A Brief Report on the Role of SPECT/TC in the Optimization of Radiotherapy Treatment with Radical Intent for Unresectable Stage III NSCLC
Abstract
:1. Introduction
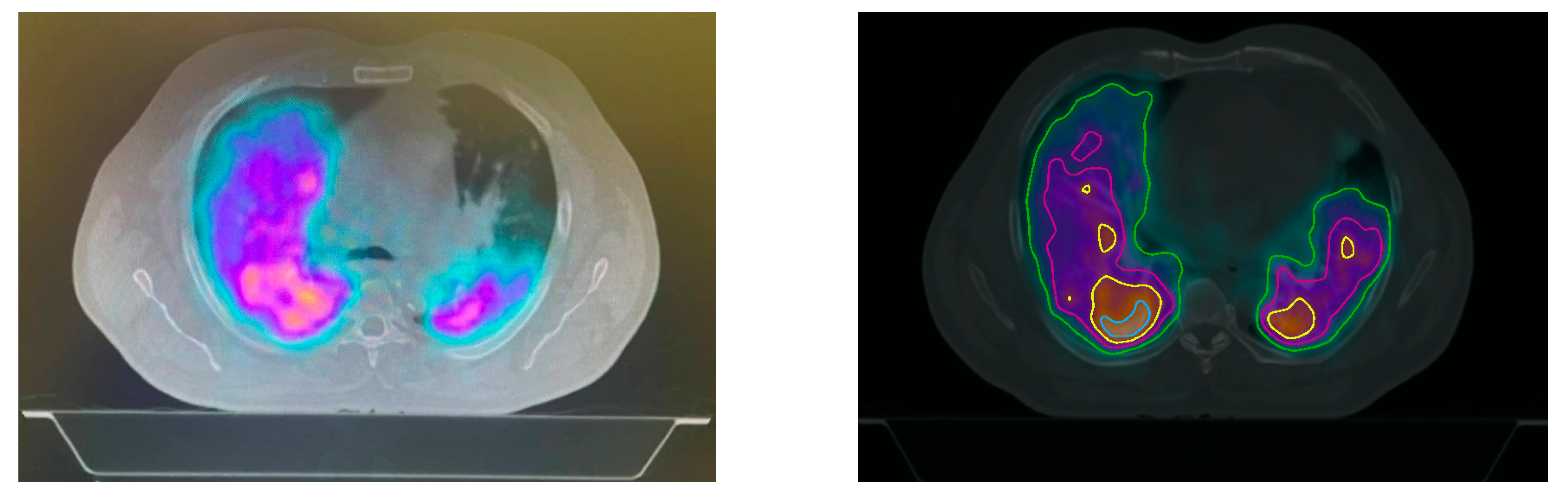
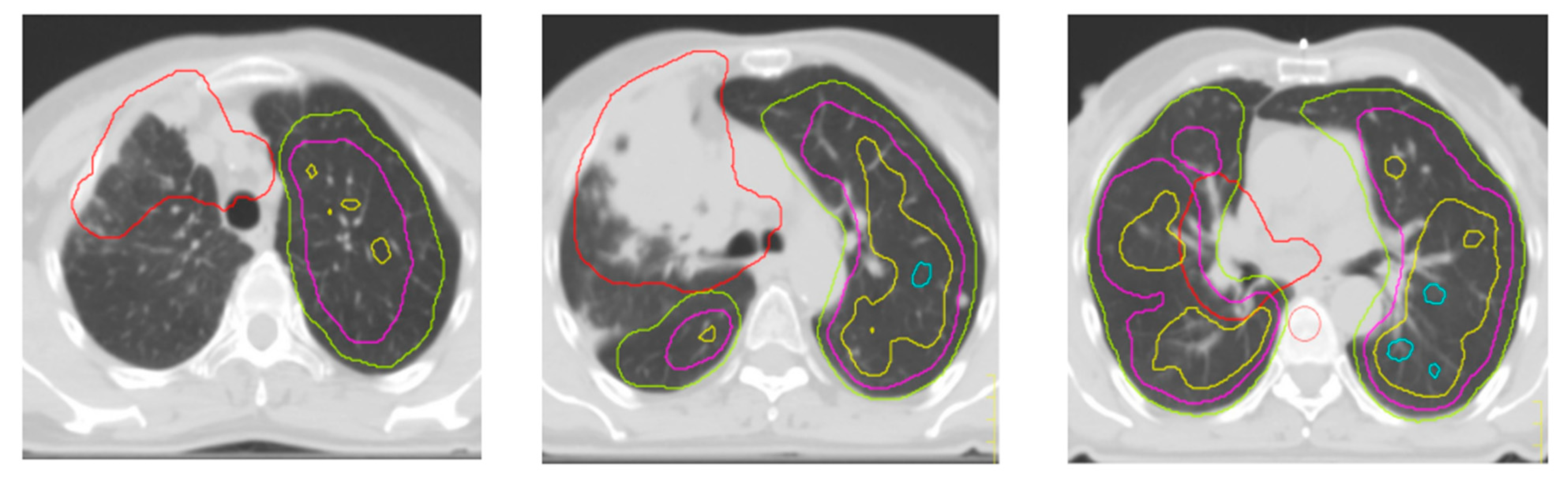
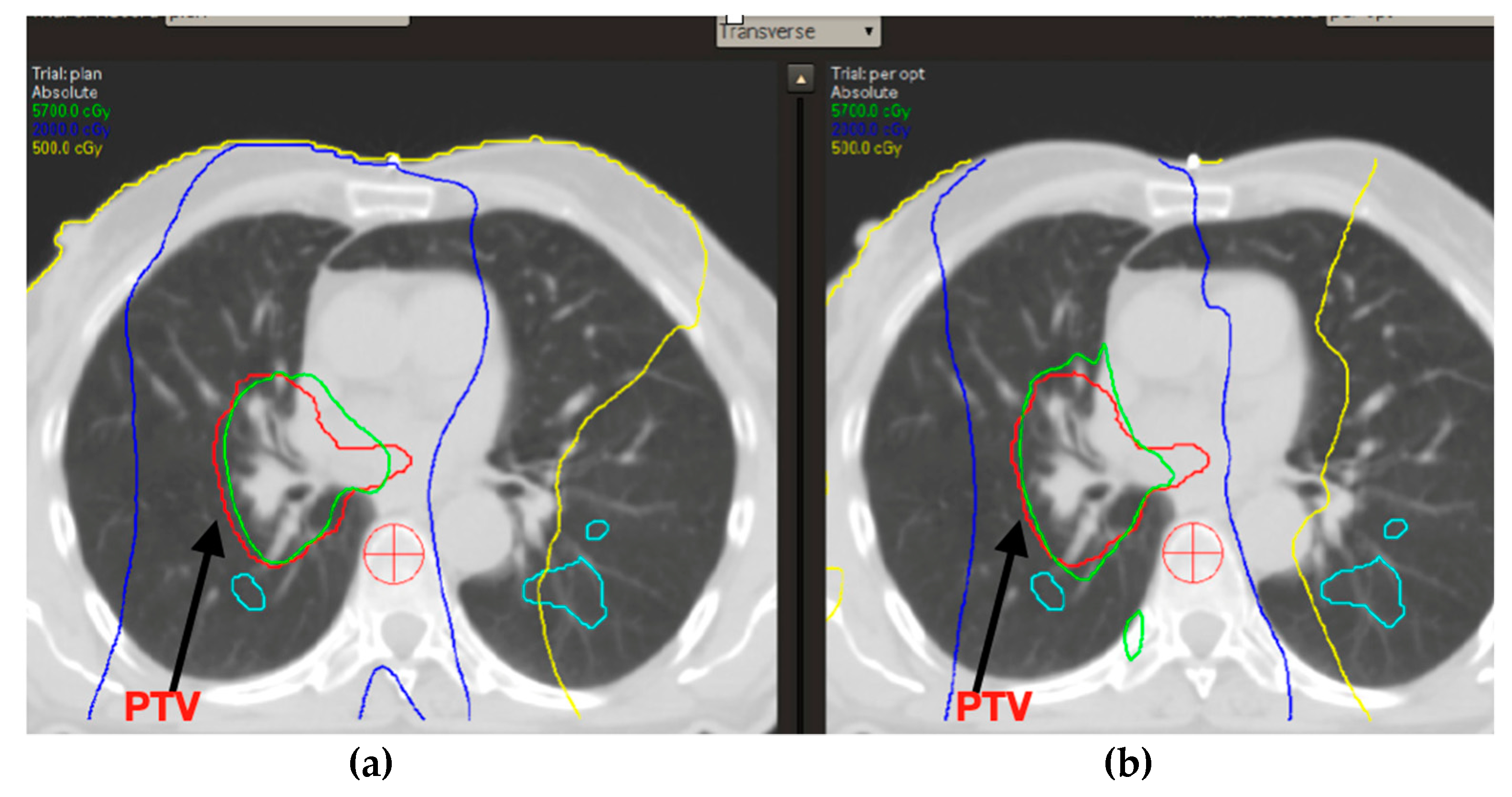
2. Materials and Methods
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Conflicts of Interest
References
- Spigel, D.R.; Faivre-Finn, C.; Gray, J.E.; Vicente, D.; Planchard, D.; Paz-Ares, L.; Vansteenkiste, J.F.; Garassino, M.C.; Hui, R.; Quantin, X.; et al. Five-Year Survival Outcomes From the PACIFIC Trial: Durvalumab After Chemoradiotherapy in Stage III Non–Small-Cell Lung Cancer. J. Clin. Oncol. 2022, 40, 1301–1311. [Google Scholar] [CrossRef] [PubMed]
- Bruni, A.; Scotti, V.; Borghetti, P.; Vagge, S.; Cozzi, S.; D’Angelo, E.; Giaj Levra, N.; Fozza, A.; Taraborrelli, M.; Piperno, G.; et al. Corrigendum: A Real-World, Multicenter, Observational Retrospective Study of Durvalumab After Concomitant or Sequential Chemoradiation for Unresectable Stage III Non-Small Cell Lung Cancer. Front. Oncol. 2021, 11, 802949. [Google Scholar] [CrossRef]
- Chun, S.G.; Hu, C.; Choy, H.; Komaki, R.U.; Timmerman, R.D.; Schild, S.E.; Bogart, J.A.; Dobelbower, M.C.; Bosch, W.; Galvin, J.M.; et al. Impact of Intensity-Modulated Radiation Therapy Technique for Locally Advanced Non–Small-Cell Lung Cancer: A Secondary Analysis of the NRG Oncology RTOG 0617 Randomized Clinical Trial. J. Clin. Oncol. 2017, 35, 56–62. [Google Scholar] [CrossRef]
- Bradley, J.; Graham, M.V.; Winter, K.; Purdy, J.A.; Komaki, R.; Roa, W.H.; Ryu, J.K.; Bosch, W.; Emami, B. Toxicity and outcome results of RTOG 9311: A phase I–II dose-escalation study using three-dimensional conformal radiotherapy in patients with inoperable non–small-cell lung carcinoma. Int. J. Radiat. Oncol. Biol. Phys. 2005, 61, 318–328. [Google Scholar] [CrossRef]
- Cox, J.D. Are the Results of RTOG 0617 Mysterious? Int. J. Radiat. Oncol. Biol. Phys. 2012, 82, 1042–1044. [Google Scholar] [CrossRef]
- National Cancer Institute. Common Terminology Criteria for Adverse Events: CTCAE.
- Kristersson, S.; Lindell, S.-E.; Svanberg, L. Prediction of Pulmonary Function Loss Due to Pneumonectomy Using 133Xe-Radiospirometry. Chest 1972, 62, 694–698. [Google Scholar] [CrossRef]
- Evans, E.S.; Hahn, C.A.; Kocak, Z.; Zhou, S.-M.; Marks, L.B. The Role of Functional Imaging in the Diagnosis and Management of Late Normal Tissue Injury. Semin. Radiat. Oncol. 2007, 17, 72–80. [Google Scholar] [CrossRef]
- Farr, K.P.; Kallehauge, J.F.; Møller, D.S.; Khalil, A.A.; Kramer, S.; Bluhme, H.; Morsing, A.; Grau, C. Inclusion of functional information from perfusion SPECT improves predictive value of dose–volume parameters in lung toxicity outcome after radiotherapy for non-small cell lung cancer: A prospective study. Radiother. Oncol. 2015, 117, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Graham, M.V.; A Purdy, J.; Emami, B.; Harms, W.; Bosch, W.; Lockett, M.A.; A Perez, C. Clinical dose–volume histogram analysis for pneumonitis after 3D treatment for non-small cell lung cancer (NSCLC). Int. J. Radiat. Oncol. Biol. Phys. 1999, 45, 323–329. [Google Scholar] [CrossRef]
- Tsujino, K.; Hirota, S.; Endo, M.; Obayashi, K.; Kotani, Y.; Satouchi, M.; Kado, T.; Takada, Y. Predictive value of dose-volume histogram parameters for predicting radiation pneumonitis after concurrent chemoradiation for lung cancer. Int. J. Radiat. Oncol. Biol. Phys. 2003, 55, 110–115. [Google Scholar] [CrossRef]
- Nestle, U.; De Ruysscher, D.; Ricardi, U.; Geets, X.; Belderbos, J.; Pöttgen, C.; Dziadiuszko, R.; Peeters, S.; Lievens, Y.; Hurkmans, C.; et al. ESTRO ACROP guidelines for target volume definition in the treatment of locally advanced non-small cell lung cancer. Radiother. Oncol. 2018, 127, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Hodapp, N. Der ICRU-Report 83: Verordnung, Dokumentation und Kommunikation der fluenzmodulierten Photonenstrahlentherapie (IMRT) [The ICRU Report 83: Prescribing, recording and reporting photon-beam intensity-modulated radiation therapy (IMRT)]. Strahlenther. Onkol. 2012, 188, 97–100. [Google Scholar] [CrossRef] [PubMed]
- Bentzen, S.M.; Constine, L.S.; Deasy, J.O.; Eisbruch, A.; Jackson, A.; Marks, L.B.; Haken, R.K.T.; Yorke, E.D. Quantitative Analyses of Normal Tissue Effects in the Clinic (QUANTEC): An Introduction to the Scientific Issues. Int. J. Radiat. Oncol. Biol. Phys. 2010, 76, S3–S9. [Google Scholar] [CrossRef] [PubMed]
- Hoover, D.A.; Reid, R.H.; Wong, E.; Stitt, L.; Sabondjian, E.; Rodrigues, G.B.; Jaswal, J.K.; Yaremko, B.P. SPECT-based functional lung imaging for the prediction of radiation pneumonitis: A clinical and dosimetric correlation. J. Med. Imaging Radiat. Oncol. 2014, 58, 214–222. [Google Scholar] [CrossRef] [PubMed]
- Minh Duc, N. The Effects of Applying Apparent Diffusion Coefficient Parameters on the Differentiation between Fourth Ventricular Ependymoma and Diffuse Intrinsic Pontine Glioma. J. Child Sci. 2020, 10, e169–e174. [Google Scholar] [CrossRef]
- Thong, P.M.; Duc, N.M. The Role of Apparent Diffusion Coefficient in the Differentiation between Cerebellar Medulloblastoma and Brainstem Glioma. Neurol. Int. 2020, 12, 34–40. [Google Scholar] [CrossRef] [PubMed]
- Siva, S.; Devereux, T.; Ball, D.L.; MacManus, M.; Hardcastle, N.; Kron, T.; Bressel, M.; Foroudi, F.; Plumridge, N.; Steinfort, D.; et al. Ga-68 MAA Perfusion 4D-PET/CT Scanning Allows for Functional Lung Avoidance Using Conformal Radiation Therapy Planning. Technol. Cancer Res. Treat. 2016, 15, 114–121. [Google Scholar] [CrossRef] [PubMed]
| Variables | Patients | |
|---|---|---|
| Age | 66 (56–75) | 55 |
| Diagnosis | squamous cell carcinoma adenocarcinoma | 3 5 |
| Stage | IIIA IIIB IIIC | 1 5 2 |
| BPCO o other respiratory diseases | 0 | |
| Charlson comorbidity index | <7 | 8 |
| >7 | 0 | |
| chemotherapy | Carboplatin/paclitaxel trisettimanale CDDP/Pemetrexed | 6 2 |
| RIP | G3 G2 G1 G0 | 1 0 0 7 |
| Plane 1 | Plane 2 | p | |
|---|---|---|---|
| D95 PTV | 55 | 55 | ns |
| Mean dose of cumulative lung minus PTV | 13 | 13 | ns |
| Mean dose of ipsilateral lung | 23 | 23 | ns |
| Mean dose of contralateral lung | 9 | 9 | ns |
| V5 | 56% | 56% | ns |
| V20 | 23% | 23% | ns |
| Mean dose of esophagus | 27 | 27 | ns |
| Mean dose of heart | 15 | 15 | ns |
| IsoROI > 20% Max Perfusion | Plane 1 | Plane 2 | p |
|---|---|---|---|
| Mean dose cumulative lung minus PTV | 14 | 14 | ns |
| V20 | 20 | 20 | ns |
| V5 | 54 | 57 | ns |
| IsoROI > 40% max perfusion | Plane 1 | Plane 2 | p |
| Mean dose cumulative lung minus PTV | 14 | 13 | 0.042 |
| V20 | 20 | 19 | ns |
| V5 | 56 | 56 | ns |
| IsoROI > 60% max perfusion | Plane 1 | Plane 2 | p |
| Mean dose cumulative lung minus PTV | 14 | 11 | 0.025 |
| V20 | 23 | 16 | ns (0.05) |
| V5 | 57 | 54 | 0.023 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Imbrescia, J.; Volpi, G.; Lucchini, S.; Toraci, C.; Facheris, G.; La Mattina, S.; Singh, N.; Vaccher, F.; Guerini, A.; Buglione di Monale e Bastia, M.; et al. A Brief Report on the Role of SPECT/TC in the Optimization of Radiotherapy Treatment with Radical Intent for Unresectable Stage III NSCLC. Appl. Sci. 2022, 12, 9351. https://doi.org/10.3390/app12189351
Imbrescia J, Volpi G, Lucchini S, Toraci C, Facheris G, La Mattina S, Singh N, Vaccher F, Guerini A, Buglione di Monale e Bastia M, et al. A Brief Report on the Role of SPECT/TC in the Optimization of Radiotherapy Treatment with Radical Intent for Unresectable Stage III NSCLC. Applied Sciences. 2022; 12(18):9351. https://doi.org/10.3390/app12189351
Chicago/Turabian StyleImbrescia, Jessica, Giulia Volpi, Silvia Lucchini, Cristian Toraci, Giorgio Facheris, Salvatore La Mattina, Navdeep Singh, Filippo Vaccher, Andrea Guerini, Michela Buglione di Monale e Bastia, and et al. 2022. "A Brief Report on the Role of SPECT/TC in the Optimization of Radiotherapy Treatment with Radical Intent for Unresectable Stage III NSCLC" Applied Sciences 12, no. 18: 9351. https://doi.org/10.3390/app12189351
APA StyleImbrescia, J., Volpi, G., Lucchini, S., Toraci, C., Facheris, G., La Mattina, S., Singh, N., Vaccher, F., Guerini, A., Buglione di Monale e Bastia, M., Bruni, A., & Borghetti, P. (2022). A Brief Report on the Role of SPECT/TC in the Optimization of Radiotherapy Treatment with Radical Intent for Unresectable Stage III NSCLC. Applied Sciences, 12(18), 9351. https://doi.org/10.3390/app12189351







