- Article
Continuous Positive Airway Pressure Versus Nocturnal Oxygen in Obstructive Sleep Apnea: A Propensity Score Matching Study
- Carlos Granados-Burgos,
- Eduardo Tuta-Quintero and
- Juan Hernández
- + 13 authors
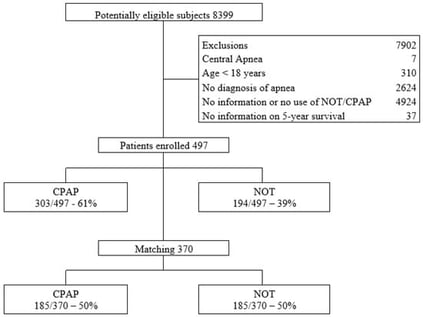
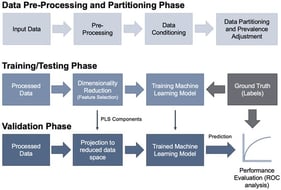
Background: Obstructive sleep apnea (OSA) affects quality of life and increases cardiovascular risk. Nocturnal oxygen therapy (NOT) offers a potential alternative for patients intolerant to CPAP. The objective of this study was to compare NOT and continuous positive airway pressure (CPAP) by evaluating five-year survival in patients with obstructive sleep apnea. Methods: A retrospective cohort study was conducted using propensity score matching (PSM) methodology. A PSM analysis was conducted to reduce selection bias due to differences in baseline characteristics between patients using CPAP and those receiving oxygen therapy. Balance between treated and untreated groups was assessed using standardized mean differences. A PSM was estimated using a logistic regression model, matching patients adherent to CPAP therapy to those treated with NOT. Results: A total of 497 patients with a confirmed diagnosis of OSA were included in the analysis. The mean age was 62.1 years (SD13.6), and 54.3% (270/497) were male. Overall, 42.1% (209/497) of the patients were over 65 years old. Of the total, 303 patients received CPAP therapy and 194 received NOT. After PSM, a matched cohort of 370 patients (185 per group) was obtained. The CPAP-treated group showed a significantly lower residual Apnea–Hypopnea Index compared to the oxygen therapy group (3.9, IQR: 1.8–6.5 vs. 15, IQR:7.5–29.1; p < 0.001), indicating better physiological control of respiratory events. Treatment with CPAP was associated with a significantly lower risk of mortality compared with NOT across analytical approaches, including weighted logistic regression (OR = 0.11; 95% CI 0.02–0.48; p = 0.004) and PSM with bootstrap estimation (ATT = −0.12; 95% CI −0.22 to −0.01; p = 0.030). Conclusions: In this cohort, higher five-year survival was observed among patients with OSA treated with CPAP compared with those receiving supplemental oxygen. These findings indicate a favorable association between CPAP use and long-term outcomes, supporting its role as the preferred first-line therapy in patients with OSA.
26 January 2026