Medical Imaging for Radiotherapy
A special issue of Applied Sciences (ISSN 2076-3417). This special issue belongs to the section "Applied Biosciences and Bioengineering".
Deadline for manuscript submissions: closed (10 October 2022) | Viewed by 5138
Special Issue Editors
Interests: radiotherapy; imaging; SABR; lung cancer; onco-hematology; melanoma
Interests: machine learning; convolutional neural networks; automation in treatment planning; target motion management; deformable image registration (DIR)
Special Issue Information
Dear Colleagues,
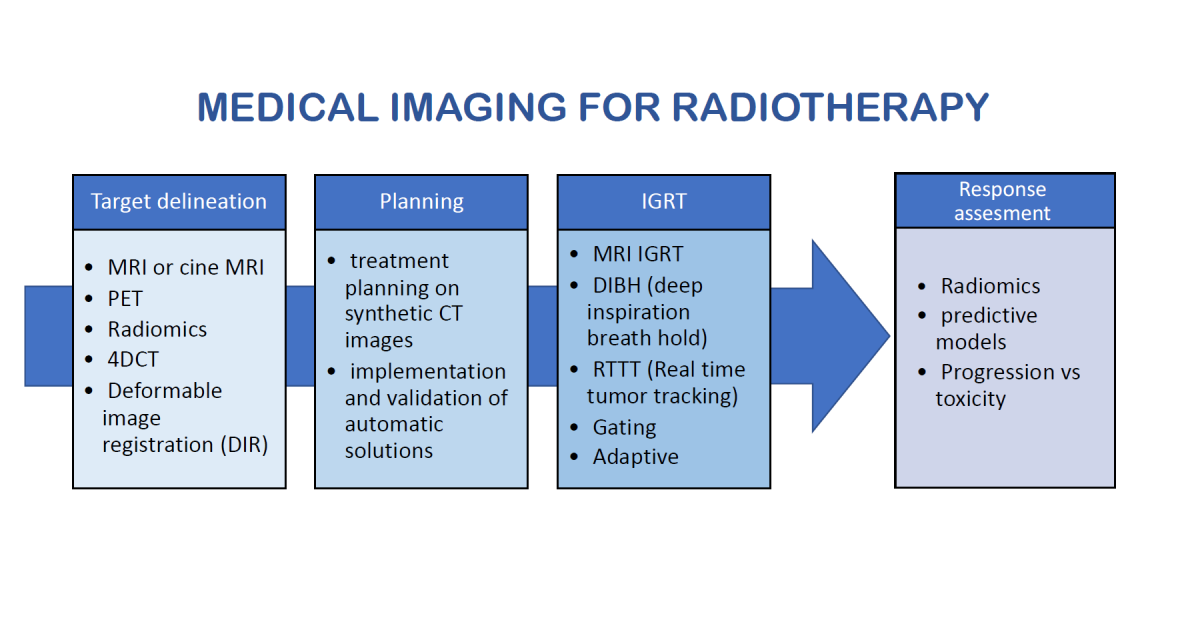
Radiotherapy was born from radiological imaging more than one hundred years ago and evolved over the years to stop being a rib of radiodiagnostic but starring in cancer cure. However, most of the clinical workflow in radiation oncology is still tied to imaging. The target definition, usually delineated on a conventional CT scan, can often be integrated with multimodality imaging to identify cancer boundaries and a tumor’s proliferative heterogeneity or with dedicated technology to reduce uncertainties for organ motion. The second important step in the workflow is the physics planning calculation, a core based on imaging voxel information. Another step is the radiation dose delivery, guided by the imaging onboard the linear accelerators (IGRT) to assess the precision to hit the target and avoid healthy tissues. Then, at last, imaging is also used to evaluate the response at the end of the radiation treatment. Today, all these steps are undergoing frequent updates due to the highly flourishing research on medical imaging, physics, and radiotherapy.
This Special Issue aims to offer the opportunity to all the researchers and clinicians involved in radiation oncology to publish scientific revisions of this changing world or present their early results from original and promising research on:
- Multiparametric or metabolic imaging (MRI, PET) for target definition or predicting the radiation response;
- Radiomics and radiotherapy;
- Treatment planning on synthetic CT images;
- Implementation and validation of automatic solutions for treatment planning;
- Deformable image registration (DIR): potential applications in radiotherapy;
- Target delineation with organ motion management via 4D CT or cine MRI;
- Image-Guided Radiotherapy (IGRT) by MRI or any advanced technique for organ motion control;
- Imaging and strategy for “Adaptive” radiotherapy, with or without re-planning;
- The best imaging to assess response to radiation.
Dr. Stefano Vagge
Dr. Michele Zeverino
Dr. Niccolò Giaj-Levra
Guest Editors
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the special issue website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Applied Sciences is an international peer-reviewed open access semimonthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2400 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- IGRT
- adaptive radiotherapy
- radiomics
- MRI
- molecular imaging
- advanced radiotherapy
- 4DCT
- organ motion
- image reconstruction
- image registration
- automatic planning
Benefits of Publishing in a Special Issue
- Ease of navigation: Grouping papers by topic helps scholars navigate broad scope journals more efficiently.
- Greater discoverability: Special Issues support the reach and impact of scientific research. Articles in Special Issues are more discoverable and cited more frequently.
- Expansion of research network: Special Issues facilitate connections among authors, fostering scientific collaborations.
- External promotion: Articles in Special Issues are often promoted through the journal's social media, increasing their visibility.
- Reprint: MDPI Books provides the opportunity to republish successful Special Issues in book format, both online and in print.
Further information on MDPI's Special Issue policies can be found here.






