusual case with multiple bowel perforations. Med. J. Armed Forces India 2024, 80, 365–368. [Google Scholar] [CrossRef] [PubMed]
- Özcan, R.; Hakalmaz, A.E.; Kalyoncu Uçar, A.; Beser, O.; Emre, S. Chronic jejuno-colonic fistula and intestinal malabsorption due to multiple magnet ingestions: A case report and systematic review. Ulus. Travma Acil Cerrahi Derg. 2024, 30, 361–369. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, J.M.; Kumta, N.A.; Lai, J. Successful endoscopic removal of high-power magnetic balls embedded in the duodenal wall. JPGN Rep. 2024, 5, 182–185. [Google Scholar] [CrossRef] [PubMed]
- Altokhais, T. Magnet Ingestion in Children Management Guidelines and Prevention. Front. Pediatr. 2021, 9, 727988. [Google Scholar] [CrossRef] [PubMed]
- CPSC Approves New Federal Safety Standard for Magnets to Prevent Deaths and Serious Injuries from High-Powered Magnet Ingestion. U.S. Consumer Product Safety Commission. Available online: https://www.cpsc.gov/Newsroom/News-Releases/2022/CPSC-Approves-New-Federal-Safety-Standard-for-Magnets-to-Prevent-Deaths-and-Serious-Injuries-from-High-Powered-Magnet-Ingestion (accessed on 4 December 2024).
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).