Journal Description
Endocrines
Endocrines
is an international, peer-reviewed, open access journal on endocrinology published quarterly online by MDPI.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High Visibility: indexed within ESCI (Web of Science), Scopus, CAPlus / SciFinder, and other databases.
- Journal Rank: CiteScore - Q2 (Medicine (miscellaneous))
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 39.9 days after submission; acceptance to publication is undertaken in 5.8 days (median values for papers published in this journal in the second half of 2025).
- Recognition of Reviewers: APC discount vouchers, optional signed peer review, and reviewer names published annually in the journal.
Latest Articles
Metabolic Surgery as a Modulator of the Thyroid–Gut Axis: A Narrative Review on Autoimmunity, Function, and Levothyroxine Pharmacokinetics
Endocrines 2026, 7(1), 6; https://doi.org/10.3390/endocrines7010006 - 6 Feb 2026
Abstract
Background: The interplay between obesity and thyroid dysfunction is complex, characterized by adaptive hyperthyrotropinemia and peripheral hormone resistance. Metabolic and Bariatric surgery (MBS) has emerged not only as a weight-loss (WL) intervention but also as a potent modulator of the thyroid–gut axis.
[...] Read more.
Background: The interplay between obesity and thyroid dysfunction is complex, characterized by adaptive hyperthyrotropinemia and peripheral hormone resistance. Metabolic and Bariatric surgery (MBS) has emerged not only as a weight-loss (WL) intervention but also as a potent modulator of the thyroid–gut axis. Methods: We conducted a narrative review of the literature (2015–2025), synthesizing data from prospective cohorts, meta-analyses, and mechanistic studies to evaluate the impact of MBS on thyroid function, autoimmune dynamics, and drug pharmacokinetics. Discussion: Current evidence suggests that MBS promotes a recalibration of the thyroid axis. Post-operative WL is independently associated with a significant reduction in serum thyroid-stimulating hormone (TSH) and free triiodothyronine (fT3) levels, reversing obesity-induced peripheral resistance. Concurrently, the reduction in systemic inflammation (NOD-like receptor protein 3 (NLRP3) inflammasome deactivation) may dampen lymphocytic infiltration, while the amelioration of gut dysbiosis and intestinal permeability is hypothesized to reduce cross-reactivity mechanisms (molecular mimicry), leading to decreased antibody titers in Hashimoto’s thyroiditis. However, these benefits are counterbalanced by altered drug absorption mechanisms. While most hypothyroid patients benefit from reduced Levothyroxine (L-T4) requirements due to decreased lean mass, malabsorptive procedures (Roux-en-Y Gastric Bypass, One Anastomosis Gastric Bypass) can precipitate refractory hypothyroidism due to bypassed absorptive surfaces and altered gastric pH. Conclusions: MBS offers a dual benefit of functional restoration and modulation of autoimmune markers. However, post-surgical management requires a tailored approach. Clinicians must distinguish between the physiological decline in TSH (adaptive) and iatrogenic malabsorption, advocating for liquid L-T4 formulations in complex malabsorptive phenotypes.
Full article
(This article belongs to the Section Obesity, Diabetes Mellitus and Metabolic Syndrome)
►
Show Figures
Open AccessSystematic Review
Medication Adherence and Its Impact on Biochemical Outcomes and Quality of Life in Hypoparathyroidism and Related Endocrine–Metabolic Disorders: A Systematic Review and Meta-Analysis
by
Mariam S. Alharbi
Endocrines 2026, 7(1), 5; https://doi.org/10.3390/endocrines7010005 - 26 Jan 2026
Abstract
►▼
Show Figures
Objectives: This study aimed to evaluate adherence to therapy in hypoparathyroidism and related endocrine–metabolic disorders and to assess its association with biochemical outcomes, hypocalcemia episodes, and health-related quality of life (HRQoL). Methods: In accordance with PRISMA 2020 guidelines, PubMed, Scopus, Google Scholar, and
[...] Read more.
Objectives: This study aimed to evaluate adherence to therapy in hypoparathyroidism and related endocrine–metabolic disorders and to assess its association with biochemical outcomes, hypocalcemia episodes, and health-related quality of life (HRQoL). Methods: In accordance with PRISMA 2020 guidelines, PubMed, Scopus, Google Scholar, and the Cochrane Library were searched until September 2025. The eligible studies were randomized controlled trials, cohort, case–control studies, cross-sectional, and observational studies that reported adherence to calcium/vitamin D or recombinant parathyroid hormone therapy. Results: twenty-three studies were included in the qualitative synthesis, and 11 studies were included in the quantitative meta-analysis. Pooled medication adherence compliance was 70–82% and improved with simplified regimens and the use of recombinant PTH. Additionally, this was also associated with an improvement in HRQoL (p < 0.0001) and a lower risk of hypocalcemia (p < 0.0001). Conversely, multifactorial regulation was observed as the level of adherence had no significant effect on serum calcium levels (p = 0.7116). Sensitivity analyses demonstrate the strength of findings and indicate no significant publication bias. Conclusions: Medication adherence is a key factor in determining patient-centered outcomes in hypoparathyroidism. Better adherence is linked to a higher quality of life and fewer episodes of hypocalcemia, while its effect on biochemical parameters seems minimal. Educational programs, simple treatment regimens, and wider access to rhPTH therapy can be used to improve patient management of the disease over time.
Full article

Figure 1
Open AccessReview
Endocrine and Metabolic Modulation of Vascular Dysfunction in the Diabetic Foot: A Narrative Review
by
Luca Galassi, Erica Altamura, Elena Goldoni, Gabriele Carioti, Beatrice Faitelli, Matteo Lino Ravini, Niccolò Le Donne and Kristi Nika
Endocrines 2026, 7(1), 4; https://doi.org/10.3390/endocrines7010004 - 25 Jan 2026
Abstract
Diabetic foot complications represent a major global health burden and arise from a multifactorial interaction between neuropathy, ischemia, infection, and impaired wound repair. Increasing evidence suggests that, beyond traditional vascular and metabolic risk factors, endocrine dysregulation plays a central role in shaping vascular
[...] Read more.
Diabetic foot complications represent a major global health burden and arise from a multifactorial interaction between neuropathy, ischemia, infection, and impaired wound repair. Increasing evidence suggests that, beyond traditional vascular and metabolic risk factors, endocrine dysregulation plays a central role in shaping vascular dysfunction and tissue vulnerability in patients with diabetes. This narrative review provides an updated overview of the endocrine–vascular axis in the development, progression, and healing of diabetic foot ulcers (DFUs), integrating evidence from experimental and clinical studies identified through targeted searches of PubMed, Embase, and Scopus. We examine how alterations in insulin signaling, relative glucagon excess, adipokine imbalance, dysregulation of stress hormones, and thyroid dysfunction interact with chronic hyperglycemia, dyslipidemia, mitochondrial dysfunction, and low-grade inflammation to impair endothelial homeostasis. These disturbances promote oxidative stress, reduce nitric oxide bioavailability, and compromise microvascular perfusion, thereby creating a pro-ischemic and pro-inflammatory tissue environment that limits angiogenesis, extracellular matrix (ECM) remodeling, immune coordination, and effective wound repair. By linking pathophysiological mechanisms to clinical relevance, this review highlights potential biomarkers of endocrine–vascular dysfunction, implications for risk stratification, and emerging therapeutic perspectives targeting metabolic optimization, endothelial protection, and hormonal modulation. Finally, key knowledge gaps and priority areas for future translational and clinical research are discussed, supporting the development of integrated endocrine-based strategies aimed at improving DFU prevention, healing outcomes, and long-term limb preservation in patients with diabetes.
Full article
(This article belongs to the Section Obesity, Diabetes Mellitus and Metabolic Syndrome)
►▼
Show Figures

Figure 1
Open AccessEditorial
Endocrines: A Passion for Endocrinology, Five Years on
by
Antonio Brunetti
Endocrines 2026, 7(1), 3; https://doi.org/10.3390/endocrines7010003 - 19 Jan 2026
Abstract
Endocrines was launched five years ago with a clear goal: to offer an open, rigorous, and inclusive forum for research spanning basic, translational, and clinical endocrinology and metabolism [...]
Full article
Open AccessArticle
General Characteristics of Papillary Thyroid Cancer Among Adolescents and Young Adults: A Single Large Center Experience
by
Elabbass A. Abdelmahmuod, Mohamad Abufaied, Shehab F. Mohamed, Nada Elharabi, Ahmed Elmudathir Osman, Rafal Al-Shibly, Raghad Bataineh, Maab F. Elhaj, Dabia Al-Mohanadi, Mohammed Bashir and Tania Jaber
Endocrines 2026, 7(1), 2; https://doi.org/10.3390/endocrines7010002 - 19 Jan 2026
Abstract
Background: Papillary thyroid cancer (PTC) incidence is rising, particularly among Adolescents and Young Adults (AYA, 15–39 years). However, data on PTC characteristics in the AYA population, especially from the Middle East, remain limited. This study aims to describe the clinicopathological features of
[...] Read more.
Background: Papillary thyroid cancer (PTC) incidence is rising, particularly among Adolescents and Young Adults (AYA, 15–39 years). However, data on PTC characteristics in the AYA population, especially from the Middle East, remain limited. This study aims to describe the clinicopathological features of PTC in AYA patients treated at a large tertiary center in Qatar. Methods: A retrospective chart review was conducted for AYA patients diagnosed with PTC between May 2015 and December 2020 at Hamad General Hospital, Qatar. Data on demographics, tumor characteristics, histopathology, staging, risk stratification, and treatment were extracted and analyzed. We stratified the cohort based on sex. Results: We studied 326 AYA patients (mean age 33.0 ± 5.2 years); the majority were females (72.7%) and were mostly of Asian origin (51.5%). Most patients underwent total thyroidectomy (77.6%), while 22.4% underwent partial thyroidectomy. Histologically, classic PTC was most common (83.38%), followed by the follicular variant (16.00%). Capsule invasion occurred in 21.04%, vascular invasion in 11.76%, and lymphatic invasion in 14.38%. Most patients were at low ATA risk (68.61%), with intermediate (20.06%) and high risk (11.33%) less common. Distant metastases were rare (0.3%), and 59.1% received Radioactive iodine (RAI). Compared to females, males had larger tumors (mean 2.65 cm vs. 2.01 cm, p = 0.0009), higher rates of vascular invasion (22.4% vs. 7.7%, p < 0.001), affected lymph nodes (mean 4.2 vs. 2.4, p = 0.0223), and ATA high-risk proportions (23.5% vs. 7.0%, p < 0.001). Conclusions: This study provides the first detailed characterization of PTC in AYA patients from Qatar. While confirming female predominance, males exhibited more aggressive features (larger tumors, higher LN involvement, and ATA risk). These findings emphasize the need to consider gender-specific differences in managing PTC within the AYA population.
Full article
(This article belongs to the Section Thyroid Endocrinology)
►▼
Show Figures

Figure 1
Open AccessArticle
Skeletal Muscle Myofiber Development in Non-Human Primate Offspring Deprived of Estrogen in Utero
by
Phillip J. Gauronskas, Terrie J. Lynch, Eugene D. Albrecht and Gerald J. Pepe
Endocrines 2026, 7(1), 1; https://doi.org/10.3390/endocrines7010001 - 22 Dec 2025
Abstract
Introduction: We previously showed that baboon offspring born to mothers deprived of estrogen during the second half of gestation exhibited insulin resistance prior to and after the onset of puberty. Moreover, the size of skeletal muscle myofibers and the number of microvessels important
[...] Read more.
Introduction: We previously showed that baboon offspring born to mothers deprived of estrogen during the second half of gestation exhibited insulin resistance prior to and after the onset of puberty. Moreover, the size of skeletal muscle myofibers and the number of microvessels important for delivery of insulin/glucose to myofibers were lower in near-term fetuses deprived of estrogen during pregnancy, and myofiber capillarization remained reduced in post-pubertal offspring deprived of estrogen in utero. However, it remains to be determined whether skeletal muscle size is restored to normal in animals deprived of estrogen in utero after the onset of puberty/gonadal estrogen production. Methods: To answer this question, the current study quantified the size and number of slow and fast fibers in biopsies of vastus lateralis skeletal muscle obtained from post-pubertal female baboon offspring 9–12 years old, born to mothers who were untreated (n = 7) or treated during the second half of gestation with letrozole (n = 6; suppressed maternal and fetal estrogen by >90%) or letrozole plus estradiol benzoate (n = 3). Results: Results indicated that skeletal muscle slow and fast fiber growth in female offspring appeared to occur by hypertrophy and that respective size of fibers after the onset of puberty was similar in offspring born to mothers who were untreated or deprived of estrogen in utero. Conclusions: Postnatal myofiber hypertrophy likely reflects the impact of the pubertal surge in and continued exposure of offspring myofibers to ovarian estrogen and is restored to normal in post-pubertal female offspring deprived of estrogen in utero.
Full article
(This article belongs to the Section Female Reproductive System and Pregnancy Endocrinology)
►▼
Show Figures

Figure 1
Open AccessArticle
The Impact of Chronic Autoimmune Thyroiditis During Pregnancy on Maternal and Fetal Outcomes
by
Olesea Scrinic, Eduard Circo and Seila Musledin
Endocrines 2025, 6(4), 56; https://doi.org/10.3390/endocrines6040056 - 20 Nov 2025
Abstract
Background/Objectives: Thyroid dysfunction during pregnancy is associated with a range of adverse perinatal outcomes. This study aims to evaluate the effect of maternal thyroid autoimmunity on selected gestational and perinatal outcomes of the newborn in a region with adequate iodine intake. Methods
[...] Read more.
Background/Objectives: Thyroid dysfunction during pregnancy is associated with a range of adverse perinatal outcomes. This study aims to evaluate the effect of maternal thyroid autoimmunity on selected gestational and perinatal outcomes of the newborn in a region with adequate iodine intake. Methods: This retrospective study included 74 full-term singleton pregnancies from women living in the coastal region of Romania. Participants were divided into two groups: group 1—women with chronic autoimmune thyroiditis and euthyroidism; group 2—women without thyroid disorders, serving as the control group. Maternal variables assessed included serum thyroid hormone levels and antithyroid autoantibodies. For newborns, parameters such as birth weight, neonatal TSH levels, and the incidence of gestational and perinatal events were evaluated. Results: The incidence of chronic autoimmune thyroiditis in the study population was 36.4%. Maternal thyroid autoimmunity was associated with an increased incidence of low birth weight, observed in 11% of the autoimmune group compared with 2.1% in the control group (p = 0.099). The incidence of preterm birth was significantly higher in the autoimmune group (18.5% vs. 4.2% in controls, p = 0.043), corresponding to a 4.3-fold increase in relative risk. The most frequent perinatal complication observed in pregnant women with thyroid autoimmunity was spontaneous abortion (11.1%). The median urinary iodine concentrations were within the adequate range in both study groups. Conclusions: Thyroid autoimmunity during pregnancy presents significant clinical challenges, even in areas with adequate iodine intake. Maternal autoimmune thyroiditis constitutes an established risk factor for impaired fetal development and adverse perinatal outcomes. Early assessment of thyroid function prior to conception or during the first trimester is recommended for both diagnostic and preventive purposes.
Full article
(This article belongs to the Section Female Reproductive System and Pregnancy Endocrinology)
Open AccessReview
Diagnosis of Congenital and Acquired Generalized Lipodystrophies—Similarities and Differences
by
Josivan Gomes Lima, Lucas Nobrega Lima, Vitor Yan Bezerra Araujo, Lucia Helena Coelho Nobrega and Julliane Tamara Araújo de Melo Campos
Endocrines 2025, 6(4), 55; https://doi.org/10.3390/endocrines6040055 - 17 Nov 2025
Abstract
Generalized lipodystrophies (GLs) are rare diseases characterized by a lack of body fat. When patients with a GL phenotype are referred with a presumptive diagnosis of congenital generalized lipodystrophy (CGL) but genetic testing for known pathogenic variants is negative, the diagnosis of acquired
[...] Read more.
Generalized lipodystrophies (GLs) are rare diseases characterized by a lack of body fat. When patients with a GL phenotype are referred with a presumptive diagnosis of congenital generalized lipodystrophy (CGL) but genetic testing for known pathogenic variants is negative, the diagnosis of acquired generalized lipodystrophy (AGL) becomes a more likely diagnosis. No single test confirms such a diagnosis, and it is crucial to recognize the similarities and differences between these diseases. We review the literature and report four GL cases from our lipodystrophy outpatient clinic, highlighting the main points for an accurate diagnosis. Similarities: phlebomegaly, umbilical scar protrusion, loss of Bichat’s fat pad, muscle hypertrophy, and hepatomegaly can occur in both. Cirrhosis can also arise, but in AGL, it occurs as a consequence of hepatic steatosis and also due to autoimmune hepatitis. Insulin resistance is frequent, and patients present acanthosis nigricans and acrochordons and may develop difficult-to-control diabetes and its complications, despite very high daily doses of insulin. Low HDL and hypertriglyceridemia are frequent and may progress to acute pancreatitis. Serum leptin levels are typically low and contribute to hyperphagia. Differences: AGL patients’ body fat loss occurs gradually in childhood or adolescence, whereas CGL patients are born with the characteristic phenotype. Evaluating photographs of AGL patients in the first years of life can provide evidence of this selective and gradual fat loss. Some AGL patients may have panniculitis (inflamed and painful subcutaneous nodules), with or without autoimmune diseases. In conclusion, recognizing both similarities and differences is crucial for making an accurate diagnosis and ensuring the most appropriate treatment.
Full article
(This article belongs to the Section Obesity, Diabetes Mellitus and Metabolic Syndrome)
►▼
Show Figures

Figure 1
Open AccessReview
The Role of Follicle-Stimulating Hormone in Bone Loss During Menopause Transition: A Narrative Review
by
Nida Jugulytė and Daiva Bartkevičienė
Endocrines 2025, 6(4), 54; https://doi.org/10.3390/endocrines6040054 - 5 Nov 2025
Cited by 1
Abstract
For many years, menopause-related bone loss has been attributed solely to declining estrogen levels. Recently it has been suggested that bone loss accelerates during perimenopause, often preceding declines in estradiol (E2), proposing that follicle-stimulating hormone (FSH), the levels of which are
[...] Read more.
For many years, menopause-related bone loss has been attributed solely to declining estrogen levels. Recently it has been suggested that bone loss accelerates during perimenopause, often preceding declines in estradiol (E2), proposing that follicle-stimulating hormone (FSH), the levels of which are high during late perimenopause, may play a role in skeletal deterioration independently of E2. The aim of this narrative review was to present aspects of bone health throughout the menopause transition with a focus on the relationship between FSH and bone-related outcomes. Epidemiological studies evaluating bone mineral density (BMD) and bone turnover markers (BTMs) were analyzed. Higher FSH levels were associated with reduced BMD, particularly at the spine and hip, as well as enhanced bone remodeling activity. In several longitudinal studies, FSH was found to be a more reliable predictor of bone loss than estrogen. In conclusion, FSH may serve as an early marker of perimenopausal bone health deterioration by identifying women at risk for bone loss and allowing for more personalized prevention strategies; however, further research is needed before its clinical use.
Full article
(This article belongs to the Section Female Reproductive System and Pregnancy Endocrinology)
Open AccessFeature PaperReview
The Mechanisms of Angiogenesis and Apoptosis During the Functional Formation and Regression of the Corpus Luteum in the Ovarian Reproductive Endocrine System
by
Dody Houston Billhaq and Seunghyung Lee
Endocrines 2025, 6(4), 53; https://doi.org/10.3390/endocrines6040053 - 21 Oct 2025
Abstract
The ovarian corpus luteum has functional mechanisms for formation and regression in the reproductive endocrine system. The main functional events of the corpus luteum are angiogenesis and apoptosis mechanisms. The development of the corpus luteum involves homogeneous physiological mechanisms, including cellular functions and
[...] Read more.
The ovarian corpus luteum has functional mechanisms for formation and regression in the reproductive endocrine system. The main functional events of the corpus luteum are angiogenesis and apoptosis mechanisms. The development of the corpus luteum involves homogeneous physiological mechanisms, including cellular functions and reproductive hormones. Angiogenesis is controlled by pro-angiogenic and anti-angiogenic factors. The microenvironment involves various signaling molecules and pathways that may play a potential role in angiogenic response during corpus luteum growth. In luteolysis, the corpus luteum undergoes degeneration, notably induced by reproductive hormones that promote programmed cell death in luteal cells through the apoptosis mechanism. In this sudy, we discuss the mechanisms and functional roles of angiogenesis and apoptosis in the endocrine microenvironment during corpus luteum formation and regression, based on the interrelationship of physiological events in the ovary.
Full article
(This article belongs to the Section Female Reproductive System and Pregnancy Endocrinology)
►▼
Show Figures

Figure 1
Open AccessArticle
Gestational Weight Gain and Adverse Pregnancy Outcomes in Women with Gestational Diabetes Mellitus and Obesity
by
Filipe Dias de Souza, Patrícia Medici Dualib, Martha Camillo Jordão, Micaela Frasson Montero, Maria Carolina Oliveira Abate, Leonardo Luna, Rosiane Mattar and Bianca de Almeida-Pititto
Endocrines 2025, 6(4), 52; https://doi.org/10.3390/endocrines6040052 - 20 Oct 2025
Abstract
Background/Objectives: The association between gestational weight gain (GWG) and adverse outcomes in individuals with gestational diabetes mellitus (GDM) and obesity remains unclear. This study aimed to evaluate the relationship between total GWG and maternal, obstetric, and neonatal outcomes in patients with GDM, stratified
[...] Read more.
Background/Objectives: The association between gestational weight gain (GWG) and adverse outcomes in individuals with gestational diabetes mellitus (GDM) and obesity remains unclear. This study aimed to evaluate the relationship between total GWG and maternal, obstetric, and neonatal outcomes in patients with GDM, stratified by obesity class. Methods: This retrospective cohort included 695 pregnant individuals with GDM treated at a tertiary university hospital in Brazil between 2007 and 2021. GWG was categorized as insufficient, adequate, or excessive per National Academy of Medicine guidelines. Outcomes included maternal, obstetric, and neonatal events. Analyses were conducted for the entire cohort and stratified by obesity class (I and II/III), using multivariate regression models adjusted for maternal age, parity, and pre-pregnancy BMI. Results: The mean age was 33.6 (SD 5.7) years. GWG was insufficient in 33.2%, adequate in 28.2%, and excessive in 37.8%. Excessive GWG was associated with increased odds of cesarean delivery (OR 1.69; 95% CI 1.15–2.48) and large-for-gestational-age newborns (OR 3.29; 95% CI 1.61–6.46). As a continuous variable, GWG was positively associated with cesarean delivery (OR 1.04), LGA (OR 1.10), and birthweight (β = 0.02). Lower GWG was independently associated with reduced preeclampsia risk (OR 1.09 per kg). Insufficient GWG was not linked to increased risk of small-for-gestational-age newborns or other adverse outcomes and was associated with lower insulin requirement. Results remained consistent across obesity subgroups, except for cesarean delivery in class II/III obesity. Conclusions: In individuals with GDM and obesity, insufficient GWG was not associated with increased adverse outcomes, while excessive GWG was consistently linked to unfavorable maternal and neonatal risks. Stricter GWG control may be safe and beneficial in this population.
Full article
(This article belongs to the Section Obesity, Diabetes Mellitus and Metabolic Syndrome)
►▼
Show Figures
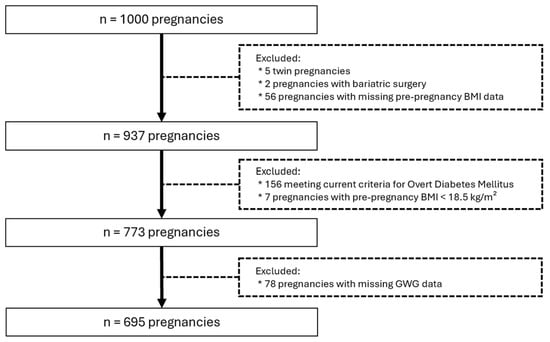
Figure 1
Open AccessArticle
Circulating miR-122 and miR-139-3p: Association with Lipid, Inflammatory, and Glycemic Profile in Adolescents with Insulin-Resistant and Overweight
by
Tanyara Baliani Payolla, Paula Nascimento Brandão-Lima, Gabrielli Barbosa de Carvalho, Flávia Mori Sarti, Regina Mara Fisberg and Marcelo Macedo Rogero
Endocrines 2025, 6(4), 51; https://doi.org/10.3390/endocrines6040051 - 15 Oct 2025
Abstract
Background/Objectives: Insulin resistance (IR) in adolescents contributes to the development of metabolic and immunological alterations. These alterations can lead to chronic, systemic, low-grade inflammation in adulthood. Evidence suggests that alterations in miRNA expression play a significant role in the onset of IR by
[...] Read more.
Background/Objectives: Insulin resistance (IR) in adolescents contributes to the development of metabolic and immunological alterations. These alterations can lead to chronic, systemic, low-grade inflammation in adulthood. Evidence suggests that alterations in miRNA expression play a significant role in the onset of IR by influencing insulin signaling pathways. Therefore, identifying specific miRNAs may aid in the early diagnosis of cardiometabolic risk, particularly during the transition from adolescence to adulthood. Methods: This population-based study aimed to analyze the expression of 21 miRNAs in the plasma of adolescents. We considered IR status, overweight, sex, and age for the analyses. The study measured miRNA expression in plasma samples from 187 adolescents aged 12 to 19 years from the cross-sectional study of the 2015 São Paulo Health Survey (ISA-Nutrition). MiRNA expression was assessed using Exiqon® assays on Fluidigm® technology (Les Ulis, France). Statistical analyses were performed to identify differences in miRNA expression and correlations between variables, using a complex research design to ensure representativeness at the population level. Results: The incidence of IR and overweight was high in adolescents (44% and 33%, respectively). High-sensitivity C-reactive protein (hs-CRP) concentration was higher in overweight adolescents. IR was correlated with higher plasma expression of miR-122 and miR-139-3p. Furthermore, miR-486, miR-363, miR-30d, miR-28, miR-223, miR-21, miR-146, miR-130b, miR-126, miR-122, and miR-139-3p showed specific correlations with individual risk for IR, sex, and adolescent stage. Conclusions: The miRNAs showed differential expression according to sex and adolescent stage, and were correlated with cardiometabolic risk factors, suggesting their potential utility for early screening in adolescents. The study highlights age- and sex-related differences in miRNA levels between adolescents with IR and overweight. The cross-sectional design is a limitation of this study, as we cannot infer causality for the associations observed here.
Full article
(This article belongs to the Section Obesity, Diabetes Mellitus and Metabolic Syndrome)
►▼
Show Figures

Figure 1
Open AccessArticle
Obesity Is Associated with Larger Thyroid Nodules but Not with Malignant Cytology
by
Stefania Giuliano, Giuseppe Seminara, Stefano Iuliano, Stefania Obiso, Eusebio Chiefari, Daniela P. Foti, Maria Mirabelli and Antonio Brunetti
Endocrines 2025, 6(4), 50; https://doi.org/10.3390/endocrines6040050 - 14 Oct 2025
Abstract
Background: Obesity has been proposed as a risk factor for differentiated thyroid carcinoma (DTC), though findings in the literature remain conflicting. While some studies suggest an association between elevated body mass index (BMI) and thyroid malignancy, others attribute this link to diagnostic bias.
[...] Read more.
Background: Obesity has been proposed as a risk factor for differentiated thyroid carcinoma (DTC), though findings in the literature remain conflicting. While some studies suggest an association between elevated body mass index (BMI) and thyroid malignancy, others attribute this link to diagnostic bias. The Calabria region in Southern Italy, historically affected by iodine deficiency and endemic goiter, offers a valuable population for investigating this relationship. Objective: This study aimed to evaluate the association between obesity and clinical, sonographic, and cytological characteristics of thyroid nodules in a Calabrian cohort undergoing fine-needle aspiration biopsy (FNAB). Methods: This retrospective observational study included 1192 patients evaluated at a single endocrine referral center between 2015 and 2024. Patients were stratified by BMI (<30 vs. ≥30 kg/m2). Demographic, biochemical, ultrasound, and cytological data were collected and analyzed. Cytological results were classified according to the SIAPEC 2014 system. Results: Obese patients had significantly larger thyroid nodules in terms of anteroposterior and transverse diameters, as well as overall volume (p < 0.05). However, the distribution of high-risk cytological categories (TIR 3B, TIR 4, and TIR 5) did not differ significantly between obese and non-obese patients (9.4% in both groups). Multivariate analysis confirmed that BMI was not an independent predictor of malignancy risk (OR 0.988; p = 0.723), whereas younger age was inversely associated with malignancy. Conclusions: Obesity appears to influence thyroid nodule size but does not constitute an independent risk factor for cytological malignancy. BMI should not influence indications for FNAB or subsequent treatment decisions. Thyroid nodule management should instead rely on ultrasound risk stratification and cytological findings. Special attention should be given to younger patients as they may carry a higher malignancy risk.
Full article
(This article belongs to the Special Issue Feature Papers in Endocrines 2025)
Open AccessEditor’s ChoiceReview
Sleep Deprivation and Its Impact on Insulin Resistance
by
Margarida C. Pinheiro, Henrique E. Costa, Melissa Mariana and Elisa Cairrao
Endocrines 2025, 6(4), 49; https://doi.org/10.3390/endocrines6040049 - 11 Oct 2025
Cited by 2
Abstract
►▼
Show Figures
Background/Objectives: Adequate sleep has a fundamental role in human health, mainly in cognitive and physiological functions. However, the daily demands of modern society have led to a constant pursuit of better living conditions, requiring more active hours at the expense of sleeping
[...] Read more.
Background/Objectives: Adequate sleep has a fundamental role in human health, mainly in cognitive and physiological functions. However, the daily demands of modern society have led to a constant pursuit of better living conditions, requiring more active hours at the expense of sleeping hours. This sleep deprivation has been associated with human health deterioration, namely an increase in Diabetes Mellitus incidence. This metabolic disease is a chronic pathology that imposes a big burden on health systems and is associated with the rise in insulin resistance. In this sense, the aim of this review is to analyze the relation between sleep deprivation and insulin resistance, emphasizing the metabolic parameters and hormones that may be involved in the subjacent mechanism. Methods: A literature review of the last 10 years was performed with specific terms related to “sleep deprivation” and “insulin resistance”. Results: Overall, the studies analyzed showed a decrease in insulin sensitivity in cases of sleep deprivation, even with different study protocols. In addition, an association between sleep deprivation and increased non-esterified fatty acids was also noticeable; however, other parameters such as cortisol, metanephrines, and normetanephrines showed no consistent results among the studies. Conclusions: This review allowed us to confirm the relationship between sleep deprivation and insulin resistance; however, despite the difficulties to monitor sleep, more research is needed to understand the related mechanisms that have not yet been clarified.
Full article

Graphical abstract
Open AccessEditor’s ChoiceReview
Comparing Glucometer-Based and Laboratory-Based OGTT for Diabetes Diagnosis: A Narrative Review
by
Tanvir Ahmed, Jaimala Kishore, Mensila Onamika, Shuvratithi Goswami, Iffat Rahman Momo, Hanif Sumon and Rodney G. Bowden
Endocrines 2025, 6(3), 48; https://doi.org/10.3390/endocrines6030048 - 18 Sep 2025
Cited by 2
Abstract
Background: The oral glucose tolerance test (OGTT) is the gold standard for diagnosing diabetes; however, its use is often limited by the need for laboratory infrastructure, trained personnel, and extended turnaround times. In contrast, glucometer-based OGTT offers a convenient and affordable alternative, especially
[...] Read more.
Background: The oral glucose tolerance test (OGTT) is the gold standard for diagnosing diabetes; however, its use is often limited by the need for laboratory infrastructure, trained personnel, and extended turnaround times. In contrast, glucometer-based OGTT offers a convenient and affordable alternative, especially in resource-limited settings. Objective: This narrative review aims to assess the diagnostic accuracy of glucometer-based OGTT compared to standard laboratory-based OGTT, while also evaluating its feasibility and potential application in diabetes screening programs. Evidence Summary: Studies consistently demonstrate a strong correlation between capillary glucose levels measured by glucometers and venous plasma glucose concentrations obtained through standard laboratory methods. Many studies reported high sensitivity and specificity, often exceeding 90%, particularly when using well-calibrated, newer-generation devices. These findings support the diagnostic utility of glucometer-based OGTT in various populations, although performance may vary by device model and clinical context. Standardization of testing protocols remains essential for consistent results. Conclusions: Glucometer-based OGTT shows promise as a reliable, rapid and cost-effective diagnostic approach, particularly in low-resource and community-based settings. While it is not a complete substitute for laboratory-based OGTT, it offers substantial advantages in accessibility, affordability, and scalability. Continued research with newer-generation glucometers and standardized testing protocols is essential to support broader clinical implementation and public health integration.
Full article
(This article belongs to the Section Obesity, Diabetes Mellitus and Metabolic Syndrome)
Open AccessReview
Diabetes and Sarcopenia: Unraveling the Metabolic Crossroads of Muscle Loss and Glycemic Dysregulation
by
Jose Jorge Ortez Toro
Endocrines 2025, 6(3), 47; https://doi.org/10.3390/endocrines6030047 - 18 Sep 2025
Cited by 1
Abstract
The intersection of type 2 diabetes mellitus (T2DM) and sarcopenia, often termed diabetic sarcopenia, represents a critical yet underrecognized comorbidity that significantly impacts the quality of life and functional capacity of older adults. This paper explores the complex interplay between T2DM and sarcopenia,
[...] Read more.
The intersection of type 2 diabetes mellitus (T2DM) and sarcopenia, often termed diabetic sarcopenia, represents a critical yet underrecognized comorbidity that significantly impacts the quality of life and functional capacity of older adults. This paper explores the complex interplay between T2DM and sarcopenia, focusing on the prevalence, risk factors, and underlying mechanisms driving muscle mass and strength decline in this population. Drawing from recent clinical studies, we highlight a prevalence of sarcopenia ranging from 15.36% to 30.2% among elderly T2DM patients, with notable gender disparities (41.3% in men versus 20.1% in women) and regional variations. Key risk factors identified include poor glycemic control (HbA1c ≥8%), longer diabetes duration (>5 years), low body mass index (BMI), and reduced levels of 25-hydroxyvitamin D and insulin-like growth factor-1 (IGF-1). We also recommend a practical screening algorithm for diabetic sarcopenia, integrating tools like the SARC-F questionnaire, dynamometry, and BMI-adjusted calf circumference to facilitate early diagnosis and staging in clinical settings. The review underscores the need for a multidisciplinary approach—encompassing pharmacological optimization, nutritional interventions with high-protein diets, and tailored physical exercise—to mitigate muscle loss and improve metabolic outcomes. Future research directions should focus on validating diagnostic protocols and diagnosis techniques and further exploring specific therapies to effectively address this dual burden.
Full article
(This article belongs to the Section Obesity, Diabetes Mellitus and Metabolic Syndrome)
Open AccessEditor’s ChoiceReview
Remnant Cholesterol: From Pathophysiology to Clinical Implications in Type 1 Diabetes
by
Fernando Sebastian-Valles, Álvaro Montes Muñiz and Mónica Marazuela
Endocrines 2025, 6(3), 46; https://doi.org/10.3390/endocrines6030046 - 15 Sep 2025
Cited by 1
Abstract
Remnant cholesterol, contained within triglyceride-rich lipoproteins such as VLDL and IDL, has emerged as an independent risk factor for atherosclerotic cardiovascular disease (ASCVD) in both the general population and individuals with diabetes. Unlike LDL cholesterol, remnant cholesterol has not traditionally been a therapeutic
[...] Read more.
Remnant cholesterol, contained within triglyceride-rich lipoproteins such as VLDL and IDL, has emerged as an independent risk factor for atherosclerotic cardiovascular disease (ASCVD) in both the general population and individuals with diabetes. Unlike LDL cholesterol, remnant cholesterol has not traditionally been a therapeutic target, despite growing evidence of its role in the pathophysiology of atherosclerosis. These particles exhibit high atherogenic and pro-inflammatory potential, and their metabolism is altered in states of insulin resistance and hepatic dysfunction, both common in diabetes. Epidemiological studies have shown its association with ischemic heart disease, peripheral artery disease, progression of nephropathy, and cardiovascular events in type 2 diabetes. In individuals with type 1 diabetes (T1D), the evidence is more recent but relevant: elevated levels of remnant cholesterol have been linked to persistent hyperglycemia, diabetic nephropathy, diabetic foot, subclinical myocardial dysfunction, and carotid atherosclerosis, even when LDL-C levels are within target range. Moreover, lifestyle factors such as physical activity and a healthy diet are associated with lower levels of remnant cholesterol, suggesting opportunities for non-pharmacological interventions. Despite this, treatments targeting remnant cholesterol have shown limited efficacy in reducing clinical events, and individuals with T1D remain underrepresented in clinical trials. Overall, this review highlights the need to incorporate remnant cholesterol into the assessment of residual cardiovascular risk and into personalized therapeutic strategies, especially for vulnerable populations such as those with T1D.
Full article
(This article belongs to the Section Lipid Metabolism and Cardiovascular Endocrinology)
►▼
Show Figures

Figure 1
Open AccessReview
When a Sellar Mass Is Not a Pituitary Adenoma: A Literature Review and Lessons from a Case of Pituicytoma
by
Maria Petersson and Charlotte Höybye
Endocrines 2025, 6(3), 45; https://doi.org/10.3390/endocrines6030045 - 10 Sep 2025
Abstract
Background: Pituicytomas are rare, low-grade gliomas arising from pituicytes in the posterior pituitary or infundibulum. Due to its rarity and nonspecific clinical and radiological characteristics, it is frequently misdiagnosed as pituitary adenomas or other sellar tumors. Aims: To present an overview of pituicytoma,
[...] Read more.
Background: Pituicytomas are rare, low-grade gliomas arising from pituicytes in the posterior pituitary or infundibulum. Due to its rarity and nonspecific clinical and radiological characteristics, it is frequently misdiagnosed as pituitary adenomas or other sellar tumors. Aims: To present an overview of pituicytoma, including clinical presentation, radiological and histopathological characteristics, differential diagnosis and treatment strategies, illustrated by a case report. Methods: A literature review was conducted to contextualize our patient with a sellar tumor, and to highlight key diagnostic and therapeutic considerations. Results/Case report: A 12-year-old boy presented with visual disturbances. MRI revealed a well-defined contrast-enhancing sellar mass, and the patient underwent transsphenoidal surgery. The diagnosis was assumed to be a nonfunctioning pituitary adenoma (NFPA). Two years later a residual tumor was treated with proton irradiation. Six years after the radiotherapy, the patient had epistaxis. Imaging showed a tumor in the sphenoidale sinus, which was surgically resected. The tumor had histopathological features of pituicytoma and immunoreactivity for TTF-1 and S100. The tissue from the first operation was reviewed, showing more characteristics with pituicytoma than NFPA, leading to re-definition of the initial diagnosis. Follow-up has been without any signs of residual tumor. Conclusion: Our case and literature review emphasize the importance of considering pituicytoma in the differential diagnosis among sellar lesions. The diagnosis relies on a combination of preoperative imaging, intraoperative findings and histopathology. Pituitary surgery is the first-line treatment, and the outcome is generally good. Increased awareness of pituicytomas is necessary to improve preoperative diagnostic accuracy and guide appropriate management.
Full article
(This article belongs to the Section Neuroendocrinology and Pituitary Disorders)
Open AccessArticle
Novel Anthropometric Indices: An Allometric Perspective
by
Nir Y. Krakauer and Jesse C. Krakauer
Endocrines 2025, 6(3), 44; https://doi.org/10.3390/endocrines6030044 - 4 Sep 2025
Cited by 3
Abstract
Background/Objectives: Anthropometric indices based on height (H), weight (W), waist circumference (WC) and hip circumference (HC) can identify incident and future health risks. While BMI provides a standard for relative W (adjusted for H), there is no standard for indices using WC
[...] Read more.
Background/Objectives: Anthropometric indices based on height (H), weight (W), waist circumference (WC) and hip circumference (HC) can identify incident and future health risks. While BMI provides a standard for relative W (adjusted for H), there is no standard for indices using WC and HC. A body shape index (ABSI) and hip index (HI) have been proposed to extend to respectively WC and HC the same allometric power-law approach used to derive BMI to be independent of H. Here, we compared the mutually independent allometric set H, BMI, ABSI, HI with other proposed indices. Methods: We examined the formulas and rationales of published indices, and used Third National Health and Nutrition Examination Survey (NHANES III) cohort data to investigate their inter-correlations and association with mortality. Results: Many of the proposed indices are based on geometric (isometric) similarity, which does not match human body variability patterns. Unlike ABSI and HI, most proposed indices showed large correlations with BMI, complicating interpretation when considered together with BMI. Indices’ association with mortality risk were generally consistent with their correlations with BMI and ABSI. Combining the separable mortality risks associated with BMI and ABSI, even in a simplified way, outperformed any single index. Conclusions: With calls for incorporating additional indices incorporating WC and HC to supplement BMI in defining obesity, only ABSI and HI are independent of BMI. Additionally, separate risk estimates from these allometric indices can be readily combined to optimize overall risk assessment.
Full article
(This article belongs to the Special Issue Feature Papers in Endocrines 2025)
►▼
Show Figures

Figure 1
Open AccessReview
Energy Homeostasis and Kisspeptin System, Roles of Exercise and Outcomes with a Focus on Male Reproductive Health
by
Mario Ruggiero, Antonella Vicidomini, Domenico Tafuri, Filomena Mazzeo and Rosaria Meccariello
Endocrines 2025, 6(3), 43; https://doi.org/10.3390/endocrines6030043 - 28 Aug 2025
Cited by 1
Abstract
►▼
Show Figures
Background: Obesity is a multisystemic health problem causing chronic diseases like diabetes or cardiovascular diseases, but also reproductive dysfunctions like infertility in adults or altered puberty onset in children. Exercise is a recognized intervention to control or prevent energy imbalance, thus deeply contributing
[...] Read more.
Background: Obesity is a multisystemic health problem causing chronic diseases like diabetes or cardiovascular diseases, but also reproductive dysfunctions like infertility in adults or altered puberty onset in children. Exercise is a recognized intervention to control or prevent energy imbalance, thus deeply contributing to metabolic health in physiological and pathological conditions. The kisspeptin system (KS), the main gatekeeper of reproduction and puberty onset in mammals, is also an upcoming “metabolic sensor”, linking energy homeostasis to reproductive ability both centrally and peripherally. Objectives: This narrative review aims at summarizing recent evidence from animal models and human studies on the role of the KS in energy homeostasis, with a focus on the upcoming role of the KS as a metabolic sensor able to modulate the functionality of the hypothalamus–pituitary–gonad axis in males as an adaptive response to exercise. Methods: PubMed and Scopus search (date: 2015–2025; keywords: kisspeptin and metabolism, male reproduction or exercise; kisspeptin and doping). Results and Conclusions: This review article illustrates the crucial role of the KS in linking energy homeostasis and male reproduction at the central and peripheral levels, and modulation of the KS by exercise in physiological and pathological conditions. Due to the large amount of data from animal models, knowledge gaps occur in the analysis of the relationship among KS, energy homeostasis, male reproduction and exercise in humans, particularly in the case of overtraining. Lastly, kisspeptin inclusion in the doping list is also discussed.
Full article

Figure 1
Highly Accessed Articles
Latest Books
E-Mail Alert
News
Topics
Topic in
Biomedicines, Diagnostics, Endocrines, JCM, JPM, IJMS
Development of Diagnosis and Treatment Modalities in Obstetrics and Gynecology
Topic Editors: Osamu Hiraike, Fuminori TaniguchiDeadline: 20 March 2026

Conferences
Special Issues
Special Issue in
Endocrines
Recent Advances in Type 1 Diabetes
Guest Editors: Marina Basina, Daniela FotiDeadline: 31 March 2026